Abstract
Objectives
The aim of this pilot study was to estimate the sample size for a large pragmatic study of the comparative effectiveness of electroacupuncture (EA) for low back pain (LBP) after back surgery.
Design
A randomised, active-controlled, assessor-blinded trial.
Participants
Patients with recurrent or persistent LBP, defined as a Visual Analogue Scale (VAS) score of ≥50 mm, with or without leg pain after back surgery.
Interventions
Patients were randomised to an EA plus usual care (UC) group or to a UC alone group at a 1:1 ratio. Patients assigned to each group received UC, including drug therapy, physical therapy and back pain education, twice a week for 4 weeks; those assigned to the EA plus UC group additionally received EA.
Outcome measures
The primary outcome was severity of LBP as measured by VAS. Secondary outcomes included back pain-related disability, assessed using the Oswestry Disability Index (ODI) and quality of life, assessed using the EuroQol Five Dimensions (EQ-5D) questionnaire. Statistical analysis was performed using paired and independent t-tests. A p value of <0.05 was considered statistically significant.
Results
Thirty-nine patients were allocated to receive EA plus UC (n=18) or UC alone (n=21). There was no statistically significant difference in VAS or EQ-5D scores between the two groups, but there was a significant decrease in ODI scores (p=0.0081). Using G*Power, it was calculated that 40 participants per group would be needed for a future trial according to VAS scores. Considering for a 25% dropout rate, 108 participants (54 per group) would be needed.
Conclusions
A future trial addressing the risk of bias and including the estimated sample size would allow for better clinical assessment of the benefits of EA plus UC in treatment of patients with non-acute pain after back surgery.
Trial registration number
Keywords: electroacupuncture, low back pain, back surgery, postoperative pain, integrative medicine, pilot trial
Strengths and limitations of this study.
This trial was designed as a feasible, comparative effectiveness trial which reflects common clinical situations.
Individualised acupuncture points according to patients’ symptoms during the delivery of acupuncture treatment reflect real-world clinical practice of acupuncture.
We expect that this pilot study will provide the clinical basis and information that is required to assess the feasibility of a future large-scale trial.
The size of the study sample of the current study limits the power of the observations.
Introduction
Low back pain (LBP) afflicts approximately 10% of people worldwide and is a source of considerable social and economic burden.1 Although there are a number of surgical options available to treat LBP,2 many people develop complications after lumbar spine surgery and some report that their symptoms are worse after surgery.3 The most common complication is LBP which occurs in about 40% of patients after back surgery.4 Therefore, management of postoperative pain is a very important component of patient care,5 and a wide range of treatments, including physical and/or cognitive-behavioural modalities, systemic or local pharmacological therapies, and neuraxial treatments, are used.6 Opioids, in particular morphine, hydromorphine and meperidine, are commonly used in the management of postoperative pain,7 but have significant side effects, including sedation, nausea, vomiting and itching.8 Therefore, a safe and effective method for management of pain after back surgery is required.
Several studies have shown that acupuncture is a safer9 10 and cost-effective11 treatment compared with usual care (UC) which comprises drug treatment and physical therapy,12 13 and that electroacupuncture (EA) is one of the most common strategies used for pain management.14–16 Therefore, EA could be a good method for treating pain after back surgery. There has been a systematic review of the evidence for acupuncture as a non-pharmacological strategy in treatment of acute postoperative pain after back surgery.17 However, very few clinical trials18 19 have assessed the effectiveness of EA for non-acute pain after back surgery, and the quality of the relevant research is too poor to reach any valid conclusions.
We have conducted a pilot study to compare the effectiveness of EA in combination with UC with that of UC alone in controlling non-acute pain and improving function at ≥3 weeks20 after back surgery. The primary purpose of this study was to estimate the appropriate sample size needed for a future confirmative, pragmatic, comparative randomised controlled trial (RCT) to determine the effectiveness of EA in combination with UC when compared with UC alone in relieving non-acute pain and dysfunction after back surgery. This research adhered to STandards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA)21 and CONsolidated Standards of Reporting Trials22 (CONSORT) guidelines.
Methods
Study design
This randomised, active-controlled, assessor-blinded, parallel-group pilot trial was conducted at Pusan National University Korean Medicine Hospital (PNUKH) in Yangsan, Korea between 26 September 2013 and 30 June 2015. Patients were recruited for the trial between 29 October 2013 and 18 September 2014. The details have been published in the study protocol.23 In addition to this trial on the effectiveness of EA for LBP after surgery, qualitative research and economic evaluations as conducted by other researchers were performed concurrently.
