Abstract
Objectives
The use of thio-urethane oligomers has been shown to significantly improve the mechanical properties of resin cements (RCs). The aim of this study was to use thio-urethane-modified RC to potentially reinforce the porcelain-RC structure and to improve the bond strength to zirconia and lithium disilicate.
Methods
Six oligomers were synthesized by combining thiols - pentaerythritol tetra-3-mercaptopropionate (PETMP, P) or trimethylol-tris-3-mercaptopropionate (TMP, T) –with di-functional isocyanates - 1,6-Hexanediol-diissocyante (HDDI) (aliphatic, AL) or 1,3-bis(1-isocyanato-1-methylethyl)benzene (BDI) (aromatic, AR) or Dicyclohexylmethane 4,4'-Diisocyanate (HMDI) (cyclic, CC). Thio-urethanes (20 wt%) were added to a BisGMA/UDMA/TEGDMA organic matrix. Filler was introduced at 60 wt%. The microshear bond strength (μSBS), Weibull modulus (m), and failure pattern of RCs bonded to zirconia (ZR) and lithium disilicate (LD) ceramics was evaluated. Biaxial flexural test and fractographic analysis of porcelain discs bonded to RCs were also performed. The biaxial flexural strength (σbf) and m were calculated in the tensile surfaces of porcelain and RC structures (Z=0 and Z=-t2, respectively).
Results
The μSBS was improved with RCs formulated with oligomers P_AL or T_AL bonded to LD and P_AL, P_AR or T_CC bonded to zirconia in comparison to controls. Mixed failures predominated in all groups. σbf had superior values at Z=0 with RCs formulated with oligomers P_AL, P_AR, T_AL, or T_CC in comparison to control; σbf increased with all RCs composed by thio-urethanes at Z=-t2. Fractographic analysis revealed all fracture origins at Z=0.
Conclusion
The use of specific thio-urethane oligomers as components of RCs increased both the biaxial flexural strength of the porcelain-RC structure and the μSBS to LD and ZR.
Clinical Significance
The current investigation suggests that it is possible to reinforce the porcelain-RC pair and obtain higher bond strength to LD and ZR with RCs formulated with selected types of thio-urethane oligomers.
Keywords: ceramic interface strengthening, mechanical reliability, bond to ceramics, resin cements, thio-urethane oligomers
1. Introduction
Resin cements (RCs) have gained clinical popularity in Dentistry because of their ability to bond both to the tooth structure and to the majority of restorative materials when associated with chemical components such as silanes and phosphate-based primers [1]. The use of RCs is indicated for several clinical applications that include adhesion of complete crowns, fixed partial prosthesis, partial coverage, and intracanal posts. The main advantages of RCs over other traditionally used cements, such as zinc-phosphates and glass-ionomers, are the reduced risk of microleakage, and the decreased sorption, solubility, and staining, which results in the maintenance of the interface integrity [2].
Glass-ceramics and polycrystalline ceramics are available for use in clinical practice. Loss of retention might represent a technical complication, compromising the lifetime of the restoration [3]. Glass-ceramics have been widely used for years due to the possibility of producing total or partial coverage, maintaining the maximum integrity of the remaining coronal structure. Considering that glass-ceramic restorations have been extensively used in partial coverage with preparations that do not have sufficient mechanical retention, high bond strength values are important for restoration successful clinical outcome. However, the current bond protocols are not very efficient for polycrystalline ceramics, since they are acid resistant and therefore cannot be treated by conventional etching [4]. Moreover, silane treatments are also not adequate for materials such as highly crystalline zirconia, which do not form covalent bonds with the alkoxy silane group of the coupling agent [4]. This problem has led to extensive research in the recent years focusing on the improvement of bonding strategies for this class of ceramic material, which has been used mostly for full coverage. More recently, partial polycrystalline structures have also been recommended [5], increasing the need for resin cements that provide higher bond strength and retention stability.
Besides providing bonding stability for ceramic restorations, RCs have been recognized to significantly strengthen bonded restoration [6,7]. Studies have demonstrated that the increase in the elastic modulus of RCs has a favorable impact on the mechanical strength of a dental feldsphatic porcelain [6,7]. Moreover, cement characteristics such as the reduced volumetric shrinkage and, as a consequence, low polymerization stress might have a positive impact on the ceramic strength [8]. These cement characteristics are of great interest, especially for restorations made of dental porcelains or glass-ceramics. These materials provide excellent esthetic characteristics and have been used for years in different applications. However, they are intrinsically fragile structures, i.e., have very low fracture toughness in comparison to other dental ceramics.
Recent publications showed that RCs formulated with thio-urethane oligomers as part of the organic matrix presented increased mechanical properties when compared to materials composed only by traditional monomers. Mechanical properties such as flexural strength, flexural modulus, and fracture toughness are the ones mostly improved by the addition of thio-urethanes [9,10]. These improvements are achieved because of a combination of factors, including the low Tg of the additive [10], which provides opportunities for stress relaxation within the glassy methacrylate network [11], but also possibly due to active strand behavior on the thio-urethane oligomer [12]. In addition to that, the fact that the additive is pre-polymerized leads to a reduction in volumetric shrinkage and polymerization stress, observed in conjunction with an increase in the degree of conversion and delayed gelation/vitrification, which are in turn a function of the chain-transfer-capable thiol pending functionalities [9].
