Abstract
Integrating Biology and the Bedside (i2b2) is the de-facto open-source medical tool for cohort discovery. Fast Healthcare Interoperability Resources (FHIR) is a new standard for exchanging health care information electronically. Substitutable Modular third-party Applications (SMART) defines the SMART-on-FHIR specification on how applications shall interface with Electronic Health Records (EHR) through FHIR. Related work made it possible to produce FHIR from an i2b2 instance or made i2b2 able to store FHIR datasets. In this paper, we extend i2b2 to search remotely into one or multiple SMART-on-FHIR Application Programming Interfaces (APIs). This enables the federation of queries, security, terminology mapping, and also bridges the gap between i2b2 and modern big-data technologies.
Introduction
Learning Health Systems aim to maximize the potential of large-scale, harmonized data from variable, quickly developing digital sources such as Electronic Health Records (EHRs), which are emerging as powerful tools to facilitate discoveries that can improve health. Data heterogeneity is one of the critical problems in analyzing, reusing, sharing or linking datasets. With the development of platforms enabling the linking and federation of phenome, genome and exposome data across sites in US,1,2 Europe3,4 or at international scale5 a key challenge is to define harmonized access to heterogeneous EHR-based data.
i2b2 is the de-facto open-source medical tool for cohort discovery and allows healthcare practitioners to easily subset patient data to address research questions. i2b2 has been described as being used by more than 200 hospitals6 over the world, and the recent migration of i2b2 to GitHub has facilitated development work. The tool is flexible, supporting its own star schema and ontology model as well as exploiting alternative information models such as PCORnet7 and the OMOP common data model8 without requiring changes to the underlying data. Many initiatives have extended the primary goal of cohort discovery, providing functionality to carry out statistical analysis in place, as well as federated queries over multiple centers, and even genomic analytics.9,10 Well-known tools that extend the i2b2 functionality in this way include SHRINE, INSITE, tranSMART, and TRINETX9,11-13.
i2b2 and derived solutions do have room for improvement. For example, in terms of data variety, federation tools such as SHRINE, INSITE, and TRINETX are inconsistent in terms of their terminology mapping processes14. When mapping details are provided2, they are time consuming and software specific15. In terms of freshness of the data, Extract Transform Load processes (ETL) feeding traditional relational databases supported by the i2b2 tools (e.g. postgreSQL, Oracle, MSSQL) are resource consuming, taking considerable amounts of time, maintenance, and diskspace. Though ETL procedures are still feasible these days, the emergence of high-throughput healthcare data and the “Internet of Things” demands the development of new approaches that allow data to be queried in place (i.e. directly within EHRs) or in optimized, dedicated places such as RDF triple stores or NO-SQL databases. The time delta due to data migrations and transformations poses problems of data veracity because the source data is susceptible to be modified in the interval, and multiple transformations are error prone. In terms of data volume, data such as omics, exposomics, imaging or free text notes are more and more produced at hospital level while they still are challenging to store and therefore to analyse. In order for the data to be analyzed properly and efficiently, specialized and dedicated technologies are required. While there have been several engineering attempts to create i2b2 based data-warehouses solutions that work with technologies other than traditional relational databases16, the cost to create such interfaces is high. The i2b2 star schema model is highly optimized for fast retrieval of lists of patients matching criteria, but it is not intended for statistical analytics or data exploration17. Although there are some bridges with other common datamodels such as OMOP, the extended i2b2 architecture is still limited on RDBMS7. The emergence of new technologies is faster than i2b2’s ability to exploit them. In terms of software accessibility, for example, physicians spend time switching between applications, writing their login and password credentials again & again. Providing these users with the “one login/multiple application” paradigm would optimize the time spent on the computer and thus improve patient care.
