To the Editor
Primary cutaneous follicle center lymphoma and primary cutaneous marginal zone lymphoma are the most common types of indolent primary cutaneous B-cell lymphoma ( pcBCL). Although pcBCLs are skin-limited and rarely demonstrate extracutaneous spread,1 they can be distressing to patients and disfiguring. Common local therapies include intralesional steroid injection, topical steroids,2 and excision.3 Steroid injections induce a durable complete remission in only 44% of patients and may require multiple rounds of injections; topical steroids are typically ineffective.2 Excision can be definitive, but these lymphomas have a strong propensity for local recurrence, making field therapy preferable. Locoregional radiation therapy (RT) is an alluring option with significantly higher complete remission rates.4,5
Current barriers to referral for RT include the number of treatments needed (12–20) and side effects of standard dose RT (SD-RT). The National Comprehensive Cancer Network recommends 24 to 40 Gy for the treatment of pcBCL (www.nccn.org/about/nhl.pdf). Although effective, SD-RT is associated with dose-dependent cutaneous side effects, including erythema, desquamation, ulceration, and alopecia. While the latter grade 3 toxicities are quite rare even at the highest recommended radiation doses, very low-dose RT (VLD-RT; 2 Gy × 2 treatments) is an attractive alternative currently used in the treatment of indolent nodal non-Hodgkin’s lymphoma that can also be applied to cutaneous disease.
In this retrospective study, we compared the efficacy of VLD-RT to SD-RT for treatment of pcBCLs. A total of 54 patients with 98 lesions of pcBCL were identified (31 with primary cutaneous marginal zone lymphoma, 27 with primary cutaneous follicle center lymphoma, and 1 patient with low grade B-cell lymphoma not otherwise specified) (Table I). Lesions were treated with either VLD-RT (4–8 Gy in 2 treatments) or SD-RT (24–40 Gy in 12–20 treatments). Some patients had SD-RT to an initial lesion but then received VLD-RT to sites of distant relapse; the subsequent lesions were excluded, leaving 88 lesions for analysis. To account for correlation within-person, repeated measures models were used. The median lesion follow-up was 4.8 years.
Table I.
Characteristics of lesions treated with very low-dose radiation therapy and standard dose radiation therapy and side effects of treatment
| Lesion information | VLD-RT (n = 51) | SD-RT (n = 37) | P value* | ||
|---|---|---|---|---|---|
| Lesion diagnosis, n (%) | .1912 | ||||
| pcMZL | 34 (66.7) | 17 (48.6) | |||
| pcFCL | 17 (33.3) | 18 (51.4) | |||
| NOS | 0 | 2 (0.05) | |||
| Location, n (%) | .5184 | ||||
| Head | 15 (29.4) | 17 (46.0) | |||
| Trunk | 21 (41.2) | 8 (21.6) | |||
| Extremities | 15 (29.4) | 12 (32.4) | |||
| Lesion size (cm) | .0145 | ||||
| N | 33 | 27 | |||
| Range | 0.2–6.0 | 0.2–14.0 | |||
| Median | 1.0 | 3.0 | |||
| Duration of follow-up ( years) | .0271 | ||||
| Range | 0.02–12.6 | 0.2–18.8 | |||
| Median | 3.9 | 7.0 | |||
| Immediate side effects, n (%) | <.0001 | ||||
| No | 43 (84.3) | 8 (21.6) | |||
| Yes | |||||
| Erythema | 8 (15.7) | 5 | 29 (78.4) | 22 | |
| Itch | 1 | 2 | |||
| Fatigue | 1 | 2 | |||
| PIH | 1 | 0 | |||
| Erythema and fatigue | 0 | 1 | |||
| Itch and fatigue | 0 | 1 | |||
| Pain and fatigue | 0 | 1 | |||
| Long-term side effects (>6 months), n (%) | .0036 | ||||
| None | 47 (92.2) | 22 (59.5) | |||
| Yes | |||||
| PIH | 4 (7.8) | 2 | 15 (40.5) | 9 | |
| Hair loss | 2 | 4 | |||
| Pain | 0 | 1 | |||
| PIH and hair loss | 0 | 1 | |||
| CR, n (%) | .4937 | ||||
| No | |||||
| No response | 3 (5.9) | 0 | 1 (2.7) | 1 | |
| PR | 2 | 0 | |||
| PR with recurrence | 1 | 0 | |||
| Yes | |||||
| CR | 48 (94.1) | 39 | 36 (97.3) | 25 | |
| CR with in-field occurrence of new lesions | 5 | 2 | |||
| CR with out-of-field occurrence of new lesions | 0 | 8 | |||
| CR with relapse of same lesions | 4 | 1 | |||
CR, Complete response; NOS, not otherwise specified; pcFCL, primary cutaneous follicle center lymphoma; pcMZL, primary cutaneous marginal zone lymphoma; PIH, postinflammatory hyperpigmentation; PR, partial response; SD-RT, standard dose radiation therapy; VLD-RT, very low-dose radiation therapy.