The objective of the present study was to determine the bond strength of resin cements to ceramic materials as function of the cement formulation (six oligomers) and the ceramic substrate (zirconia or lithium disilicate). In addition, the Weibull parameter of bilayered discs (0.15 mm of cement and 0.8 mm of ceramic) was determined for porcelain/RC specimens using the six experimental cement compositions. The discs were tested with the cement layer positioned on the tensile side of the biaxial flexural strength test. The hypothesis was that the properties evaluated would be significantly improved by the formulation of RCs containing thio-urethanes.
2. Materials and Methods
2.1 Resin cements composition
The experimental resin cements formulated for the study were composed of Bis-phenol A diglycidyl dimethacrylate (Bis-GMA; Esstech, Essington, PA, USA), urethane dimethacrylate (UDMA; Esstech) and tri-ethylene glycol dimethacrylate (TEGDMA; Esstech) in a 50:30:20 mass ratio. Photoinitiators were added to the monomers as follows: 0.6 wt% of a tertiary amine (EDMAB - ethyl 4-dimethylaminobenzoate; Avocado, Heysham, England), 0.2 wt% of dl-camphoroquinone (Polysciences Inc., Warrington, PA, USA), and 0.5 wt% inhibitor (BHT-2,6-di-tert-butyl-4-methylphenol; SigmaAldrich, St. Louis, MO, USA).
Six different oligomers were synthesized in solution in the presence of catalytic amounts of trimethylamine. Multi-functional thiols were combined with di-functional isocyanates in 4 x volume of dichloromethane (very diluted solution) as presented in Table 1. In addition, the isocyanate:thiol ratio was kept at 1:2 (by mol) to avoid gelation of the oligomer during reaction, according to the Flory-Stockmeyer theory [13], leaving pendant thiols. Oligomers were purified by precipitation in hexanes and rotaevaporation, and then characterized by 1H-NMR and mid-IR spectroscopy [14]. The disappearance of the isocyanate peak at 2270 cm−1 and the appearance of resonance signals at 3.70 ppm were used as evidence for completion of isocyanate reaction and thio-urethane bond formation, respectively [15]. The thiol group (SH) concentration for each oligomer was determined using a titration method with Ellman's reagent well established in the literature [16]. Thio-urethane oligomers were added to the methacrylate organic phase in proportion of 20wt%, as defined in our previous investigation [9]. The final oligomer product presented as a viscous liquid at room temperature, and was completely miscible with methacrylate monomers. A resin cement formulated without oligomer served as control.
Table 1.
Combination of isocyanates with thiols for the composition of the six thio-urethane oligomers used in the study.
| Thiol (abbreviation) | Isocyanate (abbreviation) | Thio-urethane formed |
|---|---|---|
| Pentaerythritol tetra-3-mercaptopropionate (PETMP) | 1,6-Hexanediol-diissocyante (aliphatic, AL) | P_AL |
| Pentaerythritol tetra-3-mercaptopropionate (PETMP) | 1,3-bis(1-isocyanato-1-methylethyl)benzene (aromatic, AR) | P_AR |
| Pentaerythritol tetra-3-mercaptopropionate (PETMP) | Dicyclohexylmethane 4,4'-Diisocyanate (cyclic, CC) | P_CC |
| Trimethylol-tris-3-mercaptopropionate (TMP) | 1,6-Hexanediol-diissocyante (aliphatic, AL) | T_AL |
| Trimethylol-tris-3-mercaptopropionate (TMP) | 1,3-bis(1-isocyanato-1-methylethyl)benzene (aromatic, AR) | T_AR |
| Trimethylol-tris-3-mercaptopropionate (TMP) | Dicyclohexylmethane 4,4'-Diisocyanate (cyclic, CC) | T_CC |
Filler was introduced to all groups at 60 wt% (Barium glass 0.7 μm, density 3.0 g/ml, refractive index 1.553 - V117 4107, Esstech), with the aid of a mechanical mixer (DAC 150 Speed mixer, Flacktek, Landrum, SC, USA) for 5 min at 2400 rpm. All procedures were carried out under yellow lights.
2.2 Microshear bond strength (μSBS) to ceramics
Forty-two specimens (14 mm long, 12 mm wide and 3 mm thick) of yttrium-stabilized tetragonal polycrystalline zirconia (Y-TZP) (inCoris TZI mono L, Sirona Dental Inc, USA) or lithium disilicate ceramic (LD) (IPS e.max CAD, HT, shade A1, Ivoclar Vivadent, Liechtenstein) were produced (n=6 per group). Materials were processed as per the manufacturer’s instructions. After sintering, the Y-TZP bonding surface was sandblasted with 30 μm silica-coated aluminum oxide particles (CoJetTM Sand S30, 3M ESPE, USA) for 15 s (at a distance of 5 mm and 2.5 bar of pressure) and ultrasonically cleaned for 10 min. Samples were silanated (Silano, Angelus, Brazil) and coated with a layer of 10-MDP (Metal/Zirconia Primer, Ivoclar Vivadent). LD specimens were etched with 10% hydrofluoric acid (Condac porcelain, FGM Dental Products, Brazil) for 20 s, cleaned with water and oil-free compressed air for 30 s and silanated (Silano, Angelus).
