Abstract
Using a large sample of college students, objectives were to examine (1) the overlap between poor sleep and suicide risk status, (2) whether poor sleep was associated with suicide behaviors above and beyond depression, (3) whether sleep problems and depression interacted to predict increased suicidal behaviors or risk, and (4) which specific components of sleep were uniquely associated with suicidal behaviors. Participants were 1,700 college students (ages 18–29 years; 65% female) from two universities who completed measures assessing sleep, depressive symptoms, and suicidal behaviors (Suicidal Behaviors Questionnaire–Revised [SBQ-R], a composite measure including ideation, past attempt, disclosure to others, and future likelihood of suicide that includes a cutoff for determining participants with suicide risk). Approximately one-quarter (24%) of participants were classified with suicide risk. Four-fifths (82.7%) of participants classified with suicide risk also met cutoff criteria for sleep problems; conversely, almost one-third (31.3%) of the participants classified with sleep problems were also classified with suicide risk. Total sleep problems remained significantly associated with suicidal behaviors above and beyond depressive symptoms, though sleep and depression did not interact to predict suicidal behaviors or risk. When considered together and controlling for sex, the odds of being classified with suicide risk were 6.54 times greater for participants with elevated depressive symptoms and 2.70 times greater for participants with sleep problems. Analyses examining specific sleep domains found shorter sleep duration, having bad dreams, feeling too cold while sleeping, and sleep medication use to each be independently associated with suicidal behaviors. Findings add to a growing body of literature linking sleep and suicide in college students.
Keywords: daytime sleepiness, depression, insomnia, nightmares, SBQ-R, sleep, suicide
1. Introduction
Evidence from cross-sectional, longitudinal, case control, and psychological autopsy studies support a link between sleep problems and suicidal behaviors (Bernert et al., 2015, Pigeon et al., 2012, Woznica et al., 2015). However, even though sleep problems are common in college students (Lund et al., 2010, Orzech et al., 2011) and suicide is a leading cause of death in young adults (Centers for Disease Control and Prevention, 2015, Schwartz, 2006), few studies have examined sleep in relation to suicidal behaviors in college student samples. In fact, a systematic review published in 2015 (Bernert et al., 2015) found only three studies examining sleep and suicide risk in college students (Cukrowicz et al., 2006, Nadorff et al., 2011, 2013), with four additional studies published after the systematic review was conducted (Bernert et al., 2017, Bozzay et al., 2016, Nadorff et al., 2014, Supartini et al., 2016) and one additional study not included in the systematic review (Vail-Smith et al., 2009). As described next, these studies have made important contributions to our understanding of sleep in relation to suicidal behaviors in college students, yet also point to the need for additional research in this area.
Five of the studies to date examined insomnia symptoms (Bozzay et al., 2016) or both insomnia symptoms and nightmares in relation to suicide ideation/behaviors (Cukrowicz et al., 2006, Nadorff et al., 2014, Nadorff et al., 2011, 2013). In a sample of 438 female college students from a single university, Bozzay and colleagues (2016) found insomnia symptoms were significantly associated with suicidal ideation after controlling for depression. In a sample of 222 college students, Cukrowicz and colleagues (2006) found nightmares, but not insomnia symptoms, to be significantly associated with suicidal ideation when depressive symptoms were controlled. This differential finding was replicated by Nadorff et al. (2011) in a larger study of 583 students. However, in a separate sample of 673 college students, Nadorff and colleagues (2013) found both insomnia symptoms and nightmare duration to be independently associated with suicide behaviors, above and beyond internalizing symptoms. A third study by Nadorff and colleagues reported mixed evidence for whether nightmares alone or both insomnia symptoms and nightmares were associated with increased suicide risk/attempts in two samples of college students (Ns = 747 and 604) (Nadorff et al., 2014). Studies to date have largely focused on whether sleep problems are independently associated with suicidal behaviors, with most studies examining whether sleep problems are incrementally associated with suicidal behaviors above and beyond depression Extant studies in non-college student samples have not found support for this sleep interacting with depression in predicting suicidal behaviors (Ferentinos et al., 2016, Gelaye et al., 2016), though we are not aware of any studies that have tested this possibility in college students. Considered together, the handful of existing studies have laid the groundwork for examining sleep and suicide in college students, yet these studies were unable to examine other sleep domains outside of insomnia symptoms and nightmares that may also be associated with suicidal behaviors. This is consistent with the broader literature examining the link between sleep and suicide, which has primarily focused on insomnia symptoms (broadly defined) and nightmares (McCall and Black, 2013, Woznica et al., 2015). Even among these studies, “few studies [have] attempted to identify associations between specific insomnia symptoms and suicide risk” (Woznica et al., 2015, p. 41), making this a clear research priority.
Two studies have examined sleep in relation to suicidal ideation among college students beyond insomnia symptoms and nightmares. One study of 859 college students found that students who reported suicidal ideation reported significantly worse overall sleep quality than students who did not report suicidal ideation (Vail-Smith et al., 2009). More recently, Supartini et al. (2016) used the Pittsburgh Sleep Quality Index (PSQI) (Buysse et al., 1989) in a sample of 1,992 Japanese college students and found that students with suicidal ideation were more likely to be classified with poor sleep than students without suicidal ideation. Poor overall sleep quality remained associated with suicidal ideation when accounting for depressive symptoms and other covariates (e.g., age, sex). Although important, this study did not examine specific sleep domains on the PSQI (e.g., sleep duration, sleep quality) and used a single yes/no item to assess suicidal ideation. Our study aims to build on these findings by using the PSQI in a sample of United States college students.
