Abstract
Introduction
A new rehabilitative approach, called UPper Limb Children Action Observation Training (UPCAT), based on the principles of action observation training (AOT), has provided promising results for upper limb rehabilitation in children with unilateral cerebral palsy (UCP). This study will investigate if a new information and communication technology platform, named Tele-UPCAT, is able to deliver AOT in a home setting and will test its efficacy on children and young people with UCP.
Methods and analysis
A randomised, allocation concealed (waitlist control) and evaluator-blinded clinical trial with two investigative arms will be carried out. The experimental group will perform AOT at home for 3 weeks using a customised Tele-UPCAT system where they will watch video sequences of goal-directed actions and then complete the motor training of the same actions. The control group will receive usual care for 3 weeks, which may include upper limb training. They will be offered AOT at home after 3 weeks. Twenty-four children with UCP will be recruited for 12 participants per group. The primary outcome will be measured using Assisting Hand Assessment. The Melbourne Assessment 2, ABILHAND, Participation and Environment Measure-Children and Youth and Cerebral Palsy Quality of Life Questionnaire will be included as secondary measures. Quantitative measures from sensorised objects and participants worn Actigraphs GXT3+ will be analysed. The assessment points will be the week before (T0) and after (T1) the period of AOT/standard care. Further assessments will be at T1 plus, the week after the AOT period for the waitlist group and at 8 weeks (T2) and 24 weeks (T3) after AOT training.
Ethics and dissemination
The trial has been approved by the Tuscany Paediatric Ethics Committee (169/2016). Publication of all outcomes will be in peer-reviewed journals and conference presentations.
Trial registration
Keywords: action observation training, unilateral cerebral palsy, tele-rehabilitation, upper limb, randomized controlled trial, information and communication technologies
Strengths and limitations of this study.
This is the first protocol study where an information and communication technology platform is proposed, called Tele-UPCAT, to deliver the action observation training (AOT) at home.
The study is a well-designed randomised controlled trial aimed to investigate the UPper Limb Children Action Observation Training (UPCAT) approach at home and to measure its efficacy in children, adolescents and young adults with unilateral cerebral palsy.
The Tele-UPCAT platform allows individualised customisation of the intervention according to the different levels of upper limb severity and the different ages of participants.
The sample size, even if it will be calculated and powered on the previous clinical studies, is modest.
The Tele-UPCAT platform does not obtain quantitative measurements of force and pressure hand measurements during AOT session.
Background
Cerebral palsy (CP) is the most common cause of childhood chronic physical disability in Europe and in other industrialised societies.1 The incident rate is between 2 and 3 per 1000 live births and increases to 40–100 per 1000 live births among very premature and very low birthweight babies, which represent the population with highest rate of neurodevelopmental disorders.2 Unilateral cerebral palsy (UCP) (ie, a motor impairment impacting one side of the body more than the other side) constitutes the most frequent form of CP, about 30%–40% of all affected children.3 Recent estimations of incidence and prevalence of CP have shown a significant increase in UCP in Europe over the last years.4 5 The upper limb (UL) of children with UCP is generally more involved than the lower limb, and the consequent disability affects their participation, quality of life, independence at home, school and community. Despite this large impact, the current clinical practice for UCP mainly includes consultative intervention or time-limited therapy following pharmacological intervention.
In the last decades, targeted UL therapies such as constraint-induced movement therapy, hand–arm bimanual intensive training and combined approaches have emerged. Reviews on these models have clearly shown that intensive models of therapy achieves modest to strong effects to improve UL function compared with standard care (SC) and that bimanual and unimanual training demonstrate similar gains in UL outcomes.6–10
In this field, one of the most recent models is the action observation training (AOT), based on the discovery of the Mirror Neuron System, whose core regions are the ventral premotor and inferior parietal cortex. These areas are activated when individuals perform goal-directed motor acts (eg, grasping an object) as well as if they simply observe the performance of the same or a similar action and trigger recruitment of the same network as the actual physical action.11 12 AOT is mainly based on observation of meaningful actions, and their successive imitation. AOT has been used as new intervention model in many adult studies for neurological and non-neurological diseases (such as Parkinson’s disease, stroke and orthopaedic surgery), and there is growing evidence of its effectiveness.13–18 Recent studies carried out in children with CP indicate positive effects on UL function in younger population.19–21 We have recently completed a clinical study called UPper Limb Children Action observation Training (UPCAT) with children with UCP based on 3 weeks of AOT, providing evidence of its efficacy in improving UL activity performance in daily activities.21 To date, the UPCAT study has only been carried out in a clinical rehabilitation setting with children who were living near the two clinical centres and whose parents are willing to commit to a 3-week intensive therapy programme with consequently high costs for both health services and families. In addition, the parents, even if able to participate, found the need to attend every working day for 3 weeks too burdensome and suggested the delivery of the intervention at home.
Biotechnologies, telerehabilitation and eHealth provide a promising approach to deliver telemonitored home programmes for a large number of participants at a relatively low cost. In this field, our group has recently experienced the design, the build and the clinical validation of new technological information and communication technologies (ICT) for providing in the first year of life telerehabilitation programmes at home for infants at risk for developing neurodevelopmental disorders22–25 In this context, similar approaches could represent viable option in providing AOT programmes at home, in a user-friendly, playful and rehabilitative setting in children. The core of AOT relies on the content of actions to be observed and on the patients’ motivation in carefully observing to imitate and actively replicate them. For these reasons, the AOT can be easily carried out at home. The present study protocol, designed as an exploratory randomised controlled trial (RCT), has the purpose to investigate the feasibility of a new ICT platform, named Tele-UPCAT, to provide the UPCAT approach at home. This RCT aims to measure its efficacy in a group of children, adolescents and young adults with UCP comparing the effects of Tele-UPCAT approach (experimental group) with the SC (control group).
The primary aim will evaluate the immediate effects (T1, in the week after the end of the treatment) of this new approach (home AOT) on bimanual hand function (Assisting Hand Assessment (AHA)26–28) and assess whether these effects will be retained at a medium-term and long-term follow-up (ie, 8 weeks and 24 weeks after the end of treatment, T2 and T3). In addition, the feasibility of the Tele-UPCAT system as a comfortable, reliable and customisable tool for delivering a home AOT to UCP participants and their families will be assessed using semistructured interviews.
Secondary aims will investigate the immediate (T1) and long-term clinical effects (T2 and T3) on unimanual capacity (Melbourne Assessment 2 (MA 2)29 and Box and Block Test (BBT)30) and on bimanual daily activities at home and in the community (ABILHAND-Kids31), participation (Participation and Environment Measure – Children and Youth (PEM-CY))32 33 and perception of quality of life (Cerebral Palsy Quality of Life Questionnaire (CP-QOL)).34–36 Further aims will assess the feasibility of Tele-UPCAT platform on assessing, monitoring and detecting changes during and after the AOT programme by comparing the data of the clinical outcome measures with those of quantitative measurement of manual activity, obtained using sensorised objects and Tele-UPCAT platform. Finally, a cost-effective analysis will be carried out using both the perspective of the patient/caregivers and the healthcare system.