RC application on the ceramic treated surfaces was performed by filling plastic cylinders (0.8 mm wide and 1 mm long, Tygon® Tubing, Bio-Rad Laboratories, USA) with RC – 04 RC cylinders for each ceramic specimen, totalizing 24 bonded cylinders in each group. The RC was light activated for 60 s at 800 mW/cm2 (Bluephase, Ivoclar Vivadent). The plastic cylinders were removed after RC polymerization. Samples were water-stored for one week at a temperature of 37°C. Specimens were tested in a universal testing machine at a crosshead speed of 0.5 mm/min using a metal wire. Data were obtained in MPa by dividing the force in Newton (N) by the bonding surface area (A) (A= π*r2, where r is the RC cylinder radius = 0.4 mm). The mean fracture strength (MPa) in each specimen was calculated.
The fractured surfaces were evaluated by stereomicroscope (Olympus, Japan) and the failure patterns classified as adhesive, cohesive in cement, cohesive in ceramic, or mixed.
2.3 Porcelain-RC biaxial flexural strength
Two hundred and ten disc-shaped porcelain specimens were produced. The porcelain powder (Super Porcelain EX-3, Noritake, Japan) was mixed with the modeling liquid to produce a thick slurry, which was condensed into a metallic mold (12-mm diameter, 1-mm thickness). The mold was overfilled and placed on a vibrating table for 90 seconds, with excess liquid removed with absorbent paper. The surface was leveled with a razor blade to produce discs of uniform thickness. Each disc was removed carefully from the mold, placed on a refractory substrate, and fired in a ceramic furnace (Vacumat 40, Vita Zahnfabrik) according to the manufacturer’s instruction. The discs were cooled to room temperature and visually inspected. Discs with defects or visible cracks observed under a stereo microscope were discarded and replaced. The discs were manually wet ground on both sides with 320-grit SiC abrasive papers (Norton S.A., Brazil) to produce flat surfaces 0.8±0.1 mm in thickness. Wet polishing was performed with 600- and 1200-grit SiC abrasive papers for 60 seconds on each surface. Final dimensions were checked with a digital caliper (Absolute Digimatic, Mitutoyo, Japan), and the porcelain discs were randomly divided into seven groups (n=30 per group) according to the RC tested.
The bonding surface of each porcelain disc was etched with 10% hydrofluoric acid (Condac porcelain, FGM) for 60 s, washed for 30 s with water and oil-free compressed air for 30 s and silanated (Silano, Angelus). The resin cement coating was applied with the aid of a digital caliper were a cement layer of 150 μm was standardized [17]. The RC was light activated with 800 mW/cm2 (Bluephase, Ivoclar Vivadent) by 60 s through the porcelain disc. Samples were stored for 24 h in dark containers until final degree of conversion was obtained. The biaxial flexural strength (σbf) of the porcelain-RC specimens was determined on the mechanical testing machine using a ball-on-ring setup. The discs were centrally placed on a 10-mm diameter knife-edged support and loaded with a spherical indenter (4-mm diameter) at a crosshead speed of 1 mm/min.
The σbf was calculated according to the analytical solutions described and tested before [7, 18–23]. First, the E of the porcelain ( ) and RC ( ) were calculated as a function of the Poisson’s ratio of the porcelain and RC, according to Equation 1:
| (Eq. 1) |
where E1is the Eof porcelain [24], and E2 the Eof the RC defined previously according to ISO 4049 [10]. ν1 and ν2 the Poisson’s ratios of the porcelain (0.25) [24] and resin-based luting agents (0.27) [25]. The neutral plane (tn) of the coated porcelain specimens was calculated as a function of the porcelain and RC thicknesses (t1 and t2) and the calculated and , using Equation 2:
| (Eq. 2) |
The σbf was calculated at z-axial positions at the center of the discs, where the porcelain surface at the bonded interface is located (position z=0) and the RC surface that contacts the ring of the ball-on-ring setup is located (position z=-t2), according to Equations 3, 4, and 5:
| (Eq. 3) |
| (Eq. 4) |
| (Eq. 5) |
For the fractographic analysis, the fractured specimens retrieved from the biaxial flexural test were coated with gold and observed at varied magnifications under optical microscopy and SEM (JSM-6610; JEOL Ltd., Tokyo, Japan) to identify fracture features and to determine the critical flaw origin. An evaluation of the number of fracture fragments for each sample was also performed.
