Abstract
The causes of obesity worldwide are complex and multilevel, including changing food environments, physical activity levels, policies, and food production systems. This intricate context requires multilevel and multicomponent (MLMC) interventions to improve health outcomes. We conducted a literature review of MLMC interventions for obesity prevention and mitigation; 14 studies meeting search criteria were identified. We found examples of successes in preventing obesity, reducing overweight, improving healthful behaviors, and enhancing some psychosocial indicators. Of eight studies that reported health and behavioral results, five showed no significant impact and three showed reductions in obesity. Four studies showed significant improvement in dietary behavior, and five reported significant desirable effects in physical activity or screen time. Five studies reported psychosocial impacts, and three of these showed significant improvements. MLMC approaches show promising results, particularly when they are able to integrate components at the policy, community, and interpersonal levels.
Keywords: Obesity, Prevention, Multilevel, Multicomponent, Community-based interventions, Review, Health promotion, Research design, Health behavior, Lifestyle, Minority populations, Child, Adult
Introduction
The causes of the global rise in obesity are complex and multilevel, including changing food and physical activity environments, policies, and food production systems [1, 2]. In particular, widespread availability of low-cost, calorie-dense, nutrient-poor foods has led to increased energy intake without an equivalent rise in energy expenditure, resulting in population-level increases in overweight and obesity [1]. This complex context requires multilevel and multicomponent (MLMC) interventions that take a systems approach to effectively improve health outcomes [3, 4].
Multilevel approaches focus on changing health behaviors by acting on multiple contexts, communities, and environments that influence the individual. A common framework to describe this approach is the Social Ecological Model (SEM), which incorporates individual, interpersonal, organizational, community, and policy levels [5]. A single-level intervention impacts only one of these levels of influence, for example classes to provide nutrition education to children, operating only at the individual level. Multilevel interventions reach two or more levels, for example, by educating children at school and changing the school food service, operating at both the individual and organizational levels.
Multicomponent interventions incorporate more than one strategy or mechanism to achieve an improved health outcome within the same level. For example, at the organizational level, a corner store both enacts a marketing campaign with posters to promote healthy beverages and increases the supply and variety of options on the shelves. Thus, the store would be using two strategies at the same level.
The obesity prevention literature has frequently included interventions that reach only a single institution or only operate at the individual level. Commonly, within any particular level, multicomponent approaches are not employed. To date, there have been no literature reviews that broadly examine MLMC approaches for preventing obesity across all age groups. This review seeks to fill the gap by addressing the following key research questions:
What MLMC interventions have been/are being tested for obesity prevention, and what study designs, intervention components/levels, and evaluation approaches are used?
How effective have tested MLMC interventions been in improving health, behavioral, and psychosocial outcomes?
Methods
Overview
A literature review was performed to assess current studies using an MLMC approach for obesity prevention. Articles selected for inclusion met three inclusion criteria. First, a direct measure of obesity was required. Second, the study intervention components took place at more than one level (individual, interpersonal, organizational, community, or policy), engaging various stakeholders. Third, the study clearly articulated a strategy with multiple mechanisms for impact on behavior and weight status.
Literature Search Steps
As an emerging approach to obesity interventions, MLMC trials pose a unique challenge to review. Few studies characterize themselves as MLMC in the search terms or in the text, thus the electronic search terms were designed to encompass a broad body of literature producing a large number of articles that required both electronic and manual filtering. The search was limited to the last 10 years to include all indexed journal articles based on studies using human subjects published in English between January 2006 and January 2016 (see Appendix). Notably, this excludes some foundational studies in community-based interventions that were published more than 10 years ago, or that did not specifically look at obesity, but instead focused exclusively on non-communicable diseases (NCDs) [6–8]. Figure 1 outlines the steps in the literature search.
Fig. 1.
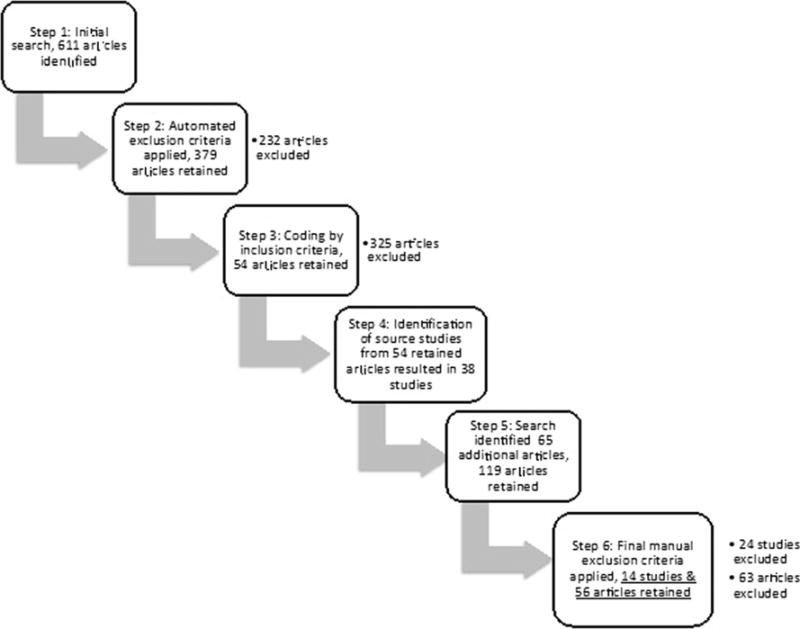
Literature search procedures to identify multilevel, multicomponent obesity prevention and control studies
Step 1: Initial Search
Three search concepts for (1) MLMC approach, (2) obesity, as well as (3) environmental influences and health behavior were constructed using a combination of Medical Subject Headings (MeSH), title and abstract text, and the full article text. The intersection of these three concepts resulted in 611 articles.
Step 2: Application of Primary Exclusion Criteria
Six exclusion concepts were constructed and applied to exclude studies with primary foci outside the scope, including smoking, meal replacement diets, specific single food or beverage consumption, surgical care or drugs, other disease conditions, and testing or validating novel statistical methodologies. Filtering based on these concepts excluded 232 articles and retained 379.
Step 3: Focused Application of Inclusion Criteria
Next, the 379 abstracts were re-reviewed manually and received binary codes in Excel for three inclusion criteria: obesity, multilevel, and multicomponent. Those that did not meet all three requirements were discarded. Requirements were defined in the following ways. Obesity had to be measured, for example, with body mass index (BMI), waist circumference, or other measure; of the 379 articles, 107 did not meet this criterion. The multilevel criterion necessitated that the intervention substantively engage subjects at more than one level. For example, studies conducted in school environments that simply sent information to parents reached only the organizational level and were discarded; of the 379 articles, 299 did not meet this criterion. Finally, multicomponent required more than one mechanism to impact the outcomes of focus. For example, a design that included both a curriculum intervention and organizational changes to improve cafeteria offerings in a school setting met the multicomponent requirement, whereas an intervention that consisted only of an educational strategy was not considered multicomponent; 217 did not meet this criterion. When the 324 articles that lacked any one of these three requirements were excluded (some studies lacked more than one criterion), 54 articles remained.
Step 4: Identification of Individual Studies
The remaining 54 articles were read and the specific study that had produced the publication was identified, resulting in 38 originating studies.
Step 5: Identification of Additional Articles Associated with Originating Studies
Further searches were conducted on each individual study by author and by study name to identify related publications that best explained the scope, method, intervention strategies, design, and relevant results of each. This was especially relevant for research that was scaled up over time or large multisite studies, and included 65 additional papers.
