Abstract
Aims
Coronary computed tomography angiography (CCTA) and coronary artery calcium score (CACS) have prognostic value for coronary artery disease (CAD) events beyond traditional risk assessment. Age is a risk factor with very high weight and little is known regarding the incremental value of CCTA over CAC for predicting cardiac events in older adults.
Methods and results
Of 27 125 individuals undergoing CCTA, a total of 3145 asymptomatic adults were identified. This study sample was categorized according to tertiles of age (cut-off points: 52 and 62 years). CAD severity was classified as 0, 1–49, and ≥50% maximal stenosis in CCTA, and further categorized according to number of vessels ≥50% stenosis. The Framingham 10-year risk score (FRS) and CACS were employed as major covariates. Major adverse cardiovascular events (MACE) were defined as a composite of all-cause death or non-fatal MI. During a median follow-up of 26 months (interquartile range: 18–41 months), 59 (1.9%) MACE occurred. For patients in the top age tertile, CCTA improved discrimination beyond a model included FRS and CACS (C-statistic: 0.75 vs. 0.70, P-value = 0.015). Likewise, the addition of CCTA improved category-free net reclassification (cNRI) of MACE in patients within the highest age tertile (e.g. cNRI = 0.75; proportion of events/non-events reclassified were 50 and 25%, respectively; P-value <0.05, all). CCTA displayed no incremental benefit beyond FRS and CACS for prediction of MACE in the lower age tertiles.
Conclusion
CCTA provides added prognostic value beyond cardiac risk factors and CACS for the prediction of MACE in asymptomatic older adults.
Keywords: elderly, risk assessment, coronary computed tomography angiography, coronary artery calcium score
Introduction
In recent years, risk assessment of coronary artery disease (CAD) based on traditional risk factors such as Framingham 10-year risk score (FRS) has been widely used.1,2 However, previous studies have documented that these risk prediction tools display limited predictive value in asymptomatic populations within a primary prevention setting.3,4 To this end, much effort has focused on improving CAD risk prediction, particularly by employing more novel non-invasive imaging modalities such as the coronary artery calcium score (CACS).
Coronary computed tomography angiography (CCTA) has emerged as a highly useful non-invasive diagnostic tool for the diagnosis of CAD since it permits reliable visualization of the coronary arteries and identification of coronary artery stenosis.5–7 Even though it has clearly been demonstrated that coronary atherosclerosis shown by contrast-enhanced CCTA has predictive value regarding future cardiovascular disease events, several studies and analyses have shown no or very limited incremental value of CCTA beyond CACS in the general asymptomatic population.8,9 However, there was a demonstrable incremental value of CCTA for risk stratification beyond CACS in some high-risk populations, for example in patients with diabetes, high clinical risk score, or high calcium score.10–12
Advanced age is a strong risk factor for CAD development and its progression, and is closely associated with future adverse CAD outcomes.13 Little is known about the incremental benefit of CCTA for predicting adverse cardiac events beyond CACS in older adults. This study sought to evaluate the incremental value of CCTA beyond traditional cardiac risk factors and CACS in a sample of asymptomatic adults stratified by age.
Methods
Study population
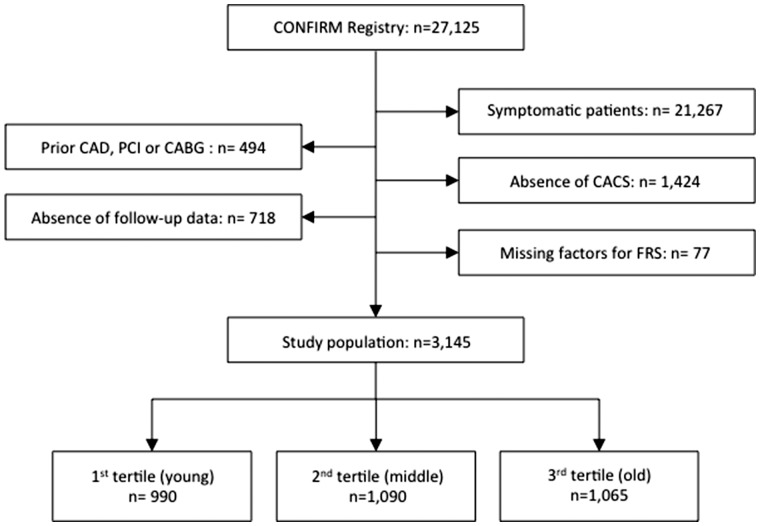
The Coronary CT Angiography Evaluation for Clinical Outcomes: An International Multicenter (CONFIRM) registry is a dynamic, international, multicentre, observational cohort study designed to evaluate the association between patient characteristics, CCTA findings and adverse clinical events. In total, 27 125 consecutive patients underwent CCTA at 12 centres in 6 countries (USA, Canada, Germany, Italy, Switzerland, and South Korea) between 2005 and 2009. Details of the rationale and design of the CONFIRM registry have been described previously.14 Various sub-studies have been published or submitted from the CONFIRM registry (see Supplementary data online, Table S1). For the purpose of this study, we excluded individuals who had previous chest pain or shortness of breath (n = 21 267), a prior history of obstructive CAD, coronary revascularization, myocardial infarction, or coronary artery bypass surgery (n = 494). We further excluded patients with an absence of concurrent CACS (n = 1424), lack of available follow-up data for all-cause mortality and non-fatal myocardial infarction (n = 718), or missing risk factor information that would preclude calculating the FRS (n = 77). Hence, a total 3175 patients remained for the current analysis (Figure 1). The study population was stratified into tertiles based on age and defined as: young (age < 52 years), intermediate (age 52–62 years), or old age (age > 62 years). Indications for performing CCTA in asymptomatic individuals were the assessment of CAD in patients with previous history of peripheral artery disease and/or cerebrovascular disease, pre-operational evaluation, pre-procedural assessment for electrophysiological procedure or congenital heart disease. However, site-initiated clinical indications were unavailable for review. The appropriate institutional review board committees approved the study protocol for all centres and informed consent was provided by all of the study participants.
