Abstract
Introduction
This is the 2016 Annual Report of the University of Kansas Health System Poison Control Center (PCC). The PCC is one of 55 certified poison control centers in the United States and serves the state of Kansas 24-hours a day, 365 days a year, with certified specialists in poison information and medical toxicologists. The PCC receives calls from the public, law enforcement, health care professionals, and public health agencies. All calls to the PCC are recorded electronically in the Toxicall® data management system and uploaded in near real-time to the National Poison Data System (NPDS), which is the data repository for all poison control centers in the United States.
Methods
All encounters reported to the PCC from January 1, 2016 to December 31, 2016 were analyzed. Data recorded for each exposure includes caller location, age, weight, gender, substance exposed to, nature of exposure, route of exposure, interventions, medical outcome, disposition and location of care. Encounters were classified further as human exposure, animal exposure, confirmed non-exposure, or information call (no exposure reported).
Results
The PCC logged 21,965 total encounters in 2016, including 20,713 human exposure cases. The PCC received calls from every county in Kansas. The majority of human exposure cases (50.4%, n = 10,174) were female. Approximately 67% (n = 13,903) of human exposures involved a child (defined as age 19 years or less). Most encounters occurred at a residence (94.0%, n = 19,476) and most calls (72.3%, n = 14,964) originated from a residence. The majority of human exposures (n = 18,233) were acute cases (exposures occurring over eight hours or less). Ingestion was the most common route of exposure documented (86.3%, n = 17,882). The most common reported substance in pediatric encounters was cosmetics/personal care products (n = 1,362), followed by household cleaning product (n = 1,301). For adult encounters, sedatives/hypnotics/antipsychotics (n = 1,130) and analgesics (n = 1,103) were the most frequently involved substances. Unintentional exposures were the most common reason for exposures (81.3%, n = 16,836). Most encounters (71.1%, n = 14,732) were managed in a non-healthcare facility (i.e., a residence). Among human exposures, 14,679 involved exposures to pharmaceutical agents while 10,176 involved exposure to non-pharmaceuticals. Medical outcomes were 32% (n = 6,582) no effect, 19% (n = 3,911) minor effect, 8% (n = 1,623) moderate effect, and 2% (n = 348) major effects. There were 15 deaths in 2016 reported to the PCC. Number of exposures, calls from healthcare facilities, cases with moderate or major medical outcomes, and deaths all increased in 2016 compared to 2015.
Conclusion
The results of the 2016 University of Kansas Health System Poison Control annual report demonstrates that the center receives calls from the entire state of Kansas totaling over 20,000 human exposures per year. While pediatric exposures remain the most common, there is an increasing number of calls from healthcare facilities and for cases with serious outcomes. The experience of the PCC is similar to national data. This report supports the continued value of the PCC to both public and acute health care in the state of Kansas.
Keywords: drug overdose, poisoning, ingestion, toxicology
Introduction
This is the 2016 Annual Report of University of Kansas Health System Poison Control Center (PCC). The PCC is a 24-hour 365 day/year health care information resource serving the state of Kansas. It was founded in 1982 and is certified with the American Association of Poison Control Centers (AAPCC). Currently, there are 55 certified poison control centers in the United States. The PCC is staffed by 10 certified specialists in poison information who are either critical care trained nurses or doctors of pharmacy. There is 24-hour back up provided by board certified medical toxicologists. The PCC receives calls from the public, law enforcement, health care professionals, and public health agencies. Encounters may involve an exposed animal or human (Exposure Call) or a request for information with no known exposure (Information Call). The PCC follows all cases to make management recommendations, monitor case progress, and document medical outcome. This information is recorded electronically in the Toxicall® data management system and uploaded in near real-time to the National Poison Data System (NPDS). NPDS is the data warehouse for all of the nation’s poison control centers.1 The NPDS utilizes a products database that contains over 427,000 products to classify exposures. The database is maintained and updated continuously by data analysts at the Micromedex Poisindex® System.1 The average time to upload data for all PCs is 9.52 minutes, creating a real-time national exposure database and surveillance system.1 The PCC has the ability to share NPDS real time surveillance with state and local health departments and other regulatory agencies. What follows is analysis and summary of all encounters reported to the PCC from January 1, 2016 to December 31, 2016.
Methods
All PCC encounters recorded electronically in the Toxicall® data management system from January 1, 2016 to December 31, 2016 were analyzed. Cases were first classified as either an exposure or suspected exposure (Human Exposure, Animal Exposure, Non-Exposure Confirmed Cases) or a request for information with no reported exposure (Information Call). Data extracted includes caller location, age, weight, gender, exposure substance, number of follow-up calls, and nature of exposure (i.e., unintentional, recreational, or intentional). Additional data collected included exposure scenario, route of exposure (oral, dermal, parenteral), interventions, medical outcome (no effect, minor, moderate, severe, or death), disposition (admitted to noncritical care unit, admitted to critical care unit, admitted to psychiatry unit, lost to follow-up, or treated and released) and location of care (non-health care facility or health care facility). For this analysis, a pediatric case was defined as any patient 19 years of age or less. This is consistent with NPDS methodology. For medical outcome, the following definitions were used: minor - minimally bothersome symptoms, moderate - more pronounced symptoms, usually requiring treatment, and major life threatening signs and symptoms.
Data were analyzed using Microsoft Excel (Microsoft Corp, Redmond, WA).
Results
The PCC logged 21,965 total calls in 2016, including 20,713 human exposure cases, 87 non-exposure confirmed cases, 112 animal exposure cases, and 1,053 information calls. For information calls, drug information (n = 308) was most common reason for calling. Table 1 further describes the encounter types. The PCC made 32,137 follow-up calls in 2016. Follow-up calls were done in 60.9% of human exposure cases. One follow-up call was made in 29.5% of human exposure cases and multiple follow-up calls (range 2 – 44) were made in 31.3% of cases. In human exposure calls for which follow-up calls were made, an average of 2.54 follow-up calls per case were performed.
