Abstract
Youth who exhibit externalizing problems during childhood and adolescence are at an increased risk for a wide range of detrimental life outcomes. Despite the profound consequences of externalizing problems for children, their families, and their communities, we know less about the precise trajectory of externalizing symptoms across late childhood and adolescence, due to the paucity of fine-grained longitudinal research. The present study examined the development of externalizing symptoms in a large sample (N=674) of Mexican-origin youth, assessed annually from age 10 to 17. Specifically, we conducted analyses to better understand the trajectories of Attention-Deficit/Hyperactivity Disorder (ADHD), Oppositional Defiant Disorder (ODD), and Conduct Disorder (CD) symptoms (and their co-development), as well as how gender and cultural factors influence symptom trajectories. On average, ADHD symptoms slowly declined from age 10 to 17; ODD symptoms increased until age 13 and then declined thereafter; and, CD symptoms slowly increased until age 15 and then leveled off. ADHD, ODD, and CD symptoms predicted change in each other, indicating youth may accumulate multiple forms of externalizing problems over time. Boys reported fewer externalizing problems than girls, contrary to expectations. Consistent with the Immigrant Paradox, we found that 2nd+ generation youth, youth who endorsed fewer traditional Mexican cultural values (traditional gender roles, traditional family values, religiosity), and youth who engaged in less Spanish/more English language use were at increased risk for exhibiting ADHD, ODD, and CD symptoms from childhood through adolescence. We discuss the theoretical and practical implications of these developmental patterns among Mexican-origin youth. (248/250 words)
Keywords: ADHD, ODD, CD, externalizing, longitudinal, Mexican
Externalizing problems, or maladaptive behaviors directed toward the external environment, typically have their onset in childhood, with symptoms peaking in adolescence and (for some) persisting throughout the life course (Moffitt, Caspi, Rutter, & Silva, 2001). The transition from late childhood to adolescence is thought to be a time when externalizing problems, like inattention and hyperactivity problems (Attention-Deficit Hyperactivity Disorder; ADHD), can increase risk for and transform into more severe forms of disruptive behaviors such as defiance of authority (Oppositional Defiant Disorder; ODD) and vandalism, theft, and physical aggression (Conduct Disorder; CD) (Beauchaine & McNulty, 2013; Loeber, Burke, & Pardini, 2009). Although the experience of externalizing symptoms for some individuals is limited to childhood and adolescence, the repercussions of persistent ADHD, ODD, and CD symptoms include an increased risk for academic failure, unemployment, substance abuse and dependency, unwanted pregnancy, delinquency and incarceration (Fergusson, Horwood, & Ridder, 2005; Moffitt, Caspi, Rutter, & Silva, 2001). Given these adverse consequences, there is a dire need to better understand how various forms of externalizing problems develop and interrelate over time, especially among ethnic minority youth.
The present study examined the development of externalizing problems using data from a longitudinal study of 674 Mexican-origin youth, who completed a psychiatric interview annually from age 10 to 17. Previous studies of the development of externalizing problems have been based largely on White, non-Latino, or African-American samples. Research on Latino populations is particularly important because they are at increased risk for a wide range of adolescent problems, yet are less likely to be diagnosed as having a conduct disorder even when they exhibit the same behavioral problems as non-Latino, White children (Pottick, Kirk, Hsieh, & Tian, 2007). The current size and expected growth of the Latino population (the majority of whom are of Mexican-origin) underscores the importance of improving our understanding of how externalizing problems develop in this at-risk population.
To better understand the development of externalizing symptoms, we focus on several, fundamental questions: (a) what are the precise developmental trajectories of ADHD, ODD, and CD from late childhood to late adolescence?; (b) how are these trajectories interrelated (i.e., how do ADHD, ODD, and CD co-develop)?; (c) do the trajectories differ for boys and girls?; and (d) are cultural factors (nativity status, cultural values, language use) associated with initial levels and escalation of youth externalizing problems?
Developmental Trajectories of Externalizing Symptoms from Late Childhood through Adolescence
A developmental psychopathology approach conceptualizes psychopathology as a deviation from normative development and aims to understand the continuity and discontinuity of psychopathology via risk and protective factors ranging from biological processes to socio-cultural factors (Cicchetti & Rogosch, 1996). Equifinality (the same outcome originates from different antecedents) and multifinality (multiple outcomes originate from the same antecedent) are critical for understanding developmental pathways to psychopathology (Cicchetti & Rogosch, 1996). Researchers have debated equifinality and multifinality issues in relation to externalizing disorders, with competing perspectives asserting that: (1) ADHD, ODD, and CD are due to common causes, (2) ADHD, ODD, and CD are part of a broader externalizing factor that predicts outcomes better than the disorders separately, (3) ADHD is conceptually and empirically distinct from ODD and CD, given its recent reclassification as a neurodevelopmental disorder, instead of an externalizing disorder, in the Diagnostic and Statistical Manual of Mental Disorders (DSM), and (4) ADHD, ODD and CD are best understood by developmental sequence models, where individuals progress through the externalizing disorders with age (Beauchaine & Hinshaw, 2015). These different perspectives range from expecting identical developmental trajectories and correlates to expecting relatively distinct trajectories and correlates across the externalizing disorders. Thus, one way to better understand equifinality and multifinality pathways is to examine the developmental trajectories of ADHD, ODD, and CD symptoms.
ADHD, the earliest-occurring form of externalizing behavior, is characterized by inattention and hyperactive-impulsive behaviors that pervade multiple, social contexts (American Psychological Association [APA], 2013). Although originally conceptualized as a childhood disorder, it is now widely recognized that ADHD can persist into adolescence and adulthood (Beauchaine & Hinshaw, 2015; Davidson, 2008). ADHD symptoms generally decline from childhood through adolescence (Pingault et al., 2015; Willoughby, 2003). However, the inattention component of ADHD shows a flat trajectory into adulthood whereas the hyperactive-impulsive component decreases from childhood to adulthood (Barkley, Fischer, Smallish, & Fletcher, 2002; Davidson, 2008).
ODD encompasses behaviors such as defying authority, easily losing one’s temper, and acting vindictively toward others (APA, 2013). Typically, children show symptoms of ODD prior to age 10, and prevalence rates of ODD symptoms increase into adolescence (Maughan et al., 2004; Nock, Kazdin, Hiripi, & Kessler, 2007). However, cross-sectional data tell us little about the developmental course of ODD symptoms. Longitudinal research has documented small gradual decreases or no change in ODD from childhood through adolescence (Tremblay et al., 2013; van Lier, van der Ende, Koot, & Verhulst, 2007). Moreover, ODD includes symptoms related to two conceptually distinct facets (Burke, Hipwell, & Loeber, 2010; Herzhoff & Tackett, 2016); the irritability facet (emotion dysregulation) remains stable from early adolescence to young adulthood, whereas the defiance facet (oppositionality) declines over this period (Leadbeater & Homel, 2015).
CD is characterized by more severe externalizing behaviors such as theft, destruction of property, and physical assault (APA, 2013). Longitudinal studies have identified two common developmental pathways for CD: (1) life-course persistent, where CD symptoms emerge in childhood and persist throughout the life course, and (2) adolescence-limited, where CD symptoms are confined to adolescence (Moffitt, 2006). However, not all youth with childhood-onset CD exhibit a life-course persistent pathway (Moffitt, 2006). Overall, longitudinal research suggests that CD is relatively stable from adolescence to adulthood (Diamantopoulou, Verhulst, & van der Ende, 2011), and symptoms increase during adolescence before tapering off in adulthood (Moffitt, 2006).
Previous research has several limitations that restrict our ability to draw conclusions about the developmental trajectories of ADHD, ODD, and CD. First, many previous studies were based on cross-sectional data, and thus do not provide a strong basis for inferences about individual development over time. Second, many previous longitudinal studies were confined to only one developmental period (typically early childhood) and/or did not have frequent enough assessments to precisely track changes over time. Third, we know little about the developmental course of the facets of ADHD (inattention vs. hyperactive-impulsive) and ODD (irritability vs. defiant), which would provide a more nuanced understanding of how different aspects of each disorder change over time. Finally, most (if not all) longitudinal studies used samples comprised of majority non-Latino white youth or African-American youth. Thus, little is known about whether the developmental trajectories of ADHD, ODD, and CD symptoms are the same for Latino youth.
Co-Development of ADHD, ODD, and CD Symptoms
In addition to analyzing the trajectory of each individual disorder, we also examined how ADHD, ODD, and CD symptoms trajectories interrelate over time. Examining co-developmental patterns among these disorders can inform competing theoretical conceptions of their distinct vs. shared developmental pathways, as well as the developmental sequencing of their emergence. ADHD, ODD, and CD are widely known to be strongly comorbid in child and adolescent samples. Moreover, longitudinal research suggests that ADHD symptoms put youth at risk for developing ODD (Burns & Walsh, 2002; Harvey, Metcalfe, Herbert, & Fanton, 2011) and early-onset CD symptoms (Loeber, Green, Keenan, & Lahey, 1995) and can contribute to the developmental progression of ODD to CD (Waschbush, 2002). However, ODD symptoms do not always influence later ADHD symptoms (Burns & Walsh, 2002; Harvey, Breaux, & Lugo-Candelas, 2016), nor do children with ODD always or necessarily progress to CD. Thus, the research to date does not provide a clear or nuanced picture of how exactly ADHD, ODD, and CD symptoms co-develop from childhood through adolescence.