Methods/design
Study design
The Tele-UPCAT trial is an exploratory randomised, allocation concealed (waitlist controlled) and evaluator-blinded clinical trial with two investigative arms using an AOT intensive rehabilitation programme of home-based AOT compared with SC in children and young people with UCP. This study is a waitlist-controlled trial, in order to allow all enrolled participants to perform AOT either immediately or after a waitlist period. After obtaining informed consent and completing baseline assessment (T0), participants will be block randomised into pairs according to the House functional classification system (HFCS) activity level (grades 2–3, 4–5 and 6–8) and age (5–14 years and 15–20 years),37 38 using a computer-generated set of random numbers. Randomisation, sequence generation and preparation of group allocation materials will be carried out by an independent researcher who will be not involved in the trial. Pairs will be divided randomly into two groups with 1:1 experimental/SC (waitlist) ratio. Participants allocated in the experimental group will immediately start AOT for a 3-week period, while those in the SC group will continue with their usual care.
A predefined diary for recording all daily activities (eg, times of sleep, weak-up, meals, school, therapies for UL or for lower limb and their dose) will be filled in by all the participants and their parents. In addition, to record the acceptability and feasibility of the training, participants and/or families allocated in the experimental group will fill in a multiple choice questionnaire (with box for notes) for ascertaining the perception about their experiences of using the Tele-UPCAT system.
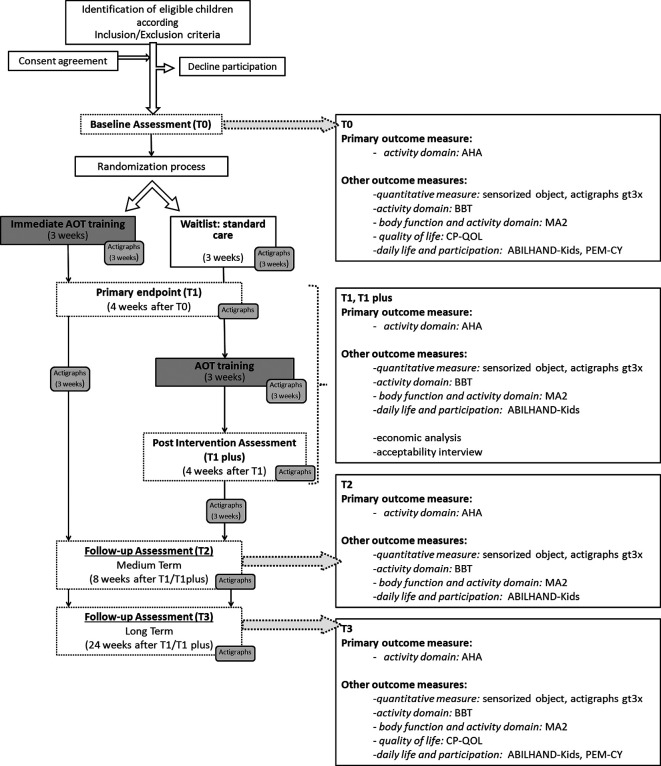
All participants will be re-evaluated after the period of experimental training/SC (T1) with standardised tests and questionnaires (see outcome measures). T1 will be the primary endpoint aimed at evaluating the short-term effects of AOT according to Consolidated Standards of Reporting Trials (CONSORT) guidelines (see figure 1).39
Figure 1.
Flow chart of Tele-UPCAT study according to CONSORT guidelines. AHA, Assisting Hand Assessment; AOT, action observation training; BBT, Box and Block Test; CP-QOL, Cerebral Palsy Quality of Life; CONSORT, Consolidated Standards of Reporting Trials; MA 2, Melbourne Assessment 2; PEM-CY, Participation and Environment Measure – Children and Youth.
After this phase, participants previously allocated to the experimental group will continue SC, while who started with SC will then commence home-based AOT. The participants of this SC group will be reassessed at the end of training (T1 plus). Further assessment of all participants will be performed after 8 weeks (T2) and 24 weeks (T3) from the end of AOT training (T1 or T1 plus, for the experimental and waitlist group, respectively), to evaluate the medium-term and long-term effects of AOT. All the assessments will be carried out at home by trained therapists.
In summary, assessments will be performed at:
T0, baseline: the week before the period of AOT/SC.
T1: at 1 week after period of AOT/SC.
T1 plus: the week after period of AOT, for waitlist group.
T2: 8 weeks after end of AOT.
T3: 24 weeks after end of AOT.
The details of the study design are reported according to CONSORT guidelines39 (figure 1), Standard Protocol Items: Recommendations for Intervention Trials (SPIRIT) statement40 and Template for Intervention Description and Replication (TIDier) Checklist41 42 (online supplementary materials 1, 2 and 3). The programme of enrolment, interventions and assessments designed according to SPIRIT guidelines are shown in figure 2.
Figure 2.
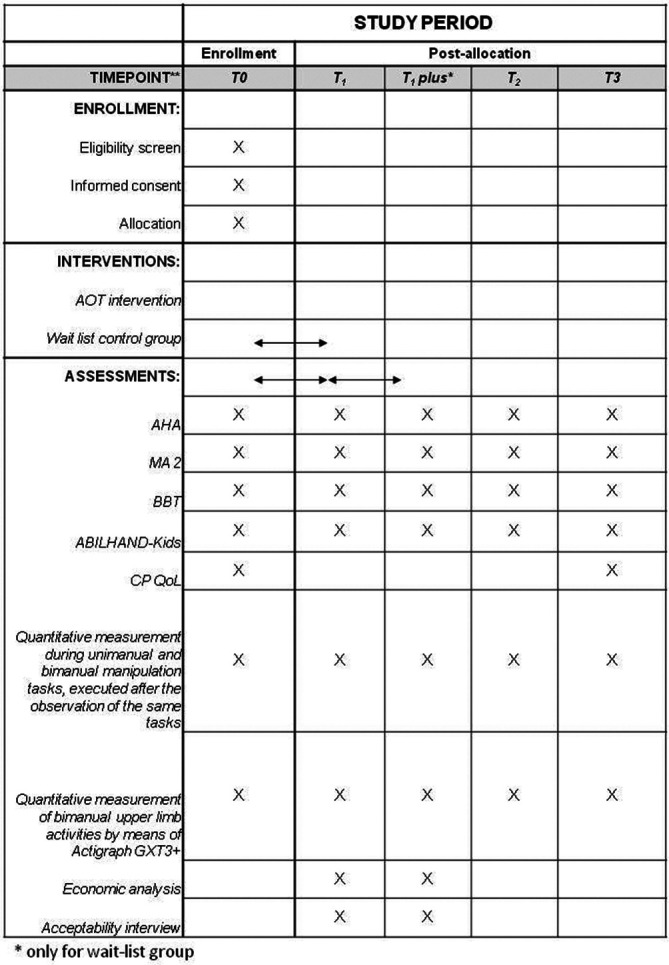
Schedule of enrolment, interventions and assessments. AHA, Assisting Hand Assessment; AOT, action observation training; BBT, Box and Block Test; CP-QOL, Cerebral Palsy Quality of Life Questionnaire; MA 2, Melbourne Assessment 2.
Blinding
All the clinical outcome measures (AHA,26–28 MA-229 and BBT30) will be videotaped by a therapist blind to group assignment. Videotapes will be randomised and scored by assessors blind to group allocation and order of assessments. During each assessment, all the participants will wear two Actigraphs (wGT3X-BT and wActiSleep-BT), one for each wrist.