The present study adds to the limited empirical evidence examining the link between sleep and suicide risk in college students. Using validated measures of both sleep and suicidal behaviors in a large sample of college students, we examined (1) the proportion of students meeting cutoff criteria for suicide risk who also met cutoff criteria for poor sleep, (2) whether poor sleep was associated with suicide behaviors above and beyond depression (with all variables examined both continuously and categorically), and (3) whether the association between sleep problems and suicidal behaviors was moderated by depression. We hypothesized that the majority of students meeting the cutoff for suicide risk would also be classified with poor sleep and that poor sleep would remain associated with suicidal behaviors/risk after controlling for depression, though we did not expect sleep and depression to interact in predicting suicidal behaviors/risk. Finally, since most studies have examined insomnia specifically as opposed to more specific sleep domains, we explored (4) whether specific aspects of sleep and/or daytime sleepiness were uniquely associated with suicidal behaviors.
2. Material and methods
2.1. Participants
Participants were 1,700 college students enrolled in two public universities in the Midwestern United States.1 Participants ranged in age from 18 to 29 years (M = 18.97, SD = 1.26). As summarized in Table 1, the majority of participants self-identified as female (65%), White (82%), and non-Hispanic (96%). Most participants (63%) were in their first year of college.
Table 1.
Demographic Characteristics of Study Participants
| Variable | % (N) |
|---|---|
| Sexa | |
| Male | 35.2% (597) |
| Female | 64.5% (1,095) |
| Other | 0.4% (6) |
| Year of Study | |
| Freshman | 63.5% (1,080) |
| Sophomore | 23.6% (401) |
| Junior | 8.7% (148) |
| Senior | 3.9% (67) |
| Other | 0.2% (4) |
| Racea | |
| White | 81.8% (1,386) |
| Asian | 7.7% (131) |
| Black | 6.0% (101) |
| Native American | 0.4% (6) |
| Native Hawaiian/Pacific Islander | 0.1% (2) |
| Biracial/Multiracial | 4.0% (68) |
| Ethnicitya | |
| Non-Hispanic | 95.6% (1,625) |
| Hispanic | 4.3% (73) |
| Family Income in USDa | |
| Up to $39,999 | 5.9% (101) |
| $40,000 – $79,999 | 12.1% (205) |
| $80,000 – $119,999 | 19.2% (326) |
| $120,000 – $159,999 | 14.1% (239) |
| $160,000 or greater | 27.5% (467) |
| Don’t know | 21.2% (361) |
Note. N = 1,700. USD = U.S. dollar.
Two participants did not complete the sex question, 6 did not complete the race question, 2 did not complete the ethnicity question, and 1 did not complete the family income question.
2.2. Procedures
This study was approved by the local Institutional Review Board (IRB) at each institution and was conducted in accordance with the ethical standards of the 1964 Declaration of Helsinki and its later amendments. Participants at each institution were provided with information regarding the study and informed that participation was optional. Participants then completed the survey in Qualtrics anonymously and received course credit for participation. All participants received the contact information of the local investigator, IRB, and student counseling center.
2.3. Measures
2.3.1. Sleep
The Pittsburgh Sleep Quality Index (PSQI) (Buysse et al., 1989) was used to assess sleep. The PSQI has 9 items (including one multi-part item with 10 subitems) that assess seven well-validated components of sleep: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbance, use of sleep medication, and daytime dysfunction. Scoring for all components is based on a four-point scale with higher scores reflecting poorer sleep over the past month. Four items (e.g., assessing sleep duration; sleep latency) are open-ended responses that, based on participants’ answers, are converted to the four-point scale. A global PSQI score is also calculated, with scores >5 used to classify participants as “poor sleepers” (i.e., clinically significant sleep problems) and scores =5 used to classify participants as “good sleepers” (Buysse et al., 1989). The PSQI is internally consistent (Buysse et al., 1989, Carpenter and Andrykowski, 1998), is reliable across four weeks (Lund et al., 2010), correlates with other measures of sleep disturbance and daily diaries of sleep activity (Carpenter and Andrykowski, 1998), and has been frequently used with college students (Lund et al., 2010, Orzech et al., 2011). The PSQI total score is strongly correlated with scores on the Insomnia Severity Index (ISI) in college students (r = 0.63) (Dietch et al., 2016). In the present study, α = 0.69. In addition, for analyses examining specific sleep domains, we only used the “trouble staying awake” item of the daytime dysfunction component since the other daytime dysfunction item assesses energy and likely overlaps significantly with depressive symptoms; the individual items of the night disturbance component (e.g., bad dreams, night/early morning wakings) were also entered individually to evaluate whether specific nighttime disturbances were uniquely associated with suicidal behaviors.
2.3.2. Depression
Depressive symptoms were assessed using the depression subscale of the Depression Anxiety Stress Scales-21 (DASS-21) (Antony et al., 1998, Lovibond and Lovibond, 1995a). The depression subscale (e.g., “I felt down-hearted and blue”) consists of seven items, none of which focus on suicide or sleep problems. Each item is rated using a four-point scale (0 = did not apply to me at all, 3 = applied to me very much or most of the time) in reference to the past week. In the present study, α=.90. Scores on the DASS-21 can be multiplied by two to calculate a total score with cutoff recommendations (Lovibond and Lovibond, 1995b). In the present sample, 162 participants (9.5%) were classified with severe depressive symptoms (total score ≥ 21) (Lovibond and Lovibond, 1995b).
2.3.3. Suicidal behaviors
The Suicidal Behaviors Questionnaire–Revised (SBQ-R) (Osman et al., 2001) is a four-item self-report measure assessing aspects of suicidal behavior. The SBQ-R is a validated and reliable measure that can be used to identify suicide risk and behaviors (Osman et al., 2001). The four items assess lifetime ideation/attempt, frequency of ideation over the past 12 months, telling someone else about ideation, and likelihood of attempting suicide in the future. Osman et al. (2001) found a cutoff score of 7 to maximize sensitivity and specificity in identifying suicidal college students. In the present study, α=.82.
