Abstract
Across the globe, dietary habits include the consumption of foods and drinks between main meals. Although often described as “snacks” or “snacking,” there is no scientific consensus of what constitutes a snack, either as an eating occasion or as a snack food. Nonetheless, food-based dietary guidelines, compiled at national or regional levels by governments, learned societies, and health organizations, frequently refer to snacking habits and desirable or undesirable snack food choices. This review aims to provide a comprehensive snapshot of snacking recommendations worldwide. From a search of 207 countries and organizations, 49 countries and 7 regional or global organizations were identified that referred to snacks, snack foods, or snacking. A total of 136 snacking-specific recommendations or examples were identified, which varied in nature whereby some provided advice on the quality of the snack food choice and others focused on the frequency or energy and nutrient composition of such snacks. Guidelines varied in terms of the detail of foods and drinks identified, wherein some recommendations focused only on foods or food categories to include (e.g., fruit or dairy) or to exclude (e.g., processed foods), whereas other recommendations made reference to both. Both individual foods (e.g., apples) and food categories (e.g., fruit) were mentioned. Reasons or rationales to support the snacking choices were less frequently identified and varied across regions. It is hoped that this analysis will stimulate discussion on the need for a consensus in the scientific community and beyond with regard to snacking. An agreed-upon definition of snacks, snacking, and snack foods could be used to inform a number of stakeholders and ultimately help consumers adhere to healthful diets as defined locally.
Keywords: snacks, snack foods, snacking, dietary guidelines, dietary recommendations
Introduction
Analyses of national diet and nutrition surveys provide concrete evidence that all population groups regularly eat between meals (1–8). Such eating patterns are sometimes described as “snacks” or “snacking” (i.e., eating a snack) (9). To date, a number of studies have analyzed whether a relation exists between snack foods or the act of snacking on subsequent food and nutrient intakes (8, 10–15), energy balance and adiposity (11, 16–19), or cardiometabolic health (20–22). Despite rigorous analyses, it is still unclear whether snacking has a positive or negative impact on nutrition and health outcomes, leading to the inability to reach a consensus on the relation between snacking and health (9, 23). This is perhaps unsurprising given the lack of an agreed-upon scientific definition on what constitutes a meal, a snack, or an eating occasion for either children or adults (9, 16, 24). For snacks and snacking, a number of definitions have been used in the literature. These can be both objective or subjective in nature and can include criteria such as time, energy content, type of food, and location of consumption, or can be based on participant- or researcher-led classifications (1, 2, 6, 16, 24–29). The interpretation of the terms “snacks” and “snacking” by the lay audience also appears to have some interindividual variation (30–32), which could influence consumer behaviors or, more importantly, the comparability of research relying on self-reported snacking data. An additional level of uncertainty exists with how scientific messages on snacking are translated into food-based dietary guidelines (FBDGs) and how these may vary by region or country. FBDGs have been described by the WHO and the FAO as the “expression of the principles of nutrition education mostly as foods” (33). Compiled by many national, regional, and global authorities, they are designed to provide science-based nutrition education and guidance to the public. To be successful, they should be easily understood, culturally appropriate, and acceptable and may therefore vary by country or region (33). An initial study of FBDGs of selected regions identified different degrees of focus on snacking specifically compared with other eating occasions and overall diet and also in the foods recommended as snacks (9).
This review aims to characterize the diversity of references to snacks, snack foods, and snacking in dietary recommendations around the world. It will first describe the process followed to identify snacking recommendations available worldwide, and subsequently describe the composition and variety of available snacking recommendations.
Methods
Search strategy and selection process
In the current review, a systematic search for all published FBDGs was completed to identify all available snacking recommendations. FBDGs are typically published locally in native languages and are not available in any of the usual scientific search engines. However, the FAO has compiled a repository of FBDGs globally, with links to each country's FBDG (34). This repository was the main search engine used for this review.
All population groups aged >2 y were considered. In addition, a search of national nutrition societies and, where necessary, cross-checking through personal communications was completed. The main searches were conducted between June 2015 and October 2015. All references to “snacks,” “snack foods,” “snacking,” and “in between meals” were included.
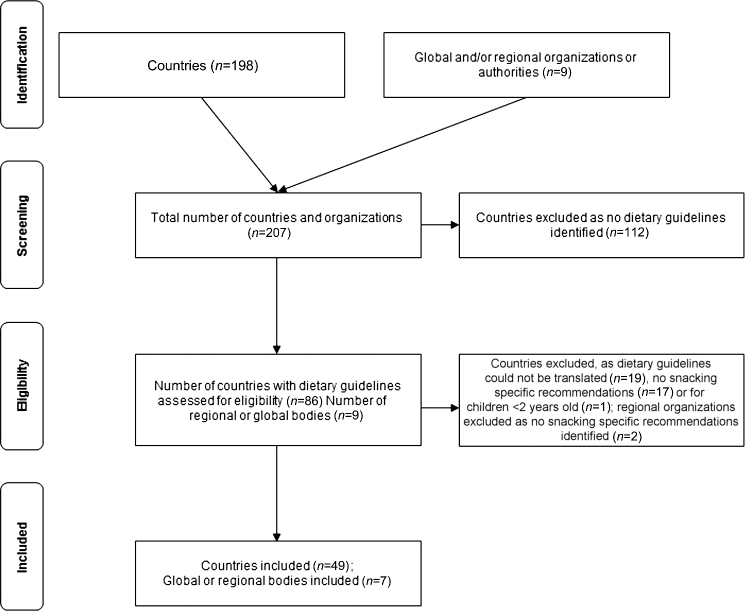
After a search of 198 countries and all regional authorities and organizations with nutrition expertise (e.g., the WHO or the European Food Safety Authority), a total of n = 207 countries and organizations were searched. After screening, a total of 112 countries were excluded because no dietary guidelines were identified. Dietary guidelines from the remaining 86 countries and n = 9 global or regional organizations or authorities (Supplemental Table 1) were screened for eligibility. After the eligibility check, a total of 2 regional organizations were excluded as no snacking-specific recommendations were identified and 37 countries were excluded because 1) guidelines could not be translated (n = 19), 2) no snacking-specific recommendations were identified (n = 17), or 3) recommendations were only for children aged <2 y (n = 1). In total, 143 recommendations for 49 countries and 7 global or regional bodies were included (Figure 1). All references were cross-checked for accuracy in December 2016. Translation was performed through an expert network of nutritionists who were comfortable both with the original language of the document and English. No such experts could be identified for the guidelines that were not translated.
FIGURE 1.
Search overview of available snacking recommendations in food-based dietary guidelines.
Data extraction
Data were extracted for each country including the following: presence or absence of FBDGs, snacking recommendations, year of publication, target population group, and whether a definition of snacking was provided. Where possible, recommendations were classified as either qualitative in nature if the wording related to the quality of the snack (e.g., “healthy” or “nutritious”) or quantitative in nature if the wording or meal-plan examples related to snack quantity (e.g., snacking frequency or calorie content). In addition, any rationale provided in support of the recommendations was recorded (e.g., limiting sugary snacks for dental health benefits). If specific food groups were recommended or discouraged in the recommendations, these were recorded and separated into 1 of 6 categories: “fruit, vegetables and juice,” “starchy foods,” “dairy,” “combinations of foods,” “other foods,” and “foods to limit” (e.g., savory snacks or confectionery). In instances in which the suggested foods involved ≥2 food groups (e.g., meat or cheese sandwich or breakfast cereal and milk), these were described as “combinations of foods.” Food groups outside of these categories (e.g., nuts, seeds, pulses, hummus, eggs) were classed as “other foods.”
Results
Snacking definition
Where snacking recommendations existed, only 5 countries provided a precise definition of snacking. In 4 instances, snacks were defined as foods or drinks consumed between main meals (35–38). In one instance, a caloric value (<150 kcal) was attributed (39). For Mexico, it was also suggested that snacks were usually foods that children could consume by themselves and were convenient and easy to prepare (38).
Global and regional recommendations: numbers identified and target populations
Snacking guidance was published by the WHO, 2 WHO regional offices (Asia and Eastern Mediterranean Region), the FAO in the Caribbean, and one each by Nordic and Mediterranean groups (Table 1) (40–46). Quantitative snacking frequencies for children aged <18 y (1–2 snacks/d) were listed by the WHO Asia Region (41) and for underweight individuals by the WHO East Mediterranean Region (5 small meals with snacks) (40). Qualitative recommendations included examples of snacks to choose, such as fruit and vegetables (fresh or dried) (40, 42, 44), whole-grain–based snacks and cereals (40), “nutritious snacks” (41), and “nutrient-dense snacks” (43, 45). Most organizations gave broad examples of snacks to limit—for example, packaged snacks (46), sugary or salty snacks (40, 42, 43, 45), or foods high in fat (43, 45). Overall, both global WHO recommendations were similar in nature, suggesting examples of snacks to limit (e.g., sugar-containing beverages and snacks) (42, 46), with greater diversity provided in the regional recommendations, which mentioned specific foods to avoid and to include (40, 45) and that were also quantitative in nature (1–2 snacks/d) (40, 41). In contrast, there were no snacking-specific FBDGs identified for the WHO European Region (47) or by the European Food Safety Authority (48). Those recommendations issued for Northern Europe (43) focused on foods to limit, whereas those issued for Southern Europe by the Mediterranean Diet Foundation focused on snacks to choose (e.g., fruit) (44).
