Abstract
Background
Excessive sedentary time is ubiquitous in Westernized societies. Previous studies have relied on self-report to evaluate the total volume of sedentary time as a prognostic risk factor for mortality and have not examined whether the manner in which sedentary time is accrued (in short or long bouts) carries prognostic relevance.
Objective
To examine the association of objectively-measured sedentary behavior (its total volume and accrual in prolonged, uninterrupted bouts) with all-cause mortality.
Design
Prospective cohort study.
Setting
Contiguous United States
Participants
7,985 black and white adults ≥45 years.
Measurements
Sedentary time was measured using a hip-mounted accelerometer. Prolonged, uninterrupted sedentariness was expressed as mean sedentary bout length. Hazard ratios [HRs] were calculated comparing quartiles 2-4 to quartile 1 for each exposure (quartile cutpoints: 689.7, 746.5, and 799.4 min/day for total sedentary time; 7.7, 9.6, and 12.4 min/bout for sedentary bout duration) in models that included moderate-vigorous physical activity.
Results
Over a median follow-up of 4.0 years, there were 340 deaths. In multivariable adjusted models, greater total sedentary time (HR [95% CI]: 1.22 [0.74-2.02], 1.61 [0.99-2.63], and 2.63 [1.60-4.30]; P-trend <0.001) and longer sedentary bout duration (HR [95% CI]: 1.03 [0.67-1.60], 1.22 [0.80-1.85], and 1.96 [1.31-2.93]; P-trend <0.001) were each associated with a higher all-cause mortality risk. Evaluation of their joint association showed that participants classified as high for both sedentary characteristics (e.g. high sedentary time [≥12.5 h/day] and high bout duration [≥10 min/bout]) had the highest morality risk.
Limitations
Participants may not be representative of the general US population.
Conclusions
The total volume of sedentary time as well as how one accrues sedentary time are both associated with all-cause mortality; suggestive that physical activity guidelines should target reducing and interrupting sedentary time to reduce mortality risk.
Primary Funding Source
National Institutes of Health
INTRODUCTION
Adults spend an alarming 9-10 hours/day sedentary.(1) Accordingly, the phrase “sitting is the new smoking” has been coined by popular press to describe a current epidemic of developed nations.(2–4) Evidence indicates sedentary time is associated with incident cardiovascular disease (CVD), incidence of CVD-related risk factors, and mortality.(5, 6) Importantly, the risk conferred by prolonged sedentariness is eliminated only with high levels of moderate-vigorous intensity physical activity (MVPA, ~60-75 min/day) which exceed physical activity recommendations.(7, 8) As such, sedentary behavior is now thought to represent a clinically important aspect of an individual’s physical activity profile and is no longer considered simply to be the extreme low end of the physical activity continuum.(5)
Studies linking sedentary behavior to health outcomes have relied almost exclusively on self-reported sedentary time – methodology subject to reporting bias and measurement error.(9) A 2015 systematic review identified only one study that examined the association of objectively-measured sedentary time with health outcomes;(5) a study (the National Health and Nutrition Examination Survey [NHANES]) limited by a small event rate.(10) New studies utilizing NHANES data have since been published with longer follow-up and higher event rates.(11–15) However, conflicting results have been reported as objectively-measured sedentary time was associated with mortality in some studies,(11, 14, 15) but not others.(12, 13) Additional cohort studies are thus needed to rectify evidence gaps. Furthermore, studies utilizing accelerometers to objectively measure sedentary behavior conventionally operationalize sedentary time as the total number of minutes/day. This approach ignores patterns of accumulated sedentary behavior over time. For example, accumulation of sedentary time in a few long bouts or many short bouts represents two distinct patterns of sedentary time accrual. Experimental studies have demonstrated that acute periods of prolonged, uninterrupted sedentary behavior elicit greater detrimental cardio-metabolic effects compared to sedentary behavior that is periodically interrupted,(16–18) suggestive that it is not just total sedentary time that is relevant to health outcomes, but also the manner in which it is accumulated. Few longitudinal studies, however, have explored the association of prolonged uninterrupted sedentary behavior with morality to corroborate these findings.
To inform physical activity guidelines regarding how to reduce sedentary behavior (e.g. target reductions in overall sedentary time; or target interrupting prolonged sedentary bouts), evidence from prospective studies is needed to (1) confirm the association of total sedentary time with mortality using objective measures, (2) determine if prolonged sedentary bouts confer mortality risk, and (3) elucidate whether total volume of sedentary time and its pattern of accumulation individually or jointly contribute to risk for mortality. The purpose of this study, therefore, was to examine the associations of objectively-measured sedentary time (both its total volume and accrual in prolonged bouts) with all-cause mortality in a national cohort of U.S. middle-aged and older adults enrolled in the Reasons for Geographic and Racial Differences in Stroke (REGARDS) study.
METHODS
Study Population
REGARDS is a population-based study designed to examine racial and regional disparities in stroke. It is comprised of 30,239 white and black adults ≥45 years of age, enrolled between 2003 and 2007 from across the contiguous U.S.(19, 20) Detailed design and methods for REGARDS are described elsewhere.(21) Briefly, demographic and cardiovascular risk factor data were collected by telephone interview and an in-home physical assessment upon enrollment. A detailed summary of baseline measures is provided in the Appendix (available at www.annals.org). Participants (or their proxies) were then followed at 6-month intervals to ascertain vital status. Objective measurements of sedentary behavior were collected from active REGARDS participants from 2009 to 2013 (mean years from study enrollment: 5.7 years [standard deviation, SD: 1.5 years]; range: 1.9-9.5 years).(22) A total of 7,985 participants provided compliant accelerometer wear (≥4 days with accelerometer wear ≥10 hours) and follow-up data and were available for the current analyses (Appendix Figure 1). Appendix Table 1 shows the characteristics of REGARDS participants who were included vs. excluded from the current analyses. All participants provided informed consent.
Accelerometer Data Collection
Methods for accelerometer data collection are described elsewhere.(22) Briefly, participants were fitted with an Actical™ (Respironics, Inc., Bend, OR) secured to their right hip using a nylon belt and were instructed to wear the device during waking hours for seven consecutive days. The Actical has been validated for measurement of physical activity and sedentary behavior and shown to have acceptable reliability.(23–25)
Activity counts were summed over 1-minute epochs. Non-wear periods were defined as ≥150 consecutive minutes of 0 activity counts. This non-wear algorithm was previously validated against daily log sheets in REGARDS participants.(26) Counts of 0-49 counts per minute (cpm), 50-1064 cpm, and ≥1065 cpm distinguished sedentary behavior, light intensity physical activity (LIPA), and MVPA, respectively, as determined in a laboratory-based calibration study.(27) A sedentary bout was defined as consecutive minutes in which the accelerometer registered <50 cpm. A sedentary break was defined as at least 1 minute in which counts registered ≥50 cpm after a sedentary bout. Both sedentary bouts and breaks were exclusively continuous periods with no interruptions or non-wear intervals allowed in the definition.
Outcome Ascertainment
All-cause mortality was the primary outcome, defined as any death after completion of the accelerometer protocol regardless of cause. Dates of death were confirmed through review of death certificates, medical records, and administrative databases. Deaths occurring through September 4, 2015 were included in the current analysis.
