Abstract
BACKGROUND:
Maternal and infant mortality rates reported in rural Panama are greater than those in urban regions. Bocas del Toro is a region of Panama inhabited by indigenous people at greater risk for pregnancy-related complications and deaths due to geographic isolation and limited access to health care. Portable ultrasound training programs have recently been implemented in low-resource settings to increase access to diagnostic imaging. The goal of this study is to determine the feasibility of teaching first-year medical students the Rural Obstetrical Ultrasound Triage Exam (ROUTE) to help identify pathology in pregnant women of the Bocas del Toro region of Panama.
METHODS:
Eight first-year medical students completed ROUTE training sessions. After training, the students were compared to professional sonographers to evaluate their accuracy in performing the ROUTE. Students then performed the ROUTE in mobile clinics within Bocas del Toro. They enrolled women pregnant in their 2nd or 3rd trimesters and measured biparietal diameter, head circumference, amniotic fluid index, fetal lie and placental position. Any abnormal measurement would be further analyzed by the lead physician for a potential hospital referral.
RESULTS:
A total of 60 women were enrolled in the study. Four women were detected as having a possible high-risk pregnancy and thus referred to a hospital for further evaluation.
CONCLUSION:
Based on our data, first-year medical students with additional training can use the ROUTE to identify complications in pregnancy using ultrasound in rural Panama. Additional studies are required to determine the optimal amount of training required for proficiency.
Keywords: Point of care ultrasound, Ultrasound education, Rural Panama, Obstetrics ultrasound
INTRODUCTION
Complications of pregnancy and childbirth continue to be a leading cause of death in developing countries, claiming the lives of both mothers and infants worldwide.[1] In rural areas of Panama, infant and maternal mortality rates are reported to be significantly greater than those in urban regions of the country. The United Nations Population Fund has determined the maternal death rate in Panama to be 70 deaths per 100,000 live births, but this number increases to 658 deaths per 100,000 live births in the rural, indigenous populations.[2,3] Lack of access to health care due to extreme poverty, lack of transportation, deeply rooted cultural beliefs, and, in some areas, a distrust of modern health services all contribute to this dichotomy within maternal health rates in Panama.[2,3] Similar trends are seen in infant mortality rates in rural versus urban Panama. In Bocas del Toro, a primarily indigenous province of Panama populated by the Ngobe Bugle people, the infant mortality rate is three times greater than that of the country as a whole.[4] Infant mortality is so pervasive, that the Ngobe refer to all children under the age of 3 as “chichi” meaning “baby” until the child comes of age.
Due to the need for health care in rural settings, ultrasound has become more prevalent in resource poor environments. Given the declining costs of portable ultrasound machines and ability to obtain diagnoses at bedside, ultrasound is emerging as a key imaging modality in the developing world.[5] The relatively high diagnostic capabilities within the field of obstetrics and the increasing availability of ultrasound machines have recently made them a useful tool in addressing high maternal mortality rates in developing countries. Adler et al[6] introduced portable ultrasound in a refugee camp in Tanzania with the purpose of triaging for a variety of physical presentations and found it to be a useful innovation. He found that health care workers with basic training could learn how to use ultrasound for obstetric indications. This use of ultrasound resulted in a change in management in 14% of cases. Another group led a two-week ultrasound-training program in rural Gambia and found that it became a useful tool in addressing the specific needs of the population.[7] Currently, local physicians have embraced ultrasound into daily use and adapted it into their training.
In 2010, Kimberly et al[8] implemented a six-month ultrasound training aimed at establishing ROUTE in rural Zambia utilizing midwives. Eight midwives trained in ultrasound demonstrated improved clinical ultrasound examination skills near the end of the program. Furthermore, the use of ultrasound for diagnostic indications led to a change in management of 17% of the patients. Previous studies with similar designs have shown that minimally trained medical students are capable of learning ROUTE effectively and that medical students are capable of teaching ROUTE to others.[9,10]
The goal of this study was to determine if first-year medical students were able to perform and interpret the ROUTE after minimal training and obtain adequate quality images to assess for obstetric ultrasound abnormalities as compared to professionally trained sonographers. A secondary outcome was to determine if minimally trained first-year medical students were able to identify specific obstetric pathology that could be validated by review of a board certified Obstetrician and Gynecologist.
