Abstract
Osteonecrosis of the femoral head is an orthopedic disease caused by femoral head damage or insufficient blood supply, which leads to the death of bone cells and bone marrow. Osteonecrosis of the femoral head leads to changes in the structure of the femoral head, femoral head collapse and joint dysfunction. Bone morphogenetic protein-2 (BMP-2) exhibits beneficial effects on bone formation, repair and angiogenesis at the femoral head. In the present study, the therapeutic effects of recombinant human BMP-2 containing an Fc fragment (rBMP-2/Fc) were investigated on a steroid induced mouse model of osteonecrosis of the femoral head. Bone cell viability was used to determine the in vitro effects of rBMP-2/Fc. The therapeutic efficacies of rBMP-2/Fc on mice with osteonecrosis of the femoral head were evaluated using clinical arthritis scores. The expression levels of inflammatory factors in the mice were analyzed by reverse transcription-quantitative polymerase chain reaction. Histological analysis was used to evaluate the effects of rBMP-2/Fc on the femoral head. The results revealed that rBMP-2/Fc treatment significantly increased the IL-6, IL-10, vascular endothelial growth factor and macrophage colony-stimulating factor expression levels in synovial cells compared with the control group (P<0.01). Furthermore, it was observed that rBMP-2/Fc significantly improved the viability and growth of synovial cells (P<0.01) through the nuclear factor (NF)-κB signaling pathway. Treatment with rBMP-2/Fc significantly decreased receptor activator of NF-κB ligand expression levels. Furthermore, in vivo experiments demonstrated that rBMP-2/Fc treatment markedly relieved the arthralgia and damage caused by osteonecrosis of the femoral head. In conclusion, rBMP-2/Fc treatment may be beneficial for articular cartilage repair by the upregulation of angiogenesis factors through the down regulation of the NF-κB signaling pathway in mice with osteonecrosis of the femoral head. This preclinical data suggests that rBMP-2/Fc may be a promising novel agent for treatment of osteonecrosis of the femoral head.
Keywords: osteonecrosis of the femoral head, recombinant bone morphogenetic protein-2/Fc fragment, nuclear factor-rag angiogenesis
Introduction
Arthritis is a degenerative disease characterized by joint pain, tenderness, stiffness, swelling, restricted movement and joint deformities (1). There are a number of different types of arthritis, including rheumatic arthritis, rheumatoid arthritis, osteoarthritis, gouty arthritis, ankylosing spondylitis, reactive arthritis, infectious arthritis and other factor-induced arthritis (2,3). In recent years, the number of osteoarthritis has risen and an increasing number of individuals have been clinically diagnosed with the condition, which presents a serious threat to human health and quality of life (4,5). Osteonecrosis of the femoral head is a specific type of osteoarthritis that significantly affects the patient's ability to move and exhibits the most serious degeneration of the joints among osteonecrosis diseases (6,7).
Osteonecrosis of the femoral head may be divided into different categories, including traumatic, drug-induced and alcohol-stimulated femoral head necrosis, which have different degrees of pathogenesis and disease progression (4,8). Previous studies have demonstrated that osteonecrosis of the femoral head is an autoimmune disease and primarily manifests as inflammatory arthritis (9,10). The causes of femoral head necrosis are diverse and complex, meaning they are difficult to comprehensively explain in a classification system. Additionally, the pathogenesis of osteonecrosis of the femoral head is not fully understood (11–13). Therefore, a variety of treatments for osteonecrosis of the femoral head have previously been proposed (14–16). Although the outcomes described in previous studies are encouraging, the failure rates remain high due to the failure of bone generation and revascularization in the femoral head (17–19).
Bone morphogenetic proteins (BMPs) belong to the transforming growth factor-β superfamily that regulates a number of cellular activities (20). Previous studies have demonstrated that BMPs serve important roles in different forms of arthritis and their disease activity (21–23). Grcevic et al (24) previously reported that the peripheral blood expression profiles of BMPs may act as predictive markers for the development of arthritis, its disease activity, therapeutic responsiveness and overall prognosis. Lories and Luyten (25) previously suggested that BMPs are beneficial for the repair of joint destruction and tissue responses that may form the basis of chronic arthritis. BMP-2 is a member of the BMP family that contributes to bone formation, joint anti-inflammation and synovial repair (26,27). Previous research has suggested that recombinant BMP-2may induce bone formation and osteoblastic differentiation by regulating endochondral ossification (28,29). In addition, abnormal expression of BMP-2 in mesenchymal cells has been investigated in association with rheumatoid arthritis (30). Furthermore, BMP-2 has been used clinically during spinal fusion procedures and treatment outcomes have indicated that it is effective in regulating joint inflammation and damage in rats and rabbits (31,32). However, the in vivo effects of BMP-2 in humans are unpredictable due to its short half-life in patients with rheumatoid arthritis (33).
In the present study, the beneficial effects of recombinant BMP-2 containing the Fc fragment (rBMP-2/Fc) were investigated in a mouse model of osteonecrosis of the femoral head. The results indicated that rBMP-2/Fc significantly improved the viability and growth of synovial cells through the nuclear factor (NF)-κB signaling pathway. In vivo experiments demonstrated that rBMP-2/Fc treatment markedly relieved the arthralgia and repaired the damaged osteonecrosis of the femoral head by promoting angiogenesis of the femoral head.
Materials and methods
Animal protocol
A total of 60 male 6–8 week old, C57BL/6J mice were purchased from Shanghai SLAC Laboratory Animal Co., Ltd. (Shanghai, China). All mice were identified by ear punching and housed in temperature-controlled room (25±1°C; humidity, (50±5°C) with an artificial 12 h light/dark cycle and ad libitum free access to food and water. A steroid-induced osteonecrosis of the femoral head (SI-OTFD) mouse model was established as previously described, via the subcutaneous administration of 100 mg/kg steroid (Glucocorticoid; ModiQuest Research, Oss, The Netherlands). The mice were divided into the following three groups (n=20 per group): i) The control group (healthy mice), ii) the BMP-2/Fc group and iii) the dexamethasone (DEX) group (positive control). On day 7 following model establishment, the mice received treatment with either BMP-2/Fc (10 mg/kg, Sigma-Aldrich; Merck KGaA, Darmstadt, Germany), DEX (10 mg/kg; Sigma-Aldrich; Merck KGaA) or the same volume of PBS (control group) via intravenous injection. The body weights of the experimental mice were measured prior to each administration. The treatments were administered seven times, once every three days for a total of 21 days. Mice were sacrificed on day 32 for histological analysis with 100 mg/kg 1% intravenous sodium pentobarbital. Clinical osteonecrosis of the femoral head was evaluated using a scale of 0–2 as previously described (34). A total of 10 randomly selected mice were sacrificed on day 32 and the remainder were housed for a 120-day observation. Body and spleen weights of mice were measured post-sacrifice on day 32. Arthritic scores were measured from mice as previously described (35).
The present study was performed in strict accordance with the recommendations of the Guide for the Care and Use of Laboratory Animals of the Tianjin Medical University (36). All animal procedures were reviewed and approved by the Ethical Committee of Shandong Medical University (Shandong, China). All surgeries and euthanasia were performed under sodium pentobarbital anesthesia (1% sodium pentobarbital, 40 mg/kg, Sigma-Aldrich; Merck KGaA) by intraperitoneal injection. All efforts were made to minimize the suffering of the experimental mice.
Cells and reagents
Experimental mice were anesthetized using sodium pentobarbital anesthesia (1% intravenous sodium pentobarbital, 40 mg/kg, Sigma-Aldrich) and Synoviocytes were isolated from the experimental mice on day 32 as described previously (37) and then cultured at 37°C in a 5% CO2 humidified atmosphere in minimum essential medium (Sigma-Aldrich; Merck KGaA) with 10% fetal bovine serum (FBS; Sigma-Aldrich; Merck KGaA). BMP and BMP receptor (BMP-2R) were also purchased from Sigma-Aldrich (Merck KGaA). Saos-2 cells were purchased from the American Type Culture Collection (Manassas, VA, USA) and cultured in Dulbecco's modified Eagle's medium (DMEM; Sigma-Aldrich; Merck KGaA) with 10% FBS for 12 h at 37°C in a 5% CO2 humidified atmosphere. Synoviocytes from PBS-treated mice were treated with rBMP-2/Fc (10 ng/ml), BMP-2R (10 ng/ml) or PBS (Control) for 24 h at 37°C in a 5% CO2 humidified atmosphere to analyze the activity and function of rBMP-2/Fc in synoviocytes.
