Abstract
Purpose
Exposure to nature and natural environments may be beneficial for mental health, however, most population-based studies have been conducted among adults while few have focused on adolescents. We aimed to investigate the relationship between both greenness (vegetation) and blue space (water), and depressive symptoms among teenagers in the United States.
Methods
The study population included 9,385 participants ages 12–18 in the 1999 wave of the Growing Up Today Study (GUTS). We characterized greenness exposure using the Normalized Difference Vegetation Index (NDVI) at a 250 and 1250m radius around a subject’s residence using data from the Moderate-resolution Imaging Spectroradiometer onboard NASA's Terra satellite. Exposure to blue space was defined as the presence of blue space within a 250m and 1250m radius and distance to the nearest blue space. We used logistic regression models to examine associations with high depressive symptoms, measured using self-reported responses to the McKnight Risk Factor Survey.
Results
An interquartile range higher peak greenness in the 1250m buffer was associated with 11% lower odds of high depressive symptoms (95% CI 0.79–0.99). While not statistically significant, this association was stronger in middle school students than high school students. No such association was seen for blue spaces.
Conclusions
Surrounding greenness, but not blue space, was associated with lower odds of high depressive symptoms in this population of more than 9,000 US adolescents. This association was stronger in middle school students than high school students. Incorporating vegetation into residential areas may be beneficial for mental health.
Keywords: Built environment, natural environment, greenness, green space, blue space, mental health, depression
Introduction
There is emerging evidence that exposure to nature, particularly in the residential environment, may confer mental and physical health benefits[1,2]. Nature may directly influence mental health by improving people’s affective states[3,4] and activating restorative processes related to cognition and attention[5]. Natural environments can also provide opportunities to engage in physical activity and social interactions which may in turn benefit both physical and mental health[1,2,6,7].
Studies across many countries, mostly cross-sectional, have observed associations between surrounding greenness or green space and lower stress, psychological distress, and depressive symptoms[1,2,6], primarily in adults. Greenness has been associated with reduced risk of clinically-relevant disorders including anxiety and major depressive disorder[1,2]. Many of the pathways connecting greenness and health, including stress reduction, increased physical activity, and social interaction and cohesion, are particularly relevant for the outcome of depression or depressive symptoms[1], a major contributor to morbidity in the US and around the world[8]. Findings from studies of greenness and depression in adults have been mixed but suggest an association[9,10][11,12].
Evidence for a relationship between greenness and mental health, including depression, in children and adolescents is more limited[2]. Some studies have shown associations between both objectively and subjectively measured green spaces and outcomes such behavioral problems[13] or Attention Deficit and Hyperactivity Disorder symptoms among children and adolescents ages 5–18[14]. Two population-based studies found higher objectively-assessed greenness was associated with lower emotional distress among children between ages 3 and 10[15,16] but did not assess this association in adolescence. Adolescence, often defined as the period between ages 11 and 24, is an important period for many aspects of development including behavioral and mental health[17].
In a given year depression impacts one in nine adolescents in the US[18] and experiencing depression in adolescence is associated with subsequent episodes in adulthood[19]. We are aware of only one study which considered the association between nature and depressive symptoms in adolescence[11], in which no associations between changes in self-reported greenery and changes in depressive symptoms were observed. Objective characterizations of exposure can strengthen our understanding of this association[2].
Much of the existing research has focused on exposure to greenness or green spaces, but recent studies have begun to consider whether exposure to blue space (surface water) may also benefit health[2,20]. Blue space may provide similar benefits for cognitive restoration and stress reduction[7] but population-based evidence is limited and mixed, and most studies have been conducted in adults[2,20–25]. The mixed findings may be attributed in part to heterogeneous exposure definitions, including linear distance to coast and presence of any blue space within various buffers, or to variable outcomes including self-reported general health and various mental health measures.
The current study investigated the relationship between residential exposure to natural environments and depressive symptoms in a large cohort of teenagers living in the United States. We hypothesized that residential exposure to greenness and blue space would be associated with lower depressive symptoms. Given the relatively limited evidence for the association between nature, particularly blue space, and health and the lack of consistent exposure definitions we focus on a cross-sectional analysis in this paper. We consider potential confounding by important neighborhood and environmental attributes that co-vary with greenness, including air pollution and socioeconomic conditions, and possible effect modification by grade level, gender, and region.
Methods
Study participants were from the Growing Up Today Study (GUTS). GUTS was founded in 1996 by inviting mothers from the ongoing Nurses’ Health Study II (NHS II) to enroll their children ages 9–14. Once parental consent was obtained, participants who returned completed questionnaires at baseline were considered enrolled (n = 16,875). The study was approved by the Brigham and Women's Hospital Institutional Review Board.
For this analysis, eligible participants were 12–18 year-olds who completed the 1999 wave of GUTS (N=12,413, 74% of the original sample) because that was the first wave at which depressive symptoms were assessed. We excluded participants who did not report on depressive symptoms in 1999 (N=1,599), who lived outside the contiguous United States (N=27), or who were younger than 12 when they completed the 1999 questionnaire (N=2). Study participants were assigned addresses based on the addresses of their mothers participating in NHS II. Addresses of all NHS II participants had been previously geocoded and we assigned each eligible GUTS participant the latitude and longitude values corresponding to their mother’s address in 1999. Since address assignment was based on mother’s reported residence we excluded subjects who reported not living with their mothers on the previous questionnaire (N=1,149), attending military or boarding school (N=61), or attending college (N=190), leaving 9,385 participants. Socioeconomic and environmental characteristics of the neighborhoods where the mothers of included subjects lived did not differ substantially from those who were excluded.
