Abstract
The current study examined the cumulative risk, age of initiation, and functional impairments among adults with substance use problems (N = 1748) by child abuse status. Child abuse was associated with earlier initiation of marijuana, cocaine, and heroin use, and had greater risks for all the drugs studied (hazard ratios, 1.7–3.2). Furthermore, child abuse was associated with increased medical and functional impairments, including ER visits, health problems, drug dealing, drug dependence, and drug cravings. Provision of social services and parenting education during the perinatal period may prevent the long-term impact of child abuse on substance use and related impairments. The study’s limitations are noted.
Keywords: child abuse, craving, parenting skills, risk
INTRODUCTION
A large body of research has demonstrated that child–parent conflict (MacMillan, Niec, & Offord, 1995; McCord, 1982; Dahlberg, 1998), influence of delinquent peers (Thornberry, Krohn, Lizotte, & Chard-Wierschem, 1993), poverty, neighborhood impoverishment (Freisthler, Merritt, & LaScala, 2006; Leventhal & Brooks-Gunn, 2000; Sampson, Morenoff, & Gannon-Rowley, 2002), and child abuse are associated with an increased risk1 for substance use (Dube et al., 2001; Debellis, 2000; Moran, Vuchinich, & Hall, 2004; Simpson & Miller, 2002) and earlier initiation of use (Hyman, Garcia, & Sinha, 2006; Kilpatrick et al., 2000; Kingston & Raghavan, 2009).
Among these risk factors, a history of child abuse has been found to be a robust predictor of substance use, and has been linked to increased use of medical and psychiatric services later in life (Green, Flowe-Valencia, Rosenblum, & Tair, 1999; Newman et al., 2000; Salmon & Calderbank, 1996; Walker et al., 1999). While a large number of studies have established a link between child abuse and future substance use, to date, several issues remain unresolved. First, little is known about the risk for substance use among abused individuals in the general population because the majority of the studies used clinically referred adults who were sexually or physically abused as children (Lo & Cheng, 2007; Wall & Kohl, 2007). Except for a few prospective studies (Cohen, Brown, & Smailes, 2001; Fergusson, Boden, & Horwood, 2008; Horwitz, Widom, McLaughlin, & White, 2001; Lansford et al., 2002; Widom, Marmorstein, & White, 2006; Wilson & Windom, 2009), the majority of studies examined cross-sectional associations between substance use and a history of sexual abuse in girls and physical abuse in boys. Second, although a few studies have found that child abuse was associated with early onset of substance abuse2 (Cervantes, Duenas, Valdez, & Kaplan, 2006; Hyman et al., 2006; Kilpatrick et al., 2000), their findings are limited since they only compare the endpoint, that is, mean ages at first initiation of substance use for abused and non-abused children, even if in one study severity of substance use was additionally assessed (Hyman et al., 2006). However, assessing the trajectory of initiation and evaluating cumulative risk over time from childhood to adulthood is lacking. Third, there still is a need to examine the child’s behavioral and temperamental characteristics that may make parenting more challenging, especially for parents who lack adequate financial and emotional resources (Brown, Cohen, Johnson, & Salzinger, 1998; O’Connor, 2002). It is possible that the association between child abuse and subsequent substance use is accounted by one or more correlated environmental risks (Gilbert et al., 2009) (e.g., poverty) or behavioral problems (e.g., childhood behavioral and conduct problems) or familial risk (parental substance use), and therefore it is important to rule out possible spurious relationships between child abuse and subsequent increased risk for substance use.
The main goal of this study was to examine the long-term effects of child abuse on the use of various substances during a period of transition between adolescence and adulthood, using data from a randomly sampled, regionally representative community-based study (N = 1,748) that followed children from birth to over 30 years of age. We compared the cumulative risk for substance use with and without child abuse among male and female individuals. We hypothesized that individuals who were abused during childhood, compared to those were not would have:
an elevated risk for substance use in both male and female cohorts;
elevated cumulative risks and earlier age of initiation for substance use; and
an elevated risk for health care utilization and higher prevalence of problems in functioning and relationships due to substance use.
The effects of potential confounders, including demographic and childhood characteristics (see detail in the method section), were controlled for in all analyses.
METHODS
Population
The Johns Hopkins Collaborative Perinatal Study consists of data collected from pregnant women who received prenatal care and delivered their babies at Johns Hopkins Hospital between January 1, 1960, and December 31, 1964. Infants were continuously followed until 8 years of age. The participation rates varied between 90% during the first years to 88% at ages 7 and 8. Between January 1, 1992, and December 31, 1994, the adult follow-up study, Pathway to Adulthood Study, bridged the period from 7–8 to 27–33 years of age (PIs: J. Hardy & S. Shapiro). The follow-up study participants were randomly selected from the original 2,694 second generation participants who had received the 7-year psychological and/or 8-year language, hearing and speech assessment (all but a few, <1.0%, received both). The interviews were, for the most part, conducted face-to-face (70%). When the respondent lived beyond the greater Baltimore area or refused a personal interview, it was conducted by telephone. A random 10% of all interviews were verified with a brief telephone interview within 10–14 days to maintain the data accuracy (Fan & Eaton, 2001; Hardy, Astone, Brooks-Gunn, & Shapiro, 1998; Hardy et al., 1997).
Of the 2,694 offspring eligible for a follow-up, 2,220 (82%) were located and 1,758 completed interviews (71.4% response rate for known outcomes and 65.3% completed the full interview). Those who were located, but did not complete full interviews, had mothers with characteristics generally similar to those who were interviewed. An additional 10 offspring were excluded from this study due to missing information on substance use, leaving us 1,748 offspring in the current study.
Analyses of demographic differences among the 1,748 offspring who were included and the remaining 946 who were eligible for follow-up but excluded revealed no differences in race (81.8% blacks vs. 81.9%), number of siblings (3.2 vs. 3.3), maternal monthly income during pregnancy ($1,028 vs. $993), and maternal age at birth (25.0 vs. 24.5). Furthermore, there was no difference on any of the childhood behavioral characteristics, including frustration tolerance, attention span, impulsivity, and activity level. However, the included offspring were more likely to be female than the excluded (54.1% vs. 41.3%, p < .0001).
Measures
Substance Use
Data were derived from respondents’ answers to questions from the National Survey of Drug Abuse (Abelson, Fishburne, & Cisin, 1979) used in the Pathway to Adulthood Study, described in detail elsewhere (Hardy et al., 1997). In brief, participants’ substance use has been ascertained through a face-to-face interview at adult follow-up assessment phase when the participants were between 27 and 33 years old. This study provides a large sample size and multiple indicators of childhood poverty and behavioral characteristics. Intensive assessment of use of various substances was undertaken, including (1) health care utilization due to substance use; (2) problems as a result of substance use; (3) current (last week, last month, and recent) substance use, such as marijuana, cocaine, heroin, methadone, opiate, and glue, gasoline, or poppers; (4) age of initiation for each substance used; and (5) life-time history of each substance used.