The solution explored in this work is to bring the latest accomplishments of the Health Level Seven (HL7) Fast Healthcare Interoperability Resources (FHIR) community to i2b2. In particular, to bring the flexibility, the extensibility, the standardization, and the interoperability efforts of FHIR to i2b2. In the domain of patient care, several large-scale efforts have been underway for over a decade with the goal of specifying both the structure and the semantics of patient clinical information in a manner that enables computable semantic interoperability between diverse systems. Although there is no consensus in the medical informatics community regarding a standard patient information model, FHIR specifications are gaining interest and show promise to mitigate the classic site-specific data mapping problem. FHIR is built on lessons18 from previous standards, including the Reference Information Model (RIM) which became an ISO standard in 2003, and the Clinical Document Architecture designed to express a single clinical document as a message using HL7 version 3 RIM classes. FHIR specifies a RESTful API to access resources. Several initiatives facilitate the adoption of FHIR, including the Argonaut project19 and the Clinical Information Modeling Initiative (CIMI)20. SMART-on-FHIR21 is an open, standards based technology platform that enables innovators to create apps that seamlessly and securely run across the healthcare system. Using EHRs or data warehouses that support the SMART standard, patients, doctors, and healthcare practitioners can draw on this library of applications to improve clinical care, research, and public health. SMART improves the user experience with regard to login details in the way OAuthentication does for many websites, and there exist currently more than 50 applications that are able to consume FHIR resources in a consistent way.
FHIR and SMART-on-FHIR appear to be good candidates for overcoming several of i2b2’s architectural weaknesses. Several studies have explored how to bridge i2b2 and FHIR. One approach22 aims at allowing mobile phones to push FHIR resources into the i2b2 star schema. Other approaches23,24 allow an existing i2b2 instance to supply their star schema data through a FHIR-API, allowing SMART-on-FHIR applications to run on top of i2b2. In contrast to this prior work our proposal does the exact opposite, in that we build a general interface that allows i2b2 to consume data from any FHIR endpoint. This approach enables clinical datasets to be queried by exploiting FHIR search, Terminology Mapping25 and SMART Oauth2 security26 specifications. The aim is not only to bridge the gap between patient care and research communities, but also to open i2b2 to new and improved data types, as well as security and interoperability management in the context of scalable solutions for cross-border and cross-domain networking of data. The ultimate goal of the architecture presented in this paper is to allow multiple institutions to quickly and effectively engage in massive, international cohort discovery studies.
Methods
To meet our objectives, the existing i2b2 traditional query search module (i2b2crc) code source is extended to meet the SMART-on-FHIR API specifications and the FHIR search specifications. Figure 1 shows the overall architecture and how the three-tier i2b2 application integrates with remote institutions. The figure shows how an i2b2 application gives access to users in a SMART-on-FHIR application modality. In this context, users log-in to any SMART application or EHR system just once, and get access to a set of specialized applications, such as i2b2. The architecture allows queries to be combined over multiple endpoints: zero to one i2b2 star schemas and/or zero to many SMART-on-FHIR APIs.
Figure 1:
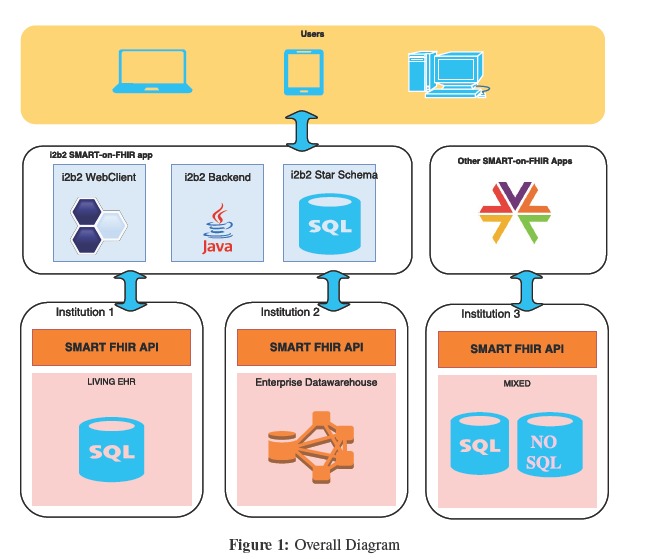
Overall Diagram
Figure 2is a detailed UML sequence diagram. The scenario describes a user who runs a query over an i2b2 instance containing both data in its star schema and data present in multiple remote FHIR-API endpoints. The solid arrows represent the specific new methods introduced in this work, the dotted arrows represent the existing i2b2 way of doing. The user first logs into the system with his or her login credentials, which are verified by the i2b2 project management cell (i2b2pm). The i2b2pm lets the user choose from an i2b2 project list according a set of defined roles. After building and running a multiple panel query across different medical domains, the user gets back a patient cohort set by picking concepts from the i2b2 ontology. Some domains are linked to the FHIR endpoints, others are linked to the local star schema. At first, the i2b2crc conducts a patient-set lookup in its local database. Then, for the FHIR-based concepts, the system loops over the following steps against the SMART-on-FHIR API. The i2b2pm first gets its Oauth2 authentication credentials because it is known as a trusted application within the SMART-Auth layer.