Two independent researchers (two paediatric neurologists) without competing interests will comprise the data monitoring committee for this study. They will review all adverse events (deciding to stop the trial if necessary), the retention of participant in each study arm and the compliance of study protocol at 12-weekly intervals. Each participant will have a study number in a dedicated data file. The file with participant’s numbers and personal data will be stored in a password-protected file, accessible only by the principal investigator. In order to promote participant’s retention, all the assessment will be completed at home. The clinical primary and secondary outcome measures will be completed within 1 week. Enrolled participants are ethically able to withdraw from this study any time and have been notified that their usual follow-up and clinical care would not be impacted.
Study sample and recruitment
Enrolment and clinical trial management will be carried out by paediatric neurologists and physiatrists at the Department of Developmental Neuroscience of IRCCS Fondazione Stella Maris (FSM, Pisa, Italy), with the collaboration of the Unit of Children Rehabilitation of S. Maria Nuova Hospital (Reggio Emilia, Italy).
Potential participants will be identified according to inclusion criteria (see below), from UCP patients of the clinical departments. Suitable participants and their parents will be invited to participate and will be enrolled in the RCT only after written consent has been obtained.
Inclusion criteria are participants with:
Confirmed diagnosis of spastic motor type UCP.3 43
Aged between 5 years and 20 years at time of recruitment.
Predominant UL spasticity.
HFCS score ≥2, that is, able to passively hold an object in the hand or better.37 38
Cognitive level within normal limits, that is, IQ ≥70, as assessed in the last year prior to recruitment on the Wechsler Preschool and Primary Scale of Intelligence-Third Edition (WPPSI-III),44 Wechsler Intelligence Scale for Children Fourth Edition (WISC-IV)45 or Wechsler Adult Intelligence Scale (WAIS).46
Participants and parents willing to commit to the intensive therapy programme for a 3-week period.
Participants will be excluded in case of:
Previous orthopaedic surgery or botulinum toxin A (BoNT-A) injection in the UL within 6 months prior to the enrolment of this study.
Sample size
Even if this study will be planned as an exploratory study, a sample size estimates, according to CONSORT guidelines,38 40 have been based on projected treatment effect on the primary outcome measure, AHA. Taking account of the study design and the stratification, a minimum sample size of 10 per group will be required in order to detect a 1.40 effect size (value based on our preliminary data) at significant level of 0.05% and 80% power.20 21 Considering a 20% of possible drop-outs, a minimum of 12 participants per group will be recruited, with a total sample of 24 participants.
Study treatment
The Tele-UPCAT system has been designed through the close collaboration between the rehabilitation staff (child neurologists and child therapists) of IRCCS Fondazione Stella Maris and biomedical engineers of BioRobotics Institute Scuola Superiore Sant’Anna. Taking into account the previous clinical experience on UPCAT, the main components of the Tele-UPCAT system (eg, the size of the screen, the need of a guide for alternating the time of observation and of execution and the key words for catching the attention), the AOT library of exercises (eg, the adaptation of the objects for enlarging the exercises to more impaired hands) and the experimental training (eg, time and duration) have been defined. In general, the training will be structured in one session per day to be executed five working days for three consecutive weeks (ie, 15 sessions in total). The duration of daily sessions will be about 1 hour per day for a total of 15 hours. The participants undergoing the AOT intervention through the Tele-UPCAT system will watch 3 min first-person video sequences of unimanual or bimanual goal-directed actions followed by their execution for 3 min. Three different actions will be proposed twice each day.
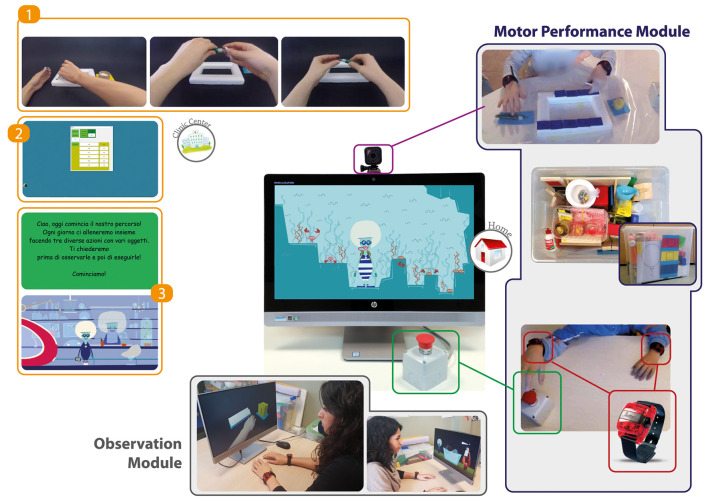
Tele-UPCAT system
Tele-UPCAT system (see figure 3) has been designed and built and will be provided at home by the BioRobotics Institute of Scuola Superiore Sant’Anna (Pontedera, Italy).
Figure 3.
Tele-UPCAT platform. Set-up of the Tele-UPCAT platform for delivering the AOT at home. It includes an observation module for the presentation of AOT videos (1) selected in the clinical interface (2) by the clinical staff in relation to HFCS level (6–8, 4–5 or 2–3), side of impaired hand and type of interface. A dedicated software, aimed at guiding and motivating subjects to perform AOT, is also provided with age-related features (3) for teenagers or little boys and girls. The motor performance module for the execution of actions is composed of a kit of common objects and toys, identical to those shown in the videos and a couple of Actigraphs (wGT3X-BT and wActiSleep-BT) worn on both wrists and a button. The integrated camera records subject’s attention during the observation task and exercise execution. AOT, action observation training; HFCS, House functional classification system.
It is a platform for delivering AOT designed to be user-friendly, by subjects at home in a playful setting with integrated smart features.
The platform has been designed and developed by integrating two different modules:
The observation module (OM) for the presentation of AOT videos and recording of participant’s attention and exercise execution. This consists of a computer with 23′ desktop, a dedicated software and a video camera. The OM has been obtained by integrating a large all-in-one personal computer (All-in-One touch HP Elite One 800 G2 - L3N93AV), a large switch and a video camera (GoPro HERO Session), which will record a whole field, including subject’s face and hands and table with objects. The OM is important to determine whether the participant is looking at the monitor during observation phase and has an overall view of the execution of actions. A dedicated software, designed after a deep and specific literature analysis, was developed for guiding and motivating participants through the phases of AOT (observation followed by execution). In addition, the software was customised for the wide age range of participants providing an interactive game with an engaging story different for every day of training for school-aged children, and a slideshow with a voiceover for adolescents and young people. The general architecture of the software is based on the following sequence: observation of a 3 min video followed by execution of the same action for 3 min. Subsequently, the same video will be replayed and then executed a second time. As stated before, a 60 min session, including rest intervals, of three different goal-directed actions of increasing complexity are observed and imitated twice every day. At the end of each day, the software will terminate the session and automatically update it for the next day.
The motor performance module (MPM) for the execution of actions. This will be mainly composed of a kit of exactly the same common objects and toys shown in the videos and two Actigraphs (wGT3X-BT and wActiSleep-BT; for more details, see http://actigraphcorp.com/support/activity-monitors/gt3x/) worn one for each wrist. With this design, it will be possible to measure the UL activity during the AOT, while the lack of sensorised toys embedded in the MPM will not allow to measure quantitative measures of hand activity (eg, force or pressure) during the AOT.
The first prototype of Tele-UPCAT system has been widely tested before the beginning of the RCT in order to test the stability and reliability of the system.