2.4. Analytic Approach
2.4.1. Survey validity checks
In order to improve the quality of participant responses, we utilized an instructional manipulation check (IMC) (Oppenheimer et al., 2009), “trap questions” (e.g., “If you are paying attention, please click on the response ‘sometimes’”), and a question at the end of the full survey that asked participants the following: “How much effort did you put into this study from 0 to 10 (0 = not much effort at all, 5 = moderate effort, 10 = my best effort)?”. The IMC consists of a set of instructions and a question similar to other survey questions, but the instructions indicate that the respondent should ignore the question and click on a specific answer. Respondents were required to answer the question correctly to proceed with the survey. To ensure the validity of responding, we set a threshold of 50% accuracy or higher for the “trap questions” and a self-reported effort rating of 5 or higher to ensure that participants were putting forth sufficient effort while also not excluding participants who might have responded inaccurately due to attention lapses or impulsive responding (e.g., those with elevated ADHD symptoms). This threshold was met by 1,708 of the 1,812 participants (94%) who completed the survey, and 1,700 of these 1,708 participants (99.5%) completed the items necessary for scoring both the PSQI and the SBQ-R; these 1,700 participants were used in analyses.
2.4.2. Statistical analyses
First, participants were classified as meeting cutoff criteria for sleep problems (total PSQI score >5) or suicide risk (total SBQ-R score ≥7), with a particular interest in how many participants classified with suicide risk were also classified with sleep problems. Second, zero-order Pearson correlation analyses were conducted to examine the correlations among the study variables. An absolute correlation of r < 0.10 is considered trivial, r = 0.10–0.29 is considered a small effect, r = 0.30–0.49 is considered a medium effect, and r ≥ 0.50 is considered a large effect (Cohen et al., 2003). Third, hierarchical regression analyses were conducted to examine the unique effects of total sleep problems in relation to suicide behaviors. A hierarchical multiple regression analysis was used to examine participant sex, depressive symptoms, and PSQI total score in relation to the continuous SBQ-R total score variable, and a hierarchical logistic regression analysis was used to examine sex, depression status, and sleep problem status in relation to the dichotomous suicide risk classification variable. Site was also included as a covariate. Site, sex, and depression were entered at Step 1, and sleep was entered at Step 2. The logistic regression allows for a test of whether participants with and without sleep problems differ in their likelihood of being classified with suicide risk; odds ratio was used as a measure of effect size, with 1.5–3.49 considered a small effect, 3.5–8.9 a medium effect, and ≥9.0 a large effect (Cohen et al., 2003). These models were re-run to examine whether sleep problems and depressive symptoms interacted to increase suicidal behaviors and/or suicide risk. Finally, a hierarchical multiple regression analysis was conducted to examine daytime sleepiness and specific sleep domains of the PSQI, above and beyond sex and depressive symptoms, in relation to suicidal behaviors.
3. Results
3.1. Overlap between Sleep Problem and Suicide Risk Status
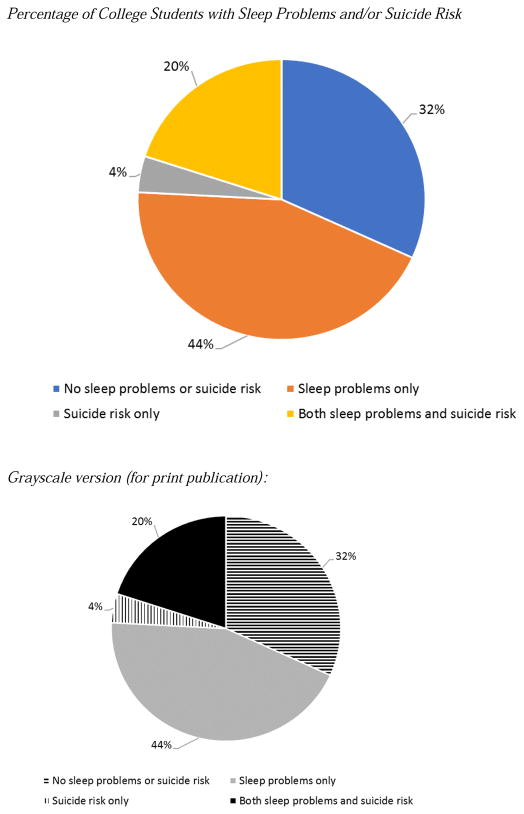
Approximately two-thirds of participants (64%; n = 1,088) were classified with sleep problems (total PSQI score >5), and approximately one-quarter (24%, n = 411) were classified with suicide risk (total SBQ-R score ≥7). The overlap between participants classified with sleep problems and/or suicide risk is shown in Figure 1. Of the 411 participants classified with suicide risk, 82.7% (n = 340) were also classified with sleep problems. Conversely, of the 1,088 participants classified with sleep problems, 31.3% were also classified with suicide risk.
Figure 1.
3.2. Correlation Analyses
Table 2 provides the intercorrelations and descriptive statistics of the study variables (see Table S2 for correlations of the specific sleep disturbance items in relation to the depression and suicide variables). All seven sleep domains were significantly correlated with suicidal behaviors, defined continuously or categorically (all ps < .001; see Table 2). Most correlations were of small effect size. Depressive symptoms were strongly correlated with suicidal behaviors. To facilitate comparisons with future research using the PSQI, Table S3 provides the descriptive statistics of the sleep variables separately for participants with and without suicide risk classification.
Table 2.