Cell viability
Synoviocytes form experimental mice following treatment were seeded at a density of 1×103 cells/well in 96-well plates with DMEM containing 10% FBS at 37°C for certain time periods (12, 24, 36, 48, 60 and 72 h). Following incubation, 20 µl MTT reagent (Sigma-Aldrich; Merck KGaA) in 20 µl PBS was added into each well and cells were incubated at 37°C for 4 h, to enable the formation of water insoluble formazan crystals. The formazan crystals were then dissolved using dimethyl sulfoxide (200 µl/well) and their absorbance (optical density, OD) at 570 nm was measured using a microplate spectrophotometer (Bio-Rad Laboratories, Inc., Hercules, CA, USA). The inhibition rate of cell viability was calculated using the following equation: Inhibition rate (%)=(ODcontrol-ODtreated)/ODcontrol ×100.
Cell differentiation
Synoviocytes from sacrificed experimental mice following treatment were seeded at a density of 1×105 cells/cm2 for 12 h at 37°C. At 85% confluence, the cells were cultured in osteogenic medium (Invitrogen; Thermo Fisher Scientific, Inc., Waltham, MA, USA) containing 5% fetal bovine serum (Gibco; Thermo Fisher Scientific, Inc.) in the presence of the aforementioned reagents. The procedures used for characterizing Synoviocyte differentiation were as described in a previous study (38).
ELISA analysis
The concentration of vascular endothelial growth factor (VEGF; cat. no. MMV00; Bio-Rad Laboratories, Inc.), BMP-2R (MAB3552; Bio-Rad Laboratories, Inc.), receptor activator of NF-κB ligand (RANKL; cat. no, Hu7596RY; Huiying, Shanghai, China) and macrophage colony-stimulating factor (M-CSF; cat. no. KHG00112; Thermo Fisher Scientific, Inc.) In the synovial cells of experimental mice were analyzed using ELISA. Synovial cells were harvested and homogenized in an Instant One ELISA Cell Lysis Buffer (Invitrogen; Thermo Fisher Scientific, Inc.). The synovial cells were subsequently separated by centrifugation at 6,000 × g for 10 min at room temperature and the homogenate was quantified according to a previously described method (39). The levels of BMP-2R (cat. no. FK-R0025; Huiying), M-CSF (cat. no. KHG00112; Thermo Fisher Scientific, Inc.) and RANKL (cat. no, Hu7596RY; Huiying) were measured using ELISA according to the manufacturers' protocols. Levels of BMP-2 (cat. no. ab119582), IL-6 (cat. no. ab100712) and IL-10 (cat. no. ab100765) were assessed using ELISA kits obtained from Abcam (Cambridge, UK) according to the manufacturers' protocol.
Formation of the rBMP2/Fc protein
The human BMP-2 linked with the Fc fragment was obtained form the Department of Orthopedics, Shandong Provincial Hospital Affiliated to Shandong University (Jinan, China). The gene was sequenced by Invitrogen (Thermo Fisher Scientific, Inc.) and the BMP-2/Fc gene (200 ng) was inserted into pET27b vectors and named pET27b-BMP-2/Fc. The pET27b-BMP-2/Fc was expressed in Escherichia coli Rossetta (Invitrogen; Thermo Fisher Scientific, Inc.) by transforming the recombinant pET27b-BMP-2/Fc plasmid using electro transformation (40). The bacteria were grown in lysogeny broth medium (Invitrogen; Thermo Fisher Scientific, Inc.) for 12 h at 37°C and 0.5 mM isopropylthio-β-d-galactoside (IPTG, Sigma-Aldrich; Merck KGaA) was used to induce BMP-2/Fc expression. Subsequently, the cells were disrupted following a 12 h induction with IPTG and dissolved in 15 ml PBS. The protein underwent denaturation for 12 h at 90°C and renaturation for 12 h at 4°C and ion exchange chromatography was used to purify the protein of interest. The purified protein was collected and 1.5% gel filtration chromatography (glucan) further purified the rBMP-2/Fc protein.
Reverse transcription-quantitative (RT-q) PCR
Total RNA from the synovial cells was extracted using a RiboMinus™ Eukaryote kit (Invitrogen; Thermo Fisher Scientific, Inc.) according to the manufacturer's protocol. The concentration of RNA was quantified by spectrophotometry at 260 nm (SmartSpec 3000; Bio-Rad Laboratories, Inc.). The quantified RNA was subjected to RT into cDNA using a QuantiTect Reverse Transcription kit (Qiagen Sciences, Inc., Gaithersburg, MD, USA) and the quality was confirmed by electrophoresis. The cDNA was diluted 1/10 with distilled water and 10 µl was used for amplification. The RT-qPCR was performed using a real-time quantitative PCR machine (Roche Molecular Diagnostics, Pleasanton, CA, USA) with QuantiNova SYBR Green RT-PCR Kit (Qiagen Sciences, Inc., Gaithersburg, MD, USA) according to the manufacturer's protocol. Forward and reverse primers were synthesized by Invitrogen (Thermo Fisher Scientific, Inc.) and their sequences were as follows: RANKL, forward 5′-GCAGAGAAAGCGATGGTGGA-3′ and reverse 5′-GGAACCAGATGGGATGTCGG-3′; VEGF, forward 5′-TGCATTCACATTGTGCTGCTGTAG-3′ and reverse 5′-GCAGATTATGCGGATCAAACC-3′; M-CSF forward 5′-ACCACCTATGCGGATTTCAT-3′ and reverse 5′-TCATTACGCAGGCACAAAAG-3′; intercellular adhesion molecule 1 (ICAM-1), forward 5′-TGCTGAACTGAAGTACACTGGCATTGGTTTTG-3′ and reverse 5′-CCTGAACTGAAGTACTGGCATTGGTCAGTCA-3′; platelet-derived endothelial cell growth factor (PD-ECGF), forward 5′-AGAACCCGAGGAATGGCGA-3′ and reverse 5′-AGGCCTTTGCCACTGCTTGTA-3′; and β-actin, forward 5′-CGGAGTCAACGGATTTGGTC-3′ and reverse 5′-AGCCTTCTCCATGGTCGTGA-3′. The thermo cycling conditions of PCR were as follows: A preliminary denaturation at 94°C for 2 min, followed by 40 cycles of 95°C for 30 sec. The annealing temperature was then reduced to 58°C for 30 sec and 72°C for 300 sec. The reaction total reaction volume was 20 µl and contained 50 ng genomic cDNA, 200 µM dNTPs, 200 µM primers and Taq DNA polymerase and SYBR-Green (both 2.5 U; Thermo Fisher Scientific, Inc.). Relative mRNA expression changes were quantified using the 2−ΔΔCq method (41). The results are presented as the n-fold change compared with β-actin.
Pain-associated behavior tests
During treatments the mechanical allodynia test and spontaneous lifting behaviors were used to evaluate the paw withdrawal mechanical threshold (PWMT). These tests were performed as previously described (42).
Western blot analysis
Synovial cells were treated with PBS, DEX or rBMP-2/Fc, homogenized in a lysate buffer (radio immunoprecipitation assay buffer) containing protease inhibitor (Sigma-Aldrich; Merck KGaA) and centrifuged at 6,000 × g at 4°C for 10 min. The supernatant was used to analyze the expression levels of specific proteins. Protein concentration was measured with a BCA protein assay kit (Thermo Fisher Scientific, Inc.). A total of 10 µg/lane protein was separated in 15% SDS gel and then transferred onto poly vinylidene fluoride membranes (EMD Millipore, Billierica, MA, USA). Prior to western blot analysis the membranes were blocked with 5% skimmed milk for 1 h at 37°C and subsequently incubated at 4°C overnight with rabbit anti-mouse primary antibodies sourced from Sigma-Aldrich (Merck KGaA) directed against: NF-κB (cat. no. SAB4501987), p65 (cat. no. SAB4502615), inhibitor of NF-κB kinase-β (IKK-β; cat. no. SAB1300467) and NF-κB inhibitor-α (IκBα; cat. no. SAB4501997). The following antibodies sourced from Abcam (Cambridge, UK) were also utilized: ALP (cat. no. ab83259), Runx2 (cat. no. ab23981), Osterix (cat. no. ab22552), Osterocalcir (cat. no. ab93876), pSmad-1 (cat. no. ab71720), pSmad-5 (cat. no. ab11437), pSmad-8 (cat. no. ab110288) and β-actin (cat. no. ab8227). All antibodies were diluted at 1:1,000. The membranes were then incubated with goat anti-rabbit horseradish peroxidase-labeled immunoglobulin G secondary antibodies (1:2,000; cat. no. PV-6001; OriGene Technologies, Inc., Beijing, China) for 24 h at 4°C. The results were visualized using a chemiluminescence detection system (Roche Diagnostics, Basel, Switzerland) and with BandScan 5.0 software (Glyko, Inc.; BioMarin Pharmaceutical Inc., Novato, CA, USA).