TABLE 1.
Overview of snacking recommendations from global or regional authorities
| Authority, year | Countries | Target | Nature |
|---|---|---|---|
| (reference) | reached | population group | of recommendation |
| WHO Eastern Mediterranean Region, 2012 (40) | Afghanistan, Bahrain, Djibouti, Egypt, Iraq, Islamic Republic of Iran, Jordan, Kuwait, Morocco, Occupied Palestinian Territory, Oman, Pakistan, Qatar, Saudi Arabia, Somalia, South Sudan, Sudan, Tunisia, United Arab Emirates, Yemen | All | Quantitative recommendation for underweight (5 small meals and snacks to include high-fat foods) |
| Gives examples of foods to limit (e.g., sweetened beverages and foods, cakes, baklava, cookies, knafeh, confectionery) and snacks to choose (e.g., raw, fresh or dried fruit and vegetables, whole-grain–based snacks and cereals, plain popcorn) | |||
| WHO Asia Region, 2011 (41) | Bangladesh, Bhutan, Cambodia, Democratic People`s Republic of Korea, India, Indonesia, Lao People`s Democratic Republic, Maldives, Malaysia, Myanmar, Nepal, Philippines, Sri Lanka, Thailand, Timor-Leste, Vietnam | Children aged 2–18 y | Quantitative recommendation for number of daily snacks for 2–12 y olds (2/d), 12–18 y olds (1/d); qualitative recommendation for “nutritious snacks” |
| WHO, 2015 (42) | Global | All | Gives examples of snacks to limit (e.g., salty snack foods and sugary snacks) and snacks to choose (raw fruit and vegetables) |
| Nordic Council of Ministers, 2012 (43) | Denmark, Finland, Iceland, Norway, Sweden and the Faroe Islands, Greenland, Åland | All | Gives examples of foods to limit (e.g., savory snacks, foods high in fat and added sugar) for energy density and dental caries risk |
| Mediterranean Diet Foundation, 2016 (44) | Mediterranean regions | All | Recommends fruit, nuts, and seeds for snacks |
| FAO, 2007 (45) | Dominica, Grenada, St. Lucia and St. Vincent, and the Grenadines | All | Recommends reduced consumption of salty and high-fat snacks (e.g., chips and cheese curls) and choice of nutrient-dense snacks |
| WHO, 2003 (46) | Global | All | Links snacking/eating frequency to overweight/obesity; gives examples of foods to limit (e.g., packaged snacks and sugar-sweetened soft drinks) |
Country-specific recommendations: numbers identified and target populations
A total of 136 examples of guidelines specific to snacking and to the consumption of snack foods were identified from 49 unique countries. More than one snacking recommendation was identified in 16 countries. The snacking recommendations from 6 of these countries came from different national bodies [e.g., in Switzerland one of the snacking recommendations came from the Swiss Nutrition Society (49) and the other came from the Federal Office of Public Health (50)]. In other cases, recommendations were issued on a state level rather than on a country level (e.g., India), which explained the multitude of recommendations. Multiple recommendations also existed in order to target different age groups (e.g., New Zealand).
To aid in interpretation, Table 2 summarizes the country-specific recommendations grouped by population age group, with supporting information available in Supplemental Tables 2 and 3. Hence, snacking recommendations were grouped depending on whether they were targeted at children (ages 2–13 y), adolescents (aged >13–17 y), or adults (aged ≥18 y). A fourth group of recommendations was not targeted at any specific population group and so was assumed to be for the “general population.” Within this, some countries (n = 16; e.g., the United States) had tailored recommendations for ≥1 population group, whereas others (n = 14; e.g., Oman) issued a single recommendation for the general population. By using these broad population groupings, it can be observed that most snacking recommendations were targeted at either children aged 2–13 y (64 recommendations from 25 countries) or at the general population (66 recommendations from 41 countries), with much lower numbers targeted specifically at adults aged ≥18 y (15 recommendations from 10 countries) or adolescents (5 recommendations from 5 countries). From the recommendations identified, Asia and the Pacific region appeared to be as active in issuing recommendations as North America and Canada, although the latter focused mainly on recommendations for children. The Middle East was the least active region, with recommendations only for the general population and adults. Broadly, equal (circa 50%) numbers of qualitative and quantitative recommendations were available for all population groups, except for adolescents for whom 75% of the available recommendations were qualitative in nature. Thirteen countries had simultaneously quantitative and qualitative snacking recommendations.
TABLE 2.
Overview of countries surveyed and recommendations identified for each of the population groups1
| Number of countries with | ||||
|---|---|---|---|---|
| Countries with | Qualitative | Quantitative | Rationale for | |
| Region | recommendations, n | recommendations | recommendations | recommendations |
| General population (no age specified) | ||||
| Asia and the Pacific | 10 | 10 | 13 | 6 |
| Europe | 14 | 10 | 12 | 7 |
| Africa and South Africa | 2 | 1 | 1 | 2 |
| North America and Canada | 3 | 7 | 0 | 3 |
| Latin America and the Caribbean | 9 | 6 | 3 | 2 |
| Middle East | 3 | 2 | 1 | 1 |
| Total | 41 | 36 | 30 | 21 |
| Children aged 2–13 y | ||||
| Asia and the Pacific | 5 | 8 | 5 | 4 |
| Europe | 11 | 5 | 15 | 6 |
| Africa and South Africa | 4 | 5 | 1 | 1 |
| North America and Canada | 3 | 12 | 8 | 9 |
| Latin America and the Caribbean | 2 | 2 | 3 | 0 |
| Middle East | 0 | 0 | 0 | 0 |
| Total | 25 | 32 | 32 | 20 |
| Adolescents aged 13–17 y | ||||
| Asia and the Pacific | 1 | 1 | 0 | 0 |
| Europe | 2 | 1 | 1 | 0 |
| Africa and South Africa | 1 | 1 | 0 | 0 |
| North America and Canada | 1 | 1 | 0 | 0 |
| Latin America and the Caribbean | 0 | 0 | 0 | 0 |
| Middle East | 0 | 0 | 0 | 0 |
| Total | 5 | 4 | 1 | 0 |
| Adults aged ≥18 y | ||||
| Asia and the Pacific | 2 | 2 | 1 | 1 |
| Europe | 4 | 2 | 3 | 1 |
| Africa and South Africa | 1 | 2 | 1 | 0 |
| North America and Canada | 1 | 1 | 1 | 1 |
| Latin America and the Caribbean | 1 | 0 | 1 | 0 |
| Middle East | 1 | 1 | 0 | 0 |
| Total | 10 | 8 | 7 | 3 |
| Overall total | 81 | 80 | 70 | 44 |
1Qualitative recommendations included wording related to the quality of a snack or snack example, including names of foods or food groups from which to choose or abstain from as snacks; quantitative recommendations related to snacking frequency, energy or nutrient content, or both. The number of countries searched (n = 198) comprised the following: Asia and the Pacific, including Australia, New Zealand, and Oceanic Islands/Polynesia (n = 38); Europe, including Russia, Ukraine, Georgia, and Turkey (n = 49); Africa and islands (n = 51); Latin American and Caribbean, including Mexico (n = 35); the Middle East (n = 22); and North America and Canada, including Greenland (n = 3).
Country-specific quantitative recommendations
Quantitative recommendations (Table 2) most often related to frequency of snacking throughout the day (∼85% of quantitative recommendations; n = 59), with approximately half of these (n = 30) aimed specifically at children (data not shown). Quantitative guidance was not common in recommendations targeted at adolescents or adults aged ≥18 y. Of all the recommendations, only 2 suggested avoidance of snacks (Brazil and Namibia) (51, 52). In contrast, most (n = 47) quantitative recommendations suggested an intake of 2–3 snacks/d (36–39, 53–76), with recommendations of 1 (53, 69, 77) and 4 snacks/d also noted (60). Less common were prescriptive guidelines suggesting suitable energy or nutrient contents or ranges per snacking occasion (n = 13), with slightly greater numbers targeted at the general population (n = 8) than for children (n = 5). Suggested caloric values for snacks aimed at the general population included <150 kcal/serving (39), <250 kcal/snack (78), or <300 kcal/serving (79). Where caloric ranges were provided, they suggested that energy intakes from snacks (or light meals) should be 5–15% of the daily energy intake per occasion (56, 68, 80–84), with no difference in guidance on energy for children and the general population. From these guidelines, it was observed that quantitative recommendations from countries in the European region tended to give percentage ranges for energy intake from snacks for the general population, children, or both (56, 68, 80, 83, 84), whereas those from Asia and South American regions listed caloric values aimed at the general population (39, 78, 79). Furthermore, 2 recommendations from the European region provided specific quantitative guidance for nutrients. One of these recommendations for children specifically listed approximate values for protein, fat, and carbohydrate in grams for morning and afternoon snacks (3.25, 2.8, and 24 g and 7, 6, and 41 g for morning and afternoon, respectively) (85). For adults, one recommendation provided maximal targets for content of added sugar [<10% of energy intake (EI)], total fat (<30% EI), and saturated fat (<10% EI) (84). None of the quantitative recommendations identified focused specifically on fiber and micronutrients.
