Abstract
Social determinants of health (SDOH) are important considerations in diagnosis, prevention, and health outcomes. However, they are often not well documented in the EHR and found primarily in unstructured or semi-structured text. Building upon previous work, we analyzed all flowsheet data in 2013 for information related to the SDOH topic areas of Residence, Living Situation, and Living Conditions. Overall, 91 rows were identified as being related to the topics areas resulting in 604,616 unique observations. Individual rows contained SDOH data often covered multiple concepts especially free-text entries. These data included most often references to the residence, residence details, and with whom the patient lives. Very few contained living condition references. Additionally, there was significant duplication and inconsistency of row labels, as well as variation in value list content for rows collecting the same concepts. Our findings demonstrate significant opportunities to improve and achieve better standardization in documentation around these SDOH.
Introduction
Social and individual behavioral factors play an important role in diagnosis, prevention, health outcomes, and quality of life.1-4 Social determinants of health (SDOH) in many instances have a profound impact on our overall health. SDOH includes behavioral components, such as alcohol, drug, and tobacco use, as well as physical environmental factors that can influence the patient’s health such as living conditions, social support, occupation, and physical activities.1 They have been shown to contribute to mortality, as well as a causal mechanism for disease.5-9 Insecurity related to housing has been associated with poor health among children,10 barriers related to access to health care,11 and chronic disease management.12 Living situation, such as residence type, with whom the patient lives, housing density, physical living conditions, and social support, all have been shown to have significant impact on a patient’s health outcomes.13, 14 The National Academy of Medicine (NAM), formerly Institute of Medicine (IOM), suggests that a health policy framework implemented around SDOH would achieve better population health, less inequality, and lower costs.15 There are many public health related initiatives aimed at addressing social determinants and health outcomes as well as recommendations by NAM for SDOH documentation in the EHR.16-18.
While much work has been done to demonstrate the effect of behaviors such as alcohol and tobacco use on health outcomes,19 the majority of other social determinants have not been investigated as thoroughly. In general, housing insecurity has been associated with poor health in children, has been shown to have an impact on chronic disease management, and is linked to depression, stress, smoking, and drug use.10-12 Housing, for example, has been studied with respect to the impact of homelessness on various conditions and housing related exposures.20-28 However, little work has been done around examining the health affects of housing density or with whom the patient lives.29 Knowledge regarding the patient’s physical living space, with whom the patient lives, and related exposures would benefit clinicians and other stakeholders in providing appropriate care as well as facilitation of appropriate housing interventions when needed.30
The tremendous increase in the use of EHRs provides unprecedented opportunity to collect and analyze patient data. Even though SDOH documentation has increased in the EHR, social history information is often lacking or inadequate despite its fundamental role in understanding the context of the patient’s story.31 Having SDOH data available in a format that can be analyzed and reused for clinical care along with other associated clinical data would enable development of more informative clinical decision support tools, better evaluation of patient outcomes, generation of additional evidence based care guidelines, and identification of patients who may benefit from special services or interventions or those who may be at higher risk for potentially preventable events.
However, well-designed discrete data collection tools for many aspects of social history information have not been widely developed and incorporated to the EHR. Currently, our work has shown that SDOH documentation may be documented as structured data or unstructured text (e.g., in clinical notes or free-text data collection fields).32 Moreover, end-users and healthcare institution are left to utilize ill-fitting tools for data collection such as flowsheets. Also, it is common practice for health care organizations to customize their EHR, such as work building flowsheets or other tools to fit specific workflows. In some cases, this customization results in SDOH information be documented in various areas of the chart ultimately making this information difficult for providers to locate. Lastly, comprehensive standards have not yet been developed to encompass all the SDOH topic areas especially the topic areas of interest in this work, namely: Residence, Living Situation, and Living Conditions. In previous work, we found overall that Systematized Nomenclature of Medicine - Clinical Terms (SNOMED CT) was the most comprehensive source covering these three topic areas followed by the Omaha System.33 However, both of these sources lacked substantial detail pertaining to the three target topic areas of interest in this work. There is ongoing work to map flowsheet rows to coding systems such as SNOMED CT and Logical Observation Identifiers Names and Codes (LOINC®). 34, 35 However, those data models are still under development and, as such, they are not quite ready for widespread use in clinical documentation.
Flowsheets are critical tools in the EHR for documenting longitudinal data and information such as assessments and observations, as well as providing checklists for routine care tasks. Nurses and allied health staff, such as social workers, physical therapists, and occupational therapists are the typical primary documenters and users of flowsheet data. Since they are used by many different members of the interdisciplinary care team, they naturally provide a mechanism for communication between team members as well as the ability to combine the documentation from disparate disciplines into a single format for visualization.
