Abstract
CONTEXT:
Timed up-and-go (TUG) test is a valid, reliable, and an objective test for quantifying functional mobility and assessing the fall risk in all age groups. The analysis of patient scores on TUG test is limited by lack of data, having a wide range of performance scores among people without disabilities.
AIM:
The objective of the study was to provide the reference value for TUG test in healthy individuals of Gujarat, India.
SUBJECTS AND METHODS:
It was a cross-sectional observational study. Five hundred and twenty healthy individuals, aged 40–70 years, were recruited from various regions of Gujarat based on convenient sampling. All the participants were made to perform TUG test in a controlled environment in community. Three readings of the actual test were obtained and averaged.
RESULTS:
Data were analyzed with mean, standard deviation, confidence intervals (CIs 95%) and Pearson's correlation coefficient (r) with α = 0.05 by age groups (40–50, 51–60, and 61–70 years) and gender. The mean (CI 95%) TUG time for healthy adults of Gujarat was 8.46 (8.35–8.57) s and demonstrated age-related decline for both male and female participants. TUG time also demonstrated strong correlation with the height of individuals.
CONCLUSION:
This preliminary data can be used as a reference only for specific population with specific age groups due to variability in test results among the different population due to age, gender, anthropometric measures such as height, weight, and body mass index, geographical variation, nutritional support, and cognitive status.
Keywords: Accidental falls, activities of daily living, gait, middle aged, reference values, timed up-and-go test
Introduction
Physical mobility refers to the capacity of a person to move around their surroundings, and it largely depends on the muscle strength, cardiorespiratory fitness, neuromuscular coordination, and postural stability or balance. The assessment of physical mobility is an essential component of elderly individuals as the aging is inevitably accompanied with constrained movements and loss of balance.
Physical mobility can be assessed by several measures. The traditional neuromuscular examination, though useful for determining disease progression and severity, has been considered to be insufficient for assessing overall functional capacity. Apart from conventional physical examination, laboratory testing procedures accurately measure multiple components of balance and gait, reliably separate fallers from nonfallers, and predict future falls. However, these techniques are costly, arduous, and unfeasible in most clinical settings. These constraints have prompted the development of mobility tests that contain the balance and gait maneuvers used in daily life and are simple and inexpensive. One of these tests is the timed up-and-go test (TUG).[1,2]
Podsiadlo in 1991 developed test TUG as a test of basic mobility skills, a modified, timed version of “get-up-and-go (GUG) test” (Mathias et al. 1986). GUG test was developed formerly as a clinical evaluation of balance in elderly and was scored on an ordinal scale of 1–5 based on an observer's insight of the performer's risk of fall during the test.
Podsiadlo and Richardson modified the original test by timing the task and projected its use as a test of basic ability skills for frail community-dwelling elderly. More specifically, it assesses the ability to perform sequential motor task relative to walking and turning.[3]
The TUG is an easy tool to assess the overall motor function and to follow up its evolution in clinical setting. It has been frequently used to assess functional mobility of pediatric population, adolescents, adults, and elderly individuals and has been found highly correlated with functional markers, namely, stair climbing; balance and walking speed; predictive of falls, and mortality.[4,5,6]
The test measures the time taken to stand up from a standard chair, walk 3 m, turn, walk back to the chair, and sit down again. It takes one to 2 min to administer, is quick, requires no special equipment, and can easily be performed during a routine medical examination. The test quantifies the functional mobility and this can be useful for following a clinical change over a period of time.[1] It is a commonly used screening tool for fall risk in the inpatient and the community setting and is recommended as a routine screening tool for falls by American Geriatrics Society and British Geriatrics Society.[7] The National Institute of Clinical Evidence (NICE) guidelines also advocate the use the TUG for assessment of gait and balance in the prevention of falls in older people.[8] The use of TUG has been recommended in emergency department too to identify patients at risk of functional decline following a minor trauma and is considered to be strongly associated with functional decline at 3 and 6 months post injury.[9]
TUG in community adults has also been said to be associated with several physical health-related factors such as age, gender, height, weight, body mass index (BMI), nutritional status, and cognitive impairments.[6,10]
The normal values of the test are age specific, with walking speed decreasing with age. Till date, there is no literature available on the norms of TUG in Indian population; therefore, it is necessary to have a reference values which can be used for comparison in various settings, for example, acute care, in- and out-patients rehabilitation, home health care, and community. Thus, the present study was undertaken to determine the reference value for TUG test in healthy adults of Gujarat, India.
