Abstract
Parent history of psychopathology is an established marker of children’s own risk for later disorder, and can therefore be used as a means of validating other risks, such as child temperament. While associations between children’s temperament and parent psychopathology have been reported, few studies have used observational measures of child temperament or examined trait interactions, particularly between children’s affective and regulatory traits such as Effortful Control (EC). In this bottom-up, family study of 968 3-year-olds and their parents, we examined interactions between preschoolers’ observed positive and negative affectivity (PA and NA) and EC as predictors of a known marker of psychopathology risk: parent history of disorder. Children with lower PA had an increased probability of paternal depression history in the context of higher child NA. In addition, children with lower EC and higher NA had an increased probability of maternal anxiety. Findings shed new light on the main effects and interactions that account for associations between child temperament and parent history of disorder, one of the best-established markers of an individual’s own risk for future disorder, implicating reactive and regulatory traits that merit special consideration in future longitudinal work.
Keywords: Child temperament, family study, effortful control, positive affectivity, negative affectivity, psychopathology risk
Introduction
Models of temperament have converged to indicate that trait-like aspects of emotional reactivity and regulation account for much of the substantive variability in individual differences in child- and adulthood1–3. Although the specifics of conceptual models vary, most contemporary theories emphasize trait-like differences in affective reactivity 1,4 and regulation.1,2,5,6 Indeed, virtually all prominent models of both child and adult temperament include higher-order factors comprised of affective and regulatory traits 3,7, highlighting the explanatory power of these constructs for behavior across the lifespan.
In addition to characterizing normative individual differences, temperament constructs have also been invoked as a means of understanding vulnerability to psychopathology7,8 (see 9 for a discussion of the processes by which temperament-disorder links may emerge); many of these models have focused on three key traits,7 which are negative affectivity (NA), positive affectivity (PA), and a regulatory dimension typically referred to as either disinhibition on the low end, or constraint or effortful control (EC). NA is implicated in virtually all forms of psychopathology,7 and may be best understood as a trait that differentiates impaired from adaptive psychological functioning 10. Low PA may show more specific associations with select disorders such as depression, certain anxiety disorders, and possibly schizophrenia.8 While much of the aforementioned work has focused on adolescents and adults, deficits in self-regulation (hereafter referred to as Effortful Control/EC) in both adults and young children have been implicated in externalizing psychopathology 7,11, with associations between EC and internalizing disorders showing a more mixed pattern 11–13, with both higher and lower EC linked to internalizing symptoms.
We describe relevant work in the following section, where we focus on studies of temperamental risk for psychopathology that have used observational measures of child temperament. Although the literature is replete with work on temperament-disorder links, the vast majority of research has used questionnaire measures, which may be subject to reporting biases 11,12,14. This is of particular concern in studies of child temperament, which almost always draw on parent reports as the source of information on children’s individual differences. While affordable and broad in coverage of child behavior across contexts and time, parent reports capture both objective aspects of child behavior as well as parent characteristics such as symptoms and personality,15,16 and typically show poor convergence with other measures 17. Further, many studies of child temperament and risk rely on parent reports of both youth temperament and psychopathology, potentially inflating associations between temperament and symptoms and other risk markers due to shared methods and informant biases. In contrast, laboratory observation measures of child temperament serve the critical function of eliminating monomethod bias. Laboratory indices of child temperament have other advantages, such as the use of standardized stimuli and objective coding to minimize rater bias, and the capacity to elicit child behaviors that may be present at lower rates in naturalistic settings.18
Using a bottom-up family study design, whereby family history of disorder serves as the outcome and putative vulnerabilities are the predictor of such outcomes, Durbin, Klein, Hayden, Buckley, and Moerk19 examined associations between parent depression as a marker of children’s own depression risk, and children’s observed positive and negative emotionality, related albeit broader conceptualizations of PA and NA. Associations between children’s low positive emotionality and maternal depression history were found; positive emotionality was unrelated to maternal anxiety or substance use disorder, and paternal disorder. Using composite observational ratings of children’s temperament in a follow-up of this same sample, Dougherty et al.20 found that lower PE at age 3 predicted greater depressive symptoms in children at age 10. While providing support for observed child temperament as a marker of psychopathology risk, both these studies used a relatively small sample. In a high-risk offspring study, Olino et al.21 found that children of mothers with childhood-onset depression had lower PA in late infancy and throughout childhood. A more recent, larger family study of a larger sample of 3-year-olds (N = 536)22 found complex associations between positive and negative emotionality in predicting parent depression: surprisingly, higher levels of negative emotionality were associated with a higher likelihood of having a depressed parent only in children with moderate to high positive emotionality. Kotelnikova et al.23 recently found that children’s low EC assessed via laboratory methods was associated with steeper increases in depressive symptoms in middle childhood; otherwise, there is surprisingly little published on associations between observed EC and markers of psychopathology risk.
Other significant gaps in knowledge remain regarding the nature of associations between temperament and disorder risk. First, surprisingly little is known is about whether PA and NA interact either with each other or with EC in predicting risk, such that the association between an individual temperament factor and risk is either reduced or increased based on another trait. For example, high NA may be more strongly associated with depression risk markers when PA is low; this would be consistent with models positing that positive emotions mitigate the associations between other vulnerabilities and negative outcomes 7,24,25. Additionally, lower EC may result in difficulties managing negative emotions, such that those with high NA who also have more difficulty regulating such emotions are at the greatest risk for disorder.11 Characterizing such interactions may be key for developing more precise models of risk, as any individual trait is unlikely to account for more than modest variance. Additionally, unlike more complex individual difference factors, the basic temperament traits described above can be reliably measured in early childhood,18 broadening the period of development in which risk can be identified, potentially extending the window for prevention and early intervention. However, greater precision in modeling temperamental risk may enhance targeted early intervention and preventative efforts.