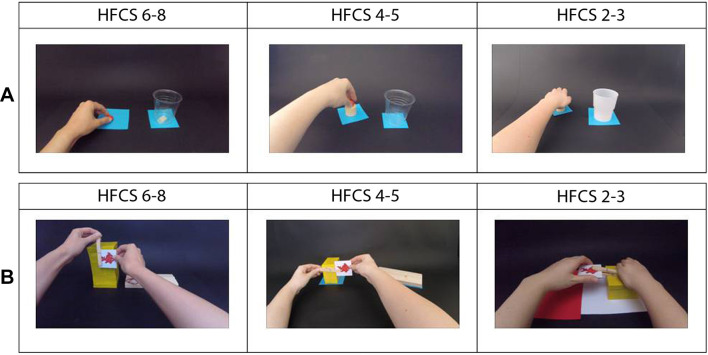
AOT library
On the basis of the previous AOT exercises,20 21 rehabilitation staff (child neurologist and child therapists) has created a library of rehabilitation packages composed of three different series of AOT exercises suitable to be executed at home. They differ for complexity of action and range of UL capabilities conceived in relation to HFCS levels (≤4, 5–6 and 7–8).37 38 Each series is organised into customised sequences designed to cover unimanual and bimanual UL goal-directed actions with a variety of objects and toys commonly used in routine life. For each series, experimental training is composed of 15 sets (eight unimanual followed by seven bimanual) of routine UL activities, to be completed in 3 weeks (5 days per week). Each set has a general common goal (eg, drinking a glass of water) composed of three sequential tasks of increasing complexity (eg, from picking up a bottle of water, to opening the cap, to pouring the water into a glass). As previously indicated, in order to grade the activities according to the range of capabilities, three series of sets have been planned. The actions of each series have the same goal, but the material and type of movement (ie, range of movement and type of grasp) are customised in order to guarantee feasibility of the proposed activity while maintaining the same overall objective (see table 1 and figure 4). Each action of the three series performed by an actor is videotaped so that the videos show only the hand and arm from the first perspective; each video is then edited to last 3 min. A right-handed actor uses one or two hands for unimanual and bimanual exercises, respectively, for participants with right UCP. For the left UCP, the previous videos were reversed if they maintained the same characteristic of the setting and of the hand movement, while the remaining videos were specifically videotaped.
Table 1.
List of goal-directed actions planned for the AOT training grouped in unimanual (days 1-8) and bimanual (days 9-15) actions
| Days | Action A | Action B | Action C |
| 1 | Uncover a little ball by lifting a box. | Place a little ball in a glass. | Fill a glass with water. |
| 2 | Pick coloured card and match it to the same colour. | Move a coloured card and place it on a base. | Pick a card and place it on the similar one. |
| 3 | Pick up a rubber stamp and move from/to different positions. | Pick up a rubber stamp and press it against horizontal plane to print a figure. | Pick up a rubber stamp and press it against sloping plane to print a figure. |
| 4 | Pick up coin, put it in piggy bank through the slot on the top
or pick up a magnet and place it on a horizontal magnetic board. |
Pick up coin, put it in piggy bank through the vertical slot on
the side or pick up a magnet and place it on a sloping magnetic board. |
Pick up coin, put it in piggy bank through the horizontal slot on
the side or pick up a magnet and place it on a vertical magnetic board. |
| 5 | Pick up a wooden rubber stamp and move to different positions. | Pick up a wooden rubber stamp and press it against horizontal plane to print a figure. | Pick up a wooden rubber stamp and press it against sloping plane to print a figure. |
| 6 | Move a spray can or move the bottle with a little ball inside. |
Place the spray can on a support or remove a little ball from the bottle. |
Put the spray can into a cup or press the catapult and launch a little ball. |
| 7 | Move a container filled with shimmy powder. | Open the container. | Sprinkle shimmery powder on a paper. |
| 8 | Place magnetic fish on a paper. | Pick up fishing rod and catch magnetic fish. | Pick up magnetic fish and place them in a container. |
| 9 | Move a hole punch. | Insert a sheet of paper and make holes. | Match holes on sticks. |
| 10 | Wet a cloth placing it in a container with water. | Wring cloth and place it in a plate. | Open a toy washing machine and insert the cloth inside. |
| 11 | Pick up a card and place it on a support. | Pick up a card and insert it in a clothespin. | Pick up a card and insert it in a clothespin in a different orientation. |
| 12 | Pick up and handle a piece of Play-Doh. | Divide it in two pieces. | Open a toy oven and insert a saucepan (with Play-Doh in it). |
| 13 | Search for coin in the bag and place it on a support. | Take the coin and insert it in a wallet. | Open a box and place the wallet inside. |
| 14 | Open a tube of tempera paint. | Wet a brush with tempera paint. | Make figure using a stencil with the brush dipped in tempera paint. |
| 15 | Move a glitter glue tube. | Open it. | Decorate a frame by pasting pieces of mosaic. |
AOT, action observation training.
Figure 4.
(A) Example of the unimanual action B of day 1 for the left hand, with a different pattern of movement, based on subject HFCS level, maintaining the same goal. (B) Example of the bimanual action B of day 11 for the right hand, with a different pattern of movement, based on subject HFCS level, maintaining the same goal. HFCS, House functional classification system.
Experimental training
Before delivering the Tele-UPCAT platform, the training will be customised individually for each participant. The rehabilitation staff will select, on the basis of age and HFCS level, from the library the most appropriated AOT rehabilitation packages for each participant, then the engineers will upload them in the OM. For the MPM, the therapists will organise a container of all the objects identifying them with numbers relative to the training day (eg, little ball number 1, which means day 1 of the training). In addition, a dedicated printed manual with instructions and guidelines related to the different steps of the training and for system management, and the setup will be provided. The manual contains also all the contacts of both technical and rehabilitation staff for remote assistance in case of any problems during the training. Two Actigraphs (wGT3X-BT, wActiSleep-BT) will be initialised for the recording period (3 weeks) to be worn on each wrist.
The ICT platform will be delivered to the participant’s home by the engineers that are in charge of the installation of the system. The families will identify a designated position with a table or a desk of about 80×100 cm near to a socket where the ICT platform will be placed. Engineers and rehabilitation staff will train both parents and participants about the correct use of the system, including safety aspects. During the first two training days, a therapist will visit each participant and their parents to confirm the set-up.
During the training sessions, each participant will sit on a chair with both arms placed on a table in front of a platform positioned at about 1 m. Especially when the participant will be a child, a parent will be seated on his or her more impaired side to prompt attention during task execution and assist if necessary. The software will guide the participant in the sequence of observations and executions.
Standard care
Participants previously allocated in the SC group will continue their usual care for 3 weeks. Usual care for recruited participants could be consisted for physical or occupational therapy.
The frequency, dose and the type of all therapies will be recorded accurately by a diary in both groups.