Step 6: Full-Text Review
Finally, the lead author (EE-P) read the full text and bibliography of the 119 papers remaining. The “backwards” search and full-text read did not identify additional articles. Articles in early pilot stages were excluded, resulting in 56 articles published from 14 studies. The final included studies are Ballabeina Study (Ballabeina), Baltimore Healthy Eating Zones (BHEZ), Childhood Obesity Prevention and Treatment Research (COPTR), Childhood Obesity Research Demonstration (CORD), Children’s Healthy Living (CHL), Girls Health Enrichment Multi-site Studies Phase II (GEMS), Healthy Caregivers-Healthy Children (HC2), Healthy Families Study (HFS), Intervention Centered on Adolescents Physical Activity and Sedentary Behavior (ICAPS), National Institute of Public Health (INSP), Shape Up Somerville (SUS), Switch What You Do, View, and Chew (Switch), Texas Expanded Food and Nutrition Education Program (TEFNEP), and TriAtiva Program: Education, Nutrition and Physical Activity (TriAtiva).
Coding Included Research Studies
The final set of studies were coded by EE-P and independently coded by a coauthor (MJMR) to identify study location, community and cultural context, demographics of the audience, design and methodology, intervention levels, process evaluation, and outcomes. Data in each of these categories were collected from one or more publications produced by each study and coded by study. Inconsistencies in coding were adjudicated by the third coauthor (JG).
Results
Fourteen studies met the search criteria. Studies took place in the continental U.S. (9 of 14), Europe (2), Latin America (2), and the Pacific Islands (1). Evaluation sample sizes ranged from more than 4300 (CORD) to 211 households (HFS). All studies in the final pool targeted childhood obesity. Adults were also targeted in five of the studies. Table 1 describes general characteristics of included studies; Table 2 reports the intervention, levels, and process evaluation; and Table 3 shows the outcomes.
Table 1.
General characteristics of selected multilevel multicomponent trials published January 2006–January 2016
| Study name | Citations | Location | Design | Years | Trial participants (N) | Participant group characteristics |
|---|---|---|---|---|---|---|
| Ballabeina Study (Ballabeina) | [19–24] | St. Gallen and Vaud, Switzerland | Cluster randomized controlled trial (RCT) | 2008–2009 (1 academic year) | 655 | Preschool students, largely immigrants |
| Baltimore Healthy Eating Zones (BHEZ) | [25, 26] | Baltimore, MD, USA | Cluster RCT | 2009–2010 (8 months) | 242 pairs | Pairs of African-American youth ages 10–14 years and a primary caregiver |
| Childhood Obesity Prevention and Treatment Research (COPTR) | [27••, 28–31] | Cleveland, OH, Davidson County, TN, East Palo Alto, Menlo Park and Redwood City, CA and MN, USA | Individually randomized group treatment and RCT | ~2012–2018 (7 years) | 1700 | Low-income, minority 3–13-year-olds and their parents |
| Childhood Obesity Research Demonstration (CORD) | [32–41] | Brawley, El Centro and Calexico, CA, Fitchburg, New Bedford and Lowell MA, and Austin and Houston, TX, USA | Factorial | 2011–2014 (2 years) | 4314 in 3 sites | Low-income, minority 2–12-year-olds |
| Children’s Healthy Living(CHL) | [4, 42–48] | AK and HI, USA, American Samoa, Northern Mariana Islands and Guam | Cluster RCT | 2011–2016 (5 years) | 4100 | Children ages 2–8 in communities with large native Pacific Islander populations |
| Girls health Enrichment Multi-site Studies Phase II (GEMS) | [49–53] | Oakland, CA and Memphis, TN, USA | RCT | (2 years) | 303 | Low-income, minority girls ages 8–10 years, who are overweight or who have one overweight or obese caregiver, and the caregiver |
| Healthy Caregivers-Healthy Children (HC2) | [54, 55] | Miami-Dade County, FL, USA | Cluster RCT | 2010–2013 (3 years) | 1211 children, 1080 parents, and 122 teachers | Low-income, minority children in daycare, their parent, and teachers |
| Healthy Families Study (HFS) | [56] | Boston, MA, USA | Cluster randomized | (3 years) | 211 households | Mother-daughter pairs in public housing residents |
| Intervention Centered on Adolescents Physical activity and Sedentary behavior (ICAPS) | [57–60] | Bas-Rhin, France | RCT | 2002–2006 (4 academic years) | 954 | Students, grade 6 in public middle schools |
| National Institute of Public Health (INSP) | [14, 17] | Mexico City, Mexico | RCT | 2003–2005 (2 years) | 886 students and 27 schools | Students 9–11 years old |
| Shape Up Somerville (SUS) | [13••, 61, 62, 63•, 64, 65] | Somerville, MA, USA | Community-based participatory research and non-randomized controlled trial | 2003–2005 (3 years) | 1178 | Students grades 1–3 in public elementary schools in low-income, ethnically and racially diverse, high proportion of non-English-speaking communities |
| Switch what you Do, View, and Chew (Switch) | [66, 67] | Lakeville, MN and Cedar Rapids, IA, USA | RCT | 2005–2006 (1 academic year) | 1323 students and 10 schools | Students graded 3–5 and their families |
| Texas Expanded Food and Nutrition Education Program (TEFNEP) | [68, 69] | Austin, Houston and San Antonio, TX, USA | RCT | 2006–2007 (13 months) | 1006 | Clients of a publicly funded nutrition assistance program |
| TriAtiva Program: Education, Nutrition and Physical Activity (TriAtiva) | [70] | Porto Alegre, Brazil | Cluster RCT | 2013 (6 months) | 600 | Brazilian public primary school students |
Table 2.
Intervention overview of selected multilevel multicomponent obesity prevention trials and process evaluation
| Study | Intervention | Intervention levels
|
Process evaluation | ||||
|---|---|---|---|---|---|---|---|
| Individual | Interpersonal | Organizational | Community | Policy | |||
| Ballabeina | Increase PA, improve diet and reduce ST | Students | Parents, teachers and local health promoters | Schools | New national PA program | 88 % achievement of teacher outcomes, 85 % of environmental outcomes, and more than 75 % of all child outcomes | |
| BHEZ | Promotion of food alternatives and messages on food-related behaviors | Youth and caregiver pairs | Peer educators, primary caregiver and graduate students | we | Wholesalers, restaurants, carryouts, corner stores, rec. centers and community-based orgs | Measures of reach, dose, and fidelity by level and phase showed that 4 intervention components were not achieved and 2 were achieved | |
| COPTR | Visitation program and parenting classes aimed at parents; social media and phone coaching; primary-care counseling, screen-time reduction; goal-setting, skill building, changing family environment. Interventions tailored to site | Children and parents | Teachers | Primary care facilities | Rec. centers and other community resources | Evaluation plans are site specific and vary in design. Results not yet published | |
| CORD | Tailored interventions at each study site focused on improvements in FV and water consumption, PA, and quality sleep | Children | Community health workers, teachers, and parents | Schools, child care centers and healthcare facilities | Restaurants and rec. centers | Families are eligible for benefits under Title XXI (CHIP) or Title XIX (Medicaid) | Context, reach, dose delivered, dose received, and intervention fidelity. Results not yet published |
| CHL | Community prioritized, tailored intervention strategies: policy supports, growing and eating local healthy foods, role models, accessibility of PA environments, water access, and health workforce training | Children | University students | Health workforce training programs | Community orgs and community leader advisory committee | Support policy for healthy eating and PA. Increase accessibility of environments for safe play and PA | Fidelity measures scored “somewhat well” in 3 of the 4 crosscutting functions |
| GEMS | Culturally tailored after-school dance classes with daily transportation provided to centers. Home-based screen-time reduction lessons, monitoring, and mentorship | Youth and caregivers | Family screen-time intervention mentor | Rec. centers | Attendance at dance classes and family receipt of screen-time intervention was lower than planned. Strong receipt and reading of newsletters | ||
| HC2 | Childcare centers healthy menu changes and family-based education focused on increased PA and FV intake, decreased intake of simple carbohydrate snacks, and decreased ST | Parents and children | Teachers | New center policy for dietary requirements for diet, PA, and ST | Attendance, activity engagement, newsletter use, and satisfaction completed. Results not yet published | ||
| HFS | Residence-based health screenings, walking groups, nutrition and cooking demos, and healthy purchasing options | Mother-daughter pairs | Residents trained in community outreach support program and families | Public housing residences | Public housing program | Surveys group activities, participant evaluations, and paraprofessional leaders on activities, communication, and satisfaction. Results not yet published | |
| ICAPS | Change knowledge, attitudes, beliefs, and motivation toward PA and improved environmental conditions supporting PA | Youth | Teachers, medical staff and families | PA clubs | Rec. centers | ~50 % of the students participated in at least one weekly activity. All intervention students exposed to at least two educational sessions. Mobilization and implication of the teachers, the families, and partners in and outside schools increased throughout | |
| INSP | Education curriculum and environmental changes to diet and PA | Students | Parents, families, and PE teachers | Principals and school authorities | Policy makers and researchers collaborate | Year one: intervention 75 % of nutrition, 70 % of PA, 90 % communication/ed. implemented. Year two: 80, 70, and 95 %, respectively | |
| SUS | Diet and PA campaigns, improved foods available in schools and restaurants, education, and community activities | Students and parents | Families, teachers | Schools | Restaurant owners and community organizations | New school wellness policy and state-level policy base | 100 % of 1 to 3 grade classrooms implemented school curriculum 21 restaurants recruited to become SUS approved and 10 of 21 restaurants fully complied with all approval criteria |
| Switch | Students increase the amount of habitual PA, reduce the amount of total ST, and increase FV intake | Children and families | Parents, teachers | Schools | Child, parent, and teacher surveys. Results not yet published | ||
| TEFNEP | Increase habitual PA, reduce ST, and increase FV consumption | Parents | Trained paraprofessional teachers | TEFNEP state program used as foundation | Fidelity to the intervention class session structure was high | ||
| TriAtiva | Students receive nutrition education and increased PA with families and school. Policy regulation of foods available | Students | Families, teachers and nutritionists | Schools | Law regulates snack food sold and school lunches | Not evaluated | |
Table 3.