Country-specific qualitative recommendations
On examination of the qualitative recommendations (n = 80; Table 2, Supplemental Table 3), 4 themes emerged (Table 3). The most common theme related to recommendations mentioning the words “healthy” or “nutritious” (n = 21) (36, 37, 49, 52, 55, 70, 78, 79, 81, 86–97), which was further expanded in a second theme where the words “nutrient density” or “energy density” were used (n = 5) (37, 87, 94, 98, 99). Recommendations in a third recurring theme (n = 17) related to snacking suitability or moderation, including snacks being “part of a reasonable diet” (54, 55, 86, 90, 100) or complementing, rather than replacing, meals (53, 55, 80, 95, 99, 101–104). A fourth theme (n = 6) was described as “other” because it contained a variety of qualitative recommendations, including avoiding snacks on the basis of taste and preference (55), acting as a role model (89), encouraging children to invent new snacks (106), and rewarding with attention not with treats (95). Food-based qualitative recommendations were often used (e.g., fruit, vegetables and juices, starchy foods, dairy foods, combinations of foods, other foods, foods to limit). Many of these food-based recommendations were not mutually exclusive and co-existed alongside quantitative recommendations or rationales for such recommendations; hence, these will be discussed in more detail later in this review.
TABLE 3.
Examples of the qualitative recommendations identified (n = 80), as grouped into themes and shown by region and age group1
| Theme | Example text | Source regions (recommendations per region, n) | Target age group [recommendations per age group, n] | Source (reference) |
|---|---|---|---|---|
| Healthy/nutritious | “Nutritious snacks”; “healthy snacks” | Asia and the Pacific (7) | General population [9] Children [9] Adolescents [2] Adults [1] | (36, 37, 49, 52, 55, 70, 78, 79, 81, 86–97) |
| Europe (4) | ||||
| Africa and South Africa (4) | ||||
| North America and Canada (5) | ||||
| Latin America and the Caribbean (0) | ||||
| Middle East (1) | ||||
| Nutrient/energy density | “Snacks that are high in nutrients and low in calories”; “nutrient-dense snacks”; “healthy snacks; high in essential nutrients and low in fat and/or sugar”; “ideal snacks provide energy, protein, carbohydrate, vitamins, minerals, dietary fiber and a good balance of dietary fats” | Asia and the Pacific (3) | General population [2] | (37, 87, 94, 98, 99) |
| Europe (0) | Children [2] | |||
| Africa and South Africa (0) | Adolescents [0] | |||
| North America and Canada (1) | Adults [1] | |||
| Latin America and the Caribbean (0) | ||||
| Middle East (1) | ||||
| Moderation/suitability of snack | “Equal distribution of energy intake over the day”; “suitable snacks”; “snacks should be part of a reasonable diet”; “snacks should not replace main meals”; “enjoy snacks moderately”; “alcohol contains calories and may promote snacking” | Asia and the Pacific (7) | General population [6] Children [7] Adolescents [3] Adults [1] | (53–55, 80, 86, 90, 95, 99–105) |
| Europe (5) | ||||
| Africa and South Africa (2) | ||||
| North America and Canada (3) | ||||
| Latin America and the Caribbean (0) | ||||
| Middle East (0) | ||||
| Other | “Do not choose snacks only based on the taste and preference”; “according to the needs of physical or learning activities, take snacks in the right amount between meals, but not too often every day”; “encourage kids to invent new snacks”; “whole grains can be healthy snacks: be good role models”; “rewarding with sweet desserts or snacks may encourage them to think that treats are better than other foods. Comfort and reward with care and praise not food” | Asia and the Pacific (3) | General population [1] Children [4] Adolescents [1] Adults [0] | (55, 89, 95, 106) |
| Europe (0) | ||||
| Africa and South Africa (0) | ||||
| North America and Canada (3) | ||||
| Latin America and the Caribbean (0) | ||||
| Middle East (0) |
1Single reference sources may have contained ≥1 recommendation; hence, numbers of recommendations and references do not tally.
Overall, within each qualitative theme, recommendations were more likely to arise from countries in the Asia and the Pacific region than for any other region, with 37–60% of recommendations within any individual theme from the Asian regions. Recommendations from European countries were more likely to fit within the theme suggesting moderation in snack intake and referring to suitable snacks (25% of recommendations within the “moderation/suitability of snacks” theme). Finally, most recommendations within any one theme were targeted at children and at the general population, except for recommendations within the theme “other,” which were more likely to be targeted at children (e.g., focusing on foods as rewards).
Country-specific recommendations specifically listing foods to choose or limit
As mentioned, specific foods or drinks were regularly suggested as part of qualitative or quantitative recommendations or the rationale for particular snacking habits. Given the wide breadth of foods listed in the guidelines, a record was kept of each food or food category and was described as “fruit, vegetables and juice,” “starchy foods,” “dairy,” “combinations of foods,” “other foods,” or “foods to limit.” Across recommendations (Supplemental Table 3), “fruits, vegetables and juices” were most frequently mentioned (n = 67), followed by “starchy foods” (n = 29; e.g., bread, whole grains, crackers, oatcakes, rice, yams, potatoes, pastas, plain popcorn) and “dairy products” (n = 43; e.g., milk, cheese, or yogurt). A further 53 acknowledged “combinations of food groups” and 40 acknowledged “other foods.” Examples of “combinations of foods” included vegetables and dip or dairy, fruit and dairy, or starch and dairy (e.g., cheese sandwich). “Other foods” included nuts or seeds, hummus, or eggs. Furthermore, 70 of all recommendations identified listed specific foods (e.g., confectionery, chocolates) or characteristics of foods to avoid or limit (e.g., foods high in fat, sugar, salt, or saturated or trans fat or ultraprocessed foods). Hence, substantial variation existed between countries with respect to specific foods listed. Table 4 provides a short summary of the most commonly repeated snacks. It is noticeable that substantial variability also existed within countries, depending on the organizations that commissioned the recommendations. For instance, in Brazil, 2 recommendations that targeted children were identified: one recommends fruit, vegetables, and juice, whereas the second did not and focuses instead on “foods to limit” (51, 76). The same pattern was seen in other countries with guidelines focusing more on foods to limit or foods to promote. Variability also existed between guidelines for different age groups [e.g., in New Zealand, the Ministry of Health provided guidelines to children and young people (99), older people (87), and healthy adults (97)]. Despite differences in how the messages were worded and presented, antagonistic statements in the guidelines were not a common finding, even when they were issued from different governing bodies.
TABLE 4.
Overview of most commonly repeated snacks to promote and to limit
| Snacks to promote | Snacks to limit |
|---|---|
| Vegetables (no condition) | High-sodium and/or -fat foods (e.g. salty biscuits, crisps, salted nuts) |
| Fruit1 (raw, fresh, dried) | High-sugar and/or -fat foods (e.g. biscuits, cakes, chocolate, candy bars, sugar, confectionery) |
| Dairy (no-fat/low-fat milk, cheese, yogurt) | High-sugar drinks1 |
| Starchy foods (e.g., bread, whole grains, crackers, oatcakes, rice, yams, potatoes, pastas, plain popcorn) | Fried foods |
| Combinations of foods (e.g., vegetables and dip/dairy, fruit and dairy, starch and dairy) | |
| Nuts/seeds (unsalted) |
1100% fruit juices were mentioned both in snacks to promote and snacks to limit.