Figure 1.
Study flow chart. CAD, coronary artery disease; PCI, percutaneous coronary intervention; CABG, coronary artery bypass graft; CACS, coronary artery calcium score; FRS, Framingham 10-year risk score.
DATA and image acquisition
CCTA was performed with site-specific protocols using multi-detector CT scanners with more than 64 detector rows and following Society of Cardiovascular Computed Tomography (SCCT) guidelines.15 CACS was calculated according to the methods described by Agatston et al.16 CCTA data were interpreted on-site using multi-planar reconstruction and maximum intensity projections. Results were documented per coronary segment based on a 16-segment modified SCCT coronary artery model. In each coronary segment, coronary atherosclerosis was defined as any tissue structure >1 mm2 either within the coronary artery lumen or adjacent to the coronary artery lumen that could be discriminated from surrounding pericardial tissue, epicardial fat, and the vessel lumen itself. The severity of obstructive CAD was defined as no CAD (0%), non-obstructive CAD (1–49%), or obstructive CAD (≥50%), and was further categorized according to the number of major epicardial vessels with the presence of ≥50% stenosis. Presence of ≥50% stenosis in the left main coronary artery was considered as a 3-vessel disease equivalent.
Study endpoint
Participants were followed for major adverse cardiovascular events (MACE), with MACE was defined as all-cause mortality and non-fatal MI. In this study, MI was defined according to the Universal Definition of Myocardial Infarction.17 The study procedures for follow-up have been previously described in detail.14 Briefly, ascertainment of death and MI events were determined by direct/telephone interview, as well as review of medical charts, and/or query of the national medical database at each institution by a dedicated physician and/or research nurse.
Statistical methods
Continuous variables are expressed as mean ± standard deviation (SD), and categorical variables are reported as counts with proportions. Comparisons between age tertiles were performed by use of a one-way analysis of variance for continuous variables (ANOVA) and by Pearson’s χ2 test for categorical measures. The FRS was calculated using a traditional risk stratification algorithm as described elsewhere,2 and participants were assigned to either low (<10%), intermediate (10–20%), or high (>20%) risk groups. For CACS, participants were categorized based on the following scores: 0–10, 11–100, and >100. The incidence of MACE (events per 1000 person-years at risk) was calculated to determine the risk of MACE across age tertiles. Cox proportional hazards regression was performed to test the interaction between older age and stenosis severity in CCTA on MACE. When assessing the incremental prognostic value of CCTA over risk factors and CACS, we employed the following models: FRS alone, FRS + CACS, and FRS + CACS + CCTA stenosis severity. Harrell’s C-index was used to assess discrimination of MACE events for each model and C-indexes were compared using the method described by DeLong et al.18 Category-free net reclassification improvement (cNRI) was used to estimate reclassification performance of each model. In addition, we performed cNRI to account for CCTA over CAC after stratified by FRS categories. All statistical analyses were performed using SAS (version 9. 3; SAS Institute, Cary, NC, USA) and STATA (version 14; StataCorp, College Station, TX, USA), and a P-value <0.05 was considered statistically significant.
Results
Baseline characteristics
The mean age in the 3175 patients was 56.6 ± 11.3 years and 62.7% were male. Tertiles of age were 18–51 years (young), 52–62 years (intermediate), and 63–92 years (elderly) (Table 1). The prevalence of hypertension, diabetes, and dyslipidaemia tended to rise with increasing age. Conversely, the proportion of male gender, current smoking status, and family history of CAD declined with advancing age. High CACS categories were more prevalent within the older age tertile. Likewise, the percentage of patients in higher FRS categories significantly increased with advancing age (see Table 1).
