Abstract
Objective
A common cavity deformity (CCD) is a deformed inner ear in which the cochlea and vestibule are confluent forming a common rudimentary cystic cavity that results in profound hearing loss. There are few studies paying attention to common cavity. Our group is engrossed in observing the improvement of auditory and verbal abilities in children who have received cochlear implantation (CI), and comparing these targets between children with common cavity and normal inner ear structure.
Material and methods
A retrospective study was conducted in 12 patients with profound hearing loss that were divided into a common cavity group and a control group, six in each group matched in sex, age and time of implantation, based on inner ear structure. Categories of Auditory Performance (CAP) and speech intelligibility rating (SIR) scores and aided hearing thresholds were collected and compared between the two groups. All patients wore CI for more than 1 year at the Cochlear Center of Anhui Medical University from 2011 to 2015.
Results
Postoperative CAP and SIR scores were higher than before operation in both groups (p < 0.05), although the scores were lower in the CCD group than in the control group (p < 0.05). The aided threshold was also lower in the control group than in the CCD group (p < 0.05).
Conclusion
Even though audiological improvement in children with CCD was not as good as in those without CCD, CI provides benefits in auditory perception and communication skills in these children.
Keywords: Cochlear implant, Common cavity, Outcome, Inner ear deformity, Hearing threshold
Abbreviations: CCD, common cavity deformity; CAP, categories of Auditory Performance; SIR, speech intelligibility rating; CI, cochlear implantation; IAC, Internal auditory canal
1. Introduction
Hearing loss is a common human inborn defect. The prevalence of neonatal hearing impairment is 1.4%, and 20% of these infants are diagnosed as profound hearing loss (Caluraud et al., 2015). But congenital ear malformation is not a common clinical condition in children. The incidence rate of congenital ear malformation is 20%–30% (Sennaroglu, 2010). In 1987, Jackler et al. (1987) firstly proposed a classification system for inner ear malformations based on inner ear development during embryo growth. It is known that common cavity deformity (CCD) will appear if any interruption occurs during the 4th week before the otocyst differentiates into the primordial cochlea, vestibule and semicircular canals. A common rudimentary cystic cavity is formed by the fusion of cochlea and vestibule that results in severe or profound hearing loss. These abnormalities may affect not only the patient's prognosis regarding auditory improvement, but also the risk of complications such as cerebrospinal fluid rhinorrhea and meningitis (Young et al., 2014). With the development of medical imaging technologies and cochlear implants, CCD is no longer a contraindication for surgery, but there are few reports of such cases. The objective of this study was evaluating outcomes (CAP and SIR scores, hearing thresholds) and feasibility of cochlear implantation in children with CCD in comparison to those without CCD.
2. Material and methods
Subjects were identified from patients with profound sensorineural deafness who had undergone cochlear implantation at the Cochlear Implant Centre of First Affiliated Hospital of Anhui Medical University from August 2011 to August 2015. Data from chart review in 12 children were included in a case-control, retrospective study.