Intercorrelations and Descriptive Statistics of Study Variables
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Sex | -- | .01 | .02 | .01 | .08** | .09** | .04 | .07** | .07** | .05* | −.01 | .01 | .05* | .06* |
| 2. Sleep quality | -- | .41*** | .42*** | .21*** | .32*** | .18*** | .28*** | .69*** | .50*** | .32*** | .21*** | .24*** | .21*** | |
| 3. Sleep latency | -- | .22*** | .22*** | .33*** | .22*** | .11*** | .67*** | .56*** | .21*** | .14*** | .18*** | .15*** | ||
| 4. Shorter sleep duration | -- | .37*** | .10*** | .04 | .21*** | .60*** | .45*** | .21*** | .17*** | .17*** | .16*** | |||
| 5. Sleep efficiency | -- | .17*** | .12*** | .06** | .54*** | .37*** | .15*** | .12*** | .08*** | .09*** | ||||
| 6. Sleep disturbancea | -- | .24*** | .22*** | .54*** | .41*** | .28*** | .15*** | .23*** | .20*** | |||||
| 7. Sleep medication | -- | .11*** | .48*** | .31*** | .11*** | .04 | .12*** | .09*** | ||||||
| 8. Daytime sleepinessb | -- | .41*** | .29*** | .28*** | .17*** | .21*** | .19*** | |||||||
| 9. Total sleep problems | -- | .75*** | .42*** | .28*** | .33*** | .29*** | ||||||||
| 10. Sleep status | -- | .30*** | .19*** | .24*** | .22*** | |||||||||
| 11. Depressive symptoms | -- | .75*** | .55*** | .44*** | ||||||||||
| 12. Depression status | -- | .42*** | .32*** | |||||||||||
| 13. SBQ-R total score | -- | .84*** | ||||||||||||
| 14. Suicide risk status | -- | |||||||||||||
|
| ||||||||||||||
| Mean | -- | 1.20 | 1.43 | 0.94 | 0.54 | 1.28 | 0.44 | 1.14 | 6.95 | -- | 0.57 | -- | 5.17 | -- |
| SD | -- | 0.65 | 0.98 | 0.86 | 0.79 | 0.56 | 0.85 | 0.78 | 3.20 | -- | 0.62 | -- | 2.81 | -- |
Note. N = 1,700. For sex, 0 = male, 1 = female (n = 1,692 for these correlations). For depression status, 0 = not severe depression score on Depression Anxiety Stress Scale (DASS), 1 = severe depression score on DASS. For sleep status, 0 = good sleep, 1 = poor sleep. For suicide risk, 0 = not at risk, 1 = at risk. SBQ-R = Suicidal Behavior Questionnaire-Revised.
For intercorrelations of the individual PSQI Sleep Disturbance items with the depression and suicide variables, see Table S2
The daytime sleepiness variable is the single “how often had you had trouble staying awake while driving, eating meals, or engaged in social activity?” PSQI item.
p < .05.
p < .01.
p < .001.
3.3. Regression Analyses with Total Sleep
Results of the hierarchical multiple regression analysis of total sleep in relation to suicidal behaviors are summarized in Table 3. As expected, depressive symptoms were strongly associated with suicidal behaviors (Step 1). Total sleep problems were significantly associated with increased suicidal behaviors above and beyond sex and depression (Step 2), though the amount of additional variance explained was small (1%). The sleep × depression interaction term added to the model was nonsignificant (p > .05).
Table 3.
Hierarchical Regression Analysis Examining Total Sleep Problems in Relation to Suicidal Behaviors in College Students
| Step 1
|
|||||
|---|---|---|---|---|---|
| B | SE | β | t | p | |
|
| |||||
| F(4,1695) = 190.67***, R2 = .31 | |||||
| Sex (Male = 0, Female = 1) | .31 | .12 | .05 | 2.58 | .009 |
| Sex (Male = 0, Other = 1) | 1.65 | .96 | .04 | 1.72 | .09 |
| Depressive Symptoms | 2.47 | .09 | .54 | 26.75 | <.0001 |
| Step 2
|
|||||
| B | SE | β | t | p | |
|
|
|||||
| F(1,1694) = 26.23***, R2 = .32, ΔR2 = .01 | |||||
| Sex (Male = 0, Female = 1) | .26 | .12 | .04 | 2.17 | .03 |
| Sex (Male = 0, Other = 1) | 1.509 | .95 | .03 | 1.57 | .12 |
| Depressive Symptoms | 2.26 | .10 | .49 | 22.33 | <.001 |
| Total Sleep Problems | .10 | .02 | .11 | 5.13 | <.001 |
Note. Site was also included as a dichotomous covariate.
p < .001.
Results of the hierarchical logistic regression analysis examining depression status and sleep problem status in relation to suicide risk status are summarized in Table 4. As shown, female sex, depression status, and sleep problem status were each uniquely associated with a higher likelihood of suicide risk status in Block 2. Specifically, the odds of being classified with suicide risk were 6.54 times greater for participants with depression (medium effect size) and 2.70 times greater for participants with sleep problems (small effect size). The sleep status × depression status interaction term added to the model was nonsignificant (p > .05).
Table 4.
Hierarchical Logistic Regression Analysis Examining Depression and Sleep Problem Status in Relation to Suicide Risk Status in College Students
| Block 1
|
|||||
|---|---|---|---|---|---|
| B | SE | Wald | p | OR (95% CI) | |
|
| |||||
| χ2(4) = 176.04, p < .001, Nagel. R2 = .15 | |||||
| Sex (Male = 0, Female = 1) | .32 | .13 | 6.03 | .01 | 1.38 (1.06, 1.77) |
| Sex (Male = 0, Other = 1) | 1.73 | .83 | 4.33 | .04 | 5.63 (1.11, 28.69) |
| Depression Status | 2.11 | .18 | 135.64 | <.001 | 8.23 (5.77, 11.73) |
| Block 2
|
|||||
| B | SE | Wald | p | OR (95% CI) | |
|
|
|||||
| χ2(1) = 50.42, p < .001, Nagel. R2 = .19 | |||||
| Sex (Male = 0, Female = 1) | .28 | .13 | 4.46 | .04 | 1.32 (1.02, 1.71) |
| Sex (Male = 0, Other = 1) | 1.38 | .83 | 2.77 | .10 | 3.99 (0.78, 20.35) |
| Depression Status | 1.88 | .18 | 104.28 | <.001 | 6.54 (4.56, 9.37) |
| Sleep Problem Status | .99 | .15 | 45.37 | <.001 | 2.70 (2.02, 3.61) |
Note. Site was also included as a dichotomous covariate. For depression status, 0 = not severe depression score on Depression Anxiety Stress Scale (DASS), 1 = severe depressive symptom score on DASS. For sleep status, 0 = good sleep, 1 = poor sleep. For suicide status, 0 = not at risk, 1 = at risk. Nagel. = Nagelkerke. OR = odds ratio.
p < .001.