Histopathological analysis
Mice were sacrificed under pentobarbital anesthesia on day 32 and their hips joints were separated and fixed with 10% formalin for 30 min at 37°C. The joints were subsequently decalcified and embedded in paraffin. Sections of hip joints (5 µm) from the experimental mice were stained with hematoxylin and eosin for 1 h at 37°C and the sections were used to evaluate the therapeutic effects of rBMP-2/Fc, DEX and PBS in an SI-OTFD mouse model. Tissue sections were observed using a light microscope (Olympus Corporation, Tokyo, Japan) at a magnification of ×40. The severity of the arthritis in the joints was scored on a scale of 0–5 as previously described (43).
Vascular density measurements and evaluation of bone reabsorption activity
The vascular density measurements and an evaluation of the bone reabsorption activity of mice following treatment with rBMP-2/Fc, DEX and PBS (n=6) were conducted as previously described (44,45). Briefly, for the vascular density, factor VIII-associated antigen-stained images were captured at a magnification of ×200 using an ECLIPSE E600 microscope with a 20× objective lens (Nikon Corporation, Tokyo, Japan). Two images were randomly selected and the most highly vascularized area of the femoral head was recorded. The area of one image was 0.330 mm2. The vascular densities were analyzed using an image analysis system (analysis; Soft Imaging System GmbH, Munster, Germany). The vascular density was calculated as follows: (Factor VIII stained vascular area/total image area in ×200 magnification) ×100. For bone reabsorption activity, the cluster of differentiation 68-positive multinucleated cells containing three or more nuclei were counted in five random high-power fields (magnification, ×400) in each femoral head. The area of one high-power field was 0.238 mm2. The total area analyzed per case was 1.188 mm2. A total of 6 randomly selected mice from each group were evaluated.
Half-life assays
The half-life of BMP-2 and rBMP-2/Fc were assessed via half-life experiments as described previously (46). Briefly, BMP-2 or rBMP-2were labeled with IRDye 800CW NHS Ester (LI-COR Biosciences, Lincoln, NE, USA) and the degree of labeling was determined according to the manufacturer's protocol. A total of 50 µg labeled BMP-2 or rBMP-2 was injected retro-orbitally into the C57BL/6J mice and blood was harvested from the tail every 60 min and collected in heparin coated tubes. The tubes were protected from light and kept at 4°C until blood collection was complete. Infrared luminescence was measured using the Odyssey Infrared Imaging system (LI-COR Biosciences) and analyzed using ImageJ software version 1.2 (National Institutes of Health, Bethesda, MD, USA).
Statistical analysis
All data are presented as the mean + standard deviation of three independent experiments. Unpaired data was determined using Student's t-test and comparisons between multiple groups were made using one-way analysis of variance followed by a post-hoc Tukey's test. Kaplan-Meier was used to estimate the survival rate during the 120-day long-term treatment. P<0.05 was considered to indicate a statistically significant difference.
Results
In vitro effects of rBMP-2/Fc on synovial cells from a SI-OTFD mouse model
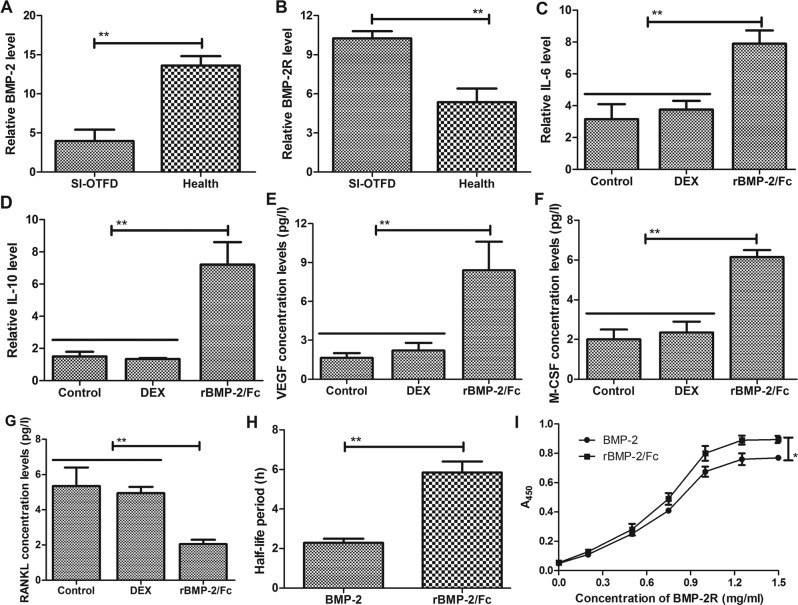
To investigate the efficacy of rBMP-2/Fc on SI-OTFD, the levels of BMP-2 and BMP-2R in synovial cells were measured. BMP-2 expression levels were significantly lower in synovial cells from the mouse model of SI-OTFD compared with the healthy mice group (Fig. 1A), whereas BMP-2R was significantly increased in the SI-OTFD group compared with the healthy group (Fig. 1B). The effect of rBMP-2/Fc on the expression of IL-6, IL-10, VEGF and M-CSF in synovial cells was investigated; DEX was used as a control. The expression of IL-6, IL-10, VEGF and M-CSF were significantly upregulated in rBMP-2/Fc-treated synovial cells compared with the control and DEX groups (Fig. 1C-F, respectively). Conversely the expression of RANKL was significantly decreased following treatment with rBMP-2/Fc compared with the control and DEX groups (Fig. 1G). It was also observed that the half-life of rBMP-2/Fc was significantly increased compared with BMP-2 (Fig. 1H) and rBMP-2/Fc presented a higher affinity for BMP-2 (Fig. 1I). These results suggest that rBMP-2/Fc effectively binds with BMP-2R and that rBMP-2/Fc treatment may regulate the expression of IL-6, IL-10, M-CSF and RANKL in synovial cells.
Figure 1.
Effects of rBMP-2/Fc on synovial cells isolated from experimental mice. The expression of (A) BMP-2 and (B) BMP-2R in synovial cells from a mouse model of osteonecrosis of the femoral head were determined by ELISA. The expression of (C) IL-6 (D) IL-10, (E) VEGF, (F) M-CSF and (G) RANKL in synovial cells were analyzed by ELISA. (H) The half-life periods of rBMP-2/Fc and BMP-2 were determined by pharmacokinetic methods. (I) The affinity of rBMP-2/Fc for BMP-2R was measured. *P<0.05, **P<0.01. BMP-2, bone morphogenetic protein-2; rBMP, recombinant bone morphogenetic protein; Fc, Fc fragment; BMP-2R, bone morphogenetic protein-2 receptor; Il, interleukin; VEGF; vascular endothelial growth factor; M-CSF, macrophage colony-stimulating factor; RANKL, receptor activator of NF-κB ligand; SI-OTFD, steroid-induced osteonecrosis of the femoral head; DEX, dexamethasone.