2.1. Cases, criteria and methods
Six cases with CCD diagnosed by temporal bone CT scan were set as the test group (CCD group) and six cases with normal CT inner ear findings as the control group. Subjects in the two groups were matched in sex, age and time of implantation. All the patients had pre-lingual deafness and used cochlear implants for more than one year. The details are demonstrated as follows:
-
(a)
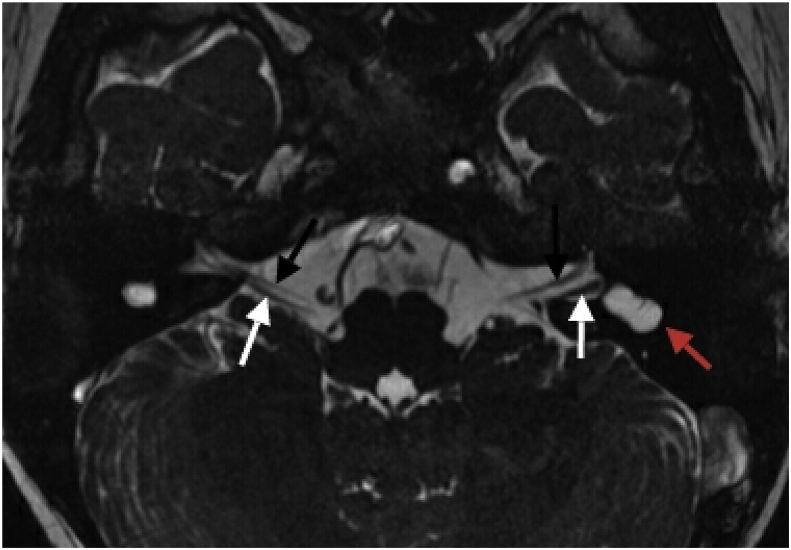
CCD group: The mean age at the time of implantation was 6.36 years in the 6 children (5 boys, 1 girl). All the subjects were diagnosed with bilateral CCD with normal development of the internal auditory canal (IAC) and cochlear nerve (Fig. 1). Only 1 child had residual hearing whereas the rest had complete hearing loss as revealed by auditory brainstem responses (ABR), auditory steady state response (ASSR) and otoacoustic emissions (TEOAE, DPOAE). Two children wore hearing aids and received rehabilitation training before CI operation and another 2 children wore hearing aids but did not receive rehabilitation training, whereas the rest 2 children had neither hearing aids nor rehabilitation training.
-
(b)
Control group: The 5 boys and 1 girl in the control group all had profound sensorineural hearing loss with normal cochlea structure on CT scan, and their mean age at the time of implantation was 6.07 years. None of these prelingually deafened children had residual hearing and they all could communicate with sign language before CI.
Fig. 1.
Magnetic resonance imaging (MRI) of inner ear demonstrates the deformity of common cavity (red arrowhead), normal developed facial nerve (black arrowheads) and cochlear nerve (white arrowheads).
2.2. Surgical techniques
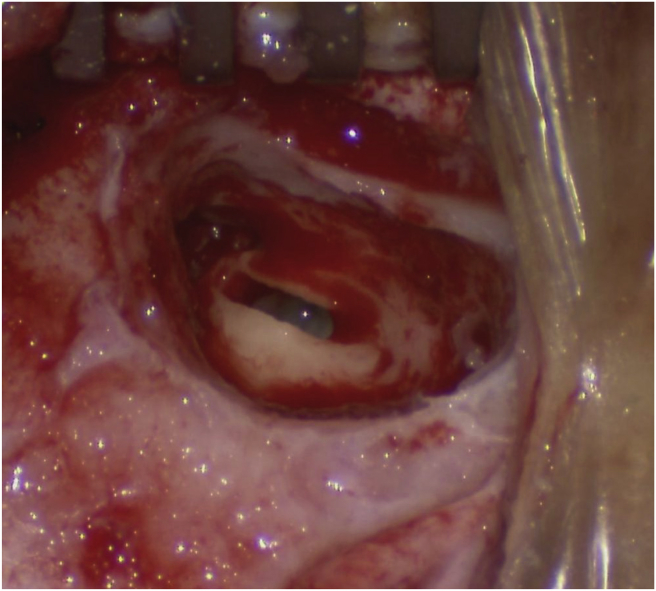
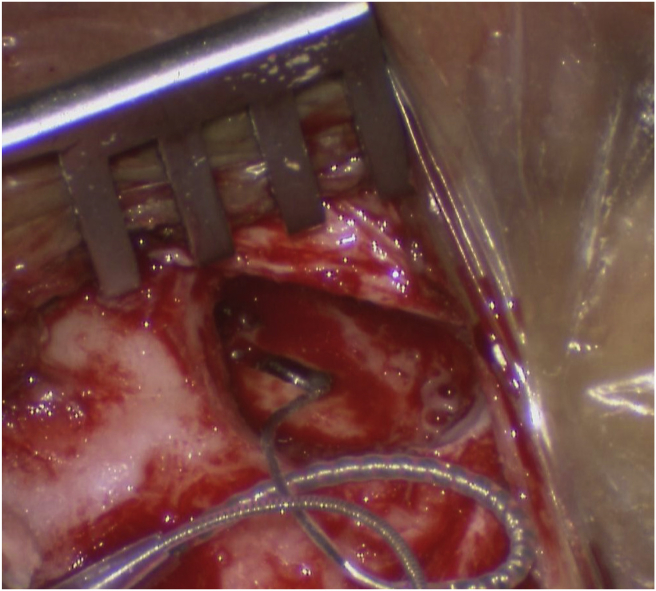
The standard transmastoid facial recess approach was used in cases in the control group, while a modified transmastoid labyrinthotomy approach was used in patients with CCD. The epitympanum was opened and the lateral semicircular canal was identified, followed by removal of the outer wall along the long axis of lateral semicircular canal (posterosuperior wall of CCD). A 1 × 3 mm rectangular hole was created for electrode insertion (Fig. 2). The electrode array was bent into a “C” shape and inserted into the anteroinferior part of the cavity beyond the fundus of IAC with the curved end of the electrode array preventing intrameatal placement or undesirable folding of the tip (Fig. 3). A small temporalis muscle fascia or the periosteum graft was placed over the electrode to seal the common cavity and to secure the attachment of the electrodes to the anteroinferior wall of the cavity. In case of cerebrospinal fluid (CSF) gusher, the hole was packed with temporalis muscle or fascia grafts and sealed with medical aural and encephalic glue (EC glue).