There are three models of how and why the three disruptive disorders may co-develop. First, the overlap among the incidence and development of ADHD, ODD, and CD symptoms may be due to genetic and/or shared environmental factors that underlie all three disorders (Burt, Krueger, McGue, & Iacono, 2001; Tuvblad, Zheng, Raine, & Baker, 2009). If so, we would expect ADHD, ODD and CD symptoms to be interrelated because they share underlying risk factors, but symptoms of one disorder should not predict change over time in another disorder. Second, there may be a specific developmental progression from ADHD to ODD, and then from ODD to CD. In this case, ADHD symptoms should predict change over time in ODD symptoms, and ODD symptoms should predict change over time in CD symptoms, but no other prospective effects should emerge (e.g., ODD should not predict change in ADHD). This progression of symptoms implies that the manifestation of the underlying externalizing disorder changes over time. Finally, the three forms of externalizing problems may have reciprocal influences on each other (e.g., ADHD increases risk for ODD, and conversely, ODD increases risk for ADHD). This co-developmental pattern implies that youth are not changing their manifestation of externalizing problems, but rather, they are accumulating or co-developing multiple forms simultaneously.
Gender Differences in the Development of Externalizing Problems
Boys generally exhibit more externalizing problems than girls. Some studies suggest that the male-to-female disparity in externalizing symptoms increases with age, whereas other studies suggest that the two sexes become more comparable as they transition into adolescence (Cohen et al., 1993; Fontaine et al., 2009; Lahey et al., 2000; SAMHSA, 2015). Furthermore, gender differences in the prevalence of ADHD, ODD, and CD symptoms tell us little about whether there are developmental differences between boys and girls in the growth of externalizing behaviors from childhood through adolescence.
Several models have been proposed to describe how and why boys and girls might differ in the developmental course of externalizing problems. First, both boys and girls experience childhood-onset and adolescence-limited externalizing pathways, but there are fewer girls that fit into either developmental trajectory, which suggests that the difference may be in the prevalence, rather than the developmental course, of the disorder (Moffitt & Caspi, 2001). Second, boys and girls show a similar age of onset of externalizing behaviors (Keenan et al., 2010; Lahey et al., 2006), but then differ in the developmental course of these behaviors, which would suggest that socialization pressures shape the trajectories of externalizing problems differently for boys and girls (Keenan & Shaw, 1997). Third, boys and girls may differ in the way they express externalizing pathology, with boys displaying more physical aggression and girls displaying more relational aggression, leading boys to exhibit more CD symptoms (Beauchaine & Hinshaw, 2015; Keenan, Coyne, & Lahey, 2008). Additionally, boys are higher on the hyperactive-impulsive dimension of ADHD, whereas girls are higher on the inattention dimension of ADHD (Rucklidge, 2010). In contrast, there is no gender difference in the irritability and defiance components of ODD (Herzhoff & Tackett, 2016). We know little about these possibilities because girls are often understudied by researchers, as well as underidentified and underdiagnosed by clinicians (Javdani, Sadeh, & Verona, 2011; Ohan & Johnston, 2005). Thus, there is a strong need for longitudinal studies that directly evaluate whether girls and boys show different externalizing trajectories across childhood and adolescence (Berkout, Young, & Gross, 2011).
Acculturation Differences in the Development of Externalizing Problems
An important issue is whether the developmental course of externalizing problems observed in majority samples generalizes to Mexican-origin youth, and whether there are cultural factors unique to Mexican-origin youth that increase risk for, or promote resilience to, externalizing problems. According to Garcia-Coll’s integrative model of ethnic minority development (Garcia-Coll et al., 1996), attributes such as ethnicity and race propel individuals into various rungs of the social hierarchy that can differentially impact subsequent developmental processes via social stratification mechanisms such as racism, segregation, and discrimination. Thus, ethnic minority youth development is shaped by culture-specific environmental, familial, cultural, and child factors. Based on the integrative model, we examine the most proximal influences on the development of externalizing problems among Mexican-origin adolescents: adaptive culture and family factors (i.e., nativity status, cultural values, and cultural practices).
Nativity status
Nativity status (e.g., born in the U.S. vs Mexico) is one aspect of ‘social position’ that can influence social stratification mechanisms and the developmental processes that follow. In general, first-generation immigrant families maintain attitudes, values, and practices rooted in their heritage culture (e.g., familism, respect for elders, Spanish language use) that are believed to buffer youth against maladaptive developmental trajectories (Garcia-Coll & Marks, 2011; Schwartz, Unger, Zamboanga, & Szapoznik, 2010). First-generation immigrants generally have fewer behavioral and mental health problems than more acculturated individuals, a pattern referred to as the Immigrant Paradox (Garcia-Coll & Marks, 2011, but see Teruya & Bazargan-Hejazi, 2013). Given previous patterns of intergenerational differences in conduct problems (Gonzales et al., 2002), we expect youth who were born in the U.S. to show higher levels and more rapid escalation of ADHD, ODD, and CD symptoms from late childhood to adolescence.
Cultural values
Ethnic minorities respond to social stratification mechanisms like discrimination and segregation by developing and maintaining their heritage values (Garcia-Coll et al., 1996). In the present study, we focus on three cultural values that are critically important for Mexican-origin youth (Knight et al., 2010): traditional gender roles (i.e., beliefs that men should be dominant and powerful figures in the family), traditional family values (i.e., beliefs about the importance of harmonious bonds within the family and respect for elders), and religiosity (i.e., beliefs about the centrality of religion to everyday life). Cross-sectional studies have shown that youth who endorse more negative gender roles (i.e., aggressive masculinity, submissive femininity), fewer traditional family values, and fewer religious beliefs demonstrate more externalizing problems (Germán, Gonzales, & Dumka, 2009; Kulis, Marsiglia, & Nagoshi, 2010; Marsiglia, Ayers, & Hoffman, 2011). Longitudinal research has demonstrated that youth who endorse more traditional family values show decreases in externalizing behaviors two years later (Berkel et al., 2010).
Cultural practices
Another way that ethnic minorities respond to social stratification mechanisms is by engaging in behaviors and practices that distinguish them from the receiving culture (Garcia-Coll et al., 1996). One marker of this is sociolinguistic orientation, or the extent to which Mexican-origin youth use Spanish and English in their everyday life. Mexican-origin youth who maintain Spanish language use are decreased risk for externalizing problems, whereas Mexican-origin youth who prefer English are at increased risk for conducts problems (Allen et al., 2008; Gonzales et al., 2002), perhaps because English language use indicates a shift toward the receiving culture.
Given the dearth of longitudinal studies of Mexican-origin youth, we know very little about how cultural factors are related to the development of externalizing symptoms in this ethnic group. Previous research has examined the influence of familism and acculturation level on changes in “risky behaviors”, broadly defined (Wheeler et al., 2017); however, in the present study, we are able to examine cultural influences on specific externalizing symptoms (ADHD, ODD, and CD). Furthermore, we investigate several of the main components of acculturation: nativity status, cultural values, and cultural practices (Schwartz, Unger, Zamboanga, & Szapoznik, 2010), which have been implicated as proximal influences on the normative development of ethnic minority children (Garcia-Coll et al., 1996). Additionally, we examine intergenerational effects (moderation of externalizing trajectories by nativity status) and intragenerational effects (co-development of cultural values/practices and externalizing problems). We expect 1st generation Mexican-origin youth, youth who endorse more traditional Mexican cultural values, and youth who maintain Spanish language use to show lower average levels of externalizing behaviors and greater declines (or less steep increases) in externalizing behaviors from childhood to adolescence. There is no strong theoretical basis for predicting that cultural factors will matter more for one disorder than another, or that any one cultural factor will be particularly consequential. However, because ADHD is assumed to be rooted in neurodevelopmental deficits to a greater extent than ODD/CD, it is possible that cultural factors exert a greater influence on the development of ODD and CD, especially if rules about appropriate behavior are encoded into cultural norms and scripts (Cicchetti & Rogosch, 2002; Garcia-Coll et al., 1996). Finally, cultural values may demonstrate the strongest associations with externalizing symptoms, because they provide a more direct index of acculturation than nativity status and language use.
The Present Study
The present study extends previous research in several important ways. First, we used data from a large community sample, which increases generalizability to the broader population of Mexican-origin youth than studies of clinical populations. Second, we conducted annual assessments of externalizing symptoms from late childhood through adolescence (8 waves), allowing us to identify more precise trajectories of individual-level change, and test for more complex non-linear trajectories. Third, we assessed externalizing symptoms using a well-validated and standardized psychiatric interview. Fourth, we investigated all three forms of externalizing symptoms (ADHD, ODD, and CD), as well as the facets of ADHD and ODD, from late childhood through adolescence, which can provide insight into the co-development of multiple forms of externalizing problems. Fifth, many past longitudinal studies of externalizing problems have included only boys, whereas our sample consists of boys and girls, allowing us to test for gender differences in the trajectories of ADHD, ODD, and CD. Sixth, we studied these questions in an ethnic minority group that has been relatively neglected in past longitudinal research on the development of externalizing problems. Furthermore, we were able to examine culture-specific factors that may increase risk for, or promote resilience to, externalizing problems.
