Abstract
Purpose of review
High protein intake may lead to increased intraglomerular pressure and glomerular hyperfiltration. This can cause damage to glomerular structure leading to or aggravating chronic kidney disease (CKD). Hence, a low protein diet (LPD) of 0.6–0.8 g/kg/day is often recommended for the management of CKD. We reviewed the effect of protein intake on incidence and progression of CKD and the role of LPD the CKD management.
Recent findings
Actual dietary protein consumption in CKD patients remain substantially higher than the recommendations for LPD. Notwithstanding the inconclusive results of the Modification of Diet in Renal Disease (MDRD) study, the largest randomized controlled trial to examine protein restriction in CKD, several prior and subsequent studies and meta-analyses including secondary analyses of the MDRD data appear to support the role of LPD on retarding progression of CKD and delaying initiation of maintenance dialysis therapy. LPD can also be used to control metabolic derangements in CKD. Supplemented LPD with essential amino acids or their keto-analogs may be used for incremental transition to dialysis especially in non-dialysis days. An LPD management in lieu of dialysis therapy can reduce costs, enhance psychological adaptation, and preserve residual renal function upon transition to dialysis. Adherence and adequate protein and energy intake should be ensured to avoid protein-energy wasting.
Summary
A balanced and individualized dietary approach based on LPD should be elaborated with periodic dietitian counselling and surveillance to optimize management of CKD, to assure adequate protein and energy intake and to avoid or correct protein-energy wasting.
Keywords: Low protein diet, progression of chronic kidney disease, Glomerular hyperfiltration, incremental hemodialysis, Protein energy wasting
Introduction
The crucial role of the kidney in amino acid and protein metabolism including breakdown and excretion of protein metabolites heralds paramount impact of dietary protein intake on metabolic processes regulated by kidney and on kidney function itself. High protein diet may cause damage to kidney and may lead to accumulation of toxic protein metabolites, while a low protein diet (LPD) offers a variety of clinical benefits in patients with renal insufficiency. However, interests and effort to adopt the merit of LPD in the management of chronic kidney disease (CKD) remain variable. This review focuses on the reasons as to why a high dietary protein intake may cause harm to the kidney, how lower protein intake may prolong kidney longevity, and why dietary protein restriction should be considered for and how it works in the management of CKD.
Impact of High Protein Diet on Renal Function
High protein diet, usually defined as >1.2 grams of dietary protein per kilogram of body weight per day (g/kg/day), is known to induce significant alterations in renal function and kidney health.[1] In contrast to dietary intake of fat and carbohydrates, higher protein intake modulates renal hemodynamic by increasing renal blood flow and elevating intraglomerular pressure leading to higher glomerular filtration rate (GFR) and more efficient excretion of protein-derived nitrogenous waste products, while an increase in kidney volume and weight may ensue.[2] The so-called “glomerular hyperfiltration” that is induced by high protein diet has been well reported in both animal models and in different clinical studies in human subjects (Table 1), [3–8] and confirmed in a recent meta-analysis including 30 randomized controlled trials (RCTs).[9] High protein diet associated glomerular hyperfiltration, together with resultant increase in urinary albumin excretion, may have deleterious consequences on kidney and other organs in long term.[1] Experimental studies have revealed that glomerular injury by an increase in intraglomerular pressure and flow can lead to progressive glomerular damage and sclerosis.[2,10]
Table 1.
Recent randomized controlled trials of high protein diet on renal function with over 24-week follow-up period including more than 50 participants.
| References | Sample size | Mean age (years) | Duration (weeks) | Protein amount (% of total energy amount or g/kg/day) | Renal function changes |
|---|---|---|---|---|---|
| Li et al, 2010[3] | 100 | 49.3 | 52 | HP-30%, 2.2g/kg/d NP/LP-15%, 1.1g/kg/d |
Cr and Ccr tended to increase in HP group, but not significant |
| Larsen et al, 2011[4] | 99 | 59.4 | 52 | HP-30% NP/LP-15% |
No significant differences of eGFR and mAlb. |
| Krebs et al, 2012[5] | 419 | 57.8 | 104 | HP-30% NP/LP-15% |
No significant differences of serum Cr and mAlb. |
| Friedman et al, 2012[6] | 307 | 45.5 | 104 | HP-LC diet (unlimited protein intake) NP/LP 15% |
eGFR and mAlb tended to increase in HP group, but not significant |
| Wycherley et al, 2012[7] | 68 | 50.8 | 52 | HP-1.24g/kg/d NP/LP-0.82g/kg/d |
Ccr tended to increase in HP group, but not significant |
| Tirosh et al, 2014[8] | 318 | 51.1 | 104 | HP-LC diet (unlimited protein intake) NP/LP 18.8–19.1% |
eGFR increased in HP group especially among CKD stage III patients. |
Abbreviations: HP-high protein diet; NP/LP-normal protein/low protein diet, LC diet-low carbohydrate diet; Cr-creatinine; eGFR-estimated glomerulofiltration rate; mAlb-microalbuminuria; CCr-creatinine clearance rate; CKD-chronic kidney disease.
Hence, whereas the GFR may increase in short-term, kidney damage may ensue and the renal function will decline with long-term exposure to high dietary protein intake. This is important in the contemporary life style where a high protein diet for weight management has gained increasing popularity.
It is not clear whether the potentially deleterious effects of high protein intake are equally observed in people with normal kidney function when compared to those with pre-existing kidney disorders. In the Nurses’ Health Study, high protein diet was associated with a faster decline in estimated GFR in people with subnormal kidney function, but not in those with normal kidney function.[11] It was the first large-scale observational study followed-up more than 10 years about the impact of high protein diet on renal function in general population. There are additional studies with conflicting results for the impact of high protein diet on renal function decline in the general population.[12,13]
A recent prospective study of the general population in Singapore indicated that the impact of protein consumption on the risk of end-stage renal failure (ESRD) may depend on the type of protein sources.[14] Specifically, red meat intake was strongly associated with ESRD risk in a dose dependent manner, while other protein sources such as poultry, fish, eggs, or dairy products did not show such a deleterious association. Higher acid load induced by sulfur-containing amino acids and end products from animal protein may exert detrimental effect on renal function. Meanwhile, another community-based cohort study showed the association of high protein intake with cardiovascular events but not with loss of kidney function.[12] Additional studies to examine these differences are warranted. Relevant data from selected observational studies are summarized in Table 2.[15,16]
Table 2.