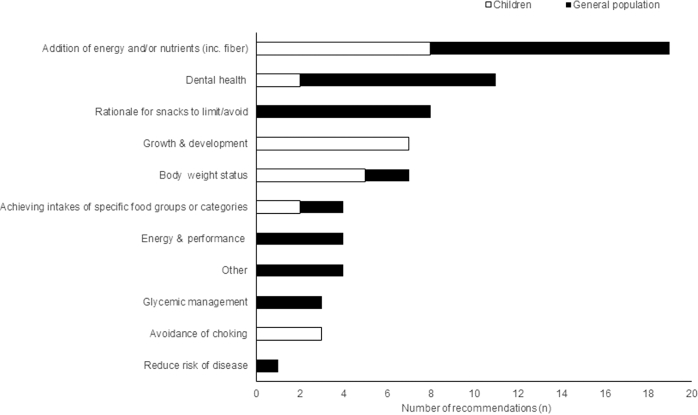
Rationales for global, regional, and country-specific recommendations
In total, 50 unique recommendations provided ≥1 rationale for the snacking guidance, with 44 from national organizations (Table 2) and 6 from global or regional organizations. Figure 2 provides a summary of the diversity of rationales suggested, for children and for the general population (with details provided in Supplemental Table 4). Across the globe, the most frequent rationale (n = 19) suggested snacking as a way to contribute to energy or nutrient intake (including fiber) for both children (n = 8) and the general population (n = 11) (36, 37, 40, 43, 52, 53, 72, 78, 82, 85, 87, 100, 102, 107), with examples of supporting text including “snacking can add vitamins, minerals and other nutrients to the diet” (78) and “snacks make a valuable contribution to energy and nutrient intake between main meals” (37). The second most- frequent rationale (n = 11) related to dental health, with these messages again targeted at both the general population and children—for example, “to reduce dental decay, restrict the frequency of eating foods and drinking beverages with a high sugar content” (97) and avoid sugary snacks to have “less problems with dental caries/tooth decay” (108). Although recommendations relating to growth and development (n = 7) and avoidance of choking (n = 3) were solely aimed at children, recommendations relating to reduced risk of disease (n = 1), improved glycemic management (n = 3), and rationale for foods to limit or avoid as snacks (n = 8) were targeted at adults. Examples of these latter rationales included “benefits of less salty snacks: good control of blood pressure, decreased risk of heart and blood vessel diseases” (108) or “because of their ingredients, ultra-processed foods—such as packaged snacks, soft drinks, and instant noodles—are nutritionally unbalanced” (51). Recommendations within the category “other” (n = 4) ranged from “fulfilling social needs” (78) to “respecting the body” (109).
FIGURE 2.
Summary schematic of the rationale provided for snacking recommendations globally by target population group. inc, including.
There was some heterogeneity observed in the specific rationale of the recommendations depending on geography. For example, Caribbean countries were more likely to focus on reduced consumption of salted snacks in the context of controlling blood pressure and reducing the risk of diseases of the heart and blood vessels (108, 110–112), whereas Oman focused on salt and trans FAs as risk factors for hyperlipidemia (98). Furthermore, countries outside of the European and North American regions were more likely to feature body weight status—for example, “Use local fruits and vegetables for snacks instead of sugary snacks” as providing “better weight control” (St. Kitts and Nevis) (112) and Oman’s recommendations link an increase in snacking to rising rates of overweight and obesity (98). Although global recommendations make reference to snacks in the context of overweight and obesity, regional WHO recommendations allude to the role of snacks in underweight individuals as well (40, 42, 46). Collectively, this suggests that countries and authorities have different focuses depending on the perceived role of snacking and relative value of nutrients or health states.
Finally, across the range of qualitative or quantitative recommendations and their supporting rationales identified, it was observed that specific foods were more often mentioned in association with qualitative recommendations as being “healthy” or “nutritious” or as “foods to limit” (e.g., choose healthy foods such as fruit, salads, and vegetables for snacks; don't eat salty snacks like crisps every day) (86). In contrast, when a rationale was provided, it was more likely to also mention specific nutrients contained within the foods and their relation with health (e.g., dairy foods are a great source of calcium, which helps to build strong bones and teeth; most calcium is obtained from milk and other dairy products) (36).
Discussion
To our knowledge, this is the first comprehensive review of snacking recommendations globally. This review highlights that there is considerable variation in the nature of the recommendations and in the level of detail presented, both within and between countries and regions.
Since 1992, the FAO and WHO have promoted the use of FBDGs to improve dietary practices and reduce diet-related public health problems (33, 113). Despite their efforts to promote the proliferation of FBDGs (114), our analysis, like others, shows that a large number of countries (57% of the countries surveyed in this analysis) do not have easily identifiable official dietary guidelines (115). Nonetheless, snacking seems to be a prominent topic, with more than half of the countries that issue guidelines (n = 49) having ≥1 or even several recommendations on the topic. Still, guidelines vary considerably on what is a snack and what its role is in the diet, if any. It is still unclear whether the variations among guidelines stem from a gap of scientific evidence or how the evidence is translated into FBDGs, or whether the guidelines require modification on the basis of country-specific public health nutrition needs (33).
In the absence of any consensus definition of what constitutes a snack (9, 23, 24), this review was structured to first identify the presence or absence of any snacking recommendations and, second, to try and understand the nature of the recommendations identified and whether they varied by population and region. By using this structure, we observed that snacking guidance was typically targeted at younger children and at the general population, with a greater presence of such guidelines in the broader Asian, European, and US regions; guidance for adolescents and in regions such as Africa, Latin America, and the Middle East was less commonly found. This adds to recent research, which reported that lower income and African countries were less likely to have guidelines (115). Of particular note was the very limited targeted guidance for adolescents, given both the increased nutritional requirements characteristic of this life stage coupled with other lifestyle factors that can influence food choice and nutrient intake (e.g., exams, sports, or fear of fatness) (116).
When the identified recommendations were classified as being related to the quality of snack foods (qualitative) or to the quantity of snack foods consumed (quantitative), it became apparent that overall broadly equal numbers of both types of recommendation existed (∼50%), but not always in parallel. This may reflect the fact that recommendations may have different target audiences; quantitative recommendations are reported to be useful for health professionals and policy makers, whereas qualitative recommendations are useful for the public (33). However, even within the recommendation types, considerable variance was observed. For example, nearly as many qualitative recommendations were identified that were related to “healthy/nutritious” (n = 21) as for “snack suitability and/or moderation” (n = 17). Furthermore, there were also a considerable number of qualitative recommendations (n = 11 in total), which provided guidance ranging from nutrient or energy density to the use of foods as rewards. This may suggest that dietary guidance on snacking reflects national health priorities. It may also acknowledge the different aspects of food intake insofar as multiple factors influence food choice. However, this also results in multiple messages that could be viewed, in some instances, as positive (“gain framed”) or negative (“loss framed”) in nature (e.g., choice of healthy snacks compared with avoidance of unhealthy snacks) and, in some instances, listed concurrently (55, 86, 95). It has been suggested that “gain framed” messages are more effective with the general population, whereas “loss framed” messages are more likely to succeed with health professionals (117). In the context of FBDGs, original FAO/WHO advice suggested that “dietary guidelines need to be positive and encourage enjoyment of appropriate dietary intakes” (33). Collectively, this suggests that snacking messages should be tailored to the intended audience to ensure greater responsiveness and compliance to dietary goals, with more positive “gain framed” qualitative messages more likely to succeed with the general public (117).
Within the quantitative recommendations provided, there was greater agreement as to an acceptable frequency of snack intake and suitable nutritional criteria. Where stated, most countries recommended consuming 2 snacks/d (54%), but recommendations also varied from none to 3 and 4 snacks/d. It was typically unclear whether the recommended snacking frequency was based on actual consumption patterns identified from national food consumption surveys, published studies, or expert opinion accounting for life stage, cultural norms, and working environments. Unsurprisingly, half of these recommendations were targeted at children because of their high energy requirements to support growth and development (118). However, the remainder were targeted at other life stages, suggesting that most FBDGs globally acknowledge, at least subtly, that there is a role for snacking at all ages. Where provided, suitable energy contents for snacks ranged from 150 to 300 kcal/d for adults to 5–15% of total daily energy intake for children and adults, as described earlier. Of note, this concurs with the many definitions of snacks as used in the scientific literature in which snacks have been defined as <15% of total daily energy intake (11, 119, 120) or ≥210 kJ (50 kcal) (26). Quantitative guidance for intakes of macronutrients (e.g., fat and saturated fat) was identified, perhaps reflecting published articles that linked energy-dense snack foods and beverages with excess intakes of these nutrients or unfavorable dietary patterns (16, 119, 121). However, scientific research on the contribution of snacks to fiber and micronutrients did not appear to be translated to specific recommendations (122–124). The potential of introducing snacks formulated to address micronutrient insufficiencies globally has previously been identified (9) and merits further consideration.
Considerable effort was made during this review to detail examples of the foods and food categories that were encouraged to include or exclude as snacks and any rationale provided. Unsurprisingly, “fruit, vegetables and juice,” “starchy foods,” and “dairy foods” were most frequently recommended; and foods high in fat, saturated fat, salt, or sugar were proposed to be restricted. There was no clear pattern with respect to the specific food examples given. Some countries and organizations listed names of specific foods to include or limit (37, 40, 50, 53, 79, 97, 108), whereas others simply mentioned broad categories (42, 43, 46, 98). Advice to choose foods “low” in sugar or salt was also common, but no quantitative benchmark was provided to define whether a food would be “high” or “low” in a particular nutrient (37, 98).