Statistical Analyses
Sedentary and physical activity variables were averaged across compliant days (≥10 hours of wear). Because of a high correlation between total sedentary time and wear time (Appendix Figure 2), we corrected for the influence of wear time by standardizing total sedentary time to 16 hours of wear time/day using the residuals obtained when regressing total sedentary time on wear time (see Appendix Methods).(28–30)
Participants were stratified into quartiles according to total sedentary time and, separately, mean sedentary bout duration (a measure of overall prolonged, uninterrupted sedentary behavior). Cox proportional-hazards regression modelling was used to calculate the hazard ratio (HR) for all-cause mortality associated with total sedentary time (and separately mean sedentary bout length) quartiles. Crude HRs were initially calculated. Subsequently, HRs were calculated with adjustment for age, race, sex, region of residence, education, and season the accelerometer was worn (Model 1), with further adjustment for current smoking, alcohol use, body mass index (BMI), diabetes, hypertension, dyslipidemia, estimated glomerular filtration rate (eGFR) <60 ml/min/1.73 m2, atrial fibrillation, history of coronary heart disease (CHD), and history of stroke (Model 2). Models were additionally adjusted for MVPA expressed continuously (Model 3). Tests for linear trend across quartiles were conducted by including the quartile for each participant as an ordinal variable in regression models. Proportional-hazards assumptions were confirmed with a Kolmogorov-type supremum test.(31) The above analyses were then repeated in a fully adjusted model testing interactions for age (<65 and ≥65 years), sex (male and female), race (black and white), BMI category (normal weight and overweight/obese), and MVPA category (<150 min/week and ≥150 min/week).
As a secondary analysis, we examined the continuous dose-response relationship between each sedentary characteristic and all-cause mortality in a fully adjusted model (Model 3) using restricted cubic splines.(32) Cubic polynomials were fitted with the mean of each sedentary characteristic set as the reference and knots placed at the 5th, 35th, 65th, and 95th percentiles.(33) Non-linear associations were evaluated using the likelihood ratio test. For non-linear associations, spline models were used to describe the associations and when the association was determined to be linear, a linear model was used.
Because of multicollinearity between total sedentary time and mean sedentary bout duration (r=0.61), both variables were not included in the same model. Alternatively, to examine the individual and joint associations of total sedentary time and prolonged, uninterrupted sedentary behavior with mortality, participants were classified into four categories: low total sedentary time (<750 min/day) and low prolonged sedentary bout time (<10 min/bout), low total sedentary time and high prolonged sedentary bout time (≥10 min/bout), high total sedentary time (≥750 min/day) and low prolonged sedentary bout time, and high total sedentary time and high prolonged sedentary bout time. HRs for all-cause mortality were calculated for each joint category in comparison to the low/low group in a fully adjusted model (Model 3). Thresholds for total sedentary time (750 min/day) and mean sedentary bout duration (10 min) were selected on the basis of the restricted cubic splines and were confirmed using a method described by Contal and O’Quigley (see Appendix Methods).(34)
To allow for the possibility that sedentary bouts of a certain length may have greater or lesser association with mortality, the percent of total sedentary time accumulated in bouts of 1-29, 30-59, 60-89, and ≥90 min was quantified. Participants were subsequently stratified into quartiles for each bout length. Analyses were then repeated testing associations of each sedentary bout threshold quartile with risk of all-cause mortality. To determine the bout length that confers the greatest mortality risk (as well as elucidate the risk associated with each bout length after accounting for one’s entire pattern of sedentary time accrual), models were mutually adjusted (e.g., all bout thresholds included in a single model) in a fourth model (Model 4).
As breaks in sedentary time have received interest as a potentially important adjunct to physical activity guidelines, as a tertiary analysis we also examined the association of sedentary break characteristics (total number, breaks/sedentary hour, break duration, and break intensity) with risk of all-cause mortality. To evaluate the potential for reverse causality, we conducted a sensitivity analysis excluding participants who died in the first year of follow-up. We also conducted a sensitivity analysis to assess how substantial any unmeasured confounding would need to be to explain the observed associations.(35) Analyses were conducted using SAS version 9.4 (SAS Institute, Cary, NC), with the PROC PHREG procedure used to conduct Cox regression models and the LGTPHCURV9 macro used to conduct cubic splines.(36)
Institutional Review Board Approval
The REGARDS study protocol was approved by Institutional Review Boards at participating institutions.
Role of the Funding Source
The National Institutes of Health and Coca-Cola Company had no role in the design, conduct, or analysis of the study or in the decision to submit the manuscript for publication.
RESULTS
Participant Characteristics
Sedentary behavior accounted for 77.4% (SD: 9.4) of wear time, equivalent to 12.3 (SD: 1.4) hours/day over a 16-hour waking day. Mean sedentary bout length was 11.4 (SD: 8.1) min/bout. The percent of total sedentary time accumulated in bouts 0-29, 30-59, 60-89, and ≥90 min was, on average, 52.0% (SD: 15.5), 22.1% (SD: 6.2), 11.8% (SD: 5.7), and 14.1% (SD: 12.8), respectively.
Participant characteristics stratified by total sedentary time quartile are presented in Table 1. On average, participants with greater total sedentary time were older, more likely to be black, smoke, live in a non-stroke belt/buckle region, and have diabetes, hypertension, dyslipidemia, eGFR <60 ml/min/1.73 m2, atrial fibrillation, history of CHD, and history of stroke. They were also less likely to be moderate or heavy drinkers, had greater BMI, and had lower levels of LIPA and MVPA. Participant characteristics stratified by mean sedentary bout length quartiles are presented in Table 2.
Table 1.
Characteristics of REGARDS accelerometer study participants (n=7,985) by total sedentary time quartile.
| Variable | Quartile 1 (n=1996) |
Quartile 2 (n=1996) |
Quartile 3 (n=1997) |
Quartile 4 (n=1996) |
P-Trend |
|---|---|---|---|---|---|
| Baseline Data* | |||||
| Age | 59.2 (7.1) | 61.9 (7.6) | 64.4 (7.9) | 68.7 (8.4) | <0.001 |
| Male (%) | 48.8 | 45.1 | 43.2 | 46.3 | 0.058 |
| Black race (%) | 26.0 | 28.4 | 31.3 | 39.8 | <0.001 |
| Region of Residence† (%) | <0.001 | ||||
| Non-belt/buckle | 42.5 | 43.9 | 46.8 | 49.0 | |
| Stroke buckle | 22.6 | 23.0 | 21.0 | 18.9 | |
| Stroke belt | 34.9 | 33.1 | 32.2 | 32.1 | |
| Education (%) | <0.001 | ||||
| Less than High School | 4.4 | 4.4 | 6.1 | 9.8 | |
| High School Graduate | 21.9 | 20.4 | 22.6 | 24.6 | |
| Some College | 26.8 | 26.2 | 26.6 | 27.5 | |
| College graduate | 46.9 | 49.0 | 44.7 | 38.1 | |
| Current Smoker (%) | 9.9 | 10.2 | 10.9 | 11.7 | 0.043 |
| Alcohol Drinking‡ (%) | <0.001 | ||||
| None | 50.0 | 51.5 | 57.6 | 65.0 | |
| Moderate | 44.4 | 42.9 | 38.2 | 31.3 | |
| Heavy | 5.6 | 5.6 | 4.2 | 3.7 | |
| Body Mass Index (kg/m2) | 27.3 (4.8) | 28.3 (5.4) | 29.1 (5.8) | 29.8 (6.4) | <0.001 |
| Diabetes (%) | 7.6 | 11.8 | 15.3 | 23.5 | <0.001 |
| Hypertension (%) | 38.0 | 48.0 | 54.9 | 65.9 | <0.001 |
| Dyslipidemia (%) | 52.5 | 55.0 | 60.3 | 63.4 | <0.001 |
| eGFR < 60 mL/min/1.73 m2 (%) | 1.9 | 4.6 | 8.3 | 13.3 | <0.001 |
| Atrial fibrillation (%) | 4.7 | 6.1 | 6.5 | 9.2 | <0.001 |
| History of CHD (%) | 8.6 | 10.9 | 12.6 | 19.8 | <0.001 |
| History of Stroke (%) | 1.6 | 2.8 | 3.2 | 6.4 | <0.001 |
| Accelerometer Data | |||||
| Age at time of accelerometer testing | 65.3 (7.3) | 68.0 (7.7) | 70.7 (8.0) | 75.2 (8.5) | <0.001 |
| Season accelerometer worn§ (%) | 0.20 | ||||
| Summer | 25.8 | 25.1 | 21.7 | 27.0 | |
| Autumn | 26.2 | 25.1 | 24.3 | 24.4 | |
| Winter | 25.1 | 26.3 | 25.0 | 23.9 | |
| Spring | 23.0 | 23.6 | 29.0 | 24.8 | |
| Wear Time (min/day) | 875.1 (107.8) | 860.5 (111.9) | 852.2 (112.4) | 873.7 (140.8) | <0.001 |
| Valid wear days (%) | 0.73 | ||||
| 4–5 days | 1.3 | 1.4 | 1.3 | 1.4 | |
| 6–7 days | 98.7 | 98.6 | 98.7 | 98.6 | |
| Sedentary Time‖ (min/day) | 635.3 (47.7) | 719.2 (16.6) | 771.8 (15.1) | 841.0 (33.2) | <0.001 |
| Sedentary Bout Duration (min/bout) ¶ | 6.9 (1.4) | 8.7 (1.4) | 10.8 (1.7) | 19.2 (12.9) | <0.001 |
| LIPA** (min/day) | 285.5 (51.7) | 209.1 (27.7) | 159.7 (26.0) | 98.2 (38.8) | <0.001 |
| MVPA†† (min/day) | 26.9 (23.7) | 14.9 (15.0) | 8.1 (10.4) | 2.9 (6.2) | <0.001 |
Data presented as mean (standard deviation) or percent.
