Abstract
Middle ear surgery is usually performed using a surgical microscope. Initially, in otorhinolaryngology practice, endoscopes were used for paranasal sinus surgeries. It was only later that they were applied in the area of otology. In otologic surgeries, endoscopes were first used to visualize the middle ear, before being used to assist with visualization of instruments during cholesteatoma surgeries, although they are still not used alone in various otologic surgeries. As in other surgical fields, there is also a trend towards minimally invasive intervention in the field of otorhinolaryngology. Smaller incisions performed under the guidance of endoscopes are preferred over conventional large incisions. Using this approach, improved outcomes can be achieved and postoperative morbidities can be reduced. In addition, the outcomes of grafts performed using the endoscopic approach are similar to that achieved by the microscopic approach. Therefore, endoscopic ear surgery implementations are becoming increasingly popular.
Keywords: Endoscopic, Tympanoplasty, Myringoplasty
1. Introduction
Although microscopes have been effectively used in otology practice for many years, recently there has been no significant improvement in their basic optical characteristics. Endoscopes have long been used in the field of otorhinolaryngology for sinus surgeries. However, their implementation in otology practice has been gradual. Endoscopes were initially used only to visualize the middle ear. They later started to be used in addition to microscopes during all surgical procedures involving the middle ear, and eventually they are now sometimes used as standalone instruments (Tuncer, 2016). For surgical purposes, the earliest use of endoscopes in otology dates back to the 1990s (Thomassin et al., 1993, McKennan, 1993). Tarabichi (1997) published the first report of patients treated using the endoscopic approach alone. There has been a recent increase in the number of publications reporting that standard otologic interventions can be performed endoscopically (Thomassin et al., 1990, Tarabichi, 2010). The endoscopic approach can also be preferred in procedures such as ventilation tube insertion, myringoplasty, tympanoplasty, ossicular reconstruction for malformation and ossicle trauma, cholesteatoma surgeries, otosclerosis surgeries and cochlear implantation (Tarabichi, 2000, Migirov et al., 2011, Ayache et al., 2008, Kakehata et al., 2006, Poe and Bottrill, 1994).
1.1. Myringoplasty and tympanoplasty
Tympanoplasty and myringoplasty are commonly used procedures for the treatment of chronic otitis media. Myringoplasty is a surgical procedure performed only on the tympanic membrane, without manipulation on the middle ear or the ossicles (Sarkar, 2013). Tympanoplasty involves eradication of the disease in the middle ear, repair of the perforated tympanic membrane and restoration of hearing. Endaural, transcanal and postauricular approaches are used during myringoplasty and tympanoplasty. Recently, transcanal endoscopic approaches have become popular. The endoscopic approach provides a much larger field of view. When training interns, this view translates into a better visual image, as the middle ear and the ossicles can be visualized through the perforation. In the microscopic approach, a retroauricular approach is preferred for anterior perforations, while the endaural approach is preferred for posterior perforations, and small perforations are commonly treated using the transcanal approach (Coskun et al., 2006, Kessler et al., 1994, Jako, 1967). The tortuous anatomy of the outer ear and bone protrusions negatively affect microscopic views and impair visualization of deep structures. Canalplasty may be required in such cases. On the other hand, the panoramic and wide angled views obtained by the back and forth movements of the endoscope are not affected by the tortuous anatomy of the external ear canal. The view beyond the end of the endoscopy is easily presented to the surgeon, while magnification can also be achieved through various endoscope manipulations, eliminating the need for canalplasty (Patel et al., 2015).
1.2. Equipment for endoscopic approach
Endoscopes: 0°, 30° and 45° rigid endoscopes with diameters of 2.7 mm, 3 mm and 4 mm and lengths of 16–18 cm (Fig. 1).
Fig. 1.
Endoscopes used in otologic surgery.
Video equipment: High-resolution camera and monitor, light source, fiberoptic cable.
Instruments: Surgical instruments used for conventional otologic surgeries.
The monitor should be placed facing the surgeon. A microscope can be made available to enable a switch to microscopic surgery, when necessary.
1.2.1. Advantages and disadvantages of endoscopic approach
Advantages
-
1.