Child Abuse
Child abuse history was obtained retrospectively through face-to-face interviews from the adult participants by trained researchers using the Conflict Tactics Scale (CTS) (Straus, 1979). The CTS is a 19-item measure, rated on a 5-point Likert scale (Straus, 1990; Straus, Hamby, Finkelhor, Moor, & Runyan, 1998) that assesses intrafamilial violence, including physical and verbal violence. The CTS has good reliability (ranging 0.78–0.96, in this study Cronbach’s Alpha = 0.82) (Amato, 1991; Cervantes et al., 2006; Schumm, Martin, Bollman, & Jurich, 1982; Straus, 1990; Yodanis, Hill, & Straus, 1997) and validity (concurrent and construct) to detect intrafamilial violence (Cervantes et al., 2006; Straus, 1990; Straus et al., 1998). The mean (SD) total score in our sample was 19.07 (12.88). Mean score plus one standard deviation (31.96) was the cut-off used to create a dichotomous abuse variable with 1 representing a high level of exposure to child abuse (Nomura & Chemtob, 2007). The 15.5% of the sample fell in this category. Throughout this paper, a high-level of exposure to child abuse will be referred to as “child abuse.”
Potential Confounders
Socio-demographic characteristics associated with substance use were measured and included in the analyses as potential confounders, namely, age at last interview, gender, race (white vs. nonwhite), poverty level (below and above the poverty line) at birth and at age 7, number of siblings in the family, mother’s mental health status, including substance use and alcoholism, and mother’s education at the time of the birth of the child. We also considered childhood behavioral characteristics measured by research child psychologists at age 7, including frustration tolerance, hyperactivity, short attention span, and impulsivity as potential confounders. Except for Cox proportional hazards regression and survival analysis, age at the last interview was not included in our model for statistical adjustment because those statistical methodologies take age (or follow-up time) into account. When we evaluated the gender specific effect, we excluded gender from the set of potential confounders.
Statistical Analysis
Preliminary analyses of group differences in the mean values for continuous outcomes by child abuse (high and low) were tested by t-tests, and categorical outcomes were compared by the X2-test. In order to control for the potential confounding effects in the analysis, the following approaches were used. Cross-sectional categorical outcomes (e.g., health care utilization) were analyzed using logistic regression. Continuous outcomes were analyzed using linear analysis of covariance (ANCOVA) with child outcomes such as number of different substances used as the dependent variables and child abuse as the predictor variable.
Further, survival analysis techniques adjusting for correlated survival times were used to estimate (1) the age-specific incidence rates and (2) cumulative lifetime rates of each of the six substances used including marijuana, cocaine, heroin, methadone, opiate, and glue, gasoline and poppers use, by child abuse status, using a modified Kaplan–Meier method (Williams, 1995). In order to estimate the relative risks of substance use by child abuse status, Cox proportional hazards regression models (Cox, 1972), modified to adjust for cluster data (Binder 1992), were performed while controlling for potential confounders. To evaluate the strength of the difference in the survival curves between individuals who were abused and those who were not abused, X2 value was estimated using the Wilcoxon test. To explore whether the cumulative risk and patterns of incidence across time differed between individuals with and without a history of abuse as a function of gender, the same set of Cox proportional hazards regression models was repeated with gender and the interaction between abuse status and gender.
To avoid Type I errors due to multiple testing, the level of significance was adjusted using Holm’s correction (Holm, 1979). Furthermore, the generalized estimating equations (GEE) were used to account for potential nonindependence of outcomes for children from the same family (Liang & Zeger, 1986).
RESULTS
Subjects
Table 1 shows the characteristics of our sample by child abuse status. At the 30-year follow-up assessment in adulthood, subjects with and without a child abuse history did not differ by maternal or family characteristics, including mother’s marital status, mother’s educational attainment, mother’s lifetime history of mental health status, and poverty status at birth. Nor were there differences in most offspring demographics characteristics. Notable demographic differences between offspring with and without child abuse include race, childhood poverty status at age 7, and offspring’s educational attainment by the time of the adult follow-up. Compared to those not abused, a greater proportion of offspring abused in childhood were White (28.9% vs. 16.3%, p < .0001), lived under the poverty line at age 7 (40.7% vs. 28.8%, p = .0001), and had attained fewer years of education at the follow-up interview (11.3 vs. 12.4 years, p < .0001). With regards to offspring childhood behavioral characteristics there were significant differences in frustration tolerance ( p < .0001) and impulsivity ( p = .04), but not in attention span or activity level between the abused and the nonabused individuals at age 7.
TABLE 1.
Characteristics in mothers and their offspring with and without child abuse
| Variable | Total (n = 1748) | Child abuse no (n = 1478) | Child abuse yes (n = 270) | Statistics |
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | ||
| Offspring educational attainment (years) | 12.22 (2.14) | 12.30 (2.14) | 11.39 (2.27) | F1,1744 = 40.89, p < .0001 |
| Offspring age at the last interviewed | 30.28 (1.53) | 30.28 (1.53) | 30.25 (1.58) | F1,1746 = .10, p = .75 |
| Number of sibling (maternal parity) | 3.25 (2.32) | 3.29 (2.31) | 3.04 (2.37) | F1,1734 = 2.80, p = .09 |
| N (%) | N (%) | N (%) | ||
| Poverty at birth (below a poverty line) | 750 (42.9) | 634 (42.9) | 116 (43.0) | X2(2) = 0.1, p = .98 |
| Poverty at 7 (below a poverty line) | 536 (30.7) | 426 (28.8) | 110 (40.7) | X2(2) = 15.3, p = .0001 |
| Mother’s marital status | ||||
| Never married | 394 (23.1) | 341 (23.7) | 53 (20.0) | X2(2) = 3.2, p = .21 |
| Married | 1, 175 (68.9) | 990 (68.7) | 185 (69.8) | |
| Formally married | 137 (8.0) | 110 (7.6) | 27 (10.2) | |
| Mother’s educational attainment | ||||
| <8 grades | 246 (14.4) | 200 (13.8) | 46 (17.4) | X2(5) = 9.4, p = .09 |
| 8 grades | 247 (14.4) | 204 (14.1) | 43 (16.2) | |
| Some high school | 734 (42.9) | 613 (42.4) | 121 (45.7) | |
| High school | 363 (21.2) | 322 (22.3) | 41 (15.5) | |
| Some college | 108 (6.3) | 95 (6.6) | 13 (4.9) | |
| 4-year college | 12 (0.7) | 11 (0.8) | 1 (0.4) | |
| Mother’s lifetime history of mental illness | 38 (2.9) | 20 (2.4) | 5 (3.1) | X2(1) = 0.31, p = .58 |
| Race | ||||
| White | 319 (18.2) | 241 (16.3) | 78 (28.9) | X2(1) = 24.2, p < .0001 |
| Black | 1, 429 (81.8) | 1, 237 (83.7) | 192 (71.1) | |
| Gender | ||||
| Male | 801 (45.8) | 673 (45.5) | 128 (47.4) | X2(1) = 0.32, p = .57 |
| Female | 947 (54.2) | 805 (54.5) | 142 (52.6) | |
| Offspring frustration tolerance at age 7a | ||||
| Withdraws completely | 6 (0.3) | 3 (0.2) | 3 (1.1) | X2(4) = 20.9, p < .0001 |
| Occasionally withdraws | 368 (21.1) | 323 (21.9) | 45 (16.8) | |
| Attempts to cope | 1, 351 (77.6) | 1, 138 (77.3) | 213 (79.5) | |
| Becomes quite upset | 12 (0.7) | 7 (0.5) | 5 (1.9) | |
| Extreme acting-out | 3 (0.2) | 1 (0.1) | 2 (0.7) | |
| Offspring attention span at age 7a | ||||
| Very brief | 18 (1.0) | 15 (1.0) | 3 (1.1) | X2(4) = 3.4, p = .50 |
| Short | 188 (10.8) | 152 (10.3) | 36 (13.4) | |
| Adequate | 1, 415 (81.4) | 1, 202 (81.8) | 213 (79.5) | |
| More than average | 114 (6.6) | 99 (6.7) | 15 (5.6) | |
| Highly preservative | 3 (0.2) | 2 (0.1) | 1 (0.4) | |
| Offspring activity level at age 7a | ||||
| Extremely inactive | 7 (0.4) | 6 (0.4) | 1 (0.4) | X2(4) = 2.8, p = .58 |
| Little inactive | 299 (17.2) | 258 (17.5) | 41 (15.3) | |
| Normal amount | 1, 262 (72.5) | 1, 069 (72.6) | 193 (72.0) | |
| Unusual amount | 158 (9.l) | 127 (8.6) | 31 (11.6) | |
| Extremely over-active | 14 (0.8) | 12 (0.8) | 2 (0.7) | |
| Offspring impulsivity at age 7a | ||||
| Extremely rigid | 3 (0.2) | 3 (0.2) | 0 (0) | X2(4) = 10.0, p = .04 |
| Some rigid | 83 (4.8) | 70 (4.8) | 13 (4.9) | |
| Flexible | 1, 559 (89.6) | 1, 322 (89.8) | 237 (88.4) | |
| Frequently impulsive | 88 (5.1) | 74 (5.0) | 14 (5.2) | |
| Extremely impulsive | 7 (0.4) | 3 (0.2) | 4 (1.5) |
Behavioral characteristics among offspring were evaluated by a trained child psychologist at age 7.