In the Epic EHR, flowsheets are very flexible in design and fairly easy to build and implement; thus, they offer a popular option for building discrete data collection tools. A flowsheet “Row” is equivalent to a field in a database designed to collect “Observations” or data points. Each flowsheet row can be formatted to collect measure values (e.g., as free-text, numeric, or selection from a custom list) and each row also allows for the entry of free-text comments to accompany each measure value. Flowsheet displays are similar to spreadsheets and are intended to document brief results. Longer text strings or larger blocks of free-text cannot be displayed completely, and therefore these data are cumbersome to review in this format. Lastly, information entered as measure value comments are free-text blocks and are not accessible for typical clinical decision support purposes or for secondary use in population health research. Since flowsheets are so flexible and easy to implement, they can be overused or sometimes misused. The sheer number of rows and the organizational structure can get unwieldy unless care is taken in planning and design of these tools to ensure that each row is unique to capture a specific discrete measurement or concept.
This study is focused on the three target topic areas of Residence, Living Situation, and Living Conditions. Using definitions developed from previous work, Residence describes dwelling types, physical residence, and geographic location and includes safety considerations such as railings or number of floors and steps. Living Situation describes with whom the patient lives such as roommates, family members, multi-resident dwelling as well as how many others they live with. Lastly, Living Conditions describes environmental cleanliness and precautions against infection and disease and includes such things as animals, and presence of mold or an unclean living space.
The goals of this descriptive study were to: (1) examine flowsheet rows relevant to the three target topic areas and (2) characterize flowsheet documentation content and compare flowsheet content to that found in previous work, which analyzed existing standards and terminologies as well as unstructured text.32, 33
Methods
Data Sources
The data used in this study originated from the Fairview Health System (FHS) EHR system and included only data from inpatients from 2013 who had consented for their medical records to be used in research. The primary data source for this work was the Academic Health Center Information Exchange (AHC-IE) data repository, which contains clinical data from the University of Minnesota (UMN), Academic Health Center (AHC), FHS, University of Minnesota Physicians (UMP), and other external data sources (e.g., geocoding data and Minnesota Department of Health death data). Our data exploration focused on EHR data for inpatient visits for 2013 for both FHS and UMP.
Flowsheet Review
A complete dataset of all unique flowsheet row unique IDs, system names, and display names, were extracted from the AHC-IE including rows that had been retired. System Names are names given to the rows which are not visible to the end user whereas the Display Names are visible to the end user when they are documenting. The dataset was systematically searched using the list of search terms compiled from previous work, which reviewed existing interface terminologies, standards, specifications, coding terminologies, vocabularies, documentation guidelines, measures, and surveys.33 The complete dataset of flowsheet rows was then also manually reviewed to ensure complete capture of rows that may have been missed with the search term list and related rows identified. The final set of search terms obtained from the flow sheet data review are summarized in Table 1.
Table 1.
Final set of search terms for flow sheet review.
| Search terms from standards | Added search terms from flowsheet review |
|---|---|
| “home”, “house”, “housing”, “residence”, “live”, “living”, “lives”, “people”, “mold”, “insect”, “rodent”, “water”, “heat”, “social”, “density” | “Stairs”, “railings”, “safety”, “safe”, “facility”, “group home”, “skilled nursing facility”, “assisted living facility”, “support system”, “family”, “support”, “housing conditions”, “caregiver”, “bathroom”, “community support”, “rehab”, “assistive device”, “social/environment”, “equipment”, “social support”, “household”, “transitional care”, “social connectedness”, “live alone” |
For all rows identified as being related to the three topic areas, observation measure values and observation free-text comments were extracted. Each of the flowsheet rows and observations were examined to ensure relevance to one or more of the three topic areas and unrelated rows and observations were excluded. Rows and observations found to not be related to one or more of the three topic areas were removed from the dataset the final set of observation measure values and observation comments were reviewed. Rows were classified into target domain categories, and sorted based on data collection type, i.e., rows designed to be entered using a drop-down value list or by the entry of free-text. For those rows utilizing drop-down value lists, the complete value list values were extracted, combined, and sorted to develop harmonized value lists for the elements. Meta-data for rows utilizing value lists that included frequency of value lists updates were examined. Measure values from rows that were free-text entry as well as comment text were compiled and reviewed. Lastly the overall flowsheet documentation content was compared to content findings from previous standards work (Figure 1).32, 33
Figure 1:
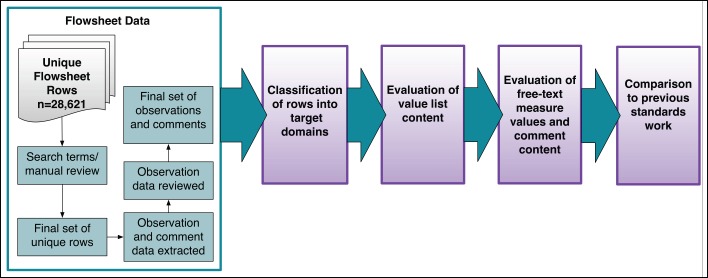
Flowsheet review methods.