All supporting rationale statements were grouped into 1 of 11 categories, with the most frequent rationale listing the ability of snacks to contribute to energy and nutrient intake followed by the influence of snacks on dental health. This reflects published studies, which have tended to focus on the contribution of snacks to nutrient intake, energy density, and dietary quality (121–124, 125) or on the influence of dietary components on dental health (126). Greater variation was observed with respect to other rationales provided, with few recommendations providing rationales for health-related conditions such as body weight status, glycemia, and heart health. Such variation likely mirrors a lack of consensus in the literature in which snacking has been reported to have benefits for heart health (20–22) but to have a less clear relation with adiposity and body weight status (2, 3, 120, 125). It has also been suggested that any relation between snack choices and weight status may be dependent on the pre-existing health status of the individual (127). To date, there has been no systematic review of studies examining if a relation exists between snack choices and health outcomes. Such an analysis would be helpful not only for research but also to provide practical guidance to the public.
Strengths of this review include the extensive nature of the search and systematic approach to describing and cross-checking the data. It builds on previous work, which provides useful insight of snacking recommendations in English-speaking countries (9), and it is hoped that such analysis will generate discussion on the role of snacks in the diet and to provide guidance to stakeholders, ranging from health professionals to the food industry. Limitations include the reliance on identifying recommendations in English and the use of local translation where necessary. It is also possible that countries had guidelines that were not identified due to language and cultural barriers. Limitations of the approach taken to classify the identified recommendations in terms of themes and rationales are also acknowledged. However, this approach was necessary to combine the aim of the review with the volume of data generated.
In conclusion, this review provides a comprehensive snapshot of snacking recommendations worldwide. On the basis of our findings, the terms “snack” and “snacking” are used interchangeably to describe calories coming from foods or beverages consumed in-between main meals. Each of these “snacks” provides ∼10% of daily energy, with a most commonly recommended frequency of 2 “snacks”/d. Although snack foods are derived from all food groups (e.g., dairy, fruit, vegetables), guidelines distinguish between snacks to limit and snacks to promote, with the former being nutrient-poor and energy-dense foods (e.g., high in SFAs, high sugar, high sodium, treats), whereas the latter focuses on nutrient density (including fiber-rich foods).
It is hoped that this analysis will stimulate further research and discussion to better understand the role of different snacking patterns and choices on diet quality. A first step toward this would be achieving a consensus definition of the terms snack, snacking, and snack foods to help align guidelines and dietary intake research. Such actions will be helpful for the general public, health care professionals, and discussions with other stakeholders.
Supplementary Material
Acknowledgments
We thank Frank Thielecke and Anne Nugent for editorial assistance. All authors read and approved the final manuscript.
Notes
Author disclosures: MP and UL are employed by Nestec Ltd. AV was employed by Nestec at the time the analysis was carried out.
Supported by Nestec Ltd.
Supplemental Tables 1–4 are available from the “Supplementary data” link in the online posting of the article and from the same link in the online table of contents at https://academic.oup.com/advances/.
References
- 1. Duffey KJ, Pereira RA, Popkin BM. Prevalence and energy intake from snacking in Brazil: analysis of the first nationwide individual survey. Eur J Clin Nutr 2013;67(8):868–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Duffey KJ, Popkin BM. Energy density, portion size, and eating occasions: contributions to increased energy intake in the United States, 1977–2006. PLoS medicine 2011;8(6):e1001050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Duffey KJ, Popkin BM. Causes of increased energy intake among children in the U.S., 1977–2010. Am J Prev Med 2013;44(2):e1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Garriguet D. Canadians' eating habits. Health Reports 2007;18(2):17–32. [PubMed] [Google Scholar]
- 5. Piernas C, Popkin BM. Snacking increased among U.S. adults between 1977 and 2006. J Nutr 2010;140(2):325–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wang Z, Zhai F, Zhang B, Popkin BM. Trends in Chinese snacking behaviors and patterns and the social-demographic role between 1991 and 2009. Asia Pac J Clin Nutr 2012;21(2):253–62. [PMC free article] [PubMed] [Google Scholar]
- 7. Kerr MA, Rennie KL, McCaffrey TA, Wallace JM, Hannon-Fletcher MP, Livingstone MB. Snacking patterns among adolescents: a comparison of type, frequency and portion size between Britain in 1997 and Northern Ireland in 2005. Br J Nutr 2009;101(1):122–31. [DOI] [PubMed] [Google Scholar]
- 8. Bellisle F, Dalix AM, Mennen L, Galan P, Hercberg S, de Castro JM, Gausseres N. Contribution of snacks and meals in the diet of French adults: a diet-diary study. Physiol Behav 2003;79(2):183–9. [DOI] [PubMed] [Google Scholar]
- 9. Hess JM, Jonnalagadda SS, Slavin JL. What Is a Snack, Why Do We Snack, and How Can We Choose Better Snacks? A Review of the Definitions of Snacking, Motivations to Snack, Contributions to Dietary Intake, and Recommendations for Improvement. Adv Nutr 2016;7(3):466–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Murakami K, Livingstone MB. Energy density of meals and snacks in the British diet in relation to overall diet quality, BMI and waist circumference: findings from the National Diet and Nutrition Survey. Br J Nutr 2016;116(8):1479–89. [DOI] [PubMed] [Google Scholar]
- 11. Murakami K, Livingstone MB. Associations between meal and snack frequency and overweight and abdominal obesity in US children and adolescents from National Health and Nutrition Examination Survey (NHANES) 2003–2012. Br J Nutr 2016;115(10):1819–29. [DOI] [PubMed] [Google Scholar]
- 12. Taillie LS, Afeiche MC, Eldridge AL, Popkin BM. Increased Snacking and Eating Occasions Are Associated with Higher Energy Intake among Mexican Children Aged 2–13 Years. J Nutr 2015;145(11):2570–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Roos E, Prattala R. Meal pattern and nutrient intake among adult Finns. Appetite 1997;29(1):11–24. [DOI] [PubMed] [Google Scholar]
- 14. Murakami K, Livingstone MB. Meal and snack frequency in relation to diet quality in US children and adolescents: the National Health and Nutrition Examination Survey 2003–2012. Public Health Nutr 2016;19(9):1635–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Zizza CA. Snacking is associated with overall diet quality among adults. J Acad Nutr Diet 2012;112:291–6. [DOI] [PubMed] [Google Scholar]
- 16. Murakami K, Livingstone MB. Associations between energy density of meals and snacks and overall diet quality and adiposity measures in British children and adolescents: the National Diet and Nutrition Survey. Br J Nutr 2016;116(9):1633–45. [DOI] [PubMed] [Google Scholar]
- 17. Yannakoulia M, Melistas L, Solomou E, Yiannakouris N. Association of eating frequency with body fatness in pre- and postmenopausal women. Obesity (Silver Springs) 2007;15(1):100–6. [DOI] [PubMed] [Google Scholar]
- 18. Hampl JS, Taylor C. A.. Snacking patterns influence enrgy and nutrient itnakes but not body mass index. J Hum Nutr Diet 2003;16:3–11. [DOI] [PubMed] [Google Scholar]
- 19. Holmback I, Ericson U, Gullberg B, Wirfalt E. A high eating frequency is associated with an overall healthy lifestyle in middle-aged men and women and reduced likelihood of general and central obesity in men. Br J Nutr 2010;104(7):1065–73. [DOI] [PubMed] [Google Scholar]
- 20. Smith KJ, Blizzard L, McNaughton SA, Gall SL, Dwyer T, Venn AJ. Daily eating frequency and cardiometabolic risk factors in young Australian adults: cross-sectional analyses. Br J Nutr 2012;108(6):1086–94. [DOI] [PubMed] [Google Scholar]
- 21. Bhutani S, Varady KA. Nibbling versus feasting: which meal pattern is better for heart disease prevention? Nutr Rev 2009;67(10):591–8. [DOI] [PubMed] [Google Scholar]
- 22. Edelstein SL, Barrett-Connor EL, Wingard DL, Cohn BA. Increased meal frequency associated with decreased cholesterol concentrations; Rancho Bernardo, CA, 1984–1987. The American journal of clinical nutrition 1992;55(3):664–9. [DOI] [PubMed] [Google Scholar]
- 23. Leech RM, Worsley A, Timperio A, McNaughton SA. Understanding meal patterns: definitions, methodology and impact on nutrient intake and diet quality. Nutr Res Rev 2015;28(1):1–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Leech RM, Worsley A, Timperio A, McNaughton SA. Characterizing eating patterns: a comparison of eating occasion definitions. Am J Clin Nutr 2015;102(5):1229–37. [DOI] [PubMed] [Google Scholar]
- 25. Ritchie LD. Less frequent eating predicts greater BMI and waist circumference in female adolescents. Am J Clin Nutr 2012;95(2):290–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Gibney MJ, Wolever TM. Periodicity of eating and human health: present perspective and future directions. Br J Nutr 1997;77 Suppl 1:S3–5. [DOI] [PubMed] [Google Scholar]
- 27. Lipoeto NI, Geok Lin K, Angeles-Agdeppa I. Food consumption patterns and nutrition transition in South-East Asia. Public Health Nutr 2013;16(9):1637–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Nicklas TA, Yang SJ, Baranowski T, Zakeri I, Berenson G. Eating patterns and obesity in children. The Bogalusa Heart Study. Am J Prev Med 2003;25(1):9–16. [DOI] [PubMed] [Google Scholar]
- 29. Jennings A, Cassidy A, van Sluijs EM, Griffin SJ, Welch AA. Associations between eating frequency, adiposity, diet, and activity in 9–10 year old healthy-weight and centrally obese children. Obesity (Silver Spring) 2012;20(7):1462–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Wansink B, Payne CR, Shimizu M. “Is this a meal or snack?” Situational cues that drive perceptions. Appetite 2010;54(1):214–6. [DOI] [PubMed] [Google Scholar]
- 31. Chamontin A, Pretzer G, Booth DA. Ambiguity of ‘snack’ in British usage. Appetite 2003;41(1):21–9. [DOI] [PubMed] [Google Scholar]
- 32. Marshall D, Bell R. Meal construction: exploring the relationship between eating occasion and location. Food Qual Pref 2003;14:53–64. [Google Scholar]
- 33. FAO/WHO. Preparation and Use of Food-Based Dietary Guidelines. In: WHO , ed. WHO Technical Report Series Geneva: FAO/WHO, 1998, 4. [PubMed] [Google Scholar]
- 34. FAO. Food-based dietary guidelines 2017[cited 2017 Sept 4]. Available from: http://www.fao.org/nutrition/nutrition-education/food-dietary-guidelines/en/.