CHD, coronary heart disease; LIPA, light intensity physical activity; MVPA, moderate or vigorous intensity physical activity.
Demographic data, cardiovascular risk factors, and chronic disease status/medical history data were collected at the original baseline (see Appendix Methods).
Stroke buckle: coastal plain region of North Carolina, South Carolina, and Georgia; stroke belt: remainder of North Carolina, South Carolina, and Georgia, plus Alabama, Mississippi, Tennessee, Arkansas, and Louisiana.
None: 0 drinks per week; Moderate: >0 to 14 drinks per week for males and >0 to 7 drinks per week for females; Heavy: >14 drinks per week for males and >7 drinks per week for females.
Summer: June 21-September 20; Autumn September 21-December 20; Winter: December 21-March 20; Spring: March 21-June 20.
Minutes in which the accelerometer registered <50 counts per minute. Corrected for wear time and expressed as the estimated minutes/day of sedentary time given a standardized 16 hours of accelerometer wear (see Methods).
sedentary bout is defined as consecutive minutes in which the accelerometer registered <50 counts per min.
Minutes in which the accelerometer registered 50–1064 counts per minute.
Minutes in which the accelerometer registered ≥1065 counts per minute.
The quartile cutoff points were <689.7, ≥689.7 to <746.5, ≥746.5 to <799.4, and ≥799.4 min/day.
Table 2.
Characteristics of REGARDS accelerometer study participants (n=7,985) by mean sedentary bout length quartile.
| Variable | Quartile 1 (n=1996) |
Quartile 2 (n=1996) |
Quartile 3 (n=1997) |
Quartile 4 (n=1996) |
P-Trend |
|---|---|---|---|---|---|
| Baseline Data* | |||||
| Age | 59.9 (7.4) | 62.4 (7.8) | 64.0 (8.0) | 67.8 (8.8) | <0.001 |
| Male (%) | 38.2 | 45.2 | 48.4 | 51.7 | <0.001 |
| Black race (%) | 31.1 | 27.9 | 30.9 | 35.6 | <0.001 |
| Region of Residence† (%) | <0.001 | ||||
| Non-belt/buckle | 41.3 | 44.9 | 46.1 | 49.9 | |
| Stroke buckle | 22.6 | 22.3 | 22.2 | 18.4 | |
| Stroke belt | 36.1 | 32.8 | 26.0 | 31.7 | |
| Education (%) | 0.35 | ||||
| Less than High School | 5.4 | 5.6 | 5.1 | 8.8 | |
| High School Graduate | 24.7 | 20.4 | 21.9 | 22.3 | |
| Some College | 29.1 | 25.5 | 26.7 | 25.8 | |
| College graduate | 40.8 | 48.5 | 46.3 | 43.1 | |
| Current Smoker (%) | 12.7 | 9.5 | 9.7 | 10.7 | 0.062 |
| Alcohol Drinking‡ (%) | <0.001 | ||||
| None | 55.8 | 52.9 | 54.4 | 61.0 | |
| Moderate | 38.0 | 42.4 | 41.6 | 35.0 | |
| Heavy | 6.2 | 4.7 | 4.0 | 4.0 | |
| Body Mass Index (kg/m2) | 27.2 (4.9) | 28.2 (5.3) | 29.1 (5.7) | 30.0 (6.4) | <0.001 |
| Diabetes (%) | 8.6 | 12.6 | 14.1 | 22.9 | <0.001 |
| Hypertension (%) | 42.1 | 47.3 | 54.0 | 63.3 | <0.001 |
| Dyslipidemia (%) | 51.3 | 56.1 | 60.1 | 63.6 | <0.001 |
| eGFR < 60 mL/min/1.73 m2 (%) | 2.1 | 6.2 | 6.8 | 13.0 | <0.001 |
| Atrial fibrillation (%) | 5.4 | 5.6 | 7.1 | 8.3 | <0.001 |
| History of CHD (%) | 9.8 | 10.9 | 12.3 | 19.0 | <0.001 |
| History of Stroke (%) | 2.1 | 2.5 | 3.3 | 6.2 | <0.001 |
| Accelerometer Data | |||||
| Age at time of accelerometer testing | 66.0 (7.6) | 68.6 (7.9) | 70.2 (8.1) | 74.3 (8.9) | <0.001 |
| Season accelerometer worn§ (%) | 0.55 | ||||
| Summer | 24.8 | 25.7 | 22.8 | 26.4 | |
| Autumn | 26.1 | 25.1 | 24.8 | 24.0 | |
| Winter | 25.2 | 24.6 | 24.2 | 25.3 | |
| Spring | 23.9 | 24.0 | 28.2 | 24.3 | |
| Wear Time (min/day) | 855.9 (105.6) | 871.6 (109.5) | 871.2 (117.8) | 862.8 (140.7) | <0.001 |
| Valid wear days (%) | 0.34 | ||||
| 4–5 days | 1.2 | 1.1 | 1.4 | 1.5 | |
| 6–7 days | 98.8 | 98.9 | 98.6 | 98.5 | |
| Sedentary Time‖ (min/day) | 649.3 (58.3) | 717.6 (40.7) | 766.0 (36.6) | 834.5 (42.0) | <0.001 |
| Sedentary Bout Duration¶ (min/bout) | 6.5 (0.9) | 8.7 (0.5) | 10.9 (0.8) | 19.6 (12.7) | <0.001 |
| LIPA** (min/day) | 274.7 (58.2) | 211.0 (42.1) | 165.7 (36.7) | 101.0 (42.7) | <0.001 |
| MVPA†† (min/day) | 20.0 (21.1) | 16.1 (18.1) | 11.9 (16.0) | 4.9 (10.1) | <0.001 |
Data presented as mean (standard deviation) or percent.