Results
Flowsheet Observations
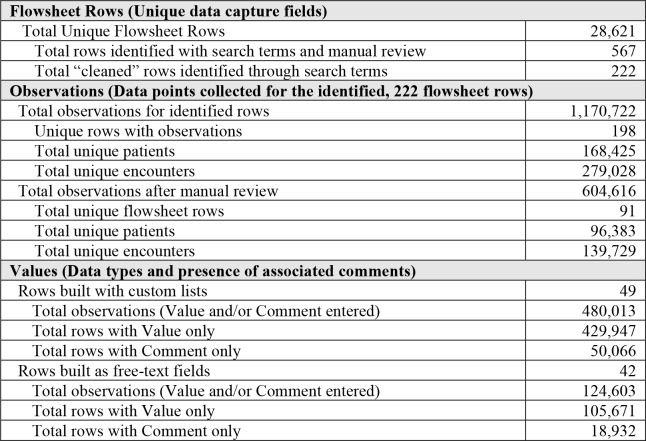
The 28,621 unique flowsheet rows system and display names were analyzed systematically using search terms (Table 1). The initial analysis yielded an initial set of 567 rows that were potentially relevant to the target topic areas. After manual review of system and display names, rows found to be unrelated to the topic areas were removed resulting in a final list of 222 unique flowsheet rows that could potentially contain data related to the three topic areas of interest.
Flowsheet observation data were extracted from the AHC-IE database for these 222 rows resulting in an initial dataset containing 198 unique flowsheet rows with a total of 1,170,722 observations. Twenty-four of the 222 flowsheet rows were not documented on in the study period so, while they were in the list of rows, they were not represented in the final set of observations. This observation dataset represented 169,425 unique patients and 279,028 encounters. The 198 unique flowsheet rows were reviewed for relevance to the three topic areas and 107 rows were removed form the dataset leaving a total of 91 unique flowsheet rows found to be related to one or more of the three target topic areas (Table 2).
Table 2.
Summary of Flowsheet Rows, Observations, and Values.
Of the 91 unique flowsheet rows, 49 were found to have been built using custom lists, i.e., pre-built value lists that the user can select from. The remaining 42 rows were built as free-text measure values. Of the 49 rows built with custom lists, 41 were designed to allow the user to select multiple values from a custom list.32 The 49 rows with custom lists accounted for a total of 480,013 observations where there was either a measure value or comment documented. For 50,066 observations, the measure value was null but there was a free-text comment entered. The 42 rows built as free-text fields resulted in 124,603 observations, i.e., observations that had a value, comment, or both. Of these, 18,932 observations had a null measure value but had a free-text comment entered.
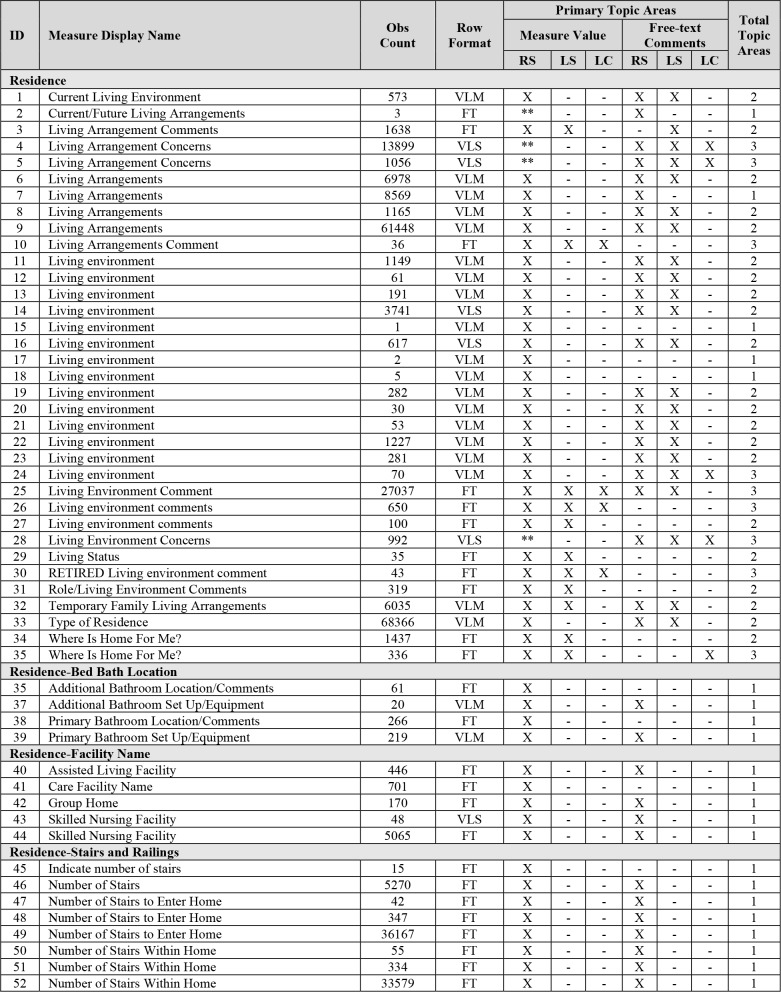
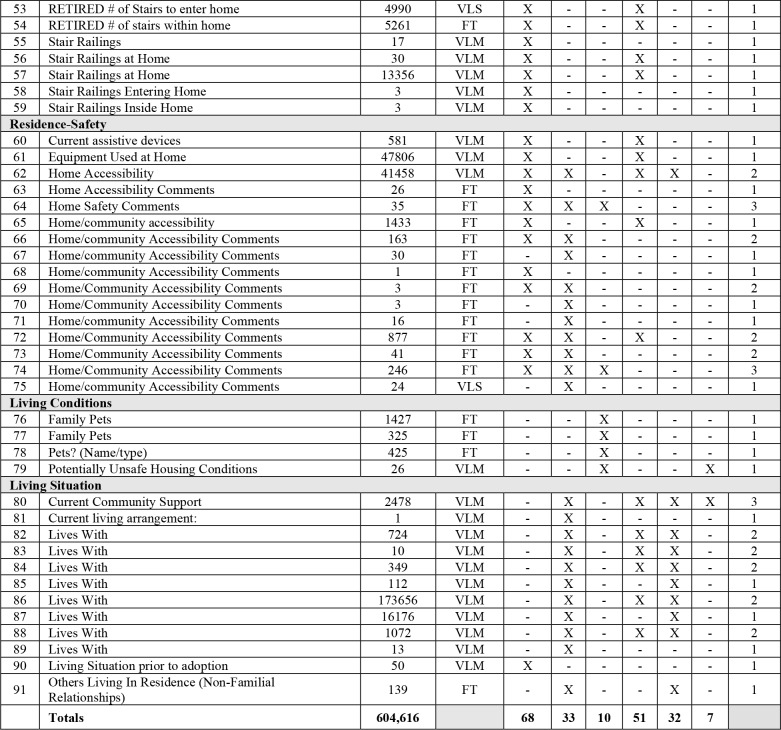
