Abstract
INTRODUCTION:
Antibiotics are considered the most commonly sold drugs in developing countries. In India, these drugs are very much accessible without a prescription. This irrational and misuse of antibiotics results not only in the emergence of resistance of bacterial strains but also leads to adverse reactions.
AIM:
The aim of this study was to investigate the level of knowledge, attitude, and practice of antibiotics usage among dental patients.
MATERIALS AND METHODS:
Study design: This study was a cross-sectional design; a prevalidated structured questionnaire comprising 24 questions was used.
SAMPLE SIZE:
Six hundred and ten patients visiting a dental hospital, Chennai, Tamil Nadu, India, were included in the study.
RESULTS:
The dental patients involved in self-medication were more than 70%. 80.2% of the study group opted selection of antibiotics from their previous prescription from dental or medical professional. Adverse effects were faced by 7.8% of patients on taking self-medication. The study group was aware of the common dental procedures such as extraction and root canal treatment in which antibiotics were commonly prescribed. Half of the patients (53.8%) do not know the term antibiotic misuse, and 43.3% of the group opted antibiotic misuse to be unacceptable.
CONCLUSION:
The study revealed the knowledge, attitude, and practice of the patients about self-medication in the Indian scenario. There is need for health-care professionals and government bodies to enlighten the public about the harmful effects of self-medication with antibiotics to overcome the antibiotic resistance.
Keywords: Antibiotics, drug resistance, self-medication
Introduction
Antibiotic resistance is one of the world's major concern public health problems. The inappropriate use of antibiotics may contribute to the emergence of antibiotic resistance. Self-medication has been observed most frequently in the countries of economic transition where the prescription legislation is not well enforced and the drugs are freely available over the counter.[1]
Self-medication is defined as obtaining and consuming drugs without the surveillance of treatment.[2] This includes acquiring medicines without prescription, resubmitting old prescription to purchase medicines, sharing medicines, or using leftover medicines stored at home.
In India, almost every pharmacy sells drugs without a prescription, a phenomenon seen in many developing countries. Consequently, antibiotics and potentially habit-forming medicines are easily available to the common human. This together with poor awareness leaves people uninformed about the potentially lethal effects of some of these drugs. In addition, the lack of a good primary health-care system coupled with cost issues causes the general in irrational use of antibiotics, leading to antibiotic resistance.[3]
With regard to the rational use of antibiotics, the World Health Organization (WHO) at world assembly recommended to improve access to suitable antibiotics, to rationalize use of antibiotics, to strengthen health systems along with their ability to perform surveillance on microbial use, to ensure compliance with sanitary regulation, and to foster research into novel drugs and or vaccines.[4]
The aim of the study was to find the level of knowledge, attitude, and practice about antibiotics among dental patients.
Materials and Methods
This was a cross-sectional study to analyze the patients' knowledge, attitude, and practice of self-medication with antibiotics. A prevalidated structured questionnaire comprising 24 questions was distributed among 610 dental patients who visited the dental college during a period of 6 months from August 2016 to January 2017.
Validation of the questionnaire was done by an internal committee of six panelists who selected 24 questions from a preliminary pool of 45 questions. The sample size was calculated based on estimated population of 5000 potential patients, with confidence level of 95% and confidence interval of 3.75% (i.e., 4% margin of error). Systematic random sampling method was used for the survey.
Inclusion criteria included healthy individuals aged 18–65 years, who were able to understand the survey and questions, and who were able to give objective assessment and replies. Exclusion criteria included children and old age (>65 years) individuals and those who were physically and mentally unable to participate and give objective replies.
The questionnaire included structured panels such as knowledge about antibiotics, their indications, side effects, the behavior and attitude about the risk of self-medication with antibiotics, the prevalence and reasons for self-medication. The data were collected from dental patients of a Chennai City Hospital via a direct interview after obtaining oral consent and analyzed. Google percentage calculation, an online tool, was employed to calculate percentage and generate charts for pictographic representation of our results.
Results
A total of 610 patients participated in the survey; among them, 48.7% were male and 51.7% were female. The knowledge about antibiotics was well known by 64.9% [Chart 1] and recognition of the drug in the prescription can be done by 44.4% of the respondents. 80.2% of the study group opted selection of antibiotics from their previous prescription from dental or medical professional, while the remaining study group opted friends, family, online, and advertisements as other sources.