Method
Participants and Procedures
We used data from the California Families Project, a longitudinal study of Mexican-origin youth and their parents (N=674). Children were drawn at random from rosters of students in the Sacramento and Woodland, CA, school districts. The focal child had to be in the 5th grade, of Mexican origin, and living with his or her biological mother. Approximately 72.6% of the eligible families agreed to participate in the study, which was granted approval by the University of California, Davis Institutional Review Board (Protocol # 217484, Mexican Family Culture and Substance Use Risk and Resilience). The children (50% female) were assessed annually from 5th (Mage at Wave 1=10.86, SD=0.51) through 12th grade (Mage at Wave 8=17.69 SD=0.48). Of the original 674 families, 85%, 86%, 89%, 91%, 89%, 90%, and 92% were retained at Waves 2 through 8, respectively.1 Participants were interviewed in their homes in Spanish or English, depending on their preference (across waves, 4% to 15% of youth and 79% to 87% of parents, were interviewed in Spanish). Interviewers were all bilingual and most (~75%) were of Mexican heritage.
Sixty-three percent of mothers and 65% of fathers had less than a high school education (median=9th grade for both mothers and fathers); median total household income was between $30,000 and $35,000 at Wave 1 (range = < $5,000 to > $95,000). About 83.6% of mothers and 89.4% of fathers were born in Mexico.
Measures
Externalizing symptoms - ADHD, ODD and CD
The National Institute of Mental Health (NIMH) Diagnostic Interview Schedule for Children-IV (DISC-IV) was administered to the child annually from age 10 to 17. The DISC-IV is a comprehensive psychiatric interview that assesses mental health problems using DSM-IV criteria; it is the most widely-used mental health interview that has been tested in both clinical and community populations and validated in both English and Spanish (Costello, Edelbrock, & Costello, 1985). Responses were recorded dichotomously (0=no, 1=yes) as the symptom being present or not in the past year. The ADHD module included 24 questions about attention-related behaviors such as, “[Did you have] trouble keeping your mind on task for more than a short period of time?” and hyperactivity problems such as “[Did you] often climb on things/run around when you weren’t supposed to?” The ODD module included 12 questions about irritability such as, “[Did you] lose your temper?” and defiant behaviors such as “[Did you] do things on purpose that caretakers said not to do?” The CD module included 23 questions about more severe delinquent behavior such as “[Did you] break/damage someone else’s things on purpose?” and “[Did you] bully someone smaller who wouldn’t fight back?” For each disorder, we summed the responses at each wave to create composite symptom counts from age 10 to 17. In addition, we computed symptom counts for the inattention (11 items) and hyperactive-impulsive (12 items) facets of ADHD, and for the irritability (4 items) and defiant (8 items) facets of ODD.
Nativity status
Seventy-one percent of the youth were born in the U.S., and 29% were born in Mexico.2
Cultural values
At ages 10, 12, 14 and 16, the child completed the Mexican American Cultural Values Scale (MACVS; Knight et al., 2010). Response options ranged from 1 (Not at all) to 4 (Very much) for all scales. The 5-item Traditional Gender Roles scale (α=.64–.75 across waves) includes statements such as, “It is important for the man to have more power in the family than the woman.” The Traditional Family Values scale includes 16 items related to familism values and 8 items related to respect for parents and elders. We computed an overall traditional family values score (α=.85–.91) comprised of these 24 items because the familism and respect subscales were highly correlated across waves (rs=.60–.70). Sample items include, “Children should always do things to make their parents happy” and “Children should respect adult relatives as if they were parents”. Last, the 6-item Religiosity scale (α=.76–.93) includes statements such as, “It is important to follow the word of God”.
Language use
At ages 10, 11, 12, 13, 14, and 15, the child completed the Acculturation Rating Scale for Mexican–Americans-II (ARSMA–II; Cuellar, Arnold, & Maldonado, 1995) to assess Spanish use (5 items; α=.80–.83) and English use (5 items; α=.71–.77). Items asked participants how frequently they spoke, wrote, thought, listened to music, and watched television in each language, using a four-point scale ranging from 1 (Never or almost never) to 4 (Always or almost always).
Statistical Analyses
All analyses were conducted using Mplus Version 6 (Muthén & Muthén, 1998–2011). We used a maximum likelihood estimator (ML) to account for non-normal distributions of observed variables and full information maximum likelihood procedure (FIML) to account for missing data. We used univariate latent growth curve (LGC) models to examine the growth of ADHD, ODD, and CD (and related facets) over time. LGC models describe the average initial level (intercept) and growth over time (slope) of a construct, as well as how much variability there is in the intercept and slope. To find the best-fitting growth trajectory for each disorder, we conducted a series of model comparisons and evaluated changes in chi-square, degrees of freedom, root mean-square-error of approximation (RMSEA), Comparative Fit Index (CFI), and the Tucker-Lewis Index (TLI). Specifically, we compared three models: (1) no growth model, where the slope is fixed to be zero over time; (2) linear growth model, where the slope linearly increases by one unit over time, with the first time point centered at ‘0’, the second time point fixed at ‘1’,…, and the last time point is fixed at ‘7’; and (3) a latent basis model, where the first and last time points of the slope are fixed (at ‘0’ and ‘7’, respectively) and the middle time points are freely estimated to the data. In all models, path coefficients from the intercept to the repeated assessments are fixed to 1, and the intercept and slope are allowed to covary.
To examine the co-development of externalizing symptoms, we conducted bivariate LGC models and specified correlations among the levels and slopes of externalizing symptoms. To examine gender and nativity status differences in the externalizing trajectories, we conducted multiple group LGC analyses. We began with a model where all parameters are constrained to be equal across groups, and then removed the constraints and examined changes in the chi-square, degrees of freedom, and alternative fit indices. For each disorder, we examined whether the groups differed in: (1) initial level (i.e., mean of the intercepts); (2) average rate of change from age 10 to 17 (i.e., the mean of the slopes); (3) variability around the rate of change (i.e., the variance of the slopes); and (4) age-to-age growth over time (i.e., the slope coefficients). If freely estimating the parameter did not significantly improve model fit, we retained the constraints. To investigate the influence of Mexican cultural values and language use, we fit a univariate LGC model to estimate trajectories of cultural values and language use, and then conducted bivariate LGC models to examine associations between the cultural values/language use trajectories and the externalizing problems trajectories.
Results
Table S1 shows descriptive statistics for all study variables. Table S2 shows concurrent correlations among all study variables.
Growth Trajectories of ADHD, ODD and CD Symptoms
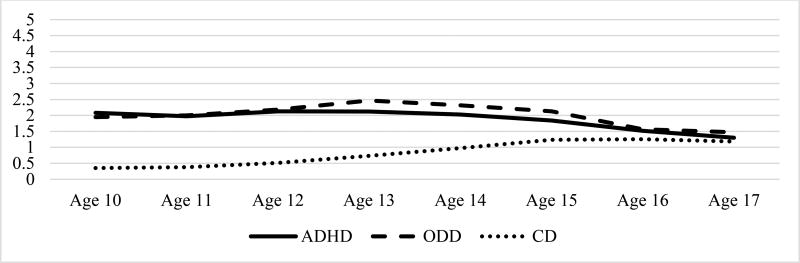
For all three disorders (and associated facets), the latent basis growth curve model fit the data best, indicating non-linear patterns of growth (see Table S3). Figure 1 shows the estimated growth trajectories derived from this model for ADHD, ODD, and CD symptoms. On average, ADHD symptoms remained relatively flat from age 10 to 13, and then slowly decreased to age 17. ODD symptoms increased from age 10 to 13, when symptom presentation peaked, and then decreased to age 17. In contrast, CD symptoms slowly increased from age 10 to 15, and then leveled off to age 17.
Figure 1. Estimated growth trajectories for ADHD, ODD, and CD symptoms.
Note. ADHD = Attention-Deficit/Hyperactivity Disorder. ODD = Oppositional Defiant Disorder. CD= Conduct Disorder.
Figure S1 shows the estimated growth trajectories for the facets of ADHD and ODD (see Table S4). Both ADHD facets (inattention and hyperactivity) decreased very slightly from age 10 to 17, with hyperactivity showing a slightly more rapid decrease from age 14 to 17. For the ODD facets, we found that irritability decreased from age 10 to 17, whereas defiance increased from age 10 to 13, and then decreased from 14 to 17, which more closely mirrors the overall ODD trajectory.
Co-Development of ADHD, ODD, and CD
Table 1 shows results from bivariate LGC models. For all forms of externalizing symptoms, the initial levels of ADHD, ODD, and CD symptoms were significantly intercorrelated. That is, youth who exhibited symptoms of any one disorder also tended to exhibit symptoms of the other two disorders (the intercorrelations among the facets showed the same pattern).We also found significant correlations among the trajectories. First, change over time in ADHD symptoms was associated with change in ODD symptoms; this association held for both ADHD facets with ODD, and both ODD facets with ADHD. Second, change in ODD symptoms (and both facets) was associated with change in CD symptoms. In contrast, change in ADHD (or its facets) symptoms were not associated with change in CD symptoms.
