Abstract
Background
Primary osteoporosis is a common disease among postmenopausal women and the elderly; low back pain is the most typical clinical manifestation an is the primary reason for a clinic visit, and directly affects patients’ quality of life. Anti-osteoporosis medications have undesirable side effects, and many kinds of special traditional Chinese moxibustion methods have been widely used in the clinical treatment of osteoporosis low back pain. The purpose of this study was to observe whether thunder-fire moxibustion therapy, compared to calcium supplements alone, can ease osteoporosis low back pain, improve quality of life, and reduce tension of the multifidus.
Material/Methods
Sixty-three eligible patients were enrolled in the study (7 of these patients did not finish the study and are not included in analysis). Participants were randomly divided into 2 groups: a moxibustion group that received calcium carbonate D3 and thunder-fire moxibustion therapy, and a control group that received calcium carbonate D3 only. Level of pain experienced, assessed using the visual analogue scale (VAS), and quality of life (SF-36) were measured pre-treatment, at the end of 4 weeks of treatment, and at a 1-month post-treatment evaluation. Changes in values of Young’s modulus of the multifidus were also collected before and after treatment.
Results
After 4 weeks of treatment and at 1 month after treatment had ended, low back pain in both groups was reduced relative to pre-treatment levels. The moxibustion group was significantly improved at BP, GH, SF, and MH dimensions compared to pre-treatment levels. The control group improved in BP dimensions, but not to the same extent as the moxibustion group. Similarly, after treatment for 4 weeks with moxibustion, multifidus tension was significantly reduced.
Conclusions
Thunder-fire moxibustion is an effective method for treating low back pain due to primary osteoporosis.
MeSH Keywords: Low Back Pain, Osteoporosis, SF-36, Thunder-Fire Moxibustion, VAS, Yang’s Modulus
Background
Primary osteoporosis (POP) is defined as low bone mass and is a systemic bone disease characterized by degeneration of the micro-architecture of bone tissue that leads to an increase in bone brittleness and bones that fracture easily. It is a common disease, occurring frequently in postmenopausal women and the elderly [1]. The National Health and Nutrition Examination Surveys (NHANES) III [2] found that more than 9.9 million Americans suffer from osteoporosis, and about 43.1 million Americans suffer from osteopenia. Epidemiology shows that China has more than 210 million people aged >60 years (~15.5% of the total population), nearly 140 million people aged >65 years (~10.1% of the total population) [3], and has the largest population of elderly people in the world. In 2006, China had nearly 70 million cases of osteoporosis and more than 200 million cases of osteopenia [4]. Despite a lack of recent epidemiological data, it is certain that the number of people with osteoporosis and osteopenia in China is now even greater, given the aging trend of the population. Low back pain is the most typical clinical manifestation of POP and is the primary reason for visiting a clinic; limited lumbar back pain accounts for 70% of the cases of osteoporosis with pain in China, and directly affects a patient’s quality of life [5,6].
Clinical practice shows that drug therapy has definite limitations. Bisphosphonates are the most widely used anti-osteoporosis drugs in clinical practice, but they do not relieve pain quickly. The benefits of treatment for more than 5 years are limited and may increase the risk of jaw osteonecrosis or atypical femoral fracture [7,8]. Calcitonin can increase bone mass and effectively relieve bone pain [9–13], but may increase tumor risk, and is limited to no more than 3 months of continuous use [14].
Traditional Chinese moxibustion methods have been widely used in the clinical treatment of low back pain of POP. The other type of moxibustion [15–17] has a clear analgesic effect on osteoporosis low back pain. A meta-analysis concluded that non-thunder-fire moxibustion plus calcium supplementation may have a better effect on alleviating pain than calcium supplements alone [18].
Thunder-fire moxibustion is a moxibustion method used in various Chinese medicines that is characterized by strong penetration, a strong effect on blood stasis and swelling, and pain relief. The treatment characteristics of thunder-fire moxibustion are as follow. The first characteristic is that, according to the principle of TCM syndrome differentiation and treatment, a variety of drugs are used to make different kinds of thunder-fire moxibustion columns. The second characteristic is the use of a variety of therapeutic techniques such as the method of finches and array method. The third characteristic is that, when burnt, thunder-fire moxibustion produces a powerful potency, with drug factors rapidly adsorption in the human body surface, forming high-consistency medicine in areas around the skin, penetrates into acupuncture points and through the human body meridian transmission to improve treatment effect [19]. With the help of thermal radiation, thunder-fire moxibustion can improve circulation by penetrating into deep tissue through heat [20]. The operation is simple, the target acupoint location is accurate, the heat is easy to control, scald danger is low and safety high, and the moxibustion smog is reduced, making it suitable for clinical application. It is often used for various spine-related pain treatments [21]. However, clinical studies on its use for the treatment of POP low back pain have not been reported. Zhang [22] showed that thunder-fire moxibustion can reduce the pain of knee osteoarthritis and decrease dysfunction.