Although interactions are likely important in shaping vulnerability, most observational studies of child temperament have focused on direct associations between traits and risk. This is likely because such studies, due to the expense of observational data, tend to use smaller samples and thus have less power to test interactions. In the current study, we examined associations between observational measures of children’s temperamental reactivity and regulation, specifically PA, NA, and EC, and an established risk marker of psychopathology: parent history of disorder.26 We combined two large, independent samples of families of young children, allowing us to test models in almost 1,000 preschool-aged children, by far the largest sample assessed for temperament via structured laboratory observational methods. We examined associations between parent disorder and temperament in preschoolers as these children are prior to the age of risk for the onset of many major forms of psychopathology,27 thus facilitating the examination of aspects of temperamental emotionality that are less likely to be contaminated by current or past disorder, a significant problem when using older individuals.
We focused on cross-sectional associations between child temperament and risk (as indexed by parental psychopathology) for practical reasons: prospective studies of children are quite expensive, requiring decades of follow-up since the incidence of some disorders does not peak until adulthood.28 Although longitudinal studies are essential for testing causal models, determining whether putative markers of vulnerability are associated cross-sectionally with more established risk markers, such as family history, is a crucial short-term strategy. When descriptive studies indicate that risk for disorder “runs in families,” complementary, more expensive work can be undertaken that is aimed at teasing apart the genetic and environmental mechanisms that account for this familiality.29
We conducted these analyses within the well-established, “bottom-up” family study framework26, in which temperament in child probands served as the predictor of risk, as indicated by familial history of disorder. While the family study method is one of the oldest methodologies used in psychopathology research,30 it continues to be widely used in contemporary research 31 because of its potential to inform our understanding of familial contributions to psychopathology. Our design follows the classic framework outlined in Zubin and Spring,32 who describe the merit of gathering supporting evidence for a putative vulnerability marker by examining whether it differs cross-sectionally between high and low risk groups (e.g., in those with and without a family history of disorder) before conducting longitudinal studies to test prospectively whether the vulnerability predicts onset of disorder. While many family studies look at patterns of disorder in families, we examined child temperament-parent disorder links as a means of establishing whether temperament traits that putatively play a mechanistic role in disorder are associated reliably with what is arguably the best-established marker of psychopathology risk: family history. We examined links between child temperament and both mothers’ and fathers’ history of disorder, in contrast to much of the literature, which has focused on maternal disorder only.33
Based on theory,7 we expected that higher child NA would be generally related to parent history of multiple disorders, and that lower child PA would be tied most closely to parental history of depressive and perhaps anxiety disorders 8,34. However, we also examined interactions between trait vulnerabilities. There is little extant research on trait interactions in child temperament and how these might relate to risk, which speaks to the importance of the current study while also limiting our ability to make strong hypotheses based on past work. Nevertheless, we anticipated that children’s PA and NA would interact in relating to parental depression, such that child low PA and high NA would be associated with higher rates of depression in parents. In addition, we expected that higher EC would moderate associations between parent disorder history and children’s observed low PA or high NA, reducing associations between these traits and parental disorder.
Method
The sample was 968 three-year-old children and their biological parents from two independent samples. Site 1 consisted of 559 families from a suburban community in New York, USA. Related data from a subset of this sample were previously reported22. Children were 42.2 months old (SD = 3.1); 289 (53.9%) were boys. Mothers were 36.0 years old (SD = 4.5) and fathers were 38.3 years old (SD = 5.4). Most participants (86.9%) were White and middle class, as measured by Hollingshead’s Four Factor Index of Social Status (M = 45.1; SD = 10.9). Children were of average cognitive ability according to the Peabody Picture Vocabulary Test (PPVT35; M = 102.9, SD = 13.9).
Site 2 was 409 children from a suburban community in Ontario, Canada (see 36). Children were 40.7 months old (SD = 3.51); 201 (49.1%) were boys. Mothers were 35.8 years old (SD = 4.6) and fathers were 37.5 years old (SD = 4.8). Most participants (93.4%) were White, and middle class as measured by annual family income data (5.5% < $20,000; 11% = $20,000 – $40,000; 22.7% = $40,001 – $70,000; 31.2% = $70,001 – $100,000; 29.5% > $100,001). Children were of average cognitive ability (PPVT35; M = 111.9, SD = 14.3).
Children in both samples were administered the same battery of observational tasks, and similar measures of child symptoms and parent psychopathology were collected in both studies. Study procedures were identical across both sites except where noted. The appropriate ethics committee approved study procedures at both institutions; thus, both studies were conducted in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. In terms of demographic variables, the two samples did not differ significantly in terms of proportion that were boys or proportion that were White, or parent age (all ps > .16); however, children in Site 2 were significantly younger and had higher PPVT scores than children in Site 1 (ps < .001), although these site differences did not influence our findings.
Child Temperament
Each child completed a 2-hr observational laboratory assessment of temperament that included 10 standardized episodes from the Laboratory Temperament Assessment Battery (Lab-TAB37)1. Each task was videotaped through a one-way mirror. To prevent carryover effects, no episodes presumed to evoke similar affective responses occurred consecutively and each episode was followed by a brief play break to allow the child to return to a baseline state. A parent was in the room with the child for all episodes except “Stranger Approach” and “Box Empty” (see below) but was instructed not to interact with the child (except in “Pop-Up Snakes”) and was seated facing away from the experimenter and child and given questionnaires to complete. The episodes were as follows:
Risk Room
Child explored a set of novel and ambiguous stimuli, including a Halloween mask, balance beam, and black box.
Tower of Patience
Child and experimenter alternated turns in building a tower of blocks. The experimenter took increasing amounts of time before placing her block.
Stranger Approach
Child was left alone briefly in the room before a male accomplice entered, speaking to the child while slowly walking closer.
Make That Car Go
Child and experimenter raced remote-controlled cars.
Transparent Box
Experimenter locked an attractive toy in a transparent box, leaving the child alone with a set of nonworking keys. After a delay, the experimenter returned and explained that she had left the wrong keys. The child used the new keys to access the toy.
Pop-Up Snakes
Child and experimenter surprised the parent with a can of potato chips that actually contained coiled snakes.