Reported results of multilevel multicomponent obesity prevention trials
| Study | Health | Behavior | Psychosocial |
|---|---|---|---|
| Ballabeina | More beneficial effects on overweight (OW) vs. normal weight children on waist circumference interaction p = 0.001, and for low fit children vs. normal fit on all adiposity outcomes (BMI, sum of four skinfolds, and waist circumference) interaction p = 0.027. Intervention children showed reductions in % body fat p = 0.02, sum of four skinfolds p = 0.001, and lower increases in waist circumference p = 0.001 than control children. No effect of prevalence of overweight p = 0.23 or BMI p = 0.31. No difference in effects on migrants vs. non-migrants. Interaction BMI p = 0.849, % body fat p = 0.966, waist p = 0.824. No difference in effects by educational level (EL), BMI interaction p = 0.306, body fat p = 0.181, waist p = 0.454 | No differential effect on OW vs. normal weight children, interaction p = 0.60, p = 0.18, respectively. On low fit vs. normal fit interaction p = 0.318, p = 0.467, respectively. Significantly higher increase in aerobic fitness p = 0.01, motor agility p = 0.004, reduced ST p = 0.03, higher prevalence of active children p = 0.01 and improved healthy eating p = 0.04 in the intervention group than in the control group. No effect on measured PA p = 0.54 or sleep duration p = 0.97. No difference in effects on migrants vs. non-migrants. Interaction shuttle run p = 0.085 and obstacle course p = 0.685. No difference in effects by EL, interaction shuttle run p = 0.058, obstacle course p = 0.258 | No effect on the quality of life p = 0.17 or cognitive abilities: attention duration p = 0.98, attention accuracy p = 0.87, spatial working memory p = 0.58 |
| BHEZ | BMI for age percentiles significantly decreased on average in the intervention group but not in the comparison group in all analyses, entire sample: p = 0.04, overweight and obese girls and boys: p < 0.001, and overweight and obese girls only p = 0.001 | Intervention arm significantly decreased purchasing healthful beverage p = 0.003 and snacks p = 0.01, as well as purchasing unhealthful snacks p = 0.02 and eating fast food p = 0.02. No significant impact on purchasing healthful food p = 0.13, purchasing unhealthful food p = 0.31 or beverage p = 0.52, or healthful food preparation p = 0.13 | Significant impact in intervention group: decreased behavioral intentions p = 0.01, increased outcome expectancies p = 0.02, and increased knowledge p < 0.001. No significant impact on self-efficacy p = 0.54 |
| GEMS | No significant difference in adjusted BMI difference per year 0.04 kg/m2, 95 % CI (−0.18 to 0.27). Significant decrease in total cholesterol −3.49 mean adjusted fasting, 95 % CI (−5.28 to −1.70), LDL cholesterol −3.02 mg/dL, 95 % CI (−4.74 to −1.31) and hyperinsulinemia relative risk RR = 0.35, 95 % CI (0.13 to 0.93). Greater effectiveness (lower mean BMI change per year) in high-risk groups | No difference in most measured behavioral outcomes: accelerometer counts, vigorous PA, or ST. At the Memphis site, eating habits worsened less for the intervention than control group: SSB 0.19 fewer servings/day (p = 0.075), 0.21 more servings/day water (p = 0.022), 0.15 more servings/day vegetables (p = 0.069). No significant difference in eating habits observed at Oakland site | Significant difference in depressive symptoms in intervention compared to control −0.21 (0–20 Child Depression Inventory scale), 95 % CI (−0.42 to −0.001). No difference in self-esteem, school performance, activity preferences, or other outcomes |
| HC2 | No statistically significant association found between parent/home intervention activities and BMI p = 0.81 | No statistically significant differences in PA levels between the control and intervention groups and from baseline to 6-month follow-up in both groups. Analysis of lesson plans and class schedules revealed that over time, children in the control centers spent significantly more time on the computer p < 0.01 and watching TV p < 0.0001 than children attending intervention centers | None reported |
| ICAPS | Intervention students had a lower increase in BMI p = 0.01 and age- and gender-adjusted BMI p < 0.02 over time than controls; increase of high-density cholesterol concentrations p < 0.0001 | Independent of initial weight status, compared with controls, intervention adolescents had an increase in supervised PA p < 0.0001, and a decrease of TV/video viewing p < 0.01 | Self-efficacy and social support toward PA not significant at follow-up. Intention to PA significantly improved p < 0.001 |
| SUS | Parent BMI decreases 0.411 kg/m2 95 % CI (−0.725 to −0.097). Significant change in child z-BMI at 2 years p = 0.0054. Prevalence of child overweight/obesity decreased in males OR = 0.61, p = 0.01 and females OR = 0.78, p = 0.013. Average change in BMI z-score = 0.1005 95 % CI (0.1151 to 0.0859), p = 0.001 after controlling for covariates | Reduced SSB consumption −2.0 oz per day; 95 % CI (−3.8 to −0.2). Increased PA 0.20 sports or activities per year 95 % CI (0.06 to 0.33). Reduced ST −0.24 h per day 95 % CI (−0.42 to −0.06). Participation in school breakfast and lunch up 3 %. Fresh produce expenditure up $27,000 from previous year; 21 restaurants joined | None reported |
| Switch | No significant impact on BMI | At post, parent report of ST p < 0.05, Cohen’s d = 0.69 and FV consumption significant p < 0.05, Cohen’s d = 1.36. Child report of FV consumption near significant p < 0.06, Cohen’s d = 0.52. Changes in PA or child report of ST not significant | None reported |
| TEFNEP | Significant BMI decrease at post compared to baseline for the intervention group only; change was not maintained at follow-up p < 0.05 | Greater goal attainment significantly associated with improvement in various dietary practices p < 0.05. Parents who reported attaining more goals reported greater self-efficacy p < 0.05. Goals for regular vegetables and water use correlated with regular vegetable p < 0.05 and water p < 0.01 consumption at post. Water significant at follow-up p < 0.05. Various significant dietary changes at post in control group | Significant time effect regardless of group for all measured variables |
Approaches
Theoretical Foundations
Thirteen studies identified a theoretical framework foundation; Social Cognitive Theory (SCT) and SEM were the most common theoretical frameworks used. Only three of the studies (BHEZ, CHL, and SUS) discussed using community-based or community-based participatory research approaches. Behavior change theories were also referenced by four studies (CORD, CHL, HC2, and INSP).