In the present study, we tested whether thunder-fire moxibustion can affect degree of pain, quality of life, and Young’s modulus of multifidus in POP patients.
Material and Methods
Design
A randomized controlled trial was performed; all clinical examinations and non-drug treatments were provided free of charge because we had sufficient funding for the project. The 63 patients recruited were randomly divided into a moxibustion group (n=32) or a control group (n=31), with all patients having equal access to either group. To randomize patient group assignment, the envelope method was used as follows: (i) a person unaware of the trial put the numbers 1 to 63 in 63 opaque envelopes; (ii) the patient randomly selected an envelope; (iii) patients selecting an odd number were place in the moxibustion group and given calcium carbonate D3 (CC D3) combined with thunder-fire moxibustion therapy, while patients with an even number were placed in the control group and given only CC D3 treatment. Of the 63 participants, we were unable to collect data from 7; 3 patients failed to complete 4 weeks of treatment, and 4 patients refused to return to the hospital for a follow-up evaluation. In the end, we had data for 56 patients. Recruitment of the participants was done in October 2016 and post-intervention assessments were completed in November 2017.
Participants
Cases of potential POP with low back pain (n=142) were collected from the Department of Acupuncture and Rehabilitation, and the Department of Orthopedics, at the Affiliated Hospital of Nanjing University of Traditional Chinese Medicine. The diagnosis of osteoporosis densitometry (DXA) is still the criterion standard. The World Health Organization (WHO) defines osteoporosis by quantitative densitometry measurements of bone mineral density (BMD) in terms of deviations in relation to a young healthy person. According to this definition, a BMD value of less than 2.5 standard deviations below the mean is defined as osteoporosis, while values from 1.5 to 2.5 standard deviations below the mean are defined as osteopenia.
Study inclusion criteria were: postmenopausal women aged 50–80 years; a double-energy X-ray bone density lower than 2.5 standard deviations below normal; and presence of lower back pain for more than 3 months at a moderate level (3≤ VAS ≤7). Exclusion criteria were: secondary or idiopathic osteoporosis; taking of anti-osteoporosis drugs or other drugs that affect bone metabolism for 6 months; lumbar compressibility fractures; lumbar disc herniation, lumbar spondylolisthesis, or lumbar stenosis; serious underlying diseases that might affect treatment; and a history of smoking, alcohol abuse, or other habits deleterious to health.
Sixty-three eligible participants provided written informed consent after receiving an explanation of the study (Table 1).
Table 1.
Baseline clinical characteristics of participants.
| Moxibustion group (n=32) | Control group (n=31) | P value | |
|---|---|---|---|
| Age (years) | 65.16 | 63.90 | P>0.05 |
| ±6.82 | ±7.59 | ||
| Height (cm) | 159.31 | 158.65 | P>0.05 |
| ±6.60 | ±5.31 | ||
| Body weight (kg) | 55.95 | 56.53 | P>0.05 |
| ±9.41 | ±6.83 | ||
| Duration of back pain (months) | 11.31 | 11.32 | P>0.05 |
| ±4.03 | ±4.16 | ||
| BMI | 22.00 | 22.31 | P>0.05 |
| ±3.02 | ±2.56 |
The Ethics Committee of the Affiliated Hospital of Nanjing University of Traditional Chinese Medicine approved this study (ethics review number 2017NL-001-01).
Intervention
The moxibustion treatment group (n=32) received thunder-fire moxibustion as well as oral CC D3. All the moxa-cigars for the moxibustion are produced from the Traditional Medicine Research Institute of Zhao’s thunder-fire moxibustion. Each moxa-cigar is 10×3 cm and 25 g.
The treatment site was the local lumbago, using acupoint selections Pishu (BL 20), Shenshu (BL 23), Yaoyangguan (DU 3), and Mingmen (DU 4). Treatments were done at room temperature (20–25ºC), with the subject in a relaxed prone position. Two moxa-cigars were placed in a 2-hole moxibustion box and the tops of the moxa-cigars were lit. The moxibustion box was then placed on the treatment site, with the fire head 2–3 cm from skin. Moxibustion was performed on the local low back pain area for a treatment time of 30 min. The moxibustion box and treatment area were covered with a thick treatment towel to maintain temperature and control smoking. Treatments were given 3 days per week for 4 weeks (Figures 1–3).
Figure 1.

preparation of thunder-fire moxibustion box.
Figure 2.

position of moxibustion treatment.
Figure 3.

moxibustion box covered with treatment towel.
The calcium D treatment consisted of CC D3 (1.5 g/125 u per tablet), with 1 tablet per day taken orally. The control group (n=31) received only the CC D3 treatment.
Outcome measures
Visual Analogue Scale (VAS). A 10-cm linear visual analogue scale was used to assess each participant’s rating of their level of pain [20]. The visual analogue scale is a double-anchored horizontal line where each end represents opposite ends of a continuum that extends from “not at all” (score=0) at the left end of the scale to “the worst possible” (score=10) at the right end of the line. Participants were instructed to indicate their level of pain with a mark made on the linear scale.