Fig. 2.
The position and shape of labyrinthotomy.
Fig. 3.
“C” shaped electrode and insertion into the common cavity.
2.3. Rehabilitation assessment
Categories of Auditory Performance (CAP) describe a scale used to rate outcomes from pediatric cochlear implantation in everyday life. It can be easily understood by non-specialist professionals and by parents and is reliable for users of cochlear implant to measure postoperative outcomes (Archbold et al., 1998). In our study CAP and SIR scores were collected through questionnaire follow-up with parents or other guardians who lived with the patient and participated in family rehabilitation. Telephone calls were made by professional staff to ask parents about the patient's performance in daily life. Then the CAP and SIR scores were assigned based on their performance by the investigator. The specific scoring criteria are shown in Table 1, Table 2.
Table 1.
Criteria for CAP score.
| CAP score | |
|---|---|
| 0 | No awareness of environmental sounds |
| 1 | Awareness of environmental sounds |
| 2 | Responses to speech sounds (e.g. ‘go’) |
| 3 | Identification of environmental sounds |
| 4 | Discrimination of some speech sounds without lip reading |
| 5 | Understanding of common phrases without lip reading |
| 6 | Understanding of conversation without lip reading |
| 7 | Use of telephone with a known listener |
Table 2.
Criteria for SIR score.
| SIR score | |
|---|---|
| 1 | Unintelligible |
| 2 | Intelligible speech is developing in single words |
| 3 | Intelligible to a listener who concentrates & lip-reads |
| 4 | Intelligible to a listener who has little experience of a deaf person's speech |
| 5 | Intelligible to all listeners |
Postoperative cochlear implant aided thresholds at 0.25, 0.5, 1.0, 2.0 and 4.0 kHz were measured through sound field speakers using a modified Hughson–Westlake procedure with a 5 dB step size (Beahan et al., 2012). The subjects sat at the reference point in the soundproof booth, with the background noise at lower than 30 dB SPL, facing the speaker and tests were completed by the same audiologist. Visual reinforcement audiometry (Norrix, 2015) was used in very young aged children and patients with poor reactions.
2.4. Statistical analysis
All clinical variables were subjected to statistical analysis using the SPSS16.0 software. Independent-Sample t Test was used in comparing hearing thresholds, while Wilcoxon rank sum test was used in comparing CAP and SIR scores between the two groups. Wilcoxon signed rank test was used to compare the difference between preoperative and postoperative CAP and SIR scores. p < 0.05 was considered statistically significant.