Outcome
The primary outcome of interest was high depressive symptoms in 1999, assessed using the McKnight Risk Factor Survey (MRFS). The depressive symptom questions on the MRFS consist of six items each scored on a five-point Likert scale[26]. Each item was scored zero (never) to four (always) and the mean was taken. Scores on the MRFS were highly correlated with the more commonly used Centers for Epidemiologic Studies of Depression (CES-D)[26]. Subjects missing one item were included with their mean score calculated from available responses; subjects missing two or more items were excluded. Our final sample of 9,385 individuals included 122 subjects who responded to 5 of 6 items and 9,263 subjects who responded to all 6. An age-specific z-score was calculated for each age at the time of questionnaire return using all available MRFS questionnaires completed by GUTS participants. The MRFS does not have an established clinical cut-off for high depressive symptoms. The prevalence of depression in this age range is estimated at 11.5%[18], so we considered those subjects with the highest 11.5% of scores to be cases of “high depressive symptoms”. In sensitivity analyses we also separately considered the highest 5% and highest 15% of scores as cases.
Exposures
Greenness was characterized using the NDVI, an index of vegetative density commonly used in studies of health outcomes[1,27–29]. NDVI leverages the fact that chlorophyll in plants absorbs visible light (0.4–0.7 μm), while leaves reflect near-infrared light (0.7–1.1 μm). NDVI is calculated as the ratio of the difference between the near-infrared and red reflectance to the sum of these two values. It ranges from −1.0 to 1.0, with larger values indicating higher levels of vegetative density.[30] Reflectance data were downloaded at a 250m resolution from the Moderate-resolution Imaging Spectroradiometer (MODIS) on board NASA’s Terra satellite.[31] We used data collected in 2000 to create two measures of greenness exposure at the 250m resolution: mid-July for our primary exposure (“peak” greenness), and an annual average created using one measurement from each season (“average” greenness). We also calculated NDVI in a 1250m buffer surrounding a subject’s residence. The smaller resolution captures an area relatively proximal (and more likely visible) from the home, while the larger spatial area captures a typical walking distance for someone in this age range[32].
Locations of blue spaces were characterized using the 2014 National Hydrography Dataset (NHD) for interior surface waters and data from the National Oceanic and Atmospheric Administration’s National Centers for Environmental Information for coastlines[33]. The NHD is developed by the U.S. Geological Survey in cooperation with the U.S. Environmental Protection Agency and available for download through the Environmental Systems Research Institute (Esri, Redlands, CA). It identifies all water bodies that comprise the surface water drainage system of the United States including types (river, lake, wetland, etc.), location, and area. Ground-truth confirmation demonstrates that 90% of NHD features fall within 50 ft. of their true position and that less than 1% of the NHD changes over 50 years (J. Simley, Personal Correspondence, September 2015). Our primary analysis considered all types of perennial (non-intermittent) water together and coasts and inland water bodies (such as lakes and rivers) separately. In all analyses we excluded swamps, ice masses, inundation areas, water treatment facilities, and water bodies characterized as intermittent.
There is no consensus in the literature about the best way to operationalize exposure to blue space, with multiple metrics implemented previously,[16,21–24] so we considered several exposure characterizations. Consistent with our neighborhood definitions for greenness, we considered the presence of blue space within 250m and 1250m circular buffers surrounding a subject’s residence as a dichotomous measure. We also considered continuous Euclidian distance to the closest blue space.
Covariates
We considered individual, household and neighborhood covariates that vary with exposure to natural environments and have been identified as potential risk factors for depressive symptoms as potential confounders. Individual covariates were ascertained from GUTS surveys and included participant self-reported race/ethnicity (provided on the baseline questionnaire), grade level, age, and gender. Household covariates included income (reported by mothers in 2001), father’s education (reported by mothers in 1999), and maternal history of depression. Due to small numbers of participants reporting race/ethnicity other than non-Hispanic white, we combined these participants into a single category. Participants were considered to have a maternal history of depression if their mothers reported antidepressant use or depression diagnosis on any previous questionnaire, or if they scored above cutoff for probable depression on the Mental Health Inventory administered as part of the NHS II surveys.[34,35] We considered census tract demographics including median income, home value, percent white, and percent college educated using data from the 2000 United States Census.[36] We also considered region of the country and rural/urban classification using the US Census definitions,[37] and air pollution using household location estimates of concurrent and annual average particulate matter less than 2.5 microns in aerodynamic diameter (PM2.5) estimated from GIS-based spatio-temporal models of PM levels[38]. We included concurrent (July) PM2.5 in peak greenness models and 1999 average PM2.5 in all other models. Missing data on covariates was addressed by including a missing indicator.