3.4. Regression Analysis with Specific Sleep Domains
Results of the hierarchical multiple regression analysis of the specific sleep domains/items in relation to suicidal behaviors are summarized in Table 5. Above and beyond sex and depressive symptoms, shorter sleep duration, having bad dreams, feeling too cold while sleeping, and sleep medication use were each uniquely associated with increased suicidal behaviors (ps < .05).
Table 5.
Hierarchical Regression Analysis Examining Specific Sleep Domains in Relation to Suicidal Behaviors in College Students
| Step 1
|
|||||
|---|---|---|---|---|---|
| B | SE | β | t | p | |
|
| |||||
| F(4,1695) = 190.55***, R2 = .31 | |||||
| Sex (Male = 0, Female = 1) | .31 | .12 | .05 | 2.58 | .009 |
| Sex (Male = 0, Other = 1) | 1.65 | .96 | .04 | 1.72 | .09 |
| Depressive Symptoms | 2.47 | .09 | .54 | 26.75 | <.001 |
| Step 2
|
|||||
| B | SE | β | t | p | |
|
|
|||||
| F(14,1681) = 3.50***, R2 = .33, ΔR2 = .02 | |||||
| Sex (Male = 0, Female = 1) | .21 | .12 | .04 | 1.71 | .09 |
| Sex (Male = 0, Other = 1) | 1.17 | .96 | .03 | 1.23 | .22 |
| Depressive Symptoms | 2.20 | .10 | .48 | 21.08 | <.001 |
| Sleep Quality | .04 | .11 | .01 | 0.40 | .69 |
| Sleep Latency | .06 | .07 | .02 | 0.85 | .40 |
| Shorter Sleep Duration | .18 | .08 | .06 | 2.32 | .02 |
| Sleep Efficiency | −.15 | .08 | −.04 | −1.85 | .07 |
| Sleep Disturbance: Night/early morning waking | .03 | .06 | .01 | 0.52 | .60 |
| Sleep Disturbance: Have to use bathroom | .06 | .06 | .02 | 1.00 | .32 |
| Sleep Disturbance: Cannot breathe comfortably | .05 | .09 | .01 | 0.59 | .56 |
| Sleep Disturbance: Cough or snore loudly | −.12 | .07 | −.04 | −1.70 | .09 |
| Sleep Disturbance: Feel too cold | .15 | .07 | .05 | 2.21 | .03 |
| Sleep Disturbance: Feel too hot | −.02 | .06 | −.01 | −0.28 | .78 |
| Sleep Disturbance: Have bad dreams | .14 | .07 | .05 | 2.04 | .04 |
| Sleep Disturbance: Have pain | .11 | .08 | .03 | 1.34 | .18 |
| Sleep Medication | .14 | .07 | .04 | 2.03 | .04 |
| Daytime Dysfunction: Trouble staying awake | .12 | .08 | .03 | 1.54 | .12 |
Note. All sleep variables are component scores from the Pittsburgh Sleep Quality Index (PSQI), with higher scores indicative of poorer sleep for all variables. Site was also included as a dichotomous covariate (full results available from corresponding author).
p < .001.
4. Discussion
This study makes an important contribution to the limited research examining sleep in relation to suicidal behaviors in college students. Using a large sample of students recruited from two universities, poorer overall sleep functioning was not only associated with increased suicidal behaviors but remained associated with suicidal behaviors when controlling for depression. Furthermore, findings suggest that some specific sleep components – shorter sleep duration, more frequent bad dreams, and feeling too cold while sleeping – are particularly associated with increased suicidal behaviors in college students.
To our knowledge, this is the first study to directly examine the overlap between poor sleep and suicide risk status in college students. We found that the four-fifths of college students who were classified with suicide risk were also classified with poor sleep (conversely, almost one-third of the participants classified with sleep problems were also classified with suicide risk). Furthermore, poor sleep remained significantly associated with increased suicide risk after controlling for sex and depression. Consistent with previous research (Ferentinos et al., 2016, Gelaye et al., 2016), sleep problems and depression were both independently associated with increased suicidal behaviors/suicide risk but did not together interact in predicting suicidal behaviors/risk. It is important to note that the incremental contribution of sleep problems was small after accounting for the very strong association between depression and suicidal behaviors, though even small effects are important to identify and may be clinically meaningful when examining correlates of suicidal behaviors. Furthermore, being classified with poor sleep status was associated with an almost three-fold increased likelihood of being classified with suicide risk, above and beyond sex and depression status. As such, our findings add to a growing body of literature pointing to sleep as an important component to include in screening and intervention efforts to prevent suicidal ideation and attempts on college campuses. For instance, there is preliminary evidence for an online suicide risk screening and intervention for college students (King et al., 2015), but as part of the screening procedures only students who initially screened positive for possible depression were administered the full Patient Health Quetionnaire-9 (PHQ-9) (Spitzer et al., 1999) screening measure that also includes items assessing both poor sleep (“Trouble falling or staying asleep, or sleeping too much”) and daytime dysfunction (“Feeling tired or having little energy”). It may be important to include sleep as part of the initial screening process, in part because of the clear association between sleep and suicide in our sample (as well as other studies), and in part because not all college students with suicidal ideation are also depressed (Cukrowicz et al., 2011). Sleep is modifiable, and some students may be more willing to seek help for sleep problems than for depression or suicidal behaviors specifically (McCall and Black, 2013, Woznica et al., 2015). Further, there is evidence that cognitive behavioral therapy for insomnia (CBT-I) not only improves sleep functioning, but also reduces suicidal ideation among adults with both low or high levels of depression (Manber et al., 2011; see also McCall et al., 2015).
