Abstract
BACKGROUND:
We sought to evaluate the risk factors for developing ventilator-associated pneumonia (VAP) and whether the location of intubation posed a risk in trauma patients.
METHODS:
Data were retrospectively reviewed for adult trauma patients requiring intubation for > 48 hours, admitted between 2010 and 2013. Patients’ demographics, clinical presentations and outcomes were compared according to intubation location (prehospital intubation [PHI] vs. trauma room [TRI]) and presence vs. absence of VAP. Multivariate regression analysis was performed to identify predictors of VAP.
RESULTS:
Of 471 intubated patients, 332 patients met the inclusion criteria (124 had PHI and 208 had TRI) with a mean age of 30.7±14.8 years. PHI group had lower GCS (P=0.001), respiratory rate (P=0.001), and higher frequency of head (P=0.02) and chest injuries (P=0.04). The rate of VAP in PHI group was comparable to the TRI group (P=0.60). Patients who developed VAP were 6 years older, had significantly lower GCS and higher ISS, head AIS, and higher rates of polytrauma. The overall mortality was 7.5%, and was not associated with intubation location or pneumonia rates. In the early-VAP group, gram-positive pathogens were more common, while gram-negative microorganisms were more frequently encountered in the late VAP group. Logistic regression analysis and modeling showed that the impact of the location of intubation in predicting the risk of VAP appeared only when chest injury was included in the models.
CONCLUSION:
In trauma, the risk of developing VAP is multifactorial. However, the location of intubation and presence of chest injury could play an important role.
Keywords: Ventilator-associated pneumonia, Trauma, Mechanical ventilation, Intubation location, Intensive care unit
INTRODUCTION
Ventilator-associated pneumonia (VAP) is the most frequent cause of nosocomial infection among critically ill patients requiring mechanical ventilation, with an estimated incidence of 9%–27%.[1] VAP is associated with the need for prolonged ventilatory support, ICU and hospital length of stay, and increased healthcare cost.[2,3] Data from the National Healthcare Safety Network report showed a 4-fold higher rate of VAP in intubated trauma ICU patients as compared with non-trauma cases.[3] This is likely due to the fact that trauma patients have more risk factors for VAP. These include prehospital intubation, emergency intubation, closed head and spinal cord injury, blunt chest trauma, high injury severity, and shock.4–10 The type of strains involved in the pathogenesis of VAP also showed an association with duration of mechanical ventilation. Early-VAP is associated with more antibiotic-sensitive microorganisms, while resistant strains are frequently observed with late-onset VAP.[11] Some investigators have identified predisposing factors such as pre-injury environmental exposure, patients’ demographics, chest injury burden, traumatic brain injury, pre-existing comorbidities and antibiotic exposure as additional risk factors for developing VAP post injury.[4,12] Moreover, previous studies have suggested that trauma patients undergoing emergent intubation in the prehospital setting have an increased risk of acquiring VAP.[9,10,13,14] Others have demonstrated no difference in the rate of VAP according to location of intubation.[15,16] Controversy continues regarding the role of intubation location in the development of VAP following trauma. In addition, information regarding the occurrence and predisposing factors for VAP in trauma patients in the Gulf region is not well studied yet. Data regarding the effect of intubation location on VAP incidence in our locality could be useful for risk stratification and early diagnosis. Therefore, the purpose of the present study is to explore the risk factors for developing VAP in trauma patients from a rapidly developing Middle Eastern country, and in particular, whether the location of intubation poses an additional risk for pneumonia.
METHODS
We performed a retrospective chart review of all consecutive adult trauma patients requiring intubation and ventilation to the level 1 trauma centre of Hamad General Hospital (HGH) from January 2010 to January 2013.
HGH is a 590-bed hospital serving as the only tertiary care center in Qatar. The Trauma Centre is Trauma Association Canada (TAC) accredited and includes a specialized 19-bed trauma intensive care unit. Our emergency medical service (EMS) program constitutes ground and helicopter ambulance (Life Flight) services with advanced airway management skill capabilities. These include rapid sequence intubation with neuromuscular blockade. All airways are secured by orotracheal route. Intubation in the prehospital setting is performed by a dedicated critical care paramedic staff trained in airway management. In the Trauma Resuscitation Room intubations (TRI) are performed by experienced trauma anesthesiologists, or by trauma surgeons trained in intubation.