Quality of Life Assessment. The Medical Outcomes Study 36-Item Short-Form Health Survey (SF-36) [23] is a concise health measurement scale developed by the Boston Institute of Health. It has 8 dimensions and 36 clauses, including the dimensions physical functioning (PF), physical role limitation (RP), bodily pain (BP), general health (GH), vitality (V), social functioning (SF), emotional role limitation (RE), and mental health (MH). Question responses are transformed into a point scale ranging from 0 to 100.
Shear-Wave Elastography (SWE) Image. All quantitative ultrasound examinations of the lumbar multifidus muscles were taken using an ultrasound imaging device with SWE (Aixplorer, Supersonic Imagine, Aix-en-Provence, France) with a 10-2 MHz linear array transducer (model SL10-2, 7 MHz of center frequency, Aixplorer, Supersonic Imagine, France). The rehabilitation ultrasound model was selected and the maximum range of SWE set at 50 KPa. The square-shape region of interest (ROI) was 10×10 mm and the diameter of the Q-box (Supersonic, Imagine, Inc) was 10 mm.
Patients were asked to take a prone position on the bed, without a pillow, the head to one side, the upper limbs on either side of the body, and both lower limbs straight. The transducer was positioned on the skin so that it was centered on the spine. Then, the L4 and L5 spinous processes above the sacroiliac joint were found and the transducer moved to the right or left side, in order to display the L4 and L5 zygapophyseal joints. A mark was made on the skin.
The values of Young’s modulus of the multifidus were measured in the L4 plane. The shear elastic modulus of the lumbar multifidus was evaluated 3 times by measuring the shear wave propagation speed in the tissues to assess muscle stiffness. The average values of maximum, minimum, and mean shear elastic modulus in each ROI were computed. The shear elastic modulus was computed from the shear wave propagation speed. This method was used to obtain measures before and immediately after 4 weeks of treatment. All ultrasonic measurements were performed by a physician who had over 10 years of experience in musculoskeletal ultrasound.
Data analysis
SPSS ver. 18.0 was used for all data analyses. Data normality was tested using Shapiro-Wilk’s tests; all variables appeared normally distributed. Independent t tests and chi-square tests were used for differential testing. A paired t test was used for comparison of within-group differences. An independent t test was used for comparison of exercise differences between groups. Significance level was set at P=0.05 for all analyses.
The minimum sample size required for the groups was calculated using the function: n1=n2=[2*σ2*(μα+μβ)2]/δ2 where α=0.05, μα=1.96, and β=0.2, μβ=0.84, and statistical efficiency was 80%. By reference to the relevant literature [24], the standard deviation of VAS was set at σ=1.1, δ=5.3*20%=1.06. The required sample size of each group was 16; thus, we aimed to enroll 30 cases in each group for this clinical study.
Results
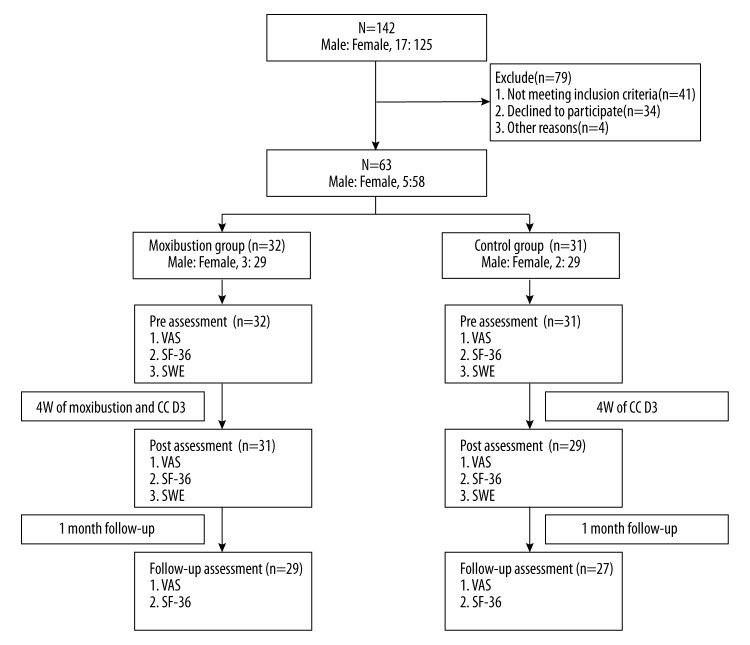
Sixty-three participants with POP low back pain participated in the study. Seven participants dropped out: 3 participants from the moxibustion group and 4 participants from control group (Figure 4).
Figure 4.
Participants flow diagram.
Participants in the moxibustion and control groups were similar in general characteristics and no significant differences were noted between groups (Table 1).