METHODS
Study design and setting
Eight first-year medical students from the United States completed six training sessions of the ROUTE with a third-year Obstetrics and Gynecology resident physician. All students had completed an entire first year of medical education which included human physiology, human anatomy, gastrointestinal and genitourinary anatomy, and a basic ultrasound program. In addition, all eight students received a total of twelve hours of obstetric ultrasound instruction, termed the “Rural Obstetric Ultrasound Triage Exam” (ROUTE). ROUTE includes the identification of the following variables: fetal lie, placental position, deepest vertical pocket (DVP), amniotic fluid index (AFI), biparietal diameter (BPD), and head circumference (HC) for patients in the second or third trimester of pregnancy.
At the completion of all six training sessions, students were evaluated for competency by a board-certified Obstetrics and Gynecology physician in performing the ROUTE at the UC Irvine Center for Fetal Evaluation (UCI CFE). Patients presenting for evaluation by sonographers were consented for ultrasound scanning by medical students. All students recorded each of the variables included in the ROUTE prior to scanning by a professional sonographer. Values and measurements obtained by each student included fetal lie, placental position, deepest vertical pocket (DVP), amniotic fluid index (AFI), biparietal diameter (BPD), and head circumference (HC). Students were also evaluated on their ability to detect fluid abnormalities by determining if the DVP or AFI was within normal range. Pregnant women presenting with multiparity, breech fetal lie, oligohydramnios/polyhydramnios (DVP <2 cm or >8 cm, respectively), low amniotic fluid index, or placenta previa were considered as a positive result for the respective categories. Finally, students were assessed on their ability to detect placental location (anterior/posterior/fundal) and indicate whether or not the placental proximity to the cervix may put a patient at risk for complications during delivery.
Application of ROUTE in Panama
This was a blinded, investigational study utilizing a convenience sample of pregnant patients presenting for voluntary evaluation between June 20, 2017 to July 11, 2017. The study was approved by the domestic site Institutional Review Board. The study took place in Bocas Del Toro, Panama where a mobile clinic was established for community healthcare screening and ultrasonographic evaluation by medical student volunteers and international board certified physicians. Ultrasound screening took place on selected days throughout this time period.
Pregnant women in their second or third trimesters that presented to the clinic for evaluation were approached by one of the medical students after treatment was completed. A study information sheet outlining the details of the study in Spanish was given to the patients. Additionally, Spanish and Ngobe bedside translators were used to introduce and explain the study to all participants. Informed written and verbal consent was obtained from each patient prior to enrollment.
Intervention
Enrolled patients were taken into private patient rooms to perform the ROUTE. Prior to conducting the scan, patients were asked a series of questions to obtain the following: last menstrual period (LMP), pre-existing conditions, gravidity, parity, history of pregnancy complications if applicable, history of twins, current pregnancy complications if known, use of contraception, desire to use contraception in the future, and prenatal vitamin use. LMP was used to approximate gestational age before performing the ROUTE to determine which specific parameters to scan. Medical students used ultrasound to measure biparietal diameter, head circumference, fetal lie, and placental location for all pregnancies. For second trimester patients, deepest vertical pocket (DVP) was obtained while for third trimester patients, amniotic fluid index (AFI) was measured.
The ultrasound scan was performed using a curvilinear probe (C60) on the obstetrical exam setting with a Sonosite M-Turbo ultrasound machine. Based on variable records, images were categorized by students as “normal” or “abnormal”. Biparietal diameter and head circumference measurements were compared to gestational age to determine if growth was within normal limits. Additionally, placental location and fluid levels were measured to detect for abnormalities. Students documented all findings, which were then reviewed by the treating physician. The physician then informed the patient of any identified abnormalities. Any patient confirmed to have abnormalities requiring advanced care was instructed to be transferred to the nearest hospital for continued care and management.
Images of all findings were recorded and retrospectively reviewed by a blinded Obstetrics and Gynecology physician trained in the use and interpretation of ultrasound. Ultrasound scans were recorded and sent electronically over an encrypted server to confirm findings. All findings for each patient were recorded onto standardized data collection sheets and then coded into electronic documentation for storage and data analysis. Paper copies of all data were subsequently destroyed at the end of the data enrollment period. Patients with abnormal findings were notified and referred to see an Obstetrics and Gynecologic Physician for further testing.
Methods of measurement and outcome measures
The primary outcome of the study was to determine if first-year medical students were able to obtain adequate quality images to assess for obstetrical anomalies in pregnant patients as compared to professional sonographers. This outcome was determined by comparing image quality from student scans compared to sonographer scans. Images included all findings required by the ROUTE criteria. A secondary outcome was to determine if minimally trained first-year medical students were able to identify specific obstetric pathology that could be validated by review of a board certified Obstetrician and Gynecologist.