Table 3 characterizes the final dataset comprised of 91 unique flowsheet rows identified after manual review and the total count of observations found for each row during the study period. The Row Format column indicates the data type of the row measure value observation, i.e., whether the row is a free-text entry or uses a value list, i.e. hard coded list of options to select from with single or multiple select. This table is sorted alphabetically by Measure Display Name to show the duplication in concepts being collected via separate flowsheet rows and variation in the way identical measures are being collected wither by formatted list of single-and multi-select options or by free-text Each row measure value was categorized according to topic area as were free-text comments. Many rows covered more than one of the three topic areas as shown in the last column “Total Topic Areas”.
Table 3.
Unique flowsheet rows with observation counts and topic areas. Obs Count: number of observations for the row in the final dataset. Row Format (Data Type): FT=free-text, VLM=value list multi-select, VLS=value list single-select. Topic Areas: RS=Residence, LS=Living Situation, LC=Living Conditions. **Value lists contained only “yes” and “no” values with free-text comments.
Of the total 91 rows, 46% (42) were built for free-text documentation, 45% (41) were built with value lists that allowed for multiple values to be selected from the value list, and 9% (8) were built with value lists that allowed only one value to be selected from the list. Of the 49 rows with value lists, 34 had value lists that contained values related to Residence, 13 related to Living Situation, and 1 had a value list related to Living Conditions. Overall, 53% (48) of the 91 rows contained data related to a single topic area, 34% (31) contained data related to two topic areas, and 13% (12) contained data related to all three topic areas. Of the 42 rows with value lists, 62% (26) contained data for a single topic area, 21% (9) two topic areas, and 17% (7) to all three topic areas. Of the 49 rows that were built to collect free-text, 45% (22) contained data related to a single topic area, 45% (22) related to 2 topic areas, and 10% (5) contained data related to all three topic areas. Lastly there were two rows “Living Environment Concerns” and “Living Arrangement Concerns” that had values of “YES” and “NO”.