Recent observational studies about high protein diet on renal function.
| References | Sample size | Mean age (years) | Duration (years) | HP diet | Baseline eGFR (ml/min per 1.73 m2) | Renal function changes |
|---|---|---|---|---|---|---|
| Knight et al. 2003[11] | 1,624 | 55.4 | 11 | Divided into quintiles (5th group: 93 g/day) |
Normal: >80 Mild CKD: 55–80 |
HP was not associated with eGFR decline in normal renal function. However, it was associated with accelerated eGFR decline in mild CKD, particularly with high intake of non-dairy animal protein. |
| Halbesma et al, 2009[12] | 8,461 | 49.8 | 6.4 | Divided into quintiles (5th group: 1.42–3.27 g/kg/day) |
mean 80.6 | There was no association of protein intake and rate of eGFR changes. |
| Lin et al, 2011[15] | 3,121 | 67 | 12 | Divided into quartiles (4th group: 78 g/day) |
median 76 | HP was directly associated with microalbuminuria (highest quartile vs. lowest OR, 2.17; 95% CI, 1.18–3.66; p=0.01), and rapid eGFR decline (OR, 1.77; 95% CI, 1.03–3.03). |
| Dunkler et al, 2013[16] | 6,123 | 66.6 | 5.5 | High: 0.96 g/kg/day Low: 0.36 g/kg/day |
mean 74.3 | Lower total and animal protein intake was associated with increased risk of CKD (highest tertile vs. lowest for total protein OR, 1.16; 95%CI, 1.05–1.30) |
| Cirillo et al, 2014[13] | 1,522 | 49.3 | 12 | High ≥ 1.6g/kg/day Low< 1.0g/kg/day |
mean 84.0 | HP was associated cross-sectionally with higher eGFR, but longitudinally with greater eGFR decline over time. |
| Lew et al, 2016[14] | 60,198 | 56.5 | 15.5 | Divided into quartiles (4th group: 65.3 g/day) |
n.d | Protein intake amount, especially consumption of red meat was strongly associated with ESRD risk. |
Abbreviations: CKD-chronic kidney disease; HP-high protein diet; eGFR-estimated glomerulofiltration rate; OR-odd ratios; CI-confidence interval; yr-year; n.d-not described; ESRD-end stage renal disease
Dietary Protein Intake in North Americans with and without Chronic Kidney Disease
LPD as a means of slowing CKD progression is not largely prescribed in the current clinical setting in North America.[1] Besides inconclusive data on the effectiveness of LPD (see below) and concerns about aggravation of protein-energy wasting (PEW), [2] one of main obstacles to the implementation of LPD is the big gap in protein intake between the amount of recommendations from guidelines and what is consumed contemporarily in the USA.[17] According to the National Health and Nutrition Examination Survey (NHANES) between 2001 and 2008, average dietary protein intake was 1.34 g/kg ideal body weight (IBW) per day or 1.09 g/kg actual body weight (ABW) per day in the US general population, [18] which is higher than the recommended protein intake for normal healthy adults (i.e., 0.8g/kg·ABW/day).[19] There were also variabilities in protein intake depending on CKD stages, and average protein intake was 1.04 g/kg·IBW/day or 0.81 g/kg·ABW/day in those with advanced stages of CKD.[18]
Benefits of Protein Restriction in Patients with Chronic Kidney Disease
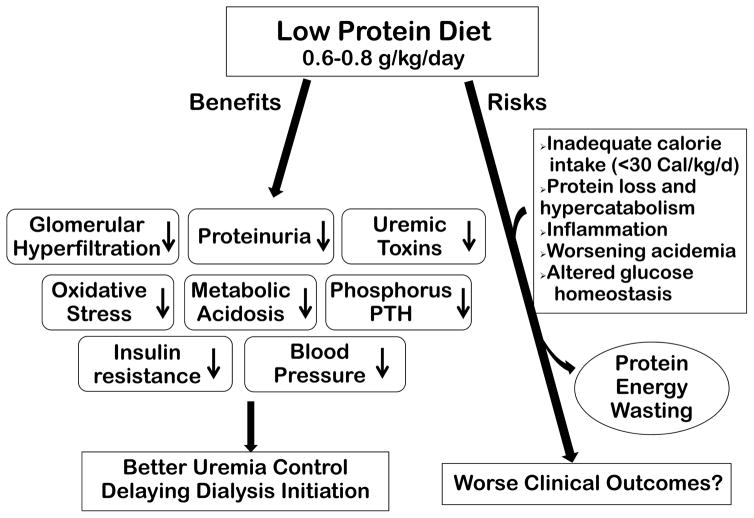
LPD reduces nitrogen waste products and decrease kidney workload by lowering intraglomerular pressure, which may protect the kidneys especially in patients with decreased nephron capital and renal function. It leads to favorable metabolic effects that can preserve kidney function and control of uremic symptoms as listed below and depicted in Figure 1.[2,10,20]
Figure 1.
Diagram of the role of low protein diet in the management of chronic kidney disease.
Effect of Protein Restriction on Proteinuria and Albuminuria
Urinary protein or albumin excretion, a surrogate of the progression of CKD, increases with damages in podocytes and proximal tubular cells.[21] In turn proteinuria induces apoptosis of renal tubules and impairs podocyte regeneration, which leads to tubular atrophy and progressive renal failure (Figure 2).[22] Protein restriction has been demonstrated to lower proteinuria by 20–50% in patients with CKD, and a linear-relationship between reduction of protein intake and decrease in proteinuria is reported.[23] LPD may exert its vasoconstrictive effect at afferent arterioles while the renin-angiotensin system (RAAS) inhibition treatment preferentially decreases efferent resistance. Indeed LPD shows additive anti-proteinuric effect over the RAAS inhibition treatment.[2] Thus, the combined treatment with LPD and the RAAS blockade may be warranted to achieve lower urinary protein levels and to further reduce risk of CKD progression.
Figure 2.