CHD, coronary heart disease; LIPA, light intensity physical activity; MVPA, moderate or vigorous intensity physical activity.
Demographic data, cardiovascular risk factors, and chronic disease status/medical history data were collected at the original baseline (see Appendix Methods).
Stroke buckle: coastal plain region of North Carolina, South Carolina, and Georgia; stroke belt: remainder of North Carolina, South Carolina, and Georgia, plus Alabama, Mississippi, Tennessee, Arkansas, and Louisiana.
None: 0 drinks per week; Moderate: >0 to 14 drinks per week for males and >0 to 7 drinks per week for females; Heavy: >14 drinks per week for males and >7 drinks per week for females.
Summer: June 21-September 20; Autumn September 21-December 20; Winter: December 21-March 20; Spring: March 21-June 20.
Minutes in which the accelerometer registered <50 counts per minute. Corrected for wear time and expressed as the estimated minutes/day of sedentary time given a standardized 16 hours of accelerometer wear (see Methods).
sedentary bout is defined as consecutive minutes in which the accelerometer registered <50 counts per min.
Minutes in which the accelerometer registered 50–1064 counts per minute.
Minutes in which the accelerometer registered ≥1065 counts per minute.
The quartile cutoff points were <7.7, ≥7.7 to <9.6, ≥ 9.6 to <12.4, and ≥12.4 min/bout.
Total Sedentary Time, Sedentary Bout Length and All-Cause Mortality
There were 340 deaths over a median follow-up of 4.0 years (range 0.1 to 6.1 years). When expressed as quartiles, greater total sedentary time and longer mean sedentary bout duration were each dose-dependently associated with a higher risk of all-cause mortality (Figure 1 and Appendix Table 2). Adjustment for MVPA attenuated these associations, but all results remained statistically significant. The associations of total sedentary time and sedentary bout duration quartiles with all-cause mortality did not vary by age, sex, race, BMI, or MVPA category (interaction p-values >0.10; Appendix Figures 3 and 4).
Figure 1. Adjusted cumulative mortality by total sedentary time (Panel A) and mean sedentary bout duration (Panel B) quartiles.
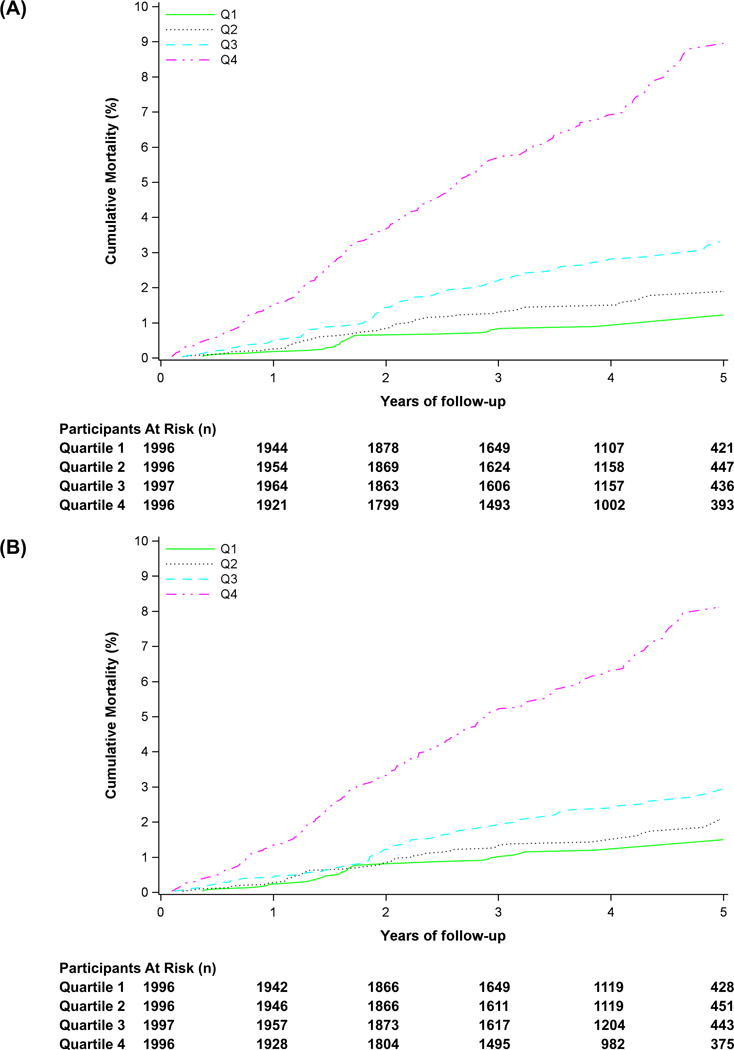
Models adjusted for age, sex, race, region of residence, education, season, current smoking, alcohol use, body mass index, diabetes, hypertension, dyslipidemia, estimated glomerular filtration rate <60 mL/min/1.73 m2, atrial fibrillation, history of coronary heart disease, history of stroke, and moderate-vigorous physical activity. The quartile cutoff points were <689.7, ≥689.7 to <746.5, ≥746.5 to <799.4, and ≥799.4 min/day for total sedentary time and <7.7, ≥7.7 to <9.6, ≥ 9.6 to <12.4, and ≥12.4 min/bout for sedentary bout duration.
Figure 2 shows the cubic splines for risk of all-cause mortality when total sedentary time and mean sedentary bout duration were expressed continuously. Total sedentary time was significantly associated with all-cause mortality in a linear, dose-dependent fashion (p-value for overall effect <0.001, p-value for non-linear relationship=0.70). In contrast, mean sedentary bout duration was significantly associated with all-cause mortality in a non-linear manner (p-value for overall effect <0.001, p-value for non-linear relationship <0.001). A marked increase in mortality risk was observed at ~10 min/bout; suggestive of a threshold effect.
Figure 2. Hazard ratio of all-cause mortality as a function of total sedentary time (Panel A) and mean sedentary bout duration (Panel B) expressed continuously.