Study Design
Most studies (12 of 14) were randomized controlled trials (RCTs), one used a quasi-experimental design (SUS), and one used a factorial design (CORD). Half of the studies (COPTR, CORD, CHL, HC2, SUS, Switch, and TEFNEP) evaluate samples of more than 1000 participants. Four include 501 to 1000 participants (Ballabeina, ICAPS, INSP, and TriAtiva) and three include 500 participants or fewer (BHEZ, GEMS, and HFS). The durations varied—four lasted less than one calendar year, four covered a period of 1 to 2 years, and six lasted or are planned to last for more than two calendar years.
Population Characteristics
Unique socio-cultural contexts and the policy environment were described for all studies and varied widely across studies. Nonetheless, poor accessibility of affordable healthy foods, declining levels of physical activity (PA), and lifestyles not conducive to healthful options due to urbanization were commonly reported.
A focus on children was not an inclusion criterion, yet all of the included studies center on children, adolescents, or youth and four also focused on adults (HC2, HFS, Switch, and TEFNEP). Many targeted vulnerable sub-populations, like racial and ethnic minorities (11), low-income families (8), or girls and women (3).
Venues of Intervention
All studies included multiple venues or locations for implementation. Six included a school-based component. Other venues included food stores, restaurants, or small food vendor businesses (5), community recreation centers (rec. centers) (4), primary care settings (3), and public assistance programs (3).
Levels and Components
All studies incorporated components acting at the individual and interpersonal levels. Most frequently, these were individual children and their caregivers working at an interpersonal level with teachers or trained paraprofessionals, such as community health workers. Organizational entities like schools or clinics were involved in 12 studies. Seven studies included community-level institutions like stores, wholesalers, or rec. centers (BHEZ, COPTR, CORD, CHL, GEMS, ICAPS, and SUS). Nine studies involved, or were influenced by, a policy component such as leveraging a local law or execution within a public assistance program (Ballabeina, CORD, CHL, HC2, HFS, INSP, SUS, TEFNEP, and TriAtiva).
Observed Impacts
Process evaluations were conducted in most studies to report reach, dose, and fidelity (Table 2), and study results have been grouped into three outcome categories: psychosocial, behavioral, and health (Table 3).
Process Evaluation
Most studies include a process evaluation (13 of 14), and eight of these published results in the period of this review. The number of participants who received any amount of the intervention was the reach, dose was the amount and frequency of delivery to the target population, and fidelity was how closely the implementation reflected the design. Studies did not report specific reach, dose, or fidelity scores, but selected various indicators. Ballabeina reported better than 75 % achievement at all levels. GEMS experienced low adherence to the two individual-level components while the family level had strong adherence. ICAPS reported that students achieved some components while parent, teacher, and community achievement was low. BHEZ reported achievement of two of six intervention components. CHL developed “crosscutting functions” (similar to components) and performed “somewhat well” in three of the four. INSP reported above 70 % achievement for all components. SUS reported high adherence in school components and lower adherence in restaurant components. Finally, TEFNEP reported high fidelity and did not report dose or reach.
For the purpose of generalizing process evaluation results, a measure of community adherence was developed. Good community adherence was defined as achieving more than half of the study components at most (more than half) of the observations, while poor community adherence meant reporting that same level of success at fewer than half of the observations. Six studies reported good community adherence (Ballabeina, CHL, ICAPS, INSP, SUS, and TEFNEP) and two studies reported poor adherence (BHEZ and GEMS). The remaining five studies have not yet published their process evaluation results (COPTR, CORD, HC2, HFS, and Switch). Neither of the two studies that reported poor adherence included a policy component and both reported challenges with community support for at least one intervention component.
Health Outcomes
Eight of the fourteen studies reported impact on health outcomes. The other six studies are ongoing. An obesity measure like BMI or waist circumference was an inclusion criterion for this study, so all studies utilized at least one. Ballabeina (p = 0.001 for BMI, sum of four skinfolds, and waist circumference), BHEZ (p = 0.04 for BMI for age percentile and p < 0.001 among only overweight and obese children), SUS (p = 0.0054 for child BMI z-score and parent BMI decrease 0.411 kg/m2, 95 % CI (−0.725 to −0.097)), and TEFNEP (BMI decrease at post p < 0.05 but not maintained at followup) showed improvements among the intervention group or an intervention sub-group. Two studies reported success in preventing an increase in BMI within the intervention group as opposed to the control group (GEMS and ICAPS), but no overall reduction in BMI among overweight or obese participants in the intervention group. HC2 and Switch showed no impact on BMI or other obesity measure among the intervention group.
Additionally, blood tests (lipids, insulin, etc.) were included in the GEMS, ICAPS, and COPTR studies. One of the two GEMS sites showed improvements in total cholesterol (−3.49 adjusted mean difference in fasting total cholesterol, 95 % CI (−5.28 to −1.70)), low-density cholesterol (LDL) (−3.02 mg/dL per year, 95 % CI (−4.74 to −1.31)), and incidence of hyperinsulinemia (RR=0.35, 95 % CI (0.13 to 0.93)), and ICAPS showed improved high-density cholesterol concentrations (HDL) (p < 0.0001), while COPTR is still ongoing.
Several studies showed differences among sub-groups. SUS (p = 0.0054) showed a sustained reduction in BMI among child participants who were overweight or obese at baseline. SUS further showed BMI decrease among parents of children in the intervention group relative to the control group parents (−0.411 kg/m2, 95 % CI (−0.725 to −0.097)). Ballabeina showed greater beneficial impacts on low-fit (p = 0.027) and overweight children (p = 0.001) than on fit and normal weight children. BHEZ showed greater impact on overweight and obese girls and boys (p < 0.001).
Behavioral Outcomes
All studies included behavioral change measures, centering on diet, PA, or both, and eight published results by January 2016 (Ballabeina, BHEZ, GEMS, HC2, ICAPS, SUS, Switch, and TEFNEP). Six reported desirable behavioral results as a consequence of the intervention (Ballabeina, BHEZ, HC2, ICAPS, SUS, and Switch).
Ballabeina, BHEZ, SUS, and Switch showed that the intervention seemed to impact at least one dietary outcome positively, while TEFNEP showed significant desirable dietary changes in both the intervention and the control groups and GEMS showed mixed outcomes. Ballabeina, HC2, ICAPS, SUS, and Switch showed improvements in PA indicators (including screen time/media use (ST)).
Ballabeina showed improvements in diet (p = 0.04) and BHEZ showed reduced purchasing of less-healthful snacks (p = 0.02) and fast food (p = 0.02). However, BHEZ also showed a reduction in purchasing healthful snacks (p = 0.01) and overall negative behavioral impacts in both the intervention and control groups. GEMS showed no significant dietary impacts at one site, and the other site showed worsened behaviors for both control and intervention groups, but the intervention group was less negatively impacted. The intervention arm showed 0.19 fewer servings per day of SSBs (p = 0.075), 0.21 more servings per day of water (p = 0.022), and 0.15 more servings per day of vegetables (p = 0.069) consumed when compared to the control. SUS showed reduced sugar-sweetened beverage (SSB) intake (−2.0 oz per day (95 % CI −3.8 to −0.2)) and improved foods available (21 restaurants joined the program). Switch showed improved fruit and vegetable (FV) consumption (p < 0.05). TEFNEP showed an association between better goal attainment and improved dietary outcomes in the intervention and control groups.
For PA outcomes, Ballabeina showed reduced ST (p = 0.03). HC2 showed that control group children spent more time on the computer (p < 0.01) and watching television (p < 0.0001) than the intervention. ICAPS showed increased PA (p < 0.0001) and decreased ST (p < 0.01). SUS showed increases in PA (0.20 sports or activities per year (95 % CI 0.06 to 0.33)) and reduced ST (−0.24 h per day, 95 % CI (−0.42 to −0.06)). Finally, Switch showed reduced ST (p < 0.05).