Table 1.
Co-Development of ADHD, ODD, and CD Symptoms
| r (Level1, Level2) | r (Slope1, Slope2) | r (Level1, Slope2) | r (Level2, Slope1) | |
|---|---|---|---|---|
| 1. ADHD & 2. ODD | .72* [.66,(78] | .48* [.27,(70] | −.52* [−.67, –.37] | −.36* [−.54, –.19] |
| 1. Inattention & 2. ODD | .67* [.58,(75] | .33* [.11,(56] | −.43* [−.59, –.28] | −.03 [−.17,(12] |
| 1. Hyperactivity & 2. ODD | .65* [.58,(71] | .37* [.14,(60] | −.52* [−.69, –.36] | −.32* [−.45, –.18] |
| 1. ADHD & 2. Irritability | .69* [.62,(76] | .22* [.01,(43] | −.27* [−.41, –.13] | −.23* [−.38, –.09] |
| 1. ADHD & 2. Defiance | .66* [.58,(73] | .62* [.37,(87] | −.53* [−.70, –.36] | −.37* [−.61, –.13] |
| 1. ADHD & 2. CD | .39* [.28,(50] | −.09 [−.26,(09] | .36* [.25,(47] | −.20* [−.36, –.03] |
| 1. Inattention & 2. CD | .46* [.25,(67] | .49* [.30,(68] | .11 [−.19,(41] | −.10 [−.36,(16] |
| 1. Hyperactivity & 2. CD | .37* [.26,(48] | −.09 [−.24,(06] | .36* [.25,(47] | −.17* [−.32, –.02] |
| 1. ODD & 2. CD | .43* [.33,(53] | −.33* [−.54, –.12] | .49* [.40,(59] | −.23* [−.44, –.03] |
| 1. Irritability & 2. CD | .43* [.31,(54] | .27* [.11,(43] | .20* [.06,(35] | −.35* [−.49, –.21] |
| 1. Defiance & 2. CD | .50* [.38,(61] | −.45* [−.63, –.26] | .51* [.40,(61] | −.20 [−.41,(01] |
Note. ADHD = Attention-Deficit/Hyperactivity Disorder. ODD = Oppositional Defiant Disorder. CD = Conduct Disorder. r = Correlation. Values in brackets are the 95% confidence intervals. The ‘1.’ and ‘2.’ in the row labels correspond to the subscript numbers in the column headers, in order to distinguish which constructs are the levels/slopes in the analysis of correlation coefficients.
p <(05.
Finally, we examined whether the initial level of each disorder was correlated with change over time in the other two disorders. We found that a higher initial level of ADHD symptoms was associated with a steeper inverted u-shaped trajectory of ODD symptoms (see Figure S2) and greater increases in CD symptoms. A higher initial level of ODD symptoms was associated with greater decreases in ADHD symptoms and greater increases in CD symptoms. A higher initial level of CD symptoms was associated with greater decreases in ADHD symptoms and a steeper inverted u-shaped trajectory of ODD symptoms (see Figure S3).3
Gender Differences in the Development of Externalizing Symptoms
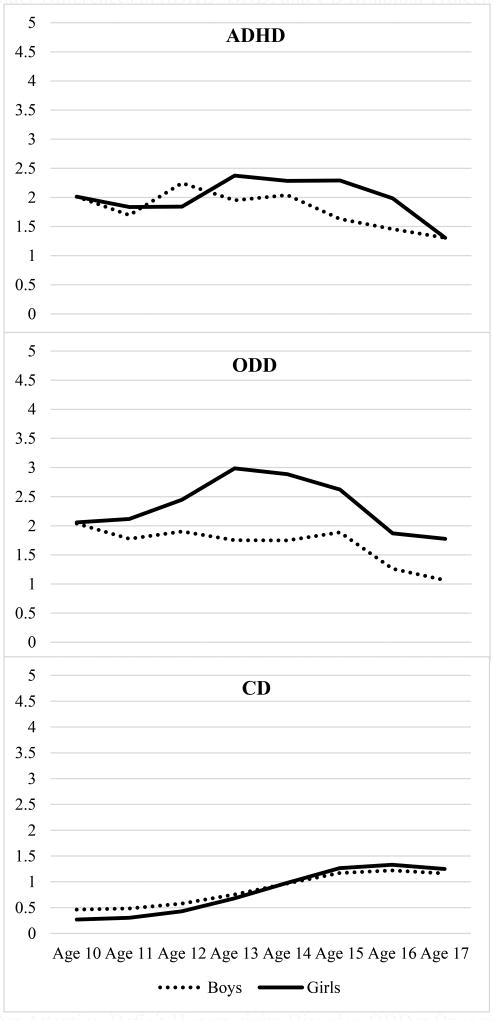
Figure 2 shows the estimated growth trajectories of ADHD, ODD and CD separately for boys and girls (see Tables S5–S7). Boys showed lower average levels of ADHD symptoms over time, whereas girls had a higher average trajectory of ADHD symptoms, with an increase in symptoms to age 13 and a steeper decline to age 17, in comparison to boys.4 For ODD, boys showed a much lower average trajectory of ODD symptoms, with girls increasing more rapidly from age 10 to 13, but then decreasing to age 17. For CD, although boys start out at a higher level, girls have a more rapid increase in CD symptoms across adolescence and surpass the average trajectory of boys from age 15 to 17.
Figure 2. Gender Differences in ADHD, ODD, and CD Symptom Trajectories.
Note. ADHD = Attention-Deficit/Hyperactivity Disorder. ODD = Oppositional Defiant Disorder. CD= Conduct Disorder.
Figure S4 shows the estimated growth trajectories of the ADHD and ODD facets by gender (see Tables S8–S9). For ADHD, boys and girls had comparable levels of inattention and hyperactivity from age 10 to 12, but then started to slightly diverge from age 13 to 16 (with girls showing higher levels), before returning to comparable levels at age 17. For the irritability facet of ODD, girls had a higher average trajectory and a larger increase over time than boys. For the defiance facet, boys and girls had comparable levels at ages 10 and 11, but then girls began to diverge from boys (showing a higher average trajectory of defiance over time) to ages 16 and 17.
Acculturation Differences in the Development of Externalizing Symptoms
Nativity status
For ADHD, American-born youth had a higher average level of ADHD symptoms compared to youth born in Mexico, with more consistent and flat levels of ADHD symptoms over time (see Figure S5 and Table S5); this effect was driven by the hyperactive-impulsive facet of ADHD (see Figure S5 and Table S8). For ODD and CD symptoms, the constrained models did not fit significantly worse than the freely estimated models, which suggests that the ODD and CD trajectories did not differ by nativity (see Tables S6–S7). Thus, the claim that more acculturated (i.e., American-born) youth would exhibit more externalizing problems than less acculturated (e.g., foreign-born) youth received support for ADHD, but not ODD and CD.
Cultural values
Mexican cultural values generally decreased over time (see Figure S6 and Table S10). Table 2 shows the standardized regression coefficients from bivariate LGC models of Mexican cultural values and externalizing symptoms. Consistent with the Immigrant Paradox, youth who endorsed more traditional gender roles exhibited lower initial levels of ODD (irritability and defiance) symptoms. Similarly, youth who endorsed more traditional family values showed lower initial levels of ODD (defiance) and CD symptoms. Moreover, higher initial levels of ODD symptoms were associated with greater decreases in traditional family values; these findings were driven by the defiance component. And, greater decreases in traditional family values were related to steeper increases in CD symptoms. For religiosity, youth high in religiosity had lower initial levels of CD symptoms. Last, youth who experienced greater decreases in religiosity showed greater decreases in ADHD symptoms.
Table 2.