Table 1.
Encounter type.
| Number | % | |
|---|---|---|
| Exposure | ||
| Human Exposure | 20,713 | 94.32 |
| Animal Exposure | 112 | 0.51 |
| Subtotal | 20,825 | 94.83 |
| Non-Exposure Confirmed Cases | ||
| Human Non-Exposure | 87 | 0.39 |
| Subtotal | 87 | 0.39 |
| Information Call | ||
| Drug information | 308 | 1.40 |
| Drug identification | 189 | 0.86 |
| Environmental information | 123 | 0.56 |
| Medical information | 30 | 0.14 |
| Occupational information | 1 | 0.00 |
| Poison information | 110 | 0.50 |
| Prevention / Safety / Education | 30 | 0.14 |
| Teratogenicity information | 1 | 0.00 |
| Other information | 49 | 0.22 |
| Substance Abuse | 6 | 0.03 |
| Administrative | 16 | 0.07 |
| Caller Referred | 190 | 0.86 |
| Subtotal | 1,053 | 4.78 |
| Total | 21,965 | 100.00 |
The PCC received calls from all 105 counties in Kansas. The county with the most number of calls was Sedgwick County with 3,358. In addition, calls were received from 47 states, the District of Columbia, and 12 calls were from foreign countries, including Turkey and Uganda.
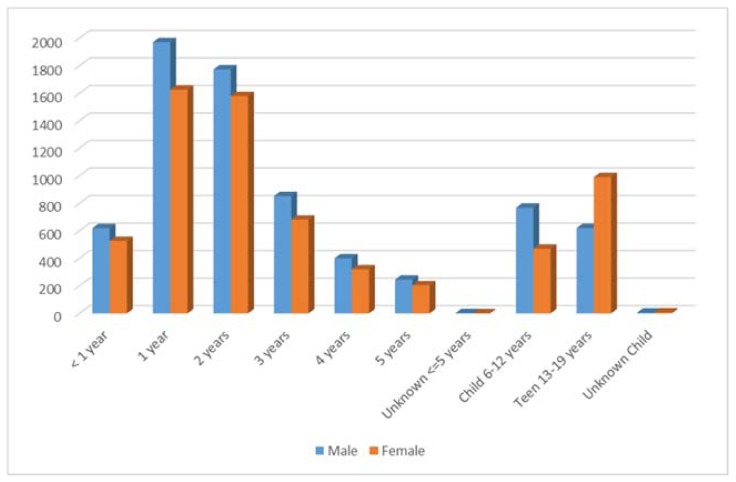
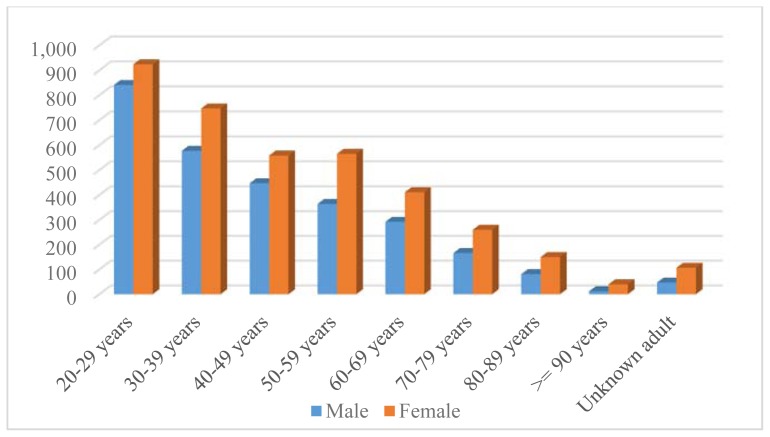
The majority of human exposure cases (50.4%, n = 10,174) were female. A male predominance was found among encounters involving children younger than 13 years of age, but this gender distribution was reversed in teenagers and adults, with females comprising the majority of reported exposures. Approximately 67% (n = 13,903) of human exposures involved a child (defined as age 19 years or less). Table 2 illustrates distribution of human exposures by age and gender. Figure 1 demonstrates that patients 1 year of age were the most common age group involved in encounters reported to the PCC. For adults, the age group of 20 – 29 years old was encountered most commonly (Figure 2). Seventy-five (75) exposures occurred in pregnant women (0.4% of all human exposures). Of these exposures, 26.7% occurred in the first trimester, 42.7% occurred in the second trimester, and 28.0% occurred in the third trimester. Most of these exposures (78.7%) were unintentional exposures and 12.0% were intentional exposures. There were no reported deaths to PCC in pregnant women in 2016.
Table 2.
Distribution of human exposures by age and gender.