Outcome measures
After treatment for 4 weeks and a follow-up of 1 month, VAS scores were significantly lower in the 2 groups (p<0.05) than at the start of the experiment, and overall, the moxibustion group had lower VAS than in the control group (p<0.05; Table 2).
Using the SF-36 evaluation, after 4 weeks of treatment and 1-month follow-up, 4 dimensions (BP, GH, SF, and MH) in the moxibustion group had significantly improved. In the control group, only the BP dimension improved (p<0.05), and the moxibustion group was better than the control group (p<0.05; Table 3).
The Young’s modulus value of the moxibustion group decreased significantly (p < 0.01) immediately after 4 weeks of treatment and differed significantly from the control group (p<0.01; Table 4).
Table 2.
Changes of the pain intensity changes in VAS scoring from Pretreament to final follow-up.
| Pretreament | Treatment 4 weeks | Post treatment 1 month | |||
|---|---|---|---|---|---|
| VAS | Moxibustion group | 4.97 | 2.77 | 3.10 | T-P: P<0.01 PT-P: P<0.01 PT-T: P>0.05 |
| ±1.31 | ±0.92 | ±1.06 | |||
| Control group | 5.32 | 4.00 | 3.81 | T-P: P<0.01 PT-P: P<0.01 PT-T: P>0.05 |
|
| ±1.49 | ±1.28 | ±1.33 | |||
| P>0.05 | P<0.01 | P<0.05 |
Table 3.
Changes in the 8 items of the norm-based Short-Form-36 scores from Pretreament to final follow-up.
| Pretreament | Treatment 4 weeks | Post treatment 1 month | |||
|---|---|---|---|---|---|
| PF | Moxibustion group | 52.34 | 62.26 | 62.59 | T-P: P>0.05 PT-P: P>0.05 PT-T: P>0.05 |
| ±21.74 | ±19.70 | ±20.69 | |||
| Control group | 54.52 | 61.38 | 64.26 | T-P: P>0.05 PT-P: P>0.05 PT-T: P>0.05 |
|
| ±20.79 | ±22.87 | ±21.29 | |||
| P>0.05 | P>0.05 | P>0.05 | |||
| RP | Moxibustion group | 25.78 | 33.87 | 31.03 | T-P: P>0.05 PT-P: P>0.05 PT-T: P>0.05 |
| ±32.68 | ±36.26 | ±33.84 | |||
| Control group | 25.81 | 25.00 | 30.56 | T-P: P>0.05 PT-P: P>0.05 PT-T: P>0.05 |
|
| ±36.79 | ±36.60 | ±30.49 | |||
| P>0.05 | P>0.05 | P>0.05 | |||
| BP | Moxibustion group | 49.13 | 72.60 | 66.07 | T-P: P<0.01 PT-P: P<0.01 PT-T: P>0.05 |
| ±18.16 | ±15.43 | ±11.97 | |||
| Control group | 50.24 | 62.31 | 59.17 | T-P: P<0.01 PT-P: P<0.05 PT-T: P>0.05 |
|
| ±19.38 | ±14.59 | ±12.83 | |||
| P>0.05 | P<0.05 | P<0.05 | |||
| GH | Moxibustion group | 43.44 | 56.55 | 52.76 | T-P: P<0.01 PT-P: P<0.05 PT-T: P>0.05 |
| ±17.62 | ±16.02 | ±13.34 | |||
| Control group | 41.84 | 46.93 | 45.33 | T-P: P>0.05 PT-P: P>0.05 PT-T: P>0.05 |
|
| ±14.93 | ±15.51 | ±13.94 | |||
| P>0.05 | P<0.05 | P<0.05 | |||
| VT | Moxibustion group | 56.25 | 63.06 | 56.38 | T-P: P>0.05 PT-P: P>0.05 PT-T: P>0.05 |
| ±20.64 | ±15.20 | ±18.02 | |||
| Control group | 52.90 | 55.86 | 57.41 | T-P: P>0.05 PT-P: P>0.05 PT-T: P>0.05 |
|
| ±16.67 | ±17.12 | ±14.10 | |||
| P>0.05 | P>0.05 | P>0.05 | |||
| SF | Moxibustion group | 67.58 | 78.23 | 79.31 | T-P: P<0.05 PT-P: P<0.05 PT-T: P>0.05 |
| ±21.73 | ±16.45 | ±16.80 | |||
| Control group | 66.53 | 67.67 | 68.98. | T-P: P>0.05 PT-P: P>0.05 PT-T: P>0.05 |
|
| ±21.50 | ±21.00 | ±19.11 | |||
| P>0.05 | P<0.05 | P<0.05 | |||
| RE | Moxibustion group | 45.83 | 59.14 | 41.38 | T-P: P>0.05 PT-P: P>0.05 PT-T: P>0.05 |
| ±44.60 | ±40.10 | ±39.50 | |||
| Control group | 47.31 | 54.02 | 39.51 | T-P: P>0.05 PT-P: P>0.05 PT-T: P>0.05 |
|
| ±34.18 | ±38.23 | ±26.21 | |||
| P>0.05 | P>0.05 | P>0.05 | |||
| MH | Moxibustion group | 60.75 | 70.58 | 69.24 | T-P: P<0.05 PT-P: P<0.05 PT-T: P>0.05 |
| ±17.52 | ±17.14 | ±14.62 | |||
| Control group | 59.61 | 57.10 | 55.41 | T-P: P>0.05 PT-P: P>0.05 PT-T: P>0.05 |
|
| ±18.02 | ±20.34 | ±17.32 | |||
| P>0.05 | P<0.01 | P<0.01 |
Table 4.