3. Results
Patients were followed up for 18–64 months. Auditory perception and speech abilities manifested obvious improvements in all 12 patients, based on post-operative CAP, SIR scores and aided thresholds (Table 3, Table 4, Table 5). CAP and SIR scores showed significant improvement in both the control and CCD groups after surgery compared with preoperative scores (p < 0.05), although significant differences in the two scores were also found between patients with CCD and the control group (p < 0.05). Table 5 also demonstrates a significant hearing threshold difference as observed after surgery between patients with CCD and those with normal inner ear structure on CT scan (p = 0.006).
Table 3.
Characteristics of outcomes of 8 patients with CC deformity.
| Case | Age at CI(mo) | Side of CI | Device | Follow-up Duration (mo) | Preoperative CAP score | Postoperative CAP score | Preoperative SIR score | Postoperative SIR score | Preoperative HA and RT |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 8 | L | Sonata | 21 | 0 | 2 | 1 | 1 | None |
| 2 | 20 | L | Sonata | 34 | 0 | 3 | 1 | 1 | None |
| 3 | 44 | R | Sonata | 31 | 0 | 3 | 1 | 2 | HA: 3 months RT: none |
| 4 | 106 | R | Sonata | 27 | 3 | 4 | 1 | 2 | HA: 3 year, RT: 3 year |
| 5 | 137 | R | Sonata | 50 | 0 | 4 | 1 | 2 | HA: 1 year, RT: none |
| 6 | 144 | R | CI24R | 43 | 2 | 4 | 1 | 2 | HA: 8 year, RT: 2 year |
HA: hearing aids; RT: rehabilitation training.
Table 4.
Analysis of CAP and SIR scores.
| Comparison between preoperative and postoperative scores of CCD group |
Comparison between CCD group and normal group |
|||||||
|---|---|---|---|---|---|---|---|---|
| Positive ranks | Negative ranks | Z | p | Mean Rank |
Mean Rank |
Z | p | |
| (CCD group) | (Control group) | |||||||
| CAP | 78 | 0 | −3.089 | 0.002 | 3.50 | 9.50 | −2.934 | 0.003 |
| SIR | 45 | 0 | −2.724 | 0.006 | 3.75 | 9.25 | −2.735 | 0.006 |
Table 5.
Hearing threshold of two groups at different frequencies (dB HL, ).
| Group | Frequency |
Mean threshold | ||||
|---|---|---|---|---|---|---|
| 0.25 kHz | 0.5 kHz | 1 kHz | 2 kHz | 4 kHz | ||
| CCD group | 44.17 ± 8.61 | 49.17 ± 8.61 | 48.33 ± 7.53 | 48.33 ± 8.16 | 51.67 ± 4.08 | 48.33 ± 7.06 |
| Control group | 33.33 ± 6.06 | 35.83 ± 6.65 | 35.83 ± 5.85 | 35.00 ± 4.47 | 38.33 ± 6.06 | 35.67 ± 5.39 |
p = 0.006 (comparison between two groups of mean threshold).
4. Discussion
As mentioned above, the incidence of congenital ear malformation is found to be from 20% to 30% with CCD being the second most common malformation after Mondini deformity (Sennaroglu, 2010). We have encountered 92 cases of inner ear malformation among 498 congenitally deaf children, and seen 9 children with CCD among the 92 cases. Parents of one of these children refused surgery treatment, and two other children have just finished the operation within one year, and therefore not included in this study. The incidence of our observation is similar to previous studies. It is acknowledged that CCD can be adequately diagnosed by temporal bone CT scan and cochlear magnetic resonance imaging (DeMarcantonio and Choo, 2015). It is crucial for otologists to deliberate the indication of cochlear implantation. Some scholars believe that residual hearing is an essential condition for cochlear implantation (Zhang et al., 2007). However, most of CCD patients have no residual hearing that can be demonstrated by hearing tests. We have performed ABRs in all our cases before implantation but had positive responses in only one case. Some scholars suggest that intra-operative electrically evoked ABR (EABR) can be used to detect evoked waves stimulated by biphasic electrical stimuli with various stimulus pulse intensities (Yamazaki et al., 2014, Minami et al., 2015). Only one patient with CCD had residual hearing by ABR in our study, although meaningful evoked waves could be detected in all patients by intra-operative telemetry.