Effect of high dietary protein intake on kidney
Effect of LPD on the Progression of Chronic Kidney Disease
Experimental studies in 1980s demonstrated that LPD imposed on animal models of CKD led to a greater preservation of GFR.[10] Since then, the renoprotective effect of LPD had been supported by several clinical trials.[23] However, the Modification of Diet in Renal Disease (MDRD) study, which has thus far been the largest controlled trial of dietary protein management in CKD, failed to show the definite effectiveness of LPD on retarding CKD progression.[2,10] It contributed to form a conception that dietetic therapy plays a marginal role in the management of CKD. Yet secondary analysis of the MDRD study showed that each 0.2 g/kg/day decrease in protein intake was associated with a small amelioration in GFR decline over time, i.e., 1.15 ml/min/1.73m2/year, and with a halved risk of renal failure or death.[24] Indeed, the relatively short period of the MDRD study and the unusually large proportion of polycystic kidney patients who often have very slow CKD progression might have reduced the study power. Renoprotective effect of LPD may be reinforced proportionally with the extent of protein restriction. A recent RCT demonstrated that very low vegetarian protein diet (VLPD, 0.3g/kg/day) supplemented with keto-analogs, compared to conventional LPD (0.6g/kg/d), mitigated kidney function decline and reduced the number of patients requiring renal replacement therapy.[25] A meta-analysis of RCTs including the MDRD study also confirmed the risk reduction of the development of ESRD by protein restriction among non-diabetic patients with CKD.[26] It is postulated that LPD prevents uremic symptoms and avoids dialysis therapy despite the small effect on kidney function decline.
Effect of Low Protein Diet on Metabolic Control
LPD is beneficial to improve metabolic acidosis in CKD. Acid is generated during metabolism of proteins including sulfur containing amino-acids, and pre-dialysis serum bicarbonate concentration was lower in patients with higher protein intake.[27–29] There is a tendency toward acid retention with kidney function declines and resultant chronic metabolic acidosis in CKD impairs protein metabolism, increases muscle catabolism and wasting, and aggravates decline in renal function and uremic symptoms.[30] Indeed, LPD ameliorated metabolic acidosis among patients with advanced CKD. In a study of supplemented VLPD, mean serum bicarbonate levels remained <19 mmol/L in the control (LPD) group while it increased to the normal levels in the VLPD group.[25] Interestingly, a RCT of correcting metabolic acidosis with sodium bicarbonate supplementation among patients with stage 4 CKD showed that after 2 years of study period, participants in the intervention group experienced slower decline in kidney function, much lower incidence of ESRD, and improvements in nutritional status although they increased dietary protein intake.[31]
LPD also offers better control of CKD-mineral and bone disorder (MBD). Dietary control is essential in the management of hyperphosphatemia in CKD, because dietary protein, especially animal protein, is the major source of phosphorus.[32–34] LPD, especially with plant protein, is efficacious on lowering serum phosphorus, which results in reduction in serum levels of parathyroid hormone (PTH) and fibroblast growth factor (FGF)-23.[35,36] Although the benefits of LPD in CKD-MBD may include slowing the progression of vascular calcification and improving cardiovascular outcome, [37] it should be noted that the risk may outweigh if LPD is solely used to control hyperphosphatemia.[38,39]
Additionally, LPD may attenuate insulin resistance and oxidative stress, the common features that may play roles in accelerating atherosclerosis among patients with CKD.[2,40]. VLPD supplemented with keto-analogs also ameliorated erythropoietin responsiveness.[23,41] These metabolic advantages of LPD in CKD aid better control of uremic symptoms, decrease in cardiovascular risk, and less medications leading to better adherence.[42]
Conservative Management with Low Protein Diet in End-Stage Renal Disease
Less accumulation of protein waste products relieves clinical manifestations of uremia even in very late stage of CKD, and indeed LPD can be used effectively to delay the initiation of dialysis therapy.[10] Given that earlier dialysis initiation does not appear to offer any survival benefit, [1] conservative approaches are warranted in managing patients with advanced CKD.
A RCT among elderly patients with GFR 5–7 ml/min demonstrated that VLPD supplemented with keto-analogs and vitamins delayed the initiation of dialysis by a mean period of 10.7 months without negative consequences. Estimated economic benefit for health care system based on this study was €21,180/patient in the first year.[43] Financial saving with delayed dialysis by LPD was also confirmed in another study.[44] Delaying dialysis with LPD could also save time for maturation of arteriovenous fistula and avoid the insertion of central venous catheter.[45] Furthermore, LPD may play a role in incremental transition to dialysis therapy; once-weekly dialysis combined with LPD was found beneficial compared to thrice-weekly hemodialysis with respect to frequency of hospitalization, dose of erythropoietin, phosphorus binder, and cinacalcet therapy, without a significant difference in patient survival.[46] The importance of incremental dialysis has been revisited to preserve residual kidney function in dialysis patients, [47–51] because rapid decline in residual kidney function is associated with increased mortality.[52] Implementation of LPD regimen by dietary counselling combined with low phosphorus and high energy intake may support incremental transition to thrice a week hemodialysis.[53]
Conflicting Data and Safety Issue about Low Protein Diet in CKD
In spite of many available evidences for benefits of LPD described above, renoprotective effect of LPD has been debated due to conflicting reports and concerns with malnutrition. In fact, several studies including the MDRD study showed negative results regarding the effectiveness of LPD, [2,10] and the benefit of LPD was not confirmed in diabetic patients.[54,55]
Several studies of protein restriction in CKD in patients without other serious illnesses have shown acceptable safety and a low rate of malnutrition even with VLPD. A 0.6 g/kg/day of protein intake may meet protein requirement among clinically stable, non-dialysis-dependent CKD patients.[40] In a 48-month RCT of LPD in patients with CKD stages 3–5, dietary intervention was given under careful monitoring for nutritional status, and only 3 subjects developed malnutrition, [10] suggesting that close monitoring for nutritional status was more important to avoid malnutrition rather than the amount of protein intake itself. Some studies reported preserved body composition and skeletal muscle mass and function in CKD patients on LPD.[56]
However, protein and calorie intake tend to decrease as renal function declines, and the gastrointestinal absorption and utilization of ingested protein may be hindered in advanced CKD.[57] Given that adequate calorie intake (30–35 kcal/kg·AW/day) is needed to avoid protein catabolism and malnutrition under protein restriction ≤0.6 g/kg·ABW /day, [19,58] uremic anorexia raises a question about safety of LPD, which otherwise may induce malnutrition and aggravate protein-energy wasting (PEW) among patients with CKD.[59,60] In the MDRD study, the LPD group, compared to the usual diet group, experienced unfavorable changes of anthropometric measurements account for nutritional status such as decrease in body weight, body fat percent, skinfold thickness, and arm muscle area.[61] Furthermore, although there was no differences in nutritional parameters except for 24–hour urinary creatinine between the VLPD vs. LPD group in the MDRD study, the long-term follow-up study showed higher mortality risk associated with VLPD supplemented with amino-acids.[62] However, the energy intakes of participants were substantially low (≈22 kcal/kg/day), which may have increased the risk og malnutrition risk and PEW with VLPD. This is so far the only study that followed up participants with VLPD for up to 7 years. In a recent 18-month RCT comparing ketoanalogue-supplemented VLPD with LPD, participants in both groups showed average energy intakes ≈30 kcal/kg•IBW/day and preserved nutritional status.[25] Although the VLPD group showed a lower risk of ESRD compared to the LPD group, studies with longer follow-ups are necessary to evaluate the safety underlying VLPD.