2.4 Statistical analysis
Data from microshear bond strength tests were submitted to one-way ANOVA and Tukey’s test (α=0.05). Data passed the normality (LD: p=0,837; ZR: p= 0,069) and homoscedasticity tests (LD: p=0,743; ZR: p=0,903). Confidence intervals (95% CI) were calculated for σbf of the ceramic discs at axial positions z=0 and z=-t2. Groups were considered significantly different when the 95% confidence interval bounds did not overlap. A Weibull analysis was performed for μSBS and σbf data using the software Weibull++ (Reliasoft, Tucson, AZ, USA); m was calculated using maximum likelihood estimation and a two-parameter Weibull model, and 95% upper and lower confidence bounds were calculated using the likelihood ratio [26].
3. Results
3.1 Microshear bond strength (μSBS) to ceramics
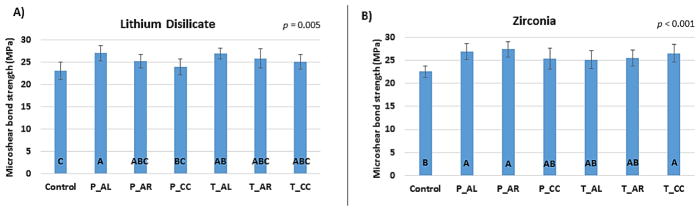
When bonded to LD (Figure 1A), RCs formulated with oligomers P_AL or T_AL showed significant higher μSBS values in comparison to that obtained for the control group. Among the groups containing oligomer-based RCs, only P_CC and P_AL showed significantly different μSBS, whereas the other oligomers results in similar bond strength values.
Figure 1.
Microshear bond strength in (A) lithium disilicate and (B) zirconia.
Considering the zirconia substrate, it is possible to note in Figure 1B that only RCs composed by the oligomers P_AL, P_AR or T_CC obtained higher bond strength in comparison to the control. No statistical difference was observed among the bond strengths obtained for the different types of thio-urethanes.
The m showed no differences in μSBS reliability for RCs composed by oligomers in comparison to control, either for LD or ZR. Within LD, the RCs formulated with P_CC and T_AR were superior to P_AR.
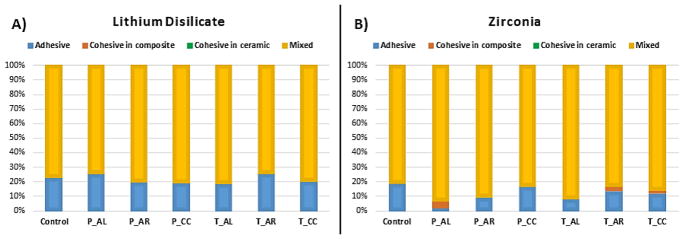
The failure patterns after μSBS testing in LD surfaces (Figure 2A) were similar for the different experimental groups, with predominance of mixed failures for all groups, ranging between 75 and 85% of all failures. The remaining failures were classified as adhesive. For zirconia substrate (Figure 2B), there was predominance of mixed failures in all groups. However, in the samples bonded to the RC composed by the oligomer P_AL, which showed the highest μSBS, cohesive failures in RC predominated over the adhesive ones.
Figure 2.
Failure patterns for microshear bond strength test in (A) lithium disilicate and (B) zirconia.
3.2 Porcelain-RC biaxial flexural strength
The results of σbf and m in the porcelain-RC specimens (z=0 and z=-t2) are shown in Table 3. Porcelain coated by RCs composed by the oligomers P_AL, P_AR, T_AL, and T_CC showed significantly higher σbf at z=0 as compared to control group, with the RC formulated with oligomer P_AL yielding the highest porcelain-RC strength. The mechanical reliability (m) of the structure at z=0 was not affected by the type of RC used. At axial position z=-t2, significant differences were observed for σbf with RC composed by oligomers leading to superior values in comparison to the control. The structural reliability at z=-t2 was independent of the RC tested, with no significant differences in m values among groups.
Table 3.
Means (95% confidence intervals) for biaxial flexural strength (σbf) and Weibull modulus (m), n=30
| Group | Axial position Z=0 | Axial position Z=-t2 | ||
|---|---|---|---|---|
| σbf (MPa) | m | σbf (MPa) | m | |
| Control | 119.7 (112.2 – 127.2)C | 7.7 (5.8 – 10.2) A | 9.5 (8.9–10.1)C | 7.6 (5.7 – 10.2) A |
| P_AL | 146 (137.7–154.4)A | 7.7 (6.0 – 9.9) A | 15.1 (14.2–15.9)AB | 7.7 (6.0 – 9.9) A |
| P_AR | 140.1 (132.8–147.4)AB | 8.3 (6.3 – 10.9) A | 14.4 (13.6–15.1)AB | 8.3 (6.3 – 11.0) A |
| P_CC | 127.5 (120.9–134)BC | 8.5 (6.3 – 10.9) A | 14.5 (13.8–15.3)AB | 8.3 (6.3 – 10.9)A |
| T_AL | 135.7 (130.1–141.3)AB | 10.4 (8.0 – 13.4) A | 13.7 (13.1–14.3)B | 10.4 (8.0 – 13.4) A |
| T_AR | 130.9 (124.9–136.9)BC | 8.9 (6.7 – 11.9) A | 15.5 (14.7–16.2)A | 8.9 (6.7 – 11.9) A |
| T_CC | 136 (129.4–142.6)AB | 9.4 (7.1 – 12.4) A | 15.6 (14.7–16.4)A | 7.9 (6.0 – 10.5) A |
Samples of porcelain-RC of control group presented a greater number of fractures in three or four-or-more fragments (13 samples) than those containing RCs formulated with oligomers, in which two fragments predominated (24 to 28 samples), as presented in Table 4.