Participants
In accordance to the published protocol, the study investigators screened patients with LBP after back surgery for eligibility. Patients were eligible if they were aged 19–70 years and had LBP that had recurred or persisted for at least 3 weeks (non-acute) after back surgery, with or without leg pain, and required medical treatment. LBP was defined as a Visual Analogue Scale (VAS) score of ≥50 mm. Patients found to be eligible and willing to participate voluntarily in this study were guided through the consent process and signed informed consent forms. The exclusion criteria were as follows: serious disease that could cause LBP (eg, cancer, vertebral fracture, spinal infection, inflammatory spondylitis, cauda equina compression); chronic disease that could influence the effects or results of treatment (eg, severe cardiovascular disease, diabetic neuropathy, dementia or epilepsy); progressive neurological deficit or severe neurological symptoms; conditions inappropriate or unsafe for EA (eg, due to haemorrhagic disease, clotting disorder, history of having received anticoagulant therapy within the preceding 3 weeks, severe diabetes with risk of infection or severe cardiovascular disease); pain not caused by spinal or soft tissue disease, such as ankylosing spondylitis, fibromyalgia, rheumatoid arthritis or gout; pregnancy or planning to become pregnant; psychiatric disease; participation in another clinical trial; inability to provide written informed consent and ineligibility for inclusion in the study in the opinion of the investigators.
Sample size
We calculated the sample size of this pilot study which was estimated according to a previously published protocol,23 using the mean difference (20) and SD (19) derived from other similar studies. The number of subjects required for each group was 16. Considering a dropout rate of 20% and a 1:1 allocation ratio, the sample size was 40 in total (20 per arm).
Interventions
Patients randomised to both treatment groups received UC for 4 weeks. UC included drug therapy, physiotherapy and an educational programme on management of LBP, and excluded such Korean medicine treatments as acupuncture, moxibustion and cupping.20 Conventional drug treatment or therapies (eg, pain medication, injections; excluding surgical procedures) for LBP after back surgery were allowed and monitored. Physiotherapy and an educational programme on back care were undertaken twice a week for 4 weeks. Interferential current therapy (OG Giken, Okayama, Japan) was administered for 15 min with application of a hot (or ice) pack for 10 min. The structured education programme explaining the physiology, pathology and epidemiology of pain after back surgery was delivered in brochure format. Korean medical doctors also demonstrated postures and exercises suitable for management of LBP in a 15 min face-to-face education session.
Patients randomised to the EA plus UC group received EA in addition to UC. In this group, the acupuncture point prescriptions used were fixed acupuncture points plus points personalised to each patient and at the discretion of the practitioner. Differentiating the acupuncture point is an important part of traditional Korean medical theory and for reflecting actual clinical situation and was used to select acupuncture points according to each patient’s symptoms. Detailed information on the method of EA administration is summarised in the published protocol23 and is based on the revised STRICTA statement.21 EA treatment procedures were designed to reflect the feasibility afforded in the actual clinical setting by consensus of five experts on acupuncture and spinal disorders. EA was performed by licensed Korean medical doctors using disposable stainless steel needles 0.25 mm in diameter and 0.40 mm in length (Dongbang Acupuncture, Seongnam, Korea). Acupuncture points included Jia-ji (Ex-B2, L3-L5; bilaterally) as fixed points, and other reasonable points could be chosen as accessory points by the practitioner. Between 6 and 15 access points were used by the physicians according to the clinical features of each individual patient. Electric stimulation was applied using an ES-160 electronic stimulator (ITO, Tokyo, Japan) twice a week for 4 weeks. Stimulation was applied with a biphasic waveform current which is a compressional wave that combines an interrupted wave and a continuous wave, in triangular form at a frequency of 50 Hz,24 and was delivered via alligator clips connected to acupuncture needles inserted at Jia-ji (Ex-B2, L3/L5; bilaterally). Each EA session lasted 15 min. Patients in both groups received eight treatment sessions over the course of 4 weeks.
Outcome measures
At the initial screening visit, a clinical research coordinator asked all patients to complete a questionnaire regarding their sociodemographic characteristics, including age, sex, height and weight, and recorded their vital signs. Before the start of treatment at each visit, each patient was assessed to record the outcomes of the previous treatment session. All patients were followed up at 4 and 8 weeks after the 4-week treatment period.
The primary outcome of back pain intensity was assessed using a 100 mm pain VAS, on which 0 indicates absence of pain and 100 indicates unbearable pain.25 26 Each patient was asked to rate his or her degree of back pain during the previous 3 days on the VAS. Back pain was measured at baseline (assessment 1 at week 0) prior to each of the eight treatment sessions (assessments 2–9 at weeks 1–4), and at the two follow-up visits (assessments 10 and 11 at weeks 8 and 12). The primary endpoint was assessment 10 (week 8) which marked the end of the eight active treatment sessions. A responder was defined as a study participant with ≥50% pain relief using the 100 mm VAS for pain intensity at assessments 9, 10 and 11, and a non-responder as having pain relief of <50%, respectively (weeks 4, 8 and 12).