Psychosocial Outcomes
Five of eight studies reported impact on psychosocial outcomes, including quality of life, behavioral intentions, self-efficacy, depressive symptoms, perceived social support, and knowledge (Ballabeina, BHEZ, GEMS, ICAPS, and TEFNEP). Ballabeina showed no significant impact on quality of life or cognitive ability. BHEZ showed decreased behavioral intentions (p = 0.01), increased outcome expectancies (p = 0.02), and increased knowledge (p < 0.001) associated with the intervention. GEMS showed a significant difference in depressive symptoms (−0.21 Children’s Depression Inventory (0–20 scale), 95 % CI (−0.42 to −0.001)). ICAPS reported changes in self-efficacy and social support toward exercise at post, but these were not significant at follow-up. Intention to practice exercise was significantly improved at follow-up (p < 0.001). TEFNEP reported significant time effects for most indicators in both the control and the intervention groups at follow-up. For example, mean parent self-efficacy for modeling fruit, juice, and vegetable (FJV) consumption control mean 1.6 self-efficacy units (scale 0–2) (SE = 0.02) versus intervention 1.6 self-efficacy units (scale 0–2) (0.02).
Discussion
This is the first literature review to examine MLMC interventions for obesity prevention and reduction. We identified 14 trials that met inclusion criteria, 8 of which reported on impact.
Impact of Tested Interventions
The MLMC intervention studies reviewed clearly show promising behavioral impacts, particularly in terms of increasing intake of healthier foods and beverages. Additionally, improvements in PA and reduction in screen time were seen in some studies. Elsewhere, researchers have reported that PA interventions have had only limited impact on children’s overall activity levels [9], so our findings provide support for MLMC interventions as a more effective approach.
MLMC interventions were associated with obesity reductions in some (three of eight) of the study results reviewed. Sustained reductions in BMI among overweight and obese participants appear to be difficult to demonstrate in these interventions, most likely due to their limited time scope. In addition, the longest duration studies included in this pool lasted only 5 years and are not yet complete, so whether or not the interventions for children reduce the risk of NCDs later in life is unknown.
Psychosocial variables appear to be reported less frequently than other types of outcomes in MLMC trials. The studies reviewed did show some desirable impacts in psychosocial outcomes, but results were mixed.
Our review suggests that MLMC interventions may perform better than single-level interventions as approaches for obesity prevention. Integrated approaches outside of the school or other single-level focus, and especially within the community, for the purpose of NCD prevention are supported by the research as early as the 1980s [8]. The North Karelia Project, a large-scale, long-term MLMC intervention in Finland, showed successful behavioral changes resulting in significant improvements in mortality and morbidity among adults [10]. The program’s success strongly suggests that theory-based sustained activity within a national policy framework can support community aims to bridge cultural, political, economic, and psychological obstacles to health [10]. Our literature review provides support for these approaches to child health. Where most previous trials have been school-based and have had limited impact on obesity, school-based trials that have had impact have almost always integrated approaches outside the school and in the community [11, 12•].
Evaluating MLMC Interventions
Several authors expressed inability to determine which components of the intervention worked best and lacked clarification on synergies between interventions [13••, 14]. Future studies such as cluster randomized trials that compare a control group to an intervention with some components to an intervention with all components might prove fruitful. Also, future reviews evaluating the quality of MLMC studies may be helpful in understanding the overall quality of the existing evidence [15].
Process evaluations and other forms of evaluation should help address these questions. However, while process evaluations were completed by nearly all studies, methodology varied considerably. Few reported on how well studies set and met standards for intervention implementation, which made it difficult to assess implementation fidelity or compare one study with another. Increased consistency in process evaluation methods might help answer questions about which types of components are implementable in varied contexts. One strategy to test different MLMC interventions alone or in combination might use systems science modeling as a means of identifying best strategies and potential unintended consequences [16].
Context Matters
Our work supports the finding of the North Karelia Project that close collaboration with community and full participation from various levels are key for successful intervention programs [10]. BHEZ, CHL, and SUS employed community-based participatory techniques to develop and pilot intervention strategies. Their work suggests that knowing the specific context and program beneficiaries’ needs impacts the way that programs are developed, implemented, and how effective they will be. Researchers reported needing additional information to parse the relationship between the context of the intervention and the efficacy of the intervention in the context or population [17].
Policy Intervention Components
Policy interventions seem essential, but can be difficult to measure because the control group is often affected by the same policies as the test group. Further, administrative or policy-level buy-in is required to facilitate implementation of the intervention and lack of buy-in limits implementation. Nine studies in this pool involved a policy component. For example, in Porto Alegre, Brazil, a municipal law was passed that requires more healthful food options be sold at shops located within schools and prohibits sale of some types of less healthful foods, providing foundational support for the TriAtiva study. Similarly, the Ballabeina study in Switzerland builds on a new national health policy for schools. In the U.S., SUS is built on a state policy called, “Mass in Motion” which supports PA. These could not be explicitly tested in the study designs because the policy affected both the intervention and control groups. Nonetheless, the policy foundation is an essential component of the intervention and implementation. It is important for the field to continue to pursue research methods that permit and support evaluations of policy interventions (e.g., natural experiments with comparison communities), include strong process evaluations, and possibly find ways to compare across contexts to better understand the impact of these policies. For example, the Staple Food Ordinance Evaluation (STORE) Study examines the effect of the Staple Foods Ordinance passed in October of 2014 in the City of Minneapolis, MN, U.S. [18]. STORE researchers will compare the nutritional quality of customer purchases at small stores in Minneapolis to those in nearby St. Paul, MN where no such ordinance exists [18].
Conclusions
MLMC approaches are being tested in RCTs and to a lesser extent with quasi-experimental designs worldwide for obesity prevention and mitigation. These designs seem to be primarily focused on children in vulnerable or minority populations. Interventions integrate multiple components both related to diet and PA that act across multiple levels of the social and environmental context. These approaches are showing promising results in health, behavioral, and some psychosocial outcomes, particularly when they are able to integrate policy and community level components.
Future research may benefit from comprehensive, holistic interventions that support longer-term strategies, and which integrate policy and community components. Further, factorial study designs that test groups of intervention components are needed. Evaluations must be conducted of programs that capture effects outside of the individual, at the interpersonal, organizational, community, and policy levels.
Supplementary Material
Acknowledgments
The work described was supported by Grant Number U54HD070725 from the Eunice Kennedy Shriver National Institute of Child Health & Human Development (NICHD). The project is co-funded by the NICHD and the Office of Behavioral and Social Sciences Research (OBSSR). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NICHD or OBSSR.
Appendix 1: Search Terms
Inclusion Search Syntax
The search below is numbered by component for clarity. When utilized in the PubMed database, these components were run together as a single search procedure. See PubMed’s Medical Subject Heading (MeSH) Database Resource for additional details on search syntax.