| Male | Female | Unknown gender | Total | Cumulative Total | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Age (yrs) | N | % of age group total | N | % of age group total | N | % of age group total | N | % of total exposure | N | % |
| < 1 year | 619 | 52.32 | 526 | 47.73 | 1 | 0.09 | 1,183 | 5.71 | 1,183 | 5.71 |
| 1 year | 1,971 | 53.26 | 1,626 | 46.50 | 2 | 0.06 | 3,701 | 17.87 | 4,884 | 23.58 |
| 2 years | 1,773 | 52.39 | 1,579 | 46.30 | 1 | 0.03 | 3,384 | 16.34 | 8,268 | 39.92 |
| 3 years | 852 | 55.32 | 681 | 45.49 | 3 | 0.20 | 1,540 | 7.43 | 9,808 | 47.35 |
| 4 years | 400 | 58.48 | 320 | 44.02 | 2 | 0.28 | 684 | 3.30 | 10,492 | 50.65 |
| 5 years | 245 | 56.71 | 204 | 47.11 | 0 | 0.00 | 432 | 2.09 | 10,924 | 52.74 |
| Unknown ≤ 5 years | 2 | 33.33 | 0 | 0.00 | 0 | 0.00 | 6 | 0.03 | 10,930 | 52.77 |
| Child 6–12 years | 768 | 61.89 | 470 | 39.83 | 1 | 0.08 | 1,241 | 5.99 | 12,171 | 58.76 |
| Teen 13–19 years | 620 | 35.98 | 990 | 62.15 | 2 | 0.13 | 1,723 | 8.32 | 13,894 | 67.08 |
| Unknown Child | 5 | 55.56 | 7 | 46.67 | 0 | 0.00 | 9 | 0.04 | 13,903 | 67.12 |
| Subtotal | 7,255 | 52.18 | 6,403 | 47.58 | 12 | 0.09 | 13,903 | 67.12 | 13,903 | 67.12 |
| 20–29 years | 841 | 47.30 | 924 | 52.77 | 1 | 0.06 | 1,778 | 8.58 | 15,681 | 75.71 |
| 30–39 years | 577 | 41.72 | 747 | 56.12 | 2 | 0.15 | 1,383 | 6.68 | 17,064 | 82.38 |
| 40–49 years | 447 | 42.53 | 558 | 56.94 | 3 | 0.31 | 1,051 | 5.07 | 18,115 | 87.46 |
| 50–59 years | 364 | 40.40 | 565 | 57.77 | 0 | 0.00 | 901 | 4.35 | 19,016 | 91.81 |
| 60–69 years | 292 | 39.25 | 411 | 57.97 | 1 | 0.14 | 744 | 3.59 | 19,760 | 95.40 |
| 70–79 years | 166 | 37.22 | 260 | 59.50 | 1 | 0.23 | 446 | 2.15 | 20,206 | 97.55 |
| 80–89 years | 81 | 33.20 | 150 | 64.94 | 1 | 0.43 | 244 | 1.18 | 20,450 | 98.73 |
| ≥ 90 years | 12 | 32.43 | 40 | 67.80 | 0 | 0.00 | 37 | 0.18 | 20,487 | 98.91 |
| Unknown adult | 47 | 36.43 | 107 | 66.88 | 1 | 0.63 | 129 | 0.62 | 20,616 | 99.53 |
| Subtotal | 2,827 | 42.11 | 3,762 | 56.69 | 10 | 0.15 | 6,713 | 32.41 | 20,616 | 99.53 |
| Total* | 10,096 | 48.74 | 10,174 | 50.59 | 26 | 0.13 | 20,713 | 100.00 | 20,713 | 100.00 |
Total includes 97 unknown age cases.
Figure 1.
Distribution of human exposures by gender in children < 19 years old.
Figure 2.
Distribution of human exposures by gender, adults > 20 years old.
For human exposures, 72.3% (n = 14,964) of calls originated from a residence (own or other), while 94.0% (n = 19,476) of these exposures actually occurred at a residence (own or other). Calls from a health care facility accounted for 21.7% (n = 4,500) of human exposure encounters. Table 3 further details the origin of human exposure calls and where the exposure took place.
Table 3.
Origin of call and site exposure for human exposure cases.
| Site | Origin of Call | Site of Exposure | ||
|---|---|---|---|---|
| N | % | N | % | |
| Residence | ||||
| Own | 14,583 | 70.41 | 18,708 | 90.32 |
| Other | 381 | 1.84 | 768 | 3.71 |
| Workplace | 324 | 1.56 | 395 | 1.91 |
| Health care facility | 4,500 | 21.73 | 71 | 0.34 |
| School | 54 | 0.26 | 242 | 1.17 |
| Restaurant / Food service | 8 | 0.04 | 30 | 0.14 |
| Public area | 63 | 0.30 | 181 | 0.87 |
| Other | 775 | 3.74 | 164 | 0.79 |
| Unknown | 25 | 0.12 | 154 | 0.74 |
The majority of human exposures (n = 18,233) were acute cases (exposures occurring over eight hours or less). Chronic exposures (exposures occurring > 8 hours) accounted for 1.6% (327) of all human exposures reported. Acute on chronic exposures (single exposure that was preceded by a chronic exposure > 8 hours) totaled 2063 (9.96%). Ingestion was the most common route of exposure documented (86.3%, n = 17,882) in all cases (Table 4).
Table 4.
Route of human exposures.
| Human exposures | |||
|---|---|---|---|
| Route | N | % of All Routes | % of All Cases |
| Ingestion | 17,882 | 82.44 | 86.33 |
| Dermal | 1,312 | 6.05 | 6.33 |
| Inhalation/nasal | 1,095 | 5.05 | 5.29 |
| Ocular | 855 | 3.94 | 4.13 |
| Bite/sting | 215 | 0.99 | 1.04 |
| Unknown | 157 | 0.72 | 0.76 |
| Parenteral | 115 | 0.53 | 0.56 |
| Other | 25 | 0.12 | 0.12 |
| Otic | 17 | 0.08 | 0.08 |
| Rectal | 8 | 0.04 | 0.04 |
| Aspiration (with ingestion) | 5 | 0.02 | 0.02 |
| Vaginal | 5 | 0.02 | 0.02 |
| Total Number of Routes | 21,691 | 100.00 | 104.72* |
Some cases may have multiple routes of exposure documented.
The most common reported substance in those less than 5 years of age was cosmetics/personal care products (n = 1,362) followed closely by household cleaning products (n = 1,301). For adult (> 20 years of age) encounters, sedatives/hypnotics/antipsychotics (n = 1,130) and analgesics (n = 1,103) were the most frequently involved substances. Among all encounters, analgesics (n = 2,813, 11%) were the most frequently encountered substance category. Table 5 lists most frequently encountered substance categories for pediatric encounters and Table 6 lists those for adult encounters. [A summary log for all exposures categorized by category and sub-category of substance is available with the manuscript on the website: kjm.kumc.edu].