The secondary outcome measures were back pain-related disability, assessed using the Oswestry Disability Index (ODI), and quality of life, assessed by the EuroQol Five Dimensions (EQ-5D) questionnaire.27 The ODI contains 10 questions about daily life and includes measures of pain intensity, personal care, lifting, walking, sitting, standing, sleeping, social life and travelling. Each question is rated on a scale of 0 to 5, with a higher score indicating more severe pain-related disability. The validated Korean version of the ODI28 was administered before treatment at assessments 2, 5, 9,10 and 11 (weeks 1, 2, 4, 8 and 12). The validated Korean version of the EQ-5D29 30 includes generic questions about personal health-related quality of life and consists of five dimensions pertaining to mobility, self-care, usual daily activities, pain and discomfort, and anxiety/depression. Each dimension is scored on a scale of 1 to 3, with a lower score indicating a better state of health. The EQ-5D was administered before treatment assessments 2, 5, 9, 10 and 11 (weeks 1, 2, 4, 8 and 12).
Randomisation
Before the first treatment session, a statistician assigned patients to one of two groups by a central telephone randomisation procedure according to a computer-generated randomisation sequence using SPSS V.22.0 software (IBM). Randomisation was performed by a trial coordinator who had no contact with the patients. The clinical research coordinator obtained the codes for the trial (A or B) from the central telephone service and informed the EA practitioner. The practitioner used these codes to assign patients to one of the two groups and to deliver the appropriate treatment.
The National Clinical Research Center for Korean Medicine at PNUKH stored the random numbers. The allocation sequence was concealed from the researchers responsible for enrolling, treating and assessing patients by dividing their roles and contact with the study participants.
Blinding
It was impossible to blind either the patients or treating clinicians in this trial as the study design was pragmatic and comparative and not placebo controlled. However, the risk of detection bias was minimal because all treatments and assessments were conducted independently, and the treating clinicians were not involved in assessment of outcomes.31 The assessors, who received standardised training, always performed the outcome assessments in a separate room and were blinded to treatment assignment. However, there was provision in the study protocol for unblinding in exceptional circumstances where knowledge of the actual treatment would be essential for further management of the patient (eg, serious adverse event).
Statistical analysis
The statistical analysis was performed on both an intention-to-treat (ITT) and a per-protocol basis. For the ITT analysis, we applied the last-observation-carried-forward (LOCF) rule for missing data. The statistical significance of differences in the data for each group was analysed using the paired t-test, and the statistical significance of differences between groups was analysed using the independent t-test. Analysis of covariance was used to analyse and adjust the baseline characteristics if there were statistically significant differences and possibility of covariance of baseline characteristics. The χ2 test or Fisher’s exact test was used to analyse categorical data, such as responses/responders, and were recorded and described as frequencies (%). We did not perform an interim analysis as we expected EA and UC to be associated with a minimal risk of harm. All statistical analyses were performed by a statistician using SPSS for Windows V.22.0 software. The significance level was set at 5%.
The sample size required for a future trial will be estimated using the free G*Power V.3.1.7 program (Franz Faul, Christian-Albrechts-Universitätzu Kiel, Kiel, Germany) which calculates the sample size using mean difference and SD.
Patient and public involvement
The aim of this pilot study was to estimate the sample size for a large pragmatic study of the comparative effectiveness of EA with UC for LBP after back surgery. Therefore, patients and the public sector were not directly involved in the design of, recruitment to and conduct of this pilot study. We developed the research question, study design, outcome measures, patient recruitment and trial conduct methodology in light of the general Korean medical environment created as a result of its dual medical system of conventional and Korean medicine. As the choice of intervention reflects this medical environment, we did not view the intervention as burdensome and the burden of the intervention was not assessed by the patients themselves. The results of the qualitative research and economic evaluation which was conducted concurrently with this pilot study will be considered along with patient and public involvement in study design in the development process of a future trial. The results of this confirmative, pragmatic, comparative RCT will be disseminated in peer-reviewed journals and at academic conferences.