- 35. Ministry of Health Malaysia My Health for Life. MyHealth 2015. [cited 2015 Jul 20] Available from: http://myhealth.gov.my/index.php/en/oral-health/general/snacking. [Google Scholar]
- 36. Ministry of Health, National Food and Nutrition Centre Food and Health Guidelines for Fiji. Fiji; 2013[cited 2015 Jul 20] Available from: http://www.fao.org/3/a-as883e.pdf. [Google Scholar]
- 37. Ministry of Health Food and Nutrition Guidelines for Healthy Children and Young People (Aged 2–18 years): A background paper. healthgovtnz; 2012. [cited 2015 Jul 8] Available from http://www.health.govt.nz/system/files/documents/publications/food-nutrition-guidelines-healthy-children-young-people-background-paper-feb15-v2.pdf. [Google Scholar]
- 38. Secretaria de salud NORMA Oficial Mexicana NOM-043-SSA2-2012, Servicios básicos de salud. Promoción y educación para la salud en maeria alimentaria. Criterios para brindar orientacion. Diario Oficial; 2013. [Google Scholar]
- 39. Universidad de Chile and Ministry of Health Feeding Guide for Children under 2 years of age, Feeding Guide for children up to adolescence. 2005. [cited 2015 Jan 20]. Available from: https://www.inta.cl/Consumidores/Revistas/guia_menor_de_2.pdf. [Google Scholar]
- 40. WHO Regional Office for the Eastern Mediterranean Promoting a healthy diet for the WHO Eastern Mediterranean Region. User-friendly guide. Cairo: The WHO; 2012. [cited 2015 Jul 10]. Available from: http://applications.emro.who.int/dsaf/emropub_2011_1274.pdf?ua=1. [Google Scholar]
- 41. WHO Regional Consultation on Food-Based Dietary Guidelines for countries in the Asia Region. World Health Organization; 2011. [cited 2015 July 10]. Available from: http://apps.searo.who.int/PDS_DOCS/B4818.pdf. [Google Scholar]
- 42. WHO Healthy Diet Fact sheet N°394. World Health Organization, 2015. [cited 2016 Dec 12]. Available from: http://www.who.int/mediacentre/factsheets/fs394/en/. [Google Scholar]
- 43. Nordic Council of Ministers Nordic Nutrition Recommendations 2012 Integrating nutrition and physical activity. 5th edition ed Copenhagen, 2012. [cited 2016 Dec 12]. Available from: http://norden.diva-portal.org/smash/get/diva2:704251/FULLTEXT01.pdf. [Google Scholar]
- 44. Mediterranean Diet Foundation Mediterranean Diet Pyramid: a lifestyle for today. Guidelines for healthy adults. 2016. [cited 2016 Dec 12]. Available from: http://dietamediterranea.com/nutricion-saludable-ejercicio-fisico/#pyramid. [Google Scholar]
- 45. FAO Developing Food Based Dietary Guidelines. A Manual from the English Speaking Carribean. FAO, 2007. [cited 2016 Dec 19]. Available from: ftp://ftp.fao.org/docrep/fao/010/ai800e/ai800e00.pdf. [Google Scholar]
- 46. WHO Diet, Nutrition and the Prevention of Chronic Diseases. World Health Organisation Technical Report Series No 916; Geneva, 2003. [cited 2016 Dec 12]. Available from: http://apps.who.int/iris/bitstream/10665/42665/1/WHO_TRS_916.pdf. [PubMed] [Google Scholar]
- 47. WHO Food Based Dietary Guidelines in the WHO European Region. Copenhagen: WHO Regional Office for Europe, 2003. [cited 2016 Dec 12]. Available from: http://www.euro.who.int/__data/assets/pdf_file/0017/150083/E79832.pdf. [Google Scholar]
- 48. EFSA Food-Based Dietary Guidelines. EFSA Journal; 2010. [cited 2017 Sept 4]. Available from: http://www.efsa.europa.eu/en/efsajournal/pub/1460. [Google Scholar]
- 49. Schweizerische Gesellschaft für Ernährung SGE Ernährung von Kindern. 2011. [cited 2015 Jul 13]. Available from: www.sge-ssn.ch/media/merkblatt_ernaehrung_von_kindern_2011_4.pdf. [Google Scholar]
- 50. Bundesamt für Gesundheit Conseils pour des dix-heueres et des gouters sains. 2012. [cited 2015 Jul 13]. Available from: http://www.sge-ssn.ch/media/sb_znueniblatt_2012_en_web.pdf. [Google Scholar]
- 51. Ministry of Health of Brazil Dietary Guidelines for the Brazilian population In: Ministry of Health of Brazil, Secretariat of Health Care, Primary Health Care Department, ed. Brazil: Ministry of Health, 2014. [cited 2016 Dec 12]. Available from: http://189.28.128.100/dab/docs/portaldab/publicacoes/guia_alimentar_populacao_ingles.pdf. [Google Scholar]
- 52. Ministry of Health and Social Services Food and Nutrition Guidelines for Namibia. Namibia: 2000. [cited 2016 Dec 8]. Available from: http://www.fao.org/3/a-as839e.pdf. [Google Scholar]
- 53. National Institute of Nutrition Dietary Guidelines for Indians - A Manual 2011. [cited 2015 July 20]. Available from: http://ninindia.org/DietaryGuidelinesforNINwebsite.pdf. [Google Scholar]
- 54. Chinese Nutrition Society and Ministry of Health Food-based dietary guidelines - China. 2015. [cited 2015 Jul 20]. Available from: http://dg.en.cnsoc.org/. [Google Scholar]
- 55. National Institute for Nutrition and Health Chinese Center for Disease Control and Prevention. Chinese children and adolescents snacking guidance China Nutrition, 2008. [cited 2015 Aug 24]. Available from: http://www.chinanutri.cn/yyjkzxpt/yyjkkpzx/xcclk/xinxi/201501/t20150115_109864.html. [Google Scholar]
- 56. Department of Public Health Recommendations on Healthy Nutrition in Albania. 2008. [cited 2015 Jul 23]. Available from: http://www.fao.org/3/a-as658e.pdf. [Google Scholar]
- 57. Health Canada Canada's Food Guide. Ottawa, Ontario: Health Canada, 2011. [cited 2016 Dec 19]. Available from: http://www.hc-sc.gc.ca/fn-an/alt_formats/hpfb-dgpsa/pdf/food-guide-aliment/view_eatwell_vue_bienmang-eng.pdf. [Google Scholar]
- 58. Centre for Chronic Disease Control Sample Menu - Northern India. 2006. [cited 2015 Jul 13] Available from: http://foodpyramidindia.org/sm-northern.html. [Google Scholar]
- 59. Centre for Chronic Disease Control Sample menu - Southern India. 2006. [cited 2015 Jul 13]. Available from: http://foodpyramidindia.org/sm-southern.html. [Google Scholar]
- 60. Centre for Chronic Disease Control Sample Menu - Western India. 2006. [cited 2015 Jul 13]. Available from: http://foodpyramidindia.org/sm-gujarati.html. [Google Scholar]
- 61. Centre for Chronic Disease Control D Sample Menu - Assam. 2006. [cited 2015 Jul 13]. Available from: http://foodpyramidindia.org/sm-assam.html. [Google Scholar]
- 62. Centre for Chronic Disease Control Sample Menu - Jain. 2006. [cited 2015 Jul 13]. Available from: http://foodpyramidindia.org/sm-jain.html. [Google Scholar]
- 63. Centre for Chronic Disease Control Northern India Food Guide. 2006. [cited 2015 Jul 13]. Available from: http://foodpyramidindia.org/fghl-north-india.html. [Google Scholar]
- 64. Centre for Chronic Disease Control Southern India. 2006. [cited 2015 Jul 13]. Available from: http://foodpyramidindia.org/fghl-south-india.html. [Google Scholar]
- 65. Centre for Chronic Disease Control Western India. 2006. [cited 2015 Jul 13]. Available from: http://foodpyramidindia.org/fghl-western-india.html. [Google Scholar]
- 66. Centre for Chronic Disease Control Assam. 2006. [cited 2015 Jul 13]. Available from: http://foodpyramidindia.org/fghl-northern-india.html. [Google Scholar]