Table 5.
Substance categories most frequently involved in exposures for age ≤ 5 years old.
| Substance category | All Substance | % | Single substance exposures | % |
|---|---|---|---|---|
| Cosmetics/Personal Care Products | 1,362 | 11.89 | 1,333 | 12.62 |
| Cleaning Substances (Household) | 1,301 | 11.36 | 1,259 | 11.92 |
| Analgesics | 1,073 | 9.37 | 966 | 9.14 |
| Foreign Bodies/Toys/Miscellaneous | 610 | 5.32 | 589 | 5.57 |
| Antihistamines | 590 | 5.15 | 537 | 5.08 |
| Topical Preparations | 577 | 5.04 | 572 | 5.41 |
| Vitamins | 510 | 4.45 | 466 | 4.41 |
| Dietary Supplements/ Herbals/ Homeopathic | 430 | 3.75 | 401 | 3.80 |
| Pesticides | 418 | 3.65 | 408 | 3.86 |
| Plants | 282 | 2.46 | 260 | 2.46 |
| Gastrointestinal Preparations | 276 | 2.41 | 246 | 2.33 |
| Cold and Cough Preparations | 250 | 2.18 | 228 | 2.16 |
| Antimicrobials | 241 | 2.10 | 213 | 2.02 |
| Hormones and Hormone Antagonists | 227 | 1.98 | 157 | 1.49 |
| Cardiovascular Drugs | 213 | 1.86 | 131 | 1.24 |
Table 6.
Substance categories most frequently involved in exposures of adults (> 20 years old).
| Substance category | All substances | % | Single substance exposures | % |
|---|---|---|---|---|
| Sedative/Hypnotics/Antipsychotics | 1,130 | 11.65 | 319 | 6.14 |
| Analgesics | 1,103 | 11.37 | 508 | 9.77 |
| Antidepressants | 786 | 8.10 | 248 | 4.77 |
| Cardiovascular Drugs | 654 | 6.74 | 223 | 4.29 |
| Pesticides | 434 | 4.47 | 378 | 7.27 |
| Cleaning Substances (Household) | 405 | 4.18 | 314 | 6.04 |
| Alcohols | 403 | 4.15 | 55 | 1.06 |
| Anticonvulsants | 378 | 3.90 | 111 | 2.14 |
| Antihistamines | 333 | 3.43 | 151 | 2.91 |
| Hormones and Hormone Antagonists | 272 | 2.80 | 135 | 2.60 |
| Stimulants and Street Drugs | 267 | 2.75 | 116 | 2.23 |
| Chemicals | 233 | 2.40 | 205 | 3.94 |
| Cosmetics/Personal Care Products | 210 | 2.16 | 188 | 3.62 |
| Cold and Cough Preparations | 197 | 2.03 | 101 | 1.94 |
| Muscle Relaxants | 190 | 1.96 | 67 | 1.29 |
There were a total of 399 plant exposures reported to the PCC. The most common plant exposure encountered was to pokeweed (Phytolacca Americana; n = 48). Table 7 lists the top 5 most encountered plants.
Table 7.
Top five most frequent plant exposures.
| Botanical Name or Category | N |
|---|---|
| Phytolacca americana (L.) (Pokeweed) | 48 |
| Plants: Unknown Toxic Types or Unknown if Toxic | 46 |
| Spathiphyllum species (Peace Lily) | 14 |
| Philodendron (Species unspecified) | 16 |
| Cherry (Species unspecified) | 12 |
Unintentional exposures were the most common reason for exposures (81.3%, n = 16,836) while intentional exposures accounted for 16.3% (n = 3,377) of exposures. Table 8 lists reasons for human exposures. A majority of unintentional exposures (n = 10,897) occurred in the less than 5 years old age group. Up to age 12, 98.9% (n = 12,171) of ingestions were unintentional. However, in the 13 – 19 year-old group, intentional exposure was most common (63.1%, n = 1,087). In total, suspected suicide attempts accounted for 11.7% (n = 2,415) of human encounters. When a therapeutic error was the reason for exposure, a double dose was the most common scenario (n = 775).
Table 8.
Reason for human exposure cases.
| Reason | N | % Human exposures | |
|---|---|---|---|
| Unintentional | |||
| Unintentional - General | 11,971 | 57.8 | |
| Unintentional - Therapeutic error | 2,361 | 11.4 | |
| Unintentional - Misuse | 1,226 | 5.9 | |
| Unintentional - Environmental | 625 | 3.0 | |
| Unintentional - Occupational | 238 | 1.1 | |
| Unintentional - Bite / sting | 217 | 1.0 | |
| Unintentional - Food poisoning | 160 | 0.8 | |
| Unintentional - Unknown | 38 | 0.2 | |
| Subtotal | 16,836 | 81.3 | |
| Intentional | |||
| Intentional - Suspected suicide | 2,415 | 11.7 | |
| Intentional - Misuse | 527 | 2.5 | |
| Intentional - Abuse | 348 | 1.7 | |
| Intentional - Unknown | 87 | 0.4 | |
| Subtotal | 3,377 | 16.3 | |
| Adverse Reaction | |||
| Adverse reaction - Drug | 286 | 1.4 | |
| Adverse reaction - Other | 44 | 0.2 | |
| Adverse reaction - Food | 29 | 0.1 | |
| Subtotal | 359 | 1.7 | |
| Unknown | |||
| Unknown reason | 77 | 0.4 | |
| Subtotal | 77 | 0.4 | |
| Other | |||
| Other - Malicious | 43 | 0.2 | |
| Other - Contamination / Tampering | 15 | 0.1 | |
| Other - Withdrawal | 6 | 0.0 | |
| Subtotal | 64 | 0.3 | |
| Total | 20,713 | 100.0 | |
Most encounters (71.1%, n = 14,732) were managed in a non-health care facility (i.e., a residence). Of the 5,747 encounters managed at a health care facility, 42% (n = 2419) were admitted. Table 9 lists the management site of all human encounters.