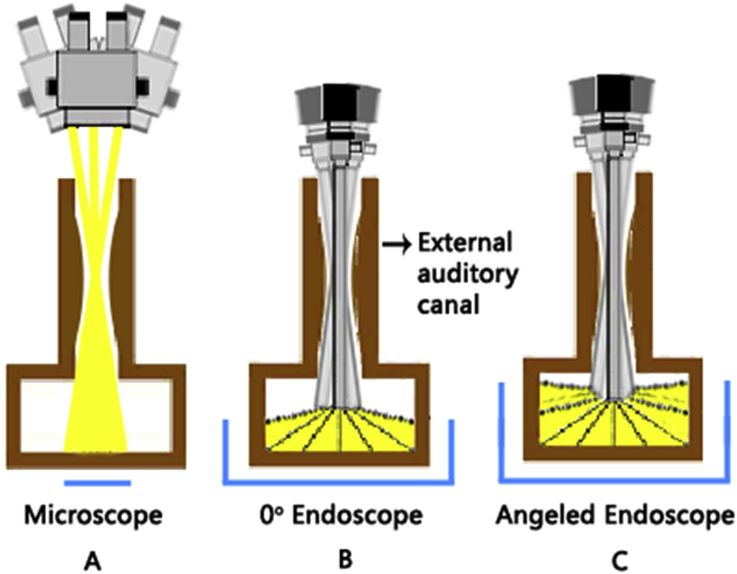
Endoscopes provide a wider and angled view of the fine structures in the middle ear (Kojima et al., 2014) (Fig. 2).
-
2.
Do not require large incisions (postauricular, endaural incisions).
-
3.
Do not require curettage, range or canalplasty of the external ear canal.
-
4.
Operation time is shorter.
-
5.
Provide less postoperative pain and sooner recovery.
-
6.
Provide better cosmetic outcomes (Badr-El-Dine et al., 2013, Pothier, 2013).
-
7.
Monitor used during endoscopic surgery provides visual content for training purposes (Kojima et al., 2014).
-
8.
Hidden deep regions, such as the anterior tympanic perforation, facial recess and hypotympanum can be directly visualized.
-
9.
Contrary to microscopy, views can be obtained from more than one angle.
-
10.
High-resolution and relatively clear images can be obtained.
Disadvantages
-
1.
Surgical manipulations must be performed using a single hand (Kojima et al., 2014).
-
2.
Since the monitor provides two-dimensional views, depth perception can be difficult.
-
3.
Mist may frequently accumulate over the endoscope.
-
4.
Requires good hemostasis of the external ear canal.
-
5.
Potential harm to surrounding structures caused by heat produced from the endoscope's light source is also a matter of concern (Badr-El-Dine et al., 2013, Furukawa et al., 2014).
-
6.
The field of magnification is limited.
-
7.
Requires training.
Fig. 2.
Microscopic (A) and endoscopic (B, C) images of the middle ear.
1.3. Indications for endoscopic ear surgery
Tympanic membrane perforation repair (myringoplasty and tympanoplasty), limited cholesteatoma, otosclerosis, round window fistula repair, ventilation tube insertion, Eustachian tube dilation (Tarabichi, 2000, el-Guindy, 1992, Karhuketo and Puhakka, 2001).
1.4. Contraindications for endoscopic ear surgery
Extensive middle ear cholesteatoma involving the mastoid, presence of obstruction and exostosis in the external ear canal preventing endoscopic access, insufficient equipment availability (Nogueira).
1.5. Endoscopic ear surgery techniques
Endoscopic ear surgery should preferably be performed under hypotensive anesthesia, and the patient should be placed in an appropriate position following the administration of local anesthetics to the field of surgery and adequate local hemostasis must be obtained. The following factors should be considered during endoscopic exploration of the middle ear: status of the ossicles, incudostapedial joint, Eustachian tube, oval and round windows.
1.5.1. Endoscopic type 1 tympanoplasty
The entire procedure can be performed using the transcanal approach. Each step of the surgical techniques is the same as the conventional transcanal microscopic myringoplasty.