Impossibly Perfect Green Circles
Experimenter repeatedly asked the child to draw a circle on a large piece of paper, mildly criticizing each attempt.
Popping Bubbles
Child and experimenter played with a bubble-shooting toy.
Snack Delay
Child was instructed to wait for the experimenter to ring a bell before eating a snack. The experimenter systematically increased the delay before ringing the bell.
Box Empty
Child was given an elaborately wrapped box to open under the impression that a toy was inside. After the child discovered the box was empty, the experimenter returned with several toys for the child to keep.
Coding procedures
Coders were trained graduate and undergraduate student coders, as well as study staff, who were unaware of information on parental psychopathology or child symptomatology. Coders were trained by calibrating their ratings against a “master coder” who had themselves been trained by a study author (either KRK, EPH, CED, or TMO). In the process of learning to code an episode, new coders were required to meet a minimum standard of agreement with the master coder (interrater correlation coefficient [ICC] = .80) on ratings of ~20 separate episodes (i.e., ~20 child participants, depending on how challenging a given episode typically was to code, completing the same episode), and any coding discrepancies were discussed during regular coder meetings. For each episode, each display of facial, bodily, and vocal positive affect, fear, sadness, and anger was rated on a 3-point scale (low, moderate, high). Ratings were summed separately within each channel (facial, bodily, vocal) across the 10 episodes, standardized, and summed across the three channels to derive composite scores for positive affect, fear, sadness, and anger. Positive Affectivity (PA) consisted of the sum of the standardized total positive affect variables. Negative Affectivity (NA) was the sum of the 2005 standardized total sadness, fear, and anger variables (see 19,22 for similar procedures). PA and NA had adequate internal consistency (Site 1 α = .82 and .74, respectively; Site 2 α = .89 and .81, respectively) and interrater reliability (Site 1 N = 28, ICCs = .89 and .82, respectively; Site 2 N = 18, ICCs = .67 and .62, respectively).
As an index of EC, Snack Delay and Tower of Patience were coded for child prompts to the experimenter, self-directs (e.g., reaching for the candy but withdrawing the hand), and failures to wait to take their turn (see 38–40 for similar procedures). Each index was averaged across each trial and then across tasks to create an aggregate scale. The three indices were then standardized and aggregated to create an overall EC score. As more prompting, self-directs, and failures to wait reflect lower EC, scores were reverse-coded to ease interpretation; thus, higher EC scores in this study reflect greater EC. EC exhibited good interrater reliability (Site 1 N = 8, ICC = .98, Site 2 N = 8, ICC = .95).
Parental Psychopathology
Children’s biological parents were interviewed for a lifetime history of disorder using the Structured Clinical Interview for DSM–IV, Non-Patient Version (SCID–NP41), either face-to-face or by telephone. Interviews were conducted by masters- or doctoral-level clinical psychology students with no knowledge of child temperament or symptom data. When biological parents were unavailable and the informant was sufficiently knowledgeable, family history interviews were conducted with the coparent (one mother and 84 fathers at Site 1; one mother and one father at Site 2). Parent psychopathology data were obtained from 932 (96.3%) mothers and 797 (82.3%) fathers. Based on audiotapes of SCID–NP interviews, kappas for interrater reliability of lifetime diagnoses were as follows: Site 1: kappa = .93 for depression, .91 for anxiety disorder, and 1.00 for substance dependence, N = 30; Site 2: kappa = 1.00 for depression, 1.00 for anxiety disorder, and 1.00 for substance dependence, N = 33). Combining the two sites, 29.6% of mothers and 15.4% of fathers had a lifetime depressive disorder; 32.6% of mothers and 17.6% of fathers had a lifetime anxiety disorder; and 5.3% of mothers and 8.4% of fathers had lifetime history of substance dependence. Of note, substance abuse was not included in analyses as dependency symptoms appear to be the strongest and most consistent predictor of adverse child outcomes.42
Data Analyses
We examined main effects of child PA, NA, and EC as well as two- and three-way interactions in association with lifetime maternal and paternal depressive and anxiety disorders and substance dependence using hierarchical logistic regression. As the current study is a bottom-up family study design, child temperament variables were treated as independent variables and parental psychopathology was the dependent variable as a marker of child disorder risk. However, it is important to note that designations of independent and dependent variables are arbitrary in cross-sectional, correlational analyses such as these, which aim to describe associations between child temperament and parent disorder rather than elucidating underlying causal processes. Because some aspects of NA are more closely linked to externalizing problems than others (e.g., anger43), follow-up analyses were performed in which significant interactions involving NA were further probed with 3 parallel models substituting anger, sadness, and fear for NA to examine whether specific aspects of NA were responsible for significant effects obtained. We initially explored three-way interactions between EC, PA, and NA, and two-, three-, and four-way interactions involving child sex. However, none of these was significant and therefore not considered further (results available from the first author).
The two sites differed significantly in the number of children with a history of maternal depression (x2(1) = 4.37, p = .04; Site 1 N = 174, 31.1%; Site 2 N = 102, 24.9%), maternal anxiety (x2(1) = 38.07, p < .01; Site 1 N = 219, 39.2%; Site 2 N = 84, 20.5%), paternal anxiety (x2(1) = 28.18, p < .01; Site 1 N = 107, 19.1%; Site 2 N = 33, 8.1%), maternal substance dependence (x2(1) = 4.88, p = .03; Site 1 N = 21, 3.8%; Site 2 N = 28, 6.8%), and paternal substance dependence (x2(1) = 4.37, p = .04; Site 1 N = 26, 4.7%; Site 2 N = 41, 10.0%). Children across sites did not differ in mean temperament scores (ps > .87). A site code was created (Site 1 = 0; Site 2 = 1) and included in all models to control for cross-site variability, although analyses without this variable yielded highly comparable results. To further address the possibility of site differences influencing our findings, we also examined whether site moderated any significant effects reported; no significant interactions with site were found.