Table 1.
Baseline characteristics according to age tertiles
| Overall | Age tertiles |
P-value | |||
|---|---|---|---|---|---|
| First (n = 990) | Second (n = 1090) | Third (n = 1065) | |||
| Age (years) | 56.6 ± 11.3 | 43.8 ± 6.6 | 56.4 ± 2.9 | 68.6 ± 5.4 | <0.001 |
| Gender (male) | 1973 (62.7) | 701 (70.8) | 678 (62.2) | 594 (55.8) | <0.001 |
| BMI | 26.7 ± 4.5 | 26.8 ± 4.6 | 26.9 ± 4.8 | 26.3 ± 4.0 | <0.001 |
| Hypertension | 1439 (46.3) | 335 (34.2) | 505 (46.9) | 599 (57.1) | <0.001 |
| Diabetes | 392 (12.5) | 76 (7.7) | 132 (12.1) | 184 (17.3) | <0.001 |
| Dyslipidaemia | 1732 (55.5) | 428 (43.5) | 658 (60.8) | 646 (61.4) | <0.001 |
| Current smoking | 405 (12.9) | 169 (17.1) | 140 (12.8) | 96 (9.0) | <0.001 |
| Fhx of CAD | 789 (25.7) | 303 (31.3) | 283 (26.5) | 203 (19.5) | <0.001 |
| CACS category | <0.001 | ||||
| 0–10 | 1873 (59.6) | 766 (77.4) | 644 (59.1) | 463 (43.5) | |
| 10–100 | 575 (18.3) | 119 (12.0) | 220 (20.2) | 236 (22.2) | |
| 101–400 | 420 (13.4) | 75 (7.6) | 145 (13.3) | 200 (18.8) | |
| >400 | 277 (8.8) | 30 (3.0) | 81 (7.4) | 166 (16.6) | |
| FRS category | <0.001 | ||||
| Low (<10) | 1687 (53.6) | 853 (84.2) | 505 (46.3) | 329 (30.9) | |
| Intermediate (10–20) | 993 (31.6) | 118 (11.9) | 457 (41.9) | 418 (39.3) | |
| High (>20) | 465 (14.8) | 19 (1.9) | 128 (11.7) | 318 (29.9) | |
BMI, body mass index; CAD, coronary artery disease; CACS, coronary artery calcium score; FRS, Framingham 10 year risk score.
Prevalence and severity of CAD in CCTA
The prevalence of any CAD was 27.2% for the first tertile, and increased monotonically for the second (51.9%), and third (67.9%) tertiles, respectively (P-value for χ2 < 0.001, Figure 2). Similarly, the percentage reflecting the number of vessels with coronary stenosis was considerably higher for the highest age tertile (P-value <0.001, for all).
Figure 2.

Prevalence of CAD by tertiles of age (P-value <0.001, for all). CAD, coronary artery disease; VD, vessel disease; LM, left main coronary artery.
MACE during study follow-up
During a median 26 (interquartile range: 18–41) months of study follow-up, a total of 59 (1.9%) MACE events (e.g. 44 deaths and 15 MIs) occurred. Foremost, the incidence of MACE was 4.4 [95% confidence interval (95% CI): 2.4–8.3] and 4.9 (95% CI: 2.8–8.4) events per 1000 person-years for the first and second tertiles, respectively, increasing further to 13.9 (95% CI: 10.1–19.3) events per 1000 person years among those belonging to the third tertile (Table 2).
Table 2.
Major adverse cardiovascular events according to age tertiles
| Number of patients | Number of MACE (Deaths) | Incident MACE per 1000 person-years | |
|---|---|---|---|
| Overall | 3145 | 59 (44) | 7.9 (6.1–10.1) |
| Age tertiles | |||
| First | 990 | 10 (7) | 4.4 (2.4–8.3) |
| Second | 1090 | 13 (9) | 4.9 (2.8–8.4) |
| Third | 1065 | 36 (28) | 13.9 (10.1–19.3) |
MACE, major adverse cardiovascular event; MACE was defined as a composite of death or MI.
Prognostic value of CCTA beyond CACS and FRS
As expected, in the overall study population, CACS displayed further incremental benefit over the FRS model for predicting MACE (e.g. C-statistic for FRS = 0.63; 95% CI, 0.55–0.71 vs. FRS + CACS = 0.71; 95% CI, 0.64–0.78, P for difference = 0.022, Table 3). In similar fashion, CCTA stenosis significantly increased the C-statistic when added to the FRS model (Table 3). Although, in the overall population, there appeared to be no further incremental value when CCTA was added to the FRS model that also contained CACS. The results of the interaction test between older age group and CCTA stenosis for MACE showed significant result (P-value 0.005).
Table 3.