The Challenge of Adherence to Low Protein Diet
Despite the established benefits of LPD in CKD management, adherence to LPD is a key element to gain its renoprotective effect. Although psychosocial factors such as knowledge, attitude, and support, are among the most important determinants of adherence, [10] successful adherence was hardly predictable.[41] Good patient-physician communication, self-monitoring of protein intake, and periodic feedback by the dietitian strengthens adherence through improved recognition of the importance of diet.[63] Education with simplified diet approach could also assist in robust adherence.[64–66] In a RCT with CKD stage 3 patients, renal nutrition education program including individual class, hands-on sessions about food types, and recipe distribution improved adherence to LPD.[67] Better knowledge about patient’s preference for food types and continuous effort to find new solutions for better tolerability would be essential for successful dietary treatment.[68] Given the high frequency of poor adherence with dietary protein restriction in some CKD management centers, there has been criticism against the role of LPD in the real-world clinical practice. In a meta-analysis of 13 RCTs the mean of protein intake in restricted group was 0.68g/kg/day, which was higher than target values and marginally below the recommended protein intake in the general population.[69] Indeed, even 0.1 to 0.2 g/kg/day reduction in protein intake from baseline appears to result in significant metabolic improvement and longer preservation of kidney health.[2] The VLPD may offer incremental renal protection and beneficial metabolic effects compared to LPD despite a more challenging adherence and somewhat higher risk of PEW (see Figure 1).[70] We believe some reduction in dietary protein intake from baseline is warranted across virtually all stages of CKD but the protein intake target range should be individualized, e.g. we suggest <1.0 g/kg.IBW/day for non-proteinuric CKD stages 1 and 2 such as in those after nephrectomy with a solitary kidney or elderly people with Stage 3b and very slow progression, and 0.6–0.8 g/kg.IBW/day for patients with eGFR<45 mg/ml/1.73m2BSA or proteinuria. Good adherence to LPD is defined as an actual intake within ±20% of the prescribed target range in 80% of the time.[1] It should be noted again that adherence to adequate energy intake (i.e., 30–35 kcal/kg·ABW/day) is also essential for the success in protein restriction, especially with more healthy and complex carbohydrates and mono- and poly-unsaturated fat.[71]
Nutritional Assessment in Low Protein Diet
Protein and energy requirement varies with clinical conditions and across severity of disease, and actual intake could also be affected with psychosocial aspects and comorbid conditions. Therefore, frequent periodic follow-up visits, e.g. every 3–4 months, for monitoring dietary intake and nutritional status is essential in the implementation of LPD. To verify if actual protein intake is in prescribed range, the amount of protein intake should be periodically evaluated preferably by nitrogen appearance via serial 24-hour urine collections.[1] Dietary intake can be assessed with dietary recalls or interviews, and food frequency questionnaires.[65] One caveat is that dietary protein intake is overestimated by UNA-based calculation if patients are on hypercatabolic states including malnutrition, inflammatory conditions, post-operative period, and burns. Because such patient would appear “non-adherent” to LPD even if they actually follow the prescribed protein intake, careful monitoring of both disease conditions and nutritional status together with other diet assessment tools is necessary before reinforcing protein restriction.
Physical measurements such as body weight and anthropometries, [72,73] or biochemical parameters such as transthyretin, cholesterol and normalized protein nitrogen appearance provide additional data on patient nutritional status.[2,74–76] However, it should be noted that in the MDRD study, the VLPD group, compared to the LPD group, did not show any significant difference in these nutritional parameters except for 24-hour urinary creatinine despite the increased mortality risk in the follow-up study in VLDP but not LPD.[62] Further studies are still necessary to develop a sensitive method to detect inadequate nutrient intake of either protein or energy.
Essential Amino-acid and Ketoanalog Supplemented Very-Low Protein Diet
To attain proper nutritional status and avoid PEW, nutritional supplementation with essential amino-acids (EAAs) and keto-analogs has been proposed primarily for VLPD.[41] EAAs need to be obtained from food, because it could not be generated in the body. Meanwhile, keto-analogs, formed by transamination of EAAs except lysine and threonine, can be utilized through their conversion to respective EAAs without providing nitrogen products.[39] Potential benefits of EAAs and keto-analogs supplementation include (1) maintaining protein-energy status without increase in nitrogen waste products; (2) reducing phosphorus and acid load given no phosphorus in purified EAA or their ketoanalogs; and (3) decreasing protein degradation and enhancing protein synthesis.[39] However, it can be argued that >25% less protein intake than recommended in the general population (given the <0.6 g/kg•ABW/day is the lowest protein requirement to avoid negative nitrogen balance) on a long-term basis might eventually compromise metabolic balance and survival through gradually deteriorating nutritional status if patients may suffer from hypercatabolic conditions such as infections. Such considerations have led to the emergence of a camp in the field of renal nutrition representing the opinion that even a protein intake of 0.6 g/kg/day needs to be supplemented by EAAs or keto-analogs.[19] Indeed in both LPD and VLPD, at least 50% of the dietary protein intake should be provided by high biologic value proteins.[24]
Although the efficacy of keto-analogs combined with VLPD, compare to standard LPD, for retarding the progression of CKD was not significant in the MDRD study, it was observed in other studies including several RCTs and meta-analyses.[2,26,38] Supplemented VLPD with keto-analogs and EAAs also had benefits for better metabolic control in hyperphosphatemia, and anemia.[38] Further studies are required to explore how to combine protein restriction and supplementation for minimizing the risk of malnutrition while maximizing the benefits of LPD.