RESULTS
A total of 60 women were enrolled in the study. Patient demographics can be seen in Table 1. First-year medical students were able to correctly identify fetal presentation, fetal number, and placental position in all 60 patients. No patients were found to have oligohydramnios or polyhydramnios. Four patients were found to have abnormal pregnancy evaluations based on initial ROUTE screening exam. Patient 2 (Table 1) was found to have a previously unknown breech fetal lie at 39 weeks and 4 days, an abnormal finding since vaginal breech delivery is associated with a significant increase in neonatal mortality or short-term serious neonatal morbidity as compared to cesarean delivery of a breech fetus.[11] Patient 11 (Figure 1) was found to have a previously undiagnosed low lying placenta (defined as <2 cm from the internal os) first noted at an advanced gestational age of 33 weeks with the placenta measuring 0.76 cm from the internal os. Patient 23 presented with an estimated GA of 27 weeks based on LMP but was found to have an estimated GA of 19w6d based on HC and BPD. Patient 35 was also found to have a low-lying placenta noted at a gestational age of 28 weeks, 3 days. All 4 patients with abnormal findings had imaging that was repeated and confirmed by the treating physician. Images were also confirmed by the blinded Obstetrics and Gynecology physician.
Table 1.
Complete patient demographics
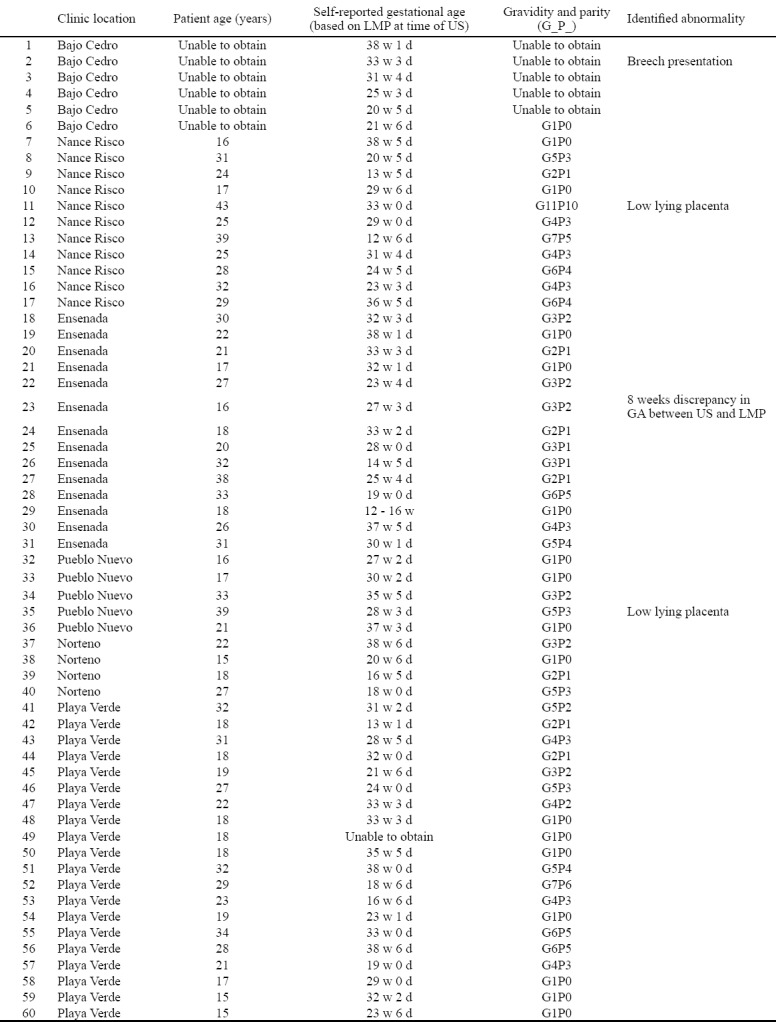
Figure 1.

Low lying placenta (placenta measuring less than 2 cm away from the internal os).
On average, participants correctly assessed BPD 95.3% (n=43) of the time and HC 90.0% (n=40) of the time (<7% error) when retrospectively reviewed by a board-certified Obstetrics and Gynecologic physician reviewing images. Additionally, the participant determined gestational age based on BPD or HC measurements had a mean difference from professional ultrasonographers of -1.5 days ± 2 days (95% confidence interval, σ=6.3) and 0.26 days ± 2 days (95% confidence interval, σ=7.4), respectively (Figures 2 and 3).