Co-Development of Mexican Cultural Values, Language Use, and Externalizing Problems
| r (Level1, Level2) | r (Slope1, Slope2) | r (Level1, Slope2) | r (Level2, Slope1) | |
|---|---|---|---|---|
| Traditional Gender Roles | ||||
|
| ||||
| 1. MCV & 2. ADHD | −.09 [−.23,(04] | .15 [−.07,(37] | −.12 [−.28,(05] | −.04 [−.21,(13] |
| 1. MCV & 2. ODD | −.20* [−.32, –.08] | −.02 [−.25,(22] | .05 [−.13,(23] | −.01 [−.17,(15] |
| 1. MCV & 2. Irritability | −.19* [−.32, –.07] | −.03 [−.26,(21] | −.02 [−.19,(15] | −.02 [−.20,(16] |
| 1. MCV & 2. Defiance | −.15* [−.28, –.02] | −.09 [−.35,(16] | .08 [−.12,(27] | −.00 [−.17,(16] |
| 1. MCV & 2. CD | .11 [−.03,(25] | −.03 [−.21,(16] | −.11 [−.25,(03] | .10 [−.08,(29] |
|
| ||||
| Traditional Family Values | ||||
|
| ||||
| 1. MCV & 2. ADHD | −.10 [−.23,(04] | .07 [−.11,(28] | −.02 [−.19,(15] | −.15 [−.32,(01] |
| 1. MCV & 2. ODD | −.15* [−.27, –.03] | .16 [−.08,(39] | .12 [−.07,(31] | −.17* [−.33, –.01] |
| 1. MCV & 2. Irritability | −.10 [−.23,(04] | .11 [−.11,(33] | .13 [−.05,(31] | −.17 [−.34,(00] |
| 1. MCV & 2. Defiance | −.22* [−.36, –.08] | .24 [−.03,(50] | .05 [−.16,(25] | −.18* [−.35, –.004] |
| 1. MCV & 2. CD | −.16* [−.31, –.01] | −.25* [−.43, –.07] | −.08 [−.23,(06] | .09 [−.09,(27] |
|
| ||||
| Religiosity | ||||
|
| ||||
| 1. MCV & 2. ADHD | −.01 [−.13,(12] | .21* [.03,(38] | −.05 [−.21,(11] | −.11 [−.25,(03] |
| 1. MCV & 2. Inattention | .01 [−.14,(16] | .05 [−.14,(23] | −.04 [−.21,(13] | −.09 [−.25,(07] |
| 1. MCV & 2. Hyperactive | .02 [−.11,(14] | .17 [−.00,(33] | −.08 [−.23,(07] | −.10 [−.24,(04] |
| 1. MCV & 2. ODD | −.05 [−.17,(07] | .08 [−.11,(27] | .01 [−.16,(19] | .05 [−.08,(18] |
| 1. MCV & 2. CD | −.21* [−.35, –.06] | −.12 [−.27,(03] | .06 [−.20,(08] | .16 [.00,(31] |
|
| ||||
| Spanish Language Use | ||||
|
| ||||
| 1. Spanish & 2. ADHD | −.15* [−.25, –.05] | .03 [−.12,(18] | .02 [−.11,(15] | .02 [−.11,(14] |
| 1. Spanish & 2. Inattention | −.07 [−.20,(07] | −.06 [−.24,(11] | −.10 [−.24,(04] | .08 [−.07,(24] |
| 1. Spanish & 2. Hyperactive | −.13* [−.23, –.03] | .07 [−.08,(21] | .04 [−.08,(17] | −.01 [−.13,(12] |
| 1. Spanish & 2. ODD | −.07 [−.17,(02] | −.05 [−.21,(12] | .07 [−.07,(21] | .01 [−.10,(13] |
| 1. Spanish & 2. CD | −.17* [−.28, –.07] | −.17* [−.29, –.03] | .06 [−.05,(17] | .11 [−.02,(25] |
|
| ||||
| English Language Use | ||||
|
| ||||
| 1. English & 2. ADHD | .19* [.07,(31] | .20* [.03,(38] | −.16* [−.31, –.01] | −.20* [−.35, –.06] |
| 1. English & 2. Inattention | −.02 [−.20,(15] | .07 [−.13,(27] | .15 [−.03,(33] | −.13 [−.32,(05] |
| 1. English & 2. Hyperactive | .21* [.09,(33] | .13 [−.04,(30] | −.18* [−.33, –.04] | −.21* [−.36, –.07] |
| 1. English & 2. ODD | .20* [.09,(30] | .11 [−.09,(30] | −.17 [−.33,(00] | −.15* [−.27, –.02] |
| 1. English & 2. Irritability | .17* [.05,(29] | .01 [−.17,(20] | −.04 [−.20,(11] | −.06 [−.20,(08] |
| 1. English & 2. Defiance | .18* [.06,(29] | .09 [−.12,(30] | −.19* [−.36, –.01] | −.20* [−.33, –.06] |
| 1. English & 2. CD | .04 [−.09,(17] | −.13 [−.28,(01] | .17* [.05,(30] | −.08 [−.23,(08] |
Note. MCV=Mexican Cultural Values. ADHD = Attention-Deficit/Hyperactivity Disorder. ODD = Oppositional Defiant Disorder. CD = Conduct Disorder. r = Correlation. Values in brackets are the 95% confidence intervals. The ‘1.’ and ‘2.’ in the row labels correspond to the subscript numbers in the column headers, in order to distinguish which constructs are the levels/slopes in the analysis of correlation coefficients.
p <(05.
Cultural practices
Spanish language use decreased and English language use increased from age 10 to 15 (see Figure S7 and Table S11). Table 2 shows the standardized regression coefficients from bivariate LGC models of Spanish/English language use and externalizing symptoms. In general, more Spanish language use was associated with lower initial levels of ADHD (hyperactivity) and CD symptoms. Moreover, steeper decreases in Spanish language use were associated with greater increases in CD symptoms. Conversely, more English use was associated with higher initial levels of ADHD (hyperactivity) and ODD (irritability and defiance) symptoms. Steeper increases in English language use were associated with greater increases in ADHD symptoms. Higher initial levels of ADHD (hyperactivity) and ODD (defiance) symptoms were associated with greater decreases in English language use. Higher initial levels of English language use were associated with slight decreases in ADHD (hyperactivity) symptoms and greater increases in CD symptoms. Taken together, these findings are consistent with the Immigrant Paradox, which suggests that maintaining heritage cultural practices, such as language use, may have protective effects for youth adjustment.
Discussion
The present study examined the development of externalizing symptoms in a large sample of Mexican-origin youth followed longitudinally from age 10 to 17. Our year-by-year assessments allowed us to track the precise trajectory of ADHD, ODD, and CD symptoms over time, and examine the degree to which these trajectories develop in tandem and are influenced by gender and acculturation processes. Given the detrimental consequences of externalizing problems, it is important to understand how externalizing problems develop from childhood to adolescence among ethnic minority youth.
ADHD, ODD, and CD Have Distinct Trajectories from Childhood through Adolescence
In general, we found that ADHD, ODD, and CD symptoms showed different developmental trajectories from late childhood to late adolescence, which suggests that, within a developmental psychopathology framework, the continuity and discontinuity of externalizing problems over time (and its correlates) may be different across separate disorders among Mexican-origin youth (Cicchetti & Rogosch, 1996). The average ADHD symptom trajectory remained relatively flat from age 10 to 13, and then slowly decreased thereafter to age 17, which is consistent with previous research (Pingault et al., 2015; Willoughby, 2003). Our findings also support the notion that while many youth “grow out” of their ADHD symptom tendencies as they progress through adolescence, others experience an increase in symptoms during adolescence (Sasser, Kalvin, & Bierman, 2016). Follow-up analyses indicate that 86.9% of the youth in our study declined in ADHD symptoms, whereas only 13.1% increased in ADHD symptoms. Also consistent with previous research, hyperactive-impulsive symptoms tended to decrease later in adolescence, whereas the trajectory of inattention remained relatively flat (Barkley, Fischer, Smallish, & Fletcher, 2002; Davidson, 2008).
The average ODD symptom trajectory increased slightly from age 10 to 13, when symptom presentation peaked, with subsequent decreases from age 14 to 17. In contrast, previous longitudinal studies have reported gradual decreases in oppositional behavior from childhood to adolescence (Tremblay et al., 2013; van Lier, van der Ende, Koot, & Verhulst, 2007). The developmental trajectories of irritability and defiance also diverged in subtle ways, consistent with prior research (Leadbeater & Homel, 2015). Irritability slightly decreased from age 10 to 17, whereas defiance slightly increased from age 10 to 13 and then decreased thereafter, with comparable average levels of irritability and defiance at age 17.
Youth exhibited very few CD symptoms at age 10, but the CD trajectory slowly increased from age 10 to 15, when symptom presentation leveled off to age 17. This pattern is consistent with both research and theory (i.e., life course persistent and adolescence-limited) concerning the development of CD behavior across childhood and adolescence (Moffitt, 2006).
Evidence for the Accumulation of Externalizing Symptoms Over Time
To better understand the co-development of externalizing problems, we examined interrelations among the ADHD, ODD, and CD trajectories. In general, our findings provide the strongest support for the idea that youth co-develop or accumulate multiple forms of externalizing symptoms over time. That is, as a whole, ADHD, ODD, and CD symptoms predicted change in each other over time, which implies that there is less support for theoretical models that suggest these disorders: (1) are separate entities, or (2) show a developmental progression from ADHD to ODD to CD (without retaining any prior symptoms). Specifically, we found that individuals who, at age 10, had higher symptom counts for any of the three externalizing disorders were more likely to have higher co-occurring symptom counts for the other two externalizing disorders; this finding replicated across both facets of ADHD and ODD. Moreover, the ADHD and ODD trajectories (and facets), and the ODD and CD trajectories (and facets), were significantly inter-correlated. Thus, individuals who are increasing in ADHD symptoms are also more likely to be increasing in ODD symptoms (and vice versa), and individuals who are increasing in ODD symptoms are more likely to be increasing in CD symptoms (and vice versa). However, the ADHD and CD trajectories were not correlated, suggesting that ADHD and CD symptoms are less likely to develop in tandem than ADHD and ODD, or ODD and CD (van Lier et al., 2007).