Statistical Analysis
For our primary analysis we constructed logistic regression models for the outcome of high depressive symptoms (present/absent), using generalized estimating equations with a robust variance estimator to account for the fact that some mothers enrolled more than one child so observations are not independent. We considered a continuous measure of depressive symptoms as an alternate outcome. Since the full range of NDVI values is -1 to 1, we scaled NDVI exposures by the interquartile range to increase interpretability of the findings. For blue space, we considered two dichotomous measures of presence of blue space (yes versus no) and a continuous measure of distance to blue space.
For each exposure we constructed crude (unadjusted), fully-adjusted, and parsimonious models. Parsimonious models included only those covariates associated with the exposure and the outcome in this study population (participant race/ethnicity, paternal education, maternal history of depression, census region, census tract percent white). Fully-adjusted models included all covariates considered potential confounders based on published literature (all variables in the parsimonious model plus census tract median income, census tract median home value, census tract percent college degree, census tract urbanicity, participant gender, and household income). We constructed separate models for blue space and greenness in our primary analysis and also considered both exposures simultaneously.
We examined the possibility of a non-linear relation between each individual exposure and the odds of depressive symptoms non-parametrically with restricted cubic splines[39]. Tests of deviations from linearity used the likelihood ratio test, comparing the model with only the linear term to the model with the linear and the cubic spline terms. For exposures where linear relationships were not appropriate we used restricted cubic splines. We also assessed possible effect modification by region, gender, and grade level (grades 6–8 versus grades 9–12, to compare middle school and high school). We used a Wald test to assess statistically significant interactions and examined stratified models.
Results
The study population of 9,385 included more female than male participants (59% versus 41%) and participants were mostly non-Hispanic white (93%). Areas with higher greenness had lower population density and slightly lower median home values and household incomes. Individuals in the highest NDVI quintile were more likely to be non-Hispanic white, and more likely to come from households making less than $75,000 per year (Table 1). Subjects in the lowest quintile of distance to blue space, those living closest to the water, were more likely to come from households making $75,000 per year or more (Supplementary Table 1).
Table 1.
Distribution of selected covariates by quintiles of peak surrounding greenness (1250m) in 9,386 US adolescents in the Growing Up Today Study, 1999
| Over all | Greenness Q1 (N=1877) Least Green |
Greenness Q2 (N=1877) | Greenness Q3 (N=1877) | Greenness Q4 (N=1877) | Greenness Q5 (N=1877) Most Green |
|
|---|---|---|---|---|---|---|
| Normalized Difference Vegetation Index (NDVI) | 0.67±0.15 | 0.41 ± 0.09 | 0.63 ± 0.04 | 0.71 ± 0.02 | 0.77 ± 0.02 | 0.84 ± 0.03 |
| Census Tract Measures | ||||||
| College Educated (%) | 33 ± 17 | 37 ± 18 | 33 ± 17 | 33 ± 17 | 32 ± 18 | 28 ± 17 |
| White (%) | 90 ± 12 | 80 ± 16 | 90 ± 12 | 92 ± 9 | 93 ± 9 | 96 ± 5 |
| Median Home Value ($) | $168K ± $117K | $244K ± $168K | $159K ± $108K | $145K ± $73K | $150K ± $87K | $144K ± $94K |
| Median Household Income ($) | $67K ± $24K | $72K ± $27K | $66K ± $23K | $66K ± $21K | $66K ± $23K | $64K ± $24K |
| Population Density (people/mi2) | 2,495 ±4,793 | 5,428 ± 9,142 | 3,247 ± 3,145 | 2,076 ± 1,977 | 1,271 ± 1,452 | 453 ± 653 |
| Region (N (%)) | ||||||
| West | 1,403 (15) | 1,180 (63) | 147 (8) | 52 (3) | 16 (1) | 8 (0) |
| Midwest | 3,358 (36) | 107 (6) | 869 (46) | 946 (50) | 756 (40) | 680 (36) |
| South | 1,369 (15) | 451 (24) | 332 (18) | 232 (12) | 202 (11) | 152 (8) |
| Northeast | 3,255 (35) | 139 (7) | 529 (28) | 647 (34) | 903 (48) | 1,037 (55) |
| Urbanicity (N (%)) | ||||||
| Metropolitan | 7,717 (82) | 1,733 (92) | 1,635 (87) | 1,536 (82) | 1,489 (79) | 1,324 (71) |
| Micropolitan | 901 (10) | 73 (4) | 174 (9) | 192 (10) | 235 (13) | 227 (12) |