Results
Participants
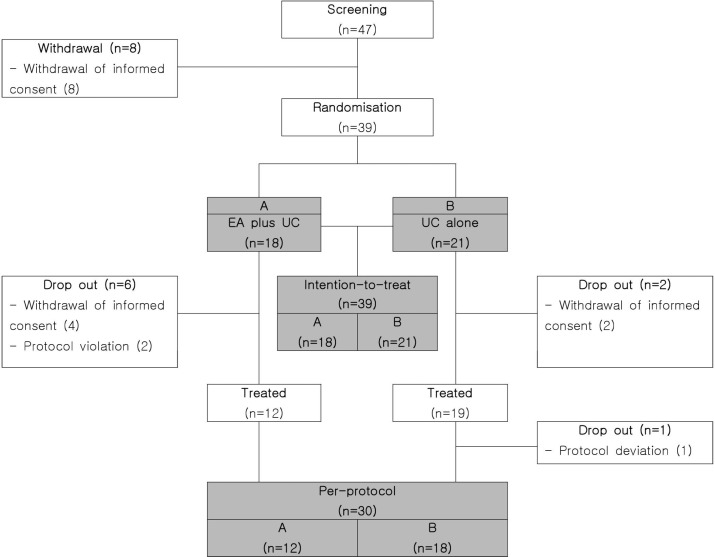
Forty-seven eligible patients agreed to participate in the trial after screening. Eight participants withdrew their informed consent before the start of treatment, leaving 39 patients who were randomly allocated to the two groups (18 in the EA plus UC group and 21 in the UC alone group). Eight of 39 patients dropped out during the treatment period due to withdrawal of informed consent or protocol violation (six in the EA plus UC group and two in the UC alone group). One more patient in UC alone group dropped out after treatment because of protocol deviation, leaving 30 patients (12 in the EA plus UC group and 18 in the UC alone group) for the per-protocol analysis (figure 1).
Figure 1.
Consolidated Standards of Reporting Trials flow diagram. EA, electroacupuncture; UC, usual care.
The mean (SD) age of the 39 treated patients was 57.6 (9.52) years, and 19 participants were men (48.7%). The detailed baseline demographic characteristics are provided in table 1. The mean scores on the VAS for non-acute back pain after surgery, and scores on the ODI and EQ-5D at the baseline evaluation are presented in table 2.
Table 1.
Demographic features of the participants at baseline
| Variables | Total | Group | |
| EA+UC (n=18) | UC alone (n=21) | ||
| Gender, n (%) | |||
| Male | 19 (48.7) | 9 (50.0) | 10 (47.6) |
| Female | 20 (51.3) | 9 (50.0) | 11 (52.4) |
| Age (years) | |||
| Mean±SD | 57.6±9.5 | 58.9±9.8 | 56.5±9.4 |
| Range | 37–70 | 40–70 | 37–70 |
| Height (cm) | |||
| Mean±SD | 164.1±9.8 | 163.0±9.0 | 165.1±10.6 |
| Range | 145–187 | 145–179 | 150–187 |
| Weight (kg) | |||
| Mean±SD | 66.9±9.8 | 67.1±9.5 | 67.1±9.5 |
| Range | 53–88 | 53–88 | 55–83 |
EA, electroacupuncture; UC, usual care.
Table 2.
Difference in primary and secondary results in the EA in combination with UC group and UC alone group between each evaluation and baseline
| Variables | Group | P values* | |
| EA+UC (n=18) | UC alone (n=21) | ||
| Mean±SD | Mean±SD | ||
| Mean (95% CI) | Mean (95% CI) | ||
| VAS (mm) | |||
| Baseline | 64.61±14.92 | 67.33±10.33 | |
| After 4 weeks | 51.78±20.62 | 60.24±19.25 | |
| Difference | −12.83 (−25.27 to 0.39) | −7.10 (−13.22 to –0.97) | 0.3919 |
| After 8 weeks | 41.50±24.75 | 58.24±20.83 | |
| Difference | −23.11 (-36.60 to 9.62) | −9.10 (−16.71 to –1.48) | 0.0675 |
| After 12 weeks | 41.78±24.62 | 53.00±21.39 | |
| Difference | −22.83 (−35.86 to 9.81) | −14.33 (−23.29 to –5.38) | 0.2553 |
| Responder (%(n)) | |||
| After 4 weeks | 22.2 (4) | 4.8 (1) | 0.1618† |
| After 8 weeks | 33.3 (6) | 9.5 (2) | 0.1123† |
| After 12 weeks | 38.9 (7) | 19.1 (4) | 0.1698‡ |
| ODI (%point) | |||
| Baseline | 44.70±15.42 | 38.23±14.5 | |
| After 4 weeks | 33.78±17.45 | 34.19±17.09 | |
| Difference | −10.93 (−15.92 to 5.94) | −4.04 (−7.59 to –0.5) | 0.021 |
| After 8 weeks | 31.95±18.57 | 32.47±16.04 | |
| Difference | −12.75 (−17.23 to 8.28) | −5.77 (−8.75 to –2.79) | 0.0081 |
| After 12 weeks | 29.67±18.46 | 28.60±16.69 | |
| Difference | −15.04 (−20.16 to 9.91) | −9.63 (−14.39 to –4.87) | 0.1137 |
| EQ-5D (point) | |||
| Baseline | 0.65±0.13 | 0.66±0.15 | |
| After 4 weeks | 0.71±0.11 | 0.72±0.14 | |
| Difference | 0.06 (0.01 to 0.12) | 0.05 (0.02 to 0.09) | 0.7698 |
| After 8 weeks | 0.74±0.15 | 0.73±0.13 | |
| Difference | 0.09 (0.02 to 0.16) | 0.06 (0.02 to 0.11) | 0.5151 |
| After 12 weeks | 0.73±0.17 | 0.74±0.13 | |
| Difference | 0.08 (0 to 0.17) | 0.08 (0.04 to 0.12) | 0.9441 |
*t-test for comparison of difference between groups.