Our findings also provide support for the idea that the presence of one form of symptomatology increases risk for another form. For example, we found that: (a) youth who exhibited more ADHD symptoms at age 10 showed accentuated (steeper inverted u-shaped) trajectories of ODD symptoms and greater increases in CD symptoms from age 10 to 17; (b) youth who exhibited more ODD symptoms at age 10 showed greater decreases in ADHD symptoms and greater increases in CD symptoms; and (c) youth who exhibited more CD symptoms at age 10 showed greater decreases in ADHD and accentuated (steeper inverted u-shaped) trajectories of ODD symptoms. In addition, by examining the facets of ADHD and ODD, we gained a more nuanced understanding of which aspects of these disorders may be especially consequential for the bidirectional nature of externalizing co-development. For example, although inattention and hyperactivity at age 10 were both related to change over time in ODD, ODD at age 10 was only associated with change in hyperactivity. Similarly, irritability and defiance at age 10 were related to change over time in CD, but CD symptoms at age 10 were only related to change in irritability. Finally, hyperactivity (but not inattention) at age 10 was associated with change in CD symptoms, and CD symptoms at age 10 were associated with change in hyperactivity (but not inattention).
These findings suggest that youth do not necessarily progress from ADHD to ODD, and then from ODD to CD, without retaining any symptoms of the earlier disorders. Rather, (some) youth are accumulating or co-developing multiple forms of externalizing problems simultaneously. More generally, it seems that youth who exhibit earlier manifestations of externalizing symptoms can be launched on trajectories toward more severe disruptive behavior problems later in development. However, the way that high initial levels of ODD and CD symptoms set youth on trajectories of experiencing fewer ADHD symptoms should be investigated in more depth. It is possible that youth who have early-onset ODD and CD symptoms are less likely to show subsequent manifestations of ADHD symptoms. Additionally, it is possible that the peak of ADHD symptoms, which serves as a precursor to ODD and CD symptoms, happens earlier in childhood, prior to our first assessment at age 10. Further, the facet-level findings indicate that ADHD, ODD, and CD co-develop in complex and distinct ways. These findings highlight the importance of hyperactivity, for example, as the driving force behind the co-development of ADHD with ODD and CD. However, further research is needed to better understand why some youth get caught in a cycle of increasingly severe problem behaviors, whereas others “grow out” of problem trajectories.
ADHD, ODD, and CD Trajectories Vary by Gender
Numerous studies have found that boys are more likely to engage in externalizing behaviors than girls. However, in our sample of Mexican-origin youth, we found that girls displayed higher average trajectories of ADHD, ODD, and CD symptoms than boys across most of the developmental period examined. These findings have several implications. First, the present study shows that both boys and girls experience late childhood manifestations of all disorders, given their comparable average levels of ADHD, ODD, and CD symptoms at age 10. Second, we found evidence for different developmental trajectories of symptoms for boys and girls from age 10 to 17, with girls showing higher peaks of symptoms and more rapid escalation of the average number of symptoms over time, highlighting the need for intervention and prevention programs tailored to each gender (e.g., in terms of the timing of the programs). These gender differences in the longitudinal course of externalizing behavior also suggest that socialization pressures, possibly unique to Mexican-origin families, may shape girls’ and boys’ trajectories differently (Keenan & Shaw, 1997). Third, in terms of the expression of ADHD, we found that girls show higher levels of both inattention and hyperactive-impulsive symptoms, contrary to research indicating that boys tend to be higher on the hyperactive-impulsive dimension and girls tend to be higher on the inattention dimension (Rucklidge, 2010). In terms of the expression of ODD, girls were higher than boys on both the irritability and defiance facets, contrary to research reporting no gender difference on either facet (Herzhoff & Tackett, 2016).
More generally, our findings run counter to a large body of research showing that boys exhibit more externalizing problems than girls (Moffitt, Caspi, Rutter, & Silva, 2001). Our discordant findings may reflect variability in the gender difference across ethnic groups; that is, among non-Latino White and African-American youth, boys show the highest levels of externalizing problems, whereas among Mexican-origin youth, it is the girls who are most prone to externalizing problems. Given the focus on males’ externalizing problems in both research and practice, more attention should be directed toward understanding precisely how boys and girls differ in their developmental trajectories, especially among minority youth who may show different gender divergences than non-Latino, White youth (Berkout, Young, & Gross, 2011). Another possibility is that boys exhibit more severe forms of externalizing problems, even when they do not exhibit relatively common externalizing symptoms. Consequently, we may be more likely to find a gender difference in a clinical sample than in a community sample, where the base-rate of symptoms is quite low. Future research should harmonize data from community-based and clinical longitudinal studies to better understand the gender dynamics that influence the development of externalizing problems in Mexican-origin youth.
Evidence for the “Immigrant Paradox” in the Development of Externalizing Symptoms
To better understand whether cultural factors protect against or exacerbate the development of externalizing symptoms by Mexican-origin youth, we investigated the effects of nativity status, cultural values, and cultural practices on ADHD, ODD, and CD trajectories. Consistent with the Immigrant Paradox, we found that American-born youth experienced higher levels of ADHD symptoms and greater increases over time, compared to youth born in Mexico (i.e., 1st generation youth). However, contrary to the Immigrant Paradox, American and Foreign-born youth did not differ in the developmental course of ODD and CD symptoms.
In addition to nativity, we also investigated intra-generational (within-group) effects by examining the extent to which cultural values and practices (Spanish/English language use) co-develop with externalizing symptoms over time. In general, youth who endorsed more heritage values (traditional gender roles, traditional family values, religiosity) and engaged in more heritage language practices (preferring Spanish to English) tended to show lower levels of externalizing problems. Moreover, with regard to the trajectories, we found that greater decreases in traditional family values (familism, respect) and heritage practices (Spanish language use) were related to greater increases in CD symptoms; conversely, greater increases in non-heritage practices (English language use) were associated with greater increases in ADHD symptoms.
Overall, our findings have several implications. First, consistent with Garcia-Coll and colleagues’ (1996) integrative model and the Immigrant Paradox, our results provide some support for the idea that maintaining values and practices rooted in one’s heritage culture is protective against externalizing problems. Protective factors for ADHD include being born in Mexico, greater religiosity, and greater Spanish and less English language use; protective factors for ODD including endorsing traditional gender roles, traditional family values, and greater English language use; and, protective factors for CD including endorsing traditional gender roles, traditional family values, religiosity, and Spanish language use. Although many effects predicted by the Immigrant Paradox did not emerge, in almost all cases we either found support for the Immigrant Paradox or found no significant differences; that is, with one exception (the positive correlation between the slopes of religiosity and ADHD symptoms), we never found that less acculturated youth (based on nativity and cultural values and practices) exhibited significantly more externalizing problems. This pattern of findings is what one would expect if the true effect size is small, but in the direction predicted by the Immigrant Paradox.
Second, we also found evidence that the experience of externalizing problems can lead to changes in cultural values, as evidenced by the association between ODD symptoms at age 10 and decreases in traditional family values. It is possible that as youth begin to engage in rule-breaking and defiance of authority, they start to reject the values and practices of their family (and heritage cultural values more generally). As a result, this may not only set youth on a trajectory of endorsing fewer protective values, but also a trajectory of worsening externalizing symptoms, through transactional associations between externalizing problems and acculturation processes. Future research should examine these co-developmental pathways more closely to better understand how engaging in externalizing behaviors can feed back to influence acculturation processes.
Third, we did not find that cultural factors mattered more or less for any particular externalizing disorder (ADHD, ODD, or CD), or that any component of acculturation (nativity, cultural values, cultural practices) mattered more or less for the development of externalizing symptoms. Future research should aim to replicate the current findings, and determine whether the particular patterns of cultural risk and resilience effects holds across samples (e.g., the finding that nativity is associated with ADHD but not ODD and CD, or that traditional gender roles are more associated with ODD and CD than with ADHD).
Overall, the findings of the present study, together with previous research, support the conclusion that more acculturated youth are at increased risk for externalizing problems. Conversely, we can conclude that endorsement of cultural values, such as familism and respect for one’s elders, and maintaining heritage cultural practices such as Spanish language use, may serve a protective function, diminishing risk for the development of ADHD, ODD, and CD symptoms. Given that nativity status cannot be changed among Mexican-origin youth, future research on preventive interventions would benefit from in-depth investigations of Mexican cultural values and practices as intervention targets. By understanding these malleable influences of cultural risk and resilience factors, we can better inform culture-specific interventions aimed at reducing externalizing problems in Mexican-origin families.