In the standard facial recess approach, a simple mastoidectomy is performed to allow access to the facial recess and then the round widow to expose the scala tympani. Unfortunately, the surgery cannot be done by the conventional approach for patients with CCD due to structural changes of the cochlea and vestibule. In previous studies on CCD, the modified transmastoid labyrinthotomy (lateral semicircular canal approach) was used (Beltrame et al., 2005, Zarandy, 2008). Some scholars hold the opinion that conventional facial recess approach can be used when there is a residual structure of cochlea in the area of promontory, while the modified transmastoid labyrinthotomy can be selected when the cochlea cannot be distinguished from the common cavity structure (Xia et al., 2015). The electrode array was inserted successfully by the modified transmastoid labyrinthotomy approach in all CCD cases in our study. Removing the bone of mastoid recess should be the focus, as the facial nerve injury can happen if the level of manipulation is inferior to the level of lateral semicircular canal. Preoperative temporal bone CT scan showed that the cochlea and vestibule was connected with the fundus of internal auditory canal in one case, but CSF leakage did not occur in any cases. We suppose that there may be a membranous structure between the common cavity and IAC.
Fayad and Linthicum, 2006 reported that the degree of hearing improvement after CI was closely related to the number and function of residual spiral ganglion cells. Khan et al. (2006) found that partial or complete lack of modiolus in CCD patients led to abnormal distribution of spiral ganglion cells, and the electrode array implanted into the common cavity could not produce sufficient stimulation because of its location away from the midiolus as compared to in a normal cochlea. Some scholars (Ahn et al., 2011) reported that the hearing and speech abilities failed to reach normal levels in communication in CCD patients after CI. In our study, postoperative CAP and SIR scores were significantly better than preoperative scores, although there were significant differences between CCD and control groups in CAP, SIR scores and aided hearing thresholds. It demonstrates that cochlear implantation is an effective treatment for patients with and without CCD, with hearing and speech outcomes in CCD patients being inferior compared to those without CCD, which is consistent with existing reports (Beltrame et al., 2013, Catli et al., 2015, Pradhananga et al., 2015). The follow-up duration in our study ranged from 18 to 64 months, making observing the time course of auditory perception and speech ability along time somewhat difficult. However, all out patients, including those with cochlear malformation, showed obvious improvement in auditory and communication functions after cochlear implantation. In addition, we found that there was a distinguished difference in rehabilitation outcomes within the CCD patients (CAP score 2–5). We suppose that this is related to preoperative rehabilitation, the number of residual spiral ganglions, the service time of cochlear implant, rehabilitation training after CI and the number of working electrodes. During the follow-up, hearing and speech abilities improvement in patients who had hearing and speech training before implantation was better than those who did not both patients with CCD and those without. Case 4 had residual hearing before operation and undertook 3 years of rehabilitation training with hearing aids in both ears. Case 6 wore hearing aids for 8 years with 2 years of rehabilitation training before operation. Teoh et al. (2004) suggested that aurally based educational programs (rehabilitation training) before and after cochlear implantation could potentially improve post-implantation audiological performance by reducing the cortical colonization phenomenon. Some scholars (Gerard et al., 2010, Guerzoni et al., 2016) found that children with better preoperative residual hearing exhibited better communication ability. However, the extent of the influence on postoperative outcomes by residual hearing and rehabilitation before implantation, as well as the mechanisms of the influence, is not clear. All these puzzling points need to be further studied. In addition, parents should have a reasonable expectation about the effect of rehabilitation and the child need to be encouraged to practice and communicate in daily life instead of totally relying on the training center. On the basis of right selection of candidates and reasonable expectation from parents, cochlear implantation can be carried out in children with CCD.