†Fisher’s exact test for comparison of difference between groups.
‡χ2 test for comparison of difference between groups.
EA, electroacupuncture; EQ-5D, EuroQol Five Dimensions Questionnaire; ODI, Oswestry Disability Index; UC, usual care; VAS, Visual Analogue Scale.
Effects of EA
In both treatment groups, there were statistically significant improvements in VAS scores for back pain, and ODI and EQ-5D scores at 8 weeks compared with baseline (table 2). However, there were no statistically significant differences in the VAS score for back pain (p=0.0675) and in the EQ-5D (p=0.5151) score between the two treatment groups at 8 weeks (table 2). There was a statistically significant decrease in the ODI after 8 weeks in the EA plus UC group when compared with the UC alone group (p=0.0081; table 2). In the ITT analysis (n=39), the proportion of responders, defined as participants with ≥50% pain relief on the 100 mm VAS for pain intensity, was 33.3% (n=6) in the EA plus UC group (n=18) and 9.5% (n=2) in the UC alone group (n=21); the difference between the groups was not statistically significant (p=0.1123; table 2). No adverse events were reported in this study.
Estimating sample size of a future trial
On completion of this pilot study, we calculated an appropriately powered sample size that would be suitable for a larger RCT, based on the difference in change in VAS score between groups, with consideration of a 5% significance level, two-tailed, 80% powered test and t-test for comparison between groups. The mean difference (SD) in the VAS score for back pain between the EA plus UC group and the UC alone group was 14.02 (22.12) mm at the primary endpoint which was 8 weeks post-treatment initiation, based on ITT analysis. On this basis, using the G*Power program, 40 participants per group would be required. Allowing for a dropout rate of 25%, a total of 108 participants (54 per group) would need to be recruited.
Discussion
Many people suffer from LBP after back surgery and experience side effects from the opioids used to relieve their pain. Previous research has shown that patients treated with acupuncture or related techniques experience less pain and consequently use less opioids for pain control.32 Therefore, it may be carefully conjectured that EA, a type of acupuncture treatment commonly used by Korean medicine doctors, may be a good alternative as a non-pharmacological treatment without the risk of opioid-related side effects. EA is known to alleviate sensory symptoms and regulate components of pain through specific neuroscientific mechanisms and is thus used to decrease pain medication dosages.33 Also, as EA is often used for management of postoperative pain,34–37 we propose that a large-scale study is necessary to confirm the effectiveness of EA combined with UC, western conventional medicine treatment, as these treatments for postoperative pain reflect real-world circumstances and settings. We therefore undertook this pilot RCT to estimate the sample size for a full-scale randomised trial. Although the number of samples included in the analysis was insufficient to confirm the effect of treatment as it was roughly estimated a priori, we focused on analysing the approximate validity and calculating the sample size needed for a future trial.
From the results of this pilot study, we determined the basis needed in carrying out a full-scale RCT. Although there was no statistically significant difference between the two groups in VAS, between-group difference in changes in ODI, which assesses back pain-related disability, was significant (p=0.0081) and favoured EA plus UC therapy in terms of functional improvement in the lumbar spine. Given the clinical reality that it is difficult to expect functional improvement without relief of pain, our basis for a full-scale RCT seems reasonable.
The observed change in VAS scores in the EA plus UC group (23.11) is greater than the minimum clinically important difference value (22.50 in LBP) reported in a previous study,38 and the mean difference (14.02) and SD (22.12) of the two groups indicate a medium-sized effect, justifying the need for a larger scale follow-up study.