Table 4.
Number of disc fragments after tested in biaxial flexure.
| Group | Number of disc fragments
|
||
|---|---|---|---|
| 02 | 03 | 04-or-more | |
| Control | 17 | 09 | 04 |
| P_AL | 26 | 02 | 02 |
| P_AR | 24 | 05 | 01 |
| P_CC | 25 | 05 | |
| T_AL | 26 | 04 | |
| T_AR | 28 | 02 | |
| T_CC | 25 | 05 | |
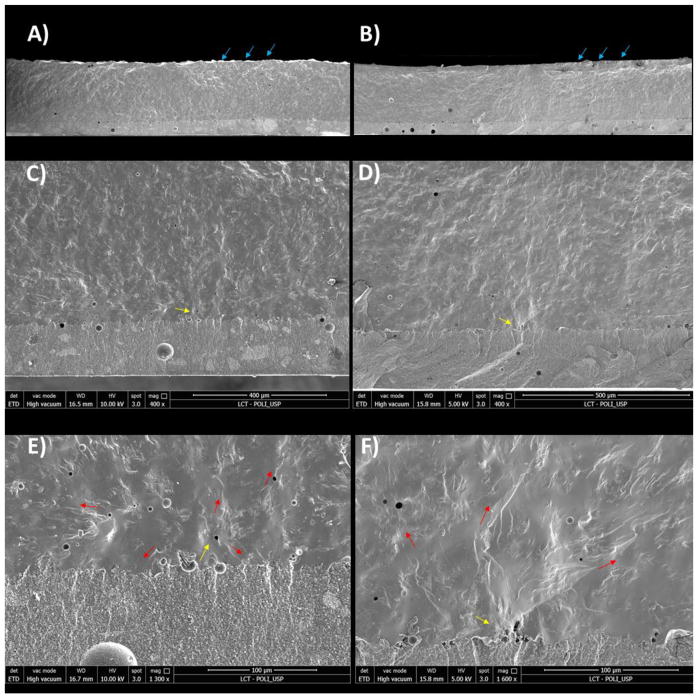
Representative images of the SEM fractographic analysis are shown in Figure 3. Failures originated on the ceramic surface at the ceramic-RC interface (Z=0), which was subjected to tensile stress, and propagated throughout the material. Pores at the porcelain-RC interface seemed sometimes associated with failure origins.
Figure 3.
SEM images of fracture surfaces. Figures ‘A’, ‘C’ and ‘E’ represent the control group; figures ‘B’, ‘D’ and ‘F’ represent a sample of porcelain bonded to a RC formulated with oligomer P_AL. Blue arrows (in Figures ‘A’ and ‘B’) indicate the compression curl; yellow arrows (Figures ‘C’-‘F’) indicate the fracture origin; red arrows (in Figures ‘E’ and ‘F’) indicate wake hackles.
4. Discussion
The results of this study demonstrate that thio-urethane-based RCs are capable of reinforcing ceramic/RC bilayers and improving the bond strength between the resin cement to both zirconia and lithium disilicate substrates. Therefore, the hypothesis of this study was accepted. Improving the bond strength of resin cements to zirconia has been a major challenge in dental materials research over the years. The inert nature of this type of ceramic substrate limits the chemical interaction with primers, adhesives and resin cements [4]. Moreover, limited topographic roughness is observed after mechanical and/or chemical-mechanical surface treatments due to the high hardness and reduced (almost absent) vitreous phase in zirconia surfaces [27]. This study showed that is possible to increase the bond strength of RC to zirconia by producing resin cements that contain TU oligomers, especially oligomers P_AL, P_AR, or T_CC. One possible mechanism to explain this is the improved toughness of the TU-modified cement, which can provide a means for energy absorption during mechanical loading [28]. These materials have been widely used for applications where high resistance to impact is desirable, exactly because of the increased toughness provided by the flexible thiocarbamate bonds [29].
The same improvement was observed in bond strength values when oligomer-based RCs were bonded to a lithium disilicate (LD) glass-ceramic. LD has been largely utilized in dentistry because of good aesthetics and good mechanical strength associated with the ability of chemically adhere to the resin cement via silane application. The most commonly used restorations produced with LD are bridges, full or partial crowns, and veneers. LD has a significant amount of vitreous phase in its composition and, therefore can be acid etched and silane-treated. The oligomer versions P_AL or T_AL resulted in significant improvement in bond strength of the cement to the LD. This may be due to several reasons. The pendant thiol functionalities from the oligomer backbone are available to react with the vinyl bonds on the methacrylates, via chain-transfer reactions [29]. This mechanism is well-known to delay the point in conversion where gelation and vitrification takes place, with two main advantages: first, the final conversion is extended, which is desirable in the dental application since higher conversions have been correlated with increased properties [9,10,14] and decreased cytotoxicity [30]. Second, the resulting polymer network becomes more homogeneous, as demonstrated by narrower tan delta peaks by dynamic mechanical analysis [29]. Third, the already mentioned improvement in toughness and fracture toughness [14] may also contribute to the stability of the bonded interface. And finally, the decrease in polymerization stress, especially in a confined situation such as the cementation line, must have also played a role. This improvement in the mechanical properties of the cement can be speculated to have played the major role in increasing the bonding to ceramics in the present study.