1.5.1.1. Surgical techniques
Rigid endoscopes of 2.7 mm and 4 mm in diameter, 0° and 16–18 cm in length are used. The ear canal is cleaned and inspected. First, the perforation and status of middle ear mucosa are examined. Local anesthetic, including epinephrine at a concentration of 1/100,000, is injected into the four quadrants of the outer ear canal. Perforation edges are de-epithelized, as appropriate. Calcified plaque in the tympanic membrane, if any, is removed. Tragal perichondrium, temporalis muscle fascia, conchal, or tragal cartilage graft is harvested. In the external ear canal, any one of the swing door, lateral circumferential or endaural incisions or other types of incisions can be used. Elevating the tympanomeatal flap and the annulus provides access to the middle ear. Continuity and movements of the ossicles and integrity of the middle ear are checked. The malleus is separated from the tympanic membrane using a pick. Ossicular chain repair can be performed if required. The prepared graft is placed lateral to the malleus and medial (over-underlay) to the membrane remnant. To complete the operation, sponges are placed in both the middle ear and the outer ear canal (Sheehy and Anderson, 1980, Halim and Borgstein, 2009, Sakagami et al., 2000, Awad and Hamid, 2015) (Fig. 3).
Fig. 3.
Endoscopic views of a perforation (A), denuded edge of the perforation (B), elevated tympanomeatal flap and middle ear cavity (C), graft placed lateral to the malleus and medial (over-underlay) to the membrane remnant (D) (M: Malleus, I: Incus, S: Stapes).
1.5.2. Endoscopic butterfly myringoplasty
First defined by Eavey (1998), butterfly myringoplasty is an inlay technique using a cartilage graft. It is performed for non-marginal perforations. The ossicular chain should be intact. It can even be performed in the presence of near total perforation (Eavey, 1998, Hod et al., 2013).
1.5.2.1. Surgical techniques
The procedure is carried out under general anesthesia. Perforation in the tympanic membrane is first evaluated by a 0° rigid endoscope of 2.7 mm or 4 mm in diameter. Perforation edges are de-epithelized. The status of the middle ear and ossicles is checked through the perforation. The size of the perforation is measured by an angled pick. From the tragal cartilage graft is prepared, with perichondrium on both sides. A 0.5–1 mm groove is opened all around the cartilage. This graft should be 0.5 mm wider than the perforation. The graft is placed medial to the membrane transcanally under the endoscope and its position is carefully checked using an aspirator and pick. Before terminating the operation, gel-foam is placed at the borders of the graft and the membrane. The endoscopic inlay cartilage butterfly myringoplasty technique does not require tympanomeatal flap or a postauricular incision. Tympanosclerotic plaque in the tympanic membrane may not be removed (Akyigit et al., 2016) (Fig. 4).
Fig. 4.
Perforation (A), graft preparation (B) and graft placed underneath the perforation (C).
2. Discussion
Conventionally, middle ear microsurgery is performed under the guidance of a microscope. However, since microscopy provides a linear view, visualization of deep recesses of the middle ear is not always possible. If the external ear canal is narrow or blocked by protruding bone, a middle ear operation can be performed only after surgical enlargement of the canal. The main advantage of the microscopic approach is that it provides a stereo-view and allows bimanual operation. Endoscopes can provide magnified views of the surgical field. Microscopes require image adjustment during operation, whereas back-and-forth movements of the endoscope can easily produce close-up and angled images when needed. Moreover, rotational movement of angled endoscopes can provide panoramic images of the deep and hidden regions of the middle ear. An endoscopic approach to the middle ear can improve visualization of structures, such as the tuba orifice, incudostapedial joint and oval/round window niches. Advantages of the endoscopic approach include shorter operation time, reduced exposure to anesthetic agents and associated side effects, and improved surgeon concentration (Huang et al., 2016). The endoscopic approach is less invasive, as it does not require incision or canaloplasty, and hair transplantation to the ear region no longer is a necessity. Compared with the microscopic approach, an endoscopic approach is associated with less postoperative bleeding and pain, and it provides improved cosmetic outcomes (Plinkert and Löwenheim, 1997).
Awad and Hamid (2015) reported that operation time is shorter in patients undergoing endoscopic surgeries, with no of incision or prophylactic antibiotics. In the study of Ghaffar et al. (2006), mean operation time was found to be 62.85 min in patients undergoing endoscopic tympanoplasty. Huang et al. (2016) reported that the mean operation times were 75.5 min and 50.4 min in patients undergoing microscopic and endoscopic tympanoplasty, respectively. In the study of Patel et al. (2015), mean time of endoscopic and microscopic tympanoplasty operations was found to be 75 min and 90 min, respectively.