Table 9.
Management site of human exposures.
| Site of management | N | % |
|---|---|---|
| Managed in healthcare facility | ||
| Treated/evaluated and released | 3,153 | 15.2 |
| Admitted to critical care unit | 1,281 | 6.2 |
| Admitted to noncritical care unit | 721 | 3.5 |
| Admitted to psychiatric facility | 417 | 2.0 |
| Patient lost to follow-up / left AMA | 175 | 0.8 |
| Subtotal (managed in HCF) | 5,747 | 27.8 |
| Managed on site, non-health care facility | 14,732 | 71.1 |
| Other | 19 | 0.1 |
| Refused referral | 197 | 1.0 |
| Unknown | 18 | 0.1 |
| Total | 20,713 | 100.0 |
Among human exposures, 14,679 involved exposures to pharmaceutical agents, while 10,176 involved exposure to non-pharmaceuticals. Because an encounter could include both a pharmaceutical agent and non-pharmaceutical agent, this total is greater than the total number of encounters. However, 88.5% (n = 18,327) of all human exposures were exposed to only a single substance. Among these single substance exposures, the reason for exposure was intentional in 19.3% (n = 3,527) of pharmaceutical-only cases compared to 3.5% (n = 641) of non-pharmaceutical single substance exposures.
When medical outcomes were analyzed, 32% (n = 6,582) of human exposures had no effect, 19% (n = 3,911) had minor effect, 8% (n = 1,623) had moderate effect, and 2% (n = 348) major effects. Moderate and major effects were more common in those over 20 years of age and in those with intentional encounters. More serious outcomes were related to single-substance pharmaceutical exposures, accounting for 66.7% (n = 10) of the fatalities. Table 10 lists all medical outcomes by age and Table 11 lists them by reason for exposure.
Table 10.
Medical outcome of human exposure cases by patient age.
| ≤ 5 yrs | 6–12 yrs | 13–19 yrs | ≥ 20 yrs | Unknown child | Unknown adult | Unknown age | Total | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Outcome | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % |
| No effect | 4,515 | 41.31 | 386 | 31.10 | 426 | 24.72 | 1,244 | 18.89 | 0 | 0.00 | 9 | 6.98 | 2 | 2.1 | 6,582 | 31.78 |
| Minor effect | 1,268 | 11.60 | 245 | 19.74 | 560 | 32.50 | 1,805 | 27.41 | 1 | 11.11 | 27 | 20.93 | 5 | 5.2 | 3,911 | 18.88 |
| Moderate effect | 92 | 0.84 | 39 | 3.14 | 309 | 17.93 | 1,112 | 16.89 | 0 | 0.00 | 2 | 1.55 | 69 | 71.1 | 1,623 | 7.84 |
| Major effect | 10 | 0.09 | 4 | 0.32 | 66 | 3.83 | 268 | 4.07 | 0 | 0.00 | 0 | 0.00 | 0 | 0.0 | 348 | 1.68 |
| Death | 0 | 0.00 | 0 | 0.00 | 1 | 0.06 | 12 | 0.18 | 0 | 0.00 | 0 | 0.00 | 0 | 0.0 | 13 | 0.06 |
| No follow-up, nontoxic | 435 | 3.98 | 31 | 2.50 | 10 | 0.58 | 39 | 0.59 | 0 | 0.00 | 2 | 1.55 | 1 | 1.0 | 518 | 2.50 |
| No follow-up, minimal toxicity | 4,305 | 39.39 | 504 | 40.61 | 242 | 14.05 | 1,542 | 23.42 | 4 | 44.44 | 53 | 41.09 | 8 | 8.3 | 6,658 | 32.14 |
| No follow-up, potentially toxic | 207 | 1.89 | 16 | 1.29 | 73 | 4.24 | 281 | 4.27 | 3 | 33.33 | 24 | 18.60 | 10 | 10.3 | 614 | 2.96 |
| Unrelated effect | 98 | 0.90 | 16 | 1.29 | 36 | 2.09 | 279 | 4.24 | 1 | 11.11 | 12 | 9.30 | 2 | 2.1 | 444 | 2.14 |
| Death, indirect report | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 | 2 | 0.03 | 0 | 0.00 | 0 | 0.00 | 0 | 0.0 | 2 | 0.01 |
| Total | 10,930 | 100.00 | 1,241 | 100.00 | 1,723 | 100.00 | 6,584 | 100.00 | 9 | 100.00 | 129 | 100.00 | 97 | 100.00 | 20,713 | 100.00 |
Table 11.