Figure 2:

UML Sequence Diagram
The i2b2crc new FHIR query builder then produces the HTTP query according to the FHIR-search specifications and makes an HTTP call to the FHIR-API. This query is extended with coding synonyms defined in the FHIR ConceptMap resources (terminology server part). The resulting query is then translated by the FHIR layer in the local database query dialect to fetch the results. The result is transformed into a FHIR json bundle only containing the information needed (patient_ids in this case). A parsing step extracts the patient_ids. They are then mapped to a unique i2b2 identifier and pushed into a temporary table that integrates all the results. Once looping is done, the i2b2crc applies a new patients security step to only keep those available for the i2b2 project selected by the user. The patient cohort set is finally returned to the user.
FHIR-search: FHIR search specifications25 describe how to communicate with a FHIR-API to get back a set of resources matching the criteria in an HTTP query. The present work exploits only the possibility to fetch one type of resource per query. This is sufficient because the traditional i2b2crc allows combining multiple filter predicates by processing each one separately and then uses a deliberation step based on temporary tables. The new i2b2crc query builder replaces the SQL queries acting over the star schema to fetch record identifiers (ID) with HTTP calls to a FHIR-API. The latter is then translated into the backend database system. The HTTP calls enabled in this design are presented in Table 1. The first row is the general template that is used, and is compared here with the SQL syntax (SELECT, FROM, WHERE):
- SELECT:
The <elements> pattern lists the resource elements that are returned by the FHIR-API. Depending on the user’s choice, patient ID, encounter ID, instance ID or date are retrieved, to respectively provide i2b2 “same patient”, “same encounter”, “same instance”, or “temporal queries” features. The way the i2b2crc retrieves those information from a given resource is described into the i2b2 FHIR config YAML file (see Figure 3).
- FROM:
The <Resource> pattern is supposed to be replaced by any existing FHIR standard resource, or any profiled resource (modification of the standard to meet the local institutions constraints). In order to let the user point to the right FHIR resource, the i2b2 traditional ontology table has been reused and populated with the needed information. Table 2 describes how to store the information into the “c_tablename” column.
- WHERE:
Both patterns <date_inf> and < date_sup> allow filtering the data based on the date range defined by the user at run time. The < custom_filter> allows to combine a predefined pattern, such as data status, or a userdefined filter based on a numerical or enumerated value (when enabled by filling the “c_metadataxml” column). The <codes> pattern can optionally specify a list of coding (e.g: from SNOMED, LOINC…) by populating the i2b2 ontology “c_basecode” column.
Table 1:
Index of HTTP request templates
| HTTP request | Description |
|---|---|
| GET <FHIR-API>/<Resource>? elements=<elements>&code=<codes> &date=gt<date inf>&date=lt<date sup> &<custom filter> | Retrieves chosen <elements> from resources optionally matching a date range or/and a list of <codes> or/and a <custom filter> |
| GET <FHIR-API>/ConceptMap?target-code=<codes> &target-system:in=<code-system> | Retrieves all codes that are mapped to <codes> & <code-system> |
Figure 3:

i2b2-FHIR YAML configuration file sample
Table 2:
i2b2 ontology adapted for FHIR
| ontology table columns | Description | Example |
|---|---|---|
| c_basecode | FHIR code_system / code pipe separated | FHIR:http://loinc.com|1234-5 |
| c_tablename | Resource / Profile pipe separated | Observation|ObservationAphp |
| c_metadataxml | An xml describing datatype (numeric, free text or enumerated) and measure units | cf: i2b2 documentation |
| c_dimcode | an optionnal additional filter | active=true&status=final |
FHIR-mapping: The second row of Table 1 describes the HTTP query template to enable terminology mapping. The i2b2crc cell is allowed to fetch synonym codes from the FHIR-Terminology server. As part of the ConceptMap25 resource, FHIR links a source code to a target with a set of semantic relation such as “equivalent” or “narrower” that characterize the way they relate to each other. The program fetches each mapping pair and only keeps the “wider” and “equivalent” semantic relations. The i2b2-FHIR code expansion exploits this mechanism to query over distinct code systems.