Results
Table 1 shows correlations between major study variables. Given our large sample size, many modest correlations attained statistical significance; such marginal associations are not discussed here, where we focus on correlations of at least .20 or greater. Lifetime depression and anxiety were associated with one another in both mothers and fathers. Associations between child NA, PA, and EC were modest (<.20).
Table 1.
Correlations between all major study variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. PPVT | - | ||||||||||||
| 2. Child Sex | .07* | - | |||||||||||
| 3. Child Age (months) | .07* | .02 | - | ||||||||||
| 4. Child Race | .06† | −.01 | −.06* | - | |||||||||
| 5. Maternal Depression | −.04 | .01 | −.00 | −.04 | - | ||||||||
| 6. Paternal Depression | −.05 | .05 | −.04 | −.03 | .09* | - | |||||||
| 7. Maternal Anxiety | −.03 | −.03 | .03 | −.02 | .29** | .10** | - | ||||||
| 8. Paternal Anxiety | −.09* | −.06 | .05 | −.07* | .16** | .27** | .14** | - | |||||
| 9. Maternal Substance Dependence | .05 | .07* | −.05 | .05 | .10** | .10** | .09* | .01 | - | ||||
| 10. Paternal Substance Dependence | .08* | .06† | −.03 | −.03 | .08* | .14** | .00 | .02 | .17** | - | |||
| 11. EC | .08* | .10* | .05 | .06 | −.06† | −.04 | −.01 | −.04 | −.03 | .00 | - | ||
| 12. PA | .08** | .03 | .15** | .04 | .00 | .01 | −.02 | −.00 | −.01 | −.01 | −.17** | - | |
| 13. NA | −.06† | −.04 | −.05 | .00 | .04 | .07* | .01 | .02 | .05 | .00 | −.16** | −.02 | - |
| Mean (SD) | 106.67 (14.73) | - | 41.80 (3.36) | - | - | - | - | - | - | - | 0 (1.00) | 0 (1.00) | 0 (1.00) |
Note: PPVT = Peabody Picture Vocabulary Test; Child sex = males 0, females 1; Child Race = 0 non-white, 1 white; Maternal/Paternal Anxiety/Depression/Substance Dependence = 0 no disorder, 1 disorder; EC = Effortful Control; PA = Positive Affect; NA = Negative Affect.
p < .01;
p < .05;
< .10
Maternal and Paternal Depression
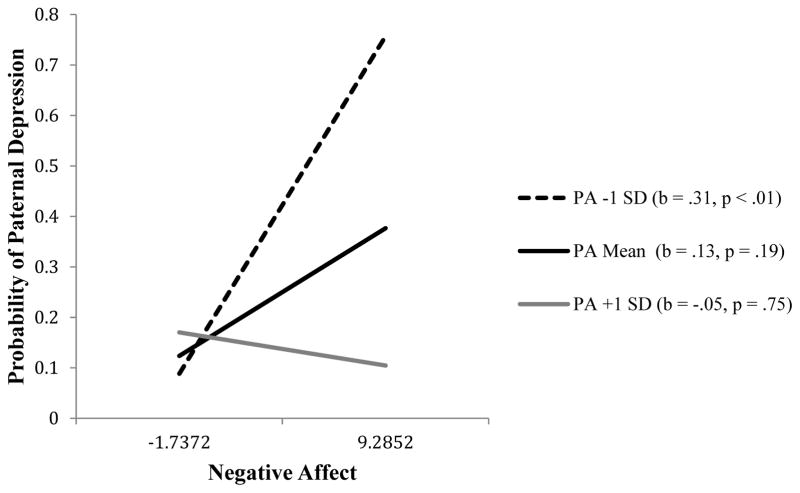
In the model predicting maternal depression history, no significant main effects were found for child temperament traits, nor were the PA-NA, NA-EC, or the PA-EC interactions associated with maternal depression (ps > .07). For paternal depression, the Hosmer and Lemeshow test of the full model was nonsignificant, [X2 (8) = 5.506, p = .702], indicating that the model’s estimates fit the data at an acceptable level. In this model, the main effect of NA was significant, with higher levels of child NA associated with a greater probability of paternal depression history; however, this was qualified by a significant PA-NA interaction (b = −.18, SE = .09, p = .04; see Table 2). Simple slopes tests indicated that at low child PA, increases in child NA were associated with a greater probability of paternal depressive disorder (−1 SD: b = .31, SE = .11, p < .01). In contrast, at moderate/average-to-high (+1 SD) child PA, there was no association between child NA and paternal depression (mean: b = .13, SE = .10, p = .19; +1 SD: b = −.05, SE = .16, p = .75; see Figure 1). Follow-up analyses exploring separate facets of NA indicated that child fear largely accounted for the NA-PA interaction (fear X PA: b = −.24, SE = .12, p = .04) and yielded a consistent pattern of simple slopes to those for NA overall; the PA-sadness and PA-anger interactions were not significant (ps > .35).
Table 2.
Multiple Logistic Regression Model of the Association Between Child Temperament and Paternal Depression, Maternal Anxiety
| Paternal Depression | Maternal Anxiety | |||
|---|---|---|---|---|
| Odds Ratio | 95% Confidence Interval | Odds Ratio | 95% Confidence Interval | |
| Site Code | 0.72 | [0.48, 1.08] | 0.39 | [0.29, 0.52]* |
| EC | 0.90 | [0.74, 1.10] | 1.00 | [0.86, 1.15] |
| PA | 1.06 | [0.87, 1.28] | 0.94 | [0.82, 1.09] |
| NA | 1.14 | [0.94, 1.39] | 1.05 | [0.90, 1.22] |
| EC X PA | 1.11 | [0.93, 1.32] | 0.99 | [0.87, 1.12] |
| EC X NA | 0.96 | [0.79, 1.16] | 0.86 | [0.74, 0.99]* |
| PA X NA | 0.84 | [0.70, 0.99]* | 1.00 | [0.87, 1.15] |
Note.
p ≤ .05; EC = Effortful Control; PA = Positive Affect; NA = Negative Affect
Figure 1.