Outcome measures
Description of sample
Children participating in the study will be classified according to HFCS, which assesses function of the impaired hand in children with CP.37 38 This classification consists of nine grades ranging from a hand that is not used at all (grade 0) to one that is used spontaneously and independently from the other one (grade 8). Due to the general approach in classifying hand functional level, this scale can also be easily applied to young adults with UCP. HFCS will be used for all ages as a criterion for inclusion in this study (from grade 2 to grade 8). In addition, they will be classified according to the Manual Ability Classification System, a classification system of the child’s ability to handle objects in daily activities on one of five levels.47
Primary outcome measure
On the basis of our scientific hypothesis and according to previous clinical experience,20 21 the primary outcome measure will be the AHA. The latest version 5.0 will be used. This assessment measures UL function during bimanual activities by evaluating spontaneous use of assisting hand during a semistructured age-appropriated 10–15 min session with specific toys or objects requiring bimanual handling. The school-kids form will be used for the assessment of UCP children aged 6–12 years,26 27 while the adolescent version (Ad-AHA), using the board game ‘Go with the Floe’,28 will be completed with participants older than 13 years. This last version, even if validated up to 18 years, will be used with potential participants aged 18–20 years to guarantee the same assessment across all participants regardless of age. Moreover, AHA has been already used, even if not validated, in young people with UCP.48 49 The scale uses a Rasch measurement model, which is a method to convert raw scores into a linear measure located on a unidimensional scale and more specifically to convert them into 0–100 logit-based AHA units, which will be used for the statistical analyses. All AHA assessments will be videotaped in a standardised manner, and the subsequent scoring will be carried out by a certified expert rater who will be masked to group allocation and assessment order.26–28
Other outcome measures
Other secondary measures will include measures of unimanual capacity (MA-229 and BBT30) and bimanual daily activities at home and in the community (ABILHAND-Kids).31 Moreover, participation and quality of life will also be assessed. All assessment will be performed at T0, T1, T1 plus, T2 and T3 unless otherwise indicated. Questionnaires will be completed by parents and/or participants at home and if doubts will occur, child neurologists or therapists will be available to discuss face to face items not clear to them.
The MA 229 measures unilateral UL function, and it is a valid and reliable tool for evaluating quality of UL movement in children with neurological conditions for ages between 2.5 years and 15 years. MA 2 is a criterion-referenced test that extends and refines the scale properties of the original Melbourne Unilateral Upper Limb assessment (MUUL), and like MUUL, it can also be used for adolescents and young adults. MA 2 measures four elements of UL movement quality: movement range, accuracy, dexterity and fluency. It comprises 14 test items of reaching, grasping, releasing and manipulating simple objects. The test is administered by videorecording the child’s performance for subsequent scoring (30 items score). A raw score is provided for each of the four sections (movement range, accuracy, dexterity and fluency) that will be analysed separately. It predominantly includes concepts within the body function domain as well as in the activity domain. Even if the MUUL and also the MA 2 have been validated up to 15 years, the first one has been used in studies involving patients with CP older than 15 year and in adults.48 49 We have chosen to use the MA 2 also for participants older than 15 years to guarantee the same assessment across all participants regardless of age instead of using other scales (eg, the Fugl-Meyer Assessment or the Action Research Arm test).50
BBT is a quick (2–5 min), simple and inexpensive test, which measures unimanual dexterity in the activity domain. BBT is composed of a test box with a partition in the middle and 150 wooden blocks (25 mm). The patient had to transport as many blocks as possible in 1 min from one compartment to another. First, the patient is asked to perform the test with the unaffected hand and then with the affected hand. The number of blocks transported by affected hand in 1 min will be counted and considered for the main analyses. It can be used for a wide range of populations from childhood to adulthood.30
ABILHAND-Kids31 is a semistructured item-response questionnaire on a three-point ordinal scale (impossible, difficult and easy) that measures daily manual activities referred to in the activity domain of International Classification of Functioning, Disability and Health (ICF). Parents will be instructed to rate their child’s perceived difficulty in performing each activity, taking account the performance of their child when performing the activity without technical or human assistance, regardless of the limb(s) and the strategies used. It has been validate for children aged 6–15 years, but it has been used for larger ranges (6–19 years).51 The questionnaire has been developed using the Rasch measurement model, which provides a method to convert the ordinal raw scores into a linear logit measures located on a unidimensional scale that will be used for the analyses. This questionnaire will be used at all assessment periods.
PEM-CY32 33 is a parent-reported instrument that evaluates participation and environment across home (10 items), school (5 items) and community (10 items) settings. For each item, the parent is asked to identify how frequent (over the past 4 months) the child has participated (eight options: daily to never); how involved the child typically is while participating (five-point scale: very involved to minimally involved); and whether the parent would like to see the child’s participation in this type of activity change (no or yes, with five options for the type of change desired). For each setting, the parent is then asked to report on whether certain features of the environment make it easier or harder for the child to participate. The following summary scores will be obtained: total score and score for each of the three setting-specific environmental supportiveness (home, school and community). Moreover, the total number of supports and the total number of barriers will be computed. This questionnaire will be used at T0 and T3.
CP-QOL – Child, 4–12 years and CP QOL – Teen, 13–18 years evaluate quality of life in children and adolescents with CP.34–36 A score on a 0–100 scale will be obtained for each of computed subdomains. In particular, the Children form filled in by the parents assesses seven subdomains (social well-being and acceptance, feelings about functioning, participation and physical health, emotional well-being and self-esteem, access to services, pain and impact of disability and family health) and five subdomains (excluding access to services and family health to the previous) for the children version. The Teen form evaluates seven subdomains (general well-being and participation, communication and physical health, school well-being, social well-being, access to services, family health and feeling about functioning) for the form filled in by the parents and five subdomains (excluding Access to services and Family health to the previous) for those filled in by the caregivers. These questionnaires will be used at T0 and T3.
Quantitative measurement during unimanual and bimanual manipulation tasks, executed after the observation of the same tasks, is a new assessment tool that consists of observation, followed by execution of three tasks of increasing difficulty (unimanual lifting, bimanual placing near and bimanual cooperation, holding and pulling) by means of a sensorised object. New technological tools such as sensorised objects can help in assessing the manipulation capabilities (reaching and grasping) in a quantitative but ecological way and the sensitivity to a training. Previous studies of the authors were focused on the development of sensorised toys for measuring infant’s manipulation.52–54 Starting from these experiences, a new sensorised object has been designed and developed by the engineers tuning the sensors sensitivity and working range to the needs of participants with UCP. Two load cells and a switch embedded in the sensorissed object allow for the measurement of the following parameters: grasping time, maximum grasping force and delay time between unaffected and affected hand in reaching for the object. This set-up is out of Tele-UPCAT system even if it was designed and developed in parallel.
Quantitative measurement of bimanual activities will be performed in all the participants enrolled in the study by means of Actigraph GXT3+, as components of MPM of Tele-UPCAT system. Actigraphs wGT3X-BT and wActiSleep-BT, equipped with a Velcro strap bracelet, will be worn, one for each wrists. As a general rule, the experimental group have to wear the Actigraphs during the training sessions and between T0 and T1 and between T1 and T2 (total 6 weeks, 24 hours per day or as much as possible), while the control group is requested to wear them between T0 and T1, between T1 and T1 plus and, if possible, also between T1 plus and T2 (total 9 weeks, 24 hours per day or as much as possible). All the daily activities, experimental training or usual care or removal will be recorded in a dedicated diary. The Actigraphs will also be worn by all the participants during each time point of clinical assessments with the outcome measures. Data will be mainly relative to the asymmetry index, which is the difference between the mean activity of the dominant with those of the non-dominant hand, and it will be correlated with the clinical scores obtained in the clinical outcome measures (mainly AHA).