-
Obesity Sphere
((“obesity “[MeSH Terms] AND (“prevention and control”[Subheading] OR “therapy”[Subheading]))
-
Multilevel Multicomponent Approach
((multi level[tw] OR multi leveled[tw] OR multi leveling[tw] OR multi levelled[tw] OR multi levels[tw]) OR (multilevel[tw] OR multilevel’[tw] OR multileveled[tw] OR multileveling[tw] OR multilevelled[tw] OR multilevelness[tw] OR multilevelpsa[tw] OR multilevels[tw] OR multilevelsupertree[tw]) OR (multi component[tw] OR multi componented[tw] OR multi componential[tw] OR multi components[tw]) OR (multicomponent[tw] OR multicomponent’[tw] OR multicomponental[tw] OR multicomponented[tw] OR multicomponential[tw] OR multicomponentness[tw] OR multicomponents[tw]) OR “health promotion”[MeSH Terms] OR “health education”[MeSH Terms]))
-
Obesity as a Risk Condition Within the MLMC Approach
(“overweight”[MeSH Terms] OR “obesity”[MeSH Terms] OR “obesity”[MeSH Terms] OR “risk”[MeSH Terms] OR Overweight[tw] OR obesity[tw] OR obese[tw])
-
Behavioral or Environmental Risk for Obesity
(“food habits”[MeSH Terms] OR “health behavior”[MeSH Terms] OR “diet”[MeSH Terms] OR “cooperative behavior”[MeSH Terms] OR “sedentary lifestyle”[MeSH Terms] OR “environment design”[MeSH Terms] OR “residence characteristics”[MeSH Terms] OR “risk reduction behavior”[MeSH Terms])
-
Study Type, Time frame, Focus Species, Language, and Article Type
Clinical Study[ptyp] AND “2006/01/28”[PDAT]: “2016/01/25”[PDAT] AND “humans”[MeSH Terms] AND English[lang] AND “journal article”[Publication Type]
Exclusion Filters Syntax
-
Smoking behavior
smoking[mh] OR tobacco[mh] OR Tobacco Smoke Pollution[mh] OR Smoking Cessation[mh]
-
Cancer
Mammography[mh] OR mastectomy[mh] OR neoplasms[mh] OR Lymphedema[mh] OR Breast Neoplasms[mh] OR Neoplasm Staging[mh]
-
Non-Food Diets
food, formulated[mh] OR “Meal replacements”[tw] OR edible grain[mh] OR Sweetening Agents[mh] OR Carbonated Beverages[mh] OR Beverages[mh] OR Dietary Carbohydrates[mh] OR Plant Extracts[mh] OR Sodium Chloride[mh] OR
-
Clinical Care
patient compliance[mh] OR postoperative complications[mh] OR nurses[mh] OR nursing[mh] OR nurse practitioners[mh] OR medication adherence[mh] OR adherence[tiab] OR Preoperative Period[mh] OR Insulin Resistance[mh] OR mass screening[mh] OR “Dietary Inflammatory Index”[tiab] OR Patient satisfaction[mh] OR Intention to Treat Analysis[mh] OR hospital[tiab] OR “bariatric surgery”[tiab] OR bariatric surgery[mh] OR bariatrics[mh] OR gastric bypass[mh]
-
Disease Conditions and Treatments Outside of the Scope
Cognitive Therapy/methods*[mh] OR Psychological Theory[mh] OR Inflammation*[mh] OR Bone Resorption[mh] OR atherosclerosis[mh] OR leptin[mh] OR “spinal stenosis”[tiab] OR “Endothelial dysfunction”[tiab] OR “spinal cord”[tiab]
-
Statistical Methods Focus
Reproducibility of Results[mh] OR Models, Statistical*[mh]
Footnotes
This article is part of the Topical Collection on The Obesity Epidemic: Causes and Consequences
Compliance with Ethics Guidelines
Conflict of Interest Ella Ewart-Pierce, María José Mejía Ruiz, and Joel Gittelsohn declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent This article does not contain any studies with human or animal subjects performed by any of the authors.
References
Papers of particular interest, published recently, have been highlighted as:
• Of importance
•• Of major importance
- 1.Swinburn BA, Sacks G, Hall KD, et al. The global obesity pandemic: shaped by global drivers and local environments. Lancet. 2011;378(9793):804–14. doi: 10.1016/S0140-6736(11)60813-1. [DOI] [PubMed] [Google Scholar]
- 2.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311(8):806–14. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gittelsohn J, Steeves EA, Mui Y, Kharmats AY, Hopkins LC, Dennis D. B’more healthy communities for kids: design of a multi-level intervention for obesity prevention for low-income African-American children. BMC Public Health. 2014;14(1):942. doi: 10.1186/1471-2458-14-942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fialkowski MK, DeBaryshe B, Bersamin A, et al. A community engagement process identifies environmental priorities to prevent early childhood obesity: the Children’s Healthy Living (CHL) program for remote underserved populations in the US Affiliated Pacific Islands, Hawaii and Alaska. Matern Child Health J. 2014;18(10):2261–74. doi: 10.1007/s10995-013-1353-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bronfenbrenner U. Ecological systems theory. In: Vasta R, editor. Six theories of child development: revised formulations and current issues. London: Jessica Kingsley Publishers; 1992. pp. 187–249. [Google Scholar]
- 6.Farquhar JW, Fortmann SP, Maccoby N, et al. The Stanford five-city project: design and methods. Am J Epidemiol. 1985;122(2):323–34. doi: 10.1093/oxfordjournals.aje.a114104. [DOI] [PubMed] [Google Scholar]
- 7.Caballero B, Clay T, Davis SM, et al. Pathways: a school-based, randomized controlled trial for the prevention of obesity in American Indian schoolchildren. Am J Clin Nutr. 2003;78(5):1030–8. doi: 10.1093/ajcn/78.5.1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Puska P, Vartiainen E, Pallonen U, et al. The North Karelia Youth Project: evaluation of two years of intervention on health behavior and CVD risk factors among 13- to 15-year old children. Prev Med. 1982;11(5):550–70. doi: 10.1016/0091-7435(82)90068-8. [DOI] [PubMed] [Google Scholar]
- 9.Metcalf B, Henley W, Wilkin T. Effectiveness of intervention on physical activity of children: systematic review and meta-analysis of controlled trials with objectively measured outcomes (Early Bird 54) BMJ. 2012;345:e5888. doi: 10.1136/bmj.e5888. [DOI] [PubMed] [Google Scholar]
- 10.Puska P. Successful prevention of non-communicable diseases: 25 year experiences with North Karelia Project in Finland. Public Health Med. 2002;4(1):5–7. [Google Scholar]
- 11.Gittelsohn J, Kumar MB. Preventing childhood obesity and diabetes: is it time to move out of the school? Pediatr Diabetes. 2007;8(Suppl 9):55–69. doi: 10.1111/j.1399-5448.2007.00333.x. [DOI] [PubMed] [Google Scholar]
- 12•.Gittelsohn J, Park S. School- and community-based interventions. In: Freemark M, editor. Pediatric obesity: etiology, pathogenesis, and treatment. New York: Humana Press; 2010. pp. 315–336. Clarifies meaning and significance of community involvement, especially for interventions focused on children. [Google Scholar]
- 13••.Economos CD, Folta SC, Goldberg J, et al. A community-based restaurant initiative to increase availability of healthy menu options in Somerville, Massachusetts: Shape up Somerville. Prev Chronic Dis. 2009;6(3):A102. MLMC approach with a novel quasi-experimental design and innovative, extensive community involvement that shows strong results at multiple levels. [PMC free article] [PubMed] [Google Scholar]
- 14.Safdie M, Cargo M, Richard L, Levesque L. An ecological and theoretical deconstruction of a school-based obesity prevention program in Mexico. Int J Behav Nutr Phys Act. 2014;11:103. doi: 10.1186/s12966-014-0103-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Briss PA, Zaza S, Pappaioanou M, et al. Developing an evidence-based Guide to Community Preventive Services—methods. The Task Force on Community Preventive Services. Am J Prev Med. 2000;18(1 Suppl):35–43. doi: 10.1016/s0749-3797(99)00119-1. [DOI] [PubMed] [Google Scholar]
- 16.Finegood DT, Cawley J. The complex systems science of obesity. The Oxford handbook of the social science of obesity. 2011:208–36. [Google Scholar]
- 17.Safdie M, Levesque L, Gonzalez-Casanova I, et al. Promoting healthful diet and physical activity in the Mexican school system for the prevention of obesity in children. Salud Publica Mex. 2013;55(Suppl 3):357–73. doi: 10.21149/spm.v55s3.5137. [DOI] [PubMed] [Google Scholar]
- 18.Laska M. STaple food ORdinance evaluation (STORE) study: assessing the impact of a local staple food ordinance on healthy food availability. http://www.globalobesity.org/our-projects/staple-food-ordinance-pilot/staple-food-ordinance-study.html. Updated 2016. Accessed 5/3, 2016.