Most previous studies have focused on insomnia and nightmares specifically (Bozzay et al., 2016, Cukrowicz et al., 2006, Nadorff et al., 2014, Nadorff et al., 2011, 2013) whereas we used a broader measure of sleep and also examined specific sleep domains. Our findings replicate previous studies in finding bad dreams to be uniquely associated with suicidal behaviors in college students (Cukrowicz et al., 2006, Nadorff et al., 2014, Nadorff et al., 2011, 2013). We also found shorter sleep duration, sleep medication use, and feeling too cold while sleeping to each be uniquely related to increased suicidal behaviors. Although Supartini and colleagues (2016) did not find sleep duration to be associated with suicidal ideation in college students, it is important to note that a single yes/no suicidal ideation item was used in that study and the sample consisted of Japanese college students. Our study used a well-validated measure of suicidal behaviors and included college students in the United States, and these two methodological differences may be why our findings differed from the Supartini et al. study. Our finding regarding sleep medication use is consistent with prior findings in clinical and non-clinical samples that found use of sleep medications to be associated with increased risk for suicide (see Pae et al., 2011 for a review). Brower and colleagues (2011) demonstrated that in a large national survey of adults, sleep medicine use was a stronger predictor of suicidal ideation and suicide attempts than insomnia and significantly increased the explanatory value of these models. Sleep medication may act as a confounder or mediator of comorbid mental health problems in predicting suicide risk (Brower et al., 2011), particularly in younger adults (Gunnell et al., 2013). The finding that feeling too cold while sleeping was associated with increased suicidal behaviors was unexpected. Sleep deprivation is associated with thermoregulation difficulties, including lower body temperature (Vaara et al., 2009), and hypothalamus/hypothalamic-pituitary-adrenal (HPA) axis dysregulation has been linked to thermoregulation difficulties as well as depression and suicide risk (Bao et al., 2008, Buckley and Schatzberg, 2005, Kirkcaldy et al., 2004). Although interesting to consider these interrelations and mechanisms that may contribute to our finding, replication is clearly needed before conclusions can be drawn. In any event, an important direction for future research will be to determine whether incorporating global sleep problems or more specific sleep functioning domains is optimal in screening/intervention efforts, with a particular need to balance thoroughness and efficiency. This is especially important because although most college students at risk for suicide in our study had sleep problems, the reverse was not true – there were many college students who had sleep problems who did not have elevated suicide risk. One worthwhile approach would be to examine what cutoff on a validated sleep measure would provide excellent sensitivity and specificity in identifying college students at elevated suicide risk, as well as whether considering specific sleep domains increases sensitivity/specificity.
Study findings should be considered in light of several limitations. Perhaps most importantly, the cross-sectional design of our study precludes making causal inferences, though evidence from longitudinal studies indicates that sleep difficulties predict subsequent suicidal ideation rather than the reverse (Ribeiro et al., 2012). Nevertheless, studies in college students specifically are needed, and longitudinal studies will also be well-positioned to examine mechanisms of the association between sleep and suicide in college students. This is especially important since the association between depression and suicidal behaviors/risk was reduced when sleep was added to our models, and recent research suggests that sleep may mediate the association between depression and suicide (Ferentinos et al., 2016). Longitudinal studies with temporally-ordered variables are needed to further test this mediational pathway. In addition, our study only included self-report rating scale measures, which may have contributed to mono-informant biases. It would be informative for future studies to also incorporate objective measures of sleep functioning (e.g., actigraphy). However, the search for biological markers of suicide behaviors remains insufficient to replace self-report (Melhem et al., 2017, Shakeri et al., 2015), and self-reported sleep behavior has been shown to have good concordance with objectively-measured sleep (Wolfson et al., 2003). Further, our methods have ecological validity in that college screening and intervention initiatives are likely to rely on self-report measures given their efficiency and low cost. Still, including objective sleep measures is an important direction for future work, particularly given recent interest in intraindividual variability of sleep as a predictor of functional outcomes (Becker et al., 2017, Bei et al., 2016), and a recent study found actigraphy-measured sleep variability to outperform depression in a short-term longitudinal study of suicidal ideation in college students (Bernert et al., 2017). Finally, although our study included college students from two universities, the sample was disproportionately female and White; future studies would benefit from greater diversity. Despite these limitations, findings from this study indicate that the majority of college students with suicide risk also experience sleep problems, that the association between sleep problems and suicide risk exists above and beyond depression, and certain sleep domains as well as daytime dysfunction are most clearly associated with suicidal behaviors in this population.
Supplementary Material
Footnotes
Although there were some differences between participants at the two universities on our primary variables of interest (see Table S1), all participants were included together in analyses in order to increase generalizability. However, to be conservative, site was included as a covariate in all analyses. In addition, when models were conducted separately for the two sites, primary findings were unchanged and consistent across both sites.