Cost effectiveness: a within-trial cost–utility analysis will be conducted to synthesise the costs and benefits of the training programme. Resource use (staff time, equipment and facility use) associated with the programme will be collected alongside the RCT. Healthcare utilisation will be collected using a resource use questionnaire previously used in CP studies.55 Health utility will be derived from the adapted Child Health Utility instrument (CHU-9D),56 a quality of life measure designed specifically for economic evaluation and which has been validated in an Australian population.57–59
A semiguided face-to-face interview (online supplementary material 4) about the acceptability of the training will be completed immediately after the training period (T1 or T1 plus). It will be performed by the rehabilitation staff with the aim of investigating participants’ and parents’ opinions about the training. It will explore the customisation of exercises, suitability to UCP children, feasibility at home, required effort by the participants and acceptability of Actigraphs, suitability of the manual and of the software.
bmjopen-2017-017819supp004.pdf (48.7KB, pdf)
Statistical analyses
Clinical data will be analysed by means of the Statistical Package for Social Sciences (SPSS). Means and SD of clinical outcome scores for both groups will be calculated to identify potential baseline differences between groups. As a first step, normality of distributions will be verified by Shapiro-Wilk’s test. Between-group differences for all selected outcome measures will be evaluated at T0, by means of t-test for unrelated samples or non-parametric Mann-Whitney U independent sample test for normal or non-normal distributed data, respectively. To test our first hypothesis, an intention-to-treat analysis will be carried out, evaluating between-group differences (delta scores) for primary and secondary outcome measures at the primary endpoint (T1), compared with T0 (T1-T0), by means of parametric or non-parametric tests for unrelated samples. The age, HFCS level, characteristics of usual care (in both groups), supervision of caregiver and acceptability of therapy (measured by semistructured interview) will be analysed for further secondary exploratory analyses (eg, regression modelling) in order to determine if some of these variables are predictive of better responses to the Tele-UPCAT training. In addition, a matched-pairs test (t-tests or Wilcoxon) will be carried out in order to assess retention of effects at follow-up periods (T1 or T1 plus, T2 and T3) relative to assessment before AOT training (T0 or T1 for experimental or waitlist group, respectively). Bonferroni corrections will not be carried out in relation to the exploratory nature of the current RCT study and the relative small number of the study sample. To detect if significant changes will correlate to HFCS levels, a correlation analysis between score changes after AOT training (T1 or T1 plus) and assessment before AOT training (T0 or T1) will be carried out. Finally, an exploratory within-group analysis will be performed for the waitlist group comparing changes during AOT with respect to those of the first SC period.
Ethics and dissemination
This study protocol describes background, hypotheses, system, clinical and technological outcome measures for a RCT designed to evaluate the Tele-UPCAT system as a new approach to deliver AOT to children and young people with UCP at home.
Any deviations from the protocol will be promptly notified to the ethics committee and applied only after its approval. The trial has been registered at http://www.clinicaltrials.gov (identifier NCT03094455). This study protocol is reported according to the SPIRIT statement (SPIRIT 2013)40 and the TIDier guidelines.41 42 We anticipate that the results of this study will be disseminated through peer-reviewed journals and national and international academic conferences only by the professionals directly involved in the clinical trial. The results of this study will be of interest for rehabilitation trials based on AOT paradigm. Referring to a previous RCT study,20 21 we suggest that the home setting might increase accessibility of rehabilitation to a large number of children and young people with UCP (eg, participants that live far from the clinical centres) with a large range of hand impairments (including also participants with HFCS level lower than 6) and older age (5–20 years instead of 5–15 years). Moreover, if the Tele-UPCAT study, using a very simple ICT solution, demonstrates to be viable for delivering AOT at home with significant improvements in UL daily activities, it could lead to the application of new solution for cost-efficient rehabilitation programmes. Implementation of new smart technologies can (1) provide user-friendly AOT programmes at home; (2) remotely manage treatment by rehabilitation staff, thus increasing the ratio ‘number of patients per therapist’; and (3) offer individualised and intensive training. It could become an economical and efficient rehabilitation programme by achieving significant long-lasting effects in UL activity and participation through an easily implementable paradigm that could become an integral part of common clinical practice. Finally, this approach could become a rehabilitation tool and be applicable to broader populations of CP and other chronic disabilities.
Project status
This project began recruitment on 29 March 2017, and we expect to complete data collection for the last training in November 2017 and close the project in April 2018.
bmjopen-2017-017819supp001.pdf (231.3KB, pdf)
bmjopen-2017-017819supp002.pdf (3.9MB, pdf)
bmjopen-2017-017819supp003.pdf (48.7KB, pdf)
Supplementary Material
Acknowledgments
We would like to acknowledge the contribution of Valentina Menici (paediatric PT), and Irene Braito, MD, for video and material collection, Siresia Bagnoli and Marco Zemolin for the design and the interface storyboard and Vincent Corsentino for English reviewing.
Footnotes
Contributors: GS is the principal investigator of the project and mainly responsible of the clinical part of it, while FC is the main responsible of the ICT platform. GS, EI, HF, KK, RNB, AF and GC designed the research study. GS, EB, EI, SP and ES were responsible for the AOT library. GS, SP and ES were in charge for participants’ recruitment in Pisa and identification of type of exercise and software and AF for Reggio Emilia. GS and EB will collect the data and will monitor the training. FC, IM, MM and FPF with the supervision of PD have designed and built the new platform. GS and GC will take the lead roles on preparation of publications on the clinical outcomes of the study. All authors have read and approved the final manuscript.
Funding: This trial has been funded by the Italian Ministry of Health to GS and FC (GR-2011-02350053).
Competing interests: None declared.
Patient consent: Not required.
Ethics approval: Tuscany Paediatric Ethics Committee (169/2016).