Medical outcome by reason for exposure in human exposures.
| Unintentional | Intentional | Other | Adverse reaction | Unknown | Total | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Outcome | N | % | N | % | N | % | N | % | N | % | N | % |
| Death | 0 | 0.00 | 13 | 0.38 | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 | 13 | 0.06 |
| Death, indirect report | 0 | 0.00 | 1 | 0.03 | 0 | 0.00 | 0 | 0.00 | 1 | 1.30 | 2 | 0.01 |
| Major effect | 53 | 0.31 | 273 | 8.08 | 0 | 0.00 | 9 | 2.51 | 13 | 16.88 | 348 | 1.68 |
| Minor effect | 2,746 | 16.31 | 1,012 | 29.97 | 19 | 29.69 | 121 | 33.70 | 13 | 16.88 | 3,911 | 18.88 |
| Moderate effect | 574 | 3.41 | 978 | 28.96 | 5 | 7.81 | 46 | 12.81 | 20 | 25.97 | 1,623 | 7.84 |
| No effect | 5,836 | 34.66 | 720 | 21.32 | 7 | 10.94 | 14 | 3.90 | 5 | 6.49 | 6,582 | 31.78 |
| No follow-up, nontoxic | 512 | 3.04 | 4 | 0.12 | 1 | 1.56 | 1 | 0.28 | 0 | 0.00 | 518 | 2.50 |
| No follow-up, minimal toxicity | 6,399 | 38.01 | 146 | 4.32 | 17 | 26.56 | 92 | 25.63 | 4 | 5.19 | 6,658 | 32.14 |
| No follow-up, potentially toxic | 391 | 2.32 | 189 | 5.60 | 7 | 10.94 | 16 | 4.46 | 11 | 14.29 | 614 | 2.96 |
| Unrelated effect | 325 | 1.93 | 41 | 1.21 | 8 | 12.50 | 60 | 16.71 | 10 | 12.99 | 444 | 2.14 |
| Total | 16,836 | 100.00 | 3,377 | 100.00 | 64 | 100.00 | 359 | 100.00 | 77 | 100.00 | 20,713 | 100.00 |
Use of decontamination and specific therapies, including antidotal therapy, is detailed in Tables 12a and 12b.
Table 12a.
Decontamination provided in human exposures by age.
| Decontamination | ≤ 5 yrs | 6–12 yrs | 13–19 yrs | ≥ 20 yrs | Unknown child | Unknown adult | Unknown age | Total |
|---|---|---|---|---|---|---|---|---|
| Cathartic | 2 | 3 | 40 | 46 | 0 | 0 | 0 | 91 |
| Charcoal, multiple doses | 1 | 2 | 9 | 5 | 0 | 0 | 0 | 17 |
| Charcoal, single dose | 87 | 14 | 176 | 202 | 0 | 0 | 0 | 479 |
| Dilute/irrigate/wash | 8,317 | 796 | 445 | 2,649 | 7 | 58 | 3 | 12,275 |
| Food/snack | 1,516 | 142 | 83 | 369 | 0 | 3 | 1 | 2,114 |
| Fresh air | 67 | 35 | 37 | 403 | 3 | 26 | 3 | 574 |
| Lavage | 0 | 0 | 1 | 6 | 0 | 0 | 0 | 7 |
| Other emetic | 57 | 6 | 4 | 39 | 0 | 1 | 0 | 107 |
| Whole bowel irrigation | 0 | 0 | 1 | 8 | 0 | 0 | 0 | 9 |
Table 12b.
Therapy provided in human exposures by age.
| Therapy | ≤ 5 yrs | 6–12 yrs | 13–19 yrs | ≥ 20 yrs | Unknown child | Unknown adult | Unknown age | Total |
|---|---|---|---|---|---|---|---|---|
| Alkalinization | 4 | 2 | 39 | 143 | 0 | 0 | 0 | 188 |
| Antiarrhythmic | 0 | 1 | 0 | 5 | 0 | 0 | 0 | 6 |
| Antibiotics | 27 | 10 | 19 | 185 | 0 | 2 | 0 | 243 |
| Anticonvulsants | 0 | 0 | 2 | 5 | 0 | 0 | 0 | 7 |
| Antiemetics | 16 | 9 | 128 | 177 | 0 | 0 | 0 | 330 |
| Antihistamines | 19 | 8 | 21 | 86 | 0 | 0 | 1 | 135 |
| Antihypertensives | 0 | 0 | 1 | 18 | 0 | 0 | 0 | 19 |
| Antivenin (fab fragment) | 1 | 1 | 2 | 8 | 0 | 0 | 0 | 12 |
| Antivenin/antitoxin | 0 | 1 | 4 | 10 | 0 | 0 | 0 | 15 |
| Atropine | 0 | 1 | 1 | 12 | 0 | 0 | 0 | 14 |
| Benzodiazepines | 17 | 7 | 93 | 270 | 0 | 0 | 0 | 387 |
| Bronchodilators | 2 | 5 | 2 | 48 | 0 | 2 | 69 | 128 |
| Calcium | 164 | 8 | 3 | 31 | 0 | 0 | 0 | 206 |
| CPR | 0 | 0 | 2 | 7 | 0 | 0 | 0 | 9 |
| Deferoxamine | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 2 |
| Ethanol | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 1 |
| Extracorp. procedure (other) | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 1 |
| Fab fragments | 0 | 0 | 0 | 8 | 0 | 0 | 0 | 8 |
| Fluids, IV | 57 | 23 | 490 | 1,313 | 0 | 1 | 1 | 1,885 |
| Flumazenil | 0 | 1 | 6 | 33 | 0 | 0 | 0 | 40 |
| Fomepizole | 4 | 0 | 2 | 15 | 0 | 0 | 0 | 21 |
| Glucagon | 1 | 0 | 4 | 25 | 0 | 0 | 0 | 30 |
| Glucose, > 5% | 4 | 0 | 1 | 42 | 0 | 0 | 0 | 47 |
| Hemodialysis | 0 | 0 | 3 | 21 | 0 | 0 | 0 | 24 |
| Hydroxocobalamin | 3 | 1 | 0 | 1 | 0 | 0 | 0 | 5 |
| Hyperbaric oxygen | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 2 |
| Insulin | 0 | 0 | 1 | 23 | 0 | 0 | 0 | 24 |
| Intubation | 3 | 3 | 27 | 153 | 0 | 0 | 0 | 186 |
| Methylene blue | 0 | 0 | 0 | 3 | 0 | 0 | 0 | 3 |
| NAC, IV | 1 | 0 | 63 | 105 | 0 | 0 | 0 | 169 |
| NAC, PO | 1 | 1 | 14 | 19 | 0 | 0 | 0 | 35 |
| Naloxone | 5 | 1 | 23 | 131 | 0 | 0 | 0 | 160 |
| Neuromuscular blocker | 2 | 0 | 0 | 6 | 0 | 0 | 0 | 8 |
| Octreotide | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| Other | 55 | 16 | 99 | 357 | 2 | 3 | 0 | 532 |
| Oxygen | 9 | 8 | 56 | 379 | 0 | 0 | 69 | 521 |
| Physostigmine | 0 | 0 | 4 | 9 | 0 | 0 | 0 | 13 |
| Phytonadione | 0 | 0 | 1 | 12 | 0 | 0 | 0 | 13 |
| Sedation (other) | 6 | 5 | 26 | 136 | 0 | 0 | 0 | 173 |
| Sodium thiosulfate | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| Steroids | 8 | 2 | 7 | 77 | 0 | 1 | 69 | 164 |
| Vasopressors | 0 | 1 | 8 | 65 | 0 | 0 | 0 | 74 |
| Ventilator | 3 | 3 | 27 | 155 | 0 | 0 | 0 | 188 |
There were 15 deaths in 2016 reported to the PCC. Fourteen of the deaths involved patients 20 years of age or older. Fourteen of the death cases involved intentional exposures. Table 13 details the 15 reported deaths.