The study included all trauma patients intubated either in the prehospital setting or in the trauma room, who were ventilated for 2 or more days and were followed during the hospital course. Patients with burns, drowning, death or who were discharged or transferred to other facilities within 48 hours of admission, were excluded. Data were extracted from the trauma registry database and medical records. Ethical approval was obtained from the Medical Research Center at Hamad Medical Corporation, Doha, Qatar, (IRB# 14014/14).
For each patient, data collection included demographics, mechanism of injury, vital signs, injury severity score (ISS), abbreviated injury score (AIS), Glasgow Coma Scale (GCS) at emergency department (ED), intubation location (prehospital or trauma room), associated injuries, blood alcohol level, clinical diagnosis of pneumonia, days to develop VAP (early (≤4 days) and late-onset(> 4 days), microbiology of VAP, ventilatory days, ICU and hospital length of stay and mortality.
The AIS for head and chest was recorded for each patient, to determine the overall ISS. The primary outcome measure was the diagnosis of VAP, and the secondary outcome measures included length of mechanical ventilation, ICU and hospital length of stay and mortality.
VAP is defined as pneumonia that occurs 48–72 hours or thereafter following endotracheal intubation, characterized by the presence of a new or progressive infiltrate on chest radiograph, signs of systemic infection (fever, altered white blood cell count), changes in sputum characteristics, and detection of a microorganism.[17] All pneumonia patients were clinically diagnosed based on the respiratory specimen finding of semi-quantitative cultures obtained by mini- bronchoalveolar (BAL). Early-onset VAP was diagnosed as pneumonia occurring less than or equal to 4 days of endotracheal intubation, and late-onset VAP as that developing more than 4 days after endotracheal intubation.
Statistical analysis
Data were presented as proportions, medians (range), or mean (±standard deviation; SD) as appropriate. Baseline demographic characteristics, clinical presentation, and outcomes were compared according to site of intubation (prehospital vs. trauma room). Occurrence of VAP based on intubation location and VAP vs. no-VAP was analyzed using the student-t test for continuous variables and Pearson’s Chi-square (χ2) test for categorical variables. We also compared microbiological characteristics in patients developed VAP according to site of intubation and days to developing VAP (early and late-onset). Multivariate regression analysis and modeling were performed to identify the predictors for VAP after adjusting for the potential relevant confounding variables. Results were presented using odds ratio (OR) and 95% confidence intervals (CI). A significant difference was considered when the two-tailed P value was less than 0.05. Data analysis was carried out using the Statistical Package for Social Sciences version 18 (SPSS Inc. USA).
RESULTS
Out of the total 471 intubated patients, 332 met the inclusion criteria; 124 (37%) were intubated in the prehospital setting (PHI) and 208 (63%) were intubated immediately upon arrival to the trauma room (TRI). The patients mean age was 30.7±14.8 years with 92.5% being male. The commonest mechanisms of injury were blunt trauma (including motor vehicle collision) (64.4%) and fall from height (22.7%). Penetrating injuries such as gunshot wounds, assault or stabbing (5.4%), and self-inflicted (1.5%), were infrequent (Table 1). The mean ISS was 21.0±9.4. Three quarters (76.1%) were victims of polytrauma; 245 had traumatic brain injury with head AIS of 3.6±0.9, and 52.0% had blunt chest trauma with chest AIS of 2.9±0.6. Thirty-nine (11.9%) cases were ethanol positive with an average blood alcohol level of 44±18 mmol/L.
Table 1.
Demographic, clinical characteristics and outcomes of all intubated trauma patients by site of intubation
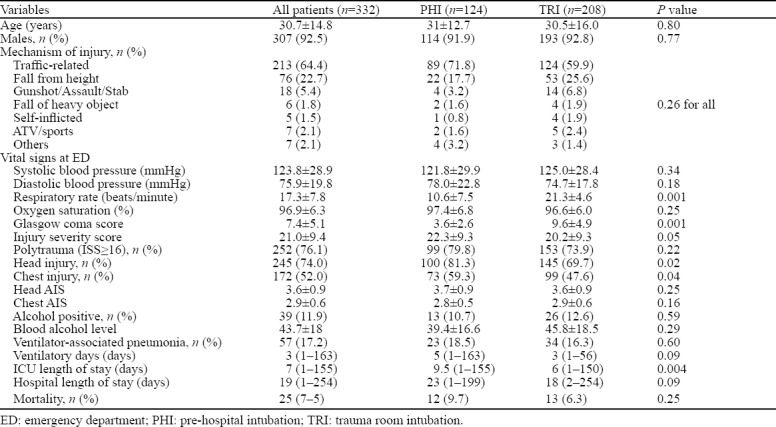
Table 1 shows the demographics, clinical characteristics and outcomes of all intubated trauma patients according to the site of intubation. The two groups were comparable for age, gender, mechanism of injury, and vital signs except respiratory rate which was significantly lower in the PHI group (10.6±7.5 vs. 21.3±4.6, P=0.001). The overall mean GCS was 7.4±5.1 and PHI group had lower GCS (3.6±2.6 vs. 9.6±4.9, P=0.001) in comparison to TRI group.