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Krägeloh-Mann I, Cans C. Cerebral palsy update. Brain Dev 2009;31:537–44. 10.1016/j.braindev.2009.03.009 [DOI] [PubMed] [Google Scholar]
- 2.Surveillance of Cerebral Palsy in Europe. Surveillance of cerebral palsy in Europe: a collaboration of cerebral palsy surveys and registers. Surveillance of Cerebral Palsy in Europe (SCPE). Dev Med Child Neurol 2000;42:816–24. [DOI] [PubMed] [Google Scholar]
- 3.Cioni G, Sgandurra G, Muzzini S, et al. Forms of hemiplegia. : Ferrari A, Cioni G, . The spastic forms of cerebral palsy. A guide to the assessment of adaptive functions. Milan, Italy: Springer-Verlag, 2009:331–53. [Google Scholar]
- 4.Andersen GL, Romundstad P, De La Cruz J, et al. Cerebral palsy among children born moderately preterm or at moderately low birthweight between 1980 and 1998: a European register-based study. Dev Med Child Neurol 2011;53:913–9. 10.1111/j.1469-8749.2011.04079.x [DOI] [PubMed] [Google Scholar]
- 5.Himmelmann K, Uvebrant P. The panorama of cerebral palsy in Sweden. XI. Changing patterns in the birth-year period 2003-2006. Acta Paediatr 2014;103:618–24. 10.1111/apa.12614 [DOI] [PubMed] [Google Scholar]
- 6.Chiu HC, Ada L. Constraint-induced movement therapy improves upper limb activity and participation in hemiplegic cerebral palsy: a systematic review. J Physiother 2016;62:130–7. 10.1016/j.jphys.2016.05.013 [DOI] [PubMed] [Google Scholar]
- 7.Sakzewski L, Ziviani J, Boyd R. Systematic review and meta-analysis of therapeutic management of upper-limb dysfunction in children with congenital hemiplegia. Pediatrics 2009;123:e1111–e1122. 10.1542/peds.2008-3335 [DOI] [PubMed] [Google Scholar]
- 8.Sakzewski L, Ziviani J, Boyd RN. Efficacy of upper limb therapies for unilateral cerebral palsy: a meta-analysis. Pediatrics 2014;133:e175–e204. 10.1542/peds.2013-0675 [DOI] [PubMed] [Google Scholar]
- 9.Inguaggiato E, Sgandurra G, Perazza S, et al. Brain reorganization following intervention in children with congenital hemiplegia: a systematic review. Neural Plast 2013;2013:1–8. 10.1155/2013/356275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ferrari A, Maoret AR, Muzzini S, et al. A randomized trial of upper limb botulimun toxin versus placebo injection, combined with physiotherapy, in children with hemiplegia. Res Dev Disabil 2014;35:2505–13. 10.1016/j.ridd.2014.06.001 [DOI] [PubMed] [Google Scholar]
- 11.Fabbri-Destro M, Rizzolatti G. Mirror neurons and mirror systems in monkeys and humans. Physiology 2008;23:171–9. 10.1152/physiol.00004.2008 [DOI] [PubMed] [Google Scholar]
- 12.Gallese V, Fadiga L, Fogassi L, et al. Action recognition in the premotor cortex. Brain 1996;119(Pt 2):593–609. 10.1093/brain/119.2.593 [DOI] [PubMed] [Google Scholar]
- 13.Ertelt D, Small S, Solodkin A, et al. Action observation has a positive impact on rehabilitation of motor deficits after stroke. Neuroimage 2007;36 Suppl 2(Suppl 2):T164–T173. 10.1016/j.neuroimage.2007.03.043 [DOI] [PubMed] [Google Scholar]
- 14.Franceschini M, Agosti M, Cantagallo A, et al. Mirror neurons: action observation treatment as a tool in stroke rehabilitation. Eur J Phys Rehabil Med 2010;46:1–7. [PubMed] [Google Scholar]
- 15.Alegre M, Rodríguez-Oroz MC, Valencia M, et al. Changes in subthalamic activity during movement observation in Parkinson’s disease: is the mirror system mirrored in the basal ganglia? Clin Neurophysiol 2010;121:414–25. 10.1016/j.clinph.2009.11.013 [DOI] [PubMed] [Google Scholar]
- 16.Pelosin E, Bove M, Ruggeri P, et al. Reduction of bradykinesia of finger movements by a single session of action observation in Parkinson disease. Neurorehabil Neural Repair 2013;27:552–60. 10.1177/1545968312471905 [DOI] [PubMed] [Google Scholar]
- 17.Bellelli G, Buccino G, Bernardini B, et al. Action observation treatment improves recovery of postsurgical orthopedic patients: evidence for a top-down effect? Arch Phys Med Rehabil 2010;91:1489–94. 10.1016/j.apmr.2010.07.013 [DOI] [PubMed] [Google Scholar]
- 18.Caligiore D, Mustile M, Spalletta G, et al. Action observation and motor imagery for rehabilitation in Parkinson’s disease: A systematic review and an integrative hypothesis. Neurosci Biobehav Rev 2017;72:210–22. 10.1016/j.neubiorev.2016.11.005 [DOI] [PubMed] [Google Scholar]
- 19.Buccino G, Arisi D, Gough P, et al. Improving upper limb motor functions through action observation treatment: a pilot study in children with cerebral palsy. Dev Med Child Neurol 2012;54:822–8. 10.1111/j.1469-8749.2012.04334.x [DOI] [PubMed] [Google Scholar]
- 20.Sgandurra G, Ferrari A, Cossu G, et al. Upper limb children action-observation training (UP-CAT): a randomised controlled trial in hemiplegic cerebral palsy. BMC Neurol 2011;11:80. 10.1186/1471-2377-11-80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sgandurra G, Ferrari A, Cossu G, et al. Randomized trial of observation and execution of upper extremity actions versus action alone in children with unilateral cerebral palsy. Neurorehabil Neural Repair 2013;27:808–15. 10.1177/1545968313497101 [DOI] [PubMed] [Google Scholar]
- 22.Sgandurra G, Lorentzen J, Inguaggiato E, et al. Effects of home-based early intervention with CareToy system in preterm infants: a Randomized Clinical Trial study. PlosOne 2017;22;12:e0173521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sgandurra G, Bartalena L, Cecchi F, et al. CareToy Consortium. A pilot study on early home-based intervention through an intelligent baby gym (CareToy) in preterm infants. Res Dev Disabil 2016;53-54:32–42. 10.1016/j.ridd.2016.01.013 [DOI] [PubMed] [Google Scholar]
- 24.Sgandurra G, Bartalena L, Cioni G, et al. CareToy Consortium. Home-based, early intervention with mechatronic toys for preterm infants at risk of neurodevelopmental disorders (CARETOY): a RCT protocol. BMC Pediatr 2014;14:268. 10.1186/1471-2431-14-268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rihar A, Sgandurra G, Beani E, et al. CareToy: Stimulation and assessment of preterm infant’s activity using a novel sensorized system. Ann Biomed Eng 2016;44:3593–605. 10.1007/s10439-016-1669-4 [DOI] [PubMed] [Google Scholar]
- 26.Krumlinde-sundholm L, Eliasson A-christin. Development of the assisting hand assessment: a rasch-built measure intended for children with unilateral upper limb impairments. Scand J Occup Ther 2003;10:16–26. 10.1080/11038120310004529 [DOI] [Google Scholar]
- 27.Krumlinde-Sundholm L, Holmefur M, Kottorp A, et al. The assisting hand assessment: current evidence of validity, reliability, and responsiveness to change. Dev Med Child Neurol 2007;49:259–64. 10.1111/j.1469-8749.2007.00259.x [DOI] [PubMed] [Google Scholar]
- 28.Louwers A, Beelen A, Holmefur M, et al. Development of the Assisting Hand Assessment for adolescents (Ad-AHA) and validation of the AHA from 18 months to 18 years. Dev Med Child Neurol 2016;58:1303–9. 10.1111/dmcn.13168 [DOI] [PubMed] [Google Scholar]
- 29.Randall M, Imms C, Carey LM, et al. Rasch analysis of the melbourne assessment of unilateral upper limb function. Dev Med Child Neurol 2014;56:665–72. 10.1111/dmcn.12391 [DOI] [PubMed] [Google Scholar]