Huang et al. (2016) performed type 1 tympanoplasty in 50 patients by microscopic approach and in another 50 patients by endoscopic approach. Similar hearing recovery and rate of perforation closure were found between the two patient groups. Moreover, shorter operation times, better views of surgical field, improved outcomes, reduced tissue injury and particularly lower rate of postoperative nausea were noted in patients undergoing endoscopic surgeries.
Karhuketo et al. (2001) stated that canaloplasty and outer ear curettage became necessary in some of their patients undergoing microscopic tympanoplasty. Conversely, none of their patients who underwent endoscopic tympanoplasty required interventions such as canaloplasty or curettage. Mokbel et al. (2015) performed cartilage myringoplasty by microscopic approach in half and by endoscopic approach in the remaining half of 80 patients with subtotal perforation. They reported improved hearing outcomes in patients undergoing endoscopic myringoplasty, as compared with those undergoing the microscopic approach.
In the study of Raj and Meher (2001), the rate of graft survival was 90% in patients undergoing endoscopic myringoplasty, and 85% in those undergoing microscopic myringoplasty. el-Guindy (1992) reported that graft success rate was 91.7% among their patients undergoing endoscopic myringoplasty. Patel et al. (2015) reported very similar graft success rates in patients undergoing endoscopic and microscopic tympanoplasty. Patel et al. (2015) also reported that the major disadvantage of endoscopic approach was the necessity to operate with a single hand. They also stated that any bleeding in the external ear canal made manipulations very difficult and underlined the necessity to achieve total hemostasis in the external ear canal.
Eavey (1998) was the first to report successful use of cartilage butterfly myringoplasty technique for small tympanic membrane perforations. In the techniques described, an inlay cartilage graft was placed by transcanal approach without elevating the tympanomeatal flap. Later on, reports were published indicating that this technique can also be applied to larger perforations (Ghanem et al., 2006, Yu and Yoon, 2010). Graft success rate was higher than 90% (Haksever et al., 2015, Akyigit et al., 2016). Couloigner et al. (2005) reported that the microscopic inlay butterfly cartilage tympanoplasty was a safe, short and easy-to-implement procedure in pediatric patients. Akyigit et al. (2016), on the other hand, performed endoscopic butterfly myringoplasty in 32 pediatric patients and reported a graft success rate of 93.7%.
Nonetheless, there are still some limitations on the implementation of endoscopy in middle ear surgeries. There is a long learning curve, and there are also some challenges and inconveniences associated with instrumentation and endoscopic techniques. Use of small-diameter endoscopes within the ear can be challenging for inexperienced surgeons and this hinders the opportunity to obtain large-angled views, which is the main advantage of endoscopy over microscopy (Rosenberg et al., 1994, Yung, 2001). There are two major drawbacks with endoscopic ear surgery. The first is heat generated by the light source, particularly, the heat released by xenon light sources. As a solution to this problem, the routinely used light source can be adjusted to operate at a lower power level. The second drawback is the trauma, which may result from unintentional head movements by the patient (Raj and Meher, 2001).
In the presence of anterior tympanic membrane perforations, the anterior part of the residual membrane may not be appropriately viewed by microscopic approach in some patients, while endoscopy allows adequate visualization of this region (Migirov and Wolf). Furukawa et al. (2014) reported that the perforation edges could not be completely visualized by microscopic approach in 12% of the cases before denudation. Moreover, they maintained that the perforation edges could not be completely visualized in 20% of the cases following membrane denudation. Endoscopic myringoplasty technique can be beneficial in patients with narrow ear canals, in the presence of anterior tympanic membrane perforations, in patients with bone protrusions in the ear canal, and in cases where the perforation edges cannot be easily visualized (Poe and Bottrill, 1994).