Outcome measurement: In order to test the FHIR DSTU3 resources compatibility coverage, the HAPI FHIR27 test server has been used as an endpoint since it contains useful demo datasets with fictitious patient data. The benchmark comparing traditional i2b2 (version 1.7.9) and FHIR-i2b2 was carried out with the same i2b2 “observation_fact” table containing 140 million records in a postgreSQL 9.6 instance. The FHIR-i2b2 has been set up by implementing HAPI-FHIR server on top of the observation_fact table into an Apache Tomcat 9 webserver, and has been accessed via the FHIR-i2b2 prototype. A FHIR-i2b2 big-data benchmark has been set up by implementing an HAPI-FHIR server on top of the MIMIC-III28 physiological data table multiplied by 15, and stored in an Apache HIVE2 table distributed over a 5-computer cluster in the Optimized Row Columnar (ORC) format distributed over HDFS. All software used: i2b2, HAPI-FHIR, postgreSQL and Apache Hive is open-source licensed.
Results
Implementation Status: The design presented below is implemented at 70%. To date, the new i2b2crc query builder is able to query on both a star schema and one remote FHIR endpoint simultaneously. Logical relations between selection criteria represented as multiple i2b2 webclient panels are also possible. The constitution of a “patient_set” can be constrained by dates, values and measurement units and by one or multiple codes. The code expansion based on FHIR terminology mapping is also implemented. A living demo is deployed29 and a screen-shot presented in Figure 4. The first panel query searched into HAPI FHIR test server for patients with LOINC glucose codes having value lower than 100ml/dl in a year range from 1979 to 2015 and is mixed with the second panel searching for patients having a diagnosis related to circulatory system within the star schema. The resulting “patient_set” contains about eight patients.
Figure 4:

i2b2-FHIR online demo screen-shot
Performance: The performance of i2b2-FHIR has been benchmarked (Figure 5a) versus a traditional i2b2 instance based on the star schema with the same amount of data and configuration (140 million records). The different patient set size corresponds to different criteria selection. The histogram shows traditional i2b2 is 20 times faster than the i2b2- FHIR version. The difference can be explained by the additional steps involved: the fetched result-set is transformed into a json bundle, sent over the network and then parsed. The performance factor tends to decrease with the number of patients matched. The second benchmark (Figure 5b) experimented connecting to an Apache HIVE table on a big-data platform containing 5 billion actual physiological patient data points. The results show that the time spent is under the minute and compatible with i2b2 promises. Moreover, the bar-plots show that the major bottleneck is the FHIR json generation step, mostly the part to produce the json (networking transfert is actually pretty fast). Such quantities of data have never been described to be handled by i2b2 before, since here we approach traditional RDBMS volume limitations. While the traditional i2b2 outperforms the FHIR based i2b2 on modest datasets, the latter opens new perspectives by enabling connections with specialized and optimized database systems.
Figure 5:


(a) Traditional versus i2b2-FHIR performance comparison (on a 150M postgreSQL table). (b) i2b2-FHIR performance (on a 5B Hive table)
i2b2 feature coverage: The i2b2 querying feature covers filtering patients facts by code, values, dates within an encounter temporal window or even a free sequence of events. By adding new temporal table mechanisms, the present work allows all of those features. Thus it does not limit the existing set of functionalities. The i2b2-FHIR configuration file Figure 3 contains information about the FHIR-API instance, such as its version, and how the resources are implemented. Depending on the kind of cohort set the user wants to extract, patient ID, encounter ID, instance ID or dates are retrieved from the FHIR-API thanks to a jsonPATH description. This then allows to populate the i2b2crc temporary tables. This is how i2b2 deliberation mechanisms can be populated, and the set built. Moreover the i2b2-FHIR implementation keeps backwards compatibility and does not impose FHIR-API usage for implementers that would not require it.
Security: A security layer has been proposed and implemented into the existing i2b2crc. A new i2b2 table allows to define which patient are part of which i2b2 project. This security layer is important because with one endpoint containing all patients records, it allows to create multiple projects with subset allowing multiple views on the dataset. In terms of performance, the table might be vertically partitioned and split by project, in order to get stable performance as the number of projects increases. This mechanism is both compatible with traditional i2b2 and i2b2-FHIR and has been deployed in production at the AP-HP hospitals where it handles more than 200 distinct projects. The Oauth2 security layer has not yet been implemented. The implementation will be inspired by the recent existing implementation such C3-PRO22 or SMART-on-FHIR23.