Analysis of the underlying mechanism of the rBMP-2/Fc-mediated signaling pathway for osteonecrosis of the femoral head in a mouse model
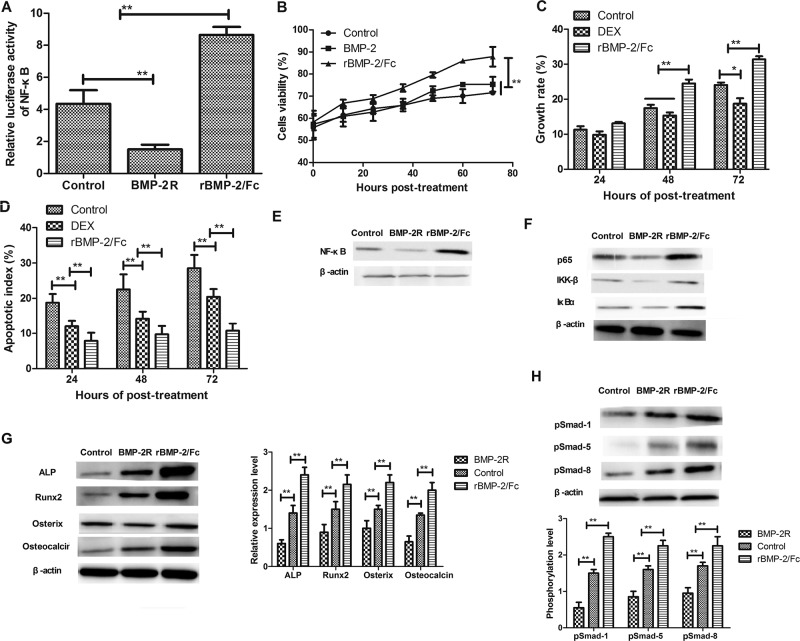
Although the benefits of BMP-2 on arthritis have been previously investigated (21), the underlying mechanism of the rBMP-2/Fc-mediated signaling pathway for osteonecrosis of the femoral head in a mouse model remains unknown. It was observed that the expression of BMP-2 was positively associated with the gene signatures of NF-κB signaling, indicating that the NF-κB signaling pathway may be regulated by BMP-2 in bone synovial cells (Fig. 2A). NF-κB was detected at significantly higher levels in the rBMP-2/Fc group compared with the control and BMP-2R groups. It was also observed that treatment with rBMP-2/Fc significantly increased the cell viability of synovial cells compared with the BMP-2 and control groups (Fig. 2B). The cell growth rate was also significantly increased in the rBMP-2/Fc group at 48 and 72 h compared with the DEX and control groups (Fig. 2C). Treatment with rBMP-2/Fc significantly decreased the apoptosis of synovial cells induced by steroids compared with the DEX and control groups (Fig. 2D). Western blot analysis revealed that the addition of BMP-2R resulted in a marked decrease in NF-κB protein expression, whereas treatment with rBMP-2/Fc markedly increased NF-κB protein expression levels in vitro (Fig. 2E). Furthermore, the protein expression levels of p65, IKKβ and IκBα were markedly increased in synovial cells treated with rBMP-2/Fc, whereas they were notably downregulated following treatment with BMP-2R (Fig. 2F). In vitro western blot analysis revealed that alkaline phosphatase (ALP), runt-related transcription factor 2 (Runx2), osterix and osteocalcin were significantly upregulated in rBMP-2/Fc-treated synoviocytes compared with the control and BMP-2R groups (Fig 2G). Additionally, treatment with rBMP-2/Fc induced a significant increase in the protein levels of phosphorylated Smad-1, Smad-5 and Smad-8 in Saos-2 cells (Fig. 2H). These results indicate that rBMP-2/Fc exerts a beneficial effect by increasing the viability of synovial cells obtained from experimental mice.
Figure 2.
Analysis of the signaling pathways mediated by rBMP-2/Fc in synovial cells. (A) Analysis of the association between BMP-2 and NF-κB expression in synovial cells as determined by luciferase activity. (B) The viability of synovial cells following incubation with rBMP-2/Fc (10 mg/ml), BMP-2 (2 mg/ml) or PBS for different time periods as determined by the refractive index. (C) The growth rate of synovial cells following treatment with PBS, DEX or rBMP-2/Fc for 24, 48 and 72 has determined by an MTT assay. (D) The effects of rBMP-2/Fc on the apoptosis of synovial cells as determined by flow cytometry. Western blot analysis was performed to determine the protein expression levels of (E) NF-κB, (F) p65, IKK-β and IκBα in synovial cells following treatment with BMP-2R or rBMP-2/Fc. The protein expression of (G) ALP, Runx2, osterix and osteocalcin, and (H) pSmad-1, pSmad-5 and pSmad-8 in Saos-2 cells was determined via western blot analysis.*P<0.05, **P<0.01. BMP-2, bone morphogenetic protein-2; rBMP, recombinant bone morphogenetic protein; Fc, Fc fragment; BMP-2R, bone morphogenetic protein-2 receptor; NF, nuclear factor; IKK-β, inhibitor of NF-κB kinase-β; IκBα, NF-κB inhibitor-α; ALP, alkaline phosphatase; Runx2, runt-related transcription factor 2; p, phosphorylated; DEX, dexamethasone.
Therapeutic effects of rBMP-2/Fc for steroid-induce osteonecrosis of the femoral head mice
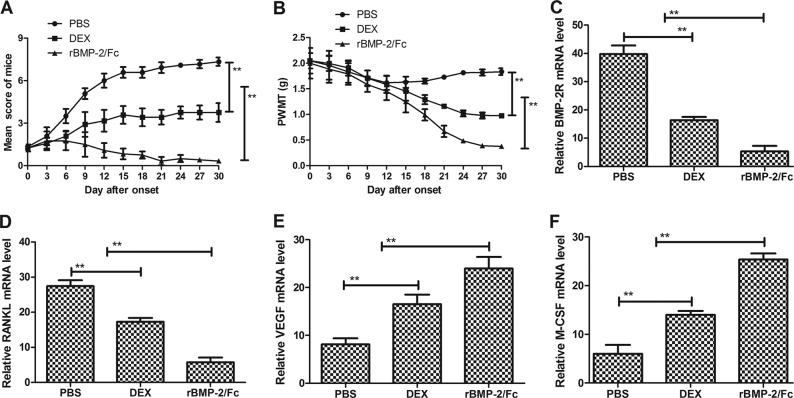
Experimental SI-OTFD mice were administered with rBMP-2/Fc, DEX or PBS as described above. The therapeutic effects of these agents were recorded every 3 days using an arthritic score in each experimental group. It was revealed that treatment with rBMP-2/Fc significantly ameliorated the clinical symptoms used to measure an arthritic score compared with the DEX- and PBS-treated mice (Fig. 3A). Additionally, rBMP-2/Fc-treated mice exhibited a significantly decreased PWMT compared with the DEX and PBS groups (Fig. 3B). Furthermore, the VEGF, BMP-2R, RANKL and M-CSF mRNA expression levels were measured in the synovial cells from mice in each treatment group. The expression levels of BMP-2R and RANKL were significantly downregulated in rBMP-2/Fc-treated mice compared with the DEX and PBS groups (Fig. 3C and D). Conversely, the expression levels of VEGF and M-CSF were significantly upregulated in mice treated with rBMP-2/Fc compared with the DEX and PBS groups (Fig. 3E and F). These results suggest that rBMP-2/Fc was able to improve the clinical symptoms and arthritis-associated factors in mice with osteonecrosis of the femoral head, which may contribute to the recovery of mice from osteonecrosis of the femoral head.
Figure 3.
In vivo effects of rBMP-2/Fc on steroid-induced osteonecrosis of the femoral head in a mouse model. (A) The clinical symptoms of mice with steroid-induced osteonecrosis of the femoral head were used to determine an arthritic score. (B) Pain-associated behaviors of experimental mice following treatment with PBS, DEX or rBMP-2/Fc were determined by PWMT. The mRNA expression levels of (C) BMP-2R, (D) RANKL, (E) VEGF and (F) M-CSF in experimental mice with steroid-induced osteonecrosis of the femoral head were determined by reverse transcription-quantitative polymerase chain reaction.**P<0.01. BMP-2, bone morphogenetic protein-2; rBMP, recombinant bone morphogenetic protein; Fc, Fc fragment; DEX, dexamethasone; PWMT, paw withdrawal mechanical threshold; BMP-2R, bone morphogenetic protein-2 receptor; VEGF; vascular endothelial growth factor; M-CSF, macrophage colony-stimulating factor; RANKL, receptor activator of NF-κB ligand.