Protein Intake in Maintenance Dialysis Patients
Dialysis treatment may stimulate protein catabolism, which aggravates PEW in ESRD patients. In a recent study, whole-body skeletal muscle metabolism appeared to increase to lead net loss of muscle protein during hemodialysis treatment.[58] Guidelines recommends much higher protein intake (1.2–1.4 g/kg.IBW/day) in ESRD patients treated with dialysis than in pre-dialysis CKD patients, [17,32] because dialysis itself is sufficient to correct uremic symptoms and metabolic derangements without LPD, and proper protein intake should be assured to avoid aggravation of PEW caused by loss of nutrients and hypermetabolism during dialysis treatment.[58,77] Low dietary protein intake is associated with higher morbidity, hospitalization and mortality in hemodialysis patients.[78] Interestingly, elements of over-nutrition such as increased body mass index or high serum cholesterol levels, which are deleterious in the general population, are paradoxically protective in dialysis patients, which is known as “obesity paradox” or “reverse epidemiology”.[79] Strict diet restrictions may cause unfavorable outcome in dialysis patients. Careful relaxation for dietary restrictions and adoption of more balanced diet regimen with individualized approach should be considered in patients treated with dialysis.[80,81]
Conclusion
The aim of LPD for handling accumulation of protein waste products conservatively and delaying the need for dialysis treatment has been hampered by the fear of PEW. Implementation of LPD as proper dietary regimen is recommended to retard decline of GFR and initiation of dialysis. Multi-directional approach including dietary approach should be considered to ensure the best outcome for CKD patients.
Key Points.
Protein intake in North America and other industrialized nations is higher than the recommended amounts including in CKD patients.
LPD can be used to attenuate glomerular hyperfiltration and proteinuria, which may lead to slow down CKD progression.
LPD may facilitate the targeted delay in the initiation of dialysis and can be used to adopt incremental or infrequent dialysis.
Effort for good adherence to LPD is essential to achieve the goals.
In dialysis patients, proper amount of protein intake should be ensured to avoid protein-energy wasting.
Acknowledgments
Funding Sources:
Supported by research grants from the National Institute of Diabetes, Digestive and Kidney Disease of the National Institutes of Health K24-DK091419 and philanthropic grants from Dr Joseph Lee and Mr. Lois Chang.
Footnotes
Important Disclosure
KKZ serves as a part-time physician in a US Department of Veterans Affairs medical center as a part-time employee of a US Department of Veterans Affairs medical center. Opinions expressed in this paper are those of the authors’ and do not represent the official opinion of the US Department of Veterans Affairs.
Potential Conflict of Interests
Dr. K. Kalantar-Zadeh has received honoraria and/or support from Abbott, Abbvie, Alexion, Amgen, ASN (American Society of Nephrology), Astra-Zeneca, Aveo, Chugai, DaVita, Fresenius, Genentech, Haymarket Media, Hofstra Medical School, IFKF (International Federation of Kidney Foundations), ISH (International Society of Hemodialysis), International Society of Renal Nutrition & Metabolism (ISRNM), JSDT (Japanese Society of Dialysis Therapy), Hospira, Kabi, Keryx, Novartis, NIH (National Institutes of Health), NKF (National Kidney Foundations), Pfizer, Relypsa, Resverlogix, Sandoz, Sanofi, Shire, Vifor, UpToDate, ZS-Pharma.
References
- *1.Kalantar-Zadeh K, Moore LW, Tortorici AR, et al. North American experience with Low protein diet for Non-dialysis-dependent chronic kidney disease. BMC Nephrol. 2016;17:90. doi: 10.1186/s12882-016-0304-9. This review paper evaluated the current status of diet pattern in North America, impact of current consumption of protein, role of low protein diet in CKD patients, and the obstacles for implementation of low protein diet in North America. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fouque D, Aparicio M. Eleven reasons to control the protein intake of patients with chronic kidney disease. Nat Clin Pract Nephrol. 2007;3:383–392. doi: 10.1038/ncpneph0524. [DOI] [PubMed] [Google Scholar]
- 3.Li Z, Treyzon L, Chen S, et al. Protein-enriched meal replacements do not adversely affect liver, kidney or bone density: an outpatient randomized controlled trial. Nutr J. 2010;9:72. doi: 10.1186/1475-2891-9-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Larsen RN, Mann NJ, Maclean E, et al. The effect of high-protein, low-carbohydrate diets in the treatment of type 2 diabetes: a 12 month randomised controlled trial. Diabetologia. 2011;54:731–740. doi: 10.1007/s00125-010-2027-y. [DOI] [PubMed] [Google Scholar]
- 5.Krebs JD, Elley CR, Parry-Strong A, et al. The Diabetes Excess Weight Loss (DEWL) Trial: a randomised controlled trial of high-protein versus high-carbohydrate diets over 2 years in type 2 diabetes. Diabetologia. 2012;55:905–914. doi: 10.1007/s00125-012-2461-0. [DOI] [PubMed] [Google Scholar]
- 6.Friedman AN, Ogden LG, Foster GD, et al. Comparative effects of low-carbohydrate high-protein versus low-fat diets on the kidney. Clin J Am Soc Nephrol. 2012;7:1103–1111. doi: 10.2215/CJN.11741111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wycherley TP, Brinkworth GD, Clifton PM, et al. Comparison of the effects of 52 weeks weight loss with either a high-protein or high-carbohydrate diet on body composition and cardiometabolic risk factors in overweight and obese males. Nutr Diabetes. 2012;2:e40. doi: 10.1038/nutd.2012.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tirosh A, Golan R, Harman-Boehm I, et al. Renal function following three distinct weight loss dietary strategies during 2 years of a randomized controlled trial. Diabetes Care. 2013;36:2225–2232. doi: 10.2337/dc12-1846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schwingshackl L, Hoffmann G. Comparison of high vs. normal/low protein diets on renal function in subjects without chronic kidney disease: a systematic review and meta-analysis. PLoS One. 2014;9:e97656. doi: 10.1371/journal.pone.0097656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bellizzi V. Low-protein diet or nutritional therapy in chronic kidney disease? Blood Purif. 2013;36:41–46. doi: 10.1159/000350585. [DOI] [PubMed] [Google Scholar]