Extensibility: To date, the query builder is compatible with the current FHIR DSTU3 version. In the future, it will maintain compatibility with each FHIR release, and also backward compatibilities. The FHIR version of each endpoint is set up in the configuration file (Figure 3). Also it is possible to exploit most aspects ofFHIR extensibility, such local profiled resources, local specific resources or element extensions (through the “c_dimcode” of the i2b2 ontology table). The FHIR access layer has been tested over the HAPI FHIR test server for all resources at least referring to a patient (68 resources), and has a complete resource coverage. The results suggest that the design is flexible enough to query multiple centers with different FHIR implementations at the same time.
Interoperability: The FHIR-ConceptMap expansion has been implemented. A set of test mappings have been produced and populated into HAPI-FHIR as a proof of concept. The HTTP query described in Table 1 (row 2) allows to fetch the equivalent codes. While there is still room for improvement, the results open the way for massive and collaborative concept mapping, with a FHIR compatible terminology server. Interoperability is also derived from the FHIR standard resource definition. However, the ability to derive from them and build Profiled Resources is handled by the i2b2-FHIR YAML configuration flexibility together with the i2b2 ontology table, as they are designed to be adapted.
Discussion
FHIR abstraction allows designing a mixed architecture based on living EHRs and big-data repositories leveraging massive and unstructured clinical data. One can choose the best technology depending on the expected usage and local specificity of the data. This flexible design allows implementers to define their own i2b2 ontologies. Finally, an i2b2 federation over FHIR is able to bridge multiple FHIR implementations at the same time. The querying benchmarks showed that performance was not really an issue. There is also room for improvements there. High level performance improvement includes parallelizing the queries over both each hospital endpoint and each i2b2 panel. In order to manage heterogeneity in endpoint performance correctly, solutions such background queries have been proposed by SHRINE and could be reproduced. Low level performance improvement includes using more optimized code at bothi2b2 and FHIR endpoint side and at each step of the process: json building, json compression, json parsing. While the FHIR resource subset feature is already used to reduce the size of the bundles, we also will give feedback to the FHIR community to propose a more compact option. Finally the recent FHIR specifications around the GraphQL API language30 will enable both query optimizations and extensions in the future. For example, GRAPHQL allows mixing multiple FHIR resources and criteria in a single call, and this would enable to combine multiple i2b2 panel criteria into a single FHIR-API call. Such simplification is neither possible with the current i2b2-FHIR implementation nor with the traditional i2b2crc based on the star schema.
By leveraging access to big-data technologies, this opens a new-area of specific solutions (such as temporal-series, text-mining, distributed, graph databases) to manage the diversity, variety and volume of healthcare data such as Genomics31, Imaging, or physiological waveforms monitoring. The abstraction provided by the FHIR layer allows plugging new text specific technologies based on Apache Lucene, such SOLR & Elastic search. This will allow clinicians to mine texts as simply as a modern search engine does. Moreover, the interoperability gain from the FHIR interface makes possible to query multiple centers on real-time data (thanks to FHIR API direclty plugged on top of EHR) and the same way (thanks to FHIR Concept Mapping ability). The security was enforced and allows multiple sub projects to access subsets of the whole patient database. This provides a restricted access to the needed data by only authorized users accordingly to patient consenting rules.
Several modules have been implemented, some aspects of the design have only been tested as separate modules. The roadmap provides for the development of multiple SMART-on-FHIR endpoints access, Oauth2 implementation, performance improvements and also the release of i2b2 as part of the SMART-on-FHIR apps. Once satisfied with the results, the system should be available in the next releases of the core i2b2. While all resources containing patient reference were tested, there is a need to propose a general mapping between traditional i2b2 objects (patient, visit, provider, observation) and FHIR specific resources (Organization, HealthcareService, Patient, EpisodeOfCare, Condition, Procedure, Medication, MedicationRequest, Observation, DiagnosticReport, ClinicalImpression…). A general algorithm to translate FHIR terminologies into i2b2 ontology will also be investigated, and implemented as complementary software. Last but not least, as a standard way to represent concept mapping, the FHIR ConceptMap resource is a great candidate to centralize and share collaborative work and tools for this major purpose.
Conclusion
By bridging current modern solutions in the field of medical data, this work paves the way for improvements that address current Learning Health Systems challenges. The challenges of data federation, data interoperability, data freshness and data security can benefit from both i2b2 experience and FHIR simplification. The challenges of data volume and data variety of medical datasets are indirectly addressed by the FHIR-API abstraction that makes possible the use of powerful and dedicated technology.