Vascular density measurements, evaluation of bone reabsorption activity and histological evaluation of femoral head mice treated by rBMP-2/Fc
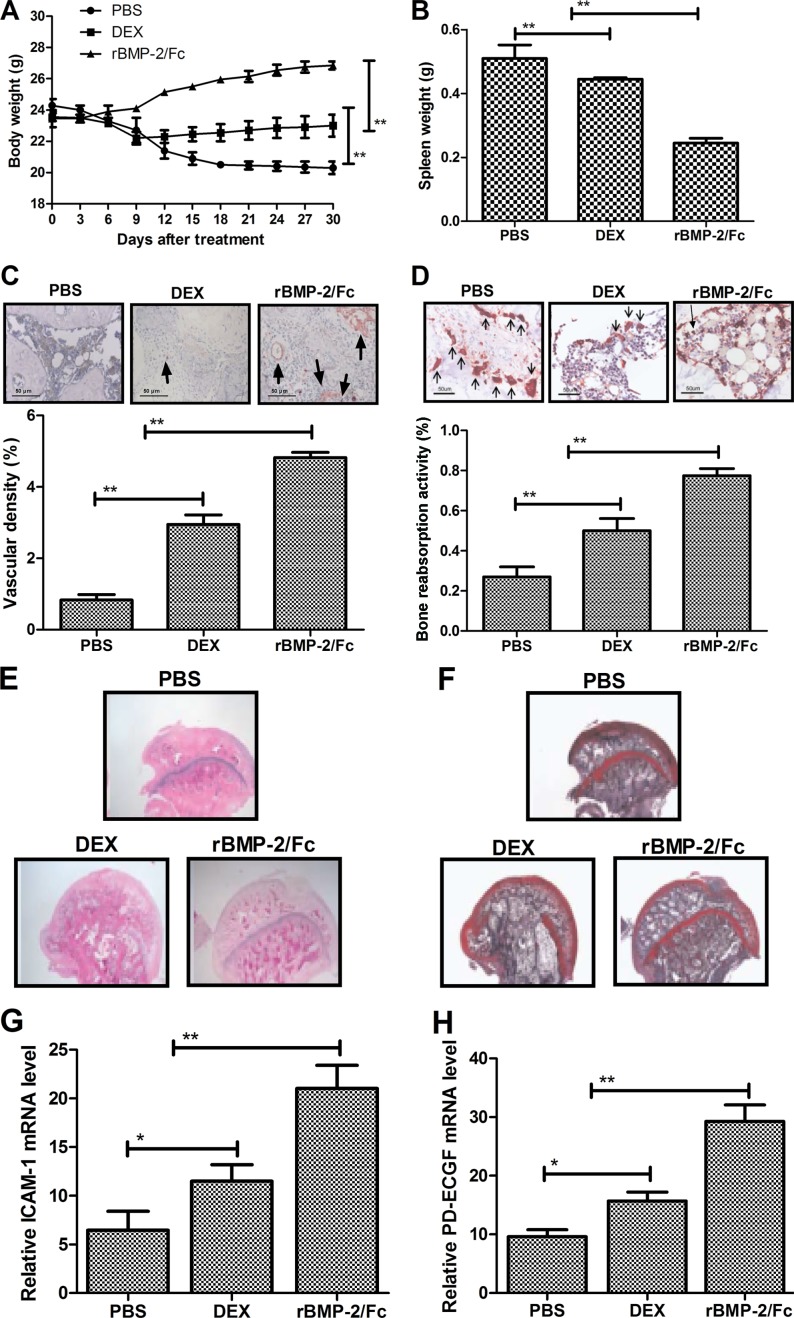
Throughout the experimental period the body and spleen weights of the mice were measured. These results revealed that at day 30 the body weights of the rBMP-2/Fc-treated mice were significantly increased compared with the DEX and PBS groups (Fig. 4A and B). The DEX group was also significantly heavier than the PBS group at day 30. The notable changes in body weight appeared to begin at day 9. The spleen weight was also significantly reduced in the rBMP-2/Fc group compared with the PBS and DEX groups. The vascular density and bone reabsorption activity of the ischemic femoral head in the rBMP-2/Fc-treated group were significantly higher compared with the DEX and PBS groups (Fig. 4C and D). Furthermore, histological analysis revealed that rBMP-2/Fc-treated mice exhibited homogeneous density and presented with notably smooth and regular articular surface (Fig. 4E). It was also identified that a well-preserved secondary ossification center and trabecular bone formation was greater (Fig. 4F) than the DEX-treated group and PBS-treated group.
Figure 4.
Histopathologic analysis of the therapeutic effects of rBMP-2/Fc in steroid-induced osteonecrosis of the femoral head in a mouse model. (A) Analysis of the (A) body weights and (B) spleen weights of mice following 30-days treatment with PBS, DEX or rBMP-2/Fc. (C) The vascular density of the femoral head in mice treated with PBS, DEX or rBMP-2/Fc was determined via Factor VIII staining of the vascular area. (D) Evaluation of bone reabsorption activity of the ischemic femoral head in mice treated with PBS, DEX or rBMP-2/Fc as determined by cluster of differentiation 68 staining. (E) Images of the smooth articular surface and (F) the well-preserved secondary ossification center in mice treated with PBS, DEX or rBMP-2/Fc were used to determine histopathologic analysis. Magnification, 40×. The mRNA expression of the angiogenesis factors (G) ICAM-1 and (H) PD-ECGF in synovial cells in experimental mice as determined by reverse transcription-quantitative polymerase chain reaction. *P<0.05; **P<0.01. BMP-2, bone morphogenetic protein-2; rBMP, recombinant bone morphogenetic protein; Fc, Fc fragment; DEX, dexamethasone; ICAM-1, intercellular adhesion molecule 1; PD-ECGF, platelet-derived endothelial cell growth factor.
The results indicated that the articular cartilage of mice treated by rBMP-2/Fc were more healthier. It was also observed that the angiogenesis factors ICAM-1 and PD-ECGF were significantly upregulated following rBMP-2/Fc treatment in synovial cells compared with the PBS and DEX groups (Fig. 4G and H). These results suggest that rBMP-2/Fc treatment markedly improves pathological status of femoral head analyzed by histological staining.
Discussion
Osteonecrosis of the femoral head is a serious arthritic disease that undergoes complex pathological processes during its initiation and development (47). Previous studies have demonstrated that core decompression combined with BMPs, growth factors, bone grafting or stem cells are therapeutic options for osteonecrosis of the femoral head (48–50). The symptoms of osteonecrosis of the femoral head are multitudinous and include pain, stiff joints with limited activity, lameness, different degrees of femoral head necrosis (5,51). In recent years the incidence rate of osteonecrosis of the femoral head has increased (52,53). Therefore, further treatment options are required to improve the prognosis and comfort of patients diagnosed with osteonecrosis of the femoral head. In the present study, the therapeutic effects of BMP-2/Fc in a mouse model of osteonecrosis of the femoral head were investigated with DEX used as a positive control. The results of the present study suggested that BMP-2/Fc is an effective agent for the treatment of osteonecrosis of the femoral head.
BMPs are members of the transforming growth factor-β superfamily, which regulates cellular metabolism and signaling pathways, including cell proliferation, migration, apoptosis, differentiation and adhesion in many types of cells (54,55). Recent studies have reported that BMP-2 may be used to reconstruct segmental mandibular defects and repair ischemic damage by inducing angiogenesis and osteogenesis, and by decreasing osteoclast bone reabsorption activity (56,57). However, the half-life of BMP-2 is short in vivo, which limits its clinical application (58,59). In the present study, a recombinant BMP-2 linked with an Fc fragment, rBMP-2/Fc, was synthesized to prolong its half-life in vivo. The longer half-life of rBMP-2/Fc significantly improved the viability of synoviocytes compared with BMP-2. The results indicated that rBMP-2/Fc is an efficient drug for the inhibition of joint inflammation and damage. The effect of rBMP-2/Fc was investigated according to its clinical presentation.
The femoral head is a highly vascularized articular tissue and angiogenesis is crucial to prevent the progression of osteonecrosis of the femoral head (60,61). Neovascularization supports the osteoblasts and mesenchymal stem cells during femoral head repair and construction (62,63). However, the mRNA levels of BMP-2R were significantly higher in SI-OTFD mice compared with the healthy mice, suggesting that they may have been downregulated by rBMP-2/Fc treatment. A recent study has summarized the different treatments available for osteonecrosis of the femoral head and the different mechanisms by which they act on osteogenesis and angiogenesis has also been discussed in association with bone regeneration (15). All treatment strategies emphasize the importance of angiogenesis for bone regeneration. In addition, osteonecrosis of the femoral head causes a reduction in vascular density, which leads to an inadequate amount of subchondral bone at the femoral head, which results in osteocyte death and the collapse of the articular surface (15). A previous study has indicated that revascularization contributes to the recovery of osteonecrosis at the femoral head, which suggests that it may be part of the underlying mechanism of initiation, development and aggravation of glucocorticoid-induced osteonecrosis of the femoral head (64). VEGF and M-CSF serve an essential role in angiogenesis and bone regeneration (23,65). The present study investigated angiogenesis and synovial repair in a mouse model of osteonecrosis of the femoral head following treatment with rBMP-2/Fc. In vivo experiments indicated that rBMP-2/Fc significantly increased VEGF and M-CSF in synovial cells and contributed to the improvement of the clinical features of angiogenesis and osteogenesis.