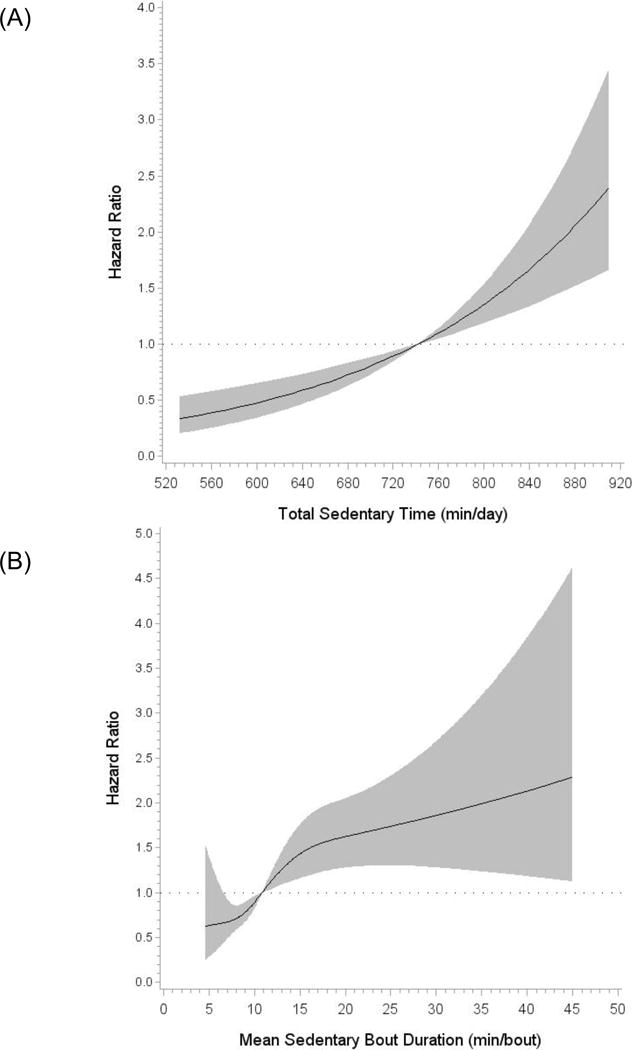
Data were fitted using restricted cubic splines with the mean set as the reference and 4 knots placed at the 5th, 35th, 65th, and 95th percentiles. Results are trimmed at the 1st and 99th percentiles and are reported as hazard ratios (black line) and 95% confidence intervals (gray shaded area). Total sedentary time is a linear model (p-value for overall effect <0.001, p-value for non-linear relationship=0.70) and mean sedentary bout duration is a non-linear model (p-value for overall effect <0.001, p-value for non-linear relationship <0.001). Models were adjusted for age, sex, race, region of residence, education, season, current smoking, alcohol use, body mass index, diabetes, hypertension, dyslipidemia, estimated glomerular filtration rate <60 mL/min/1.73 m2, atrial fibrillation, history of coronary heart disease, history of stroke, and moderate-vigorous physical activity.
Joint Associations of Total Sedentary Time and Prolonged Sedentary Bouts with All-Cause Mortality
Figure 3 shows the joint associations of total sedentary time and sedentary bout length. Participants classified as high for both sedentary characteristics had the highest risk for all-cause mortality (HR: 2.00 [95% CI: 1.45-2.75]; p<0.001). Participants classified into the high total sedentary time/ low sedentary bout duration group (HR: 1.68 [95% CI: 1.07-2.65]; p=0.026), but not those classified into the low total sedentary time/high sedentary bout duration group (HR: 1.19 [95% CI: 0.59-2.42]; p=0.62), also had a statistically significant increased risk for all-cause mortality.
Figure 3. Adjusted cumulative mortality according to joint associations of total sedentary time and prolonged, uninterrupted sedentary bouts.
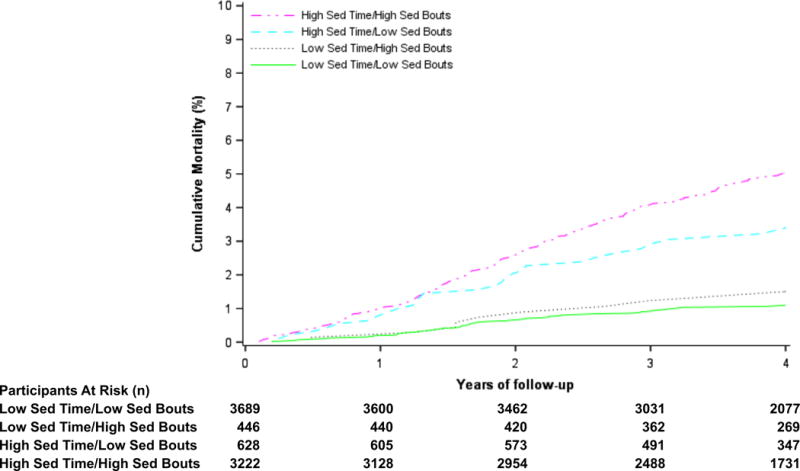
Models adjusted for age, sex, race, region of residence, education, season, current smoking, alcohol use, body mass index, diabetes, hypertension, dyslipidemia, estimated glomerular filtration rate <60 mL/min/1.73 m2, atrial fibrillation, history of coronary heart disease, history of stroke, and moderate-vigorous physical activity. High and low groups were defined as ≥12.5 and <12.5 hours/day for total sedentary time and ≥10.0 min/bout and <10 min/bout for mean sedentary bout duration. The sample size and number of deaths for each group were as follows: low total sedentary time/low sedentary bout time (n=3,689, deaths=62), high total sedentary time/low sedentary bout time (n=628, deaths=30), low total sedentary time, high sedentary bout time (n=446, deaths=9), high total sedentary time/high sedentary bout time (n=3,222, deaths=239).
Sedentary Bout Length Thresholds and All-Cause Mortality
Accumulating a greater percent of sedentary time in bouts of 1-29 min was associated with less of an increased risk for all-cause mortality (Figure 4 and Appendix Table 3) when expressed as quartiles. Conversely, accumulating a greater percent of sedentary time in bouts of 60-89 min and ≥90 min were associated with a higher risk of all-cause mortality. To distinguish the sedentary bout duration that confers the greatest risk, models were mutually adjusted by including each sedentary bout threshold in a single model. After mutual adjustment, accumulating a greater percent of sedentary time in bouts of 1-29 min remained significantly associated with less of an increased risk of all-cause mortality. Accumulating a greater percent of sedentary time in bouts of 30-59, 60-89, and ≥90 min were not significantly associated with a greater risk of all-cause mortality after mutual adjustment. The associations of each sedentary bout threshold quartile with all-cause mortality did not vary by age, sex, race, BMI, or MVPA category (interaction p-values >0.10). All results were similar when sedentary bout thresholds were expressed continuously in restricted cubic splines; with linear relationships observed for all bout thresholds (Appendix Figure 5).
Figure 4. Adjusted cumulative mortality by quartile of sedentary bout threshold.
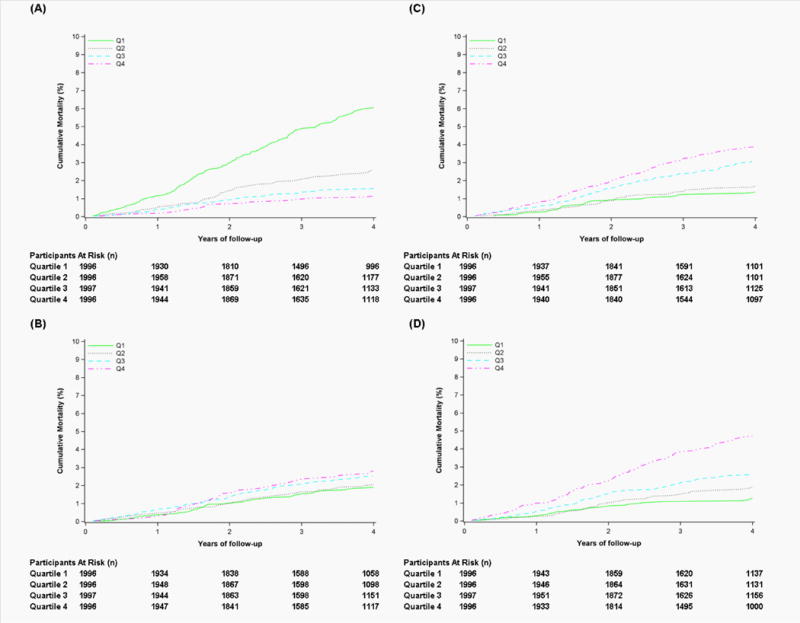
Panel A: %Sedentary Time from Bouts 1-30 min; Panel B: %Sedentary Time from Bouts 30-60 min; Panel C: %Sedentary Time from Bouts 60-90 min; Panel D: %Sedentary Time from Bouts ≥90 min. Models adjusted for age, sex, race, region of residence, education, season, current smoking, alcohol use, body mass index, diabetes, hypertension, dyslipidemia, estimated glomerular filtration rate <60 mL/min/1.73 m2, atrial fibrillation, history of coronary heart disease, history of stroke, and moderate-vigorous physical activity. The quartile cutoff points were <42.2%, ≥42.2% to <53.0%, ≥53.0% to <62.8%, and ≥62.8% for bouts 0-30 min; <18.1%, ≥18.1% to <22.1%, ≥22.1% to <26.2%, and ≥26.2% for bouts 30-60 min; <7.6%, ≥7.6 to <11.3%, ≥11.3% to <15.5%, ≥15.5% for bouts 60-90 min; and <5.2%, ≥5.2% to <10.9%, ≥10.9% to <19.0%, and ≥19.0% for >90 min bouts.