Limitations
The present study has several limitations that merit attention. First, although we examined trajectories from late childhood to late adolescence, we have no way of knowing what trajectory youth were on prior to age 10. Mapping the trajectories prior to age 10 may be particularly important for ADHD and ODD symptoms, given that the onset of these disorders typically occurs before age 10. Moreover, looking later in development, we do not yet know which youth in our study maintain their externalizing trajectories into young adulthood, which would provide insight into which youth are following a life-course persistent vs. adolescence-limited pathway. Second, as in all developmental psychopathology research that spans a substantial age range, it is difficult to know whether changes over time in symptom counts reflect true developmental change in the underlying disorder or changes in the way symptoms of the disorder are manifested during different developmental periods. However, it is important to note that the NIMH-CDISC was developed and validated for use with populations with the same age range as the present sample, so the ADHD, ODD, and CD symptoms should be appropriate for the full age range. Third, because of the low base rate of ADHD, ODD, and CD diagnoses in this community sample, we were unable to examine the developmental course of meeting diagnostic criteria for the externalizing disorders. Nonetheless, understanding how externalizing symptoms develop, and co-develop, in community samples can inform our understanding of when youth are at heightened risk for reaching diagnostic criteria. Fourth, externalizing problems were assessed via youth psychiatric interviews. Although all assessment methods have limitations, psychiatric interviews are well-validated and widely used in nationally representative studies of externalizing disorders, and youth are (arguably) the best reporters because only they know their full range of problem behaviors and delinquent activities. Nonetheless, future research should investigate whether parent-reports of externalizing problems follow the same developmental trajectories as those observed in the present study. Fifth, future research should explore a wider array of etiological factors that might shape the developmental course of ADHD, ODD, and CD symptoms in Mexican-origin youth. For example, certain temperamental tendencies, such as poor self-control, might act as precursors to more severe forms of dysregulation that constitute a core feature of all three externalizing disorders.
Conclusions
The present study provides important insights into the developmental course of externalizing problems in a sample of Mexican-origin youth, a critically important yet understudied ethnic group. The findings suggest that the developmental trajectories of ADHD, ODD, and CD symptoms of Mexican-origin youth are similar to (but do not exactly replicate) previous studies of non-Latino White youth. Moreover, gender and acculturation influenced the development of externalizing problems in interesting and complex ways. Our investigation further highlights the importance of taking into account the unique characteristics of ethnic minority youth and families, including sources of resilience such as traditional cultural values and practices, when constructing theories of externalizing problems and when designing interventions to reduce the incidence and escalation of problem behaviors in childhood and adolescence.
Supplementary Material
Acknowledgments
This research was supported by a grant from the National Institute on Drug Abuse and the National Institute on Alcohol Abuse and Alcoholism (DA017902) to Richard W. Robins and Rand D. Conger. We thank the participating families, staff, and research assistants who took part in this study.
Footnotes
We conducted attrition analyses comparing participants and non-participants at the Wave 8 (age 17) assessment on study variables measured at Wave 1 (age 10). There were no significant differences between those who remained in the study and those who dropped out on: ADHD, ODD, or CD symptoms (and related facets), gender, nativity status, or any of the cultural variables, ps >(07.
At the age 16 assessment, median years living in the U.S. for Mexican-born youth was 12.
All correlations between the growth trajectories (i.e., initial levels and slopes) of ADHD, ODD, and CD symptoms remained the same, in terms of magnitude and significance, when controlling for gender.
The slope variances were both negative, and thus, fixed at zero.
References
- Allen ML, Elliot MN, Fuligni AJ, Morales LS, Hambarsoomian K, Schuster MA. The relationship between Spanish language use and substance use behaviors among Latino youth: A social network approach. Journal of Adolescent Health. 2008;43:372–379. doi: 10.1016/j.jadohealth.2008.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- Barkley RA, Fischer M, Smallism L, Fletcher K. The persistence of attention-deficit/hyperactivity disorder into young adulthood as a function of reporting source and definition of disorder. Journal of Abnormal Psychology. 2002;111(2):279–289. [PubMed] [Google Scholar]
- Beauchaine TP, Hinshaw SP. The Oxford Handbook of Externalizing Spectrum Disorders. New York: Oxford University Press; 2015. [Google Scholar]
- Beauchaine TP, McNulty T. Comorbidities and continuities as ontogenic processes: Toward developmental spectrum model of externalizing behavior. Development and Psychopathology. 2013;25:1505–1528. doi: 10.1017/S0954579413000746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berkel C, Knight GP, Zeiders KH, Tein JY, Roosa MW, Gonzales NA, Saenz D. Discrimination and adjustment for Mexican-American adolescents: A prospective examination of the benefits of culturally-related values. Journal of Research on Adolescence. 2010;20:893–915. doi: 10.1111/j.1532-7795.2010.00668.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berkout OV, Young JN, Gross AM. Mean girls and bad boys: Recent research on gender differences in Conduct Disorder. Aggression and Violent Behavior. 2011;16:503–511. [Google Scholar]
- Burke JD, Hipwell AE, Loeber R. Dimensions of oppositional defiant disorder as predictors of depression and conduct disorder in preadolescent girls. Journal of American Academy of Child and Adolescent Psychiatry. 2010;49(5):484–492. doi: 10.1097/00004583-201005000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns GL, Walsh JA. The influence of ADHD-hyperactivity/impulsivity symptoms on the development of Oppositional Defiant Disorder symptoms in a 2-year longitudinal study. Journal of Abnormal Child Psychology. 2002;30:245–256. doi: 10.1023/a:1015102812958. [DOI] [PubMed] [Google Scholar]
- Burt SA, Krueger RF, McGue M, Iacono WG. Sources of covariation among attention-deficit/hyperactivity disorder, oppositional defiant disorder, and conduct disorder: The importance of shared environment. Journal of Abnormal Psychology. 2001;110:516–525. doi: 10.1037/0021-843X.110.4.516. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Rogosch FA. Equifinality and multifinality in developmental psychopathology. Development and Psychopathology. 1996;8:597–600. [Google Scholar]
- Cohen P, Cohen J, Kasen S, Velez CN, Hartmark C, Johnson J, Streuning EL. An epidemiological study of disorders in late childhood and adolescence, I: age and gender-specific prevalence. Journal of Child Psychology and Psychiatry. 1993;34:851–67. doi: 10.1111/j.1469-7610.1993.tb01094.x. [DOI] [PubMed] [Google Scholar]
- Costello EJ, Edelbrock CS, Costello AJ. Validity of the NIMH diagnostic interview schedule for children: A comparison between psychiatric and pediatric referrals. Journal of Abnormal Child Psychology. 1985;13:579–95. doi: 10.1007/BF00923143. [DOI] [PubMed] [Google Scholar]
- Cuellar I, Arnold B, Maldonado R. Acculturation rating scale for Mexican Americans-II: A revision of the original ARSMA scale. Hispanic Journal of Behavioral Sciences. 1995;17:275–304. doi: 10.1177/07399863950173001. [DOI] [Google Scholar]
- Davidson MA. ADHD in adults: A review of the literature. Journal of Attention Disorders. 2008;11(6):628–641. doi: 10.1177/1087054707310878. [DOI] [PubMed] [Google Scholar]
- Diamantopoulou S, Verhulst FC, van der Ende J. The parallel development of ODD and CD symptoms from childhood to adolescence. European Child and Adolescent Psychiatry. 2011;20:301–309. doi: 10.1007/s00787-011-0175-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fergusson DM, Horwood LJ, Ridder EM. Show me the child at seven: The consequences of conduct problems in childhood for psychosocial functioning. Journal of Child Psychology and Psychiatry. 2005;46(8):837–49. doi: 10.1111/j.1469. [DOI] [PubMed] [Google Scholar]
- Fontaine N, Carbonneau R, Vitaro F, Barker ED, Tremblay RE. Research review: A critical review of studies on the developmental trajectories of antisocial behavior in females. Journal of Child Psychology and Psychiatry. 2009;50(4):363–385. doi: 10.1111/j.1469-7610.2008.01949.x. [DOI] [PubMed] [Google Scholar]
- Garcia-Coll C, Crnic K, Lamberty G, Wasik BH, Jenkins R, Vazquez Garcia H, McAdoo HP. An integrative model for the study of developmental competencies in minority children. Child Development. 1996;67:1891–1914. [PubMed] [Google Scholar]
- Garcia-Coll C, Marks AK. The Immigrant Paradox in children and adolescents: Is becoming American a developmental risk? Washington DC: APA; 2011. [Google Scholar]
- Germán M, Gonzales NA, Dumka L. Familism values as a protective factor for Mexican-origin adolescents exposed to deviant peers. Journal of Early Adolescence. 2009;29:16–42. doi: 10.1177/0272431608324475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzales NA, Germán M, Kim SY, Dumka LE. Mexican-American adolescents’ cultural orientation, externalizing behavior and academic engagement: The role of traditional cultural values. American Journal of Community Psychology. 2008;41:151–164. doi: 10.1007/s10464-007-9152-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzales NA, Knight GP, Morgan-Lopez AA, Saenz D, Sirolli A. Acculturation and the mental health of Latino youths: An integration and critique of the literature. In: Contreras JM, Kerns KA, Neal-Barnett AM, editors. Latino children and families in the United States: Current research and future directions. Westport, CT: 2002. [Google Scholar]