Inflammatory cytokines have been identified as crucial regulatory signaling networks in osteonecrosis of the femoral head, which are mediated by intracellular kinase signaling pathways and regulate recruitment, stimulation, activation and the accumulation of autoimmune cells (66). The causes of osteonecrosis of the femoral head are not fully understood, however, laboratory and clinical evidence suggest that inflammatory cytokines may contribute to its pathogenesis (67,68). Therefore, blocking the inflammatory cytokine pathways may interrupt the inflammatory process and break the cycle of inflammation, thereby limiting joint damage (69,70). In the present study, the expression levels of inflammatory factors following rBMP-2/Fc treatment were measured. The results revealed that the administration of rBMP-2/Fc significantly reduced the pathogenesis of osteonecrosis of the femoral head by inhibiting the inflammatory cytokines (IL-6 and IL-10).
A previous study has demonstrated that the NF-κB signaling pathway serves an essential role in controlling revascularization and osteogenesis by regulating VEGF, BMP-2, RANKL and M-CSF expression during the progression of glucocorticoid-induced osteonecrosis of the femoral head (71). In the present study, the underlying mechanism of the rBMP-2/Fc-mediated signaling pathway in the progression of glucocorticoid-induced osteonecrosis of the femoral head was investigated. It was revealed that rBMP-2/Fc-mediated improvement may be attributed to the upregulation of the NF-κB signaling pathway, which promotes revascularization and osteogenesis in the femoral head.
In conclusion, the present study investigated the roles of rBMP-2/Fc in association with the level of cytokines present in the joint, homeostasis, revascularization and osteogenesis. The results demonstrated that rBMP-2/Fc is beneficial for the treatment of osteonecrosis of the femoral head by promoting the expression of proangiogenic factors in synovial cells. This leads to revascularization and osteogenesis through regulation of the NF-κB signaling pathway. These findings also indicate that rBMP-2/Fc treatment presents beneficial effects on alleviating joint inflammation, cartilage destruction and bone damage in mice with osteonecrosis of the femoral head, suggesting that rBMP-2/Fc may be a potential novel agent for the treatment of osteonecrosis of the femoral head in humans, although further investigation is required to confirm this.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The analyzed data sets generated during the present study are available from the corresponding author on reasonable request.
Authors' contributions
DZ designed the study and wrote the manuscript. CW and HZ performed the research and HZ analyzed the data. All authors have read and approved this manuscript.
Ethics approval and consent to participate
All animal procedures were reviewed and approved by the Ethical Committee of Tianjin Medical University (Tianjin, China; certificate no. TJMWD-2012011B) and the China Experimental Animal Protection Association. All efforts were made to minimize the suffering of the experimental mice.
Consent for publication
Not applicable.
Competing interests
All authors have no conflict of interest to declare.
References
- 1.Onuora S. Osteoarthritis: Molecular imaging detects activated macrophages. Nat Rev Rheumatol. 2016;12:313. doi: 10.1038/nrrheum.2016.70. [DOI] [PubMed] [Google Scholar]
- 2.Shepherd J, Cooper K, Harris P, Picot J, Rose M. The clinical effectiveness and cost-effectiveness of abatacept, adalimumab, etanercept and tocilizumab for treating juvenile idiopathic arthritis: A systematic review and economic evaluation. Health Technol Assess. 2016;20:1–222. doi: 10.3310/hta20340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bhadu D, Das SK, Dhakad U, Sharma M, Srivastava D, Tripathy SR. Synovial chondromatosis involving multiple joints in rheumatoid arthritis: A case report review of the literature. Int J Rheum Dis. 2017;20:2148–2151. doi: 10.1111/1756-185X.12887. [DOI] [PubMed] [Google Scholar]
- 4.Ma YW, Jiang DL, Zhang D, Wang XB, Yu XT. Radial extracorporeal shock wave therapy in a person with advanced osteonecrosis of the femoral head: A case report. Am J Phys Med Rehabil. 2016;95:e133–e139. doi: 10.1097/PHM.0000000000000484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee GW, Park KS, Kim DY, Lee YM, Eshnazarov KE, Yoon TR. Results of total hip arthroplasty after core decompression with tantalum rod for osteonecrosis of the femoral head. Clin Orthop Surg. 2016;8:38–44. doi: 10.4055/cios.2016.8.1.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhu HY, Gao YC, Wang Y, Zhang CQ. Circulating exosome levels in the diagnosis of steroid-induced osteonecrosis of the femoral head. Bone Joint Res. 2016;5:276–279. doi: 10.1302/2046-3758.56.BJR-2015-0014.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kuroda Y, So K, Goto K, Matsuda S. Extremely early stage osteonecrosis of the femoral head in a patient with hip pain secondary systemic steroid pulse therapy for Vogt-Koyanagi-Harada syndrome: A case report. Int J Surg Case Rep. 2016;25:97–101. doi: 10.1016/j.ijscr.2016.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cabrolier J, Molina M. Is instillation of bone marrow stem cells at the time of core decompression useful for osteonecrosis of the femoral head? Medwave. 2016;16(Suppl 1):e6406. doi: 10.5867/medwave.2016.6406. (In Spanish) [DOI] [PubMed] [Google Scholar]
- 9.Farzaei MH, Farzaei F, Abdollahi M, Abbasabadi Z, Abdolghaffari AH, Mehraban B. A mechanistic review on medicinal plants used for rheumatoid arthritis in traditional Persian medicine. J Pharm Pharmacol. 2016;68:1233–11248. doi: 10.1111/jphp.12606. [DOI] [PubMed] [Google Scholar]
- 10.Rajeev A, Choudhry N, Shaikh M, Newby M. Lumbar facet joint septic arthritis presenting atypically as acute abdomen-A case report and review of the literature. Int J Sur Case Rep. 2016;25:243–245. doi: 10.1016/j.ijscr.2016.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Meyers MH. Osteonecrosis of the femoral head. Pathogenesis and long-term results of treatment. Clin Orthop Relat Res. 1988:51–61. [PubMed] [Google Scholar]
- 12.Gold EW, Cangemi PJ. Incidence and pathogenesis of alcohol-induced osteonecrosis of the femoral head. Clin Orthop Relat Res. 1979:222–226. [PubMed] [Google Scholar]
- 13.Vignon G, Meunier P. Pathogenesis of primary osteonecrosis of the femoral head. Hypothesis of the subchondral fatigue fracture. Nouv Presse Med. 1973;2:1751–1753. [PubMed] [Google Scholar]
- 14.Yamamoto T, Iwamoto Y. Corticosteroids treatments and osteonecrosis of the femoral head. Fukuoka Igaku Zasshi. 2015;106:47–53. (In Japanese) [PubMed] [Google Scholar]
- 15.Wang C, Peng J, Lu S. Summary of the various treatments for osteonecrosis of the femoral head by mechanism: A review. Exp Ther Med. 2014;8:700–706. doi: 10.3892/etm.2014.1811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pelaz A, Junquera L, Gallego L, Garcia-Consuegra L, Junquera S, Gomez C. Alternative treatments for oral bisphosphonate-related osteonecrosis of the jaws: A pilot study comparing fibrin rich in growth factors and teriparatide. Med Oral Patol Oral Cir Bucal. 2014;19:e320–e326. doi: 10.4317/medoral.19458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Meloni MC, Hoedemaeker WR, Fornasier V. Failed vascularized fibular graft in treatment of osteonecrosis of the femoral head. A histopathological analysis. Joints. 2016;4:24–30. doi: 10.11138/jts/2016.4.1.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Furuya T, Maeda S, Momohara S, Taniguchi A, Yamanaka H. Dental treatments, tooth extractions and osteonecrosis of the jaw in Japanese patients with rheumatoid arthritis: Results from the IORRA cohort study. J Bone Miner Metab. 2017;35:344–350. doi: 10.1007/s00774-016-0763-x. [DOI] [PubMed] [Google Scholar]