Contributors
Dr. Becker conceived of the study, wrote the first draft of the manuscript, and carried out all statistical analyses. Dr. Becker and Dr. Luebbe facilitated data collection. Ms. Dvorsky, Dr. Holdaway, and Dr. Luebbe provided critical feedback and aided in editing the initial draft. All authors contributed to and approved the final manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Antony MM, Bieling PJ, Cox BJ, Enns MW, Swinson RP. Psychometric properties of the 42-item and 21-item versions of the Depression Anxiety Stress Scales in clinical groups and a community sample. Psychological assessment. 1998;10:176–81. [Google Scholar]
- Bao AM, Meynen G, Swaab DF. The stress system in depression and neurodegeneration: Focus on the human hypothalamus. Brain research reviews. 2008;57:531–53. doi: 10.1016/j.brainresrev.2007.04.005. [DOI] [PubMed] [Google Scholar]
- Becker SP, Sidol CA, Van Dyk TR, Epstein JN, Beebe DW. Intraindividual variability of sleep/wake patterns in relation to child and adolescent functioning: A systematic review. Sleep medicine reviews. 2017;34:94–121. doi: 10.1016/j.smrv.2016.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bei B, Wiley JF, Trinder J, Manber R. Beyond the mean: A systematic review on the correlates of daily intraindividual variability of sleep/wake patterns. Sleep medicine reviews. 2016;28:104–20. doi: 10.1016/j.smrv.2015.06.003. [DOI] [PubMed] [Google Scholar]
- Bernert RA, Hom MA, Iwata NG, Joiner TE. Objectively assessed sleep variability as an acute warning sign of suicidal ideation in a longitudinal evaluation of young adults at high suicide risk. The Journal of clinical psychiatry. 2017;78:e678–e87. doi: 10.4088/JCP.16m11193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernert RA, Kim JS, Iwata NG, Perlis ML. Sleep disturbances as an evidence-based suicide risk factor. Current psychiatry reports. 2015;17:554. doi: 10.1007/s11920-015-0554-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bozzay ML, Karver MS, Verona E. Linking insomnia and suicide ideation in college females: The role of socio-cognitive variables and depressive symptoms in suicide risk. Journal of affective disorders. 2016;199:106–13. doi: 10.1016/j.jad.2016.04.012. [DOI] [PubMed] [Google Scholar]
- Brower KJ, McCammon RJ, Wojnar M, Ilgen MA, Wojnar J, Valenstein M. Prescription sleeping pills, insomnia, and suicidality in the National Comorbidity Survey Replication. The Journal of clinical psychiatry. 2011;72:515–21. doi: 10.4088/JCP.09m05484gry. [DOI] [PubMed] [Google Scholar]
- Buckley TM, Schatzberg AF. On the interactions of the hypothalamic-pituitary-adrenal (HPA) axis and sleep: Normal HPA axis activity and circadian rhythm, exemplary sleep disorders. Journal of Clinical Endocrinology & Metabolism. 2005;90:3106–14. doi: 10.1210/jc.2004-1056. [DOI] [PubMed] [Google Scholar]
- Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry research. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- Carpenter JS, Andrykowski MA. Psychometric evaluation of the Pittsburgh Sleep Quality Index. Journal of psychosomatic research. 1998;45:5–13. doi: 10.1016/s0022-3999(97)00298-5. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Web-baased injury statisics query and reporting system (WISQARS), Leading casues of death reports, 1981–2015. Center for Disease Control and Prevention; 2015. [Google Scholar]
- Cohen J, Cohen P, West SG, Aiken LS. Applied multiple correlation/regression analysis for the behavioral sciences. Mahwah, NJ: Lawrence Erlbaum Associates; 2003. [Google Scholar]
- Cukrowicz KC, Otamendi A, Pinto JV, Bernert RA, Krakow B, Joiner TE. The impact of insomnia and sleep disturbances on depression and suicidality. Dreaming. 2006;16:1–10. [Google Scholar]
- Cukrowicz KC, Schlegel EF, Smith PN, Jacobs MP, Van Orden KA, Paukert AL, et al. Suicide ideation among college students evidencing subclinical depression. Journal of American college health : J of ACH. 2011;59:575–81. doi: 10.1080/07448481.2010.483710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dietch JR, Taylor DJ, Sethi K, Kelly K, Bramoweth AD, Roane BM. Psychometric evaluation of the PSQI in U.S. college students. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine. 2016;12:1121–9. doi: 10.5664/jcsm.6050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferentinos P, Porichi E, Christodoulou C, Dikeos D, Papageorgiou C, Douzenis A. Sleep disturbance as a proximal predictor of suicidal intent in recently hospitalized attempters. Sleep medicine. 2016;19:1–7. doi: 10.1016/j.sleep.2015.10.021. [DOI] [PubMed] [Google Scholar]
- Gelaye B, Okeiga J, Ayantoye I, Berhane HY, Berhane Y, Williams MA. Association of suicidal ideation with poor sleep quality among Ethiopian adults. Sleep & breathing = Schlaf & Atmung. 2016;20:1319–26. doi: 10.1007/s11325-016-1418-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunnell D, Chang SS, Tsai MK, Tsao CK, Wen CP. Sleep and suicide: an analysis of a cohort of 394,000 Taiwanese adults. Social psychiatry and psychiatric epidemiology. 2013;48:1457–65. doi: 10.1007/s00127-013-0675-1. [DOI] [PubMed] [Google Scholar]
- King CA, Eisenberg D, Zheng K, Czyz E, Kramer A, Horwitz A, et al. Online suicide risk screening and intervention with college students: a pilot randomized controlled trial. Journal of consulting and clinical psychology. 2015;83:630–6. doi: 10.1037/a0038805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirkcaldy BD, Eysenck MW, Siefen GR. Psychological and social predictors of suicidal ideation among young adolescents. School Psychol Int. 2004;25:301–16. [Google Scholar]
- Lovibond PF, Lovibond SH. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour research and therapy. 1995a;33:335–43. doi: 10.1016/0005-7967(94)00075-u. [DOI] [PubMed] [Google Scholar]