The failure pattern analysis of the μSBS specimens showed a majority of fractures involving both the RC/ceramic interface and the RC bulk structure (mixed fractures). It might be assumed that when comparing both the RC bulk and ceramic/cement interface they have similar strength, and therefore there is equal probability of fracture starting in both locations. Moreover, two main forces act into the RC and interface during μSBS tests explaining the failure pattern observed in the study. First, tensile forces predominate over shear ones in the interface during the test and irregularities in the interface could lead to the failure initiation. The load applied might lead to relevant amount of stress concentration into the RC, making it favorable for the fracture to happen within the bulk of the structure [31]. In addition, the RC containing oligomer P_AL when bonded to zirconia showed a higher amount of cohesive fractures because of the higher bond strength.
Results of biaxial flexure strength tests showed a significant improvement in the σbf of the ceramic/RC bilayers produced with thio-urethane-based cements. In comparison with the control group, RCs composed by oligomers P_AL, P_AR, T_AL, and T_CC led to significant higher σbf at the ceramic surface (Z=0). In addition, all RCs composed by oligomers increased the σbfin the RC surface ( Z=-t2). Micro topographical roughness features are formed in the ceramic surface after conditioning with hydrofluoric acid and removal of the vitreous phase. The resin cement fills these spaces, forming an interpenetrated resin/ceramic layer that pose an obstacle to crack propagation [19,22]. Therefore, cements with higher mechanical properties, such as those composed by TUs, are likely to produce a stronger interpenetrating layer that results in increased biaxial flexure of the bilayered structure [7].
RCs composed by oligomers showed significant lower volumetric shrinkage and polymerization stress in previous studies [9,10,14]. The higher volumetric shrinkage in the control group might have been responsible for creating interfacial defects with poor RC infiltration into the ceramic surface where crack propagation might initiate [8]. Additionally, the polymerization stress might be responsible for residual tensile stress build up at the ceramic-RC interface and around inorganic filler particles of the cement [32]. In this way, it is possible that such a higher interfacial stress in the control group may have facilitated crack propagation at the interface and around filler particles near the bonded region, therefore reducing the biaxial flexure strength of the bilayer. [33,34].
Another property that can account for this strengthening effect on the ceramic-RC bilayer is the Young’s modulus (E) of the RC [6,7]. RCs with higher E might withstand higher stress concentration in the RC layer and, therefore, reduce the magnitude of stress reaching the ceramic structure [7]. Therefore, the load necessary to fracture the specimen is increased, as observed in the present study. One example of the role of E on the ceramic-RC strengthening is the number of retrieved pieces of each sample in the experiment. Samples of porcelain-RC of control group had a greater number of specimens fractured in three or four-or-more fragments (13 samples) than those containing RCs formulated with oligomers, in which two fragments predominated (24 to 28 samples). The reduction in the number of fracture fragments generated by samples of experimental groups during biaxial flexural testing suggests reduced energy storage in the ceramic bulk, instead translated into elastic strain in the RC with higher E prior to failure [35,36]. In other words, the closer the elastic modulus of porcelain and RC, the lower the amount of stress concentration in the porcelain-RC interface.
The representation of fractographic analysis in Fig 3 shows that the fracture origin is more frequently located on the ceramic surface. This was expected as the elastic deformation of porcelain is much lower than that of the RC during the biaxial flexure test. Moreover, the presence of bubbles or porosity at ceramic-RC interface served favored stress concentration in this region, leading to crack propagation through the ceramic and RC structures.
5. Conclusions
When compared to a RC composed by an organic matrix containing only traditional monomers (BisGMA/UDMA/TEGDMA), the formulation of RCs with selected thio-urethane oligomers provided increased μSBS to zirconia and to lithium disilicate. Moreover, the use of RCs composed by oligomers increased the flexural strength of porcelain-RC bilayers.
Table 2.
Weibull modulus (m) for microshear bond strength.
| Group | m | |
|---|---|---|
| Lithium Disilicate | Zirconia | |
| Control | 2.9 (2.0 – 3.8) AB | 2.4 (1.7 – 3.1) A |
| P_AL | 3.5 (2.4 – 4.6) AB | 2.8 (2.0 – 3.5) A |
| P_AR | 2.1 (1.4 – 2.7) B | 3.4 (2.5 – 4.3) A |
| P_CC | 4.9 (3.4 – 6.3) A | 3.7 (2.8 – 4.6) A |
| T_AL | 3.3 (2.3 – 4.3) AB | 2.8 (2.1 – 3.5) A |
| T_AR | 4.8 (3.3 – 6.1) A | 3.1 (2.3 – 3.9) A |
| T_CC | 3.9 (2.6 – 5.1) AB | 3.4 (2.4 – 4.0) A |
Acknowledgments
The authors thank NIH-NIDCR (1R15-DE023211, 1U01-DE023756 and K02-DE025280) for financial support granted to C.S.P. The donation of methacrylate monomers by Esstech is also greatly appreciated. The authors would like to thank also Dr. Gabriel Kalil Rocha Pereira for his generous help with some data analysis.