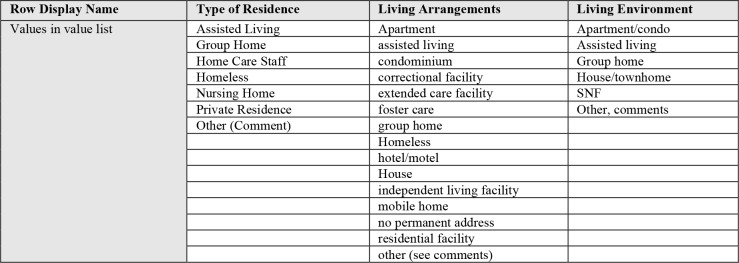
In flowsheet rows that were built with the intention of collecting the same information or concepts, the row display names and the value lists were not consistent across those rows. Table 4 shows an example of three flowsheet rows that had different display names and different value list members but all three were intended to capture the type of dwelling in which the patient lived.
Table 4.
Row display name and value lists for rows documenting the type of physical residence.
There was also inconsistent terminology used to label the free-text rows. Comparing rows with the same display name there was variability in what data the row was intended to collect. For example “Living Environment” rows that in most cases were intended to document residence type with value lists but in some cases the row was intended to document stairs and railings outside and inside the home. Subsequently, the measure values from the 49 rows with value lists were compiled into separate lists for each of the related elements (Table 5).
Table 5.
Flowsheet measure value list compilation (raw data) categorized in the three topic areas.
| Residence Type | Residence Stairs & Railings | Residence Safety (Assistive devices) | |
|---|---|---|---|
| Adult Foster Care | House | entering home | Bath bench |
| Apartment | House/townhome | inside home | Bath not on first floor |
| Apartment/condo | Independent living facility | inside, present at both sides | Bed and bath are not on the first floor |
| Assisted Living | Mobile home | inside, present on left side | Bed not on first floor |
| Condominium | No permanent address | inside, present on right side | Extended tub bench |
| Correctional facility | Nursing Home | none entering home | Grab bars present (bathtub) |
| Extended care facility | Orphanage | none inside home | Grab bars present (toilet) |
| Foster care | Private Residence | other (must comment) | Hand held shower |
| Group Home | Residential facility | other (see comments) | Raised toilet |
| Home | Ronald McDonald House | outside, present at both sides | Ramps present at home |
| Home Care Staff | Shelter | outside, present on left side | Shower grab bar |
| Homeless | SNF | outside, present on right side | Shower stall |
| Hope Lodge | Staying with family | present at both sides | Shower/tub chair |
| Hospitality house | Staying with friends | present of both sides | Toilet |
| Hotel | Townhome/townhouse | present on left side | Toilet grab bar |
| Hotel/motel | present on right side | Tub/shower combo | |
| stairs (1 railing present) | Tub/shower is not walk in | ||
| stairs (2 railings present) | |||
| stairs to enter home | |||
| stairs within home | |||
| entering home | |||
| <number> | |||
| <number x # flights> | |||
| Living Situation Subject | Living Conditions Type | ||
| Adoptive parent(s) | Grandfather | Chipped paint | No running water |
| Alone | Grandmother | Insects/pests | No smoke detector |
| Aunt | Grandparents | No air conditioning | No working appliances |
| Birth family | Half-brother | No electricity | Other (see comments) |
| Brother | Half-sister | No heat | Paint chipped |
| Child(ren) | Host family | No hot water | Stairwells unsafe |
| Child(ren), adult | Legal guardian | No indoor plumbing | Unable to assess |
| Child(ren), dependent | Mother | No lighting | Unsafe stairwells |
| Domestic partner | Mother and partner | No phone | Windows broken |
| Father | Other (see comments) | ||
| Father and partner | Other relative(s) (specify) | ||
| Foster care | Parent(s) | ||
| Foster family | Room mate | ||
| Foster parent(s) | Sibling(s) | ||
| Friend(s) | Significant other | ||
| Grandchild(ren) | |||
Groupings generated five concepts: (1) Residence Type, (2) Residence Stairs and Railings, (3) Resident Safety, (4) Living Situation Subject, and (5) Living Conditions Type. The value lists showed variability in terms used as well as terms that did not necessarily belong (e.g., names of facilities like “Ronald McDonald House”).
Lastly, differences were found in the format of a number of the rows collecting similar data. For example, five unique rows were found that were intended to collect the names and contact information for care facilities each one specific to the facility type. Four of the five flowsheet rows were built as free-text measure values. Two of the rows had the same display name but one was a free-text measure value and the other was built as a custom list.