Chart 1.

Knowledge on antibiotics
The adverse effects of the antibiotic were aware by 42.3% [Chart 2]. The selection of antibiotics was mainly influenced by adverse effects 29.4%, brand company 25.5%, indication of the drug 19.2%, price 8.5%, and random selection 11%. Half of the respondents completed the full course of treatment, whereas 14.4% stopped the medication when the symptoms disappear [Chart 3]. About 28.5% will save the remaining antibiotic for later use; among them, 8% will use it after expiry date. About 20.2% of patients are confident in using antibiotic for any type of illness by themselves successfully.
Chart 2.
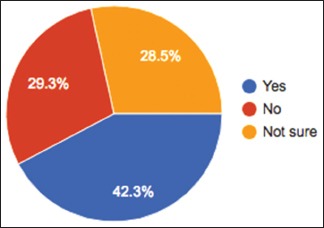
Adverse effects of antibiotics
Chart 3.
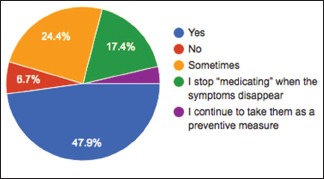
Completion of antibiotic course
Less than half of the respondents undergo self-medication for more than 6 months (40.5%), more than 2 months (17.4%), and frequently (13.6%) [Chart 4]. The dose was determined by instruction on the package by (35.1%), online resources (16%), when fell ill (20.9%). The adverse effects faced by the patients on taking self-medication were 7.8%; the remaining respondents either had mild (26%), tolerable (24.3%), or no adverse effects 62.2%. The adverse effects were stomach pain (25.7%), diarrhea (12.1%), and nausea (10.7%) [Chart 5].
Chart 4.
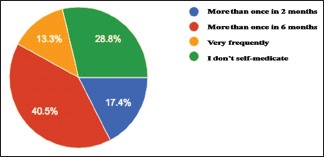
Frequency of self-medication
Chart 5.
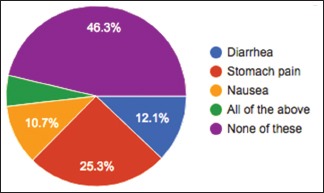
Adverse effects
About half of the respondents took antibiotic for dental problem for more than two times in the last year. The common dental procedures such as extraction and root canal treatment were prescribed with antibiotics. The dentists prescribe antibiotic for 3 days most commonly followed by 5 days and 7 days. The patients justify the use of antibiotics by previous prescription and availability of medicine 39%, personal incontinence and long waiting line in clinics (14.7%), and cost-saving reasons (7.8%) [Chart 6]. Half of the patients (53.8%) do not know the term antibiotic misuse, and 43.3% opinion about self-medication with antibiotic is unacceptable.
Chart 6.
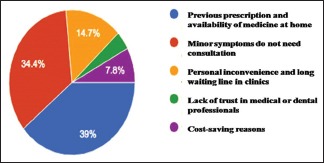
Justification of antibiotic usage
Discussion
Self-medication is the utilization of medicines by persons on their own without any proficient medical supervision.[5] In developing countries like India, most episodes are treated by self-medication due to easy availability of nonprescription drugs. It is a prominent constraint in ensuring the safe and effective use of medicines. It is more likely to be inappropriate without complete knowledge although it is becoming a routine practice nowadays, especially by the common human.
Antibiotics are the most used medicines in self-medication. Self-medication with antibiotics leads to adverse drug reactions, drug interactions, masking the correct diagnosis, and development of added infections. If they have chosen the wrong antibiotic or intake incorrect dosage, it can drastically reduce the immunity level against bacterial attacks and end up in drug resistance.[6,7]
A study conducted by the WHO showed 364 (79.8%) of the study population reported to have used self-prescribed antibiotics during the last 2 months before the study.[8] Similarly, our study revealed that nearly 71.2% of the respondents declared they self-medicated due to various justifications. It is due to lack of knowledge about the potential side effects of antibiotics and easy availabilities through previous prescriptions; people are more inclined to practice of self-medication. We inherited this act of self-medication in our society through traditions where diseases were cured by taking drugs, herbs, or home remedies without consulting a practitioner.[9,10] The other important factor is the socioeconomic status of the individuals considering the professional consultation charges. Furthermore, the lack of a good primary health-care system coupled with cost issues causes the general public to approach various other doors instead of a doctor's to seek help for a problem.