| Rural | 767 (8) | 71 (4) | 68 (4) | 149 (8) | 153 (8) | 326 (17) |
| Individual Measures | ||||||
| Female (N (%)) | 5,558 (59) | 1,125 (60) | 1,078 (57) | 1,117 (59) | 1,129 (60) | 1,109 (59) |
| Male (N (%)) | 3,827 (41) | 752 (40) | 799 (43) | 760 (41) | 748 (40) | 768 (41) |
| White (N (%)) | 8,738 (93) | 1,572 (84) | 1,761 (94) | 1,787 (95) | 1,805 (96) | 1,813 (97) |
| Household Income | ||||||
| ≥$75,000 (N (%)) | 4,887 (52) | 1078 (57) | 966 (51) | 980 (52) | 951 (51) | 912 (49) |
| <$75,000 (N (%)) | 2,828 (30) | 470 (25) | 563 (30) | 605 (32) | 578 (31) | 612 (33) |
| Missing (N (%)) | 1,670 (18) | 329 (18) | 348 (19) | 292 (16) | 348 (19) | 353 (19) |
| Maternal History of Depression (N(%)) | 2,701(29) | 509 (27) | 271 (30) | 557 (30) | 518 (28) | 546 (29) |
| Age (years) | 14.9± 1.6 | 14.9 ± 1.5 | 14.9 ± 1.6 | 14.9 ± 1.5 | 14.9 ± 1.6 | 14.9 ± 1.5 |
| July 1999 PM2.5 (μg/m3) | 16.2± 4.6 | 12.3 ± 4.8 | 17.0 ± 4.8 | 17.8 ± 4.0 | 17.9 ± 3.4 | 16.2 ± 3.6 |
| Any blue space within 1,250m (N(%)) | 3,170(34) | 482 (26) | 611 (33) | 625 (33) | 713 (38) | 739 (39) |
| Coast within 1,250m (N (%)) | 179(2) | 104 (6) | 40 (2) | 18 (1) | 12 (1) | 5 (0) |
| Interior water within 1,250m (N (%)) | 3,082(33) | 428 (23) | 597 (32) | 618 (33) | 704 (38) | 735 (39) |
The test for non-linearity suggested a linear relationship was appropriate for all models of greenness. Therefore Table 2 shows the results of crude, parsimonious, and fully adjusted logistic models for the association between a continuous measure of NDVI and the odds of high depressive symptoms. In parsimonious models, adjusted for participant race/ethnicity, paternal education, maternal history of depression, census region, census tract percent white, and estimated PM2.5 exposure, an IQR increase in peak greenness in the 1250m buffer around each participant’s home was associated with 11% lower odds of high depressive symptoms in fully adjusted models (OR 0.89, 95% CI 0.79–0.99). Annual average NDVI in the 1250m buffer was also associated with lower odds of depressive symptoms (OR per IQR increase 0.90, 95% CI 0.83, 0.99). Results for both peak and average NDVI at 250m were slightly attenuated compared to the 1250m results, but the direction of association was consistent. Full model results are presented in Supplementary Table 2.
Table 2.
Odds ratios and 95% confidence intervals for high depressive symptoms associated with a 1-IQRa increase in greenness, measured by peak and annual average NDVI at 250 and 1250 meters, in 9,385 adolescents living in the United States in 1999 (N=1,038 cases)
| Crude | Parsimoniousb | Fully Adjustedc | |
|---|---|---|---|
| Peak NDVI d | OR (95% CI) | OR (95% CI) | OR (95% CI) |
| 250me | 0.88 (0.81, 0.96) | 0.91 (0.82, 1.02) | 0.91 (0.82, 1.02) |
| 1250m | 0.87 (0.81, 0.94) | 0.89 (0.79, 0.99) | 0.88 (0.79, 0.98) |
| Annual Average | |||
| NDVIf | |||
| 250mg | 0.92 (0.85, 1.00) | 0.93 (0.86, 1.02) | 0.93 (0.86, 1.02) |
| 1250m | 0.90 (0.83, 0.98) | 0.90 (0.83, 0.99) | 0.90 (0.83, 0.99) |
1-IQR for Peak 250m: 0.232; Peak 1250m: 0.191; Annual Average 250m: 0.130; Annual Average 1250m: 0.115
Adjusted for census region, census tract percent white, estimated PM2.5, participant race, paternal education, maternal history of depression
Adjusted for census region, census tract percent white, census tract median income, census tract median home value, census tract percent college degree, census tract urbanicity, estimated PM2.5, participant race, participant gender, household income, paternal education, maternal history of depression
Peak NDVI is determined from July values
38 subjects not included because of missing NDVI values
Annual Average NDVI is calculated as the average of one measurement from each of the four seasons
61 subjects not included because of missing NDVI values
Estimates from fully adjusted models, where we further adjusted for census tract median income, census tract median home value, census tract percent college degree, census tract urbanicity, participant gender, and household income, were not substantially different from parsimonious models (Table 2). In sensitivity analyses we considered alternative cutoffs for “high depressive symptoms” at the top 5% and top 15% of subjects rather than the top 11.5%. The overall trends were similar to those observed with our primary cutoff (Supplementary Table 3).