Discussion
SDOH play an important role in the provision of care. However, EHRs, for the most part, often do not contain well-designed documentation tools to collect these data or standardized storage of this information for clinical care and secondary uses. In our analysis of a large healthcare enterprise and three key SDOH, we observed that much of this information is documented in free-text form in notes or in flowsheets rows, the latter of which was the focus of this study. Flowsheets allow for documentation in a longitudinal manner; however, their format is really most efficient for short answer or numeric values. Their ongoing management across settings and certain types of care remains an important challenge. This study demonstrates that flowsheet tools are being used to document SDOH. However, the overall design of these tools is not optimal and the use of any specific standard or terminology is not clearly evident, which has broad implications to interoperability and secondary use of these data.
In total, 91 rows were found to contain either measures and/or free-text comments related to the three topic areas. Of the 49 rows built with value lists, there was significant duplication in rows with regards to naming and also multiple rows seemingly built to collect the same concepts. For example, 22 unique rows were related to Residence and were built with value lists to collect the type of dwelling in which the patient lives. We found inconsistencies in terminology used to label rows as well as inconsistencies in terminology and content in value lists. For example, Residence Type was documented in rows that were labeled “Type of Residence”, “Living Arrangements”, and “Living Environment”. This duplication and inconsistency demonstrates a need for more rigorous content and knowledge management of EHR documentation tools as well as a need for more attention towards overall design and architecture.
The free-text comments in many cases did not match the intent of the flowsheet row as determined by review of the value lists associated with the row. For example, the row “Type of Residence”, which was built as a multi-select value list, had free-text comments that included the name of the facility, who was living with the patient in that residence, location such as addresses, and information related to residence details such as stories and stairs. In another row entitled “Lives with”, the free-text comments included information such as the facility name, dwelling type, pets (numbers and names), details about where other family members live, and number of children and their ages.
A comparison of the flowsheet value lists compiled from this work (Table 5) with the value lists obtained from previous standards work33 demonstrated overall similar values for residence type and living conditions although some standards, most prominently SNOMED CT, were more comprehensive in these topic areas. However, we found differences in details specifically values related to stairs, railings, and installed safety devices. The amount of flowsheet documentation found regarding these details, could indicate the importance and relevance of this information for patient care and therefore should be included in future comprehensive standards development work.
Another issue found was excessively long value lists that were high maintenance. The row “Skilled Nursing Facility” had a value list that contained well over 100 items. The value list items were composed of residential facility names, locations, and phone and fax numbers. Flowsheet metadata for these rows indicated that these value lists are updated frequently as facility names or phone and fax numbers change thus this model requires more maintenance to stay current. This brings to question whether a flowsheet is the optimal location in the EHR for a patients place of residence. The EHR does contain a designated place for patients address in the demographics section; however, many times for patients who live in residential facilities, the address entered into the patient demographics may be that of a relative or guardian. Also, since flowsheets are not necessarily readily available to all providers, it may be better to have residential facility information located elsewhere in the EHR such as in the demographic sections of the chart where it is more readily accessible for viewing and updates but separate from the billing address.
Next steps for this work include compiling and harmonizing the flowsheet value lists with the value lists from previous work evaluating existing standards and EHR free-text documentation.32, 33 In addition, formal annotation techniques could be used to enhance natural language processing tools for these topic areas. Since the ultimate goal is to update the model representation from previous work, that modeling should be done using formal model representation tools such as openEHR, as well as aligning the model with existing standards such as Clinical Information Modeling Initiative and terminologies such as the Omaha System36 for the three topic areas of Residence, Living Situation, and Living Conditions. Lastly, future work could also include an examination of patient level SDOH versus environmental level SDOH and impact to health outcomes.
Conclusion
In summary, this study demonstrated the wide variation in the design and use of flowsheet rows as data collection tools for SDOH information related to Residence, Living Situation, and Living Conditions. In addition, data quality is less than optimal due to the lack of standards in terminology for the element names and the value lists as well as the extensive use of free-text measure values and comments. As a result, there remains an opportunity to redesign these flowsheet rows to create efficiencies in documentation and to optimize the quality of the data being collected through pruning and combining of similar concepts into fewer rows and developing comprehensive standards and utilizing coding systems for these data. Overall, the lack of standards for SDOH documentation has implications for interoperability and secondary use of data.
Acknowledgements
This work was supported by the National Library of Medicine of the National Institutes of Health (R01LM011364) and University of Minnesota Clinical and Translational Science Award (8UL1TR000114-02). The content is solely the responsibility of the authors and does not represent the official views of the National Institutes of Health.