Patients intubated in the prehospital setting had higher frequency of head (81.3% vs. 69.7%; P=0.02) and chest (59.3% vs. 47.6%, P=0.04) injuries than those in the TRI group. The overall rate of VAP in this study was 17.2% (n=57) and the two groups did not differ significantly with respect to the frequency of VAP (18.5% vs. 16.3%; P=0.60). The median ventilatory days was 3 (1–163), ICU length of stay was 7 (1–155) days and hospital stay was 19 (1–254). Also, patients in the PHI group stayed longer in the ICU (P=0.004). The overall mortality was 7.5% (25 patients) which did not differ significantly according to the location of intubation (9.7% vs. 6.3%, P=0.25).
Table 2 shows clinical characteristics and outcomes of patients who developed VAP based on intubation location. The two groups were comparable for age, gender, and initial vitals. Patients who developed VAP in the PHI group had significantly lower respiratory rates (7.6±6.6 vs. 20.8±4.8, P=0.001) and median GCS (3 [3–3] vs. 6.5 [3–15]; P=0.001) as compared to the patients intubated in the trauma room. The ISS, head AIS and chest AIS was similar between the two groups. Also, patients with early VAP (≤4 days) and late VAP (≥4 days) did not differ significantly (P=0.41). The PHI group had a higher mean WBC count on the day of VAP onset (12.7±6.3 vs. 9.9±2.8; P=0.03) than the TRI group. The ventilator days, length of ICU and hospital stay and mortality rate (19.2% vs. 17.9%, P=0.89) were also similar between the two groups.
Table 2.
Demographic, clinical characteristics and outcomes of trauma patients developed ventilator-associated pneumonia
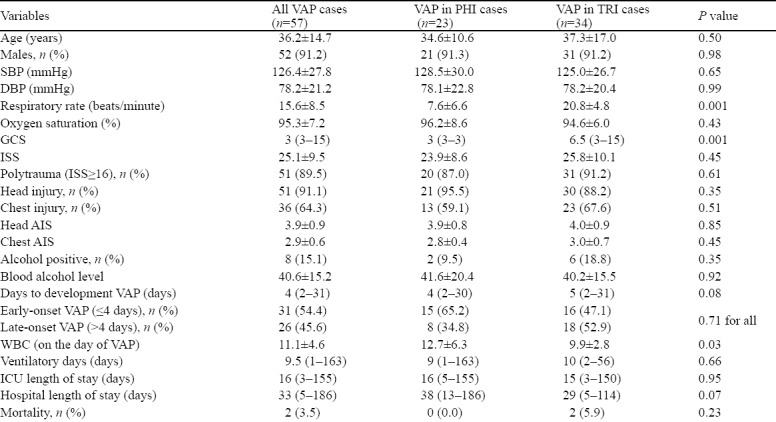
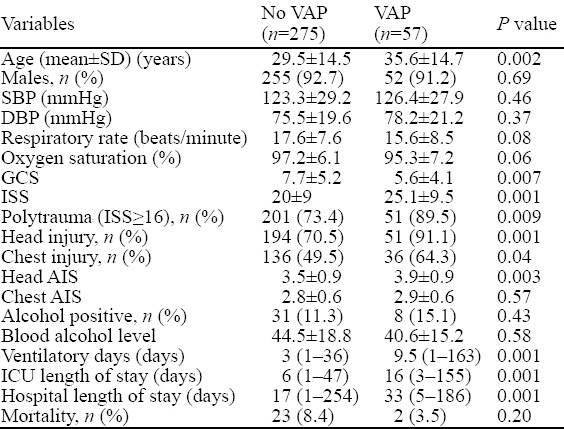
Table 3 shows the clinical profile and outcome in patients with and without VAP. Overall, 57 patients developed VAP; those who developed pneumonia were 6-years older and were more severely injured as indicated by a higher ISS (P=0.001), head AIS (P=0.003) and sustained frequent polytrauma (P=0.009), head (P=0.001) and chest (P=0.04) injuries, and had a lower GCS (P=0.007). Also, the duration of mechanical ventilation (P=0.001), length of ICU (P=0.001) and hospital stay (P=0.001) were longer in the pneumonia group. The rate of mortality did not differ significantly in the VAP and the non-VAP group (8.4% vs. 3.5, P=0.20).