The association between child NA and the probability of paternal depression as a function of child PA.
Maternal and Paternal Anxiety
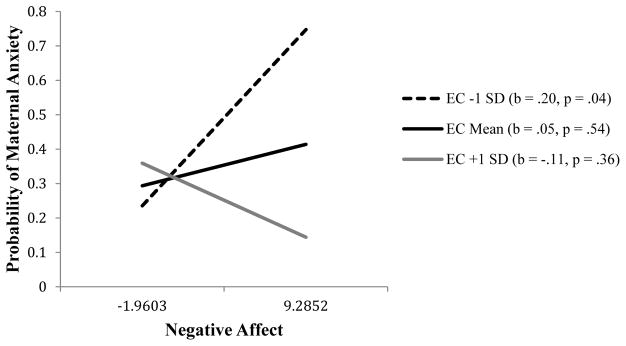
There were no significant main effects of child temperament in the models predicting maternal or paternal anxiety disorder history (ps > .28), nor were the PA-NA, NA-EC, or the PA-EC interactions associated with paternal anxiety (ps > .49). However, a significant EC-NA interaction was found in the model for maternal anxiety disorder (b = −.15, SE = .08, p = .04; see Table 2). The Hosmer and Lemeshow test of this full model was nonsignificant, [X2 (8) = 9.25, p = .322], indicating that its estimates fit the data at an acceptable level. Simple slopes tests indicated that at low child EC, increases in child NA were associated with a greater probability of maternal anxiety disorder (−1 SD: b = .20, SE = .10, p = .04). In contrast, at average-to-high (+1 SD) child EC, there was no association between child NA and maternal anxiety (mean: b = .05, SE = .08, p = .54; +1 SD: b = −.11, SE = .11, p = .36; see Figure 2). Follow-up analyses exploring separate facets of NA showed a trend-level interaction between EC and fear (b = −.16, SE = .08, p = .06) that showed a pattern of simple slopes consistent to that for the overall NA-EC interaction; the EC X sadness and EC X anger interactions were not significant (ps > .11).
Figure 2.
The association between child NA and the probability of maternal anxiety as a function of child EC.
Maternal and Paternal Substance Dependence
There were no significant main effects or PA-NA, NA-EC, or PA-EC interactions in the models predicting maternal (ps > .32) or paternal (ps > .29) substance dependence history.
Discussion
Surprisingly, many of the major theories of temperament-disorder associations do not address the role of non-additive influences of traits on risk44. Of the few family studies testing trait interactions 22, none has tested interactions between facets of temperamental reactivity and regulation. Further, much of the past work on this topic has examined older individuals that fall into the period of risk for disorder, which is problematic, as the assessment of temperament may be influenced by current or prior disorder. Additionally, the vast majority of past work has relied solely on questionnaire methods of assessing temperament and risk 45–47, which may artificially inflate associations between constructs. Our study sheds new light on the role of child temperamental risk for psychopathology by testing the associations of interactions between young children’s temperamental reactivity and self-regulation with parent psychopathology using independent measures of study constructs, including structured laboratory observational temperament measures. We were able to test more complex models of interplay among traits as we used the largest dataset of children observationally characterized on temperament that we know of. Our findings contribute important new knowledge regarding relations between risk and early temperament in a sample of children prior to the age of onset of most major forms of psychopathology. Although cross-sectional, our study speaks to the role of non-additive trait markers of children’s psychopathology risk, as indexed by parental psychopathology, and suggests models of trait interactions that should be explored using longitudinal methods.
Our results indicate that there are meaningful interactions between observed PA and NA in the association between child temperament and parental depression that are consistent with prior theory and research. In particular, we found that children’s high NA was related to a greater likelihood of having a paternal depression history when child PA was low. These findings are consistent with other recent research implicating paternal depression in temperament interactions predicting another marker of child risk, cortisol reactivity to stress 48, and with work suggesting that deficits in PA enhance the influence of other vulnerabilities 24, including higher NA in the current study. Further, when we examined facets of NA, child fear appeared central to explaining the interaction between NA and PA in the model for fathers’ depression; anger and sadness did not show significant interactions with PA. High child behavioral inhibition (BI)/fearfulness has been implicated in anxiety disorders risk49,50; it is possible that the pattern of temperamental risk implicated in our data could ultimately prove important in understanding the widespread comorbidity between depression and anxiety given that fear, in the context of other traits, predicted children’s risk for both anxiety and depression as indexed via parental history of disorder . However, this pattern of findings is somewhat discrepant to that reported by Olino and colleagues,22 who found that high BI was associated with a greater probability of parental depression only at moderate to high levels of PE in a subset of the same participants included in the current study. However, Olino and colleagues22 operationalized temperament more broadly, including both behavioral and affective markers of traits; in contrast, in the present study, we focused purely on affective behaviour. Additionally, Olino et al.22 did not include regulatory aspects of temperament in models, which could have contributed to discrepant results as well.
Surprisingly, we did not find associations between child temperament and maternal depression history. Many previous studies finding associations between maternal depression and child vulnerability have selectively recruited depressed mothers, which would increase power to detect such effects; thus, it is possible that the low-risk nature of our unselected community participants influenced our ability to detect associations between children’s vulnerability and maternal depression. Having said that, other observational studies of child temperament in unselected community samples have reported associations with maternal depression.19,22 As was the case with the paternal depression findings, differences in how temperament was operationalized and the inclusion of EC in current models could have contributed to the different pattern of effects between our sample and previous studies in community samples.
We found that the interaction of child EC with NA was associated with a greater probability of maternal anxiety history, such that children with low EC and high NA had the greatest likelihood of having a mother with a history of anxiety, our marker of children’s own risk for anxiety given the well-established familial aggregation of anxiety51. Further, this pattern of findings appeared to be due largely to child fear, rather than other facets of NA (i.e., anger, sadness). This pattern suggests that children high in fearfulness may be at the greatest risk for poor outcomes when they lack the self-regulatory capacity to downregulate such emotional responses. However, longitudinal data are needed to adequately test such models over time.
