History
A 5-year-old girl presented with a history of fever for four days associated with odynophagia. She was treated with amoxycillin prescribed by a general practitioner for 3 days prior to presentation. However, the symptoms were worsening and associated with drooling of saliva and poor oral intake. There was history of recurrent acute tonsillitis in the past two years, with 5 to 6 episodes per year. The child had completed regular immunizations up to her current age. There was no similar presentation amongst family members and friends.
On examination, the child was comfortable, with no observed stridor or wheezing. She was not tachycardia There was, as mentioned, drooling of saliva. An oral cavity examination was performed (Figure 1), and other system other system examinations were uneventful.
Figure 1:
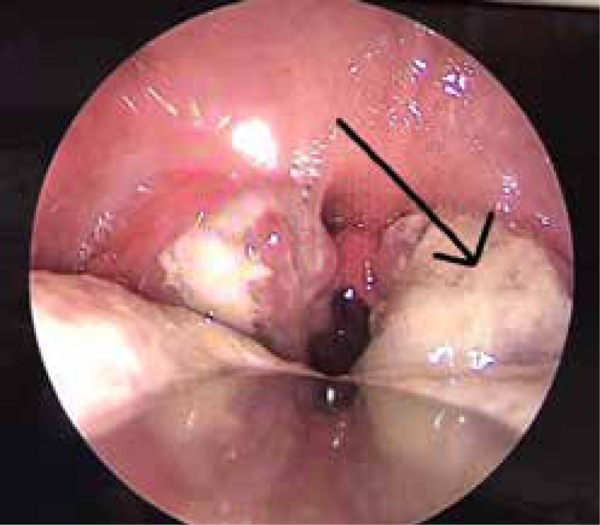
The coated tonsils in this case, with more on the left tonsil
Questions
State the findings.
What is the most probable diagnosis?
How should the diagnosis be confirmed?
What prophylactic measures should be taken?
Answers
An oral cavity examination showed bilaterally enlarged tonsils (grade 3) with a thick coating of grayish pseudomembrane, which was more pronounced on the left tonsil. Although there was no bleeding when the pseudomembrane was scraped, there was discomfort and pain associated with the act, which indicated diphtheria, although, in diphtheria, the membrane adheres and bleeds when an attempt to scrape the membrane is made.
The most probable diagnosis for this child is diphtheria. The fact that the grayish substance on the tonsils could be scraped is an indication of the presence of a pseudomembrane. The diagnosis is also supported by the fact that the child was drooling saliva.
-
To come to a diagnosis of diphtheria, a high index of clinical suspicion is required. Samples should be taken from the throat or nasopharynx or both, if necessary, and sent for culture. In other forms of diphtheria, such as the cutaneous form, culture samples should be taken from the wound or any skin lesions. When there is a membranous material, it should also be taken and examined, and care should be taken to obtain the material beneath the membrane, as well.1
Specimens obtained should be transported immediately to the laboratory to enable rapid inoculation of the organism in order to obtain the best results. Specimens should be ideally cultured in blood agar and selective tellurite media. This media inhibits the growth of normal flora, and organisms, such as diphtheria, produce characteristic black colonies.2 Other basic investigations include full blood counts, a renal function test for assessment of hydration and acute kidney injury secondary to dehydration in a child with poor oral intake, and a chest radiograph in the case of respiratory diphtheria.3
In managing diphtheria, household contacts and health personnel who were in close contact and did not not wear personal protective equipment should also be covered with post- exposure prophylaxis. In the case of close contacts, such as household contacts, diphtheria boosters appropriate for age should be administered. Contacts should receive antibiotics. A single dose of IM benzathine penicillin G (600,000 units for persons younger than 6 years old and 1,200,000 units for those 6 years old and older) should be administered or a 7 to 10 day course of oral erythromycin (40–50 mg/kg/ day, maximum 2g/day for children and 1 g/day for adults) should be prescribed.4 The health ministry should also be notified when diphtheria is suspected to enable contact tracing and further management in curbing the disease from spreading.5
References
- 1.Clarridge JE, Popovic T, Inzana TJ. Hausler WJ, Sussman M. Topley and Wilson's microbiology and microbial infections. Vol. 3. New York: Oxford University Press; 1998. Diphtheria and other corynebacterial and coryneform infections; pp. 347–71. [Google Scholar]
- 2.Efstratiou A, Engler KH, Mazurova IK, Glushkevich T, Vuopio-Varkila J, Popovic T. Current approaches to the laboratory diagnosis of diphtheria. JID. 2000;181(Supplement 1):S138–45. doi: 10.1086/315552. [DOI] [PubMed] [Google Scholar]
- 3.Bisgard KM, Hardy IR, Popovic T, Strebel PM, Wharton M, Chen RT. et al. Respiratory diphtheria in the United States, 1980 through 1995. AJPH. 1998;88(5):787–91. doi: 10.2105/ajph.88.5.787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Epidemiology and Prevention of Vaccine-Preventble Diseases 13th Edition. Centers for Disease Control and Prevention; 2015. [Accessed Apr 30;2018 ]. Diphtheria.http://www.cdc.gov/vaccines/pubs/pinkbook/downloads/dip.pdf Updated April. [Google Scholar]
- 5.Diphtheria, Case Investigation and Outbreak Management Manual for Healthcare Personnel 2014. 2016 Dec 17;