Table and Figures
References
- 1.Healthy People. Gov: U.S. Department of Health & Human services. [cited 2015 3/2/2015];2012 Available from: http://www.healthypeople.gov/2020/topicsobjectives2020/overview.aspx?topicid=39. [Google Scholar]
- 2.National Research Council. Washington DC: National Research Council: The National Academies Press; 2006. Genes, Behavior, and the Social Environment: Moving Beyond the Nature/Nurture Debate. [PubMed] [Google Scholar]
- 3.Social Determinants of Health: World Health Organization. [cited 2014 1/7/2014];2014 Available from: http://www.who.int/social determinants/sdh definition/en/index.html. [Google Scholar]
- 4.Monsen KA, Brandt J. K., Brueshoff B., Chi C. L., Mathiason M. A., Swenson S. M., Thorson D. R. Social determinants and health disparities associated with outcomes of women of childbearing age receiving public health nurse home visiting services. Journal of Obstetric, Gynecologic, & Neonatal Nursing. 2017 doi: 10.1016/j.jogn.2016.10.004. [DOI] [PubMed] [Google Scholar]
- 5.McGinnis JM, Foege WH. Actual causes of death in the United States. JAMA. 1993;270(18):2207–12. [PubMed] [Google Scholar]
- 6.Marmot MG, Shipley MJ, Rose G. Inequalities in death-specific explanations of a general pattern? Lancet. 1984;1(8384):1003–6. doi: 10.1016/s0140-6736(84)92337-7. [DOI] [PubMed] [Google Scholar]
- 7.McGinnis JM. Health in America--the sum of its parts. JAMA. 2002;287(20):2711–2. doi: 10.1001/jama.287.20.2711. [DOI] [PubMed] [Google Scholar]
- 8.Link BG, Phelan J. Social conditions as fundamental causes of disease. J Health Soc Behav. 1995:80–94. [PubMed] [Google Scholar]
- 9.Babor TF, Sciamanna CN, Pronk NP. Assessing multiple risk behaviors in primary care. Screening issues and related concepts. Am J Prev Med. 2004;27(2 Suppl):42–53. doi: 10.1016/j.amepre.2004.04.018. [DOI] [PubMed] [Google Scholar]
- 10.Cutts DB, Meyers AF, Black MM, Casey PH, Chilton M, Cook JT, et al. US Housing insecurity and the health of very young children. Am J Public Health. 2011;101(8):1508–14. doi: 10.2105/AJPH.2011.300139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bisgaier J, Rhodes KV. Cumulative adverse financial circumstances: associations with patient health status and behaviors. Health Soc Work. 2011;36(2):129–37. doi: 10.1093/hsw/36.2.129. [DOI] [PubMed] [Google Scholar]
- 12.Vijayaraghavan M, Jacobs EA, Seligman H, Fernandez A. The association between housing instability, food insecurity, and diabetes self-efficacy in low-income adults. J Health Care Poor Underserved. 2011;22(4):1279–91. doi: 10.1353/hpu.2011.0131. [DOI] [PubMed] [Google Scholar]
- 13.Thomson H, Thomas S, Sellstrom E, Petticrew M. Housing improvements for health and associated socioeconomic outcomes. Cochrane Database Syst Rev. 2013;2:CD008657. doi: 10.1002/14651858.CD008657.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shaw M. Housing and public health. Annu Rev Public Health. 2004;25:397–418. doi: 10.1146/annurev.publhealth.25.101802.123036. [DOI] [PubMed] [Google Scholar]
- 15.Adler NE, Cutler DM, Fielding JE, Galea S, Glymour MM, Koh HK, et al. Addressing Social Determinants of Health and Health Disparities: A Vital Direction for Health and Health Care 2016. [cited 2017 February 18, 2017]; Available from: https://nam.edu/wp-content/uploads/2016/09/Addressing-Social-Determinants-of-Health-and-Health-Disparities.pdf. [Google Scholar]
- 16.Denise Koo, PWOC, Andrea Harris, Karen B. DeSalvo. An Environmental Scan of Recent Initiatives Incorporating Social Determinants in Public Health. 2016 Jun 30; doi: 10.5888/pcd13.160248. 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.IOM (Institute of Medicine) Washington, D.C.: The National Academies Press; 2014. Capturing social and behavioral domains in electronic health records: Phase 1. Available from: http://nationalacademies.org/hmd/Reports/2014/Capturing-Social-and-Behavioral-Domains-in-Electronic-Health-Records-Phase-1.aspx. [PubMed] [Google Scholar]
- 18.IOM (Institute of Medicine) Washington, D.C.: The National Academies Press; 2014. Capturing Social and Behavioral Domains and Measures in Electronic Health Records: Phase 2. Available from: http://nationalacademies.org/hmd/Reports/2014/EHRdomains2.aspx. [PubMed] [Google Scholar]
- 19.Jane-Llopis E, Matytsina I. Mental health and alcohol, drugs and tobacco: a review of the comorbidity between mental disorders and the use of alcohol, tobacco and illicit drugs. Drug Alcohol Rev. 2006;25(6):515–36. doi: 10.1080/09595230600944461. [DOI] [PubMed] [Google Scholar]