In India, sale of drugs without prescription in pharmacy or medical store is almost common practice. Studies have reported different prevalence figures ranging from 43.2% to 91%.[11,12,13,14] It is very difficult to compare the prevalence of different studies with the present study due to different demographic characteristics, different methodology, and different socioeconomic status. The prevalence of self-medication was high among the medical students and youngsters.[15,16,17,18]
In our study, we acquired that mostly people are engaged in self-medication through the previous prescription, suggested medicine from family and friends and from online resources, Moreover, this practice often has many adverse effects and can lead to many problems, including global emergence of multidrug-resistant pathogens,[19] drug dependence and addiction, masking of malignant and potentially fatal diseases, hazard of misdiagnosis,[20] problems relating to over and under dosage, drug interactions,[21] and tragedies relating to the side effect profile of specific drugs.
The consumption of antibiotic for dental problems is increasing nowadays. The procedures such as extraction and root canal treatment were prescribed with antibiotics to prevent secondary microbial infection. The self-medication for dental procedures is also an alarming situation which results in antibiotic resistance.
Self-medication is at an alarming pace and education of the public is cardinal. It is difficult to eradicate and there is a significant need of measures to discourage such practices. The danger of interactions and adverse effects could increase if necessary actions are evaded. To overcome this problem, the WHO (2014) issued certain guidelines:
Authorities are required to review and classify medical products on the basis of safety and efficacy and contribute to enforcement and implementation of laws and regulations
Adaptation of self-medication protocols by the Ministry of Health and Provision of reference materials and training activities for health-care workers to meet local needs
Continuing education for pharmacists should be undertaken and supported to ensure maintenance of pharmacist's capacity to respond to the changing health needs of the public
National pharmaceutical associations should develop certain performance standard, based on the concept of performance standard, based on the concept of pharmaceutical care.[22]
The government should consider steps to supervise or control the practice of self-medication by check on availability of the medicines without prescription, controlling over-the-counter medicines, and formulating guideline for the usage of the drugs by the physician and pharmacist.
Conclusion
This study revealed that majority of dental patients lacked the knowledge about antibiotics usage. This has become a threat in terms of developing antibiotics resistance in treating disease. Therefore, it is the responsibility of the prescribing doctors and the governmental bodies to increase the awareness of antibiotic use and misuse among the general public and formulate laws in availability of drugs.
Financial support and sponsorship
This study has received no financial support or sponsorship from any individual or organization.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We wish to acknowledge all the workers and participants who directly and indirectly supported this survey.
References
- 1.Hughes CM, McElnay JC, Fleming GF. Benefits and risks of self medication. Drug Saf. 2001;24:1027–37. doi: 10.2165/00002018-200124140-00002. [DOI] [PubMed] [Google Scholar]
- 2.James H, Handu SS, Al Khaja KA, Otoom S, Sequeira RP. Evaluation of the knowledge, attitude and practice of self-medication among first-year medical students. Med Princ Pract. 2006;15:270–5. doi: 10.1159/000092989. [DOI] [PubMed] [Google Scholar]
- 3.Bauchner H, Wise PH. Antibiotics without prescription: “bacterial or medical resistance”? Lancet. 2000;355:1480. doi: 10.1016/S0140-6736(00)02160-7. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization. The Role of Pharmacist in Health Care System. 1998. [Last accessed on 2013 Jan 29]. Available from: http://www.apps.who.int/medicinedocs/en/d/Jwhozip32e .