We did not find any significant associations between temperament traits and maternal or paternal substance dependence; however, some research suggests that children’s temperamental risk for substance use disorders becomes more evident later in childhood, after the preschool period.52 It is also possible that conceptualizations of temperament need to emphasize reward and punishment sensitivity, or sensation-seeking, in order to tap temperamental aspects of risk for substance use 53; while our coding captured elements of these constructs, it was focused more specifically on emotion expression. Additionally, while three-way interactions between questionnaire-assessed temperament traits have been documented in the literature on older children,54 we did not find evidence of these in our sample. As noted, methodological differences may account for this difference in findings; relatedly, it is also possible that subjective aspects of emotional experience show distinct patterns of associations with risk not found when considering only overt manifestations of emotion. It could also be that more complex, three-way interactions between traits become more important later in development, due to changes in children’s environments with age or other dynamic factors.
Our study had numerous strengths, including an especially large sample size for a study using laboratory measures of temperament. We used structured clinical interviews for parental psychopathology conducted by clinicians blind to child temperament data; thus, measures of study constructs were obtained from independent sources. We examined associations between trait interactions and risk in young children prior to the age of risk for many forms of psychopathology, decreasing the likelihood that child temperament was influenced by past or current disorder. It is also noteworthy that we examined links between putative trait vulnerabilities in children and both mothers’ and fathers’ history of disorder, in contrast to much of the literature, which has focused on maternal disorder only.33
However, our study also had limitations. First, we tested our models using cross-sectional data with the goal of elucidating associations between child temperament and familial risk. Although our data provide important clues regarding which traits may be most relevant to children’s development of disorder, establishing causal links between temperament and disorder requires longitudinal work to examine temporal associations between constructs. For example, the cross-sectional associations observed in this study could reflect dynamic, transactional relationships between parent and child behavior27 or the effects of “third variables,” such as shared genetic influences on child temperament and parent disorder.9 Second, although we included site as a covariate to address this possibility, we cannot rule out the possibility that sample differences influenced the pattern of findings obtained. Further, differences in mean levels of study constructs between sites (e.g., parent psychopathology) do not imply differences in relationships between study constructs (i.e., parental disorder and child temperament) between the two sites; indeed, the nonsignificance of tests of interactions of findings with study site indicate that the pattern of findings obtained was consistent across sites. Finally, we limited our tests of facet-level aspects of NA (i.e., anger, fear, sadness) to follow-up analyses, pursued when an interaction with NA broadly defined was significant. This was a conservative approach taken as a means of limiting the number of analyses conducted, although it is possible that we may have overlooked other interactions with facet-level aspects of NA as a result.
In conclusion, we add to the existing literature linking early childhood temperament and risk for psychopathology, indicating that both temperamental reactivity and regulatory components should be considered when developing models of risk. Future longitudinal research is needed to understand the processes responsible for these associations, and to establish causal links between early temperamental vulnerability and later emergence of disorder.
Footnotes
the authors have no conflicts of interest to declare.
Two tasks not described here differed across the two samples’ batteries; scoring from these two tasks was not included in generating the temperament scores used in the current study (i.e., temperament scores were based on the 10 tasks that were identical across the samples).
References
- 1.Clark LA, Watson D. Temperament: a new paradigm for trait psychology. In: Pervin LA, John OP, editors. Handbook of personality: theory and research. 2. New York: Guilford Press; 1999. pp. 399–423. [Google Scholar]
- 2.Eisenberg N, Fabes RA. Emotion, regulation, and the development of social competence. In: Clark MS, editor. Emotion and social behavior. Thousand Oaks: Sage Publications, Inc; 1992. pp. 119–150. [Google Scholar]
- 3.Rothbart MK, Bates JE. Temperament. In: Damon W, Lerner RM, Eisenberg N, editors. Handbook of child psychology: Vol. 3, social, emotional, and personality development. 6. Hoboken: John Wiley & Sons Inc; 2006. pp. 99–166. [Google Scholar]
- 4.Watson D, Tellegen A. Toward a consensual structure of mood. Psych Bull. 1985;98:219–35. doi: 10.1037//0033-2909.98.2.219. [DOI] [PubMed] [Google Scholar]
- 5.Posner MI, Rothbart MK. Developing mechanisms of self-regulation. Dev Psychopathol. 2000;12:427–441. doi: 10.1017/s0954579400003096. [DOI] [PubMed] [Google Scholar]
- 6.Raffaelli M, Crockett LJ. Sexual risk taking in adolescence: the role of self-regulation and attraction to risk. Dev Psychol. 2003;39:1036–46. doi: 10.1037/0012-1649.39.6.1036. [DOI] [PubMed] [Google Scholar]
- 7.Clark LA. Temperament as a unifying basis for personality and psychopathology. J of Abn Psychol. 2005;114:505–21. doi: 10.1037/0021-843X.114.4.505. [DOI] [PubMed] [Google Scholar]