Subjects and Methods
The approval was obtained from “Human Research Ethical Committee” of H M Patel Centre of Medical Care and Education, Karamsad, before initiating the study (Ethical code: HMPCMCE/HREC/UG/PG/9/Session-1/2).
Study design
This was a cross-sectional, observational study.
Sampling method
Convenient sampling was used.
Study setting
This was a community-based study.
Subject recruitment procedure
Totally 520 normal healthy individuals from the various districts of Gujarat state, India, were recruited based on convenient sampling after explaining about the purpose and procedure of the study. Written informed consent was obtained from all the participants.
Inclusion criteria
Normal healthy individuals (Self-reported on no medication)
Age group 40–70 years
Both males and females were included in the study.
Exclusion criteria
Any musculoskeletal, cardiovascular, respiratory, or neurological disorders
Individuals with any psychiatric problem or having difficulty in understanding
Any surgical history especially of the lower limb were excluded from the study.
Materials
Chair with armrest and backrest, stopwatch, measure tape, blocks, weighing machine, height scale.
General information was collected as a part of clinical data including name, age, gender, height, and weight of all individuals.
TUG test measures the time (in seconds) taken by an individual to stand up from a chair, walk a distance of 3 m (10 feet), turn, walk back to the chair, and sit down.[1] To perform the test, the participants were asked to sit on a chair, placing his/her back against the back rest and resting his/her arms on armrests. On the instruction “Go”, the participants were asked to rise up from a chair, walk to a line/block on the floor 3 m away, turn around, return, and sit back on a chair.
All the participants were asked to walk as quickly as they feel safe and comfortable until they pass the end of marked course with both feet. All the patients were allowed to wear their regular footwear and use a walking aid if needed; however, no participant required any walking aid or self-helped device. On the word, “Go” time began and stopped after the participants sat back on the chair. A stopwatch was used to time the test (in seconds). The participants walked through the test once before being timed to become familiar with the test, and three readings of the actual test were obtained and averaged for statistical analysis.
Data analysis and results
Data analysis was carried out by calculating mean, standard deviation, and Pearson's correlation coefficient (r) with 95% confidence interval (CI) and level of significance α = 0.05.
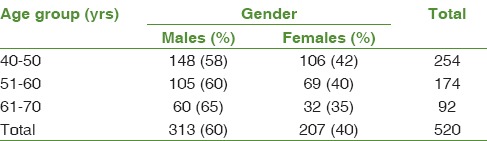
Totally 520 normal healthy individuals were evaluated for TUG test. Table 1 shows the distribution of participants according to gender in different age groups.
Table 1.
Distribution of study participants according to age group and gender
The mean (95% CI) TUG time for all the study participants (n = 520) was 8.46 + 0.11 s. The mean TUG time for three age groups was 8.12 + 0.04 s for 40–50 years, 8.61 + 0.05 s for 51–60 years, and 9.34 + 0.12 s for 61–70 years. The results showed that males had lesser TUG time compared to females in all age groups [Figure 1]; however, the difference was not statistically significant (P = 0.47). The figure also reflects that the TUG time increased with age for both males and females.
Figure 1.
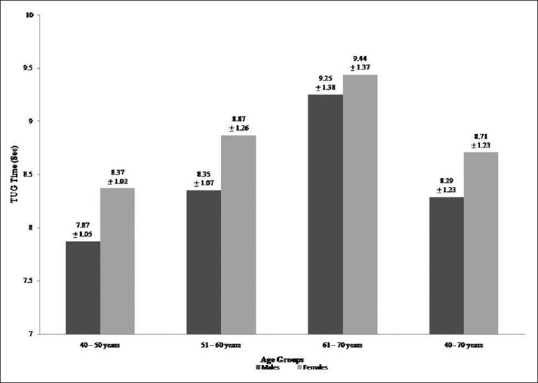
Timed up-and-go test (mean + standard deviation) in seconds in different age groups and gender
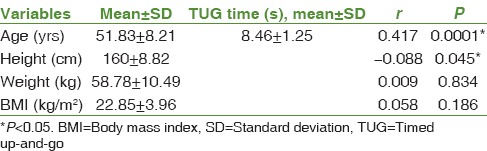
Pearson's correlation coefficient was calculated to explore the relationship between TUG time and its determining factors namely, age, height, weight, and BMI [Table 2]. The study found statistically significant correlation (P < 0.05) with age (r = 0.417) and height (r = −0.088). This suggests that as the age increases, the TUG time increases and as the height increases, the TUG time decrease.
Table 2.