Rates of Substance Use in Past Week, Past Month, and Past Year
Table 2 shows the rate of current substance use in adulthood (past week, past month, and past year). In the past week category, a little over 10% of the cohort with a history of child abuse, as compared to about 4% of those without, used marijuana (AOR = 2.5, p = .0004). Approximately 4% of those with a history of child abuse, as compared to about 1% of those without, used cocaine (AOR = 3.0, p = .008). The one-week period prevalence for heroin use among those with a history of child abuse was higher than among those without (2.6% vs. 1.3%) but the difference was not statistically significant. The prevalence rates for methadone, opiate, and glue use were too low to estimate risk.
TABLE 2.
Rate (per 100) of substance use during (A) past week, (B) past month, and (C) past year among offspring with and without childhood abuse
| (N = 1748) | Adults without child abuse (n = 1478) | Adults with child abuse (n = 270) | ||||
|---|---|---|---|---|---|---|
| (A) Substance use in past week | % (N) | % (N) | OR (95% CI) | p | AORa (95% CI) | p |
| Marijuana use | 3.9 (58) | 10.7 (29) | 2.9 (1.8–4.7) | <.00001 | 2.5 (1.5–4.3) | .0004 |
| Cocaine use | 1.4 (22) | 4.4 (12) | 3.1 (1.5–6.3) | .001 | 3.0 (1.3–6.8) | .008 |
| Heroine use | 1.3 (19) | 2.6 (7) | 2.0 (0.9–4.9) | .10 | 2.0 (0.7–5.4) | .20 |
| Methadone use | 0.2 (3) | 0 | – | – | ||
| Opiate use | 0 | 0.1 (1) | – | – | ||
| (B) Substance use in past month | % (N) | % (N) | OR (95% CI) | p | AORa (95% CI) | p |
| Marijuana use | 6.2 (92) | 14.4 (39) | 2.5 (1.7–3.8) | <.00001 | 2.5 (1.7–3.9) | <.00001 |
| Cocaine use | 3.1 (46) | 7.7 (21) | 2.6 (1.5–4.3) | <.00001 | 3.1 (1.8–5.4) | .0004 |
| Heroine use | 2.2 (32) | 4.8 (13) | 2.3 (1.2–4.4) | .01 | 2.9 (1.5–5.6) | .002 |
| Methadone use | 0.3 (3) | 0.4 (1) | 1.8 (0.2–17.6) | .60 | – | |
| Opiate use | 0.001 (1) | 0.4 (1) | 5.5 (0.3–88.0) | .29 | 4.7 (0.3–78.2) | .28 |
| (C) Substance use in past year | % (N) | % (N) | OR (95% CI) | p | AORa (95% CI) | p |
| Marijuana use | 12.7 (188) | 24.7 (67) | 2.2 (1.7–3.1) | <.00001 | 2.2 (1.6–3.1) | <.00001 |
| Cocaine use | 5.7 (85) | 13.3 (36) | 2.5 (1.4–3.8) | <.00001 | 2.7 (1.8–4.1) | <.00001 |
| Heroine use | 5.5 (81) | 11.8 (32) | 2.3 (1.5–3.6) | <.00001 | 2.8 (1.8–4.3) | <.00001 |
| Methadone use | 0.5 (7) | 1.1 (3) | 2.4 (0.6–9.2) | .20 | 2.5 (0.6–9.9) | .18 |
| Opiate use | 0.7 (10) | 2.6 (7) | 3.9 (1.5–10.4) | .003 | 3.5 (1.3–9.4) | .008 |
OR = odds ratio; CI = confidence interval; AOR = adjusted odds ratio.
N may vary slightly due to missing value.
Age, race, sex, and poverty level at birth and at age 7, maternal lifetime history of mental health, maternal education level, number of siblings, and childhood behavioral problems (activity level, low attention span, impulsivity, and low frustration tolerance) were adjusted. Holms correction for multiple testing has been used and the p-value for significance is set for .008.
As expected, the one-month prevalence rates for the six categories of substance use in the past month were slightly higher, but the patterns of risk for marijuana (14.4% vs. 6.2%, AOR = 2.5, p < .00001), cocaine (7.7% vs. 3.1%, AOR = 3.1, p = .0004), and heroine (4.8% vs. 2.2%, AOR = 2.9, p = .002) use between the cohorts with and without child abuse were the same, the individuals with child abuse having a significantly higher rate of substance use than those without. Similarly, in the past year, the cohort with child abuse, as compared to that without, had a higher rate of substance use, including marijuana (24.7% vs 12.7%, AOR = 2.2, p < .00001), cocaine (13.3% vs. 5.7%, AOR = 2.7, p <.00001), heroin (11.8% vs. 5.5%, AOR = 2.8, p < .00001), and opiate (2.6% vs. 0.7%, AOR =3.5, p = .008).
Rates and Cumulative Risk of Lifetime Substance Use Between Persons With and Without Child Abuse
Table 3 shows that lifetime prevalence rates for the use of six different substances in the entire sample and by gender of study participants. The most prevalent substance used was marijuana both in offspring with (77.9%) and without (60.8%) child abuse, and the same pattern (i.e., higher rates of use among those abused) was evident among males and females. The least common substance used among male participants was methadone (8% and 2% of abused and nonabused, respectively), and among females glue, gasoline, and poppers (3% and 1% of abused and nonabused, respectively).
TABLE 3.