- 11.Knight EL, Stampfer MJ, Hankinson SE, et al. The impact of protein intake on renal function decline in women with normal renal function or mild renal insufficiency. Ann Intern Med. 2003;138:460–467. doi: 10.7326/0003-4819-138-6-200303180-00009. [DOI] [PubMed] [Google Scholar]
- 12.Halbesma N, Bakker SJ, Jansen DF, et al. High protein intake associates with cardiovascular events but not with loss of renal function. J Am Soc Nephrol. 2009;20:1797–1804. doi: 10.1681/ASN.2008060649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cirillo M, Lombardi C, Chiricone D, et al. Protein intake and kidney function in the middle-age population: contrast between cross-sectional and longitudinal data. Nephrol Dial Transplant. 2014;29:1733–1740. doi: 10.1093/ndt/gfu056. [DOI] [PubMed] [Google Scholar]
- 14.Lew QJ, Jafar TH, Koh HW, et al. Red Meat Intake and Risk of ESRD. J Am Soc Nephrol. 2016 doi: 10.1681/ASN.2016030248. [DOI] [PMC free article] [PubMed]
- 15.Lin J, Fung TT, Hu FB, et al. Association of dietary patterns with albuminuria and kidney function decline in older white women: a subgroup analysis from the Nurses’ Health Study. Am J Kidney Dis. 2011;57:245–254. doi: 10.1053/j.ajkd.2010.09.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dunkler D, Dehghan M, Teo KK, et al. Diet and kidney disease in high-risk individuals with type 2 diabetes mellitus. JAMA Intern Med. 2013;173:1682–1692. doi: 10.1001/jamainternmed.2013.9051. [DOI] [PubMed] [Google Scholar]
- 17.Kidney_Disease_Improving_Global_Outcomes_CKD_Work_Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl. 2013;3:1–50. doi: 10.1038/ki.2013.243. [DOI] [PubMed] [Google Scholar]
- 18.Moore LW, Byham-Gray LD, Scott Parrott J, et al. The mean dietary protein intake at different stages of chronic kidney disease is higher than current guidelines. Kidney Int. 2013;83:724–732. doi: 10.1038/ki.2012.420. [DOI] [PubMed] [Google Scholar]
- 19.Kovesdy CP, Kopple JD, Kalantar-Zadeh K. Management of protein-energy wasting in non-dialysis-dependent chronic kidney disease: reconciling low protein intake with nutritional therapy. Am J Clin Nutr. 2013;97:1163–1177. doi: 10.3945/ajcn.112.036418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kovesdy CP, Kalantar-Zadeh K. Back to the future: restricted protein intake for conservative management of CKD, triple goals of renoprotection, uremia mitigation, and nutritional health. Int Urol Nephrol. 2016;48:725–729. doi: 10.1007/s11255-016-1224-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dickson LE, Wagner MC, Sandoval RM, et al. The proximal tubule and albuminuria: really! J Am Soc Nephrol. 2014;25:443–453. doi: 10.1681/ASN.2013090950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Peired A, Angelotti ML, Ronconi E, et al. Proteinuria impairs podocyte regeneration by sequestering retinoic acid. J Am Soc Nephrol. 2013;24:1756–1768. doi: 10.1681/ASN.2012090950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Riccio E, Di Nuzzi A, Pisani A. Nutritional treatment in chronic kidney disease: the concept of nephroprotection. Clin Exp Nephrol. 2015;19:161–167. doi: 10.1007/s10157-014-1041-7. [DOI] [PubMed] [Google Scholar]
- 24.Levey AS, Greene T, Beck GJ, et al. Dietary protein restriction and the progression of chronic renal disease: what have all of the results of the MDRD study shown?. Modification of Diet in Renal Disease Study group. J Am Soc Nephrol. 1999;10:2426–2439. doi: 10.1681/ASN.V10112426. [DOI] [PubMed] [Google Scholar]
- 25.Garneata L, Stancu A, Dragomir D, et al. Ketoanalogue-Supplemented Vegetarian Very Low-Protein Diet and CKD Progression. J Am Soc Nephrol. 2016;27:2164–2176. doi: 10.1681/ASN.2015040369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fouque D, Laville M. Low protein diets for chronic kidney disease in non diabetic adults. Cochrane Database Syst Rev. 2009:CD001892. doi: 10.1002/14651858.CD001892.pub3. [DOI] [PubMed] [Google Scholar]
- 27.Scialla JJ, Anderson CA. Dietary acid load: a novel nutritional target in chronic kidney disease? Adv Chronic Kidney Dis. 2013;20:141–149. doi: 10.1053/j.ackd.2012.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Goraya N, Wesson DE. Dietary management of chronic kidney disease: protein restriction and beyond. Curr Opin Nephrol Hypertens. 2012;21:635–640. doi: 10.1097/MNH.0b013e328357a69b. [DOI] [PubMed] [Google Scholar]
- 29.Kalantar-Zadeh K. Moderator’s view: Higher serum bicarbonate in dialysis patients is protective. Nephrol Dial Transplant. 2016;31:1231–1234. doi: 10.1093/ndt/gfw258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Goraya N, Wesson DE. Dietary interventions to improve outcomes in chronic kidney disease. Curr Opin Nephrol Hypertens. 2015;24:505–510. doi: 10.1097/MNH.0000000000000160. [DOI] [PubMed] [Google Scholar]
- 31.Gaggl M, Sliber C, Sunder-Plassmann G. Effect of oral alkali supplementation on progression of chronic kidney disease. Curr Hypertens Rev. 2014;10:112–120. doi: 10.2174/1573402111666141231123314. [DOI] [PubMed] [Google Scholar]
- 32.St-Jules DE, Woolf K, Pompeii ML, et al. Reexamining the Phosphorus-Protein Dilemma: Does Phosphorus Restriction Compromise Protein Status? J Ren Nutr. 2016;26:136–140. doi: 10.1053/j.jrn.2015.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Streja E, Lau WL, Goldstein L, et al. Hyperphosphatemia is a combined function of high serum PTH and high dietary protein intake in dialysis patients. Kidney Int Suppl (2011) 2013;3:462–468. doi: 10.1038/kisup.2013.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cupisti A, Kalantar-Zadeh K. Management of natural and added dietary phosphorus burden in kidney disease. Semin Nephrol. 2013;33:180–190. doi: 10.1016/j.semnephrol.2012.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Di Iorio B, Di Micco L, Torraca S, et al. Acute effects of very-low-protein diet on FGF23 levels: a randomized study. Clin J Am Soc Nephrol. 2012;7:581–587. doi: 10.2215/CJN.07640711. [DOI] [PubMed] [Google Scholar]