3. Conclusion
In conclusion, otologists have spent years endeavoring to obtain improved surgical outcomes. Although several technical improvements have been made to surgical microscopes, there remain a number of limitations. As in multiple surgical fields, there is also a trend towards minimally invasive interventions in the field of otorhinolaryngology. The endoscopic approach has introduced a new perspective to ear surgery. When compared with microscopes, endoscopes can provide larger and better images of the middle ear. Smaller incisions performed under the guidance of endoscopes are preferred over conventional large incisions. Using this method, both improved cosmetic outcomes and reduced postoperative morbidity can be achieved and consequently endoscopic ear surgery implementations have been increasingly adopted.
Footnotes
Peer review under responsibility of PLA General Hospital Department of Otolaryngology Head and Neck Surgery.
References
- Akyigit A., Karlidag T., Keles E., Kaygusuz I., Yalcın S., Polat C., Eroglu O. Endoscopic cartilage butterfly myringoplasty in children. Auris Nasus Larynx. 2016 Jun 1 doi: 10.1016/j.anl.2016.05.005. (S0385-8146(16)30154-7; Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- Awad O.G., Hamid K.A. Endoscopic type 1 tympanoplasty in pediatric patients using tragal cartilage. JAMA Otolaryngol. Head Neck Surg. 2015 Jun;141(6):532–538. doi: 10.1001/jamaoto.2015.0601. [DOI] [PubMed] [Google Scholar]
- Ayache S., Tramier B., Strunski V. Otoendoscopy in cholesteatoma surgery of the middle ear: what benefits can be expected? Otol. Neurotol. 2008 Dec;29(8):1085–1090. doi: 10.1097/MAO.0b013e318188e8d7. [DOI] [PubMed] [Google Scholar]
- Badr-El-Dine M., James A.L., Panetti G., Marchioni D., Presutti L., Nogueira J.F. Instrumentation and technologies in endoscopic ear surgery. Otolaryngol. Clin. North Am. 2013 Apr;46(2):211–225. doi: 10.1016/j.otc.2012.10.005. [DOI] [PubMed] [Google Scholar]
- Coskun B.U., Cinar U., Seven H., Ugur S., Dadas B. The effects of the incision types in myringoplasty operations on cosmesis. Eur. Arch. Otorhinolaryngol. 2006 Sep;263(9):820–822. doi: 10.1007/s00405-006-0069-z. [DOI] [PubMed] [Google Scholar]
- Couloigner V., Baculard F., El Bakkouri W., Viala P., François M., Narcy P., Van Den Abbeele T. Inlay butterfly cartilage tympanoplasty in children. Otol. Neurotol. 2005 Mar;26(2):247–251. doi: 10.1097/00129492-200503000-00020. [DOI] [PubMed] [Google Scholar]
- Eavey R.D. Inlay tympanoplasty: cartilage butterfly technique. Laryngoscope. 1998 May;108(5):657–661. doi: 10.1097/00005537-199805000-00006. [DOI] [PubMed] [Google Scholar]
- el-Guindy A. Endoscopic transcanal myringoplasty. J. Laryngol. Otol. 1992 Jun;106(6):493–495. doi: 10.1017/s0022215100119966. [DOI] [PubMed] [Google Scholar]
- Furukawa T., Watanabe T., Ito T., Kubota T., Kakehata S. Feasibility and advantages of transcanal endoscopic myringoplasty. Otol. Neurotol. 2014 Apr;35(4):e140–e145. doi: 10.1097/MAO.0000000000000298. [DOI] [PubMed] [Google Scholar]
- Ghaffar S., Ikram M., Zia S., Raza A. Incorporating the endoscope into middle ear surgery. Ear Nose Throat J. 2006;85:593–596. [PubMed] [Google Scholar]