Figure 2.
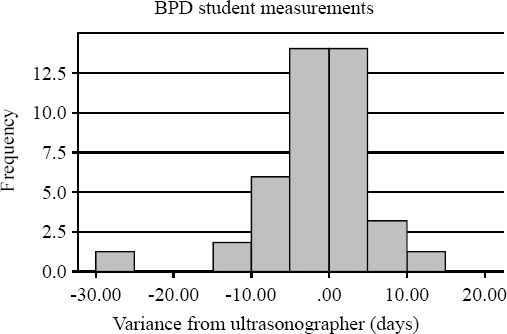
Accuracy of student BPD measurements when compared to professional sonographers at UCI CFE.
Figure 3.
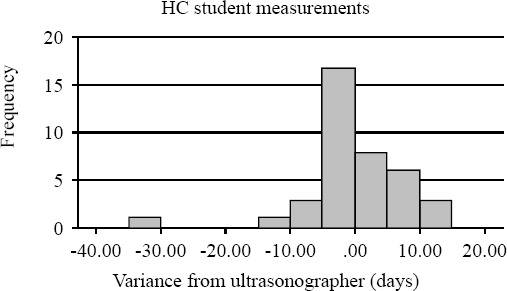
Accuracy of student HC measurements when compared to professional sonographers at UCI CFE.
DISCUSSION
According to our data, first-year medical students can successfully perform and interpret ROUTE on second and third trimester pregnant patients after additional ultrasound training sessions. Our study indicates that ultrasound triage exams such as the ROUTE can be used to screen for high-risk conditions in pregnant women in resource-limited settings. Additionally, the identification of such conditions can allow women in these areas to obtain further care as needed. The combination of geographic isolation, minimal resources, and absence of consistent health care has created an environment for point-of-care ultrasound (POCUS) to play a role in the care of obstetric patients. Given the potential for improved patient outcomes and decreased morbidity and mortality, implementing a ROUTE training program to permanent healthcare workers in rural Panama could potentially help reduce the prevalence of pregnancy related morbidity and mortality in that region.
Moreover, implementation of the ROUTE could potentially prove useful in detection of possible microcephaly. Since 2015, Zika virus has spread rapidly throughout the Americas, including Panama. Zika virus during pregnancy has been associated with a higher likelihood of neurological adverse birth defects, particularly a 50 times greater likelihood of developing microcephaly.[12] Given the accuracy of minimally trained medical students in determining obstetric measurements such as biparietal diameter and head circumference, it may be possible to train first year medical students and other health care providers to detect abnormalities such as microcephaly, which is defined as having an abnormally small head circumference with respect to fetal gestational age. One patient in this study (Patient 23, Table 1) was found to have an infant measuring 8 weeks behind the expected age based on her LMP. Although this could be due to the patient having incorrect dating based on her LMP, this discrepancy could also identify a high-risk pregnancy such as intrauterine growth restriction which would require closer monitoring. This woman was thus referred for additional testing and a higher level of obstetrical care. Thus, in a similar fashion, health care providers could potentially use the ROUTE to identify patients with potentially high-risk conditions who need more sophisticated obstetrical care earlier on in their pregnancy.
In addition to the improved outcomes based on POCUS and ROUTE, incorporating education in addition to ROUTE screening may also improve maternal and fetal health outcomes. Of the 60 total women enrolled in this study, only 25 were taking prenatal vitamins, many of who were not taking them daily or started them after their first trimester. Panama suffers from 25.1 neural tube defects (NTDs) per 10,000 births[13] and Panamanian women scored lower than Costa Rican women in most domains of knowledge regarding prenatal healthcare,[14] thus demonstrating the need to improve the antepartum care in Panamanian women. While religious and cultural beliefs may play a role in such decisions, a lack of education and access to contraceptives or prenatal vitamins is likely to be the primary barrier to adequate family planning and prenatal care.
Limitations
There are several limitations to this study. Patients enrolled in the study were done so in a convenience fashion. It is possible that patients enrolled in the study are not representative of all patients in Panama. Additionally, enrollment took place at a single site and the findings of patients in Bocas del Toro may not be applicable to other patients. The ultrasound skills of the medical students used in the study may not be applicable to all medical students. The amount of training required for proficiency was not assessed in this study. Future studies are needed to determine the minimum amount of training required for a practitioner to perform and interpret the ROUTE exam.