Discriminatory value of coronary computed tomography angiography for predicting major adverse cardiovascular events
| Model | C-statistic | 95% CI |
P-value |
|
|---|---|---|---|---|
| Versus FRS model | Versus FRS + CACS | |||
| Overall | ||||
| FRS | 0.63 | 0.55–0.71 | ||
| FRS + CACS | 0.71 | 0.64–0.78 | 0.022 | |
| FRS + CACS + CCTA stenosis | 0.72 | 0.65–0.80 | 0.015 | 0.333 |
| First tertile | ||||
| FRS | 0.53 | 0.31–0.74 | ||
| FRS + CACS | 0.53 | 0.31–0.74 | 0.990 | |
| FRS + CACS + CCTA stenosis | 0.56 | 0.34–0.78 | 0.542 | 0.424 |
| Second tertile | ||||
| FRS | 0.60 | 0.42–0.78 | ||
| FRS + CACS | 0.65 | 0.48–0.83 | 0.370 | |
| FRS + CACS + CCTA stenosis | 0.60 | 0.42–0.78 | 0.978 | 0.058 |
| Third tertile | ||||
| FRS | 0.58 | 0.47–0.68 | ||
| FRS + CACS | 0.70 | 0.63–0.77 | 0.031 | |
| FRS + CACS + CCTA stenosis | 0.75 | 0.68–0.83 | 0.004 | 0.015 |
FRS, Framingham 10-year risk score; CACS, coronary artery calcium score; CCTA, coronary computed tomography angiography.
Notably, the addition of CCTA stenosis improved discrimination beyond FRS and CACS only for those belonging to the highest (third) age tertile (e.g. C-statistic for FRS + CACS = 0.70; 95% CI, 0.47–0.68 vs. FRS + CACS + CCTA stenosis = 0.75; 95% CI, 0.68–0.83, P for difference = 0.015, Table 3). In contrast, CCTA displayed no incremental benefit over FRS and CACS for discrimination of MACE amongst the lower age tertiles. For those in the uppermost age tertile, CCTA stenosis led to improved reclassification of MACE when added to FRS and CACS (Table 4). That is, the addition of CCTA to the FRS + CACS model correctly improved reclassification of events (cNRI = 50%) and non-events (cNRI = 25%) for those belonging to the third age tertile (P-value <0.05, for both).
Table 4.
Performance of coronary computed tomography angiography for reclassifying major adverse cardiovascular events
| Model | Versus FRS |
Versus FRS + CACS |
||||||
|---|---|---|---|---|---|---|---|---|
| cNRI | 95% CI | % Events reclassified | % Non-events reclassified | cNRI | 95% CI | % Events reclassified | % Non-events reclassified | |
| Overall | ||||||||
| FRS + CACS | 0.52* | 0.26–0.77 | −5 | 57* | ||||
| FRS + CACS + CCTA stenosis | 0.49* | 0.23–0.74 | 12 | 37* | 0.47* | 0.22–0.73 | 8 | 39* |
| First Tertile | ||||||||
| FRS + CACS | −0.01 | −0.39–0.36 | −80* | 79* | ||||
| FRS + CACS + CCTA stenosis | 0.22 | −0.35–0.79 | −40 | 62* | −0.04 | −0.53–0.46 | −60 | 57* |
| Second Tertile | ||||||||
| FRS + CACS | 0.52 | −0.03–1.06 | −8 | 59* | ||||
| FRS + CACS + CCTA stenosis | −0.06 | −0.57–0.44 | −38 | 32* | −0.18 | −0.64–0.28 | −54 | 36* |
| Third Tertile | ||||||||
| FRS + CACS | 0.50* | 0.17–0.82 | 17 | 33* | ||||
| FRS + CACS + CCTA stenosis | 0.62* | 0.32–0.92 | 44* | 18* | 0.75* | 0.46–1.04 | 50* | 25* |
FRS, Framingham 10-year risk score; cNRI, category-free net reclassification index; CACS, coronary artery calcium score; CCTA, coronary computed tomography angiography.
P < 0.05.
Reclassification of elderly population by CCTA over CACS and FRS
In the uppermost age tertile, 10 MACE events (2.1%) occurred among 466 patients with 0–10 CACS (Table 5). Seven patients have non-obstructive CAD or obstructive CAD by CCTA, though CACS classified these participants as low risk category (CACS 0–10). Conversely, 101 (65.6%) patients with CACS > 400 have obstructive CAD by CCTA. In those patients with high CACS, the prevalence of MACE is significantly lower in patients with no or non-obstructive CAD (3%, 2/65) compared with patients with obstructive CAD (11.8%, 12/101).
Table 5.