- 19.Sadile F, Bernasconi A, Russo S, Maffulli N. Core decompression versus other joint preserving treatments for osteonecrosis of the femoral head: A meta-analysis. Br Med Bull. 2016;118:33–49. doi: 10.1093/bmb/ldw010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Singh K, Massel DH, Mayo BC, Bohl DD, Long WW, Modi KD. Bone morphogenetic proteins in lumbar arthrodesis: What is all the debate about? Commentary on an article by Daniel C. Beachler, PhD, MHS, et al: ‘Bone morphogenetic protein use and cancer risk among patients undergoing lumbar arthrodesis: A case-cohort study using the SEER-medicare database’. J Bone Joint Surg Am. 2016;98:e57. doi: 10.2106/JBJS.16.00316. [DOI] [PubMed] [Google Scholar]
- 21.Aruwajoye OO, Aswath PB, Kim HKW. Material properties of bone in the femoral head treated with ibandronate and BMP-2 following ischemic osteonecrosis. J Orthop Res. 2017;35:1453–1460. doi: 10.1002/jor.23402. [DOI] [PubMed] [Google Scholar]
- 22.Rahim I, Salt S, Heliotis M. Successful long-term mandibular reconstruction and rehabilitation using non-vascularised autologous bone graft and recombinant human BMP-7 with subsequent endosseous implant in a patient with bisphosphonate-related osteonecrosis of the jaw. Br J Oral Maxillofac Surg. 2015;53:870–874. doi: 10.1016/j.bjoms.2015.08.006. [DOI] [PubMed] [Google Scholar]
- 23.Wang W, Liu L, Dang X, Ma S, Zhang M, Wang K. The effect of core decompression on local expression of BMP-2, PPAR-γ and bone regeneration in the steroid-induced femoral head osteonecrosis. BMC Musculoskelet Disord. 2012;13:142. doi: 10.1186/1471-2474-13-142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Grcevic D, Jajic Z, Kovacic N, Lukic IK, Velagic V, Grubisic F, Ivcevic S, Marusic A. Peripheral blood expression profiles of bone morphogenetic proteins, tumor necrosis factor-superfamily molecules and transcription factor Runx2 could be used as markers of the form of arthritis, disease activity and therapeutic responsiveness. J Rheumatol. 2010;37:246–256. doi: 10.3899/jrheum.090167. [DOI] [PubMed] [Google Scholar]
- 25.Lories RJ, Luyten FP. Bone morphogenetic proteins in destructive and remodeling arthritis. Arthritis Res Ther. 2007;9:207. doi: 10.1186/ar2135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Postigo J, Iglesias M, Alvarez P, Jesús Augustin J, Buelta L, Merino J, Merino R. Bone morphogenetic protein and activin membrane-bound inhibitor, a transforming growth factor beta rheostat that controls murine treg cell/Th17 cell differentiation and the development of autoimmune arthritis by reducing interleukin-2 signaling. Arth Rheum. 2016;68:1551–1562. doi: 10.1002/art.39557. [DOI] [PubMed] [Google Scholar]
- 27.Brescia AC, Simonds MM, McCahan SM, Fawcett PT, Rose CD. The role of transforming growth factor β signaling in fibroblast-like synoviocytes from patients with oligoarticular juvenile idiopathic arthritis: Dysregulation of transforming growth factor β signaling, including overexpression of bone morphogenetic protein 4, may lead to a chondrocyte phenotype and may contribute to bony hypertrophy. Arth Rheum. 2014;66:1352–1362. doi: 10.1002/art.38336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Okubo Y, Bessho K, Fujimura K, Kusumoto K, Ogawa Y, Iizuka T. Osteogenesis by recombinant human bone morphogenetic protein-2 at skeletal sites. Clin Orthop Relat Res. 2000:295–301. doi: 10.1097/00003086-200006000-00035. [DOI] [PubMed] [Google Scholar]
- 29.Ozec Y, Ozturk M, Kýlýç E, Yeler H, Göze F, Gümüş C. Effect of recombinant human bone morphogenetic protein-2 on mandibular distraction osteogenesis. J Craniofac Surg. 2006;17:80–83. doi: 10.1097/01.scs.0000188747.60087.40. [DOI] [PubMed] [Google Scholar]
- 30.Marinova-Mutafchieva L, Taylor P, Funa K, Maini RN, Zvaifler NJ. Mesenchymal cells expressing bone morphogenetic protein receptors are present in the rheumatoid arthritis joint. Arth rheumatism. 2000;43:2046–2055. doi: 10.1002/1529-0131(200009)43:9<2046::AID-ANR16>3.0.CO;2-8. [DOI] [PubMed] [Google Scholar]
- 31.Issa JP, do Nascimento C, Lamano T, Iyomasa MM, Sebald W, de Albuquerque RF., Jr Effect of recombinant human bone morphogenetic protein-2 on bone formation in the acute distraction osteogenesis of rat mandibles. Clin Oral Implants Res. 2009;20:1286–1292. doi: 10.1111/j.1600-0501.2009.01799.x. [DOI] [PubMed] [Google Scholar]
- 32.Yonezawa H, Harada K, Ikebe T, Shinohara M, Enomoto S. Effect of recombinant human bone morphogenetic protein-2 (rhBMP-2) on bone consolidation on distraction osteogenesis: A preliminary study in rabbit mandibles. J Craniomaxillofac Surg. 2006;34:270–276. doi: 10.1016/j.jcms.2006.02.003. [DOI] [PubMed] [Google Scholar]
- 33.Tekari A, May RD, Frauchiger DA, Chan SC, Benneker LM, Gantenbein B. The BMP2 variant L51P restores the osteogenic differentiation of human mesenchymal stromal cells in the presence of intervertebral disc cells. Eur Cell Mater. 2017;33:197–210. doi: 10.22203/eCM.v033a15. [DOI] [PubMed] [Google Scholar]
- 34.Zalavras CG, Lieberman JR. Osteonecrosis of the femoral head: evaluation and treatment. J Am Acad Orthop Surg. 2014;22:455–464. doi: 10.5435/JAAOS-22-07-455. [DOI] [PubMed] [Google Scholar]
- 35.Greenhill CJ, Jones GW, Nowell MA, Newton Z, Harvey AK, Moideen AN, Collins FL, Bloom AC, Coll RC, Robertson AA, et al. Interleukin-10 regulates the inflammasome-driven augmentation of inflammatory arthritis and joint destruction. Arthritis Res Ther. 2014;16:419. doi: 10.1186/s13075-014-0419-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Davey G, Wu Z. Attitudes in China toward the use of animals in laboratory research. Altern Lab Anim. 2007;35:313–316. doi: 10.1177/026119290703500305. [DOI] [PubMed] [Google Scholar]
- 37.Kim HB, Lee SW, Mun CH, Yoon JY, Pai J, Shin I, Park YB, Lee SK, Cho JW. O-linked N-acetylglucosamine glycosylation of p65 aggravated the inflammation in both fibroblast-like synoviocytes stimulated by tumor necrosis factor-α and mice with collagen induced arthritis. Ar Res Ther. 2015;17:248. doi: 10.1186/s13075-015-0762-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Elsafadi M, Manikandan M, Dawud RA, Alajez NM, Hamam R, Alfayez M, Kassem M, Aldahmash A, Mahmood A. Transgelin is a TGF β-inducible gene that regulates osteoblastic and adipogenic differentiation of human skeletal stem cells through actin cytoskeleston organization. Cell Death Dis. 2016;7:e2321. doi: 10.1038/cddis.2016.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Figueiredo CP, Simon D, Englbrecht M, Haschka J, Kleyer A, Bayat S, Hueber A, Pereira RM, Rech J, Schett G. Quantification and impact of secondary osteoarthritis in patients with anti-citrullinated protein antibodies positive rheumatoid arthritis. Arth Rheumatol. 2016;68:2114–2121. doi: 10.1002/art.39698. [DOI] [PubMed] [Google Scholar]
- 40.Li H, Zhang L, Guo W, Xu D. Development of a genetically engineered Escherichia coli strain for plasmid transformation in Corynebacterium glutamicum. J Microbiol Methods. 2016;131:156–160. doi: 10.1016/j.mimet.2016.10.019. [DOI] [PubMed] [Google Scholar]
- 41.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 42.Sun Y, Jiang M, Hou B, Lu C, Lei Y, Ma Z, Gu X. Mas-related gene (Mrg) C activation attenuates bone cancer pain via modulating Gi and NR2B. PLoS One. 2016;11:e0154851. doi: 10.1371/journal.pone.0154851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bai F, Tian H, Niu Z, Liu M, Ren G, Yu Y, Sun T, Li S, Li D. Chimeric anti-IL-17 full-length monoclonal antibody is a novel potential candidate for the treatment of rheumatoid arthritis. Int J Mol Med. 2014;33:711–721. doi: 10.3892/ijmm.2013.1611. [DOI] [PubMed] [Google Scholar]