CONCLUSIONS
Ultimately, improved fetal outcomes and health care delivery depends on multiple factors. Our study has demonstrated that with minimal training, first-year medical students are able to perform and interpret the ROUTE on second and third trimester pregnant patients in rural Panama. These results demonstrate a need both for better obstetrical care, which may be accomplished by bedside ultrasound, and for local sustainability and education. Ultimately, future large-scale studies will be required in order to determine if permanent rural healthcare workers are able to adopt the ROUTE into the care they provide in order to improve the outcomes of obstetric patients in rural settings.
ACKNOWLEDGEMENTS
The authors would like to thank Floating Doctors for their compassionate care for patients in rural communities. Data was collected in collaboration with free clinics organized and supported by Floating Doctors.
Footnotes
Funding: None.
Ethical approval: The study was approved by the domestic site Institutional Review Board.
Conflicts of interest: Dr. J Christian Fox receives stock options from Sonosim for consulting. However, no Sonosim products were used in this research project.
Contributors: AV proposed the study and wrote the first draft. All authors read and approved the final version of the paper.
REFERENCES
- 1.Maternal mortality [Internet] World Health Organization. World Health Organization. Available from: http://www.who.int/mediacentre/factsheets/fs348/en/
- 2.Goodrich L, Matsuo M, Gottlieb J. Needs Assessment and Prenatal Education Program for Local Midwives of the Ngöbe Population of Panama. Journal of Global Health Perspectives [Google Scholar]
- 3.United Nations Population Fund (UNFPA) Risking death to give life in Panama's tropical forests:Maternal health among the Ngöbe people. 2007. Available: http://www.unfpa.org/news/risking-death-give-life-panamas-tropical-forests .
- 4.Holtz C. Global health care:issues and policies. Sudbury, MA: Jones and Bartlett Publishers; 2008. [Google Scholar]
- 5.Harris RD, Marks WM. Compact ultrasound for improving maternal and perinatal care in low-resource settings:review of the potential benefits, implementation challenges, and public health issues. J Ultrasound Med. 2009;28(8):1067–76. doi: 10.7863/jum.2009.28.8.1067. [DOI] [PubMed] [Google Scholar]
- 6.Adler D, Mgalula K, Price D, Taylor O. Introduction of a portable ultrasound unit into the health services of the Lugufu refugee camp, Kigoma District, Tanzania. Int J Emerg Med. 2008;1(4):261–6. doi: 10.1007/s12245-008-0074-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rooney KP, Lahham S, Lahham S, Anderson CL, Bledsoe B, Sloane B, et al. Pre-hospital assessment with ultrasound in emergencies:implementation in the field. World J Emerg Med. 2016;7(2):117–23. doi: 10.5847/wjem.j.1920-8642.2016.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kimberly HH, Murray A, Mennicke M, Liteplo A, Lew J, Bohan JS, et al. Focused maternal ultrasound by midwives in rural Zambia. Ultrasound Med Biol. 2010;36(8):1267–72. doi: 10.1016/j.ultrasmedbio.2010.05.017. [DOI] [PubMed] [Google Scholar]
- 9.Steller JG, Sims L, Fox JC, Toohey J, Major C, Speir VL. The rural obstetrical ultrasound triage exam:teaching ultrasonography to students interested in global health. Obstetrics & Gynecology. 2014;123:119S. [Google Scholar]
- 10.Sanchez O, Baker J, Vaughan J, Toohey JS. The rural obstetrical ultrasound triage exam (ROUTE):teaching health care workers in international settings [392] Obstetrics & Gynecology. 2015;125:122S. [Google Scholar]
- 11.Ghosh MK. Breech presentation:evolution of management. J Reprod Med. 2005;50(2):108–16. [PubMed] [Google Scholar]
- 12.Rasmussen SA, Jamieson DJ, Honein MA, Petersen LR. Zika virus and birth defects—reviewing the evidence for causality. N Engl J Med. 2016;2016(374):1981–7. doi: 10.1056/NEJMsr1604338. [DOI] [PubMed] [Google Scholar]
- 13.Lo A, Polšek D, Sidhu S. Estimating the burden of neural tube defects in low–and middle–income countries. J Glob Health. 2014;4(1):010402. doi: 10.7189/jogh.04.010402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guilford WH, Downs KE, Royce TJ. Knowledge of prenatal health care among Costa Rican and Panamanian women. Rev Panam Salud Publica. 2008;23(6):369–76. doi: 10.1590/s1020-49892008000600001. [DOI] [PubMed] [Google Scholar]