Table 3.
Comparison of demographics, clinical presentation and outcomes in patients with and without VAP
The diagnosis of VAP was confirmed by semi-quantitative culture obtained by mini-BAL. The microbiological characteristics of patients who developed VAP showed that Klebsieilla pneumoniae (36.1%) and Hemophilus influenza (29.8%) were the commonest identified microorganisms, followed by Staphylococcus aureus (28.1%), Streptococcus pneumoniae (15.8%), Enterobacter cloacae (12.3%) and Pseudomonas aureginosa (12.3%) (Table 4). In the PHI group, Staphylococcus aureus (34.8%) and Hemophilus influenza (30.4%) were the most frequently isolated organisms. In the TRI group, the predominantly identified species were Klebseilla pneumoniae (38.2%), Hemophilus influenza (29.4%), and Staphylococcus aureus (23.5%). The most common microorganisms in early VAP were gram-positive pathogens, while in the late VAP group gram-negative pathogens were more frequent isolated (Table 5).
Table 4.
Microbiological characteristics of patients developed ventilator-associated pneumonia by the site of intubation, n (%)
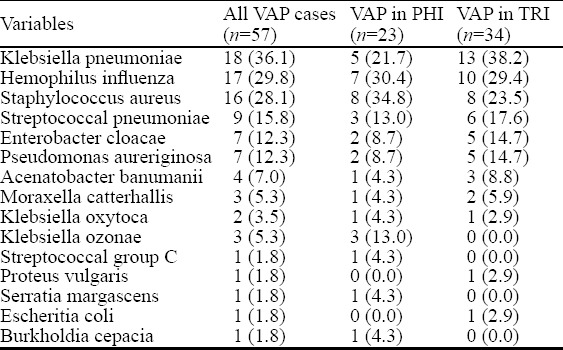
Table 5.
Sputum culture in patients with early and late onset of VAP by intubation location, n (%)
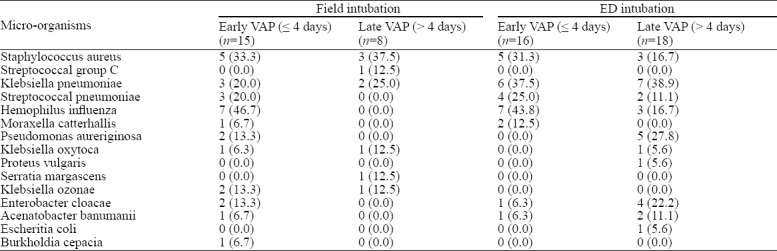
In the PHI group, out of 23 patients with VAP, only 1 patient had Multi-drug resistant organisms (MDRO) in terms of Acinetobacter Baumani sensitive to Vancomycin. In the TRI group, out of 34 patients with VAP, 2 patients had MDRO (1 patient had Acinetobacter Baumani sensitivity to Colistin and 1 patient had Staphylococcus aureus sensitive to vancomycin and this patient expired)
Figure 1 shows the association between polytrauma and the development of late-onset VAP (100% vs. 80.6%, P=0.02).
Figure 1.
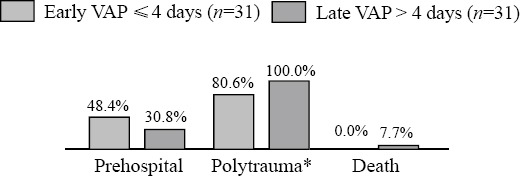
Comparison of early versus late VAP (P<0.05).
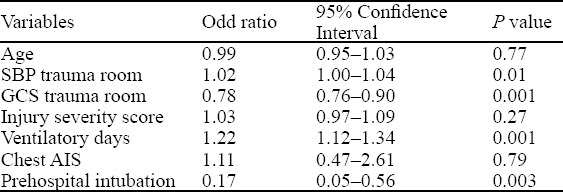
Multivariate logistic regression after adjusting for age, systolic BP in ED, GCS ED, chest AIS, head AIS, prehospital intubation, ISS, and ventilatory days, showed that systolic blood pressure (OR 1.02 [1.00–1.04], P=0.01), GCS trauma room (OR 0.78 [0.76–0.90], P=0.001), prehospital intubation (OR 0.17 [0.05–0.56]), P=0.003), and ventilatory days (OR 1.22 [1.12–1.34], P=0.001) were predictors of VAP in trauma patients (Table 6).