- 8.Watson D, Kotov R, Gamez W. Basic dimensions of temperament in relation to personality and psychopathology. In: Krueger RF, Tackett JL, editors. Personality and psychopathology. New York: Guilford Press; 2006. pp. 7–38. [Google Scholar]
- 9.Klein DN, Kotov R, Bufferd SJ. Personality and depression: explanatory models and review of the evidence. Ann Rev of Clin Psychol. 2011;7:269–95. doi: 10.1146/annurev-clinpsy-032210-104540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gamez W, Watson D, Doebbeling BN. Abnormal personality and the mood and anxiety disorders: implications for structural models of anxiety and depression. J of Anx Dis. 2007;21:526–39. doi: 10.1016/j.janxdis.2006.08.003. [DOI] [PubMed] [Google Scholar]
- 11.Eisenberg N, Valiente C, Spinrad TL, Liew J, Zhou Q, Losoya SH, et al. Longitudinal relations of children’s effortful control, impulsivity, and negative emotionality to their externalizing, internalizing, and co-occurring behavior problems. Dev Psychol. 2009;45:988–1008. doi: 10.1037/a0016213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Oldehinkel AJ, Hartman CA, Ferdinand RF, Verhulst FC, Ormel J. Effortful control as modifier of the association between negative emotionality and adolescents’ mental health problems. Dev Psychopathol. 2007;19:523–39. doi: 10.1017/S0954579407070253. [DOI] [PubMed] [Google Scholar]
- 13.Rydell A-M, Berlin L, Bohlin G. Emotionality, emotion regulation, and adaptation among 5- to 8-year-old children. Emotion. 2003;3:30–47. doi: 10.1037/1528-3542.3.1.30. [DOI] [PubMed] [Google Scholar]
- 14.Crockett LJ, Carlo G, Wolff JM, Hope MO. The role of pubertal timing and temperamental vulnerability in adolescents’ internalizing symptoms. Dev Psychopathol. 2013;25:377–89. doi: 10.1017/S0954579412001125. [DOI] [PubMed] [Google Scholar]
- 15.Durbin CE, Wilson S. Convergent validity of and bias in maternal reports of child emotion. Psychol Assessment. 2012;24:647–60. doi: 10.1037/a0026607. [DOI] [PubMed] [Google Scholar]
- 16.Hayden EP, Durbin CE, Klein DN, Olino TM. Maternal personality influences the relationship between maternal reports and laboratory measures of child temperament. J of Pers Assessment. 2010;92:586–93. doi: 10.1080/00223891.2010.513308. [DOI] [PubMed] [Google Scholar]
- 17.Olino TM, Durbin CE, Klein DN, Hayden EP, Dyson MW. Gender differences in young children’s temperament traits: comparisons across observational and parent-report methods. J of Pers. 2013;81:119–29. doi: 10.1111/jopy.12000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Durbin CE, Hayden EP, Klein DN, Olino TM. Stability of laboratory-assessed temperamental emotionality traits from ages 3 to 7. Emotion. 2007;7:388–99. doi: 10.1037/1528-3542.7.2.388. [DOI] [PubMed] [Google Scholar]
- 19.Durbin CE, Klein DN, Hayden EP, Buckley ME, Moerk KC. Temperamental emotionality in preschoolers and parental mood disorders. J of Abn Psychol. 2005;114:28–37. doi: 10.1037/0021-843X.114.1.28. [DOI] [PubMed] [Google Scholar]
- 20.Dougherty LR, Klein DN, Durbin CE, Hayden EP, Olino TM. Temperamental positive and negative emotionality and children’s depressive symptoms: a longitudinal prospective study from age three to age ten. J of Soc and Clin Psychol. 2010;29:462–88. [Google Scholar]
- 21.Olino TM, Lopez-Duran NL, Kovacs M, George CJ, Gentzler AL, Shaw DS. Individual differences in positive and negative affect over time: associations with maternal history of psychopathology. J of Child Psychol and Psychiatry. 2011;52:792–9. doi: 10.1111/j.1469-7610.2010.02331.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Olino TM, Klein DN, Dyson MW, Rose SA, Durbin CE. Temperamental emotionality in preschool-aged children and depressive disorders in parents: associations in a large community sample. J of Abn Psychol. 2010;119:468–78. doi: 10.1037/a0020112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kotelnikova Y, Mackrell SV, Jordan PL, Hayden EP. Longitudinal associations between reactive and regulatory temperament traits and depressive symptoms in middle childhood. J of Clin Child and Adol Psychol. 2015;44:775–86. doi: 10.1080/15374416.2014.893517. [DOI] [PubMed] [Google Scholar]
- 24.Meehl PE. Hedonic capacity: Some conjectures. Bulletin of the Menninger Clinic. 1975;39:295–307. [PubMed] [Google Scholar]
- 25.Tugade MM, Fredrickson BL. Resilient individuals use positive emotions to bounce back from negative emotional experiences. J of Pers and Social Psychol. 2004;86:320–33. doi: 10.1037/0022-3514.86.2.320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rende R, Weissman MV. Assessment of family history of psychiatric disorder. In: Shaffer D, Lucas CP, Richters JE, editors. Diagnostic assessment in child and adolescent psychopathology. New York: Guilford Press; 1999. pp. 230–255. [Google Scholar]
- 27.Beauchaine TB, Hayden EP. The developmental psychopathology of child disorders. In: Norcross JC, VandenBos GR, Freedheim DK, editors. APA handbook of clinical psychology. Washington: APA Press; 2016 pp. [Google Scholar]
- 28.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM–IV disorders in the National Comorbidity Survey Replication. Arch of Gen Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 29.Rende R. Liability to psychopathology: a quantitative genetic approach. In: Smolak L, Striegel-Moore R, Levine MP, editors. The developmental psychopathology of eating disorders. Mahwah: Lawrence Erlbaum Associates; 1996. pp. 59–76. [Google Scholar]
- 30.Roy MA, Walsh D, Kendler KS. Accuracies and inaccuracies of the family history method: a multivariate approach. Acta Psychoatrica Scandinavica. 1996;93:224–34. doi: 10.1111/j.1600-0447.1996.tb10639.x. [DOI] [PubMed] [Google Scholar]