Cumulative rates (per 100) of substance use over 30-year follow-up among offspring with and without childhood abuse
| Lifetime substance use | ||||||
|---|---|---|---|---|---|---|
|
| ||||||
| Total sample (N = 1748) |
No childhood abuse (N = 1478) % (95% CI) |
Childhood abuse (N = 270) % (95% CI) |
RRa (95% CI) | p-value | ARRa (95% CI) | p-value |
| Marijuana | 60.8 (58.2–63.2) | 77.9 (72.7–82.7) | 1.6 (1.4–1.9) | <.00001 | 1.7 (1.3–1.8) | <.00001 |
| Cocaine | 26.0 (23.8–28.3) | 46.9 (40.5–52.5) | 2.2 (1.8–2.8) | <.00001 | 2.1 (1.7–2.6) | <.00001 |
| Heroin | 13.1 (11.4–14.8) | 25.2 (19.7–30.1) | 2.1 (1.5–2.7) | <.00001 | 2.2 (1.6–2.9) | <.00001 |
| Methadone | 2.2 (1.5–3.0) | 5.6 (2.8–8.3) | 2.7 (1.4–5.0) | .003 | 2.6 (1.4–4.9) | .004 |
| Opiate | 5.1 (3.9–6.2) | 12.5 (8.3–15.2) | 2.6 (1.5–3.5) | <.00001 | 2.4 (1.6–3.7) | <.00001 |
| Glue, gasoline, poppers use | 2.5 (1.7–3.3) | 8.1 (4.8–11.5) | 3.4 (2.0–5.9) | <.00001 | 3.2 (1.8–5.5) | .00001 |
| Male offspring (N = 801) | (N = 673) % (95% CI) |
(N = 128) % (95% CI) |
RRa (95% CI) | p-value | ARRa (95% CI) | p-value |
| Marijuana | 70.0 (66.5–73.4) | 86.7 (80.8–92.7) | 1.9 (1.5–2.2) | <.00001 | 1.7 (1.4–2.2) | <.00001 |
| Cocaine | 35.4 (31.7–39.0) | 58.6 (49.9–67.2) | 2.3 (1.8–3.0) | <.00001 | 2.2 (1.7–2.9) | <.00001 |
| Heroin | 20.4 (17.3–23.3) | 36.7 (28.3–45.2) | 2.1 (1.4–2.9) | <.00001 | 2.1 (1.5–2.9) | <.00001 |
| Methadone | 2.4 (1.2–3.5) | 7.8 (3.15–12.5) | 4.0 (1.8–9.1) | .001 | 3.7 (1.6–8.4) | .002 |
| Opiate | 7.8 (5.8 – 9.9) | 17.1 (10.6–23.8) | 2.5 (1.5–4.1) | .00004 | 2.2 (1.3–3.8) | .003 |
| Glue, gasoline, poppers use | 4.7 (3.1–6.3) | 14.0 (8.0–20.7) | 3.3 (1.8–6.0) | <.00001 | 3.2 (1.8–5.9) | .00002 |
| Female offspring (N = 947) | (N = 805) % (95% CI) |
(N = 142) % (95% CI) |
RRa (95% CI) | p-value | ARRa (95% CI) | p-value |
| Marijuana | 53.0 (49.5–56.4) | 69.7 (61.8–77.2) | 1.5 (1.2–1.9) | .00002 | 1.4 (1.1–1.8) | .002 |
| Cocaine | 18.1 (15.4–20.8) | 35.9 (27.5–43.4) | 2.2 (1.6–3.0) | <.00001 | 2.0 (1.4–2.9) | <.00001 |
| Heroin | 6.9 (5.2–8.7) | 14.8 (8.3–20.3) | 2.3 (1.4–3.9) | .002 | 2.4 (1.4–4.1) | .001 |
| Methadone | 2.0 (1.0–3.0) | 3.5 (0.5–6.6) | 1.7 (0.6–4.7) | .28 | 1.8 (0.6–5.1) | .29 |
| Opiate | 2.7 (1.6–3.9) | 8.5 (3.3–12.3) | 3.0 (1.5–6.2) | .003 | 3.2 (1.5–6.9) | .003 |
| Glue, gasoline, poppers use | 0.6 (0.1–1.2) | 2.8 (0.6 – 5.6) | 5.6 (1.2–17.1) | .02 | 3.4 (1.0–14.3) | .05 |
Cox proportional hazards model was used awithout any confounders and bwith age, race, poverty level at birth, poverty level at age 7, maternal lifetime history of mental health, maternal education, number of siblings, and child behavioral characteristics (activity level, low attention span, impulsivity, and low frustration tolerance) at age 7 were included in the model for statistical adjustment. CI = confidence interval. RR = relative risk. ARR = adjusted relative risk. Holms correction for multiple testing has been used and the p-value for significance is set for .008.
We estimated the lifetime relative risk (hazard ratio) of substance use based on the age of first onset and the duration of the follow-up time, separately for each substance, among those with an abuse relative to those without, after controlling for potential confounders (Table 3 right two columns). Relative to persons who had not been abused, abused individuals were at an approximately three-fold increased risk for glue, gasoline, and poppers use (adjusted relative risk, ARR = 3.2, p = .00001), over two-fold increased lifetime risk for methadone (ARR = 2.6, p = .004), opiate (ARR = 2.4, p < .00001), heroin (ARR = 2.2, p < .00001), and cocaine (ARR = 2.1, p < .00001), and a slightly less than two-fold increased risk for marijuana use (ARR = 1.7, p < .00001). An examination of the cumulative risks by gender shows that, except for methadone, abused males and females were at a significantly increased risk for substance use compared to those nonabused.
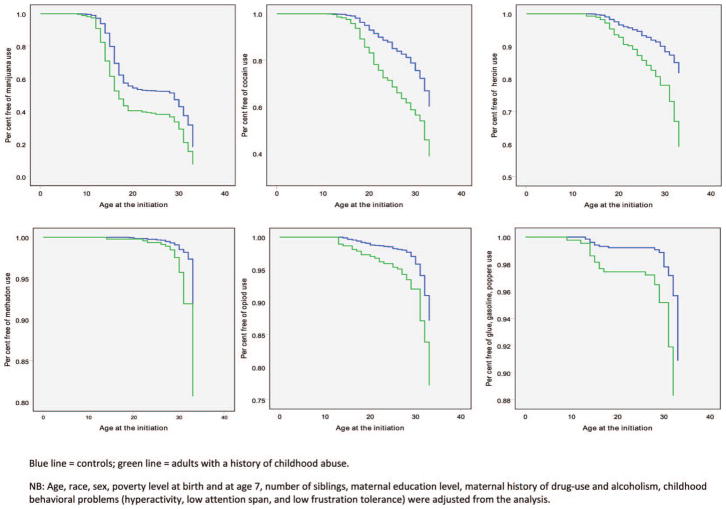
Figure 1 shows panels of the survival curves for six different substances (marijuana, cocaine, heroin, methadone, opiate, and glue, gasoline, and poppers use) between the two groups of individuals with and without a history of child abuse. Survival curves were drawn based on one (100%) minus the rate of each substance use a person initiates (age at the first onset) by child abuse status and gender. With regard to marijuana use, our abused cohort had an earlier initiation, and the difference in the risk grew wider to approximately age 19. The survival curves for the two abused groups differed significantly (X2 = 64.3, df = 1, p < .00001). Opiate (X2 = 10.7, df = 1, p = .001) and glue users (X2 = 16.2, p = .00006) manifested patterns similar to marijuana users. Individuals who had been abused reported an earlier initiation of cocaine and heroin use, and the difference in the risk grew wider as the cohort aged. There was no significant difference between the two groups for methadone use (X2 = 2.5, p = .10).