Changes in the young’s modulus value from pretreament to treatment 4 weeks (kPa).
| Pretreament | Treatment 4 weeks | |||
|---|---|---|---|---|
| Moxibustion group | Left | 16.29 | 10.37 | P<0.01 |
| ±1.68 | ±1.96 | |||
| Right | 16.58 | 9.33 | P<0.01 | |
| ±3.78 | ±1.65 | |||
| Control group | Left | 16.31 | 16.19 | P>0.05 |
| ±3.11 | ±3.03 | |||
| Right | 16.55 | 16.40 | P>0.05 | |
| ±4.15 | ±3.74 | |||
| P>0.05 | P<0.01 |
Values are expressed as mean ± standard deviation. Bold values significance p<0.05.
Discussion
This study shows that thunder-fire moxibustion therapy can significantly reduce back pain in patients with POP, can relieve tension of the multifidus, and can improve quality of life.
Except for vertebral fracture, local muscle fatigue and hypoxia spasm pain [25,26] are the most common causes of low back pain in patients with POP. Our study shows that thunder-fire moxibustion is an effective way to treat this kind of pain.
Moxibustion requires choosing specific acupoints in the body, such as Pishu (BL 20), Shenshu (BL 23), Yaoyangguan (DU 3), and Mingmen (DU 4). Moxibustion therapy warms the body, eliminating cold, regulating energy metabolism, and relieving pain [27]. According to the theory of traditional Chinese medicine, moxibustion is thought to regulate qi and the blood, improving physical fitness to eliminate pathogenesis by means of warming [28].
This study included patients with moderate back pain, having scores of VAS ranging from 3 to 7. The control group (given CC D3 only) had decreased pain levels at the 1-month post-treatment follow-up relative to before treatment, a result consistent with that of Castelo-Branco [29]. CC D3 treatment works to relieve back pain by increasing calcium intake, regulating bone absorption, and improving bone metabolism. The moxibustion group also had significantly reduced VAS at the 1-month follow-up after treatment. In addition, the moxibustion group VAS was significantly less than in the control group; the effect of thunder-fire moxibustion on POP low back pain is rapid and targeted.
A recent meta-analysis shows that neither calcium nor calcium combined with vitamin D can reduce the incidence of fracture in patients over 50 years of age; even large supplements of vitamin D allow an increase in the risk of fracture [30]. Thus, relieving pain symptoms and improving quality of life are key to clinical treatment.
We administered the SF-36 (Short-Form-36) to assess health-related quality of life [31]. At the end of 4 weeks of treatment and 1-month post-treatment follow-up, the moxibustion group showed significantly improved quality of life in the BP, GH, SF, and MH dimensions compared to before treatment. The control group, in contrast, improved only in the BP dimension relative to before treatment, and remained significantly lower than the moxibustion group at follow-up. Four weeks of physical activity and strengthening exercises in patients with osteoporosis can also reduce VAS pain scores and improve the SF-36 in all 8 dimensions [32]. Hongo [33] showed that using bisphosphonate treatment, VAS, and SF-36 did not improve in osteoporosis patients with vertebral fractures. This suggests that pain relief for POP patients is a precondition to improving quality of life. Another study using the SF-36 scale to evaluate thermal moxibustion combined with CC D3 for treating POP patients also found that VAS and quality of life were significantly improved with moxibustion [34]. To the best of our knowledge, the present study is the first to demonstrate an improvement in SF-36 with thunder-fire moxibustion treatment.
Du-moxibustion is a method used to treat disease using herb-partitioned moxibustion in the Dazhui to Yaoshu region of the governor meridian [35]. In this method, ginger is applied to the spine, then the herbal powder spread, followed by spreading ginger paste. Finally, a long moxa cone is placed on the ginger paste; the head and tail are lit and left to burn naturally. The treatment is complicated and not easy to master for general treatment staff; it is also easy to produce scalds, and the moxibustion smog created is very heavy, making this of limited clinical use.