- 31.McLaughlin KA, Gadermann AM, Hwang I, Sampson NA, Al-Hamzawi A, Andrade LH, et al. Parent psychopathology and offspring mental disorders: results from the WHO World Mental Health Surveys. Br J of Psychiatry. 2012;200:290–99. doi: 10.1192/bjp.bp.111.101253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zubin J, Spring B. Vulnerability: a new view of schizophrenia. J of Abnorm Psychology. 1977;86:103–126. doi: 10.1037//0021-843x.86.2.103. [DOI] [PubMed] [Google Scholar]
- 33.Kane P, Garber J. The relations among depression in fathers, children’s psychopathology, and father-child conflict: a meta-analysis. Clin Psychol Rev. 2004;24:339–60. doi: 10.1016/j.cpr.2004.03.004. [DOI] [PubMed] [Google Scholar]
- 34.Dougherty LR, Bufferd SJ, Carlson GA, Dyson M, Olino TM, Dubin CE, et al. Preschoolers’ observed temperament and DSM-IV psychiatric disorders assessed with a parent diagnostic interview. J of Clin Child and Adol Psychol. 2011;40:295–306. doi: 10.1080/15374416.2011.546046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kryski KR, Smith HJ, Sheikh HI, Singh SM, Hayden EP. HPA axis reactivity in early childhood: associations with symptoms and moderation by sex. Psychoneuroendocrinology. 2013;38:2327–36. doi: 10.1016/j.psyneuen.2013.05.002. [DOI] [PubMed] [Google Scholar]
- 36.Dunn LM, Dunn DM. The Peabody Picture Vocabulary Test. 4. Bloomington: NCS Pearson, Inc; 2007. [Google Scholar]
- 37.Goldsmith HH, Reilly J, Lemery KS, Longley S, Prescott A. Laboratory Temperament Assessment Battery: Preschool Version. 1995. Unpublished Manuscript. [Google Scholar]
- 38.Kochanska G, Murray K, Jacques TY, Koenig AL, Vandegeest KA. Inhibitory control in young children and its role in emerging internalization. Child Dev. 1996;67:490–507. [PubMed] [Google Scholar]
- 39.Kryski KR, Dougherty LR, Dyson MW, Olino TM, Laptook RS, Klein DN, et al. Effortful control and parenting: associations with HPA axis reactivity in early childhood. Dev Science. 2013;16:531–41. doi: 10.1111/desc.12050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Smith HJ, Kryski KR, Sheikh HI, Singh SM, Hayden EP. The role of parenting and dopamine D4 receptor gene polymorphisms in children’s inhibitory control. Dev Science. 2013;16:515–30. doi: 10.1111/desc.12046. [DOI] [PubMed] [Google Scholar]
- 41.First MB, Spitzer RL, Gibbon M, Williams JBW. The Structured Clinical Interview for DSM-IV – Non-Patient Edition. New York: Biometrics Research Department, New York State Psychiatric Institute; 1996. [Google Scholar]
- 42.Hussong AM, Huang W, Curran PJ, Chassin L, Zucker RA. Parent alcoholism impacts the severity and timing of children’s externalizing symptoms. J Abnorm Child Psychol. 2010;38:367–80. doi: 10.1007/s10802-009-9374-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhou Q, Lengua LJ, Wang Y. The relations of temperament reactivity and effortful control to children’s adjustment problems in China and the United States. Dev Psychol. 2009;45:724–39. doi: 10.1037/a0013776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Klein DN, Dyson MW, Kujawa AJ, Kotov R. Temperament and internalizing disorders. In: Zentner M, Shiner R, editors. Handbook of Temperament. New York: Guilford Press; 2012. pp. 541–561. [Google Scholar]
- 45.Joiner TE, Lonigan CJ. Tripartite model of depression and anxiety in youth psychiatric inpatients: relations with diagnostic status and future symptoms. J Clin Child Psychol. 2000;29:372–82. doi: 10.1207/S15374424JCCP2903_8. [DOI] [PubMed] [Google Scholar]
- 46.Verstraeten K, Vasey MW, Raes F, Bijttebier P. Temperament and risk for depressive symptoms in adolescence: mediation by rumination and moderation by effortful control. J Abnorm Child Psychol. 2009;37:349–61. doi: 10.1007/s10802-008-9293-x. [DOI] [PubMed] [Google Scholar]
- 47.Wetter EK, Hankin BL. Mediational pathways through which positive and negative emotionality contribute to anhedonic symptoms of depression: a prospective study of adolescents. J Abnorm Child Psychol. 2009;37:507–20. doi: 10.1007/s10802-009-9299-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mackrell SVM, Sheikh HI, Kotelnikova Y, Kryski KR, Jordan PL, Singh SM, et al. Child temperament and parental depression predict cortisol reactivity to stress in middle childhood. J of Abn Psychol. 2014;123:106–16. doi: 10.1037/a0035612. [DOI] [PubMed] [Google Scholar]
- 49.Hirshfeld-Becker DR, Biederman J, Henin A, Faraone SV, Davis S, Harrington K, et al. Behavioral inhibition in preschool children at risk is a specific predictor of middle childhood social anxiety: a five-year follow-up. J Dev Behav Pediatr. 2007;28:225–33. doi: 10.1097/01.DBP.0000268559.34463.d0. [DOI] [PubMed] [Google Scholar]
- 50.Muris P, van Brakel AM, Arntz A, Schouten E. Behavioral inhibition as a risk factor for the development of childhood anxiety disorders: a longitudinal study. J of Child and Fam Studies. 2011;20:157–70. doi: 10.1007/s10826-010-9365-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hettema JM, Neale MC, Kendler KS. A review and meta-analysis of the genetic epidemiology of anxiety disorders. Am J of Psychiatry. 2001;158:1566–78. doi: 10.1176/appi.ajp.158.10.1568. [DOI] [PubMed] [Google Scholar]
- 52.Wills TA, Dishion TJ. Temperament and adolescent substance use: a transactional analysis of emerging self-control. J of Clin Child and Adol Psychol. 2004;33:69–81. doi: 10.1207/S15374424JCCP3301_7. [DOI] [PubMed] [Google Scholar]
- 53.Brown SA, Tomlinson K, Winward J. Substance use disorders in adolescence. In: Beauchaine TP, Hinshaw SP, editors. Child and Adolescent Psychopathology. 2. Hoboken: John Wiley Publishers; 2013. pp. 497–530. [Google Scholar]
- 54.Vasey MW, Harbaugh CN, Lonigan CJ, Phillips BM, Hankin BL, Willem L, et al. Dimensions of temperament and depressive symptoms: replicating a three-way interaction. J Res Pers. 2013;47:908–21. doi: 10.1016/j.jrp.2013.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]