- 19.Michels N, Susi K, Marques-Vidal PM, Nydegger A, Puder JJ. Psychosocial quality-of-life, lifestyle and adiposity: a longitudinal study in pre-schoolers (Ballabeina Study) Int J Behav Med. 2016 doi: 10.1007/s12529-016-9537-z. [DOI] [PubMed] [Google Scholar]
- 20.Niederer I, Burgi F, Ebenegger V, et al. Effects of a lifestyle intervention on adiposity and fitness in overweight or low fit preschoolers (Ballabeina) Obesity (Silver Spring) 2013;21(3):E287–93. doi: 10.1002/oby.20119. [DOI] [PubMed] [Google Scholar]
- 21.Burgi F, Niederer I, Schindler C, et al. Effect of a lifestyle intervention on adiposity and fitness in socially disadvantaged subgroups of preschoolers: a cluster-randomized trial (Ballabeina) Prev Med. 2012;54(5):335–40. doi: 10.1016/j.ypmed.2012.02.007. [DOI] [PubMed] [Google Scholar]
- 22.Puder JJ, Marques-Vidal P, Schindler C, et al. Effect of multidimensional lifestyle intervention on fitness and adiposity in predominantly migrant preschool children (Ballabeina): cluster randomized controlled trial. BMJ. 2011;343:d6195. doi: 10.1136/bmj.d6195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Burgi F, Meyer U, Niederer I, et al. Socio-cultural determinants of adiposity and physical activity in preschool children: a cross-sectional study. BMC Public Health. 2010;10:733. doi: 10.1186/1471-2458-10-733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Niederer I, Kriemler S, Zahner L, et al. Influence of a lifestyle intervention in preschool children on physiological and psychological parameters (Ballabeina): study design of a cluster randomized controlled trial. BMC Public Health. 2009;9:94. doi: 10.1186/1471-2458-9-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shin A, Surkan PJ, Coutinho AJ, et al. Impact of Baltimore healthy eating zones: an environmental intervention to improve diet among African-American youth. Health Educ Behav. 2015;42(1 Suppl):97S–105S. doi: 10.1177/1090198115571362. [DOI] [PubMed] [Google Scholar]
- 26.Gittelsohn J, Dennisuk LA, Christiansen K, et al. Development and implementation of Baltimore healthy eating zones: a youth-targeted intervention to improve the urban food environment. Health Educ Res. 2013;28(4):732–44. doi: 10.1093/her/cyt066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27••.Pratt CA, Boyington J, Esposito L, et al. Childhood obesity prevention and treatment research (COPTR): interventions addressing multiple influences in childhood and adolescent obesity. Contemp Clin Trials. 2013;36(2):406–13. doi: 10.1016/j.cct.2013.08.010. Large-scale example of a multi-site MLMC trial effectively modeling the approach. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sherwood NE, French SA, Veblen-Mortenson S, et al. NET-works: linking families, communities and primary care to prevent obesity in preschool-age children. Contemp Clin Trials. 2013;36(2):544–54. doi: 10.1016/j.cct.2013.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Robinson TN, Matheson D, Desai M, et al. Family, community and clinic collaboration to treat overweight and obese children: Stanford GOALS—a randomized controlled trial of a three-year, multi-component, multi-level, multi-setting intervention. Contemp Clin Trials. 2013;36(2):421–35. doi: 10.1016/j.cct.2013.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Po’e EK, Heerman WJ, Mistry RS, Barkin SL. Growing right onto wellness (GROW): a family-centered, community-based obesity prevention randomized controlled trial for preschool child-parent pairs. Contemp Clin Trials. 2013;36(2):436–49. doi: 10.1016/j.cct.2013.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Moore SM, Borawski EA, Cuttler L, Ievers-Landis CE, Love TE. IMPACT: a multi-level family and school intervention targeting obesity in urban youth. Contemp Clin Trials. 2013;36(2):574–86. doi: 10.1016/j.cct.2013.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ayala GX, Ibarra L, Binggeli-Vallarta A, et al. Our choice/Nuestra Opcion: The Imperial County, California, Childhood Obesity Research Demonstration Study (CA-CORD) Child Obes. 2015;11(1):37–47. doi: 10.1089/chi.2014.0080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Joseph S, Stevens AM, Ledoux T, O’Connor TM, O’Connor DP, Thompson D. Rationale, design, and methods for process evaluation in the childhood obesity research demonstration project. J Nutr Educ Behav. 2015;47(6):560–5.e1. doi: 10.1016/j.jneb.2015.07.002. [DOI] [PubMed] [Google Scholar]
- 34.Chuang E, Ayala GX, Schmied E, Ganter C, Gittelsohn J, Davison KK. Evaluation protocol to assess an integrated framework for the implementation of the Childhood Obesity Research Demonstration Project at the California (CA-CORD) and Massachusetts (MA-CORD) sites. Child Obes. 2015;11(1):48–57. doi: 10.1089/chi.2014.0049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Davison KK, Falbe J, Taveras EM, et al. Evaluation overview for the Massachusetts Childhood Obesity Research Demonstration (MA-CORD) Project Child Obes. 2015;11(1):23–36. doi: 10.1089/chi.2014.0059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dooyema CA, Belay B, Foltz JL, Williams N, Blanck HM. The Childhood Obesity Research Demonstration Project: a comprehensive community approach to reduce childhood obesity. Child Obes. 2013;9(5):454–9. doi: 10.1089/chi.2013.0060. [DOI] [PubMed] [Google Scholar]
- 37.Foltz JL, Belay B, Dooyema CA, Williams N, Blanck HM. Childhood Obesity Research Demonstration (CORD): the cross-site overview and opportunities for interventions addressing obesity community-wide. Child Obes. 2015;11(1):4–10. doi: 10.1089/chi.2014.0159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hoelscher DM, Butte NF, Barlow S, et al. Incorporating primary and secondary prevention approaches to address childhood obesity prevention and treatment in a low-income, ethnically diverse population: study design and demographic data from the Texas Childhood Obesity Research Demonstration (TX CORD) study. Child Obes. 2015;11(1):71–91. doi: 10.1089/chi.2014.0084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.O’Connor DP, Lee RE, Mehta P, et al. Childhood obesity research demonstration project: cross-site evaluation methods. Child Obes. 2015;11(1):92–103. doi: 10.1089/chi.2014.0061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Taveras EM, Blaine RE, Davison KK, et al. Design of the Massachusetts Childhood Obesity Research Demonstration (MA-CORD) study. Child Obes. 2015;11(1):11–22. doi: 10.1089/chi.2014.0031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Blanck HM, Collins JL. The childhood obesity research demonstration project: linking public health initiatives and primary care interventions community-wide to prevent and reduce childhood obesity. Child Obes. 2015;11(1):1–3. doi: 10.1089/chi.2014.0122. [DOI] [PubMed] [Google Scholar]
- 42.Butel J, Braun KL, Novotny R, et al. Assessing intervention fidelity in a multi-level, multi-component, multi-site program: the Children’s Healthy Living (CHL) program. Transl Behav Med. 2015;5(4):460–9. doi: 10.1007/s13142-015-0334-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fialkowski MK, Delormier T, Hattori-Uchima M, et al. Children’s Healthy Living Program (CHL) indigenous workforce training to prevent childhood obesity in the underserved U.S.-affiliated Pacific region. J Health Care Poor Underserved. 2015;26(2 Suppl):83–95. doi: 10.1353/hpu.2015.0054. [DOI] [PubMed] [Google Scholar]