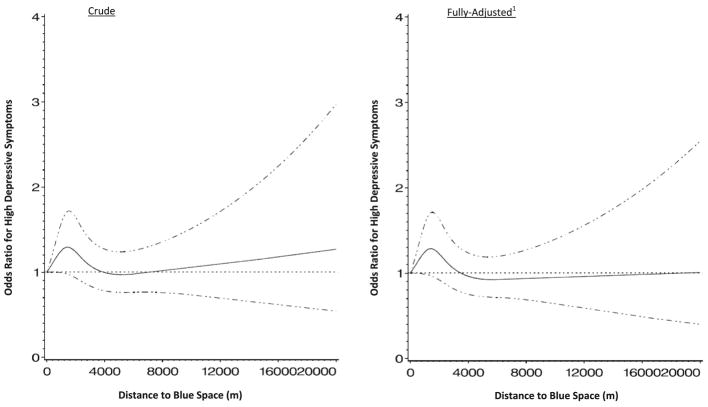
While there was no statistically significant interaction (p=0.64) between grade level and greenness, stratified models showed a suggestion of effect modification. The association between greenness and depressive symptoms was stronger in middle school students than it was in high school students (Table 3). For students in middle school, an IQR increase in peak greenness in the 1250 meter buffer was associated with 19% reduced odds of depressive symptoms (95% CI 0.68, 0.97) in fully adjusted models, while the association of greenness with depressive symptoms for high school students was substantially weaker. A similar pattern of stronger associations in middle school students was observed across all exposure characterizations. We did not observe effect modification by gender or region. Presence of blue space in either 250m or 1250m was not statistically significantly associated with depressive symptoms. This was true when all types of water were considered simultaneously and when interior and coastal water bodies were considered separately (Table 4). The results for coastal areas suggested a protective effect of living within 250m of the coast, but the confidence intervals were very wide (OR 0.29, 95% CI 0.04,2.01). We used splines to model the relationship between distance to blue space and depressive symptoms, and observed null associations in crude and adjusted models (Figure 1). When considered in models simultaneously, results for blue space and greenness were similar to what we observed in separate models, and an interaction between blue space and greenness did not reach statistical significance (p=0.36 for 1250m buffers). Results for continuous depressive symptoms were consistent in direction with the primary findings, but not statistically significant (Supplementary Table 4).
Table 3.
Odds ratios and 95% confidence intervals for high depressive symptoms associated with a 1-IQRa increase in greenness stratified by grade level in 9,385 adolescents living in the United States in 1999
| Middle School (6–8 grade) | |||
|---|---|---|---|
| N=3820 (417 cases) | |||
| Crude | Parsimoniousb | Fully Adjustedc | |
| Peak NDVId | |||
| 250me | 0.83 (0.73, 0.95) | 0.84 (0.70, 1.00) | 0.84 (0.70, 1.01) |
| 1250m | 0.83 (0.74, 0.94) | 0.82 (0.69, 0.97) | 0.81 (0.68, 0.97) |
| Annual Average NDVIf | |||
| 250mg | 0.84 (0.74, 0.96) | 0.87 (0.76, 1.00) | 0.87 (0.75, 1.00) |
| 1250m | 0.84 (0.74, 0.95) | 0.87 (0.75, 0.99) | 0.86 (0.75, 0.99) |
| High School (9–12 grade) | |||
| N=5565 (621 cases) | |||
| Crude | Parsimonious | Fully Adjusted | |
| Peak NDVI | |||
| 250mh | 0.92 (0.82, 1.02) | 0.97 (0.84, 1.12) | 0.96 (0.83, 1.11) |
| 1250m | 0.90 (0.82, 1.00) | 0.94 (0.81, 1.08) | 0.92 (0.80, 1.06) |
| Annual Average NDVI | |||
| 250mi | 0.98 (0.88, 1.09) | 0.98 (0.88, 1.09) | 0.98 (0.88, 1.09) |
| 1250m | 0.95 (0.85, 1.05) | 0.93 (0.84, 1.04) | 0.93 (0.83, 1.04) |
1-IQR for Peak 250m: 0.232; Peak 1250m: 0.191; Annual Average 250m: 0.130; Annual Average 1250m: 0.115
Adjusted for census region, census tract percent white, estimated PM2.5, participant race, paternal education, maternal history of depression
Adjusted for census region, census tract percent white, census tract median income, census tract median home value, census tract percent college degree, census tract urbanicity, estimated PM2.5, participant race, participant gender, household income, paternal education, maternal history of depression
Peak NDVI is determined from July values
17 subjects not included because of missing NDVI values
Annual Average NDVI is calculated as the average of one measurement from each of the four seasons
24 subjects not included because of missing NDVI values
21 subjects not included because of missing NDVI values
37 subjects not included because of missing NDVI values
Table 4.
Odds ratios and 95% confidence intervals for the relationship between high depressive symptoms and presence of water among 9,385 adolescents living in the United States (N = 1,038 cases)
| Presence of Water in 250m (yes vs. no) | Presence of Water in 1250m (yes vs. no) | |||||
|---|---|---|---|---|---|---|
| Crude | Parsimoniousa | Fully Adjustedb | Crude | Parsimonious | Fully Adjusted | |
| All water types | ||||||
| Yes | 0.89 (0.65 , 1.24) | 0.91 (0.66 , 1.27) | 0.92 (0.66 , 1.28) | 1.00 (0.88 , 1.15) | 1.02 (0.89, 1.17) | 1.03 (0.89 , 1.18) |
| No | Ref | Ref | Ref | Ref | Ref | Ref |
| Coast Only | ||||||
| Yes | 0.30 (0.04 , 2.05) | 0.28 (0.04 , 1.91) | 0.29 (0.04 , 2.01) | 1.01 (0.64 , 1.59) | 0.96 (0.61, 1.51) | 0.96 (0.60 , 1.53) |
| No | Ref | Ref | Ref | Ref | Ref | Ref |
| Interior water only | ||||||
| Yes | 0.95 (0.69 , 1.32) | 0.98 (0.70 , 1.36) | 0.99 (0.71 , 1.37) | 1.00 (0.87 , 1.15) | 1.01 (0.88, 1.17) | 1.02 (0.88 , 1.17) |
| No | Ref | Ref | Ref | Ref | Ref | Ref |
Adjusted for census region, census tract percent white, estimated PM2.5, participant race, paternal education, maternal history of depression
Adjusted for census region, census tract percent white, census tract median income, census tract median home value, census tract percent college degree, census tract urbanicity, estimated PM2.5, participant race, participant gender, household income, paternal education, maternal history of depression
Figure 1. Restricted cubic splines modeling the relationship between distance to blue space and odds of high depressive symptoms in 9,385 adolescents living in the United States in 1999 (N=1,038 cases).