- 36.Scialla JJ, Appel LJ, Wolf M, et al. Plant protein intake is associated with fibroblast growth factor 23 and serum bicarbonate levels in patients with chronic kidney disease: the Chronic Renal Insufficiency Cohort study. J Ren Nutr. 2012;22:379–388. e371. doi: 10.1053/j.jrn.2012.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fouque D, Horne R, Cozzolino M, et al. Balancing nutrition and serum phosphorus in maintenance dialysis. Am J Kidney Dis. 2014;64:143–150. doi: 10.1053/j.ajkd.2014.01.429. [DOI] [PubMed] [Google Scholar]
- 38.Jiang Z, Zhang X, Yang L, et al. Effect of restricted protein diet supplemented with keto analogues in chronic kidney disease: a systematic review and meta-analysis. Int Urol Nephrol. 2016;48:409–418. doi: 10.1007/s11255-015-1170-2. [DOI] [PubMed] [Google Scholar]
- *39.Shah AP, Kalantar-Zadeh K, Kopple JD. Is there a role for ketoacid supplements in the management of CKD? Am J Kidney Dis. 2015;65:659–673. doi: 10.1053/j.ajkd.2014.09.029. This review thoroughly summarized the composition of ketoacid, the role on renal progression and metabolic control in CKD patients and the results of previous studies. [DOI] [PubMed] [Google Scholar]
- 40.Chauveau P, Aparicio M. Benefits in nutritional interventions in patients with CKD stage 3–4. J Ren Nutr. 2011;21:20–22. doi: 10.1053/j.jrn.2010.11.005. [DOI] [PubMed] [Google Scholar]
- *41.Fouque D, Chen J, Chen W, et al. Adherence to ketoacids/essential amino acids-supplemented low protein diets and new indications for patients with chronic kidney disease. BMC Nephrol. 2016;17:63. doi: 10.1186/s12882-016-0278-7. This review showed the impact of low protein diet supplemented with ketoacid on metabolic, nutritional and renal parameters, and gave information how to improve adherence in diet prescription. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Molnar MZ, Gosmanova EO, Sumida K, et al. Predialysis Cardiovascular Disease Medication Adherence and Mortality After Transition to Dialysis. Am J Kidney Dis. 2016 doi: 10.1053/j.ajkd.2016.02.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Scalone L, Borghetti F, Brunori G, et al. Cost-benefit analysis of supplemented very low-protein diet versus dialysis in elderly CKD5 patients. Nephrol Dial Transplant. 2010;25:907–913. doi: 10.1093/ndt/gfp572. [DOI] [PubMed] [Google Scholar]
- 44.Mennini FS, Russo S, Marcellusi A, et al. Economic effects of treatment of chronic kidney disease with low-protein diet. J Ren Nutr. 2014;24:313–321. doi: 10.1053/j.jrn.2014.05.003. [DOI] [PubMed] [Google Scholar]
- 45.Duenhas M, Goncalves E, Dias M, et al. Reduction of morbidity related to emergency access to dialysis with very low protein diet supplemented with ketoacids (VLPD+KA) Clin Nephrol. 2013;79:387–393. doi: 10.5414/CN107460. [DOI] [PubMed] [Google Scholar]
- 46.Caria S, Cupisti A, Sau G, et al. The incremental treatment of ESRD: a low-protein diet combined with weekly hemodialysis may be beneficial for selected patients. BMC Nephrol. 2014;15:172. doi: 10.1186/1471-2369-15-172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kalantar-Zadeh K, Unruh M, Zager PG, et al. Twice-weekly and incremental hemodialysis treatment for initiation of kidney replacement therapy. Am J Kidney Dis. 2014;64:181–186. doi: 10.1053/j.ajkd.2014.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rhee CM, Unruh M, Chen J, et al. Infrequent dialysis: a new paradigm for hemodialysis initiation. Semin Dial. 2013;26:720–727. doi: 10.1111/sdi.12133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *49.Obi Y, Streja E, Rhee CM, et al. Incremental Hemodialysis, Residual Kidney Function, and Mortality Risk in Incident Dialysis Patients: A Cohort Study. Am J Kidney Dis. 2016 doi: 10.1053/j.ajkd.2016.01.008. The importance of incremental dialysis for better survival of hemodialysis patients has been revisited. This study supported the idea, and linked the importance of incremental dialysis to perserve residual renal function based on association of both parameters. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mathew AOY, Rhee CM, et al. Treatment frequency and mortality among incident hemodialysis patients in the United States comparing incremental with standard and more frequent dialysis. Kidney Int. 2016 doi: 10.1016/j.kint.2016.05.028. in press. [DOI] [PubMed] [Google Scholar]
- 51.Zhang M, Wang M, Li H, et al. Association of initial twice-weekly hemodialysis treatment with preservation of residual kidney function in ESRD patients. Am J Nephrol. 2014;40:140–150. doi: 10.1159/000365819. [DOI] [PubMed] [Google Scholar]
- *52.Obi Y, Rhee CM, Mathew AT, et al. Residual Kidney Function Decline and Mortality in Incident Hemodialysis Patients. J Am Soc Nephrol. 2016 doi: 10.1681/ASN.2015101142. This retrospective observational study based on large number of dialysis patients cohort demonstrated the importance of residual renal function in incident hemodialysis patients. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *53.Bolasco P, Cupisti A, Locatelli F, et al. Dietary Management of Incremental Transition to Dialysis Therapy: Once-Weekly Hemodialysis Combined With Low-Protein Diet. J Ren Nutr. 2016 doi: 10.1053/j.jrn.2016.01.015. This review summarized and compared between different frequency of dialysis treatment, and described a role in low protein diet for incremental transition to thrice weekly dialysis. [DOI] [PubMed] [Google Scholar]
- **54.Rughooputh MS, Zeng R, Yao Y. Protein Diet Restriction Slows Chronic Kidney Disease Progression in Non-Diabetic and in Type 1 Diabetic Patients, but Not in Type 2 Diabetic Patients: A Meta-Analysis of Randomized Controlled Trials Using Glomerular Filtration Rate as a Surrogate. PLoS One. 2015;10:e0145505. doi: 10.1371/journal.pone.0145505. The effect of low protein diet on diabetic nephropathy has been debated. Some RCTs showed beneficial effect of LPD. On the other hand, it was demonstrated not to be helpful in meta-analysis in 2007. This meta-analysis evaluated the effect of LPD on renal progression in diabetic patients based on data from RCTs according to types of diabetes. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Goldstein-Fuchs J, Kalantar-Zadeh K. Nutrition Intervention for Advanced Stages of Diabetic Kidney Disease. Diabetes Spectr. 2015;28:181–186. doi: 10.2337/diaspect.28.3.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Dumler F. Body composition modifications in patients under low protein diets. J Ren Nutr. 2011;21:76–81. doi: 10.1053/j.jrn.2010.10.005. [DOI] [PubMed] [Google Scholar]