FIGURE 1.
Survival curves for marijuana use, cocaine use, heroin use, methadone use, use, and glue, gasoline, and poppers use among adults with and without a history of childhood abuse.
While males, relative to females, had a greater cumulative risk for marijuana, cocaine, heroin, opiate, and glue, gasoline, and poppers use, the risk for the use of those substances in our cohort did not differ by gender for those people who had been abused, relative to those notabused individuals, as evidenced by the nonsignificant abuse and gender interaction (data not shown). There was no notable increase in the risk for methadone use for females.
Health Care Utilization and Problems Due to Substance use
Table 4 shows that subjects with a history of child abuse, relative to those without, were twice as likely to have a lifetime history of substance use-related emergency room (ER) use (AOR = 2.9, p = .001), and of having been admitted to an in-patient unit for substance “abuse” (AOR = 2.0, p = .05). Furthermore, those people who had reported a history of child abuse, relative to those without, were about 2 to 3 times more likely to have health problems related to substance use (AOR = 2.4, p = .003), problems with family, friends or police officers, on the job, or at school (AOR = 3.2, p < .00001), psychological problems such as feeling ”crazy,” paranoia, and depression (AOR = 2.9, p < .00001) and to have sold drugs on the street (AOR = 2.5, p < .00001). Participants with a history of child abuse, relative to those without, had over twofold increased risks for drug craving (AOR = 2.1, p < .00001) and drug withdrawal symptoms (AOR = 2.0, p = .00005).
TABLE 4.
Emergency room (ER) visits, hospitalization, and problems due to substance use (N = 1748)
| Offspring without child abuse (n = 1478) | Offspring with child abuse (n = 270) | |||||
|---|---|---|---|---|---|---|
| Emergency health care use due to substance use | % (N) | % (N) | OR (95% CI) | p | AORd(95% CI) | p |
| Ever admitted to ER | 1.9 (28) | 5.9 (16) | 3.3 (1.7–6.1) | <.00001 | 2.9 (1.5–5.6) | .001 |
| Ever admitted to in-patient unit | 2.4 (35) | 4.5 (12) | 1.9 (1.0–3.7) | .05 | 2.0 (1.0–4.0) | .05 |
| Health and psychosocial problems | % (N) | % (N) | OR (95% CI) | p | AORd(95% CI) | p |
| Had health problemsa | 3.0 (44) | 7.8 (21) | 2.7 (1.6–4.6) | <.00001 | 2.4 (1.3–4.1) | .003 |
| Problems with family, job etc.b | 13.3 (197) | 33.7 (91) | 3.3 (2.5–4.4) | <.00001 | 3.2 (2.3–4.4) | <.00001 |
| Psychological problemsc | 9.3 (137) | 24.1 (65) | 3.1 (2.2–4.3) | <.00001 | 2.9 (2.0–4.1) | <.00001 |
| Ever sold drug | 14.0 (206) | 29.3 (79) | 2.6 (1.9–3.4) | <.00001 | 2.5 (1.8–3.5) | <.00001 |
| Problems with substance use | % (N) | % (N) | OR (95% CI) | p | AOR (95% CI) | p |
| Felt dependent on it | 12.3 (182) | 27.2 (68) | 2.4 (1.7–3.3) | <.00001 | 2.2 (1.7–2.9) | <.00001 |
| Try to cut down on drugs but could not | 10.7 (158) | 23.7 (64) | 2.6 (1.9–3.6) | <.00001 | 2.5 (1.7–3.4) | <.00001 |
| Needed more drug | 11.5 (170) | 22.6 (61) | 2.2 (1.6–3.1) | <.00001 | 2.1 (1.5–3.0) | <.00001 |
| Had drug withdrawal symptoms | 8.1 (120) | 16.3 (44) | 2.2 (1.5–3.2) | <.00001 | 2.0 (1.4–3.0) | .00005 |
| Used drug daily for 2 or more weeks | 20.0 (295) | 33.3 (90) | 2.0 (1.5–2.7) | <.00001 | 1.9 (1.4–2.5) | <.00001 |
OR = odds ratio; CI = confidence interval; AOR = adjusted odds ratio. Holms correction for multiple testing has been used and the p-value for significance is set for .008.
fits, an accidental overdose, a persistent cough, or an infection as a result of using the drug.
family, friends, on the job, at school, or with the police.
feeling crazy or paranoid or depressed or uninterested in things.
Age, race, sex, and poverty level at birth and at age 7, mother’s educational level, maternal lifetime history of mental health, number of siblings, and childhood behavioral problems (activity level, low attention span, impulsivity, and low frustration tolerance) were adjusted.
DISCUSSION
This study is consistent with previous literature and extends its scope by highlighting five main findings. First, significantly higher rates of substance use, including marijuana, cocaine, and heroin, were evident among study participants with a history of child abuse relative to those without. Second, the cumulative risks of substance use were approximately two- to threefold higher among abused individuals of both genders compared to those nonabused, while as expected substance use rates were generally higher among males than females. Third, as earlier initiation of substance use and consequently a shorter period free from substance use was evident among abused individuals. Fourth, adjustment for demographic, socioeconomic factors, and parental substance use as well as childhood behavioral risk factors, did not erode significant associations between child abuse and lifetime substance use, suggesting that the increased risk and earlier onset of substance use observed in this study was directly due to child abuse and not solely related to these factors. Fifth, child abuse was associated with a significantly increased risk for medical and functional impairment, such as ER visits, health problems, drug dealing, drug dependence, and drug cravings in adulthood.
Our results suggest that exposure to child abuse is associated with a significant increased risk for substance use, including marijuana, heroin, cocaine, opiate, and glue and that it is also associated with an earlier initiation of use in both males and females. To our knowledge, this is one of a few prospective studies that examined the long-term effects of child abuse utilizing data from a community sample. The long follow-up interval (over 30 years) enabled us to documents cumulative risk of substance use. Significantly, our sample consists of 46% males and 54% females, where many prior studies focused predominantly on the consequences of sexual abuse in females (Hillis, Anda, Felitti, Nordenberg, & Marchbank, 2000; McCauley et al., 1997; Wilsnack, Vogeltanz, Klassen, & Harris, 1997) or physical abuse in males (Holmes & Sammel, 2005; Hyman, Garcia, & Sinha, 2006), and often using clinically referred samples. Furthermore, we were able to control for various potential confounders, such as mother’s educational level, child poverty level at birth and at age 7, and mother’s lifetime mental health status, including substance use and alcoholism as well as childhood behavioral characteristics likely to confer greater risk for substance use, such as hyperactivity, short attention span, impulsivity, and low frustration tolerance, as evaluated by research child psychologists at age 7. This enabled us to rule out some of the alternative and confounding mechanisms, such as increased risk for substance use due to behavioral characteristics during childhood, poverty, or familial psychopathology and to conclude that child abuse was independently associated with subsequent substance use.