1 Adjusted for census region, census tract percent white, census tract median income, census tract median home value, census tract percent college degree, census tract urbanicity, estimated PM2.5, participant race/ethnicity, participant gender, household income, paternal education, maternal history of depression
Discussion
In this population of 9,385 adolescents in the Growing Up Today Study we observed that surrounding greenness, but not proximity to blue space, was associated with lower odds of high depressive symptoms. This relationship was robust to adjustment for socioeconomic and other factors, and consistent across 250m and 1250m neighborhood definitions. Our findings are consistent with previous studies in both adults[1,9,12,22] and children[25,40], and add to the growing body of research suggesting a relationship between exposure to higher greenness and better mental health across the lifespan.
There was qualitative evidence of effect modification by grade, although the interaction was not statistically significant. We observed a significant inverse association between greenness and depression in middle school (6th–8th grade) students but not in high school (9th–12th grade) students. This may be due to differences in how students interact with their neighborhoods, particularly if high school students are more likely to attend schools further from home or access a broader range of destinations. High school students may also be affected by additional stressors such that greenness is less salient as a buffer against depression. Further research in this age range can help elucidate the diverse ways teenagers are influenced by their environments.
The observed relationships between residential proximity to blue space and depressive symptoms were consistently null across multiple measures of blue space. Huynh et al (2013) observed a weak relationship between blue space near school and emotional well-being in Canadian students of a similar age; the relationship was stronger in those students known to live near school[23]. A recent study in New Zealand used a view of water, rather than just proximity, to characterize blue space exposure and found water views were associated with lower likelihood of mental health disorders, based on self-reported measures of psychological distress[20]. The exposure in our study was limited to proximity to home and did not capture exposures near school or views of water. Moreover, the outcome measure was limited to one type of distress, as characterized by depressive symptoms. Future research should consider alternative characterizations of exposure such as whether natural environments are visible from home (viewshed analysis) and exposures beyond the residence.
This study had some important limitations. We were unable to account for the accessibility or quality of natural environments. If nearby green or blue spaces are inaccessible, unclean, or unsafe, they may prove insignificant or even detrimental to mental health. NDVI does not capture specific types of vegetation, merely its presence, and therefore our findings do not shed light on whether trees or grass, for example, are more significant for mental health. Further research incorporating sources such as land-use data can provide insights. We made assumptions about the geographic context most relevant to mental health, defining exposures as those in the areas 250m and 1250m around the home. These definitions are consistent with previous work and studies suggesting 1250m is an average walking distance for someone in this age range[32] but we may not have fully captured the relevant neighborhood environment. Our exposure definitions were based on study participants’ residential addresses; data were not available on the locations of schools or other places where adolescents may spend a considerable amount of time. We used the NHD, released in 2014, to assign exposures in 1999. Since less than 1% of hydrography changes over 50 years, we do not expect substantial misclassification to result. The fact that our outcomes were measured in 1999 should also be noted, but we do not expect substantial time trends in the relationship between nature and mental health and therefore our findings are still relevant to more modern cohorts.
Our study was cross-sectional, with depressive symptoms measured at a single point in time and contemporaneously with natural environment exposures. As a consequence, it is possible adolescents’ depressive symptoms were present prior to their exposure to their current natural environment. Residential self-selection bias is a concern, but since adolescents are not likely to be making decisions about the where they live we do not expect this to substantially impact our results. Our study population was predominantly non-Hispanic white and all participants were children of nurses, therefore our findings may not be generalizable to more diverse cohorts. Almost all participants lived in urban commuting areas and these findings may not be relevant to more rural areas.
This study of a nationwide sample of teenagers in the United States had several strengths including multiple objective measures of exposure to nature using a variety of geographic data combined with geocoded individual home addresses. Our study is among the first to consider the relationship between blue space and one measure of mental health in a United States cohort, taking advantage of detailed hydrography data not previously linked to health outcomes. The GUTS cohort includes detailed data on person-specific confounders, household characteristics and family history were available. Our relatively large sample size and the availability of data during the teenage years allowed us to observe suggestive effect modification by age.
While there is growing evidence of a relationship between natural environments and mental health, this study is among the first to focus specifically on adolescents. We observed that greenness was consistently associated with lower odds of high depressive symptoms, but we did not observe a similar relationship for proximity to blue spaces. These findings support the importance of incorporating green spaces into community planning and design. Residential development that incorporates vegetation can support the health of residents. Future studies should extend these findings using longitudinal analyses of this age range or take advantage of natural experiments, for example studies of the impact of improving surrounding greenness of an area, to better understand the relationship between greenness and mental health across the life course.