Compared to thermal therapy, thunder-fire moxibustion is based on the traditional Chinese medicine meridian theory, using drugs’ energy produced by burning, thermal infrared radiation force produced by burning and medicine chemical factor, physics factor through meridian and acupoints feeling in achieving WenTong meridian, and adjusting human body’s enginery to treat disease [36]. Thunder-fire moxibustion affects local lumbago, acupoint selection covers Pishu (BL 20), Shenshu (BL 23), Yaoyangguan (DU 3), and Mingmen (DU 4). The function of high temperature and high permeability play an important role in adjusting temperature and eliminating cold to stop pain, and can significantly reduce the pain of POP, thus improving scores of BP, GH, SF, and MH.
In this study, thunder-fire moxibustion treatment technology was used without the effect of muscle-strength training; therefore, improvement of patients’ kinetism or activity in daily living was limited. There was no improvement in the 3 dimensions (PF, RP, and VT) that correspond to the impact of exercise on quality of life with osteoporosis [37]. Administering proper exercise training along with thunder-fire moxibustion treatment could allow us to improve muscle strength, increase balance and coordination function, and ultimately improve quality of life, especially through core muscle training.
While the BP dimension of the control group significantly improved after 4 weeks of treatment, it was significantly lower than in the moxibustion group, and the other 7 dimensions of the SF-36 did not improve significantly in the control group. Regular supplementary calcium can thus improve pain perception of POP patients to a certain extent, but its efficacy is far less than that of thunder-fire moxibustion therapy, and it does not appear to have a positive effect on other dimensions of life quality (SF-36).
Young’s modulus evaluation of the multifidus has been used in many clinical studies. Moreau [38] found that for asymptomatic subjects tested in the resting position of the multifidus, Young’s modulus value is 6.8±1.2 kPa, while in the passive stretching position Young’s modulus value is 22.7±3.8 kPa. Masaki [39] found the value of Young’s modulus was 4.8±0.8 kPa in asymptomatic medical workers. However, no report on short-term clinical observation exists. The present study measured changes in the L4 plane of the multifidus tension before and after 4 weeks of treatment. In the moxibustion group, pre-treatment values were 16.29±1.68 kPa and 16.58±3.78 kPa for the left and right sides, respectively, with no difference between sides.
After treatment, Young’s modulus values were 10.37±1.96 kPa and 9.33±1.65 kPa for the left and right sides, respectively, and again sides did not differ; however, there was a significant decrease in Young’s modulus after treatment. In contrast, no significant difference was found for the control group before and after treatment. Thus, the hyperthermia of the thunder-fire moxibustion treatment, relieving muscle fatigue, and eliminating the local inflammation, ultimately reduces multifidus tension. Young’s modulus value is susceptible to the influence of fatty spaces, but the BMI of patients in this study did not significantly differ between treatment groups (moxibustion group: 22.00±3.02; control group: 22.31±2.56. At vertebral level L4–L5, the ICC of reproducibility of the multifidus measurements was 0.72, as a tool for long-term follow-up of low back pain [38]. The present study suggests that Young’s modulus can be used as an objective evaluation method of muscle tone before and after treatment of POP low back pain; but knowing whether it can be used as an indicator for long-term evaluation of clinical pain symptoms of POP requires a large sample clinical observation trial over an extended time.
This study does have limitations; the clinical treatment time was relatively short and BMD was not monitored. Clinical studies of the effects of moxibustion in the treatment of low back pain in POP from mainland China lack evidence-based medicine. Since moxibustion treatment produces some amount of smog and the risk of potential scalding, we have made efforts to improve the moxibustion box and smog control, and it is important to prevent smog and the risk of potential scalding in the treatment of thunder-fire moxibustion.
Conclusions
The findings of this study indicate that thunder-fire moxibustion is an effective method to treat POP lower back pain and is worthy of promotion and further application.
Footnotes
Conflict of interests
None.