Tertiary and Sensitivity Analyses
In unadjusted and multivariable adjusted models, a higher number, longer duration, and greater intensity of sedentary breaks were each associated with a lower risk of all-cause mortality (Appendix Table 4).
In sensitivity analyses, we found no evidence of reverse causality after the exclusion of early deaths as the pattern of all results was similar (data not shown). We also investigated the effect of a simulated unmeasured confounder on risk for all-cause mortality. For an unmeasured confounder to bring the upper confidence limit of the uppermost total sedentary time quartile below 1.00, it would have to be associated with a 2.5 fold increased probability of being in the uppermost quartile and a 3.0-fold increase in risk for all-cause mortality. For an unmeasured confounder to bring the upper confidence limit of the uppermost mean sedentary bout duration quartile below 1.00, it would have to both increase the probability of being in the uppermost quartile and increase risk for all-cause mortality by 2.0 fold.
DISCUSSION
In this prospective study of a U.S. national cohort of middle- and older-aged adults, both total sedentary time and prolonged, uninterrupted sedentary bouts were associated with an increased risk for all-cause mortality. These associations were independent of MVPA and cardiovascular risk factors (albeit with some attenuation in risk estimates). When the joint associations of both sedentary characteristics were evaluated, high total sedentary time and high sedentary bout duration together were associated with the highest risk for all-cause mortality (e.g. high total sedentary time and high sedentary bout duration). These findings highlight the importance of the total volume of sedentary time and its accumulation in prolonged bouts as important health risk behaviors.
Meta-analyses have demonstrated that total sedentary time is associated with CVD and mortality, independent of MVPA.(5, 37) However, these findings are largely based on self-reported sedentary time, data which may underestimate the magnitude of the relationship between sedentariness and health risk.(38) Use of accelerometers reduces potential biases and measurement error inherent in self-report data. Nonetheless, only one study has reported on the association of objectively-measured sedentary time and mortality. This previous study, which comprised adults enrolled in NHANES and has been reported in several separate analyses,(10–14) has yielded conflicting results with some studies reporting a significant association between objectively-measured sedentary time and all-cause mortality,(10, 11, 14, 15) but not others.(12, 13) Differences in inclusion/exclusion criteria, covariates, and follow-up time have been attributed to differences across analyses.(12) A relatively small sample size (n=1,096-4,840) and low minority representation (~9-14% black) have also limited previous findings from NHANES. Thus, our findings add to the literature by confirming the association of total sedentary time and mortality risk in a national, biracial cohort of ~8,000 middle- and older-aged adults, the largest study to date with objective measures of sedentary behavior and prospective health outcomes. The magnitude of the association of total sedentary time with all-cause mortality (2.6-fold greater risk for quartile 4 vs. quartile 1) is notably higher than reported in meta-analyses (HR=1.22 [95% CI: 1.09-1.41])(5), which could be attributed to use of objective measures and/or the analytic sample (e.g. middle- and older-aged adults, more blacks), and further underscores the total volume of sedentary behavior as a potent risk factor.
A key finding of this study is that it is the first to report that patterns of sedentary time accumulation are associated with mortality. Previous cross-sectional studies have reported associations between the total number of breaks in sedentary time/day (the reciprocal to mean sedentary bout length) and cardiometabolic biomarkers.(28, 39) These findings led to the “prolonger” vs. “breaker” hypothesis which postulates that it is not only the amount of sedentary time that is important to cardiometabolic health, but also the manner in which it is accumulated.(40) Subsequent experimental studies have corroborated this hypothesis as greater detrimental cardiometabolic effects have been observed following acute periods of prolonged, uninterrupted sedentary time relative to sedentary time that is periodically interrupted.(16, 17) Our findings extend those of previous studies by providing prospective evidence that prolonged, uninterrupted sedentary behavior is associated with a greater risk for all-cause mortality.
Current physical activity guidelines recommend all age groups minimize their amount of sedentary time.(41) These guidelines, however, are generalized and stop short of specific recommendations about how one should reduce sedentariness. Our finding of a joint association between the volume and pattern of sedentary behavior suggests that future guidelines should consider reductions in total sedentary time as well as prolonged sedentary bouts. Future randomized controlled trials, however, are still needed. Importantly, our findings also provide some of the first empirical evidence regarding how often sedentary behavior should be interrupted. We observed that accumulation of sedentary time in 60-89 min and ≥90 min bouts were associated with a greater risk for all-cause mortality, while conversely, accumulation of sedentary time in 1-29 min bouts was associated with less of an increased mortality risk. With respect to the latter finding, it should be noted that accumulation of large volumes of sedentary time is a hazardous health behavior irrespective of how it’s accumulated. Nonetheless, this finding would suggest that accruing sedentary time in shorter bouts is the least harmful pattern of accumulation.
Currently, it is unclear how often sedentary time should be interrupted to reduce the risk incurred by prolonged sedentary bouts. Sedentary breaks every 30 min have been proposed as a feasible recommendation, (1, 42) which is supported by experimental studies showing sedentary breaks every 30 min elicit beneficial cardiometabolic effects.(17) Our results suggest guidelines aimed at every 30 min could be an optimal target to interrupt sedentary behavior as it was observed that accumulation of sedentary time in bouts of 1-29 min was associated with less of an increased mortality risk even after accounting for sedentary time accrued in bouts of 60-89 and ≥90 min. From a feasibility/adoption perspective, sedentary breaks every 60 or 90 min may be more tenable to public health uptake. However, middle- and older-aged adults average only ~ 2 sedentary bouts/day longer than 60 min and <1 sedentary bout/day longer than 90 min.(43) Furthermore, in the present study the accumulation of sedentary time in bouts of 60-89 min and ≥90 min were no longer associated with mortality after accounting for the amount of sedentary time accrued from bouts of 1-29 min. However, caution is warranted when interpreting these results in light of the wide confidence intervals surrounding the point estimates for these bout thresholds.