- Ghanem M.A., Monroy A., Alizade F.S., Nicolau Y., Eavey R.D. Butterfly cartilage graft inlay tympanoplasty for large perforations. Laryngoscope. 2006 Oct;116(10):1813–1816. doi: 10.1097/01.mlg.0000231742.11048.ed. [DOI] [PubMed] [Google Scholar]
- Haksever M., Akduman D., Solmaz F., Gündoğdu E. Inlay butterfly cartilage tympanoplasty in the treatment of dry central perforated chronic otitis media as an effective and time-saving procedure. Eur. Arch. Otorhinolaryngol. 2015;272(4):867–872. doi: 10.1007/s00405-014-2889-6. [DOI] [PubMed] [Google Scholar]
- Halim A., Borgstein J. Pediatric myringoplasty: postaural versus transmeatal approach. Int. J. Pediatr. Otorhinolaryngol. 2009 Nov;73(11):1580–1583. doi: 10.1016/j.ijporl.2009.08.010. (Epub 2009 Sep. 6) [DOI] [PubMed] [Google Scholar]
- Hod R., Buda I., Hazan A., Nageris B.I. Inlay “butterfly” cartilage tympanoplasty. Am. J. Otolaryngol. 2013 Jan-Feb;34(1):41–43. doi: 10.1016/j.amjoto.2012.08.004. (Epub 2012 Sep. 10) [DOI] [PubMed] [Google Scholar]
- Huang T.Y., Ho K.Y., Wang L.F., Chien C.Y., Wang M. A comparative study of endoscopic and microscopic approach type 1 tympanoplasty for simple chronic otitis media. J. Int. Adv. Otol. 2016 Apr;12(1):28–31. doi: 10.5152/iao.2015.1011. [DOI] [PubMed] [Google Scholar]
- Jako G.J. Postaural versus endaural exposure in tympanoplasty. Laryngoscope. 1967 Nov;77(11):2022–2031. doi: 10.1288/00005537-196711000-00007. [DOI] [PubMed] [Google Scholar]
- Kakehata S., Futai K., Sasaki A., Shinkawa H. Endoscopic transtympanic tympanoplasty in the treatment of conductive hearing loss: early results. Otol. Neurotol. 2006 Jan;27(1):14–19. doi: 10.1097/01.mao.0000181181.47495.a0. [DOI] [PubMed] [Google Scholar]
- Karhuketo T.S., Puhakka H.J. Endoscope-guided round window fistula repair. Otol. Neurotol. 2001 Nov;22(6):869–873. doi: 10.1097/00129492-200111000-00027. [DOI] [PubMed] [Google Scholar]
- Karhuketo T.S., Ilomaki J.H., Puhakka H.J. Tympanoscope-assisted myringoplasty. ORL: J. Otorhinolaryngol. Relat. Spec. 2001;63:353–357. doi: 10.1159/000055773. [DOI] [PubMed] [Google Scholar]
- Kessler A., Potsic W.P., Marsh R.R. Type 1 tympanoplasty in children. Arch. Otolaryngol. Head Neck Surg. 1994 May;120(5):487–490. doi: 10.1001/archotol.1994.01880290005001. [DOI] [PubMed] [Google Scholar]
- Kojima H., Komori M., Chikazawa S., Yaguchi Y., Yamamoto K., Chujo K., Moriyama H. Comparison between endoscopic and microscopic stapes surgery. Laryngoscope. 2014 Jan;124(1):266–271. doi: 10.1002/lary.24144. [DOI] [PubMed] [Google Scholar]
- McKennan K.X. Endoscopic ‘second look’ mastoidoscopy to rule out residual epitympanic/mastoid cholesteatoma. Laryngoscope. 1993 Jul;103(7):810–814. doi: 10.1288/00005537-199307000-00016. [DOI] [PubMed] [Google Scholar]
- Migirov L., Shapira Y., Horowitz Z., Wolf M. Exclusive endoscopic ear surgery for acquired cholesteatoma: preliminary results. Otol. Neurotol. 2011 Apr;32(3):433–436. doi: 10.1097/MAO.0b013e3182096b39. [DOI] [PubMed] [Google Scholar]
- Migirov L, Wolf M. Minimally invasive transcanal endoscopic ear surgery. http://dx.doi.org/10.5772/60551.
- Mokbel K.M., Moneir W., Elsisi H., Albosky A. Endoscopic transcanal cartilage myringoplasty for repair of subtotal tympanic membrane perforation: a method to avoid postauricular incision. J. Otolaryngol. Rhinol. 2015;1:2. [Google Scholar]
- Nogueira JF. Endoscopic ear surgery. Dissection manual. www.sinuscenter.com.br.