Source of support: Nanjing Science and Technology Commission (201611008); Jiangsu Provincial Health and Family Planning Commission Cadre Health Bureau (BJ16019); Provincial Chinese Medicine Rehabilitation Demonstration (Jiangsu) Center Construction Project (K2017ykf18)
References
- 1.Consensus development conference: Diagnosis, prophylaxis, and treatment of osteoporosis. Am J Med. 1993;94(6):646–50. doi: 10.1016/0002-9343(93)90218-e. [DOI] [PubMed] [Google Scholar]
- 2.Wright NC, Looker AC, Saag KG, et al. The recent prevalence of osteoporosis and low bone mass in the united states based on bone mineral density at the femoral neck or lumbar spine. J Bone Miner Res. 2014;29(11):2520–26. doi: 10.1002/jbmr.2269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.National Bureau of Statistics of the People’s Republic of China. National bureau of statistics of China 2015. Beijing: China Statistics Press; 2015. [Google Scholar]
- 4.Editorial Board of Osteoporosis Prevention and Treatment (China White Paper), China Health Promotion Foundation. [White paper on osteoporosis]. Chinese Journal of Health Management. 2009;3(3):48–154. [in Chinese] [Google Scholar]
- 5.Liu ZH, Ma SS, Wang SL, et al. The theory of osteoporosis. Beijing: Beijing Science Press; 1998. [Google Scholar]
- 6.Li CX, Tang YJ, Hang FY, et al. [The effect of progressive lumbar dorsal muscle function exercise on the improvement of bone density and low back pain in patients with osteoporosis]. Chinese Journal of Gerontology. 2013;33(15):3623–24. [in Chinese] [Google Scholar]
- 7.Cosman F, de Beur SJ, Leboff MS, et al. The clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int. 2014;25(10):2359–81. doi: 10.1007/s00198-014-2794-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Camacho PM, Petak SM, Binkley N, et al. American Association of Clinical Endocrinologists and American College of Endocrinology clinical practice guidelines for the diagnosis and treatment of postmenopausal osteoporosis-2016 – executive summary. Endocr Pract. 2016;22(9):1111–18. doi: 10.4158/EP161435.ESGL. [DOI] [PubMed] [Google Scholar]
- 9.Chesnut CH, 3rd, Silverman S, Andriano K, et al. A randomized trial of nasal spray salmon calcitonin in postmenopausal women with established osteoporosis: The prevent recurrence of osteoporotic fractures study. PROOF Study Group. Am J Med. 2000;109(4):267–76. doi: 10.1016/s0002-9343(00)00490-3. [DOI] [PubMed] [Google Scholar]
- 10.Chesnut CH, 3rd, Azria M, Silverman S, et al. Salmon calcitonin: A review of current and future therapeutic indications. Osteoporos Int. 2008;19(4):479–91. doi: 10.1007/s00198-007-0490-1. [DOI] [PubMed] [Google Scholar]
- 11.Karachalios T, Lyritis GP, Kaloudis J, et al. The effects of calcitonin on acute bone loss after pertrochanteric fractures. A prospective, randomized trial. J Bone Joint Surg Br. 2004;86(3):350–58. doi: 10.1302/0301-620x.86b3.14300. [DOI] [PubMed] [Google Scholar]
- 12.Lyritis GP, Ioannidis GV, Karachalios T, et al. Analgesic effect of salmon calcitonin suppositories in patients with acute pain due to recent osteoporotic vertebral crush fractures: A prospective double-blind, randomized, placebo-controlled clinical study. Clin J Pain. 1999;15(4):284–89. doi: 10.1097/00002508-199912000-00004. [DOI] [PubMed] [Google Scholar]
- 13.Knopp JA, Diner BM, Blitz M, et al. Calcitonin for treating acute pain of osteoporotic vertebral compression fractures: A systematic review of randomized, controlled trials. Osteoporos Int. 2005;16(10):1281–90. doi: 10.1007/s00198-004-1798-8. [DOI] [PubMed] [Google Scholar]
- 14.Zhu HM, Liao EY. [The symposium on salmon calcitonin]. Chinese Journal of Osteoporosis and Bone Mineral Research. 2013;6(4):370–72. [in Chinese] [Google Scholar]
- 15.Dong CX, Xu YL. [Clinical comparative observation of the effect of paving moxibustion on low back pain of primary osteoporosis with kidney yang deficiency]. Journal of Sichuan of Traditional Chinese Medicine. 2013;31(3):121–23. [in Chinese] [Google Scholar]
- 16.Yang K, Cai SC, Zhu CF, et al. [Clinical study on primary osteoporosis treated with spreading moxibustion for warming yang and activating blood circulation]. Zhongguo Zhen Jiu. 2014;34(6):555–58. [in Chinese] [PubMed] [Google Scholar]
- 17.Lin HB, Li AQ, Liu CM, et al. [Clinical research of governor vessel moxibustion on treating the low back Pain in postmenopausal osteoporosis of spleen-kidney-yang deficiency]. Clinical Journal of Chinese Medicine. 2013;(13):49–51. [in Chinese] [Google Scholar]
- 18.Xu F, Huang M, Jin Y, et al. Moxibustion treatment for primary osteoporosis: A systematic review of randomized controlled trials. Plos One. 2017;12(6):e0178688. doi: 10.1371/journal.pone.0178688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liu SZ, Wang Y, Chen P. [Clinical application of thunder fire moxibustion]. Journal of Practical Traditional Chinese Medicine. 2015;31(4):362–65. [in Chinese] [Google Scholar]