- 44.Li F, Wilkens LR, Novotny R, et al. Anthropometric measurement standardization in the U.S.-affiliated Pacific: report from the Children’s Healthy Living Program. Am J Hum Biol. 2015 doi: 10.1002/ajhb.22796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Novotny R, Fialkowski MK, Li F, et al. Systematic review of prevalence of young child overweight and obesity in the U.S.-affiliated Pacific region compared with the 48 contiguous states: The Children’s Healthy Living Program. Am J Public Health. 2015;105(1):e22–35. doi: 10.2105/AJPH.2014.302283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Braun KL, Nigg CR, Fialkowski MK, et al. Using the ANGELO model to develop the children’s healthy living program multilevel intervention to promote obesity preventing behaviors for young children in the U.S.-affiliated Pacific Region. Child Obes. 2014;10(6):474–81. doi: 10.1089/chi.2014.0102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Novotny R, Fialkowski MK, Areta AA, et al. University of Hawai’i Cancer Center Connection: The Pacific way to child wellness: The Children’s Healthy Living (CHL) Program for remote underserved minority populations of the Pacific region. Hawaii J Med Public Health. 2013;72(11):406–8. [PMC free article] [PubMed] [Google Scholar]
- 48.Wilken LR, Novotny R, Fialkowski MK, et al. Children’s Healthy Living (CHL) program for remote underserved minority populations in the Pacific region: rationale and design of a community randomized trial to prevent early childhood obesity. BMC Public Health. 2013;13:944. doi: 10.1186/1471-2458-13-944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Dalton WT, Klesges LM, Sherrill-Mittleman D, Stockton MB, Allen S, Klesges RC. Family context as it relates to weight-related behaviors in preadolescent African-American girls. Am J Health Behav. 2011;35(3):269–79. doi: 10.5993/ajhb.35.3.2. [DOI] [PubMed] [Google Scholar]
- 50.Klesges RC, Obarzanek E, Kumanyika S, et al. The Memphis Girls’ Health Enrichment Multi-site Studies (GEMS): an evaluation of the efficacy of a 2-year obesity prevention program in African-American girls. Arch Pediatr Adolesc Med. 2010;164(11):1007–14. doi: 10.1001/archpediatrics.2010.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Robinson TN, Matheson DM, Kraemer HC, et al. A randomized controlled trial of culturally tailored dance and reducing screen time to prevent weight gain in low-income African-American girls: Stanford GEMS. Arch Pediatr Adolesc Med. 2010;164(11):995–1004. doi: 10.1001/archpediatrics.2010.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Klesges RC, Obarzanek E, Klesges LM, et al. Memphis Girls health Enrichment Multi-site Studies (GEMS): Phase 2: design and baseline. Contemp Clin Trials. 2008;29(1):42–55. doi: 10.1016/j.cct.2007.05.001. [DOI] [PubMed] [Google Scholar]
- 53.Robinson TN, Kraemer HC, Matheson DM, et al. Stanford GEMS phase 2 obesity prevention trial for low-income African-American girls: design and sample baseline characteristics. Contemp Clin Trials. 2008;29(1):56–69. doi: 10.1016/j.cct.2007.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Natale RA, Messiah SE, Asfour L, Uhlhorn SB, Delamater A, Arheart KL. Role modeling as an early childhood obesity prevention strategy: effect of parents and teachers on preschool children’s healthy lifestyle habits. J Dev Behav Pediatr. 2014;35(6):378. doi: 10.1097/DBP.0000000000000074. [DOI] [PubMed] [Google Scholar]
- 55.Natale R, Scott SH, Messiah SE, Schrack MM, Uhlhorn SB, Delamater A. Design and methods for evaluating an early childhood obesity prevention program in the childcare center setting. BMC Public Health. 2013;13:78. doi: 10.1186/1471-2458-13-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Quintiliani LM, DeBiasse MA, Branco JM, Bhosrekar SG, Rorie JA, Bowen DJ. Enhancing physical and social environments to reduce obesity among public housing residents: rationale, trial design, and baseline data for the Healthy Families Study. Contemp Clin Trials. 2014;39(2):201–10. doi: 10.1016/j.cct.2014.08.005. [DOI] [PubMed] [Google Scholar]
- 57.Simon C, Kellou N, Dugas J, et al. A socio-ecological approach promoting physical activity and limiting sedentary behavior in adolescence showed weight benefits maintained 2.5 years after intervention cessation. Int J Obes (Lond) 2014;38(7):936–43. doi: 10.1038/ijo.2014.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Simon C, Schweitzer B, Oujaa M, et al. Successful overweight prevention in adolescents by increasing physical activity: a 4-year randomized controlled intervention. Int J Obes. 2008;32(10):1489. doi: 10.1038/ijo.2008.99. [DOI] [PubMed] [Google Scholar]
- 59.Simon C, Wagner A, Platat C, et al. ICAPS: a multilevel program to improve physical activity in adolescents. Diabetes Metab. 2006;32(1):41. doi: 10.1016/s1262-3636(07)70245-8. [DOI] [PubMed] [Google Scholar]
- 60.Simon C, Wagner A, DiVita C, et al. Intervention Centered on Adolescents’ Physical Activity and Sedentary Behavior (ICAPS): concept and 6-month results. Int J Obes Relat Metab Disord. 2004;28(Suppl 3):S96–S103. doi: 10.1038/sj.ijo.0802812. [DOI] [PubMed] [Google Scholar]
- 61.Coffield E, Nihiser AJ, Sherry B, Economos CD. Shape up Somerville: change in parent body mass indexes during a child-targeted, community-based environmental change intervention. Am J Public Health. 2015;105(2):e83–9. doi: 10.2105/AJPH.2014.302361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Economos CD, Hyatt RR, Must A, et al. Shape up Somerville two-year results: a community-based environmental change intervention sustains weight reduction in children. Prev Med. 2013;57(4):322–7. doi: 10.1016/j.ypmed.2013.06.001. [DOI] [PubMed] [Google Scholar]
- 63•.Folta SC, Kuder JF, Goldberg JP, et al. Changes in diet and physical activity resulting from the Shape up Somerville community intervention. BMC Pediatr. 2013;13:157. doi: 10.1186/1471-2431-13-157. MLMC approach with a novel quasi-experimental design and innovative, extensive community involvement that shows strong results at multiple levels. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Goldberg JP, Collins JJ, Folta SC, et al. Retooling food service for early elementary school students in Somerville, Massachusetts: the Shape Up Somerville experience. Prev Chronic Dis. 2009;6(3):A103. [PMC free article] [PubMed] [Google Scholar]
- 65.Economos CD, Hyatt RR, Goldberg JP, et al. A community intervention reduces BMI z-score in children: Shape up Somerville first year results. Obesity (Silver Spring) 2007;15(5):1325–36. doi: 10.1038/oby.2007.155. [DOI] [PubMed] [Google Scholar]
- 66.Gentile DA, Welk G, Eisenmann JC, et al. Evaluation of a multiple ecological level child obesity prevention program: Switch what you Do, View, and Chew. BMC Med. 2009;7:49. doi: 10.1186/1741-7015-7-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Eisenmann JC, Gentile DA, Welk GJ, et al. SWITCH: rationale, design, and implementation of a community, school, and family-based intervention to modify behaviors related to childhood obesity. BMC Public Health. 2008;8:223. doi: 10.1186/1471-2458-8-223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Cullen KW, Thompson DI, Scott AR, Lara-Smalling A, Watson KB, Konzelmann K. The impact of goal attainment on behavioral and mediating variables among low-income women participating in an expanded food and nutrition education program intervention study. Appetite. 2010;55(2):305–10. doi: 10.1016/j.appet.2010.06.017. [DOI] [PubMed] [Google Scholar]
- 69.Cullen KW, Lara Smalling A, Thompson D, Watson KB, Reed D, Konzelmann K. Creating healthful home food environments: results of a study with participants in the expanded food and nutrition education program. J Nutr Educ Behav. 2009;41(6):380–8. doi: 10.1016/j.jneb.2008.12.007. [DOI] [PubMed] [Google Scholar]
- 70.Friedrich RR, Caetano LC, Schiffner MD, Wagner MB, Schuch I. Design, randomization and methodology of the TriAtiva program to reduce obesity in school children in southern Brazil. BMC Public Health. 2015;15:363. doi: 10.1186/s12889-015-1727-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