- 57.Ebner N, Springer J, Kalantar-Zadeh K, et al. Mechanism and novel therapeutic approaches to wasting in chronic disease. Maturitas. 2013;75:199–206. doi: 10.1016/j.maturitas.2013.03.014. [DOI] [PubMed] [Google Scholar]
- *58.Obi Y, Qader H, Kovesdy CP, et al. Latest consensus and update on protein-energy wasting in chronic kidney disease. Curr Opin Clin Nutr Metab Care. 2015;18:254–262. doi: 10.1097/MCO.0000000000000171. This review described the results of recent studies about the protein-energy wasting and reemphasized the importance of management of PEW in CKD patients. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Mak RH, Ikizler AT, Kovesdy CP, et al. Wasting in chronic kidney disease. J Cachexia Sarcopenia Muscle. 2011;2:9–25. doi: 10.1007/s13539-011-0019-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kalantar-Zadeh K, Rhee C, Sim JJ, et al. Why cachexia kills: examining the causality of poor outcomes in wasting conditions. J Cachexia Sarcopenia Muscle. 2013;4:89–94. doi: 10.1007/s13539-013-0111-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kopple JD, Levey AS, Greene T, et al. Effect of dietary protein restriction on nutritional status in the Modification of Diet in Renal Disease Study. Kidney Int. 1997;52:778–791. doi: 10.1038/ki.1997.395. [DOI] [PubMed] [Google Scholar]
- 62.Mitch WE, Remuzzi G. Diets for patients with chronic kidney disease, should we reconsider? BMC Nephrol. 2016;17:80. doi: 10.1186/s12882-016-0283-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ikizler TA, Franch HA, Kalantar-Zadeh K, et al. Time to revisit the role of renal dietitian in the dialysis unit. J Ren Nutr. 2014;24:58–60. doi: 10.1053/j.jrn.2013.10.006. [DOI] [PubMed] [Google Scholar]
- 64.Pisani A, Riccio E, Bellizzi V, et al. 6-tips diet: a simplified dietary approach in patients with chronic renal disease. A clinical randomized trial. Clin Exp Nephrol. 2016;20:433–442. doi: 10.1007/s10157-015-1172-5. [DOI] [PubMed] [Google Scholar]
- 65.Kalantar-Zadeh K, Kovesdy CP, Bross R, et al. Design and development of a dialysis food frequency questionnaire. J Ren Nutr. 2011;21:257–262. doi: 10.1053/j.jrn.2010.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kalantar-Zadeh K. Patient education for phosphorus management in chronic kidney disease. Patient Prefer Adherence. 2013;7:379–390. doi: 10.2147/PPA.S43486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Paes-Barreto JG, Silva MI, Qureshi AR, et al. Can renal nutrition education improve adherence to a low-protein diet in patients with stages 3 to 5 chronic kidney disease? J Ren Nutr. 2013;23:164–171. doi: 10.1053/j.jrn.2012.10.004. [DOI] [PubMed] [Google Scholar]
- 68.D’Alessandro C, Rossi A, Innocenti M, et al. Dietary protein restriction for renal patients: don’t forget protein-free foods. J Ren Nutr. 2013;23:367–371. doi: 10.1053/j.jrn.2012.12.006. [DOI] [PubMed] [Google Scholar]
- 69.Piccoli GB, Capizzi I, Vigotti FN, et al. Low protein diets in patients with chronic kidney disease: a bridge between mainstream and complementary-alternative medicines? BMC Nephrol. 2016;17:76. doi: 10.1186/s12882-016-0275-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Di Iorio BR, Bellizzi V, Bellasi A, et al. Phosphate attenuates the anti-proteinuric effect of very low-protein diet in CKD patients. Nephrol Dial Transplant. 2013;28:632–640. doi: 10.1093/ndt/gfs477. [DOI] [PubMed] [Google Scholar]
- 71.Khoueiry G, Waked A, Goldman M, et al. Dietary intake in hemodialysis patients does not reflect a heart healthy diet. J Ren Nutr. 2011;21:438–447. doi: 10.1053/j.jrn.2010.09.001. [DOI] [PubMed] [Google Scholar]
- 72.Ahmadi SF, Zahmatkesh G, Ahmadi E, et al. Association of Body Mass Index with Clinical Outcomes in Non-Dialysis-Dependent Chronic Kidney Disease: A Systematic Review and Meta-Analysis. Cardiorenal Med. 2015;6:37–49. doi: 10.1159/000437277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Wang J, Streja E, Rhee CM, et al. Lean Body Mass and Survival in Hemodialysis Patients and the Roles of Race and Ethnicity. J Ren Nutr. 2016;26:26–37. doi: 10.1053/j.jrn.2015.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Carrero JJ, Chen J, Kovesdy CP, et al. Critical appraisal of biomarkers of dietary intake and nutritional status in patients undergoing dialysis. Semin Dial. 2014;27:586–589. doi: 10.1111/sdi.12283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Lukowsky LR, Kheifets L, Arah OA, et al. Nutritional predictors of early mortality in incident hemodialysis patients. Int Urol Nephrol. 2014;46:129–140. doi: 10.1007/s11255-013-0459-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Kim Y, Molnar MZ, Rattanasompattikul M, et al. Relative contributions of inflammation and inadequate protein intake to hypoalbuminemia in patients on maintenance hemodialysis. Int Urol Nephrol. 2013;45:215–227. doi: 10.1007/s11255-012-0170-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ikizler TA, Cano NJ, Franch H, et al. Prevention and treatment of protein energy wasting in chronic kidney disease patients: a consensus statement by the International Society of Renal Nutrition and Metabolism. Kidney Int. 2013;84:1096–1107. doi: 10.1038/ki.2013.147. [DOI] [PubMed] [Google Scholar]
- 78.Ravel VA, Molnar MZ, Streja E, et al. Low protein nitrogen appearance as a surrogate of low dietary protein intake is associated with higher all-cause mortality in maintenance hemodialysis patients. J Nutr. 2013;143:1084–1092. doi: 10.3945/jn.112.169722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Rhee CM, Ahmadi SF, Kalantar-Zadeh K. The dual roles of obesity in chronic kidney disease: a review of the current literature. Curr Opin Nephrol Hypertens. 2016;25:208–216. doi: 10.1097/MNH.0000000000000212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *80.Kalantar-Zadeh K, Tortorici AR, Chen JL, et al. Dietary restrictions in dialysis patients: is there anything left to eat? Semin Dial. 2015;28:159–168. doi: 10.1111/sdi.12348. This review suggested careful modulation on diet restriction in dialysis patients to avoid PEW and to achieve better outcome. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kalantar-Zadeh K, Cano NJ, Budde K, et al. Diets and enteral supplements for improving outcomes in chronic kidney disease. Nat Rev Nephrol. 2011;7:369–384. doi: 10.1038/nrneph.2011.60. [DOI] [PMC free article] [PubMed] [Google Scholar]