MACE risk reclassification comparing CACS and CCTA categories across FRS group in third age tertile
| Third age tertile |
Reclassification accounting for CAD severity by CCTA |
||||
|---|---|---|---|---|---|
| CACS category | No CAD | Non-obstructive CAD | Obstructive CAD—single vessel | Obstructive CAD—multi vessel | Total number |
| Overall | |||||
| Participants with events | |||||
| 0–10 | 3 | 5 | 2 | 0 | 10 |
| 10–100 | 0 | 3 | 2 | 0 | 5 |
| 101–400 | 0 | 1 | 3 | 3 | 7 |
| >400 | 0 | 2 | 6 | 6 | 14 |
| Total number | 3 | 11 | 13 | 9 | 36 |
| Participants without events | |||||
| 0–10 | 303 | 123 | 19 | 11 | 456 |
| 10–100 | 22 | 176 | 21 | 9 | 228 |
| 101–400 | 10 | 123 | 42 | 18 | 193 |
| >400 | 4 | 59 | 39 | 50 | 152 |
| Total number | 339 | 481 | 121 | 88 | 1029 |
| cNRI | 51.2%, P = 0.001 | ||||
| FRS < 10% | |||||
| Participants with events | |||||
| 0–10 | 0 | 0 | 0 | 0 | 0 |
| 10–100 | 0 | 0 | 0 | 0 | 0 |
| 101–400 | 0 | 1 | 2 | 0 | 3 |
| >400 | 0 | 1 | 1 | 3 | 5 |
| Total number | 0 | 2 | 3 | 3 | 8 |
| Participants without events | |||||
| 0–10 | 138 | 32 | 4 | 3 | 177 |
| 10–100 | 6 | 55 | 4 | 2 | 67 |
| 101–400 | 3 | 28 | 15 | 3 | 49 |
| >400 | 2 | 11 | 7 | 8 | 28 |
| Total number | 149 | 126 | 30 | 16 | 321 |
| cNRI | −5.2%, P = 0.558 | ||||
| FRS 10–20% | |||||
| Participants with events | |||||
| 0–10 | 3 | 2 | 1 | 0 | 6 |
| 10–100 | 0 | 2 | 1 | 0 | 3 |
| 101–400 | 0 | 0 | 1 | 2 | 3 |
| >400 | 0 | 0 | 3 | 0 | 3 |
| Total number | 3 | 4 | 6 | 2 | 15 |
| Participants without events | |||||
| 0–10 | 124 | 51 | 4 | 3 | 182 |
| 10–100 | 12 | 73 | 7 | 2 | 94 |
| 101–400 | 5 | 58 | 10 | 7 | 80 |
| >400 | 1 | 20 | 13 | 13 | 47 |
| Total number | 142 | 202 | 34 | 25 | 403 |
| cNRI | 45.2%, P = 0.043 | ||||
| FRS >20% | |||||
| Participants with events | |||||
| 0–10 | 0 | 3 | 1 | 0 | 4 |
| 10–100 | 0 | 1 | 1 | 0 | 2 |
| 101–400 | 0 | 0 | 0 | 1 | 1 |
| >400 | 0 | 1 | 2 | 3 | 6 |
| Total number | 0 | 5 | 4 | 4 | 13 |
| Participants without events | |||||
| 0–10 | 41 | 40 | 11 | 5 | 97 |
| 10–100 | 4 | 48 | 10 | 5 | 67 |
| 101–400 | 2 | 37 | 17 | 8 | 64 |
| >400 | 1 | 28 | 19 | 29 | 77 |
| Total number | 48 | 153 | 57 | 47 | 305 |
| cNRI | 67.7%, P = 0.009 | ||||
MACE, major adverse cardiovascular event; FRS, Framingham 10-year risk score; cNRI, category-free net reclassification index; CACS, coronary artery calcium score; CCTA, coronary computed tomography angiography.
When we further stratified by FRS categories for participants in the uppermost age tertile, the improvement of reclassification of CCTA over CAC was particularly significant among patients with intermediate and high FRS (45.2% in intermediated FRS and 67.6% in high FRS, P-value <0.05 for both) (Table 5). Notably, participants with CACS 0–10 and 10–100 did not experience MACE event in low FRS group.