Supplementary Material
Implications and Contribution.
Nature, including both green spaces (vegetation) and blue (water) features, can foster mental health. In this study adolescents living in greener areas had lower depressive symptoms. Greater residential exposure to greenness or green spaces may be beneficial for mental health.
Acknowledgments
We thank the men and women in the Growing Up Today Study for their ongoing participation. A portion of these findings were presented at the International Society for Environmental Epidemiology annual meeting in September 2016. This work was funded by the National Institutes of Health (grants T32 ES 007069, K99 CA201542, R01 HD066963, R01 HD057368, P30 ES000002, R01 ES017017)
Abbreviations
- GUTS
Growing Up Today Study
- NDVI
Normalized Difference Vegetation Index
- IQR
Interquartile Range
- NHS II
Nurses’ Health Study II
- NHD
National Hydrography Dataset
- MRFS
McKnight Risk Factor Survey
- US
United States
Footnotes
Competing Financial Interests: The authors have no competing financial interests to declare.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.James P, Banay RF, Hart JE, et al. A Review of the Health Benefits of Greenness. Curr Epidemiol Reports. 2015:131–42. doi: 10.1007/s40471-015-0043-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gascon M, Trigueromas M, Martínez D, et al. Mental Health Benefits of Long-Term Exposure to Residential Green and Blue Spaces : A Systematic Review. Int J Environ Res Public Health. 2015:4354–79. doi: 10.3390/ijerph120404354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Berto R. Exposure to restorative environments helps restore attentional capacity. J Environ Psychol. 2005;25:249–59. [Google Scholar]
- 4.Bratman GN, Hamilton JP, Daily GC. The impacts of nature experience on human cognitive function and mental health. Ann N Y Acad Sci. 2012;1249:118–36. doi: 10.1111/j.1749-6632.2011.06400.x. [DOI] [PubMed] [Google Scholar]
- 5.Kaplan S. The restorative benefits of nature: Toward an integrative framework. J Environ Psychol. 1995;15:169–82. [Google Scholar]
- 6.Hartig T, Mitchell R, de Vries S, et al. Nature and health. Annu Rev Public Health. 2014;35:207–28. doi: 10.1146/annurev-publhealth-032013-182443. [DOI] [PubMed] [Google Scholar]
- 7.Völker S, Kistemann T. The impact of blue space on human health and well-being - Salutogenetic health effects of inland surface waters: A review. Int J Hyg Environ Health. 2011;214:449–60. doi: 10.1016/j.ijheh.2011.05.001. [DOI] [PubMed] [Google Scholar]
- 8.Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3:e442. doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cohen-Cline H, Turkheimer E, Duncan GE. Access to green space, physical activity and mental health: a twin study. J Epidemiol Community Health. 2015;69:523–9. doi: 10.1136/jech-2014-204667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Reklaitiene R, Grazuleviciene R, Dedele A, et al. The relationship of green space, depressive symptoms and perceived general health in urban population. Scand J Public Heal. 2014;42:669–76. doi: 10.1177/1403494814544494. [DOI] [PubMed] [Google Scholar]
- 11.Gubbels JS, Kremers SPJ, Droomers M, et al. The impact of greenery on physical activity and mental health of adolescent and adult residents of deprived neighborhoods: A longitudinal study. Heal Place. 2016;40:153–60. doi: 10.1016/j.healthplace.2016.06.002. [DOI] [PubMed] [Google Scholar]
- 12.van den Berg AE, Maas J, Verheij Ra, et al. Green Space as a Buffer Between Stressful Life Events and Health. Soc Sci Med. 2010;70:1203–10. doi: 10.1016/j.socscimed.2010.01.002. [DOI] [PubMed] [Google Scholar]
- 13.Markevych I, Tiesler CMT, Fuertes E, et al. Access to urban green spaces and behavioural problems in children: Results from the GINIplus and LISAplus studies. Environ Int. 2014;71:29–35. doi: 10.1016/j.envint.2014.06.002. [DOI] [PubMed] [Google Scholar]
- 14.Kuo FE, Faber Taylor A. A potential natural treatment for attention-deficit/hyperactivity disorder: Evidence from a national study. Am J Public Health. 2004;94:1580–6. doi: 10.2105/ajph.94.9.1580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Flouri E, Midouhas E, Joshi H. The role of urban neighbourhood green space in children’s emotional and behavioural resilience. J Environ Psychol. 2014;40:179–86. [Google Scholar]
- 16.Amoly E, Dadvand P, Forns J, et al. Green and Blue Spaces and Behavioral Development in Barcelona Schoolchildren : The BREATHE Project. 2014;122:1351–8. doi: 10.1289/ehp.1408215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Catalano RF, Fagan Aa, Gavin LE, et al. Worldwide application of prevention science in adolescent health. Lancet. 2012;379:1653–64. doi: 10.1016/S0140-6736(12)60238-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.National Institute of Mental Health. [accessed September 2016];Major Depression Among Adolescents. Available at: http://www.nimh.nih.gov/health/statistics/prevalence/major-depression-among-adolescents.shtml.