Footnotes
Conflict of interest
The authors declare no conflict of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Manso AP, Silva NRFA, Bonfante EA, Pegoraro TA, Dias RA, Carvalho RM. Cements and Adhesives for all-ceramic restorations. Dent Clin North Am. 2011;55:311–332. doi: 10.1016/j.cden.2011.01.011. [DOI] [PubMed] [Google Scholar]
- 2.Kermanshahi S, Santerre JP, Cvitkovich DG, Finer Y. Biodegradation of resin-dentin interfaces increases bacterial microleakage. J Dent Res. 2010;89:996–1001. doi: 10.1177/0022034510372885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sailer I, Makarov NA, Thoma DS, Zwahlen M, Pjetursson BE. All-ceramic or metal-ceramic tooth-supported fixed dental prostheses FDPs? A systematic review of survival and complication rates. Part I: Single crowns (SCs) Dent Mater. 2015;31:603–623. doi: 10.1016/j.dental.2015.02.011. [DOI] [PubMed] [Google Scholar]
- 4.Tzanakakis EG, Tzoutzas IG, Koidis PT. Is there a potential for durable adhesion to zirconia restorations? A systematic review. J Prosthet Dent. 2016;115:9–19. doi: 10.1016/j.prosdent.2015.09.008. [DOI] [PubMed] [Google Scholar]
- 5.Kern M, Passia N, Sasse M, Yazigi C. Tem-year outcome of zirconia ceramic cantilever resin-bonded fixed dental prostheses and the influence of the reasons for missing incisors. J Dent. 2017;65:51–55. doi: 10.1016/j.jdent.2017.07.003. [DOI] [PubMed] [Google Scholar]
- 6.Fleming GJP, Hooi P, Addison O. The influence of resin flexural modulus on the magnitude of ceramic strengthening. Dent Mater. 2012;28:769–776. doi: 10.1016/j.dental.2012.04.003. [DOI] [PubMed] [Google Scholar]
- 7.Spazzin AO, Bacchi A, Alessandretti R, Basso G, Griggs J, Moraes RR. Ceramic strenghtning by tuning the elastic moduli of resin-based luting agents. Dent Mater. 2017;117:214–217. doi: 10.1016/j.dental.2017.01.002. [DOI] [PubMed] [Google Scholar]
- 8.Magne P, Versluis A, Douglas WH. Effect of luting composite shrinkage and thermal loads on the stress distribution in porcelain laminate veneers. J Prosthet Dent. 1999;81:335–344. doi: 10.1016/s0022-3913(99)70278-7. [DOI] [PubMed] [Google Scholar]
- 9.Bacchi A, Consani RL, Martim GC, Pfeifer CS. Thio-urethane oligomers improve properties of light-cured resin composites. Dent Mater. 2015;31:565–574. doi: 10.1016/j.dental.2015.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bacchi A, Pfeifer CS. Rheological and mechanical properties and interfacial stress development of composite cements formulated with thio-urethane oligomers. Dent Mater. 2016;32:978–986. doi: 10.1016/j.dental.2016.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chung JY, Douglas JF, Stafford CM. A wrinkling-based method for investigating glassy polymer film relaxation as a function of film thickness and temperature. J Chem Phys. 2017;147:154902. doi: 10.1063/1.5006949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Xie SJ, Qian HJ, Lu ZY. Polymer brushes: a controllable system with adjustable glass transition temperature of fragile glass formers. J Chem Phys. 2014;140:044901. doi: 10.1063/1.4862234. [DOI] [PubMed] [Google Scholar]
- 13.Odian G. Principles of polymerization. New York: Wiley Interscience; 2004. [Google Scholar]
- 14.Bacchi A, Dobson A, Ferracane JL, Consani RL, Pfeifer CS. Thio-urethanes improve properties of dual-cured composite cements. J Dent Res. 2014;93:1320–1325. doi: 10.1177/0022034514551768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Silverstein R, Webster F, Kiemle D. Spectrometric identification of organic compounds. 7. Wiley Interscience; New York: 2005. [Google Scholar]
- 16.Riener CK, Kada G, Gruber HJ. Quick measurement of protein sulfhydryls with Ellman’s reagent and 4,4′-dithiodipyridine. Anal Bioanal Chem. 2002;373:266–276. doi: 10.1007/s00216-002-1347-2. [DOI] [PubMed] [Google Scholar]
- 17.Marocho SMS, De Melo RM, Macedo LGS, Valandro LF, Bottino MA. Strength of a feldspar ceramic according to the thickness and polymerization mode of the resin cement coating. Dent Mater J. 2011;30:323–329. doi: 10.4012/dmj.2010-123. [DOI] [PubMed] [Google Scholar]