Discussion
In this prospective observational multicentre registry, CCTA improved risk prediction above and beyond FRS and CACS among older aged adults. In particular, CCTA improved reclassification of elderly patients with and without MACE when added to a prediction model that comprised FRS and CACS. However, no further benefit of CCTA was observed in younger and middle aged adults. These results are fitting with prior studies that documented that CCTA provides added benefit beyond CACS in selected subgroups of asymptomatic high-risk patients.10–12,19
Previous studies have reported that CCTA might prove useful for identifying subclinical CAD in certain asymptomatic populations.20,21 Our group previously explored the predictive value of traditional risk factors, CACS, and CCTA for future CAD events in 7590 asymptomatic patients from the CONFRIM registry.8 On the background of those findings, although CCTA and CACS individually improved performance over the base model (e.g. FRS and traditional CAD risk factors), the addition of CCTA beyond a model that contained CACS failed to provide a clinically meaningful benefit. Despite this, few prior studies have reported an improved prognostic benefit of CCTA over CACS in asymptomatic individuals who presented with high risk of CAD. In another study utilizing the same cohort of the current study, CCTA findings improved risk stratification over and above CACS in asymptomatic diabetic patients, thus demonstrating the incremental benefit of CCTA beyond CACS in selected populations (Min et al.10). Not only from CONFIRM registry, Plank et al.11 revealed that CCTA parameters, especially non-calcified plaque burden, afforded additional prognostic value over CACS in 711 asymptomatic patients with high risk of CAD based on clinical risk factors.10 However, few studies have established whether the incremental value of CCTA beyond CACS and cardiac risk factors differs as a function of age. In the current study, CCTA appeared to offer additional prognostic benefit for risk stratification beyond traditional risk factors as well as CACS in the uppermost tertile, representative of older adults. To our knowledge, this is first study to assess the added predictive value of CCTA in an asymptomatic population stratified by age.
CAD risk prediction strategies often rely on the risk burden of CAD. To this end, although CACS has been shown to provide risk prediction beyond traditional risk factor scoring algorithms,22,23 prior evidence has reported that the prognostic benefit of screening for CACS often differs according to risk burden depending on the study population.24,25 Compared with CACS, a widely used risk prediction tool in asymptomatic individuals, CCTA is capable of further detecting coronary plaque burden related to the location, severity, as well as plaque characteristics. Recently, our group reported another subgroup study from the CONFIRM registry, showing CCTA provided incremental benefit towards predicting adverse cardiovascular events in patients whose CACS was >100—indicative of more than moderate CAD risk.12 When compared with the aforementioned study, similar results were observed in the current investigation—the incidence of MACE was very low in patients with low CVD risk (e.g. CAC < 100 or low FRS) and CCTA did not improve reclassification over CACS in patients with low FRS, even in the third age tertile group. However, the current study suggested that age, as baseline demographical information, might be considered when making a personalized decision for cardiovascular risk assessment at the time of evaluation. Aging reflects a non-modifiable factor that further provokes the development of atherosclerosis and progression of its components, the latter of which have previously been shown to increase in tandem with advancing age.26 Further still, the present observations have demonstrated that more than one-third of patients in the uppermost tertile of age presented with a CACS more than 100. In light of this, our findings support the contention that CCTA might serve a useful role as an effective screening tool in patients considered to be at moderate-to-high-risk, such as those with high CACS or those representative of an elderly population. Therefore, when we assess the CVD risk in asymptomatic population in clinical practice, we may need to pay special attention for CVD risk screening strategy in elderly patients rather than younger patients. CCTA can be a useful additive screening imaging tool over conventional risk scoring system as well as CACS.
In recent past, several studies emphasized the importance of CCTA for reclassifying asymptomatic individuals, particularly the correct reclassification of non-events. From one of the sub-studies from the CONFIRM registry comprised of 3217 asymptomatic patients stratified by CACS, CCTA improved reclassification, specifically in patients presenting with high CACS.12 That is, CCTA reclassified patients with high CACS, wherein the results indicated correct reclassification primarily in those without an event (e.g. NRI = 0.55 non-events correctly reclassified vs. 0.07 events correctly reclassified). Likewise, Dedic et al.19 reported the prognostic value of CCTA in patients with at least one CAD risk factor but without cardiac symptoms. Notably, the latter study found CCTA correctly reclassified only individuals without an event (e.g. NRI = 0.32 non-events correctly reclassified vs. 0.02 events correctly reclassified). The current findings substantively extend upon these prior findings whereby CCTA demonstrated correct reclassification not only among individuals without an event but also among those who experienced an event. Indeed, although it is well known that CACS > 400 is indicative of high risk for future adverse outcomes, even non-obstructive CAD, among patients with CACS > 400 most patients with events have obstructive CAD. Only two (3%) patients with no or non-obstructive CAD experienced MACE in current study. In lieu of this, CCTA may potentially afford correct reclassification of events as well as non-events, at least in older asymptomatic individuals. This is perhaps an important observation, given that approximately half of the US population aged >65 years are considered statin eligible under the American College of Cardiology/American Heart Association 2013 guidelines.27
The present study was not free from limitations. Although the CONFIRM registry was prospective in nature, we cannot discount the possibility of selection and follow-up bias as well as the potential for unmeasured confounding factors that might have influenced the clinical endpoints of this study. We included all-cause mortality in the composite endpoint. As information regarding cause-specific mortality was unavailable in the CONFIRM registry, the proportion of deaths by cardiovascular events is unknown in the current study. In addition, the acquisition of information regarding downstream pharmacological and/or interventional management after CCTA was unavailable. Therefore, the potential impact of CCTA result for treatment choices and downstream events remains unknown. It also bears mentioning that the follow-up duration was relatively short, and the rate of events were particularly low in the first and second age tertiles, which might offer some explanation to the suboptimal prognostic value of CCTA when added to conventional risk factors as well as CACS in those groups. The current study utilized the FRS for the purpose of traditional risk stratification based on 10-year risk prediction. A pressing limitation when employing this approach is the substantial disparity related to the duration of risk prediction, particularly when 10-year FRS is applied to the present study’s 26-month median follow-up duration. As such, any long-term predictive value of the current study’s CCTA findings should be interpreted with caution. Forthcoming studies with a lengthier follow-up duration are required to determine whether CCTA improves risk prediction beyond traditional approaches in asymptomatic populations.