Correlation of timed up-and-go time (Pearson's correlation coefficient - r)
Discussion
TUG test is a simple, quick, and widely used clinical performance-based measure of lower extremity function, mobility, balance, and fall risk.[11] To use the TUG test in clinical or nonclinical settings, well-established normative data are required. Majority of studies addressing the standardization of test have been performed with selected samples of individuals recruited by convenient criteria, and true population based data are scarce.
The TUG time score is considered to be reliable (both inter-rater and intra-rater), correlates well with Berg balance scale, gait speed, and Barthel index of activities of daily living, and appears to predict the patient's ability to go outside alone safely. However, test–retest reliability of measurements obtained with the TUG in a group of community-dwelling older adults without cognitive impairments is moderate, and for identifying people who fall, the TUG is found to have 87% sensitivity and specificity.[3,11]
The study participants in this study took average 8.46 (8.35–8.57) s to complete the test, increasing the time duration with age, and none of the participants used the assistive device during the test.
The reference values reported in the literature vary considerably with geographical representation of the participants.[10,12,13] Wide ranges of TUG scores have been reported for various samples of elderly people. Podsiadlo and Richardson evaluated TUG in 10 men and women without known pathology, aged 70–84 years, and found a mean TUG score of 8.5 s (7–10 s). In a study by Hughes,[14] independent community-dwelling elderly people, aged 65–86 years, had a mean TUG score of 13.05 s (8.7–17.3 s). The highest mean score of 15 s (5.4–40.8 s) for TUG has been reported by Newton[7] who used 3.05 m of walking distance and included the participants (African-American, Hispanic) who used an ambulatory device whereas Kamide et al.[12] reported the lowest score of 6.6 s (6.18–7.02 s) in Japanese elderly people.
In the present study, the mean TUG scores in males were much leaser than females; however, the difference was not statistically significant. Furthermore, the TUG time significantly correlated with age and height of participants. Numbers of trials[3,4,12,13,14,15,16,17] have proved that TUG performance highly depends on age and other non motor variables such as female gender, height, weight, nutritional status, cognitive impairment, and use of assistive device.
Balogun, et al.[16] studied 1280 healthy participants, aged 6–85 years, and found that balance performance for both males and females deteriorates with increase in chronological age with peaked deterioration at the third decade of life in males and fourth decade of life in females and progressive decline thereafter. Aging leads to slow reaction time, reduction in nerve conduction velocity, and decrease in sensory-motor and proprioceptive responses, leading to balance problem in elderly individuals. The balance is also affected by reduction in muscle strength and postural abnormalities leading to 17%–20% in gait velocity and stride length.[18]
Stride length of an individual is also affected by leg length, height, age, sex, and other variables. As the height of an individual increases, the stride length increases leading to increased gait velocity and lesser TUG time. Males are known to have better gait velocity leading to lesser TUG time compared to females. Reduced gait speed and postural stability and increased TUG time have been found in overweight sedentary middle-aged adults leading to increased risk of fall in middle-aged population.[19]
A longitudinal study carried out in China concluded that the future falls can be best predicted by the TUG test and a score of 15.96 s can be used as a cut point to screen the recurrent falls in community-dwelling elderly individuals of China.[20] Bohannon,[13] through a descriptive meta-analysis, concluded that the patients whose performance exceeds the upper limit of reported CIs of TUG time can be considered to have worse than average performance.
Conclusion
The reference value of TUG time in healthy individuals of Gujarat, India, was found to be 8.46 s which provides a standard to which patient performance can be compared with. However, it is always advisable to follow the age- and gender-specific TUG scores. The study concludes that the performance on TUG test is variable in healthy individuals and this variability can be explained using age, gender, height, use of assistive device, geographical representation of participants, etc., It is always better to standardize the testing conditions along with a control of the significant potential confounders, namely, age, gender, and comorbidities to provide better information about the TUG predictive value for future falls in older adults.[15]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors acknowledge the appreciation toward all the individuals who participated in the study and owe sincere thanks to all the authors/publishers whose articles, books, and review have been utilized for making this study more genuine. The authors especially acknowledge the gratitude toward the authors who have developed the norms for TUG in other population which has provided the strong base for the successful completion of the present study.