- 5.Pandya RN, Jhaveri KS, Vyas FI, Patel VJ. Prevalence, pattern and perceptions of self medication in medical students. Int J Basic Clin Pharmacol. 2013;2:275–80. [Google Scholar]
- 6.Okeke IN, Lamikanra A, Edelman R. Socioeconomic and behavioral factors leading to acquired bacterial resistance to antibiotics in developing countries. Emerg Infect Dis. 1999;5:18–27. doi: 10.3201/eid0501.990103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Awad A, Eltayeb I, Matowe L, Thalib L. Self-medication with antibiotics and antimalarials in the community of Khartoum state, Sudan. J Pharm Pharm Sci. 2005;8:326–31. [PubMed] [Google Scholar]
- 8.World Health Organization. Global Strategy for Containment of Antimicrobial Resistance: World Health Organization. Communicable Diseases Surveillance and Response (CRS) WHO/CDS/CRS/DRS/2001.2.2001. [Google Scholar]
- 9.Girish HO, Divya HM, Prabhakaran S, Venugopalan PP, Koppad R. A cross-sectional study on self medication pattern among medical students at Kannur, North Kerala. J Evol Med Dent Sci. 2013;2:8693–700. [Google Scholar]
- 10.Kumar N, Kanchan T, Unnikrishnan B, Rekha T, Mithra P, Kulkarni V, et al. Perceptions and practices of self-medication among medical students in coastal South India. PLoS One. 2013;8:e72247. doi: 10.1371/journal.pone.0072247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gutema GB, Gadisa DA, Kidanemariam ZA, Berhe DF, Berhe AH, Hadera MG, et al. Self-medication practices among health sciences students: The case of Mekelle University. J Appl Pharm Sci. 2011;1:183–9. [Google Scholar]
- 12.Deshpande SG, Tiwari R. Self medication – A growing concern. Indian J Med Sci. 1997;51:93–6. [PubMed] [Google Scholar]
- 13.Loyola Filho AI, Lima-Costa MF, Uchôa E. Bambuí project: A qualitative approach to self-medication. Cad Saude Publica. 2004;20:1661–9. doi: 10.1590/s0102-311x2004000600025. [DOI] [PubMed] [Google Scholar]
- 14.Figueiras A, Caamaño F, Gestal-Otero JJ. Sociodemographic factors related to self-medication in Spain. Eur J Epidemiol. 2000;16:19–26. doi: 10.1023/a:1007608702063. [DOI] [PubMed] [Google Scholar]
- 15.Klemenc-Ketis Z, Hladnik Z, Kersnik J. Self-medication among healthcare and non-healthcare students at University of Ljubljana, Slovenia. Med Princ Pract. 2010;19:395–401. doi: 10.1159/000316380. [DOI] [PubMed] [Google Scholar]
- 16.Zafar SN, Syed R, Waqar S, ZubairiAJ, Vaqar T, Shaikh M, et al. Self-medication amongst University Students of Karachi: Prevalence, Knowledge and Attitudes. J Pak Med Assn. 2008;58:214–7. [PubMed] [Google Scholar]
- 17.Kumari R, Kiran Kumar D, Bahl R, Gupta R. Study of knowledge and practices of self-medication among medical students at Jammu. J Med Sci. 2012;15:141–4. [Google Scholar]
- 18.Abay SM, Amelo W. Assessment of self-medication practices among medical, pharmacy, and health science students in Gondar University, Ethiopia. J Young Pharm. 2010;2:306–10. doi: 10.4103/0975-1483.66798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chang FR, Trivedi PK. Economics of self-medication: Theory and evidence. Health Econ. 2003;12:721–39. doi: 10.1002/hec.841. [DOI] [PubMed] [Google Scholar]
- 20.Calabresi P, Cupini LM. Medication-overuse headache: Similarities with drug addiction. Trends Pharmacol Sci. 2005;26:62–8. doi: 10.1016/j.tips.2004.12.008. [DOI] [PubMed] [Google Scholar]
- 21.Mumtaz Y, Jahangeer SM, Mujtaba T, Zafar S, Adnan S. Self-medication among university students of Karachi. J Liaquat Univ Med Health Sci. 2011;10:102–5. [Google Scholar]
- 22.World Health Organization. Guidelines for the Regulatory Assessment of Medicinal Products for Use in Self-medication. Available from: http://apps.who.int/medicinedocs/en/d/Js2218e/1.html .