Table 6.
Predictors of VAP in trauma patients
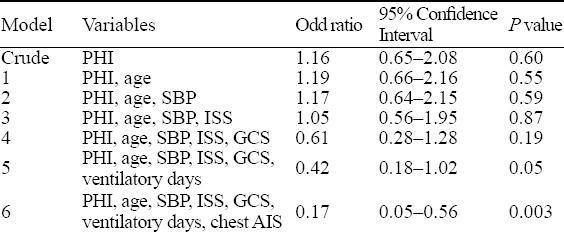
However, the multi-level regression analysis models revealed that the impact of location of intubation in predicting the risk of VAP appeared only when chest injury was included in the models; PHI (crude OR 1.16, 95% CI 0.65–2.08, P=0.60, adjusted OR 0.17, 95% CI 0.05–0.56, P<0.003) (Table 7).
Table 7.
Regression analysis models for prehospital intubation (PHI) to predict the risk of VAP
DISCUSSION
The present study describes the frequency, risk factors, and outcome of VAP in injured patients requiring intubation, and also compares the clinical characteristics and outcomes based on the location of intubation from a single level I trauma center.
Despite advances in prevention, diagnosis and treatment of VAP, it remains a major contributor to morbidity and mortality in critically ill intubated patients.[1] In our series, two-thirds of patients were intubated in the trauma room and one-third was intubated in the prehospital setting. The frequency of PHI in our study is almost half of the reported PHI by Evans et al.[15] On the other hand, an earlier study[10] from the USA reported urgent PHI in only 15% of cases. Several studies have suggested that trauma patients are particularly more susceptible to developing VAP as compared to medical and surgical patients.[6,7] This could be explained by the fact that patients undergoing emergent PHI have higher risks of aspiration, higher rates of severe head injury, more hemodynamic instability, decreased levels of consciousness and higher Injury Severity Scores.7–10 Earlier studies have identified trauma to be an independent predictor of progression to VAP.[7,18,19]
According to the present analysis, the overall rate of VAP in all intubated patients is 17.2%, which is in agreement with other studies, with an estimated incidence of 9%–27% in mechanically ventilated patients; the highest risk period appears to be early in the course of hospitalization.[17,18] Moreover, some investigators have considered a higher risk of VAP among trauma patients intubated at the scene than those intubated in the ED.[20]
Karch et al[14] retrospectively reviewed 94 severely injured cases and found that patients required PHI were three times more likely to develop VAP when compared with hospital intubation. Similarly, Eckert et al[9] performed a retrospective analysis of 571 mechanically ventilated trauma patients. The authors identified a significant association between PHI and the occurrence of VAP. However, others have failed to observe such an association and concluded that there was no association between prehospital intubation and risk of developing VAP.[15,16] Similarly, on univariate analysis we did not observe significant differences with respect to the frequency of VAP in the prehospital and trauma room intubation cohorts.
The crude odds ratio for PHI to predict VAP was statistically not significant, whereas on using multiple models, the effect of PHI became significant after introducing the chest injury variable in the model. Our findings are consistent with a study by Evan et al,[15] where the baseline VAP rate was 17.6% and the rate of VAP was similar between prehospital intubation and trauma room intubation groups.
Furthermore, Mohr et al[16] suggested that location of intubation in trauma patients did not influence the occurrence of VAP.
A recent study suggested that patients with traumatic brain injury are more likely to develop VAP.[21] Similarly, our data showed that patients who were intubated in the prehospital setting had frequent head and chest injuries, lower GCS, and higher ISS.
This indicates that severity of injury necessitates earlier airway acquisition, but did not indicate higher possibility of VAP based on intubation location (mean ISS was similar between PHI and TRI groups). This finding is particularly notable as the rate of polytrauma (ISS≥16) was fairly high in both groups. Similarly, Eckert et al[10] reported that patients with pre hospital intubation had higher ISS, and lower GCS score and Revised Trauma Scoring (RTS) as compared to ED intubation. The higher incidence of VAP among PHI patients could be attributed to the lower mean GCS which compromised the physiologic state and necessitated emergent airway acquisition.