- Harvey EA, Breaux RP, Lugo-Candelas CI. Early development of comorbidity between symptoms of ADHD and ODD. Journal of Abnormal Psychology. 2016;125(2):154–67. doi: 10.1037/abn0000090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvey EA, Metcalfe LA, Herbert SD, Fanton JH. The role of family experiences and ADHD in the early development of Oppositional Defiant Disorder. Journal of Consulting and Clinical Psychology. 2011;79(6):784–795. doi: 10.1037/a0025672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herzhoff K, Tackett JL. Subfactors of oppositional defiant disorder: Converging evidence from structural and latent class analyses. Journal of Child Psychology and Psychiatry. 2016;57(1):18–29. doi: 10.1111/jcpp.12423. [DOI] [PubMed] [Google Scholar]
- Javdani S, Sadeh N, Verona E. Expanding our lens: Female pathways to antisocial behavior in adolescence and adulthood. Clinical Psychology Review. 2011;31:1324–1348. doi: 10.1016/j.cpr.2011.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keenan K, Coyne C, Lahey BB. Should relational aggression be included in DSM-V? Journal of the American Academy of Child & Adolescent Psychiatry. 2008;47(1):86–93. doi: 10.1097/chi.0b013e31815a56b8. [DOI] [PubMed] [Google Scholar]
- Keenan K, Shaw D. Developmental and social influences on young girls’ early problem behavior. Psychological Bulletin. 1997;121:95–113. doi: 10.1037/0033-2909.121.1.95. [DOI] [PubMed] [Google Scholar]
- Keenan K, Wroblewski K, Hipwell AE, Loeber R, Stouthamer-Loeber M. Age of onset, symptom threshold, and expansion of the nosology of conduct disorder for girls. Journal of Abnormal Psychology. 2010;119:689–698. doi: 10.1037/a0019346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knight G, Gonzales NA, Saenz DS, Bonds DD, German M, Deardorff J, Updegraff KA. The Mexican American cultural values scale for adolescents and adults. Journal of Early Adolescence. 2010;30:444–481. doi: 10.1177/0272431609338178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kulis S, Marsiglia FF, Nagoshi JL. Gender roles, externalizing behaviors, and substance use among Mexican-American adolescents. Journal of Social Work and Practice in the Addictions. 2010;10:283–307. doi: 10.1080/1533256X.2010.497033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB, Schwab-Stone M, Goodman SH, Waldman ID, Canino G, Rathouz PJ, Jensen PS. Age and gender differences in oppositional behavior and conduct problems: A cross-sectional household study of middle childhood and adolescence. Journal of Abnormal Psychology. 2000;109(3):488–503. doi: 10.1037/0021-843X.109.3.488. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Van Hulle CA, Waldman ID, Rodgers JL, D’Onofrio BM, Keenan K. Testing descriptive hypotheses regarding sex differences in the development of conduct problems and delinquency. Journal of Abnormal Child Psychology. 2006;34:737–755. doi: 10.1007/s10802-006-9064-5. [DOI] [PubMed] [Google Scholar]
- Leadbeater BJ, Homel J. Irritable and defiant sub-dimensions of ODD: Their stability and prediction of internalizing symptoms and conduct problems from adolescence to young adulthood. Journal of Abnormal Child Psychology. 2015;43(3):407–421. doi: 10.1007/s10802-014-9908-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loeber R, Green SM, Keenan K, Lahey BB. Which boys will fare worse? Early predictors of the onset of conduct disorder in a six-year longitudinal study. Journal of the American Academy of Child and Adolescent Psychiatry. 1995;34:499–509. [PubMed] [Google Scholar]
- Loeber R, Burke JD, Pardini DA. Development and etiology of disruptive and delinquent behavior. Annual Review of Clinical Psychology. 2009;5:291–310. doi: 10.1146/annurev.clinpsy.032408.153631. [DOI] [PubMed] [Google Scholar]
- Marsiglia FF, Ayers SL, Hoffman S. Religiosity and adolescent substance use in Central Mexico: Exploring the influence of internal and external religiosity on cigarette and alcohol use. American Journal of Community Psychology. 2012;49(1):87–97. doi: 10.1007/s10464-011-9439-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maughan B, Rowe R, Messer J, Goodman R, Meltzer H. Conduct Disorder and Oppositional Defiant Disorder in a national sample: Developmental epidemiology. Journal of Child Psychology and Psychiatry. 2004;45(3):609–621. doi: 10.1111/j.1469-7610.2004.00250.x. [DOI] [PubMed] [Google Scholar]
- Moffitt TE. Life-course persistent versus adolescence-limited antisocial behavior. In: Cicchetti D, Cohen DJ, editors. Developmental psychopathology: Risk, disorder, and adaptation. New York: Wiley; 2006. pp. 570–598. [Google Scholar]
- Moffitt T, Caspi A, Rutter M, Silva P. Sex differences in antisocial behavior: Conduct disorder, delinquency and violence in the Dunedin longitudinal study. New York: Cambridge University Press; 2001. [Google Scholar]
- Moffitt TE, Caspi A. Childhood predictors differentiate life-course persistent and adolescence-limited antisocial pathways among males and females. Development and Psychopathology. 2001;13:355–375. doi: 10.1017/S0954579401002097. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. 6. Los Angeles, CA: 1998–2011. [Google Scholar]
- Nock MK, Kazdin AE, Hiripi E, Kessler RC. Lifetime prevalence, correlates, and persistence of Oppositional Defiant Disorder: Results from the National Comorbidity Survey Replication. Journal of Child Psychology and Psychiatry. 2007;48(7):703–13. doi: 10.1111/j.1469-7610.2007.01733.x. [DOI] [PubMed] [Google Scholar]
- Ohan JL, Johnston C. Gender appropriateness of symptom criteria for Attention-Deficit Hyperactivity Disorder, Oppositional Defiant Disorder, and Conduct Disorder. Child Psychiatry and Human Development. 2005;35(4) doi: 10.1007/s10578-005-2694-y. [DOI] [PubMed] [Google Scholar]
- Pingault JB, Viding E, Galera C, Greven C, Zheng Y. Genetic and environmental influences on the developmental course of ADHD symptoms from childhood to adolescence. Journal of the American Medical Association of Psychiatry. 2015;72(7):651–658. doi: 10.1001/jamapsychiatry.2015.0469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pottick KJ, Kirk SA, Hsieh DK, Tian X. Judging mental disorder: Effects of client, clinician, and contextual differences. Journal of Consulting and Clinical Psychology. 2007;75:1–8. doi: 10.1037/0022-006X.75.1.1. [DOI] [PubMed] [Google Scholar]
- Rucklidge JJ. Gender differences in Attention-Deficit/Hyperactivity Disorder. Psychiatric Clinics of North America. 2010;33(2):357–373. doi: 10.1016/j.psc.2010.01.006. [DOI] [PubMed] [Google Scholar]
- Sasser TR, Kalvin CB, Bierman KL. Developmental trajectories of clinically significant ADHD symptoms from grade 3 through 12 in a high-risk sample: Predictors and outcomes. Journal of Abnormal Psychology. 2016;125:207–19. doi: 10.1037/abn0000112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz SJ, Unger JB, Zamboanga BL, Szapocznik J. Rethinking the concept of acculturation: Implications for theory and research. American Psychologist. 2010;65(4):237–51. doi: 10.1037/a0019330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein GL, Gonzalez LM, Cupito AM, Kiang L, Supple AJ. The protective role of familism in the lives of Latino adolescents. Journal of Family Issues. 2014;36:1255–73. [Google Scholar]
- SAMHSA. Mental disorders. 2015 http://www.samhsa.gov/disorders/mental.
- Teruya SA, Bazargan-Hejazi S. The immigrant and Hispanic paradoxes: A systematic review of their predictions and effects. Hispanic Journal of Behavioral Science. 2013;35(4):486–509. doi: 10.1177/0739986313499004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tiet QQ, Wasserman GA, Loeber R, Miller LS. Developmental and sex differences in types of conduct problems. Journal of Child and Family Studies. 2001;10:181–197. [Google Scholar]
- Tremblay M, Duchesne S, Vitaro F, Tremblay RE. Developmental trajectories of oppositional behavior during elementary school and their risk factors. Journal of Educational and Developmental Psychology. 2013;3(1):234–243. doi: 10.5539/jedp.v3n1p234. [DOI] [Google Scholar]
- Tuvblad C, Zheng M, Raine A, Baker LA. A common genetic factor explains the covariation among ADHD, ODD, and CD symptoms in 9–10 year old boys and girls. Journal of Abnormal Child Psychology. 2009;37:153–167. doi: 10.1007/s10802-008-9278-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Lier PAC, van der Ende J, Koot HM, Verhulst FC. Which better predicts conduct problems? The relationship of trajectories of conduct problems with ODD and ADHD symptoms from childhood into adolescence. Journal of Child Psychology and Psychiatry. 2007;48(6):601–608. doi: 10.1111/j.1469-7610.2006.01724.x. [DOI] [PubMed] [Google Scholar]
- Waschbush DA. A meta-analytic examination of comorbid hyperactive-impulsive-attention problems and conduct problems. Psychological Bulletin. 2002;28:118–150. doi: 10.1037/0033-2909.128.1.118. [DOI] [PubMed] [Google Scholar]
- Wheeler LA, Zeiders KH, Updegraff KA, Umana-Taylor AJ, Rodriguez de Jesus SA, Perez-Brena NJ. Mexican-origin youth’s risk behavior from adolescence to young adulthood: The role of familism values. Developmental Psychology. 2017;53:126–137. doi: 10.1037/dev0000251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willoughby MT. Developmental course of ADHD symptomatology during the transition from childhood to adolescence: A review with recommendations. Journal of Child Psychology and Psychiatry. 2003;44:88–106. doi: 10.1111/1469-7610.t01-1-00104. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.