The pilot study was underpowered, the sample size being based on the mean difference (20) and SD (19) derived from other similar studies. However, those studies differed from our trial in terms of patients, methods of treatment and study design. It follows that the sample size for our future RCT based on a similar protocol to the pilot study should be calculated using our observed parameters so that a future study would be conservatively powered for a meaningful effect.
These preliminary findings, although limited with several limitations as mentioned above, confirm the need to proceed with future pragmatic RCTs comparing the effectiveness of EA with UC with that of UC alone for treatment of non-acute pain after back surgery. However, there are several considerations to be taken into account before proceeding with larger RCTs. First, for cultural reasons, most participants in such studies would have had acupuncture experience in countries such as Korea which would act as a limiting factor in efficacy of acupuncture-related treatment, and the reason why many clinical trials using acupuncture, or related techniques such as EA, are often considered to have high risk of bias.39 40 Also, the three main outcome measures were all patient-reported outcomes. This can serve as a limitation regarding subjective outcome measurement although we used assessor blinding to offset this limitation as much as possible. Therefore, treatment, assessment and statistical analysis should be performed independently in future trials to prevent detection bias.
Further, there were many dropouts in this pilot trial, and it is necessary to find an appropriate method of overcoming this problem. Especially in order to overcome potential problems related to withdrawal of consent before the start of treatment, such methods as adjusting the timing of randomisation or initiation of treatment may be considered in following trials. In addition to the LOCF rule, it is also necessary to consider an appropriate method for handling missing data such as multiple imputation. Also, inclusion of a patient-satisfaction survey in future trials may help shed light on this high dropout rate.
In an effort to reflect real-world situations, only western medical treatments such as drug treatment excluding surgery or injection therapy were allowed during the treatment period. In many professional conferences, it was difficult to completely rule out medication when considering the realistic aspects of pain management. Also, as this pilot trial was a pragmatic comparative effectiveness RCT, we tried to reflect real-world conditions in current clinical status too. We therefore permitted drug therapy in UC to reflect current use of medication. In addition, subgroup analyses based on diagnosis, type of surgery and duration of pain, which could not be confirmed in the present study due to limitations in data collection, should be conducted in future trials by means of structured questionnaires.
A future trial that addresses the above-mentioned concerns and covers the estimated sample size will be better equipped for clinical assessment of the benefits of EA in combination with UC in the treatment of patients with non-acute pain after back surgery. In addition, qualitative research and economic evaluation will be conducted in future trials using evaluation tools supplemented through pilot study results. The results of a follow-up trial are expected to establish a robust clinical basis for the effects of acupuncture combined with electrical stimulation in this patient population.
Supplementary Material
Acknowledgments
The authors are grateful to the patients with pain after back surgery who participated in this pilot trial.
Footnotes
Contributors: All authors conceived and designed the trial by discussion. IH wrote the manuscript. M-SH, E-HH, J-HC and I-HH helped to conceive and design the trial. B-CS as the principal investigator conceived the trial and revised the manuscript. IH and M-SH recruited the patients and conducted the trial. N-KK acted as an economic evaluation expert and clinical trial expert. D-WS was involved as a neurosurgical expert. K-MS and J-HL supervised the trial. All authors read and approved the final manuscript.
Funding: This research was supported by a grant from the Korea Institute of Oriental Medicine (K14273).
Disclaimer: The funding source had no role in the design of this study or in its execution, analyses, interpretation of the data or decision to submit the results for publication.
Competing interests: None declared.
Patient consent: Obtained.
Ethics approval: The protocol was approved by the Institutional Review Board at Pusan National University Korean Medicine Hospital in September 2013 (approval number 2013012).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Data may be requested from the corresponding author and made available to researchers who meet the criteria for access to confidential patient data according to the Institutional Review Board of Pusan National University Korean Medicine Hospital.