Conclusion
In this study, CCTA demonstrated improved risk prediction and reclassification above and beyond FRS and CACS among asymptomatic older adults. CCTA may be considered useful for extending the predictive utility beyond currently available cardiac risk factors in the elderly.
Supplementary data
Supplementary data are available at European Heart Journal - Cardiovascular Imaging online.
Funding
The research reported in this publication was funded by the Heart Lung and Blood Institute of the National Institutes of Health (Bethesda, MD, USA) under award number R01HL115150, and also supported, in part, by a generous gift from the Dalio Institute of Cardiovascular Imaging (New York, NY, USA) and the Michael Wolk Foundation (New York, NY, USA).
Conflicts of interest: Dr. James Min serves on the scientific advisory board of Arineta, has ownership in MDDX, and has a research agreement with GE Healthcare. Dr Gianluca Pontone is a member of the speakers’ bureau for GE Healthcare, Bracco, and Medtronic. He also conducts research for GE Healthcare and Heartflow. Dr Matthew Budoff receives grant support from GE Healthcare and the NIH. All other authors have no relevant disclosures.
Supplementary Material
References
- 1. Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive summary of the third report of the national cholesterol education program (ncep) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). JAMA 2001;285:2486–97. [DOI] [PubMed] [Google Scholar]
- 2. National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) final report. Circulation 2002;106:3143–421. [PubMed] [Google Scholar]
- 3. Brindle P, Beswick A, Fahey T, Ebrahim S.. Accuracy and impact of risk assessment in the primary prevention of cardiovascular disease: a systematic review. Heart 2006;92:1752–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Akosah KO, Schaper A, Cogbill C, Schoenfeld P.. Preventing myocardial infarction in the young adult in the first place: how do the National Cholesterol Education Panel III guidelines perform? J Am Coll Cardiol 2003;41:1475–9. [DOI] [PubMed] [Google Scholar]
- 5. Budoff MJ, Dowe D, Jollis JG, Gitter M, Sutherland J, Halamert E. et al. Diagnostic performance of 64-multidetector row coronary computed tomographic angiography for evaluation of coronary artery stenosis in individuals without known coronary artery disease: results from the prospective multicenter ACCURACY (Assessment by Coronary Computed Tomographic Angiography of Individuals Undergoing Invasive Coronary Angiography) trial. J Am Coll Cardiol 2008;52:1724–32. [DOI] [PubMed] [Google Scholar]
- 6. Miller JM, Rochitte CE, Dewey M, Arbab-Zadeh A, Niinuma H, Gottlieb I. et al. Diagnostic performance of coronary angiography by 64-row CT. N Engl J Med 2008;359:2324–36. [DOI] [PubMed] [Google Scholar]
- 7. Taylor AJ, Cerqueira M, Hodgson JM, Mark D, Min J, O'gara P. et al. ACCF/SCCT/ACR/AHA/ASE/ASNC/NASCI/SCAI/SCMR 2010 appropriate use criteria for cardiac computed tomography. A report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, the Society of Cardiovascular Computed Tomography, the American College of Radiology, the American Heart Association, the American Society of Echocardiography, the American Society of Nuclear Cardiology, the North American Society for Cardiovascular Imaging, the Society for Cardiovascular Angiography and Interventions, and the Society for Cardiovascular Magnetic Resonance. J Am Coll Cardiol 2010;56:1864–94. [DOI] [PubMed] [Google Scholar]
- 8. Cho I, Chang HJ, Sung JM, Pencina MJ, Lin FY, Dunning AM. et al. Coronary computed tomographic angiography and risk of all-cause mortality and nonfatal myocardial infarction in subjects without chest pain syndrome from the CONFIRM Registry (coronary CT angiography evaluation for clinical outcomes: an international multicenter registry). Circulation 2012;126:304–13. [DOI] [PubMed] [Google Scholar]
- 9. Choi EK, Choi SI, Rivera JJ, Nasir K, Chang SA, Chun EJ. et al. Coronary computed tomography angiography as a screening tool for the detection of occult coronary artery disease in asymptomatic individuals. J Am Coll Cardiol 2008;52:357–65. [DOI] [PubMed] [Google Scholar]