- 30.Mathiowetz V, Federman S, Wiemer D. Box and block test of manual dexterity: norms for 6–19 year olds. Canadian Journal of Occupational Therapy 1985;52:241–5. 10.1177/000841748505200505 [DOI] [Google Scholar]
- 31.Arnould C, Penta M, Renders A, et al. ABILHAND-Kids: a measure of manual ability in children with cerebral palsy. Neurology 2004;63:1045–52. [DOI] [PubMed] [Google Scholar]
- 32.Coster W, Bedell G, Law M, et al. Psychometric evaluation of the Participation and Environment Measure for Children and Youth. Dev Med Child Neurol 2011;53:1030–7. 10.1111/j.1469-8749.2011.04094.x [DOI] [PubMed] [Google Scholar]
- 33.Khetani M, Marley J, Baker M, et al. Validity of the Participation and Environment Measure for Children and Youth (PEM-CY) for Health Impact Assessment (HIA) in sustainable development projects. Disabil Health J 2014;7:226–35. 10.1016/j.dhjo.2013.11.003 [DOI] [PubMed] [Google Scholar]
- 34.Waters E, Davis E, Mackinnon A, et al. Psychometric properties of the quality of life questionnaire for children with CP. Dev Med Child Neurol 2007;49:49–55. 10.1017/S0012162207000126.x [DOI] [PubMed] [Google Scholar]
- 35.Davis E, Shelly A, Waters E, et al. Quality of life of adolescents with cerebral palsy: perspectives of adolescents and parents. Dev Med Child Neurol 2009;51:193–9. 10.1111/j.1469-8749.2008.03194.x [DOI] [PubMed] [Google Scholar]
- 36.Carlon S, Shields N, Yong K, et al. A systematic review of the psychometric properties of Quality of Life measures for school aged children with cerebral palsy. BMC Pediatr 2010;10:81. 10.1186/1471-2431-10-81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.House JH, Gwathmey FW, Fidler MO. A dynamic approach to the thumb in- palm deformity in cerebral palsy: evaluation and results in fifty-six patients. J Bone Joint Surg 1981;63:216–25. [PubMed] [Google Scholar]
- 38.Koman LA, Williams RM, Evans PJ, et al. Quantification of upper extremity function and range of motion in children with cerebral palsy. Dev Med Child Neurol 2008;50:910–7. 10.1111/j.1469-8749.2008.03098.x [DOI] [PubMed] [Google Scholar]
- 39.Cobos-Carbó A, Augustovski F. [CONSORT 2010 Declaration: updated guideline for reporting parallel group randomised trials]. Med Clin 2011;137:213–5. 10.1016/j.medcli.2010.09.034 [DOI] [PubMed] [Google Scholar]
- 40.Chan AW, Tetzlaff JM, Gøtzsche PC, et al. SPIRIT 2013 explanation and elaboration: guidance for protocols of clinical trials. BMJ 2013;346:e7586. 10.1136/bmj.e7586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hoffmann TC, Glasziou PP, Boutron I, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348:g1687. 10.1136/bmj.g1687 [DOI] [PubMed] [Google Scholar]
- 42.Sakzewski L, Reedman S, Hoffmann T. Do we really know what they were testing? Incomplete reporting of interventions in randomised trials of upper limb therapies in unilateral cerebral palsy. Res Dev Disabil 2016;59:417–27. 10.1016/j.ridd.2016.09.018 [DOI] [PubMed] [Google Scholar]
- 43.Bax M, Goldstein M, Rosenbaum P, et al. Executive committee for the definition of cerebral palsy: proposed definition and classification of cerebral palsy. Dev Med Child Neurol;2005:571–6. [DOI] [PubMed] [Google Scholar]
- 44.Wechsler D. WPPSI-III, Wechsler preschool and primary scale of intelligence. 3rd edn. San Antonio, TX: Psychological Corporation, 2002. [Google Scholar]
- 45.Wechsler D. WISC-IV, Wechsler intelligence scale for children. 4th edn. San Antonio, TX: Psychological Corporation, 2003. [Google Scholar]
- 46.Wechsler D. Wechsler Adult Intelligence Scale (WAIS-IV-UK) administration and scoring manual. London: Pearson, 2010. [Google Scholar]
- 47.Eliasson AC, Krumlinde-Sundholm L, Rösblad B, et al. The Manual Ability Classification System (MACS) for children with cerebral palsy: scale development and evidence of validity and reliability. Dev Med Child Neurol 2006;48:549–54. 10.1017/S0012162206001162 [DOI] [PubMed] [Google Scholar]
- 48.Nordstrand L, Eliasson AC. Six years after a modified constraint induced movement therapy (CIMT) program--what happens when the children have become young adults? Phys Occup Ther Pediatr 2013;33:163–9. 10.3109/01942638.2013.757157 [DOI] [PubMed] [Google Scholar]
- 49.Reidy TG, Naber E, Viguers E, et al. Outcomes of a clinic-based pediatric constraint-induced movement therapy program. Phys Occup Ther Pediatr 2012;32:355–67. 10.3109/01942638.2012.694991 [DOI] [PubMed] [Google Scholar]
- 50.Platz T, Pinkowski C, van Wijck F, et al. Reliability and validity of arm function assessment with standardized guidelines for the Fugl-Meyer Test, Action Research Arm Test and Box and Block Test: a multicentre study. Clin Rehabil 2005;19:404–11. 10.1191/0269215505cr832oa [DOI] [PubMed] [Google Scholar]
- 51.Bleyenheuft Y, Gordon AM, Rameckers E, et al. Measuring changes of manual ability with ABILHAND-Kids following intensive training for children with unilateral cerebral palsy. Dev Med Child Neurol 2017;59:505–11. 10.1111/dmcn.13338 [DOI] [PubMed] [Google Scholar]
- 52.Passetti G, Cecchi F, Baldoli I, et al. Sensorized toys for measuring manipulation capabilities of infants at home. Conf Proc IEEE Eng Med Biol Soc 2015;2015:7390–3. 10.1109/EMBC.2015.7320099 [DOI] [PubMed] [Google Scholar]
- 53.Sgandurra G, Cecchi F, Serio SM, et al. Longitudinal study of unimanual actions and grasping forces during infancy. Infant Behav Dev 2012;35:205–14. 10.1016/j.infbeh.2012.01.003 [DOI] [PubMed] [Google Scholar]
- 54.Serio SM, Cecchi F, Boldrini E, et al. Instrumented toys for studying power and precision grasp forces in infants. Conf Proc IEEE Eng Med Biol Soc 2011;2011:2017–20. 10.1109/IEMBS.2011.6090370 [DOI] [PubMed] [Google Scholar]
- 55.Comans T, Mihala G, Sakzewski L, et al. The cost-effectiveness of a web-based multimodal therapy for unilateral cerebral palsy: the Mitii randomized controlled trial. Dev Med Child Neurol 2017;59:756–61. 10.1111/dmcn.13414 [DOI] [PubMed] [Google Scholar]
- 56.Stevens K. Valuation of the Child Health Utility 9D Index. Pharmacoeconomics 2012;30:729–47. 10.2165/11599120-000000000-00000 [DOI] [PubMed] [Google Scholar]
- 57.James S, Ziviani J, Ware RS, et al. Randomized controlled trial of web-based multimodal therapy for unilateral cerebral palsy to improve occupational performance. Dev Med Child Neurol 2015;57:530–8. 10.1111/dmcn.12705 [DOI] [PubMed] [Google Scholar]
- 58.Boyd RN, Mitchell LE, James ST, et al. Move it to improve it (Mitii): study protocol of a randomised controlled trial of a novel web-based multimodal training program for children and adolescents with cerebral palsy. BMJ Open 2013;3:e002853. 10.1136/bmjopen-2013-002853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Manetti S, Cecchi F, Sgandurra G, et al. Early stage economic evaluation of caretoy system for early intervention in preterm infants at risk of neurodevelopmental disorders. Value Health 2015;18:A358. 10.1016/j.jval.2015.09.683 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2017-017819supp004.pdf (48.7KB, pdf)
bmjopen-2017-017819supp001.pdf (231.3KB, pdf)
bmjopen-2017-017819supp002.pdf (3.9MB, pdf)
bmjopen-2017-017819supp003.pdf (48.7KB, pdf)