Table 13.
Details on deaths and exposure related fatalities.
| Age & Gender | Substances | Substance Rank | Cause Rank | Chronicity | Route | Reason |
|---|---|---|---|---|---|---|
| NON-PHARMACEUTICAL EXPOSURES | ||||||
| Fumes/Gases/Vapors | ||||||
| 17 year Male | Carbon Monoxide | 1 | 1 | Acute | Inhal | Int-S |
| Heavy Metals | ||||||
| 68 year Female | Copper | 1 | 1 | Acute | Ingst | Int-S |
| PHARMACEUTICAL EXPOSURES | ||||||
| Analgesics | ||||||
| 73 year Male | Acetaminophen/Hydrocodone | 1 | 1 | Acute on Chronic | Ingst | Int-S |
| Zolpidem | 2 | 2 | Acute on Chronic | Ingst | ||
| Antihistamines | ||||||
| 38 year Female | Diphenhydramine | 1 | 1 | Acute | Ingst | Int-S |
| Cardiovascular Drugs | ||||||
| 21 year Female | Labetalol | 1 | 1 | Unknown | Ingst | Int-S |
| Clonazepam | 2 | 2 | Unknown | Ingst | ||
| 45 year Female | Propranolol | 1 | 1 | Acute | Ingst | Int-S |
| Valproic Acid | 2 | 2 | Acute | Ingst | ||
| Olanzapine | 3 | 3 | Acute | Ingst | ||
| Bupropion | 4 | 4 | Acute | Ingst | ||
| 46 year Male | Amlodipine | 1 | 1 | Acute on Chronic | Ingst | Int-S |
| Lamotrigine | 2 | 2 | Acute on Chronic | Ingst | ||
| Metformin | 3 | 3 | Acute on Chronic | Ingst | ||
| Citalopram | 4 | 4 | Acute on Chronic | Ingst | ||
| Fenobibrate | 5 | 5 | Acute on Chronic | Ingst | ||
| Alpha Blocker | 6 | 6 | Acute on Chronic | Ingst | ||
| Quetiapine | 7 | 7 | Acute on Chronic | Ingst | ||
| Lisinopril | 8 | 8 | Acute on Chronic | Ingst | ||
| Bupropion (Extended Release) | 9 | 9 | Acute on Chronic | Ingst | ||
| Ethanol | 10 | 10 | Acute on Chronic | Ingst | ||
| 46 year Female | Propranolol | 1 | 1 | Acute | Ingst | Int-S |
| Trazodone | 2 | 2 | Acute | Ingst | ||
| Paroxetine | 3 | 3 | Acute | Ingst | ||
| 60 year Male | Carvedilol | 1 | 1 | Acute on Chronic | Ingst | Int-S |
| Amlodipine | 2 | 2 | Acute on Chronic | Ingst | ||
| Hydrochlorothiazide/ Lisinopril | 3 | 3 | Acute on Chronic | Ingst | ||
| Clopidogrel | 4 | 4 | Acute on Chronic | Ingst | ||
| Duloxetine | 5 | 5 | Acute on Chronic | Ingst | ||
| Acetaminophen/ Hydrocodone | 6 | 6 | Acute on Chronic | Ingst | ||
| Dexlansoprazole | 7 | 7 | Acute on Chronic | Ingst | ||
| Quetiapine | 8 | 8 | Acute on Chronic | Ingst | ||
| 73 year Female | Metoprolol | 1 | 1 | Acute on Chronic | Ingst | Int-S |
| Duloxetine | 2 | 2 | Acute on Chronic | Ingst | ||
| Trazodone | 3 | 3 | Acute on Chronic | Ingst | ||
| Donepezil | 4 | 4 | Acute on Chronic | Ingst | ||
| Baclofen | 5 | 5 | Acute on Chronic | Ingst | ||
| Benztropine | 6 | 6 | Acute on Chronic | Ingst | ||
| Lurasidone | 7 | 7 | Acute on Chronic | Ingst | ||
| Alprazolam | 8 | 8 | Acute on Chronic | Ingst | ||
| Zolpidem | 9 | 9 | Acute on Chronic | Ingst | ||
| Meloxicam | 10 | 10 | Acute on Chronic | Ingst | ||
| Salicylate | 11 | 11 | Acute on Chronic | Ingst | ||
| Levothyroxine | 12 | 12 | Acute on Chronic | Ingst | ||
| Omeprazole | 13 | 13 | Acute on Chronic | Ingst | ||
| Vitamin D | 14 | 14 | Acute on Chronic | Ingst | ||
| 96 year Female | Calcium Antagonist | 1 | 1 | Acute | Ingst | Unk |
| Cold and Cough Preparations | ||||||
| 30 year Male | Dextromethorphan/ Guaifenesin | 1 | 1 | Acute | Ingst | Int-U |
| Electrolytes And Minerals | ||||||
| 63 year Female | Iron | 1 | 1 | Acute on Chronic | Ingst | Int-S |
| Ibuprofen | 2 | 2 | Acute on Chronic | Ingst | ||
| Levothyroxine | 3 | 3 | Acute on Chronic | Ingst | ||
| Sedative/Hypnotics/Antipsychotics | ||||||
| 48 year Female | Quetiapine | 1 | 1 | Acute on Chronic | Ingst | Int-S |
| Stimulants and Street Drugs | ||||||
| 20 year Male | Heroin | 1 | 1 | Acute on Chronic | Par | Int-A |
| Ethanol | 2 | 2 | Acute on Chronic | Ingst | ||
Abbreviations: Inhal: Inhalation; Ingst: Ingestion; Par: Parenteral; Int-S: Intentional-Self; Int-U; Intentional-Unknown; Int-A: Intentional-Another; Unk: Unknown.