5. Conclusions
Cochlear implantation is an effective treatment in children with CCD, with the majority of subjects showing significant benefits in their audiological development, despite being somewhat worse than those without CCD. Individual prognosis is different in each CCD patient. Children with CCD can benefit from cochlear implantation with reasonable expectations from parents.
Conflict of interests
The authors report no declarations of conflict of interests.
Acknowledgements
Authors are grateful for the untiring support from the hospital medical records section to allow access to the hospital database. Moreover, Dr. Gyanendra Shah deserves our heartfelt appreciation for helping us in improving the grammar and sentences, giving his invaluable suggestions, solving article related problems and helping with final processes of article submissions.
Footnotes
Peer review under responsibility of PLA General Hospital Department of Otolaryngology Head and Neck Surgery.
Contributor Information
Li Zhang, Email: 13965142285@163.com.
Jianxin Qiu, Email: qiujianxin@ahmu.edu.cn.
References
- Ahn J.H., Lim H.W., Lee K.S. Hearing improvement after cochlear implantation in common cavity malformed cochleae: long-term follow-up results. Acta Otolaryngol. 2011;131:908–913. doi: 10.3109/00016489.2011.570786. [DOI] [PubMed] [Google Scholar]
- Archbold S., Lutman M.E., Nikolopoulos T. Categories of auditory performance: inter-user reliability. Br. J. Audiol. 1998;32:7–12. doi: 10.3109/03005364000000045. [DOI] [PubMed] [Google Scholar]
- Beahan N., Kei J., Driscoll C., Charles B., Khan A. High-frequency pure-tone audiometry in children: a test-retest reliability study relative to ototoxic criteria. Ear Hear. 2012;33:104–111. doi: 10.1097/AUD.0b013e318228a77d. [DOI] [PubMed] [Google Scholar]
- Beltrame M.A., Birman C.S., Cervera Escario J., Kassouma J., Manolidis S. Common cavity and custom-made electrodes: speech perception and audiological performance of children with common cavity implanted with a custom-made MED-EL electrode. Int. J. Pediatr. Otorhinolaryngol. 2013;77:1237–1243. doi: 10.1016/j.ijporl.2013.04.008. [DOI] [PubMed] [Google Scholar]
- Beltrame M.A., Frau G.N., Shanks M., Robinson P., Anderson I. Double posterior labyrinthotomy technique: results in three Med-El patients with common cavity. Otol. Neurotol. 2005;26:177–182. doi: 10.1097/00129492-200503000-00008. [DOI] [PubMed] [Google Scholar]
- Caluraud S., Marcolla-Bouchetemble A., de Barros A., Moreau-Lenoir F., de Sevin E. Newborn hearing screening: analysis and outcomes after 100,000 births in Upper-Normandy French region. Int. J. Pediatr. Otorhinolaryngol. 2015;79:829–833. doi: 10.1016/j.ijporl.2015.03.012. [DOI] [PubMed] [Google Scholar]
- Catli T., Uckan B., Olgun L. Speech and language development after cochlear implantation in children with bony labyrinth malformations: long-term results. Eur. Arch. Otorhinolaryngol. 2015;272:3131–3136. doi: 10.1007/s00405-014-3319-5. [DOI] [PubMed] [Google Scholar]
- DeMarcantonio M., Choo D.I. Radiographic evaluation of children with hearing loss. Otolaryngol. Clin. N. Am. 2015;48:913–932. doi: 10.1016/j.otc.2015.07.003. [DOI] [PubMed] [Google Scholar]
- Fayad J.N., Linthicum F.H., Jr. Multichannel cochlear implants: relation of histopathology to performance. Laryngoscope. 2006;116:1310–1320. doi: 10.1097/01.mlg.0000227176.09500.28. [DOI] [PubMed] [Google Scholar]