Several limitations should be noted when interpreting our findings. First, the Actical™ cannot distinguish between different postures (e.g. sitting, standing), thus we relied on an intensity-only definition of sedentary behavior.(44) Second, only 7 days of accelerometer data were collected. Thus, the current study may have undersampled the exposure and yielded unreliable estimates of habitual sedentary time. Third, some participant risk factors were collected at baseline, several years (~6 years) prior to wearing the accelerometer, and may have changed (e.g., diabetes status). Thus, there may be residual confounding from misclassification of participants with respect to important confounders. However, in sensitivity analysis, for an unmeasured confounder to explain the association of total sedentary time or mean sedentary bout duration with all-cause mortality it would have to both increase the likelihood of being in the uppermost quartile for either sedentary characteristic and increase the risk of all-cause mortality by 2.0-3.0 fold above and beyond the measured covariates. This would constitute a substantial confounding. Fourth, there were a number of differences among REGARDS participants included vs. excluded from the current analyses. Excluded participants were more likely to be black, smoke, and have lower education levels, diabetes, hypertension, eGFR <60 mL/min/1.73 m2, and history of CHD and had a greater risk for all-cause mortality compared to included participants (Appendix Table 5). Thus, our findings may not be generalizable to the entire REGARDS cohort. Furthermore, there is potential for selection bias as those who participated in REGARDS may not be representative of the general population. Fifth, in analyses examining the joint effects of total sedentary time and prolonged, uninterrupted sedentary bouts, the sample size and number of deaths were small for the groups that were high for only one of the sedentary characteristics (e.g., high total sedentary time/low sedentary bout time and low total sedentary time, high sedentary bout time). Although the association of total sedentary time alone, but not sedentary bout duration alone, with mortality is suggestive that the volume of sedentary time may be the more hazardous sedentary characteristic, the small number of events and wide confidence intervals in these groups render these findings inconclusive. Caution is thus warranted when interpreting these results. Finally, the relatively short follow-up period may have led to reverse causation.
In conclusion, in a geographically diverse, biracial population-based sample of middle- and older aged U.S. adults, both total sedentary time and prolonged, uninterrupted sedentary bouts were associated with an increased risk for all-cause mortality, independent of physical activity levels. Our findings suggest that total sedentary time and prolonged, uninterrupted sedentary bouts are jointly associated with increased mortality risk and that breaking up sedentary time every 30 min may be protective against the health risks incurred by prolonged sedentariness. These data may be useful to inform specific recommendations for reducing sedentary behavior and support the concept that reducing and regularly breaking up sedentary time may be an important adjunct to existing physical activity guidelines.
Supplementary Material
Acknowledgments
The authors thank the other investigators, staff, and participants of the REGARDS study for their valuable contributions. A full list of REGARDS investigators and institutions can be found at http://www.regardsstudy.org.
Financial Support: This research project is supported by a cooperative agreement U01-NS041588 and investigator-initiated grant R01-NS061846 from the National Institute of Neurological Disorders and Stroke, National Institutes of Health, Department of Health and Human Services. Additional funding was provided by an unrestricted research grant from The Coca-Cola Company.
Footnotes
Disclosures: Authors have disclosed no conflicts of interest. Disclosures can also be viewed www.acponline.org/authors/icmje/ConflictOfInterestForms.
Reproducible Research Statement: Study protocol: Available at http://www.regardsstudy.org. Statistical code: Available through written agreement with authors from Dr. Diaz (e-mail, kd2442@columbia.edu). Data set: Available through data use agreement with University of Alabama at Birmingham. Contact regardsadmin@uab.edu
Requests for Single Reprints: Keith Diaz, Columbia University Medical Center, 622 W 168th Street, PH9-301, New York, NY 10032. 212-304-5231; email: kd2442@columbia.edu.
References
- 1.Dunstan DW, Howard B, Healy GN, Owen N. Too much sitting–a health hazard. Diabetes Res Clin Pract. 2012;97(3):368–76. doi: 10.1016/j.diabres.2012.05.020. [DOI] [PubMed] [Google Scholar]
- 2.Yeager S. Sitting is the new smoking - even for runner. Runner’s World. 2013 retrieved from http://www.runnersworld.com/health/sitting-is-the-new-smoking-even-for-runners in June 2016.
- 3.Strurt D, Nordstrom T. Is sitting the new smoking? Forbes. 2015 retrieved from http://www.forbes.com/sites/davidsturt/2015/01/13/is-sitting-the-new-smoking/#302dc64f239a in June 2016.
- 4.Gerstacker D. Sitting is the new smoking: ways a sedentary lifestyle is killing you. Huffington Post. 2014 retrieved from http://www.huffingtonpost.com/the-active-times/sitting-is-the-new-smokin_b_5890006.html in June 2016.
- 5.Biswas A, Oh PI, Faulkner GE, Bajaj RR, Silver MA, Mitchell MS, et al. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: a systematic review and meta-analysis. Ann Intern Med. 2015;162(2):123–32. doi: 10.7326/M14-1651. [DOI] [PubMed] [Google Scholar]
- 6.Wilmot EG, Edwardson CL, Achana FA, Davies MJ, Gorely T, Gray LJ, et al. Sedentary time in adults and the association with diabetes, cardiovascular disease and death: systematic review and meta-analysis. Diabetologia. 2012;55(11):2895–905. doi: 10.1007/s00125-012-2677-z. [DOI] [PubMed] [Google Scholar]
- 7.Ekelund U, Steene-Johannessen J, Brown WJ, Fagerland MW, Owen N, Powell KE, et al. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet. 2016;388(10051):1302–10. doi: 10.1016/S0140-6736(16)30370-1. [DOI] [PubMed] [Google Scholar]
- 8.United States. 2008 physical activity guidelines for Americans : be active, healthy, and happy! Washington, DC: U.S. Dept. of Health and Human Services; 2008. Department of Health and Human Services. [Google Scholar]
- 9.Atkin AJ, Gorely T, Clemes SA, Yates T, Edwardson C, Brage S, et al. Methods of Measurement in epidemiology: sedentary Behaviour. Int J Epidemiol. 2012;41(5):1460–71. doi: 10.1093/ije/dys118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Koster A, Caserotti P, Patel KV, Matthews CE, Berrigan D, Van Domelen DR, et al. Association of sedentary time with mortality independent of moderate to vigorous physical activity. PLoS One. 2012;7(6):e37696. doi: 10.1371/journal.pone.0037696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Matthews CE, Keadle SK, Troiano RP, Kahle L, Koster A, Brychta R, et al. Accelerometer-measured dose-response for physical activity, sedentary time, and mortality in US adults. Am J Clin Nutr. 2016;104(5):1424–32. doi: 10.3945/ajcn.116.135129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Evenson KR, Wen F, Herring AH. Associations of Accelerometry-Assessed and Self-Reported Physical Activity and Sedentary Behavior With All-Cause and Cardiovascular Mortality Among US Adults. Am J Epidemiol. 2016;184(9):621–32. doi: 10.1093/aje/kww070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Loprinzi PD, Sng E. The effects of objectively measured sedentary behavior on all-cause mortality in a national sample of adults with diabetes. Prev Med. 2016;86:55–7. doi: 10.1016/j.ypmed.2016.01.023. [DOI] [PubMed] [Google Scholar]