- 19.Pine DS, Cohen E, Cohen P, et al. Adolescent depressive symptoms as predictors of adult depression: Moodiness or mood disorder? Am J Psychiatry. 1999;156:133–5. doi: 10.1176/ajp.156.1.133. [DOI] [PubMed] [Google Scholar]
- 20.Nutsford D, Pearson AL, Kingham S, et al. Residential exposure to visible blue space (but not green space) associated with lower psychological distress in a capital city. Health Place. 2016;39:70–8. doi: 10.1016/j.healthplace.2016.03.002. [DOI] [PubMed] [Google Scholar]
- 21.Triguero-Mas M, Dadvand P, Cirach M, et al. Natural outdoor environments and mental and physical health: Relationships and mechanisms. Environ Int. 2015;77:35–41. doi: 10.1016/j.envint.2015.01.012. [DOI] [PubMed] [Google Scholar]
- 22.White MP, Alcock I, Wheeler BW, et al. Coastal proximity, health and well-being: Results from a longitudinal panel survey. Heal Place. 2013;23:97–103. doi: 10.1016/j.healthplace.2013.05.006. [DOI] [PubMed] [Google Scholar]
- 23.Huynh Q, Craig W, Janssen I, et al. Exposure to public natural space as a protective factor for emotional well-being among young people in Canada. BMC Public Health. 2013;13:407. doi: 10.1186/1471-2458-13-407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wheeler BW, White M, Stahl-Timmins W, et al. Does living by the coast improve health and wellbeing? Heal Place. 2012;18:1198–201. doi: 10.1016/j.healthplace.2012.06.015. [DOI] [PubMed] [Google Scholar]
- 25.De Vries S, Verheij Ra, Groenewegen PP, et al. Natural environments -- healthy environments? An exploratory analysis of the relationship between greenspace and health. Environ Plan A. 2003;35:1717–31. [Google Scholar]
- 26.Shisslak CM, Renger R, Sharpe T, et al. Development and evaluation of the McKnight risk factor survey for assessing potential risk and protective factors for disordered eating in preadolescent and adolescent girls. Int J Eat Disord. 1999;25:195–214. doi: 10.1002/(sici)1098-108x(199903)25:2<195::aid-eat9>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 27.Casey Ja, James P, Rudolph KE, et al. Greenness and birth outcomes in a range of Pennsylvania communities. Int J Environ Res Public Health. 2016:13. doi: 10.3390/ijerph13030311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dadvand P, de Nazelle A, Figueras F, et al. Green space, health inequality and pregnancy. Environ Int. 2012;40:110–5. doi: 10.1016/j.envint.2011.07.004. [DOI] [PubMed] [Google Scholar]
- 29.Rhew IC, Vander Stoep A, Kearney A, et al. Validation of the Normalized Difference Vegetation Index as a Measure of Neighborhood Greenness. Ann Epidemiol. 2011;21:946–52. doi: 10.1016/j.annepidem.2011.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kriegler F, Malila W, Nalepka RRW. Preprocessing transformations and their effects on multispectral recognition. Proc. Sixth Environ. Symp. Remote Sens; Ann Arbor, MI. 1969. pp. 97–131. [Google Scholar]
- 31.Carroll ML, DiMiceli CM, Sohlber RA, Townshend JR. 250m MODIS Normalized Difference Vegetation Index. Collection. 2004;4 [Google Scholar]
- 32.Austin SB, Melly SJ, Sanchez BN, et al. Clustering of Fast-Food Restaurants Around Schools: A Novel Application of Spatial Statistics to the Study of Food Environments. Am J Public Health. 2005;95:1575–81. doi: 10.2105/AJPH.2004.056341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wessel P, Smith WHF. A global, self-consistent, hierarchical, high-resolution shoreline database. J Geophys Res. 1996;101:8741. [Google Scholar]
- 34.Berwick DM, Murphy JM, Goldman PA, et al. Performance of a Five-Item Mental Health Screening Test. Med Care. 1991;29:169–76. doi: 10.1097/00005650-199102000-00008. [DOI] [PubMed] [Google Scholar]
- 35.Ware J, Snow Kristin K, Kosinski Mark, Gandek Barbara NEMCHHI. SF-36 health survey : Manual and interpretation guide. Boston: The Health Institute, New England Medical Center; 1996. [Google Scholar]
- 36.United States Census Bureau. 2000 United States Census. 2000. [Google Scholar]
- 37.Morrill R, Cromartie J, Hart G. Toward a Better Depiction of the United States. Management. n.d:727–48. [Google Scholar]
- 38.Yanosky JD, Paciorek CJ, Laden F, et al. Spatio-temporal modeling of particulate air pollution in the conterminous United States using geographic and meteorological predictors. Environ Health. 2014;13:63. doi: 10.1186/1476-069X-13-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Durrleman S, Simon R. Flexible regression models with cubic splines. Stat Med. 1989;8:551–61. doi: 10.1002/sim.4780080504. [DOI] [PubMed] [Google Scholar]
- 40.Maas J, Verheij RA, de Vries S, et al. Morbidity is related to a green living environment. J Epidemiol Community Health. 2009;63:967–73. doi: 10.1136/jech.2008.079038. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.