- 18.Hsueh CH, Lance MJ, Ferber MK. Stress distributions in thin bilayer discs subjected to ball-on-ring tests. J Am Ceram Soc. 2005;88:1687–1690. [Google Scholar]
- 19.Fleming GJ, Maguire FR, Bhamra G, Burke FM, Marquis PM. The strengthening mechanism of resin cements on porcelain surfaces. J Dent Res. 2006;85:272–276. doi: 10.1177/154405910608500313. [DOI] [PubMed] [Google Scholar]
- 20.Addison O, Fleming GJ. Application of analytical stress solutions to biaxially loaded dental ceramic-dental cement bilayers. Dent Mater. 2008;24:1336–1342. doi: 10.1016/j.dental.2008.02.013. [DOI] [PubMed] [Google Scholar]
- 21.Addison O, Sodhi A, Fleming GJ. Seating load parameters impact on dental ceramic reinforcement conferred by cementation with resin-cements. Dent Mater. 2010;26:915–921. doi: 10.1016/j.dental.2010.05.006. [DOI] [PubMed] [Google Scholar]
- 22.Spazzin AO, Guarda GB, Oliveira-Ogliari A, Correr-Sobrinho L, Moraes RR. Strengthening of porcelain provided by resin cements and flowable composites. Oper Dent. 2016;41:179–188. doi: 10.2341/15-025-L. [DOI] [PubMed] [Google Scholar]
- 23.Soares LD, Basso GR, Spazzin AO, Griggs J, Moraes RR. Mechanical reliability of air-abraded and acid-etched bonded feldspar ceramic. Dent Mater. 2016;32:433–441. doi: 10.1016/j.dental.2015.12.011. [DOI] [PubMed] [Google Scholar]
- 24.Zeng K, Oden A, Rowcliffe D. Evaluation of mechanical properties of dental ceramic core materials in combination with porcelains. Int J Prosthodont. 1998;11:183–189. [PubMed] [Google Scholar]
- 25.De Jager N, Pallav P, Feilzer AJ. The apparent increase of the Young's modulus in thin cement layers. Dent Mater. 2004;20:457–462. doi: 10.1016/j.dental.2003.07.002. [DOI] [PubMed] [Google Scholar]
- 26.Griggs JA, Zhang YL. Determining the confidence intervals of Weibull parameters estimated using a more precise probability estimator. J Mater Sci Lett. 2003;22:1771–1773. [Google Scholar]
- 27.Paes PNG, Bastian FL, Jardim PM. The influence of Y-TZP surface treatment on topography and ceramic/resin cement interfacial fracture toughness. Dent Mater. 2017;33:976–989. doi: 10.1016/j.dental.2017.06.004. [DOI] [PubMed] [Google Scholar]
- 28.Bacchi A, Nelson M, Pfeifer CS. Characterization of methacrylate-based composites cointaining thio-urethane oligomers. Dent Mater. 2015;32:233–239. doi: 10.1016/j.dental.2015.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hoyle CE, Bowman CN. Thiol–ene click chemistry. Angew Chem. 2010;49:1540–1573. doi: 10.1002/anie.200903924. [DOI] [PubMed] [Google Scholar]
- 30.Franz A, Konig F, Lucas T, Watts DC, Schedle A. Cytotoxic effect of dental bonding substances as a function of degree of conversion. Dent Mater. 2009;25:232–239. doi: 10.1016/j.dental.2008.07.003. [DOI] [PubMed] [Google Scholar]
- 31.Braga RR, Meira JB, Boaro LC, Xavier TA. Adhesion to tooth structures: a critical review of “macro” test methods. Dent Mater. 2010;26:e38–49. doi: 10.1016/j.dental.2009.11.150. [DOI] [PubMed] [Google Scholar]
- 32.Feng L, Suh BI, Shortall AC. Formation of gaps at the filler-resin interface induced by polymerization contraction stress: gaps at the interface. Dent Mater. 2010;26:719–729. doi: 10.1016/j.dental.2010.03.004. [DOI] [PubMed] [Google Scholar]
- 33.Sun CJ, Wu W, Mahanti K, Sadeghipour K, Baran G, Debnath S. Finite element analysis of toughening for a particle-resin forced composite. Polym Compos. 2006;27:360–367. [Google Scholar]
- 34.Lohbauer U, Belli R, Ferracane JL. Factors involved in mechanical fatigue degradation of dental composites. J Dent Res. 2013;92:584–591. doi: 10.1177/0022034513490734. [DOI] [PubMed] [Google Scholar]
- 35.Nakayama J. Direct Measurement of Fracture Energies of Brittle Heterogeneous Materials. J Am Ceram Soc. 1965;48:583–587. [Google Scholar]
- 36.Costa AK, Kelly RD, Fleming GJ, Borges AL, Addison O. Laminated ceramics with elastic interface: a mechanical advantage? J Dent. 2015;43:335–341. doi: 10.1016/j.jdent.2014.12.012. [DOI] [PubMed] [Google Scholar]