- Gerard J.M., Deggouj N., Hupin C., Buisson A.L., Monteyne V. Evolution of communication abilities after cochlear implantation in prelingually deaf children. Int. J. Pediatr. Otorhinolaryngol. 2010;74:642–648. doi: 10.1016/j.ijporl.2010.03.010. [DOI] [PubMed] [Google Scholar]
- Guerzoni L., Murri A., Fabrizi E., Nicastri M., Mancini P. Social conversational skills development in early implanted children. Laryngoscope. 2016;126:2098–2105. doi: 10.1002/lary.25809. [DOI] [PubMed] [Google Scholar]
- Jackler R.K., Luxford W.M., House W.F. Congenital malformations of the inner ear: a classification based on embryogenesis. Laryngoscope. 1987;97:2–14. doi: 10.1002/lary.5540971301. [DOI] [PubMed] [Google Scholar]
- Khan A.M., Levine S.R., Nadol J.B., Jr. The widely patent cochleovestibular communication of Edward Cock is a distinct inner ear malformation: implications for cochlear implantation. Ann. Otol. Rhinol. Laryngol. 2006;115:595–606. doi: 10.1177/000348940611500805. [DOI] [PubMed] [Google Scholar]
- Minami S.B., Takegoshi H., Shinjo Y., Enomoto C., Kaga K. Usefulness of measuring electrically evoked auditory brainstem responses in children with inner ear malformations during cochlear implantation. Acta Otolaryngol. 2015;135:1007–1015. doi: 10.3109/00016489.2015.1048377. [DOI] [PubMed] [Google Scholar]
- Norrix L.W. Hearing thresholds, minimum response levels, and cross-check measures in pediatric audiology. Am. J. Audiol. 2015;24:137–144. doi: 10.1044/2015_AJA-14-0095. [DOI] [PubMed] [Google Scholar]
- Pradhananga R.B., Thomas J.K., Natarajan K., Kameswaran M. Long term outcome of cochlear implantation in five children with common cavity deformity. Int. J. Pediatr. Otorhinolaryngol. 2015;79:685–689. doi: 10.1016/j.ijporl.2015.02.015. [DOI] [PubMed] [Google Scholar]
- Sennaroglu L. Cochlear implantation in inner ear malformations–a review article. Cochlear Implants Int. 2010;11:4–41. doi: 10.1002/cii.416. [DOI] [PubMed] [Google Scholar]
- Teoh S.W., Pisoni D.B., Miyamoto R.T. Cochlear implantation in adults with prelingual deafness. Part II. Underlying constraints that affect audiological outcomes. Laryngoscope. 2004;114:1714–1719. doi: 10.1097/00005537-200410000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xia J., Wang W., Zhang D. Cochlear implantation in 21 patients with common cavity malformation. Acta Otolaryngol. 2015;135:459–465. doi: 10.3109/00016489.2014.990054. [DOI] [PubMed] [Google Scholar]
- Yamazaki H., Naito Y., Fujiwara K., Moroto S., Yamamoto R. Electrically evoked auditory brainstem response-based evaluation of the spatial distribution of auditory neuronal tissue in common cavity deformities. Otol. Neurotol. 2014;35:1394–1402. doi: 10.1097/MAO.0000000000000375. [DOI] [PubMed] [Google Scholar]
- Young J.Y., Ryan M.E., Young N.M. Preoperative imaging of sensorineural hearing loss in pediatric candidates for cochlear implantation. Radiographics. 2014;34:E133–E149. doi: 10.1148/rg.345130083. [DOI] [PubMed] [Google Scholar]
- Zarandy M.M. Transmastoid labyrinthotomy approach for cochlear implantation in a common cavity malformation: a case report. Ear Nose Throat J. 2008;87:E1–E3. [PubMed] [Google Scholar]
- Zhang D., Zhang Y., Tian H. Indication and approach of cochlear implantation with common cavity. J. Clin. Otorhinolaryngol. Head Neck Surg. 2007;21:444–446. [PubMed] [Google Scholar]