- 67. Centre for Chronic Disease Control Jain Food Guide. 2006. [cited 2015 Jul 13]. Available from: http://foodpyramidindia.org/fghl-jain-india.html. [Google Scholar]
- 68. Faculty of Food Sciences University of Porto and National Council for Food and Nutrition MoH Food-based dietary guidelines – Portugal. 2003. [cited 2016 Dec 17]. Available from: www.fao.org/3/a-ax4330.pdf. [Google Scholar]
- 69. Institut national de prévention et d'éducation pour la santé. La santé vient en mangeant Le guide alimentaire pour tous. In: santé. Indpedépl, ed. Vanves: INPES, 2011. [cited 2016 Dec 19]. Available from: http://inpes.santepubliquefrance.fr/CFESBases/catalogue/pdf/581.pdf. [Google Scholar]
- 70. Ministry of Health National Nutrition Guidelines for Malawi. 2007. [cited 2015 Aug 25]. Available from: http://www.unicef.org/malawi/MLW_resources_nutritionguidelines.pdf. [Google Scholar]
- 71. Ministry of Health Dietary guidelines for Turkey. 2006. [cited 2016 Dec 17]. Available from: http://www.fao.org/nutrition/education/food-dietary-guidelines/regions/countries/turkey/en/. [Google Scholar]
- 72. US Department of Agriculture; US Department of Health and Health Services Scientific report of the 2015 Dietary Guidelines Advisory Committee. Washington (DC): 2015. [cited 2016 Dec 17]. Available from: https://health.gov/dietaryguidelines/2015/guidelines/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Ministry of Health Food-based dietary guidelines - Croacia. [cited 2016 Jul 27]. Available from http://www.fao.org/3/a-as670o.pdf. [Google Scholar]
- 74. Bundesministerium für Gesundheit GESUNDHEIT: öffentliches Gesundheitsportal österreichs. Die gesunde Mahlzeit, 2014. [cited 2015 May 5]. Available from: https://www.gesundheit.gv.at/Portal.Node/ghp/public/content/Gesunde_MahlzeitLN.html. [Google Scholar]
- 75. AID Artikel zum Thema aid-Ernährungspyramide. aid, 2013. [cited 2015 Feb 13]. Available from: http://www.aid.de/inhalt/wann-esse-ich-986.html. [Google Scholar]
- 76. Departamento Cientifico de Nutrologia Sociedade Brasileira de Pediatria Lanche Saudável - Manual de orientação. Sao Paulo, 2012. [Google Scholar]
- 77. Federal Public Service Health, Food Chain Safety and Environment Guide 2. Vivement recommandé pour enfants de 3 à 12 et leurs parents. 2005b. [cited 2016 Dec 17]. Available from: http://www.fao.org/3/a-as666f.pdf. [Google Scholar]
- 78. Ministry of Health Malaysia Healthy Snack. My Health 2008. [cited 2017 Jan 25]. Available from: http://myhealth.gov.my/index.php/en/healthy-snacks. [Google Scholar]
- 79. Nutrition Division, Ministry of Health Food based dietary guidelines for Sri Lankans. 2011. [cited 2015 Jul 20]. Available from: www.fao.org/3/a-as886e.pdf. [Google Scholar]
- 80. Russian Ministry of Health Guidelines on preventive measures for health protection and promotion of pupils/students in educational institutions. Russia: 2008. [cited 2015 Sept 26]. Available from: http://www.rosminzdrav.ru/documents/7768-rekomendatsii-206-vs-ot-15-yanvarya-2008-g. [Google Scholar]
- 81. British Nutrition Foundation Healthy Snacking. Nutrition, 2015. [cited 2015 Jul 8]. Available from: http://www.nutrition.org.uk/healthyliving/healthyeating/snacking.html?limitstart=0. [Google Scholar]
- 82. British Nutrition Foundation Putting it into practice. Nutrition, 2015. [cited 2015 Jul 8]. Available from: https://www.nutrition.org.uk/healthyliving/healthyeating/practice.html. [Google Scholar]
- 83. Ukranian Ministry of Health Guidelines for general practitioners and family doctors on recommending to patients the basic principles of healthy nutrition. 2013. [cited 2015 Sept 26] Available from: http://www.moz.gov.ua/ua/portal/dn_20130114_0016.html. [Google Scholar]
- 84. DTU Food, National Food institute Guidelines for Healthy Snacks. Denmark: 2012. [cited 2017 Feb 24]. Available from: http://www.food.dtu.dk/english/news/2012/04/guidelines_for_healthy_snacks?id=38ef277c-d365-4cb9-be4a-2a9b5e56e3bd. [Google Scholar]
- 85. Canedeias VNE, Morais C, Cabral M, Ribeiro da Silva P. Principos para uma Alimentacao Saudavel. Lisboa: Portuguese Office of Health (POH) (Direção Geral de Saúde – DGS), 2005. [Google Scholar]
- 86. Healthy Ireland and Department of Health and Children The Food Pyramid. Healthy Ireland; 2016[cited 2016 Dec 17]. Available from: http://www.healthyireland.ie/wp-content/uploads/2016/12/M9617-DEPARTMENT-OF-HEALTH_Food-Pyramid-Poster_Complex-Version.pdf. [Google Scholar]
- 87. Ministry of Health Food and Nutrition Guidelines for Healthy Older People: A background paper. Healthgov New Zealand; 2013[cited 2015 Jul 29]. Available from: http://www.health.govt.nz/system/files/documents/publications/food-nutrition-guidelines-healthy-older-people-background-paper-v2.pdf. [Google Scholar]
- 88. Department of Health, Republic of South Africa Food-Based Dietary Guidelines for South Africa. S Afr J Clin Nutr 2013;26(3 Supplement):S1–S164. [Google Scholar]
- 89. US Department of Agriculture Make half your grains whole. Choose MyPlate, 2011. [cited 2015 Jun 24]. Available from: http://www.choosemyplate.gov/food-groups/downloads/TenTips/DGTipsheet4MakeHalfYourGrainsWhole.pdf. [Google Scholar]
- 90. Health Council of the Netherlands Guidelines for a healthy diet 2006. The Hague: Health Council of the Netherlands, 2006. [cited 2017 Jan 17]. Available from: http://www.voedingscentrum.nl/Assets/Uploads/voedingscentrum/Documents/Professionals/Voedselvoorlichting/06_Richtlijnen%20Goede%20Voeding%20Gezondheidsraad%202006.pdf. [Google Scholar]
- 91. Supreme Council of Health Qatar Dietary Guidelines. Doha, 2015. [cited 2017 Jan 17]. Available from: http://www.fao.org/3/a-az908e.pdf. [Google Scholar]
- 92. Canada H. Canada's Food Guide: Smart Snacking. Health Canada, 2007. [Google Scholar]
- 93. Ministry of Health Malaysia Healthy Packed Food for School Children My Health, 2012. [cited 2016 Apr 19]. Available from: http://myhealth.gov.my/index.php/en/nutrition/kids/bekalan-makanan-sihat-untuk-kanak-kanak-sekolah. [Google Scholar]
- 94. US Department of Agriculture US Department of Health and Health Services. Dietary Guidelines for Americans 2010. 7th ed Washington (DC): US Government Printing Office, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. US Department of Agriculture Build healthy mealtime habits. Choose MyPlate, 2015. [cited 2015 Jun 24]. Available from: http://www.choosemyplate.gov/food-groups/downloads/TenTips/DGTipsheet38BuildHealthyMealtimeHabits.pdf. [Google Scholar]
- 96. Public Health England The Eatwell Guide Helping you to eat a healthy balanced diet. 2016. [cited 12.1.2017] Available from: www.gov.uk/government/uploads/system/uploads/attachment_data/file/551502/Eatwell_Guide_booklet.pdf. [Google Scholar]
- 97. Ministry of Health Food and Nutrition Guidelines for Healthy Adults: A Background Paper. New Zealand: 2013. [cited 2015 Jul 8] Available from: https://www.health.govt.nz/system/files/documents/publications/foodandnutritionguidelines-adults.pdf. [Google Scholar]