In comparison with patients who did not develop VAP, advanced age, higher injury severity, head AIS scores, presence of head and chest injuries and lower GCS were significantly associated with the development of VAP in our series. Data from other studies also identified age, ISS, head injury, extremity injury, and field intubation to be risk factors for the occurrence of pneumonia.[9] Moreover, inherent injury characteristics such as levels of consciousness (GCS), emergent intubations, and presence of chest trauma might help in predicting the risk of VAP.[13]
It is imperative to assess the microbiological findings for the distribution of infecting microorganisms. In our cohort, the frequently identified organisms were Klebseilla pneumonia, Hemophilus influenza and Staphylococcus aureus, which is consistent with other studies.[22,23] Moreover, the PHI group had a higher frequency of community acquired organisms such as Hemophillus influenza and Staphylococcus aureus which is in agreement with a previous report by Eckert et al.[10] Overall, the distributions of gram-positive and negative microorganisms were similar among the PHI and TRI groups.
Notably, we also observed an association of VAP with prolonged ventilatory days, higher length of ICU and hospital days. These findings are in agreement with earlier studies.[9,15]
Because of the high incidence of associated chest injuries, low GCS and high probability of aspiration, the clinical diagnosis of VAP is often difficult. The Center for Disease Control and Prevention (CDC) surveillance definition does not differentiate among trauma associated complications and hospital-acquired infections.[24] Mangram et al[4] concluded that the CDC surveillance definition of VAP needs to be modified to reflect the effect of trauma factors such as rib fractures, pulmonary contusions, and failed prehospital intubations (all considered significant predictors of pneumonia).
Evans et al[15] demonstrated that ISS, history of drug abuse, and low ED systolic blood pressure were associated with VAP, but not the location of intubation. Contrarily, other investigators reported age, GCS score, ISS and prehospital intubation to be strongly predictive of VAP in trauma patients.[10] Antenolli et al[25] demonstrated that the presence of pulmonary contusion and abbreviated injury scale of >4 for thorax were significant independent predictors of pneumonia after injury. Another study identified rib fractures, pulmonary contusion, and failed prehospital intubation to be important predictors of VAP.[4]
An earlier study[10] showed higher rate of mortality in the VAP group (33%) who were intubated in the prehospital setting compared to those who were intubated in the ED (6.3%) or as inpatients (24%).
It has been suggested that higher ISS, low GCS and advanced age are associated with the development of VAP in patients intubated at the scene and such factors might also contribute towards the higher mortality rate in the PHI group. Eckert et al[9] showed that patients intubated in the prehospital setting had a lower mortality despite having lower GCS and higher ISS. The incidence of VAP was similar between the two groups irrespective of the injury severity. Evans et al[15] showed that mortality was comparable in the PHI and emergency room intubation groups, despite lower GCS in the PHI group. In line with these reports, Magret et al[26] showed that VAP in trauma patients was associated with lower mortality when compared with non-trauma patients after adjusting for sex, age, severity of illness, and sepsis-related organ failure assessment score . In our series, the rate of mortality did not differ significantly among the VAP and non-VAP cases. Therefore, the attributable risk of mortality due to VAP in trauma patients remains uncertain.[27]
The present study has various limitations owing to the inherent nature of retrospective data collection and quality of reporting at the scene. There may be potential bias in defining VAP in trauma versus non-trauma patients, and this may require a more concise definition for trauma patients. The microbial culture results could be affected due to the semi-quantitative method for diagnosing VAP, instead of the more sensitive quantitative analysis. There was no documentation of history of vomiting, aspiration, bag valve mask ventilation or supraglotic airway device use – all factors that could have affected the outcomes. It is conceivable that some patients arrived at the trauma room with supraglotic devices which were later changed to an endotracheal tube but not recorded in the database. The analysis is further constrained by the deficiency of documentation regarding vasopressor use in the trauma room.
We also lack information on the frequency of failed prehospital intubations, which may influence the hospital outcomes.
CONCLUSIONS
In adult patients with polytrauma, the risk of developing VAP is multifactorial; however, the location of intubation and presence of chest injury could play an important role. Identification of risk factors is an important marker for developing strategies to reduce or eliminate the rate of VAP in trauma patients.
ACKNOWLEDGEMENT
We thank all the staff of trauma surgery for their cooperation.
Footnotes
Funding: This research did not receive any specific grant from any funding agency in the public, commercial or not-for-profit sector.