In the end, while a tool that is able to bridge international institutions together is likely to emerge, concept mapping between many institutions remains a challenge to be addressed because the use of different languages, different granularities and different medical concepts. While ontology matching is an old research area, it still presents significant challenges to overcome.
References
- 1.Omri Gottesman, Helena Kuivaniemi, Gerard Tromp, W, Andrew Faucett, Rongling Li, Teri A. Manolio, Saskia C. Sanderson, Joseph Kannry, Randi Zinberg, Melissa A. Basford, et al. The electronic medical records and genomics (eMERGE) network: past, present, and future. Genetics in Medicine. 2013 Oct;15(10):761–771. doi: 10.1038/gim.2013.72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Andrew J., McMurry Shawn, Murphy N., Douglas MacFadden, Griffin Weber, William W. Simons, John Orechia, Jonathan Bickel, Nich Wattanasin, Clint Gilbert, Philip Trevvett, et al. SHRINE: Enabling nationally scalable multi-site disease studies. PLoS ONE. 2013 Mar;8(3):e55811. doi: 10.1371/journal.pone.0055811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Georges De Moor, Mats Sundgren, Dipak Kalra, Andreas Schmidt, Martin Dugas, Brecht Claerhout, Toresin Karakoyun, Christian Ohmann, Pierre-Yves Lastic, Nadir Ammour, et al. Using electronic health records for clinical research: The case of the EHR4CR project. Journal of Biomedical Informatics. 2015 Feb;53:162–173. doi: 10.1016/j.jbi.2014.10.006. [DOI] [PubMed] [Google Scholar]
- 4.Delaney Brendan C., Vasa Curcin, Anna Andreasson, Theodoros N. Arvanitis,, Hilde Bastiaens, Derek Corrigan, Ethier Jean-Francois, Olga Kostopoulou, Wolfgang Kuchinke, Mark McGilchrist, et al. Translational medicine and patient safety in Europe: TRANSFoRm-architecture for the learning health system in europe. BioMed Research International. 2015;2015:1–8. doi: 10.1155/2015/961526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.George Hripcsak, Jon D. Duke, Nigam H. Shah, Christian G. Reich, Vojtech Huser, Martijn J, Schuemie Marc A, Suchard Rae, Woong Park, Ian Chi Kei Wong, Peter R. Rijnbeek, et al. Observational health data sciences and informatics (OHDSI): opportunities for observational researchers. Studies in health technology and informatics. 2015;216:574. [PMC free article] [PubMed] [Google Scholar]
- 6.I. S. Kohane, S. E. Churchill, S. N. Murphy. A translational engine at the national scale: informatics for integrating biology and the bedside. J Am Med Inform Assoc. 2012;19(2):181–185. doi: 10.1136/amiajnl-2011-000492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jeffrey G Klann, Aaron Abend, Vijay A Raghavan, Kenneth D Mandl, Shawn N Murphy. Data interchange using i2b2. Journal of the American Medical Informatics Association. 2016 Sep;23(5):909–915. doi: 10.1093/jamia/ocv188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.i2b2-omop documentation. [Accessed: 2017-09-28]. https://community.i2b2.org/wiki/display/OMOP/OMOP+Home.