Our data came from a predominantly impoverished inner city sample with a high lifetime prevalence of substance use. Even in a community with high rates of substance use, differences in the proportion of individuals using substances, between abused and nonabused individuals, were large and statistically significant. For instance, 78% of the abused, as compared to 61% of the nonabused subjects, had a lifetime history of using marijuana ( p < .0001); 47% of the abused, as compared to 26% of the non-abused, had a lifetime history of using cocaine ( p < .0001); and 25% of the abused, as compared to the 13% the nonabused, had a lifetime history of using heroin ( p < .0001). Of note, among community-based prospective studies, Windom et al. (2006) also reported a high rate of marijuana use both among the abused subjects and nonabused subjects (80,4% and 79.2% respectively). Fergusson reported that marijuana use earlier in adolescence or in young adulthood was a precursor for illicit drug abuse/dependence later in life, although the rates of marijuana use in their abused and nonabused participants were not reported. However, a similarly high rate of illicit drug use (noncannabis, 42.9%) was consistent with our finding.
In our sample, there was no gender difference in the increased risk for substance use, although, as expected, the rates of substance use among males were higher than among females. MacMillan et al. (2001) reported that females were at increased risk for illicit drug use and abuse, and concluded that females, but not males, with a history of child abuse had significantly higher lifetime rates of illicit drug abuse/dependence than did females with no such history. Widom et al. (2006) also reported that women, but not men, had an over twofold increased risk for marijuana and any drug use in the past year, whereas Fergusson et al. (2008) reported that being female was protective. One possible explanation may be differences in the design of the studies. Even if all are community-based studies, including ours, self-report measures of child abuse tend to capture a wide range of maltreatment, its frequency and its severity, but not the nature (sexual, psychological, physical, and neglect), This makes it harder to determine where the difference (or similarity) was derived and whether the different the nature of abuse affected genders differently.
Our study has several methodological strengths. The subjects were prospectively and systematically followed from birth into adulthood through the period of risk for substance use for over 30 years. Study subjects were children of the probands (mothers) who were initially enrolled in the study during their pregnancy and randomly selected to be representative of those who sought prenatal care at Johns Hopkins Hospital (Baltimore). Thus, compared to clinically referred samples and their controls, estimates of substance use reported here had a lesser chance of being biased and have greater generalizability. Moreover, risk factors such as childhood inattention and hyperactivity, were prospectively ascertained. The long follow-up time afforded more sophisticated analyses using the proportional hazards model and estimates of cumulative risk for each substance used among persons with child abuse and those without. Inclusion of both males and females further allowed us to examine if the patterns of initiation and increased risks for specific substance use differed by gender additionally.
Study’s Limitations
The study also has limitations. First, assessment of substance use was based on a self-report checklist inventory rather than clinical assessment, though the self-report was ascertained by an interviewer. While the validity of the instruments used to measure abuse.
CTS and substance use is widely supported, there were no external measures to validate the reliability of the self-report. Thus, reporter bias may have influenced the estimates reported here. We did not investigate the effects of different types of abuses, e.g., verbal abuse, physical abuse, and neglect even though the CTS consists of 19 different items regarding different types of abuse. It is possible that we would find gender differences if different types of abuses were examined. However, the main focus of this study is to investigate the long-term consequences of child abuse in the community. While our data include maternal mental health status including substance use and alcoholism, there is no information on paternal mental health, especially substance use, thus familial risk of developing substance use is not adequately addressed in this study. Finally, individuals were considered abused if they were subject to more than mild abuse (i.e., they had to score a standard deviation above the mean in the CTS scales to be considered abused). Other studies may have included milder forms of abuse. Despite these limitations, this study provided cumulative risks for the use of six different substances among males and females with and without child abuse, using a sample drawn from the general population. Since our sample was followed for 30 years, they had passed the at-risk period for substance use. The data presented here provides alarming evidence that child abuse has a profound and long-term impact on substance use and related impairment3, above and beyond the risk conferred by poverty and the childhood risk factors examined in this study. In order to provide effective interventions to prevent substance use, research needs to consider prospectively ascertained childhood risk factors; and policies that lead to the allocation of time and resources to social services at the first prenatal appointment in order to identify future parents who themselves grew up in abusive family environments, deserve consideration. These parents could be offered opportunities to acquire effective parenting skills, thus preventing the intergenerational transmission of child abuse.
GLOSSARY
- Child abuse
Physical, sexual, or emotional mistreatment or neglect of a child.
- Confounder
An extraneous variable that correlates with both a predictor (independent variable) and an outcome (dependent variable). A confounder is a variable that has no bearing on the likelihood of a particular outcome, but it looks as if it does. A classic example is a strong association between having a lighter (independent variable) and the risk for lung cancer (dependent variable). One should not conclude having a lighter is causally linked with an increased incidence of lung cancer. The confounder, i.e., smoking cigarettes, is associated with both the independent variable (having a lighter) and the dependent variable (incidence of lung cancer). In human studies, confounders become particularly important as there is little room for manipulating subject’s psychosocial and physical environment. For example, you cannot randomly assign children to either a warm mother or an abusive mother.
- Cronbach’s Alpha
Commonly used as a measure of internal consistency; one way to evaluate the reliability of the variables that are intended to measure abstract concepts such as drug craving, level of addiction, and quality of life. Alpha greater than .9 is usually regarded excellent, above .8 is regarded good, and above .7 is regarded acceptable.
- Illicit drug use
The use of controlled substances (prescription drugs, narcotics, street drugs) which are produced, trafficked, and consumed illicitly.
- Survival analysis
A statistical strategy to study the length of time that lapses before a particular event occurs or recurs (e.g., before someone starts smoking marijuana).
- Type I error
A type of error is said to have occurred when a null hypothesis is rejected, an alternative hypothesis is accepted, and an apparently significant association is attributed to chance.
- Validity (concurrent and construct)
Concurrent validity is demonstrated when a test correlates well with a measure that has been validated before. For example, when one develops a new measurement, it is expected to correlate well with the existing (already validated) measurement; construct validity refers to the validity of a measurement that purports to identify the underlying abstract concept, such as stress, happiness, and anger.
Biographies

Dr. Yoko Nomura, is an Assistant Professor in the Department of Psychology at Queens College, CUNY, and Clinical Assistant Professor in the Department of Psychiatry at the Mount Sinai School of Medicine. She is interested in elucidating how prenatal and early childhood adversity influences the trajectory of central nervous system development in humans. By learning underlying mechanisms, she hopes to gain insights for early identification, prevention, and intervention of substance use disorders and associated problems. Her current research involves understanding the interplay between genetic susceptibility and fetal programming on child neurobehavioral development.

Dr. Yasmin Hurd, is Professor in the Departments of Psychiatry, Pharmacology and Systems Therapeutics, and Neuroscience at the Mount Sinai School of Medicine. She is the Chief of the Center of Excellence in Mood and Motivation in the Friedman Brain Institute. She is also the Director of the MD/Ph.D. Program and serves as Chair of the Committee on Diversity in Biomedical Research. Her multidisciplinary research investigates the neurobiology underlying addiction disorders and related psychiatric illnesses with a focus on the developmental consequences of cannabis and genetics underlying disease risk. The research involves molecular techniques to study the human brain and translational animal models.
Dr. Daniel J. Pilowsky, a native of Chile, South America, is an assistant professor of clinical epidemiology and psychiatry at Columbia University. He attended medical school in Chile and Argentina, received his medical degree from the University of Buenos Aires, and received his MPH from the Bloomberg School of Public Health at Johns Hopkins University. His current research interests include children and families affected by substance abuse and HIV, HIV prevention, drug use/abuse epidemiology, and children at high risk for depression.