- 20.Li Y, Xu LF, Liu LY. Evaluation mechanism and efficacy for pain syndrome with Zhao’s Thunder-Fire Moxibustion treatment. Jilin Journal of Traditional Chinese Medicine. 2016;36(6):619–22. [in Chinese] [Google Scholar]
- 21.National medical technology cooperation group of the State Administration of traditional Chinese Medicine. Medical technical manual of traditional Chinese Medicine (2013 popular edition) Beijing: China Medical Science Press; 2013. p. 172. [Google Scholar]
- 22.Zhang HY, Xu DM, Xue L, et al. Clinical study of thunder fire moxibustion combined celecoxib for treatment of knee osteoarthritic. Journal of Nanjing University of Traditional Chinese Medicine. 2017;33(6):574–78. [in Chinese] [Google Scholar]
- 23.Ware JE. SF-36 Health survey: Manual and interpretation guide. 2005. p. 30. [Google Scholar]
- 24.Jiang JL, Liang Q, Yang HL, et al. Clinical efficacy of pulsed electromagnetic fields in the treatment of postmenopausal osteoporosis. Chinese Journal of Rehabilitation Medicine. 2017;32(02):192–94. [Google Scholar]
- 25.Hongo M, Miyakoshi N, Kasukawa Y, et al. Additive effect of elcatonin to risedronate for chronic back pain and quality of life in postmenopausal women with osteoporosis: A randomized controlled trial. J Bone Miner Metab. 2015;33(4):432–39. doi: 10.1007/s00774-014-0603-9. [DOI] [PubMed] [Google Scholar]
- 26.Ohtori S, Akazawa T, Murata Y, et al. Risedronate decreases bone resorption and improves low back pain in postmenopausal osteoporosis patients without vertebral fractures. J Clin Neurosci. 2010;17(2):209–13. doi: 10.1016/j.jocn.2009.06.013. [DOI] [PubMed] [Google Scholar]
- 27.Run MY. The origin and development of Chinese acupuncture and moxibustion. Anc Sci Life. 1985;4(4):224–28. [PMC free article] [PubMed] [Google Scholar]
- 28.Sun YJ, Yuan JM, Yang ZM. Effectiveness and safety of moxibustion for primary insomnia: A systematic review and meta-analysis. BMC Complement Altern Med. 2016;16:217. doi: 10.1186/s12906-016-1179-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Castelo-Branco C, Dávila J, Alvarez L, et al. Comparison of the effects of calcium carbonate and ossein-hydroxyapatite complex on back and knee pain and quality of life in osteopenic perimenopausal women. Maturitas. 2015;81(1):76–82. doi: 10.1016/j.maturitas.2015.02.265. [DOI] [PubMed] [Google Scholar]
- 30.Zhao JG, Zeng XT, Wang J, et al. Association between calcium or Vitamin D supplementation and fracture incidence in community-dwelling older adults a systematic review and meta-analysis. JAMA. 2017;318(24):2466–82. doi: 10.1001/jama.2017.19344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Brazier JE, Harper R, Jones NM, et al. Validating the SF-36 health survey questionnaire: New outcome measure for primary care. BMJ. 1992;305(6846):160–64. doi: 10.1136/bmj.305.6846.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cesarec G, Martinec S, Basic I, et al. Effect of exercises on quality of life in women with osteoporosis and osteopenia. Coll Antropol. 2014;38(1):247–54. [PubMed] [Google Scholar]
- 33.Hongo M, Miyakoshi N, Kasukawa Y, et al. Additive effect of elcatonin to risedronate for chronic back pain and quality of life in postmenopausal women with osteoporosis: A randomized controlled trial. J Bone Miner Metab. 2015;33(4):432–39. doi: 10.1007/s00774-014-0603-9. [DOI] [PubMed] [Google Scholar]
- 34.Ouyang JJ, Liang DB, Pang XH. [Effects of heat-sensitive moxibustion therapy on secretion of osteoprotegerin and quality of life in patients with primary osteoporosis]. Chinese Journal of Basic Medicine In Traditional Chinese Medicine. 2013;(7):812–13. [Google Scholar]
- 35.Ma MQ, Zhang XW. [Clinical treatment of du moxibustion and the composition of “du moxibustion powder”]. Journal of Clinical Acupuncture and Moxibustion. 2016;32(2):80–82. [Google Scholar]
- 36.Liao QJ, Zhang Y. [The clinical application of Zhao’s thunder-fire moxibustion]. Journal of Practical Traditional Chinese Medicine. 2014;30(6):575–76. [Google Scholar]
- 37.Li WC, Chen YC, Yang RS, et al. Effects of exercise programmers on quality of life in osteoporotic and osteopenic postmenopausal women: A systematic review and meta-analysis. Clin Rehabil. 2009;23(10):888–96. doi: 10.1177/0269215509339002. [DOI] [PubMed] [Google Scholar]
- 38.Moreau B, Vergari C, Gad H, et al. Non-invasive assessment of human multifidus muscle stiffness using ultrasound shear wave elastrography: A feasibility study. Proc Inst Mech Eng H. 2016;230(8):809–14. doi: 10.1177/0954411916656022. [DOI] [PubMed] [Google Scholar]
- 39.Masaki M, Aoyama T, Murakami T, et al. Association of low back pain with muscle stiffness and muscle mass of the lumbar back muscles, and sagittal spinal alignment in young and middle-aged medical workers. Clin Biomech (Bristol, Avon) 2017;49:128–33. doi: 10.1016/j.clinbiomech.2017.09.008. [DOI] [PubMed] [Google Scholar]