Table 14 compares key statistics from 2015 to 2016. Number of exposures, calls from healthcare facilities, moderate or major outcomes and deaths increased from 2015.
Table 14.
2015 to 2016 comparison of select statistics.
| 2015 | 2016 | |
|---|---|---|
| Total Cases | 20,109 | 21,965 |
| Calls from Health Care Facility | 4,267 | 4,514 |
| Moderate or Major Outcomes | 1,688 | 1,971 |
| Deaths | 13 | 15 |
Discussion
The University of Kansas Health System Poison Control Center has been in operation for 35 years and serves the state of Kansas 24 hours a day, 365 days a year. Receiving over 26,000 calls per year, the PCC is an integral part of the emergency medical response, public health and health care facilities in Kansas. Childhood poisonings, both unintentional and intentional, are a major focus, with calls for patients under 19 years of age accounting for approximately 2/3 of all exposures.
The PCC statistics are similar to those seen nationally.1 In 2016, 2,710,042 encounters were logged by poison control centers nationwide, including 2,159,032 human exposures. Total encounters showed a 2.9% decline from 2015, but healthcare facility (HCF) human exposure cases increased by 3.6% from 2015. More serious outcomes (moderate, major or death) also increased. Nationwide, the five substance classes most frequently involved in adult exposures were analgesics, sedative/hypnotics/antipsychotics, antidepressants, cardiovascular drugs, and cleaning substances, while the top five most common exposures in children age 5 years or less were cosmetics/personal care products, household cleaning substances, analgesics, foreign bodies/toys/miscellaneous, and topical preparations. There were 1,415 exposure related fatalities reported nationwide in 2016.
The ongoing importance of the PCC is reflected in current trends that have seen rates of poisonings and overdoses increase at an alarming rate. The PCC saw an increase in number of calls from healthcare facilities, cases with moderate or major medical outcomes and deaths in 2016 compared to 2015. In an August 2017 report, the National Center for Health Statistic noted that the age-adjusted drug-poisoning death rate increased from 6.1 per 100,000 in 1999 to 16.3 per 100,000 in 2015, totaling over 50,000 deaths in 2015.3 Teenage (age 15 – 19) overdose deaths are increasing as well.4 The ongoing “opioid epidemic” is a major driver in the rise of poisoning deaths.3
Reporting exposures to the PCC is voluntary and the PCC is not contacted for all poisonings in the state of Kansas. Furthermore, in a majority of cases there is no objective confirmation of exposure. These limitations should be noted when interpreting PCC data.
Conclusion
The results of the 2016 University of Kansas Health System Poison Control annual report demonstrated that the center receives calls from the entire state of Kansas, totaling over 20,000 human exposures per year. While pediatric exposures remain the most common, there is an increasing number of calls from healthcare facilities and for cases with serious outcomes. The experience of the PCC is similar to national data. This report supports the continued value of the PCC to both public and acute health care in the state of Kansas.
Acknowledgments
We would like to thank Poison Control Center Staff: Tama Sawyer, PharmD, Anne Marie Banks, Amber Ashworth, Mike McKinney, Kathy White, Anita Farris, Mark Stallbaumer, and Bobbie Jean Wainscott.
References
- 1.Gummin DD, Mowry JB, Spyker DA, Brooks DE, Fraser MO, Banner W. 2016 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 34th Annual Report. Clin Toxicol (Phila) 2017;55(10):1072–1252. doi: 10.1080/15563650.2017.1388087. [DOI] [PubMed] [Google Scholar]
- 2.Mowry JB, Spyker DA, Brooks DE, McMillan N, Schauben JL. 2015 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 33rd Annual Report. Clin Toxicol. 2016;54(10):924–1109. doi: 10.1080/15563650.2016.1245421. [DOI] [PubMed] [Google Scholar]
- 3.Hedegaard H, Warner M, Miniño AM. NCHS Data Brief, no 294. Hyattsville, MD: National Center for Health Statistics; 2017. Drug overdose deaths in the United States, 1999–2016. [Google Scholar]; CDC. Wide-ranging online data for epidemiologic research (WONDER) Atlanta, GA: CDC, National Center for Health Statistics; 2016. Available at http://wonder.cdc.gov. [Google Scholar]
- 4.Curtin SC, Tejada-Vera B, Warmer M. Drug overdose deaths among adolescents aged 15–19 in the United States: 1999–2015. NCHS Data Brief 2017. (282):1–8. [PubMed] [Google Scholar]