Footnotes
The reader is reminded that the concepts of “risk factors” as well as “protective factors” are often noted in the literature, without adequately noting their dimensions (linear, nonlinear; rates of development; anchoring or integration; cessation; etc.), their “demands,” the critical necessary conditions (endogenously as well as exogenously; from a micro to a meso to a macro level) that are necessary for either of them to operate (begin, continue, become anchored and integrate, change as de facto realities change, cease, etc.) or not to and whether their underpinnings are theory-driven, empirically-based, individual, and/or systemic stake holder-bound, based upon “principles of faith,” historical observation, precedents, and traditions that accumulate over time, perceptual, and judgmental constraints, “transient public opinion” or what. This is necessary to consider and to clarify if these term are not to remain as yet additional shibboleth in a field of many stereotypes, tradition-driven activities, “principles of faith,” and stakeholder objectives. Editor’s note.
The journal’s style utilizes the category substance abuse as a diagnostic category. Substances are used or misused; living organisms are and can be abused. Editor’s note.
The reader is referred to Hills’s criteria for causation that were developed in order to help assist researchers and clinicians determine if risk factors were causes of a particular disease or outcomes or merely associated. (Hill, 1965). Editor’s note.
Declaration of Interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the article.
References
- Abelson HI, Fishburne PM, Cisin I. National survey of drug abuse: National institute on drug abuse, division of research, U.S. department of health education and welfare; public health service, alcohol, drug abuse, and mental health administration. Washington DC: The National Institute on Drug Abuse; 1979. [Google Scholar]
- Amato PR. Psychological distress and the recall of childhood family characteristics. Journal of Marriage and Family. 1991;53:1011–1019. [Google Scholar]
- Binder DA. Fitting Cox’s proportional hazards models from survey data. Biometrika. 1992;79:139–147. [Google Scholar]
- Brown J, Cohen P, Johnson JG, Salzinger SA. Longitudinal analysis of risk factors for child maltreatment: Findings of a 17-year prospective study of officially recorded and self-reported child abuse and neglect. Child Abuse and Neglect. 1998;22:1065–1078. doi: 10.1016/s0145-2134(98)00087-8. [DOI] [PubMed] [Google Scholar]
- Cervantes RC, Duenas N, Valdez A, Kaplan C. Measuring violence risk and outcomes among Mexican American adolescent females. Journal of Interpersonal Violence. 2006;21:24–41. doi: 10.1177/0886260505281602. [DOI] [PubMed] [Google Scholar]
- Cohen P, Brown J, Smailes E. Child abuse and neglect and the development of mental disorders in the general population. Developmental Psychopathology. 2001;13:981–999. [PubMed] [Google Scholar]
- Cox DR. Regression models and life tables. Applied Statistics. 1972;34:187–220. [Google Scholar]
- Dahlberg LL. Youth Violence in the United States: Major trends, risk factors, and prevalent approaches. American Journal of Preventive Medicine. 1998;14:259–272. doi: 10.1016/s0749-3797(98)00009-9. [DOI] [PubMed] [Google Scholar]
- DeBellis MD. Developmental traumatology: A contributory mechanism for alcohol and substance use disorders. Psychoneuroendocrinology. 2000;27:155–170. doi: 10.1016/s0306-4530(01)00042-7. [DOI] [PubMed] [Google Scholar]
- Dube SR, Anda RF, Felitti VJ, Chapman DP, Willamson DF, Giles WH. Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span: Findings from the adverse childhood experiences study. Journal of American Medical Association. 2001;286:3089–3096. doi: 10.1001/jama.286.24.3089. [DOI] [PubMed] [Google Scholar]
- Fan AP, Eaton WW. Longitudinal study assessing the joint effects of socio-economic status and birth risks on adult emotional and nervous conditions. British Journal of Psychiatry. 2001;178:s78–s83. doi: 10.1192/bjp.178.40.s78. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Boden JM, Horwood LJ. The developmental antecedents of illicit drug use: Evidence from a 25-year longitudinal study. Drug and Alcohol Dependence. 2008;96:165–177. doi: 10.1016/j.drugalcdep.2008.03.003. [DOI] [PubMed] [Google Scholar]
- Freisthler B, Merritt DH, LaScala EA. Understanding the ecology of child maltreatment, review of the literature and directions for future research. Child Maltreatment. 2006;11:263–280. doi: 10.1177/1077559506289524. [DOI] [PubMed] [Google Scholar]
- Gilbert R, Widom SW, Browne K, Fergusson D, Webb E, Janson S. Burden and consequences of child maltreatment in high-income countries. Lancet. 2009;373:68–81. doi: 10.1016/S0140-6736(08)61706-7. [DOI] [PubMed] [Google Scholar]
- Green CR, Flowe-Valencia H, Rosenblum L, Tair AR. Do physical and sexual abuse differentially affect chronic pain states in women? Journal of Pain Symptom Management. 1999;18:420–426. doi: 10.1016/s0885-3924(99)00107-4. [DOI] [PubMed] [Google Scholar]
- Hardy JB, Astone NM, Brooks-Gunn J, Shapiro S. Like mother, like child: Inter-generational patterns of age at first birth and associations with childhood and adolescent characteristics and adult outcomes in the second generation. Developmental Psychology. 1998;34:1220–1232. doi: 10.1037//0012-1649.34.6.1220. [DOI] [PubMed] [Google Scholar]
- Hardy JB, Shapiro S, Mellits D, Skinner EA, Astone NM, Ensminger M, et al. Self-sufficiency at age 27 to 33 years: Factors present between birth and 18 years that predict educational attainment among children born to inner-city families. Pediatrics. 1997;99(1):80–87. doi: 10.1542/peds.99.1.80. [DOI] [PubMed] [Google Scholar]
- Hill AB. The environment and disease: Associations or causation? Proceedings of the Royal Society of Medicine. 1965;58:295–300. doi: 10.1177/003591576505800503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hillis SD, Anda RF, Felitti VJ, Nordenberg D, March-bank PA. Adverse childhood experiences and sexually transmitted diseases in men and women: A retrospective study. Pediatrics. 2000;106:1–6. doi: 10.1542/peds.106.1.e11. [DOI] [PubMed] [Google Scholar]
- Holm S. A simple sequentially rejective multiple test procedure. Scandinavian Journal of Statistics. 1979;6:65–70. [Google Scholar]
- Holmes WC, Sammel MD. Brief communication: Physical abuse of boys and possible associations with poor adult outcomes. Anal of Internal Medicine. 2005;143:581–586. doi: 10.7326/0003-4819-143-8-200510180-00008. [DOI] [PubMed] [Google Scholar]
- Horwitz AV, Widom CS, McLaughlin J, White HR. The impact of childhood abuse and neglect on adult mental health: A prospective study. Journal of Health and Social Behavior. 2001;42:184–201. [PubMed] [Google Scholar]