- 10. Min JK, Labounty TM, Gomez MJ, Achenbach S, Al-Mallah M, Budoff MJ. et al. Incremental prognostic value of coronary computed tomographic angiography over coronary artery calcium score for risk prediction of major adverse cardiac events in asymptomatic diabetic individuals. Atherosclerosis 2014;232:298–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Plank F, Friedrich G, Dichtl W, Klauser A, Jaschke W, Franz WM. et al. The diagnostic and prognostic value of coronary CT angiography in asymptomatic high-risk patients: a cohort study. Open Heart 2014;1:e000096.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Cho I, Chang HJ, Oh B, Shin S, Sung JM, Lin FY. et al. Incremental prognostic utility of coronary CT angiography for asymptomatic patients based upon extent and severity of coronary artery calcium: results from the COronary CT Angiography EvaluatioN For Clinical Outcomes InteRnational Multicenter (CONFIRM) Study. Eur Heart J 2015;36:501–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Odden MC, Coxson PG, Moran A, Lightwood JM, Goldman L, Bibbins-Domingo K.. The impact of the aging population on coronary heart disease in the United States. Am J Med 2011;124:827–33.e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Min JK, Dunning A, Lin FY, Achenbach S, Al-Mallah MH, Berman DS. et al. Rationale and design of the CONFIRM (COronary CT Angiography EvaluatioN For Clinical Outcomes: An InteRnational Multicenter) Registry. J Cardiovasc Comput Tomogr 2011;5:84–92. [DOI] [PubMed] [Google Scholar]
- 15. Raff GL, Abidov A, Achenbach S, Berman DS, Boxt LM, Budoff MJ. et al. SCCT guidelines for the interpretation and reporting of coronary computed tomographic angiography. J Cardiovasc Comput Tomogr 2009;3:122–36. [DOI] [PubMed] [Google Scholar]
- 16. Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M Jr, Detrano R.. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol 1990;15:827–32. [DOI] [PubMed] [Google Scholar]
- 17. Thygesen K, Alpert JS, White HD.. Universal definition of myocardial infarction. Eur Heart J 2007;28:2525–38. [DOI] [PubMed] [Google Scholar]
- 18. DeLong ER, DeLong DM, Clarke-Pearson DL.. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 1988;44:837–45. [PubMed] [Google Scholar]
- 19. Dedic A, Ten Kate GJ, Roos CJ, Neefjes LA, de Graaf MA, Spronk A. et al. Prognostic value of coronary computed tomography imaging in patients at high risk without symptoms of coronary artery disease. Am J Cardiol 2016;117:768–74. [DOI] [PubMed] [Google Scholar]
- 20. McEvoy JW, Blaha MJ, Nasir K, Yoon YE, Choi EK, Cho IS. et al. Impact of coronary computed tomographic angiography results on patient and physician behavior in a low-risk population. Arch Intern Med 2011;171:1260–8. [DOI] [PubMed] [Google Scholar]
- 21. Lee HJ, Kim YJ, Hur J, Lee JW, Hong YJ, Kim HY. et al. Prevalence and extent of atherosclerotic coronary artery disease and related outcome based on coronary computed tomographic angiography in asymptomatic elderly patients: retrospective cohort study. Int J Cardiovasc Imaging 2014;30:669–76. [DOI] [PubMed] [Google Scholar]
- 22. Greenland P, LaBree L, Azen SP, Doherty TM, Detrano RC.. Coronary artery calcium score combined with Framingham score for risk prediction in asymptomatic individuals. JAMA 2004;291:210–5. [DOI] [PubMed] [Google Scholar]
- 23. Detrano R, Guerci AD, Carr JJ, Bild DE, Burke G, Folsom AR. et al. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med 2008;358:1336–45. [DOI] [PubMed] [Google Scholar]
- 24. Okwuosa TM, Greenland P, Ning H, Liu K, Bild DE, Burke GL. et al. Distribution of coronary artery calcium scores by Framingham 10-year risk strata in the MESA (Multi-Ethnic Study of Atherosclerosis) potential implications for coronary risk assessment. J Am Coll Cardiol 2011;57:1838–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Okwuosa TM, Greenland P, Ning H, Liu K, Lloyd-Jones DM.. Yield of screening for coronary artery calcium in early middle-age adults based on the 10-year Framingham Risk Score: the CARDIA study. JACC Cardiovasc Imaging 2012;5:923–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Wang JC, Bennett M.. Aging and atherosclerosis: mechanisms, functional consequences, and potential therapeutics for cellular senescence. Circ Res 2012;111:245–59. [DOI] [PubMed] [Google Scholar]
- 27. Goff DC Jr, Lloyd-Jones DM, Bennett G, Coady S, D'agostino RB, Gibbons R. et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014;129:S49–73. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.