References
- 1. Hoy D, March L, Brooks P, et al. Measuring the global burden of low back pain. Best Pract Res Clin Rheumatol 2010;24:155–65. 10.1016/j.berh.2009.11.002 [DOI] [PubMed] [Google Scholar]
- 2. Sarrazin JL. [Imaging of postoperative lumbar spine]. J Radiol 2003;84(2 Pt 2):241–52. [PubMed] [Google Scholar]
- 3. Herrera Herrera I, Moreno de la Presa R, González Gutiérrez R, et al. Evaluation of the postoperative lumbar spine. Radiologia 2013;55:12–23. 10.1016/j.rxeng.2011.12.002 [DOI] [PubMed] [Google Scholar]
- 4. Aghion D, Chopra P, Oyelese AA. Failed back syndrome. Med Health R I 2012;95:391–3. [PubMed] [Google Scholar]
- 5. Skolasky RL, Wegener ST, Maggard AM, et al. The impact of reduction of pain after lumbar spine surgery: the relationship between changes in pain and physical function and disability. Spine 2014;39:1426–32. 10.1097/BRS.0000000000000428 [DOI] [PubMed] [Google Scholar]
- 6. Chou R, Gordon DB, de Leon-Casasola OA, et al. Management of Postoperative Pain: A Clinical Practice Guideline From the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists' Committee on Regional Anesthesia, Executive Committee, and Administrative Council. J Pain 2016;17:131–57. 10.1016/j.jpain.2015.12.008 [DOI] [PubMed] [Google Scholar]
- 7. Hutchison RW, Chon EH, Tucker WF, et al. A Comparison of a fentanyl, morphine, and hydromorphone patient-controlled intravenous delivery for acute postoperative analgesia: a multicenter study of opioid-induced adverse reactions. Hosp Pharm 2006;41:659–63. 10.1310/hpj4107-659 [DOI] [Google Scholar]
- 8. Benyamin R, Trescot AM, Datta S, et al. Opioid complications and side effects. Pain Physician 2008;11(2 Suppl):S105–20. [PubMed] [Google Scholar]
- 9. White A, Hayhoe S, Hart A, et al. Survey of adverse events following acupuncture (SAFA): a prospective study of 32,000 consultations. Acupunct Med 2001;19:84–92. 10.1136/aim.19.2.84 [DOI] [PubMed] [Google Scholar]
- 10. Wheway J, Agbabiaka TB, Ernst E. Patient safety incidents from acupuncture treatments: a review of reports to the National Patient Safety Agency. Int J Risk Saf Med 2012;24:163–9. 10.3233/JRS-2012-0569 [DOI] [PubMed] [Google Scholar]
- 11. Lin CW, Haas M, Maher CG, et al. Cost-effectiveness of guideline-endorsed treatments for low back pain: a systematic review. Eur Spine J 2011;20:1024–38. 10.1007/s00586-010-1676-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lee JH, Choi TY, Lee MS, et al. Acupuncture for acute low back pain: a systematic review. Clin J Pain 2013;29:172–85. 10.1097/AJP.0b013e31824909f9 [DOI] [PubMed] [Google Scholar]
- 13. Shin JS, Ha IH, Lee J, et al. Effects of motion style acupuncture treatment in acute low back pain patients with severe disability: a multicenter, randomized, controlled, comparative effectiveness trial. Pain 2013;154:1030–7. 10.1016/j.pain.2013.03.013 [DOI] [PubMed] [Google Scholar]
- 14. Casimiro L, Barnsley L, Brosseau L, et al. Acupuncture and electroacupuncture for the treatment of rheumatoid arthritis. Cochrane Database Syst Rev 2005;4:CD003788 10.1002/14651858.CD003788.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Zhao XB, Xing QZ, Han XC. [Observation on electroacupuncture at neimadian (extra) and neiguan (PC 6) for analgesia after thoracic surgery]. Zhongguo Zhen Jiu 2013;33:829–32. [PubMed] [Google Scholar]
- 16. Chia KL. Electroacupuncture treatment of acute low back pain: unlikely to be a placebo response. Acupunct Med 2014;32:354–5. 10.1136/acupmed-2014-010582 [DOI] [PubMed] [Google Scholar]
- 17. Cho YH, Kim CK, Heo KH, et al. Acupuncture for acute postoperative pain after back surgery: a systematic review and meta-analysis of randomized controlled trials. Pain Pract 2015;15:279–91. 10.1111/papr.12208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Huang HT, Zheng SH, Feng J, et al. Thin’s abdominal acupuncture for treatment of failed back surgery syndrome in 20 cases of clinical observation. Guid J Trad Chin Med Pharm 2012;18:63–5. [Google Scholar]
- 19. Zheng SH, Yt W, Liao JR, et al. Abdominal acupuncture treatment of failed back surgery syndrome clinical observation]. J EmergTrad Chin Med 2010;19:1497–8. [Google Scholar]
- 20. National Guideline Clearinghouse. Low Back Disorders. Rockville, MD: Agency for Healthcare Research and Quality (AHRQ), 2011. http://www.guideline.gov/content.aspx?id=38438 [Google Scholar]