Ethics approval: Ethical approval was obtained from the Medical Research Center (IRB# 14014/14) and waiver consent was approved for this retrospective study by the Hamad Medical Corporation, Doha, Qatar.
Competing interests: The authors declare that they have no competing interests.
Authors’ contributions: All authors (SA,IM,GS,AE,AH,HA) have made substantial contributions to all of the following: (1) the conception and design of the study, or acquisition of data, or analysis and interpretation of data, (2) drafting the article or revising it critically for important intellectual content, (3) final approval of the version to be submitted
REFERENCES
- 1.Kalanuria AA, Ziai W, Mirski M. Ventilator-associated pneumonia in the ICU. Crit Care. 2014;18:208. doi: 10.1186/cc13775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tablan OC, Anderson LJ, Besser R, Bridges C, Hajjeh R, Tablan OC, et al. Guidelines for preventing health-care--associated pneumonia 2003:recommendations of CDC and the Healthcare Infection Control Practices Advisory Committee. MMWR Recomm Rep. 2004;53(RR-3):1–36. [PubMed] [Google Scholar]
- 3.Dudeck MA, Weiner LM, Allen-Bridson K, Malpiedi PJ, Peterson KD, Pollock DA, et al. National Healthcare Safety Network (NHSN) report, data summary for 2012, Device-associated module. Am J Infect Control. 2013;41(12):1148–66. doi: 10.1016/j.ajic.2013.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mangram AJ, Sohn J, Zhou N, Hollingworth AK, Ali-Osman FR, Sucher JF, et al. Trauma-associated pneumonia:time to redefine ventilator-associated pneumonia in trauma patients. Am J Surg. 2015;210:1056, 61. doi: 10.1016/j.amjsurg.2015.06.029. discussion: 1061-2. [DOI] [PubMed] [Google Scholar]
- 5.Magnotti LJ, Croce MA, Fabian TC. Is ventilator–associated pneumonia in trauma patients an epiphenomenon or a cause of death? Sur Infect (Larchmt) 2004;5:237–42. doi: 10.1089/sur.2004.5.237. [DOI] [PubMed] [Google Scholar]
- 6.Rello J, Ollendorf DA, Oster G, Vera-Llonch M, Bellm L, Redman R, et al. Epidemiology and outcomes of ventilator-associated pneumonia in a large US database. Chest. 2002;122(6):2115–21. doi: 10.1378/chest.122.6.2115. [DOI] [PubMed] [Google Scholar]
- 7.Wallace WC, Cinat M, Gornick WB, Lekawa ME, Wilson SE. Nosocomial infections in the surgical intensive care unit:a difference between trauma and surgical patients. Am Surg. 1999;65:987–90. [PubMed] [Google Scholar]
- 8.Cook DJ, Walter SD, Cook RJ, Griffith LE, Guyatt GH, Leasa D, et al. Incidence of and risk factors for ventilator-associated pneumonia in critically ill patients. Ann Intern Med. 1998;129(6):433–40. doi: 10.7326/0003-4819-129-6-199809150-00002. [DOI] [PubMed] [Google Scholar]
- 9.Eckert MJ, Davis KA, Reed RL, 2nd, Santaniello JM, Poulakidas S, Esposito TJ, et al. Urgent airways after trauma:who gets pneumonia? J Trauma. 2004;57(4):750–5. doi: 10.1097/01.ta.0000147499.73570.12. [DOI] [PubMed] [Google Scholar]
- 10.Eckert MJ, Davis KA, Reed RL, 2nd, Esposito TJ, Santaniello JM, Poulakidas S, et al. Ventilator-associated pneumonia, like real estate:location really matters. J Trauma. 2006;60(1):104–10. doi: 10.1097/01.ta.0000197376.98296.7c. discussion 110. [DOI] [PubMed] [Google Scholar]
- 11.Jovanovic B, Milan Z, Markovic-Denic L, Djuric O, Radinovic K, Doklestic K, et al. Risk factors for ventilator-associated pneumonia in patients with severe traumatic brain injury in a Serbian trauma centre. Int J Infect Dis. 2015;38:46–51. doi: 10.1016/j.ijid.2015.07.005. [DOI] [PubMed] [Google Scholar]