References
- 1.Podsiadlo D, Richardson S. The timed “Up & go”: A test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39:142–8. doi: 10.1111/j.1532-5415.1991.tb01616.x. [DOI] [PubMed] [Google Scholar]
- 2.Colón-Emeric CS, Liang BA. Falls in older adults: Assessment and intervention in primary care. Hosp Phys. 2002;38:55–66. [Google Scholar]
- 3.Steffen TM, Hacker TA, Mollinger L. Age- and gender-related test performance in community-dwelling elderly people: Six-minute walk test, berg balance scale, timed up and amp; go test, and gait speeds. Phys Ther. 2002;82:128–37. doi: 10.1093/ptj/82.2.128. [DOI] [PubMed] [Google Scholar]
- 4.Pondal M, del Ser T. Normative data and determinants for the timed “up and go” test in a population-based sample of elderly individuals without gait disturbances. J Geriatr Phys Ther. 2008;31:57–63. doi: 10.1519/00139143-200831020-00004. [DOI] [PubMed] [Google Scholar]
- 5.Nicolini-Panisson RD, Donadio MV. Timed “Up & go” test in children and adolescents. Rev Paul Pediatr. 2013;31:377–83. doi: 10.1590/S0103-05822013000300016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shumway-Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community-dwelling older adults using the timed up & go test. Phys Ther. 2000;80:896–903. [PubMed] [Google Scholar]
- 7.Drootin M. Panel on Prevention of Falls in Older Persons, American Geriatrics Society and British Geriatrics Society. Summary of the Updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc. 2011;59:148–57. doi: 10.1111/j.1532-5415.2010.03234.x. [DOI] [PubMed] [Google Scholar]
- 8.Centre for Clinical Practice at NICE UK. The Assessment and Prevention of Falls in Older People. 2013. [Last accessed on 2018 Jan 28]. Available from: http://www.nice.org.uk/CG161 .
- 9.Eagles D, Perry JJ, Sirois MJ, Lang E, Daoust R, Lee J, et al. Timed up and go predicts functional decline in older patients presenting to the emergency department following minor trauma. Age Ageing. 2017;46:214–8. doi: 10.1093/ageing/afw184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Newton RA. Balance screening of an inner city older adult population. Arch Phys Med Rehabil. 1997;78:587–91. doi: 10.1016/s0003-9993(97)90423-8. [DOI] [PubMed] [Google Scholar]
- 11.Herman T, Giladi N, Hausdorff JM. Properties of the‘timed up & go' test: More than meets the eye. Gerontology. 2011;57:203–10. doi: 10.1159/000314963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kamide N, Takahashi K, Shiba Y. Reference values for the timed up and go test in healthy Japanese elderly people: Determination using the methodology of meta-analysis. Geriatr Gerontol Int. 2011;11:445–51. doi: 10.1111/j.1447-0594.2011.00704.x. [DOI] [PubMed] [Google Scholar]
- 13.Bohannon RW. Reference values for the timed up and go test: A descriptive meta-analysis. J Geriatr Phys Ther. 2006;29:64–8. doi: 10.1519/00139143-200608000-00004. [DOI] [PubMed] [Google Scholar]
- 14.Hughes C. Relationship among performance on stair ambulation, functional reach, and timed up and go tests in older adults. Issues Aging. 1998;21:18–22. [Google Scholar]
- 15.Beauchet O, Fantino B, Allali G, Muir SW, Montero-Odasso M, Annweiler C, et al. Timed up and go test and risk of falls in older adults: A systematic review. J Nutr Health Aging. 2011;15:933–8. doi: 10.1007/s12603-011-0062-0. [DOI] [PubMed] [Google Scholar]
- 16.Balogun JA, Akindele KA, Nihinlola JO, Marzouk DK. Age-related changes in balance performance. Disabil Rehabil. 1994;16:58–62. doi: 10.3109/09638289409166013. [DOI] [PubMed] [Google Scholar]
- 17.Medley A, Thompson M. The effect of assistive devices on the performance of community dwelling elderly on the timed up and go test. Issues Aging. 1997;20:e7. [Google Scholar]
- 18.Elble RJ, Thomas SS, Higgins C, Colliver J. Stride-dependent changes in gait of older people. J Neurol. 1991;238:1–5. doi: 10.1007/BF00319700. [DOI] [PubMed] [Google Scholar]
- 19.Southard V, Dave A, Douris P. Êxploring the role of body mass index on balance reactions and gait in overweight sedentary middle-aged adults: A pilot study. J Prim Care Community Health. 2010;1:178–83. doi: 10.1177/2150131910380921. [DOI] [PubMed] [Google Scholar]
- 20.Kang L, Han P, Wang J, Ma Y, Jia L, Fu L, et al. Timed up and go test can predict recurrent falls: A longitudinal study of the community-dwelling elderly in China. Clin Interv Aging. 2017;12:2009–16. doi: 10.2147/CIA.S138287. [DOI] [PMC free article] [PubMed] [Google Scholar]