- 98. Department of Nutrition, Ministry of Health The Omani Guide to Healthy Eating. 2009. [cited 2016 Dec 17] Available from: http://www.fao.org/3/a-as845e.pdf. [Google Scholar]
- 99. Ministry of Health Classifying foods and drinks for early childhood education services. New Zealand: 2013. [cited 2015 Jul 26] Available from: http://www.health.govt.nz/system/files/documents/pages/heha-ece-user-guide-section2.pdf. [Google Scholar]
- 100. Public Health Department; Ministry of Labor, Health and Social Affairs Healthy eating - The main key to health. Georgia: 2005. [cited 2015 Jul 27]. Available from: http://www.fao.org/3/a-as682e.pdf. [Google Scholar]
- 101. Ministry of Health, Labour, Welfare and Ministry of Agriculture, Forestry and Fisheries Japanese Food Guide Spinning Top. Japan: 2010. [cited 2015 Jul 13]. Available from: http://www.mhlw.go.jp/bunya/kenkou/pdf/eiyou-syokuji5.pdf. [Google Scholar]
- 102. Nutrition Division Federal Ministry of Health Food-Based Dietary Guideline For Nigeria: A Guide to healthy eating. Nigeria: 2006. [cited 2015 Jul 23]. Available from: http://www.fao.org/3/a-as841e.pdf. [Google Scholar]
- 103. American Academy of Pediatrics Choosing Healthy Snacks for children. 2015. [cited 2016 Dec 12]. Available from: https://www.healthychildren.org/English/healthy-living/nutrition/Pages/Choosing-Healthy-Snacks-for-Children.aspx. [Google Scholar]
- 104. GESUNDHEIT: öffentliches Gesundheitsportal österreichs Gesunde Rezepte für den Arbeitsalltag. Bundesministerium für Gesundheit, 2014. [cited 2015 May 5] Available from: https://www.gesundheit.gv.at/Portal.Node/ghp/public/content/ernaehrung-gesunde-rezepte-arbeitsalltag-LN.html. [Google Scholar]
- 105. US Department of Agriculture Got your dairy today? Choose MyPlate, 2011[cited 2015 Jun 24]. Available from: http://www.choosemyplate.gov/food-groups/downloads/TenTips/DGTipsheet5GotYourDairyToday.pdf. [Google Scholar]
- 106. US Department of Agriculture Cut back on your kid's sweet treats 10 tips to decrease added sugars. Choose MyPlate, 2011. [cited 2015 Jun 24]. Available from: http://www.choosemyplate.gov/food-groups/downloads/TenTips/DGTipsheet13CutBackOnSweetTreats.pdf. [Google Scholar]
- 107. Bundesministerium für Ernährung und Landwirtschaft Die zehn Regeln der DGE. Germany, 2014. [cited 2015 Jul 13]. Available from: http://www.bmel.de/DE/Ernaehrung/GesundeErnaehrung/ArbeitFreizeit/_Texte/DossierArbeitUndFreizeit.html?docId=5048102. [Google Scholar]
- 108. Ministry of Health Food-Based Dietary Guidelines for Belize. Belize: 2012. [cited 2015 Jul 28] Available from: http://www.fao.org/3/a-as852e.pdf. [Google Scholar]
- 109. Health Canada Eating Well with Canada's Food Guide First Nations, Inuit and Métis. Health Canada, 2007. [cited 2015 Jul 13]. Available from: http://www.hc-sc.gc.ca/fn-an/alt_formats/fnihb-dgspni/pdf/pubs/fnim-pnim/2007_fnim-pnim_food-guide-aliment-eng.pdf. [Google Scholar]
- 110. Health Promotion Department Ministry of Health & Social Security Dominica Food Based Dietary Guidelines. Dominica: 2007. [cited 2015 Jul 28] Available from: http://www.fao.org/3/a-as853e.pdf. [Google Scholar]
- 111. Instituto de Nutricion de Centro America Y Panama Food -Based Dietary Guidelines for Grenada. Grenada: 2006. [cited 2015 Jul 28]. Available from: http://www.fao.org/nutrition/education/food-dietary-guidelines/regions/countries/grenada/en/. [Google Scholar]
- 112. Health promotion Unit; Ministry of Health Social Services, Community Development, Culture and Gender Affairs Food-based dietary guidelines for St. Kitts and Nevis. St. Kitts and Nevis; 2010. [cited 2015 Jul 28]. Available from: http://www.fao.org/3/a-as858e.pdf. [Google Scholar]
- 113. FAO/WHO Final Report of the International Conference on Nutrition. 1992. [cited 2017 Jan 27]. Available from: http://apps.who.int/iris/bitstream/10665/61254/1/a34812.pdf. [Google Scholar]
- 114. FAO/WHO ICN2 Outcome document: Framework for Action. 2014. [cited 2017 Jan 17]. Available from: www.fao.org/3/a-mm215e.pdf. [Google Scholar]
- 115. FAO Food Climate Research Network Plates, Pyramids, Planet. Developments in national healthy and sustainable dietary guidelines: a state of play assessment. FAO; 2016. [cited 2017 Jan 17]. Available from: http://www.fao.org/3/a-i5640e.pdf. [Google Scholar]
- 116. WHO Nutrition in adolescence – Issues and Challenges for the Health Sector: Issues in Adolescent Health and Development. WHO; 2005. [cited 2017 Jan 17]. Available from: http://apps.who.int/iris/bitstream/10665/43342/1/9241593660_eng.pdf. [Google Scholar]
- 117. Wansink B, Pope L. When do gain-framed health messages work better than fear appeals? Nutr Rev 2015;73(1):4–11. [DOI] [PubMed] [Google Scholar]
- 118. Weichselbaum E, Buttriss JL. Diet, nutrition and schoolchildren: An update. Nutr Bull 2014;39(1):9–73. [Google Scholar]
- 119. St-Onge MP, Ard J, Baskin ML, Chiuve SE, Johnson HM, Kris-Etherton P, Varady K. Meal timing and frequency: implications for cardiovascular disease prevention: A scientific statement from the American heart association. Circulation 2017;135:e1–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Murakami K, Livingstone MB. Decreasing the number of small eating occasions (<15% of total energy intake) regardless of the time of day may be important to improve diet quality but not adiposity: a cross-sectional study in British children and adolescents. Br J Nutr 2016;115(2):332–41. [DOI] [PubMed] [Google Scholar]
- 121. Leech RM, Livingstone KM, Worsley A, Timperio A, McNaughton SA. Meal frequency but not snack frequency is associated with micronutrient intakes and overall diet quality in Australian men and women. J Nutr 2016;146(10):2027–34. [DOI] [PubMed] [Google Scholar]
- 122. Murakami K, Livingstone MB. Associations between meal and snack frequency and diet quality in US adults: National health and nutrition examination survey 2003–2012. J Acad of Nutr Diet 2016;116(7):1101–13. [DOI] [PubMed] [Google Scholar]
- 123. Kerver JM, Yang EJ, Obayashi S, Bianchi L, Song WO. Meal and snack patterns are associated with dietary intake of energy and nutrients in US adults. J Am Diet Assoc 2006;106(1):46–53. [DOI] [PubMed] [Google Scholar]
- 124. Sebastian RS, Cleveland LE, Goldman JD. Effect of snacking frequency on adolescents' dietary intakes and meeting national recommendations. J Adol Health 2008;42(5):503–11. [DOI] [PubMed] [Google Scholar]
- 125. Murakami K, Livingstone MB. Associations between meal and snack frequency and diet quality and adiposity measures in British adults: findings from the National Diet and Nutrition Survey. Public Health Nutr 2016;19(9):1624–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Moynihan PJ. The role of diet and nutrition in the etiology and prevention of oral diseases. Bull WHO 2005;83(9):694–9. [PMC free article] [PubMed] [Google Scholar]
- 127. O'Connor L, Brage S, Griffin SJ, Wareham NJ, Forouhi NG. The cross-sectional association between snacking behaviour and measures of adiposity: the Fenland Study, UK. Br J Nutr 2015;114(8):1286–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.