- Hyman SM, Garcia M, Sinha R. Gender specific associations between types of childhood maltreatment and the onset, escalation and severity of substance use in cocaine dependent adults. American Journal of Drug and Alcohol Abuse. 2006:655–664. doi: 10.1080/10623320600919193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilpatrick DG, Acierno R, Saunders B, Resnick HS, Best CL, Schnurr PP. Risk factors for adolescent substance abuse and dependence: Data from a national sample. Journal of Consulting and Clinical Psychology. 2000;68:19–30. doi: 10.1037//0022-006x.68.1.19. [DOI] [PubMed] [Google Scholar]
- Kingston S, Raghavan C. The relationship of secual abuse, early initiation of substance use, and adolescent trauma to PTSD. Journal of Traumatic Stress. 2009;22:50–57. doi: 10.1002/jts.20381. [DOI] [PubMed] [Google Scholar]
- Lansford JE, Dodge KA, Pettit GS, Bates JE, Crozier J, Kaplow J. Long-term effects of early child physical maltreatment on psychological, behavioral, and academic problems in adolescence: A 12-year prospective study. Archives of Pediatrics and Adolescent Medicine. 2002;156:824–830. doi: 10.1001/archpedi.156.8.824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leventhal TL, Brooks-Gunn J. The neighborhoods they live in: The effects of neighborhood residence upon child and adolescent outcomes. Psychological Bulletin. 2000;126:309–337. doi: 10.1037/0033-2909.126.2.309. [DOI] [PubMed] [Google Scholar]
- Liang KY, Zeger SL. Longitudinal data analysis using generalized linear model. Biometrika. 1986;73:13–22. [Google Scholar]
- Lo CC, Cheng TC. The impact of childhood maltreatment on young adults’ substance abuse. American Journal of Drug and Alcohol Abuse. 2007;33:139–146. doi: 10.1080/00952990601091119. [DOI] [PubMed] [Google Scholar]
- MacMillan HL, Fleming JE, Streiner DL, Lin E, Boyle MH, Jamieson E, et al. Childhood abuse and lifetime psychopathology in a community sample. American Journal of Psychiatry. 2001;158:1878–1883. doi: 10.1176/appi.ajp.158.11.1878. [DOI] [PubMed] [Google Scholar]
- MacMillan HL, Niec AC, Offord DR. Child physical abuse: Risk indicators and prevention. Recent Advances in Pediatrics. 1995;14:53–68. [Google Scholar]
- McCauley J, Kern DE, Kolodner K, Dill L, Schroeder AF, DeChant HK, et al. Clinical characteristics of women with a history of childhood abuse: Unhealed wounds. Journal of American Medical Association. 1997;277:1362–1368. [PubMed] [Google Scholar]
- McCord J. A longitudinal view of the relationship between paternal absence and crime. In: Gunn J, Farrington DP, editors. Abnormal offenders, delinquency and the criminal justice system. New York: John Wiley & Sons; 1982. pp. 113–128. [Google Scholar]
- Moran PB, Vuchinich S, Hall NK. Associations between types of maltreatment and substance use during adolescence. Child Abuse and Neglect. 2004;28:565–574. doi: 10.1016/j.chiabu.2003.12.002. [DOI] [PubMed] [Google Scholar]
- Newman MG, Clayton L, Zuellig A, Cashman L, Arnow B, Dea R, et al. The relationship of childhood sexual abuse and depression with somatic symptoms and medical utilization. Psychological Medicine. 2000;30:1063–1077. doi: 10.1017/s003329179900272x. [DOI] [PubMed] [Google Scholar]
- Nomura Y, Chemtob CM. Conjoined effects of low birth weight and childhood abuse on adaptation and well-being in adolescence and adulthood. Archives of Pediatrics and Adolescent Medicine. 1997;161:186–192. doi: 10.1001/archpedi.161.2.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connor TG. Annotation: The ‘effects’ of parenting reconsidered: Findings, challenges, and applications. Journal of Child Psychology and Psychiatry. 2002;43:555–572. doi: 10.1111/1469-7610.00046. [DOI] [PubMed] [Google Scholar]
- Salmon P, Calderbank S. The relationship of childhood physical and sexual abuse to adult illness behavior. Journal of Psychosomatic Research. 1996;40:329–336. doi: 10.1016/0022-3999(95)00580-3. [DOI] [PubMed] [Google Scholar]
- Sampson RJ, Morenoff JD, Gannon-Rowley T. Assessing neighborhood effects: Social process es and new directions in research. Annual Review of Social Sciences. 2002;28:443–478. [Google Scholar]
- Schumm WR, Martin MJ, Bollman SR, Jurich AP. Adolescent perspectives on family violence. Journal of Social Psychology. 1982;117:153–154. doi: 10.1080/00224545.1982.9713421. [DOI] [PubMed] [Google Scholar]
- Simpson TL, Miller WR. Concomitance between childhood sexual and physical abuse and substance use problems: A review. Clinical Psychology. 2002;22:27–77. doi: 10.1016/s0272-7358(00)00088-x. [DOI] [PubMed] [Google Scholar]
- Straus MA. Measuring intrafamily conflict and violence: The conflict tactics (CT) scales. Journal of Marriage and Family. 1979;41:75–88. [Google Scholar]
- Straus MA. The conflict tactics scales and its critics: An evaluation and new data on validity and reliability. In: Straus MA, editor. Physical violence in American families: Risk factors and adaptations to violence in 8,145 families. New Brunswick, NJ: Transaction Publishers; 1990. [Google Scholar]
- Straus MA, Hamby SL, Finkelhor D, Moore DW, Runyan D. Identification of child maltreatment with the parent-child conflict tactics scales: Development and psychometric data for a national sample of American parents. Child Abuse and Neglect. 1998;22:249–270. doi: 10.1016/s0145-2134(97)00174-9. [DOI] [PubMed] [Google Scholar]
- Thornberry TP, Krohn MD, Lizotte AJ, Chard-Wierschem D. The role of juvenile gangs in facilitating delinquent behavior. Journal of Research in Crime and Delinquency. 1993;30:55–87. [Google Scholar]
- Walker EA, Unutzer J, Rutter C, Gelfand A, Saunders K, VonKorff M, et al. Costs of health care use by women HMO members with a history of childhood abuse and neglect. Archives of General Psychiatry. 1999;107:332–339. doi: 10.1001/archpsyc.56.7.609. [DOI] [PubMed] [Google Scholar]
- Wall AE, Kohl PL. Substance use in maltreated youth: Findings from the national survey of child and adolescent well-being. Child Maltreatment. 2007;12:20–30. doi: 10.1177/1077559506296316. [DOI] [PubMed] [Google Scholar]
- Widom CP, Marmorstein NR, White RH. Childhood victimization and illicit drug use in middle adulthood. Psychology of Addictive Behaviors. 2006;20:394–403. doi: 10.1037/0893-164X.20.4.394. [DOI] [PubMed] [Google Scholar]
- Williams R. Product-limit survival functions with correlated survival times. Lifetime Data Analysis. 1995;1:171–186. doi: 10.1007/BF00985768. [DOI] [PubMed] [Google Scholar]
- Wilsnack SC, Vogeltanz ND, Klassen AD, Harris TR. Childhood sexual abuse and women’s substance abuse: National survey findings. Journal of Studies in Alcoholism. 1997;58:264–271. doi: 10.15288/jsa.1997.58.264. [DOI] [PubMed] [Google Scholar]
- Wilson HW, Widom CS. A prospective examination of the path from child abuse and neglect to illicit drug use in middle adulthood: The potential mediating role of four risk factors. Journal of Youth and Adolescent. 2009;38:340–354. doi: 10.1007/s10964-008-9331-6. [DOI] [PubMed] [Google Scholar]
- Yodanis CL, Hill K, Straus MA. Tabular summary of the methodological characteristics of the Conflict Tactics Scales. Durham, NH: Family Research Laboratory, University of New Hampshire; 1997. [Google Scholar]