- Patel J., Aiyer R.G., Gajjar Y., Gupta R., Raval J., Suthar P.P. Endoscopic tympanoplasty vs microscopic tympanoplasty in tubotympanic CSOM: a comparative study of 44 cases. Int. J. Res. Med. Sci. 2015;3(8):1953–1957. [Google Scholar]
- Plinkert P., Löwenheim H. Trends and perspectives in minimally invasive surgery in otorhinolaryngology-head and neck surgery. Laryngoscope. 1997 Nov;107(11 Pt 1):1483–1489. doi: 10.1097/00005537-199711000-00011. [DOI] [PubMed] [Google Scholar]
- Poe D.S., Bottrill I.D. Comparison of endoscopic and surgical explorations for perilymphatic fistulas. Am. J. Otol. 1994 Nov;15(6):735–738. [PubMed] [Google Scholar]
- Pothier D.D. Introducing endoscopic ear surgery into practice. Otolaryngol. Clin. North Am. 2013 Apr;46(2):245–255. doi: 10.1016/j.otc.2012.10.009. [DOI] [PubMed] [Google Scholar]
- Raj A., Meher R. Endoscopic transcanal myringoplasty – a study. Indian J. Otolaryngol. Head Neck Surg. 2001 Jan;53(1):47–49. doi: 10.1007/BF02910979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg S.I., Silverstein H., Willcox T.O., Gordon M.A. Endoscopy in otology and neurotology. Am. J. Otol. 1994 Mar;15(2):168–172. [PubMed] [Google Scholar]
- Sakagami M., Mishiro Y., Tsuzuki K., Seo T., Sone M. Bilateral same day surgery for bilateral perforated chronic otitis media. Auris Nasus Larynx. 2000 Jan;27(1):35–38. doi: 10.1016/s0385-8146(99)00043-7. [DOI] [PubMed] [Google Scholar]
- Sarkar S. A review on the history of tympanoplasty. Indian J. Otolaryngol. Head Neck Surg. 2013 Dec;65(Suppl. 3):455–460. doi: 10.1007/s12070-012-0534-5. (Epub 2012 Mar 22) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheehy J.L., Anderson R.G. Myringoplasty. A review of 472 cases. Ann. Otol. Rhinol. Laryngol. 1980 Jul–Aug;89(4 Pt 1):331–334. doi: 10.1177/000348948008900407. [DOI] [PubMed] [Google Scholar]
- Tarabichi M. Endoscopic management of acquired cholesteatoma. Am. J. Otol. 1997 Sep;18(5):544–549. [PubMed] [Google Scholar]
- Tarabichi M. Endoscopic management of cholesteatoma: long-term results. Otolaryngol. Head Neck Surg. 2000 Jun;122(6):874–881. doi: 10.1016/S0194-59980070017-9. [DOI] [PubMed] [Google Scholar]
- Tarabichi M. Endoscopic transcanal middle ear surgery. Indian J. Otolaryngol. Head Neck Surg. 2010 Jan;62(1):6–24. doi: 10.1007/s12070-010-0007-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomassin J.M., Duchon-Doris J.M., Emram B., Rud C., Conciatori J., Vilcoq P. Endoscopic ear surgery. Initial evaluation. Ann. Otolaryngol. Chir. Cervicofac. 1990;107(8):564–570. [PubMed] [Google Scholar]
- Thomassin J.M., Korchia D., Doris J.M. Endoscopic-guided otosurgery in the prevention of residual cholesteatomas. Laryngoscope. 1993 Aug;103(8):939–943. doi: 10.1288/00005537-199308000-00021. [DOI] [PubMed] [Google Scholar]
- Tuncer U. History of the endoscopic ear surgery. Turkiye Klinikleri J E.N.T.-Special Topics. 2016;9(1):1–3. [Google Scholar]
- Yu M.S., Yoon T.H. Bilateral same-day surgery for bilateral perforated chronic otitis media: inlay butterfly cartilage myringoplasty. Otolaryngol. Head Neck Surg. 2010 Nov;143(5):669–672. doi: 10.1016/j.otohns.2010.07.013. [DOI] [PubMed] [Google Scholar]
- Yung M.W. The use of middle ear endoscopy: has residual cholesteatoma been eliminated? J. Laryngol. Otol. 2001 Dec;115(12):958–961. doi: 10.1258/0022215011909765. [DOI] [PubMed] [Google Scholar]