- 20.Kipke MD, Weiss G, Wong CF. Residential status as a risk factor for drug use and HIV risk among young men who have sex with men. AIDS Behav. 2007;11(6 Suppl):56–69. doi: 10.1007/s10461-006-9204-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Milloy MJ, Marshall BD, Montaner J, Wood E. Housing status and the health of people living with HIV/AIDS. Curr HIV/AIDS Rep. 2012;9(4):364–74. doi: 10.1007/s11904-012-0137-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Suglia SF, Duarte CS, Sandel MT. Housing quality, housing instability, and maternal mental health. J Urban Health. 2011;88(6):1105–16. doi: 10.1007/s11524-011-9587-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Weinstein LC, Lanoue MD, Plumb JD, King H, Stein B, Tsemberis S. A primary care-public health partnership addressing homelessness, serious mental illness, and health disparities. J Am Board Fam Med. 2013;26(3):279–87. doi: 10.3122/jabfm.2013.03.120239. [DOI] [PubMed] [Google Scholar]
- 24.Costa-Font J. Housing assets and the socio-economic determinants of health and disability in old age. Health Place. 2008;14(3):478–91. doi: 10.1016/j.healthplace.2007.09.005. [DOI] [PubMed] [Google Scholar]
- 25.Rollins C, Glass NE, Perrin NA, Billhardt KA, Clough A, Barnes J, et al. Housing instability is as strong a predictor of poor health outcomes as level of danger in an abusive relationship: findings from the SHARE Study. J Interpers Violence. 2012;27(4):623–43. doi: 10.1177/0886260511423241. [DOI] [PubMed] [Google Scholar]
- 26.Ryan TJ, Arnold KJ. Residential carbon monoxide detector failure rates in the United States. Am J Public Health. 2011;101(10):e15–7. doi: 10.2105/AJPH.2011.300274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Adamkiewicz G, Zota AR, Fabian MP, Chahine T, Julien R, Spengler JD, et al. Moving environmental justice indoors: understanding structural influences on residential exposure patterns in low-income communities. Am J Public Health. 2011;101(Suppl 1):S238–45. doi: 10.2105/AJPH.2011.300119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jackson SL, Bonnie RJ. A systematic examination of smoke-free policies in multiunit dwellings in Virginia as reported by property managers: implications for prevention. Am J Health Promot. 2011;26(1):37–44. doi: 10.4278/ajhp.091005-QUAN-329. [DOI] [PubMed] [Google Scholar]
- 29.Standish K, Nandi V, Ompad DC, Momper S, Galea S. Household density among undocumented Mexican immigrants in New York City. J Immigr Minor Health. 2010;12(3):310–8. doi: 10.1007/s10903-008-9175-x. [DOI] [PubMed] [Google Scholar]
- 30.de Vet R, van Luijtelaar MJ, Brilleslijper-Kater SN, Vanderplasschen W, Beijersbergen MD, Wolf JR. Effectiveness of case management for homeless persons: a systematic review. Am J Public Health. 2013;103(10):e13–26. doi: 10.2105/AJPH.2013.301491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zulman DM, Shah NH, Verghese A. Evolutionary Pressures on the Electronic Health Record Caring for Complexity Journal of the American Medical Association. 2016 doi: 10.1001/jama.2016.9538. [DOI] [PubMed] [Google Scholar]
- 32.Winden TJ, Chen ES, Wang Y, Lindemann E, Melton GB. Residence, Living Situation, and Living Conditions Information Documentation in Practice. American Medical Informatics Association Annual Symposium 2017 Proceedings Submitted. 2016 [PMC free article] [PubMed] [Google Scholar]
- 33.Winden TJ, Chen ES, Melton GB. Representing Residence, Living Situation, and Living Conditions: An Evaluation of Terminologies, Standards, Guidelines, and Measures/Surveys. Proceedings American Medical Informatics Symposium. 2016 [PMC free article] [PubMed] [Google Scholar]
- 34.Johnson SG, Byrne MD, Christie B, Delaney CW, LaFlamme A, Park JI, et al., editors. Modeling Flowsheet Data for Clinical Research. AMIA Summits on Translational Science. 2015 [PMC free article] [PubMed] [Google Scholar]
- 35.Westra BL, Christie B, Johnson SG, Pruinelli L, LaFlamme A, Park JI, et al., editors. Expanding Interprofessional EHR Data in i2b2. Proceedings AMIA Summits on Translational Science. 2016 [PMC free article] [PubMed] [Google Scholar]
- 36.Martin KS. Omaha, NE: Health Connections Press; 2005. The Omaha System: A key to practice, documentaiton, and information management (Reprinted 2nd ed.) Martin KS. (2005). The Omaha System: A key to practice d, and information management (Reprinted 2nd ed.). Omaha, NE: Health Connections Press. [Google Scholar]