- 9.Elisabeth Scheufele, Dina Aronzon, Robert Coopersmith, Michael T. McDuffie, Manish Kapoor, Christopher A. Uhrich, Jean E. Avitabile,, Jinlei Liu, Dan Housman, Matvey B. Palchuk. tranSMART: an open source knowledge management and high content data analytics platform. AMIA Summits on Translational Science Proceedings. 2014;2014:96. [PMC free article] [PubMed] [Google Scholar]
- 10.i2b2-transmartwebsite. [Accessed: 2017-09-28]. https://avillach-lab.hms.harvard.edu/
- 11.G. M. Weber, S. N. Murphy, A. J. McMurry, D. MacFadden, D.J. Nigrin, S. Churchill, I. S. Kohane. The shared health research information network (SHRINE): A prototype federated query tool for clinical data repositories. Journal of the American Medical Informatics Association. 2009 Sep;16(5):624–630. doi: 10.1197/jamia.M3191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.insite website. [Accessed: 2017-09-28]. https://www.insiteplatform.com/
- 13.trinetx website. [Accessed: 2017-09-28]. https://www.trinetx.com/
- 14.Yannick Girardeau, Justin Doods, Eric Zapletal, Gilles Chatellier, Christel Daniel, Anita Burgun, Martin Dugas, Bastien Rance. Leveraging the EHR4CR platform to support patient inclusion in academic studies: challenges and lessons learned. BMC Medical Research Methodology. 2017 Dec;17(1) doi: 10.1186/s12874-017-0299-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rob Wynden, Mark G. Weiner, Ida Sim, Davera Gabriel, Marco Casale, Simona Carini, Shannon Hastings, David Ervin, Samson Tu, John H. Gennari, et al. Ontology mapping and data discovery for the translational investigator. Summit on Translational Bioinformatics. 2010;2010:66. [PMC free article] [PubMed] [Google Scholar]
- 16.Shicai Wang, Ioannis Pandis, Chao Wu, Sijin He, David Johnson, Ibrahim Emam, Florian Guitton, Yike Guo. High dimensional biological data retrieval optimization with NoSQL technology. BMC Genomics. 2014 Nov;15(8):S3. doi: 10.1186/1471-2164-15-S8-S3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.D. Firnkorn, S. Merker, M. Ganzinger, T. Muley, P. Knaup. Unlocking Data for Statistical Analyses and Data Mining: Generic Case Extraction of Clinical Items from i2b2 and tranSMART. Stud Health Technol Inform. 2016;228:567–571. [PubMed] [Google Scholar]
- 18.S. T. Rosenbloom, R. J. Carroll, J. L. Warner, M. E. Matheny, J. C. Denny. Representing knowledge consistently across health systems. Yearbook of Medical Informatics. 2017 Aug;26(01):139–147. doi: 10.15265/IY-2017-018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Argonaut wikipage. [Accessed: 2017-09-28]. http://argonautwiki.hl7.org/index.php?title=Main\_Page.
- 20.CIMI website. [Accessed: 2017-09-28]. http://www.opencimi.org/
- 21.SMART-on-FHIR website. [Accessed: 2017-09-28]. http://docs.smarthealthit.org/
- 22.Pascal B. Pfiffner, Isaac Pinyol, Marc D. Natter, Kenneth D. Mandl. C3-PRO: Connecting researchkit to the health system using i2b2 and FHIR. PLOS ONE. 2016 Mar;11(3):e0152722. doi: 10.1371/journal.pone.0152722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kavishwar B Wagholikar, Joshua C Mandel, Jeffery G Klann, Nich Wattanasin, Michael Mendis, Christopher G Chute, Kenneth D Mandl, Shawn N Murphy. SMART-on-FHIR implemented over i2b2. Journal of the American Medical Informatics Association. 2016 Jun;:ocw079. doi: 10.1093/jamia/ocw079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Abdelali Boussadi, Eric Zapletal. A fast healthcare interoperability resources (FHIR) layer implemented over i2b2. BMC Medical Informatics and Decision Making. 2017 Dec;17(1) doi: 10.1186/s12911-017-0513-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.FHIR specifications. [Accessed: 2017-09-28]; https://www.hl7.org/fhir/ [Google Scholar]
- 26.SMART-on-FHIR specifications. [Accessed: 2017-09-28]. http://docs.smarthealthit.org/
- 27.HAPI-FHIR website. [Accessed: 2017-09-28]. http://hapifhir.io/
- 28.AE Johnson, TJ Pollard, L Shen, LW Lehman, M Feng, M Ghassemi, B Moody, P Szolovits, LA Celi, RG Mark. MIMIC-III, a freely accessible critical care database. Sci Data. 2016 May 24;3:160035. doi: 10.1038/sdata.2016.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.i2b2-FHIR demo website. [Accessed: 2017-09-28]. http://34.205.31.28/webclient/
- 30.FHIR graphql specifications. [Accessed: 2018-01-03]. https://build.fhir.org/graphql.html.
- 31.Gil Alterovitz, Jeremy Warner, Peijin Zhang, Yishen Chen, Mollie Ullman-Cullere, David Kreda, Isaac S. Kohane. SMART on FHIR genomics: Facilitating standardized clinico-genomic apps. Journal of the American Medical Informatics Association. 2015 Jul;:ocv045. doi: 10.1093/jamia/ocv045. [DOI] [PMC free article] [PubMed] [Google Scholar]