- 14.Schmid D, Ricci C, Leitzmann MF. Associations of objectively assessed physical activity and sedentary time with all-cause mortality in US adults: the NHANES study. PLoS One. 2015;10(3):e0119591. doi: 10.1371/journal.pone.0119591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Loprinzi PD, Loenneke JP, Ahmed HM, Blaha MJ. Joint effects of objectively-measured sedentary time and physical activity on all-cause mortality. Prev Med. 2016;90:47–51. doi: 10.1016/j.ypmed.2016.06.026. [DOI] [PubMed] [Google Scholar]
- 16.Dunstan DW, Kingwell BA, Larsen R, Healy GN, Cerin E, Hamilton MT, et al. Breaking up prolonged sitting reduces postprandial glucose and insulin responses. Diabetes Care. 2012;35(5):976–83. doi: 10.2337/dc11-1931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Peddie MC, Bone JL, Rehrer NJ, Skeaff CM, Gray AR, Perry TL. Breaking prolonged sitting reduces postprandial glycemia in healthy, normal-weight adults: a randomized crossover trial. Am J Clin Nutr. 2013;98(2):358–66. doi: 10.3945/ajcn.112.051763. [DOI] [PubMed] [Google Scholar]
- 18.Howard BJ, Fraser SF, Sethi P, Cerin E, Hamilton MT, Owen N, et al. Impact on hemostatic parameters of interrupting sitting with intermittent activity. Med Sci Sports Exerc. 2013;45(7):1285–91. doi: 10.1249/MSS.0b013e318285f57e. [DOI] [PubMed] [Google Scholar]
- 19.Howard G, Anderson R, Johnson NJ, Sorlie P, Russell G, Howard VJ. Evaluation of social status as a contributing factor to the stroke belt region of the United States. Stroke. 1997;28(5):936–40. doi: 10.1161/01.str.28.5.936. [DOI] [PubMed] [Google Scholar]
- 20.Lanska DJ, Kuller LH. The geography of stroke mortality in the United States and the concept of a stroke belt. Stroke. 1995;26(7):1145–9. doi: 10.1161/01.str.26.7.1145. [DOI] [PubMed] [Google Scholar]
- 21.Howard VJ, Cushman M, Pulley L, Gomez CR, Go RC, Prineas RJ, et al. The reasons for geographic and racial differences in stroke study: objectives and design. Neuroepidemiology. 2005;25(3):135–43. doi: 10.1159/000086678. [DOI] [PubMed] [Google Scholar]
- 22.Howard VJ, Rhodes JD, Mosher A, Hutto B, Stewart MS, Colabianchi N, et al. Obtaining Accelerometer Data in a National Cohort of Black and White Adults. Med Sci Sports Exerc. 2015;47(7):1531–7. doi: 10.1249/MSS.0000000000000549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Esliger DW, Tremblay MS. Technical reliability assessment of three accelerometer models in a mechanical setup. Med Sci Sports Exerc. 2006;38(12):2173–81. doi: 10.1249/01.mss.0000239394.55461.08. [DOI] [PubMed] [Google Scholar]
- 24.Welk GJ, Schaben JA, Morrow JR., Jr Reliability of accelerometry-based activity monitors: a generalizability study. Med Sci Sports Exerc. 2004;36(9):1637–45. [PubMed] [Google Scholar]
- 25.Van Remoortel H, Giavedoni S, Raste Y, Burtin C, Louvaris Z, Gimeno-Santos E, et al. Validity of activity monitors in health and chronic disease: a systematic review. Int J Behav Nutr Phys Act. 2012;9:84. doi: 10.1186/1479-5868-9-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hutto B, Howard VJ, Blair SN, Colabianchi N, Vena JE, Rhodes D, et al. Identifying accelerometer nonwear and wear time in older adults. Int J Behav Nutr Phys Act. 2013;10:120. doi: 10.1186/1479-5868-10-120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hooker SP, Feeney A, Hutto B, Pfeiffer KA, McIver K, Heil DP, et al. Validation of the actical activity monitor in middle-aged and older adults. J Phys Act Health. 2011;8(3):372–81. doi: 10.1123/jpah.8.3.372. [DOI] [PubMed] [Google Scholar]
- 28.Healy GN, Matthews CE, Dunstan DW, Winkler EA, Owen N. Sedentary time and cardio-metabolic biomarkers in US adults: NHANES 2003-06. Eur Heart J. 2011;32(5):590–7. doi: 10.1093/eurheartj/ehq451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Willett W, Stampfer MJ. Total energy intake: implications for epidemiologic analyses. Am J Epidemiol. 1986;124(1):17–27. doi: 10.1093/oxfordjournals.aje.a114366. [DOI] [PubMed] [Google Scholar]
- 30.Qi Q, Strizich G, Merchant G, Sotres-Alvarez D, Buelna C, Castaneda SF, et al. Objectively Measured Sedentary Time and Cardiometabolic Biomarkers in US Hispanic/Latino Adults: The Hispanic Community Health Study/Study of Latinos (HCHS/SOL) Circulation. 2015;132(16):1560–9. doi: 10.1161/CIRCULATIONAHA.115.016938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lin DY, Wei L-J, Ying Z. Checking the Cox model with cumulative sums of martingale-based residuals. Biometrika. 1993;80(3):557–72. [Google Scholar]
- 32.Durrleman S, Simon R. Flexible regression models with cubic splines. Stat Med. 1989;8(5):551–61. doi: 10.1002/sim.4780080504. [DOI] [PubMed] [Google Scholar]
- 33.Harrell F. Regression modeling strategies: with applications to linear models, logistic and ordinal regression, and survival analysis. Springer; 2015. [Google Scholar]
- 34.Contal C, O’Quigley J. An application of changepoint methods in studying the effect of age on survival in breast cancer. Computational statistics & data analysis. 1999;30(3):253–70. [Google Scholar]
- 35.Ding P, VanderWeele TJ. Sensitivity Analysis Without Assumptions. Epidemiology. 2016;27(3):368–77. doi: 10.1097/EDE.0000000000000457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Li R, Hertzmark E, Louie M, Chen L, Spiegelman D. The SAS LGTPHCURV8 Macro. Boston, MA: Channing Laboratory; 2011. [Google Scholar]
- 37.Pandey A, Salahuddin U, Garg S, Ayers C, Kulinski J, Anand V, et al. Continuous Dose-Response Association Between Sedentary Time and Risk for Cardiovascular Disease: A Meta-analysis. JAMA Cardiol. 2016;1(5):575–83. doi: 10.1001/jamacardio.2016.1567. [DOI] [PubMed] [Google Scholar]
- 38.Celis-Morales CA, Perez-Bravo F, Ibanez L, Salas C, Bailey ME, Gill JM. Objective vs. self-reported physical activity and sedentary time: effects of measurement method on relationships with risk biomarkers. PLoS One. 2012;7(5):e36345. doi: 10.1371/journal.pone.0036345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Healy GN, Dunstan DW, Salmon J, Cerin E, Shaw JE, Zimmet PZ, et al. Breaks in sedentary time: beneficial associations with metabolic risk. Diabetes Care. 2008;31(4):661–6. doi: 10.2337/dc07-2046. [DOI] [PubMed] [Google Scholar]
- 40.Owen N, Healy GN, Matthews CE, Dunstan DW. Too much sitting: the population health science of sedentary behavior. Exerc Sport Sci Rev. 2010;38(3):105–13. doi: 10.1097/JES.0b013e3181e373a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Garber CE, Blissmer B, Deschenes MR, Franklin BA, Lamonte MJ, Lee IM, et al. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43(7):1334–59. doi: 10.1249/MSS.0b013e318213fefb. [DOI] [PubMed] [Google Scholar]
- 42.Atlas SJ, Deyo RA. Evaluating and managing acute low back pain in the primary care setting. J Gen Intern Med. 2001;16(2):120–31. doi: 10.1111/j.1525-1497.2001.91141.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Diaz KM, Howard VJ, Hutto B, Colabianchi N, Vena JE, Blair SN, et al. Patterns of Sedentary Behavior in US Middle-Age and Older Adults: The REGARDS Study. Med Sci Sports Exerc. 2016;48(3):430–8. doi: 10.1249/MSS.0000000000000792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gibbs BB, Hergenroeder AL, Katzmarzyk PT, Lee IM, Jakicic JM. Definition, measurement, and health risks associated with sedentary behavior. Med Sci Sports Exerc. 2015;47(6):1295–300. doi: 10.1249/MSS.0000000000000517. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