- 21. MacPherson H, Altman DG, Hammerschlag R, et al. Revised STandards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA): Extending the CONSORT statement. J Evid Based Med 2010;3:140–55. 10.1111/j.1756-5391.2010.01086.x [DOI] [PubMed] [Google Scholar]
- 22. Moher D, Hopewell S, Schulz KF, et al. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. Int J Surg 2012;10:28–55. 10.1016/j.ijsu.2011.10.001 [DOI] [PubMed] [Google Scholar]
- 23. Hwang MS, Heo KH, Cho HW, et al. Electroacupuncture as a complement to usual care for patients with non-acute pain after back surgery: a study protocol for a pilot randomised controlled trial. BMJ Open 2015;5:e007031 10.1136/bmjopen-2014-007031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Jung YP, Jung HK, Chiang SY, et al. The clinical study of electroacupuncture treatment at Hua-Tuo-Jia-Ji-Xue on spondylolisthesis. The Journal of Korean Acupuncture & Moxibustion Society 2008;25:221–32. [Google Scholar]
- 25. Revill SI, Robinson JO, Rosen M, et al. The reliability of a linear analogue for evaluating pain. Anaesthesia 1976;31:1191–8. 10.1111/j.1365-2044.1976.tb11971.x [DOI] [PubMed] [Google Scholar]
- 26. Carlsson AM. Assessment of chronic pain. I. Aspects of the reliability and validity of the visual analogue scale. Pain 1983;16:87–101. 10.1016/0304-3959(83)90088-X [DOI] [PubMed] [Google Scholar]
- 27. Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine 2000;25:2940–53. 10.1097/00007632-200011150-00017 [DOI] [PubMed] [Google Scholar]
- 28. Jeon CH, Kim DJ, Kim SK, et al. Validation in the cross-cultural adaptation of the Korean version of the Oswestry Disability Index. J Korean Med Sci 2006;21:1092–7. 10.3346/jkms.2006.21.6.1092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Rabin R, de Charro F. EQ-5D: a measure of health status from the EuroQol Group. Ann Med 2001;33:337–43. 10.3109/07853890109002087 [DOI] [PubMed] [Google Scholar]
- 30. Kang EJ, Shin SH, Park HJ, et al. A validation of health status using EQ-5D. The Korean Journal of Health Economics and Policy 2006;12:19–43. [Google Scholar]
- 31. Higgins J, Green S. Cochrane Collaboration. Cochrane Handbook for Systematic Reviews of Interventions. Chichester, UK: Wiley-Blackwell, 2008. [Google Scholar]
- 32. Wu MS, Chen KH, Chen IF, et al. The efficacy of acupuncture in post-operative pain management: a systematic review and meta-analysis. PLoS One 2016;11:e0150367 10.1371/journal.pone.0150367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Zhang R, Lao L, Ren K, et al. Mechanisms of acupuncture-electroacupuncture on persistent pain. Anesthesiology 2014;120:482–503. 10.1097/ALN.0000000000000101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Chi H, Zhou WX, Wu YY, et al. [Electroacupuncture intervention combined with general anesthesia for 80 cases of heart valve replacement surgery under cardiopulmonary bypass]. Zhen Ci Yan Jiu 2014;39:1–6. [PubMed] [Google Scholar]
- 35. Wu J, Zhao Y, Yang CM, et al. [Effects of electroacupuncture preemptive intervention on postoperative pain of mixed hemorrhoids]. Zhongguo Zhen Jiu 2014;34:279–83. [PubMed] [Google Scholar]
- 36. Zhang H, Wang L, Zhang M, et al. [Effects of electroacupuncture on postoperative functional recovery in patients with gynaecological laparoscopic surgery]. Zhongguo Zhen Jiu 2014;34:273–8. [PubMed] [Google Scholar]
- 37. Zhang Z, Wang C, Li Q, et al. Electroacupuncture at ST36 accelerates the recovery of gastrointestinal motility after colorectal surgery: a randomised controlled trial. Acupunct Med 2014;32:223–6. 10.1136/acupmed-2013-010490 [DOI] [PubMed] [Google Scholar]
- 38. Park KB, Shin J-S, Lee J, et al. Minimum Clinically Important Difference and Substantial Clinical Benefit in Pain, Functional, and Quality of Life Scales in Failed Back Surgery Syndrome Patients. Spine 2017;42:E474–E481. 10.1097/BRS.0000000000001950 [DOI] [PubMed] [Google Scholar]
- 39. Kim SI, Lee KB, Lee HS, et al. Acupuncture experience in patients with chronic low back pain(2): a qualitative study - focused on participants in randomized controlled trial. Korean J Acupunct 2012;29:581–97. [Google Scholar]
- 40. Lee H, Bang H, Kim Y, et al. Non-penetrating sham needle, is it an adequate sham control in acupuncture research? Complement Ther Med 2011;19 Suppl 1:S41–S48. 10.1016/j.ctim.2010.12.002 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.