- 12.Zarzaur BL, Bell TM, Croce MA, Fabian TC. Geographic variation in susceptibility to ventilator-associated pneumonia after traumatic injury. J Trauma Acute Care Surg. 2013;75(2):234–40. doi: 10.1097/TA.0b013e3182924c18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Croce MA, Fabian TC, Tolley EA. A formula for prediction of post-traumatic pneumonia based on early anatomic and physiologic parameters. J Trauma. 2003;54:724–30. doi: 10.1097/01.TA.0000054643.54218.C5. [DOI] [PubMed] [Google Scholar]
- 14.Karch SB, Lewis T, Young S, Hales D, Ho CH. Field intubation of trauma patients:complications, indications and outcomes. Am J Emerg Med. 1996;4(7):617–9. doi: 10.1016/S0735-6757(96)90073-X. [DOI] [PubMed] [Google Scholar]
- 15.Evans HL, Zonies DH, Warner KJ, Bulger EM, Sharar SR, Maier RV, et al. Timing of intubation and ventilator-associated pneumonia following injury. Arch Surg. 2010;145(11):1041–6. doi: 10.1001/archsurg.2010.239. [DOI] [PubMed] [Google Scholar]
- 16.Mohr NM, Harland KK, Skeete D, Pearson K, Choi K. Duration of prehospital intubation is not a risk factor for development of early ventilator-associated pneumonia. J Crit Care. 2014;29(4):539–44. doi: 10.1016/j.jcrc.2014.03.030. [DOI] [PubMed] [Google Scholar]
- 17.American Thoracic Society Infectious. Diseases Society of America. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2005;171(4):388–416. doi: 10.1164/rccm.200405-644ST. [DOI] [PubMed] [Google Scholar]
- 18.Chastre J, Fagon JY. Ventilator-associated pneumonia. Am J Respir Crit Care Med. 2002;165(7):867–903. doi: 10.1164/ajrccm.165.7.2105078. [DOI] [PubMed] [Google Scholar]
- 19.Cook DJ, Kollef MH. Risk factors for ICU acquired pneumonia. JAMA. 1998;279(20):1605–6. doi: 10.1001/jama.279.20.1605. [DOI] [PubMed] [Google Scholar]
- 20.Evans HL, Warner K, Bulger EM, Sharar SR, Maier RV, Cuschieri J. Pre-hospital intubation factors and pneumonia in trauma patients. Surg Infect (Larchmt) 2011;12(5):339–44. doi: 10.1089/sur.2010.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gianakis A, McNett M, Belle J, Moran C, Grimm D. Risk factors for ventilator-associated pneumonia:among trauma patients with and without brain injury. J Trauma Nurs. 2015;22(3):125–31. doi: 10.1097/JTN.0000000000000121. [DOI] [PubMed] [Google Scholar]
- 22.Chen LP, Chen JH, Chen Y, Wu C, Yang XH. Efficacy and safety of glucocorticoids in the treatment of community-acquired pneumonia:A meta-analysis of randomized controlled trials. World J Emerg Med. 2015;6(3):172–8. doi: 10.5847/wjem.j.1920-8642.2015.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Michelet P, Couret D, Brégeon F, Perrin G, D'Journo XB, Pequignot V, et al. Early onset pneumonia in severe chest trauma:a risk factor analysis. J Trauma. 2010;68(2):395–400. doi: 10.1097/TA.0b013e3181a601cb. [DOI] [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention. Ventillator-associated Pneumonia (VAP) Events 2017. [Accessed March 4, 2017]. Available at: https://www.cdc.gov/nhsn/pdfs/pscmanual/10-vae_final.pdf .
- 25.Antonelli M, Moro ML, Capelli O, De Blasi RA, D'Errico RR, Conti G, et al. Risk factors for early onset pneumonia in trauma patients. Chest. 1994;105(1):224–8. doi: 10.1378/chest.105.1.224. [DOI] [PubMed] [Google Scholar]
- 26.Magret M, Amaya-Villar R, Garnacho J, Lisboa T, Díaz E, Dewaele J, et al. Ventilator-associated pneumonia in trauma patients is associated with lower mortality:results from EU-VAP study. J Trauma. 2010;69(4):849–54. doi: 10.1097/TA.0b013e3181e4d7be. [DOI] [PubMed] [Google Scholar]
- 27.Melsen WG, Rovers MM, Bonten MJ. Ventilator-associated pneumonia and mortality:a systematic review of observational studies. Crit Care Med. 2009;37(10):2709–18. doi: 10.1097/ccm.0b013e3181ab8655. [DOI] [PubMed] [Google Scholar]