- 44.Kinsella S, Murphy K, Breen M, O'Neill S, McLaughlin P, Coyle J, Bogue C, O'Neill F, Moore N, McGarrigle A, et al. Comparison of single CT scan assessment of bone mineral density, vascular calcification and fat mass with standard clinical measurements in renal transplant subjects: The ABC HeART study. BMC Nephrol. 2015;16:188. doi: 10.1186/s12882-015-0182-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Morimoto Y, Hoshino H, Sakurai T, Terakawa S, Nagano A. Quantitative evaluation of bone resorption activity of osteoclast-like cells by measuring calcium phosphate resorbing area using incubator-facilitated and video-enhanced microscopy. Microsc Res Tech. 2009;72:317–322. doi: 10.1002/jemt.20654. [DOI] [PubMed] [Google Scholar]
- 46.Zhu EF, Gai SA, Opel CF, Kwan BH, Surana R, Mihm MC, Kauke MJ, Moynihan KD, Angelini A, Williams RT, et al. Synergistic innate and adaptive immune response to combination immunotherapy with anti-tumor antigen antibodies and extended serum half-life IL-2. Cancer Cell. 2015;27:489–501. doi: 10.1016/j.ccell.2015.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Pierce TP, Elmallah RK, Jauregui JJ, Poola S, Mont MA, Delanois RE. A current review of non-vascularized bone grafting in osteonecrosis of the femoral head. Curr Rev Musculoskelet Med. 2015;8:240–245. doi: 10.1007/s12178-015-9282-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pierce TP, Jauregui JJ, Elmallah RK, Lavernia CJ, Mont MA, Nace J. A current review of core decompression in the treatment of osteonecrosis of the femoral head. Curr Rev Musculoskelet Med. 2015;8:228–232. doi: 10.1007/s12178-015-9283-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Peng WX, Wang L. Adenovirus-mediated expression of bmp-2 and BFGF in bone marrow mesenchymal stem cells combined with demineralized bone matrix for repair of femoral head osteonecrosis in beagle dogs. Cell Physiol Biochem. 2017;43:1648–1662. doi: 10.1159/000484026. [DOI] [PubMed] [Google Scholar]
- 50.Shi L, Sun W, Gao F, Cheng L, Li Z. Heterotopic ossification related to the use of recombinant human BMP-2 in osteonecrosis of femoral head. Medicine (Baltimore) 2017;96:e7413. doi: 10.1097/MD.0000000000007413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mishima H, Sugaya H, Yoshioka T, Aoto K, Wada H, Akaogi H, Ochiai N. The safety and efficacy of combined autologous concentrated bone marrow grafting and low-intensity pulsed ultrasound in the treatment of osteonecrosis of the femoral head. Eur J Orthop Surg Traumatol. 2016;26:293–298. doi: 10.1007/s00590-016-1752-4. [DOI] [PubMed] [Google Scholar]
- 52.Kianmehr N, Bidari A, Mofidi M, Bahar N. Silent osteonecrosis of the femoral head following high-dose corticosteroids in patients with systemic rheumatic diseases. Med J Islam Repub Iran. 2015;29:259. [PMC free article] [PubMed] [Google Scholar]
- 53.Jin H, Xu T, Chen Q, Wu C, Wang P, Mao Q, Zhang S, Shen J, Tong P. The fate and distribution of autologous bone marrow mesenchymal stem cells with intra-arterial infusion in osteonecrosis of the femoral head in dogs. Stem Cell Int. 2016;2016:8616143. doi: 10.1155/2016/8616143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sasikumar KP, Elavarasu S, Gadagi JS. The application of bone morphogenetic proteins to periodontal and peri-implant tissue regeneration: A literature review. J Pharm Bioallied Sci. 2012;4(Suppl 2):S427–S430. doi: 10.4103/0975-7406.100320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bragdon B, Moseychuk O, Saldanha S, King D, Julian J, Nohe A. Bone morphogenetic proteins: A critical review. Cell Signal. 2011;23:609–620. doi: 10.1016/j.cellsig.2010.10.003. [DOI] [PubMed] [Google Scholar]
- 56.Hustedt JW, Blizzard DJ. The controversy surrounding bone morphogenetic proteins in the spine: A review of current research. Yale J Biol Med. 2014;87:549–561. [PMC free article] [PubMed] [Google Scholar]
- 57.Dagostino PR, Whitmore RG, Smith GA, Maltenfort MG, Ratliff JK. Impact of bone morphogenetic proteins on frequency of revision surgery, use of autograft bone and total hospital charges in surgery for lumbar degenerative disease: Review of the nationwide inpatient sample from 2002 to 2008. Spine J. 2014;14:20–30. doi: 10.1016/j.spinee.2012.10.035. [DOI] [PubMed] [Google Scholar]
- 58.Thawani JP, Wang AC, Than KD, Lin CY, La Marca F, Park P. Bone morphogenetic proteins and cancer: Review of the literature. Neurosurgery. 2010;66:233–246. doi: 10.1227/01.NEU.0000363722.42097.C2. [DOI] [PubMed] [Google Scholar]
- 59.Ye L, Bokobza SM, Jiang WG. Bone morphogenetic proteins in development and progression of breast cancer and therapeutic potential (review) Int J Mol Med. 2009;24:591–597. doi: 10.3892/ijmm_00000269. [DOI] [PubMed] [Google Scholar]
- 60.Uzun G, Mutluoglu M, Ersen O, Yildiz S. Hyperbaric oxygen therapy in the treatment of osteonecrosis of the femoral head: A review of the current literature. Undersea Hyperb Med. 2016;43:189–199. [PubMed] [Google Scholar]
- 61.Wood TJ, Hoppe DJ, Winemaker M, Adili A. Bilateral osteonecrosis of the femoral head during pregnancy following two corticosteroid injections: A case report and review of the literature. Cureus. 2016;8:e556. doi: 10.7759/cureus.556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hong GJ, Lin N, Chen LL, Chen XB, He W. Association between vascular endothelial growth factor gene polymorphisms and the risk of osteonecrosis of the femoral head: Systematic review. Biomed Rep. 2016;4:92–96. doi: 10.3892/br.2015.527. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 63.Papakostidis C, Tosounidis TH, Jones E, Giannoudis PV. The role of ‘cell therapy’ in osteonecrosis of the femoral head. A systematic review of the literature and meta-analysis of 7 studies. Acta Orthop. 2016;87:72–78. doi: 10.3109/17453674.2015.1077418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wang B, Geng Q, Hu J, Shao J, Ruan J, Zheng J. Platelet-rich plasma reduces skin flap inflammatory cells infiltration and improves survival rates through induction of angiogenesis: An experiment in rabbits. J Plas Surg Hand Surg. 2016;50:239–245. doi: 10.3109/2000656X.2016.1159216. [DOI] [PubMed] [Google Scholar]
- 65.Radke S, Battmann A, Jatzke S, Eulert J, Jakob F, Schutze N. Expression of the angiomatrix and angiogenic proteins CYR61, CTGF and VEGF in osteonecrosis of the femoral head. J Orthop Res. 2006;24:945–952. doi: 10.1002/jor.20097. [DOI] [PubMed] [Google Scholar]
- 66.Lebouvier A, Poignard A, Cavet M, Amiaud J, Leotot J, Hernigou P, Rahmouni A, Bierling P, Layrolle P, Rouard H. Development of a simple procedure for the treatment of femoral head osteonecrosis with intra-osseous injection of bone marrow mesenchymal stromal cells: Study of their biodistribution in the early time points after injection. Stem Cell Res Ther. 2015;6:68. doi: 10.1186/s13287-015-0036-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Chiu WC, Lai YP, Chou MY. Humanization and characterization of an anti-human TNF-α murine monoclonal antibody. PLoS One. 2011;6:e16373. doi: 10.1371/journal.pone.0016373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Weisman MH. TNF and anti-TNF treatment in rheumatoid arthritis (RA). What we know and what we still need to know. Ryumachi. Rheumatism. 1997;37:142–143. [PubMed] [Google Scholar]
- 69.Elliot MJ, Maini RN, Feldmann M, Long-Fox A, Charles P, Katasikis P, Brennan FM, Bijl H, Ghrayeb J, Woody JN. Treatment of rheumatoid arthritis with chimeric monoclonal antibodies to tumor necrosis factor alpha. Arthritis Rheum. 2008;58(2 Suppl):S92–S101. doi: 10.1002/art.23362. [DOI] [PubMed] [Google Scholar]
- 70.Segal B, Rhodus NL, Patel K. Tumor necrosis factor (TNF) inhibitor therapy for rheumatoid arthritis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:778–787. doi: 10.1016/j.tripleo.2008.07.025. [DOI] [PubMed] [Google Scholar]
- 71.Wang J, Wang K, Shi Z, Zhang M. Osteoprotegerin mRNA/receptor activator of NF-kappaB ligand mRNA expressions in bone tissues of glucocorticoid-induced osteonecrosis of the femoral head. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2008;22:1161–1164. (In Chinese) [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The analyzed data sets generated during the present study are available from the corresponding author on reasonable request.