- Lovibond SH, Lovibond PF. Manual for the Depression Anxiety and Stress Scales. 2. Sydney: Psychology Foundation; 1995b. [Google Scholar]
- Lund HG, Reider BD, Whiting AB, Prichard JR. Sleep patterns and predictors of disturbed sleep in a large population of college students. The Journal of adolescent health : official publication of the Society for Adolescent Medicine. 2010;46:124–32. doi: 10.1016/j.jadohealth.2009.06.016. [DOI] [PubMed] [Google Scholar]
- Manber R, Bernert RA, Suh S, Nowakowski S, Siebern AT, Ong JC. CBT for insomnia in patients with high and low depressive symptom severity: adherence and clinical outcomes. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine. 2011;7:645–52. doi: 10.5664/jcsm.1472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCall WV, Benca RM, Rosenquist PB, Riley MA, Hodges C, Gubosh B, et al. A multi-site randomized clinical trial to reduce suicidal ideation in suicidal adult outpatients with Major Depressive Disorder: Development of a methodology to enhance safety. Clin. 2015;12:189–98. doi: 10.1177/1740774515573958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCall WV, Black CG. The link between suicide and insomnia: theoretical mechanisms. Current psychiatry reports. 2013;15:389. doi: 10.1007/s11920-013-0389-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melhem NM, Munroe S, Marsland A, Gray K, Brent D, Porta G, et al. Blunted HPA axis activity prior to suicide attempt and increased inflammation in attempters. Psychoneuroendocrinology. 2017;77:284–94. doi: 10.1016/j.psyneuen.2017.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nadorff MR, Anestis MD, Nazem S, Claire Harris H, Samuel Winer E. Sleep disorders and the interpersonal-psychological theory of suicide: independent pathways to suicidality? Journal of affective disorders. 2014;152–154:505–12. doi: 10.1016/j.jad.2013.10.011. [DOI] [PubMed] [Google Scholar]
- Nadorff MR, Nazem S, Fiske A. Insomnia symptoms, nightmares, and suicidal ideation in a college student sample. Sleep. 2011;34:93–8. doi: 10.1093/sleep/34.1.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nadorff MR, Nazem S, Fiske A. Insomnia symptoms, nightmares, and suicide risk: duration of sleep disturbance matters. Suicide & life-threatening behavior. 2013;43:139–49. doi: 10.1111/sltb.12003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oppenheimer DM, Meyvis T, Davidenko N. Instructional manipulation checks: Detecting satisficing to increase statistical power. J Exp Soc Psychol. 2009;45:867–72. [Google Scholar]
- Orzech KM, Salafsky DB, Hamilton LA. The state of sleep among college students at a large public university. Journal of American college health : J of ACH. 2011;59:612–9. doi: 10.1080/07448481.2010.520051. [DOI] [PubMed] [Google Scholar]
- Osman A, Bagge CL, Gutierrez PM, Konick LC, Kopper BA, Barrios FX. The Suicidal Behaviors Questionnaire-Revised (SBQ-R): validation with clinical and nonclinical samples. Assessment. 2001;8:443–54. doi: 10.1177/107319110100800409. [DOI] [PubMed] [Google Scholar]
- Pae CU, Koh JS, Lee SJ, Han C, Patkar AA, Masand PS. Association of sedative-hypnotic medications with suicidality. Expert review of neurotherapeutics. 2011;11:345–9. doi: 10.1586/ern.11.9. [DOI] [PubMed] [Google Scholar]
- Pigeon WR, Pinquart M, Conner K. Meta-analysis of sleep disturbance and suicidal thoughts and behaviors. The Journal of clinical psychiatry. 2012;73:e1160–7. doi: 10.4088/JCP.11r07586. [DOI] [PubMed] [Google Scholar]
- Ribeiro JD, Pease JL, Gutierrez PM, Silva C, Bernert RA, Rudd MD, et al. Sleep problems outperform depression and hopelessness as cross-sectional and longitudinal predictors of suicidal ideation and behavior in young adults in the military. Journal of affective disorders. 2012;136:743–50. doi: 10.1016/j.jad.2011.09.049. [DOI] [PubMed] [Google Scholar]
- Schwartz AJ. College student suicide in the United States: 1990–1991 through 2003–2004. Journal of American college health : J of ACH. 2006;54:341–52. doi: 10.3200/JACH.54.6.341-352. [DOI] [PubMed] [Google Scholar]
- Shakeri J, Farnia V, Valinia K, Hashemian AH, Bajoghli H, Holsboer-Trachsler E, et al. The relationship between lifetime suicide attempts, serum lipid levels, and metabolic syndrome in patients with bipolar disorders. International journal of psychiatry in clinical practice. 2015;19:124–31. doi: 10.3109/13651501.2014.988271. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA : the journal of the American Medical Association. 1999;282:1737–44. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- Supartini A, Honda T, Basri NA, Haeuchi Y, Chen S, Ichimiya A, et al. The impact of sleep timing, sleep duration, and sleep quality on depressive symptoms and suicidal ideation amongst Japanese Ffreshmen: The EQUSITE study. Sleep disorders. 2016;2016:8737654. doi: 10.1155/2016/8737654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaara J, Kyrolainen H, Koivu M, Tulppo M, Finni T. The effect of 60-h sleep deprivation on cardiovascular regulation and body temperature. European journal of applied physiology. 2009;105:439–44. doi: 10.1007/s00421-008-0921-5. [DOI] [PubMed] [Google Scholar]
- Vail-Smith K, Felts WM, Becker C. Relationship between sleep quality and health risk behaviors in undergraduate college students. College Student Journal. 2009;43:924–30. [Google Scholar]
- Wolfson AR, Carskadon MA, Acebo C, Seifer R, Fallone G, Labyak SE, et al. Evidence for the validity of a sleep habits survey for adolescents. Sleep. 2003;26:213–6. doi: 10.1093/sleep/26.2.213. [DOI] [PubMed] [Google Scholar]
- Woznica AA, Carney CE, Kuo JR, Moss TG. The insomnia and suicide link: toward an enhanced understanding of this relationship. Sleep medicine reviews. 2015;22:37–46. doi: 10.1016/j.smrv.2014.10.004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.