Obtained from generalized repeated measures linear models with the appropriate link function based on the distribution of the lesion characteristic. Continuous measures were transformed when their distributions were skewed.
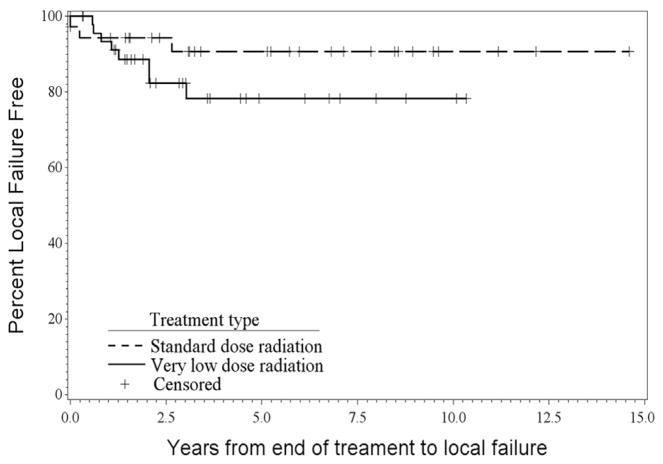
Of lesions treated with VLD-RT, 94.1% achieved an initial complete response (CR); 97.3% of lesions treated with SD-RT achieved an initial CR (P = .49). Of those achieving a CR, there was no significant difference for time to local failure (P = .07), with 1-year Kaplan–Meier failure rates of 6.7% for VLD-RT and 5.6% for SD-RT (Fig 1). Location of lesion (leg vs. nonleg) did not impact the response rate.
Fig. 1.
Kaplan–Meier curve showing the freedom from local failure for very low-dose radiation therapy and standard dose radiation therapy. Although they initially have similar response rates, lesions treated with very low-dose radiation therapy are more likely to have recurrences or in-field relapses than those treated with standard dose radiation therapy. This difference is not statistically significant, with a log-rank P value for the comparison of 0.07.
SD-RT was associated with a significant increase in acute toxicities (P < .0001), most commonly erythema, but none greater than grade 2. Patients receiving SD-RT were more likely (P = .004) to experience long-term side effects (lasting >6 months), such as postinflammatory hyper/hypopigmentation or alopecia.
In this study, we found no difference in CR rates between VLD-RT and SD-RT. In addition, the shorter course of therapy is associated with fewer toxicities, including skin dyspigmentation. We recommend that VLD-RT be considered a preferred initial strategy for treatment of pcBCL because of the minimal time commitment (2 treatments), excellent toxicity profile, and improved efficacy over other treatment modalities, such as repeated intralesional steroid injections. The limitations of this study include its retrospective nature and limited sample size.
Acknowledgments
Statistical analysis (by Mr Isom) supported by the Wake Forest Baptist Comprehensive Cancer Center’s National Cancer Institute Cancer Center Support Grant P30CA012197.
Footnotes
Presented at the 57th Annual Meeting of the American Society of Radiation Oncology, San Antonio, Texas, October 18–21, 2015.
Conflicts of interest: None declared.
References
- 1.Hoefnagel J, Vermeer MH, Jansen PM, et al. Primary cutaneous marginal zone B-cell lymphoma: clinical and theraputic features in 50 cases. Arch Dermatol. 2005;141:1139–1145. doi: 10.1001/archderm.141.9.1139. [DOI] [PubMed] [Google Scholar]
- 2.Perry A, Vincent BJ, Parker SRS. Intralesional corticosteroid therapy for primary cutaneous B-cell lymphoma. Br J Dermatol. 2010;163:223–225. doi: 10.1111/j.1365-2133.2010.09798.x. [DOI] [PubMed] [Google Scholar]
- 3.Parbhakar S, Cin AD. Primary cutaneous B-cell lymphoma: role of surgery. Can J Plast Surg. 2011;19:e12–e14. [PMC free article] [PubMed] [Google Scholar]
- 4.Neelis KJ, Schimmel EC, Vermeer MH, Senff NJ, Willemze R, Noordijk EM. Low-dose palliative radiotherapy for cutaneous B- and T-cell lymphomas. Int J Radiat Oncol Biol Phys. 2009;74:154–158. doi: 10.1016/j.ijrobp.2008.06.1918. [DOI] [PubMed] [Google Scholar]
- 5.Akhtari M, Reddy JP, Pinnix CC, et al. Primary cutaneous B-cell lymphoma (non-leg type) has excellent outcomes even after very low dose radiation as single-modality therapy. Leuk Lymphoma. 2016;57:34–38. doi: 10.3109/10428194.2015.1040012. [DOI] [PMC free article] [PubMed] [Google Scholar]