Abstract
Background
Substance misuse and associated health-risking behaviors are prevalent in emerging adulthood. There is a knowledge gap concerning the post-high school effects of community-based delivery systems for universal preventive interventions implemented during young adolescence. This study reports effects of the PROSPER delivery system through age 19, 7.5 years past baseline.
Methods
A cohort sequential design included 28 public school districts randomly assigned to the PROSPER partnership delivery system or usual-programming conditions. PROSPER community teams implemented a family-focused intervention in 6th grade and a school-based intervention in 7th grade. Outcomes for the age 19, post-high school report included lifetime, current, and frequency of substance misuse, as well as antisocial and health-risking sexual behaviors. Intent-to-treat, multi-level analyses of covariance of point-in-time outcomes were conducted, along with analyses of risk-related moderation of intervention effects.
Results
Results showed emerging adults from PROSPER communities reported significantly lower substance misuse across a range of types of substances, with relative reduction rates of up to 41.0%. No significant findings were observed for associated antisocial and health-risking sexual behavior indices; nor for lifetime rates of sexually transmitted infections. Risk-related moderation effects were non-significant, suggesting generally comparable outcomes across higher- and lower-risk subgroups of emerging adults.
Conclusions
The PROSPER delivery system for brief universal preventive interventions has potential for public health impact by reducing long-term substance misuse, with positive results extending beyond high school.
Keywords: Emerging adult outcomes, evidence-based, universal preventive intervention, community-university partnership model, delivery system
Epidemiological data show that substance misuse, antisocial behavior, and other health-risking sexual behaviors (HRSBs) are prevalent in emerging adulthood, both in the US–the setting for the PROSPER study–and internationally. For example, in 2014, the US annual prevalence estimates for any illicit drug use were highest among 19–22 year olds (41%; Johnston et al. 2015a). Especially noteworthy is the 6.7% annual prevalence estimate of narcotic use, including heroin and non-medical use of prescription opioids, which is higher among young adults (aged 19–26) than any other age group. As an example of the prevalence of HRSBs, in the US approximately 24% of young adults have more than one sex partner annually and 30% of unmarried respondents report never using a condom (Johnston et al. 2015b). Concerning antisocial behaviors, offending behavior (violence and theft) peaks at around 10–12% between ages 17–19, although it then begins to decline (Piquero et al. 2007; Loeber et al. 2008).
Internationally, surveys of 18–29 year olds in several major countries in Europe, Africa, Asia, and the Americas have been conducted by the World Health Organization and other international agencies. They show pervasive substance misuse among young adults, albeit with a high degree of variability in the drugs of choice across countries. For example, while 44.1% of 22–29 year olds living in France reported that they used cannabis, only 13.7%, 1.8%, and 1.9% of those living in Italy, China, and Nigeria, respectively, reported such use (Degenhardt et al. 2008).
Substance use and associated health-risking behaviors have health, social, and economic consequences, at both the individual and societal levels. These problems can lead to later substance abuse and dependence (Swendsen et al. 2010); marijuana use has been linked to later addiction, altered brain development, diminished achievement, and ongoing mental health difficulties (Fergusson & Boden, 2008; US Department of Justice, Drug Enforcement Administration, 2014; Volkow et al. 2014; Fischer et al. 2015; Coffey & Patton, 2016); alcohol misuse is associated with multiple health-related disease and injury conditions (Rehm, 2011); and deaths from prescription drug overdose in the US included 1,741 young adults in 2014 (National Institute on Drug Abuse, February, 2016a). HRSBs can lead to sexually-transmitted diseases, unplanned pregnancy, and early parenthood (Van Ryzin et al. 2011). Socially, emerging adults who exhibit substance misuse and other health-risking behaviors may not transition into positive adult roles; they may show interpersonal difficulties, drop out of school, become parents while relatively young, or take on undesired full-time employment (Sussman, 2013). The costs of tobacco, alcohol, and illicit drug use to the US economy has been estimated at over $700 billion annually (National Institute on Drug Abuse, February, 2016b); the costs of sexually transmitted infections have been estimated at $16 billion in lifetime direct medical costs alone (National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, 2013).
The primary adolescent socializing environments (family and school/peer) exert substantial influence on risk and protective factors for substance misuse and other health-risking behaviors during adolescence. Protective factors include family relationship quality, monitoring, and parent-child warmth and affection; positive peer relationships distinguished by trust and affection; and school engagement, along with school task completion (Murray & Farrington, 2010; Stone et al. 2012). For this reason, preventive interventions designed to influence family-, school-, and peer-related risk and protective factors have been developed and tested with positive results (NRC-IOM, 2009). The literature emphasizes the importance of providing preventive intervention during the developmental window when adolescents are just beginning to use substances and conduct problems are escalating (Offord & Bennett, 2002; Anthony, 2003; Chen et al. 2004; Spoth et al. 2009a).
There is an emerging literature on effects of universal preventive interventions implemented during young adolescence, especially effects on young adult substance misuse (Hawkins et al. 2005; Poduska et al. 2008; Riggs et al. 2009; Spoth et al. 2013b; Botvin & Griffin, 2014a; Kellam et al. 2014). A subset of articles report on substance misuse outcomes among young adults for the same interventions that were implemented through the PROSPER delivery system (detailed in the Methods section, Spoth et al. 2009b, 2014b, 2016). The pattern of positive, long-term findings across multiple trials is noteworthy, especially considering that effects persist even after students leave the settings in which the interventions were implemented and setting-related factors are no longer operative (e.g., reduced negative peer influences, see Osgood et al. 2013).
There is evidence that interventions addressing multiple risk and protective factors, designed to reduce substance misuse, also have crossover effects on other young adult health-risking behaviors or problems (e.g., conduct problem behaviors or internalizing outcomes)–even when no intervention content directly addresses those behaviors or problems (Trudeau et al. 2012; Kellam et al. 2014; Oesterle et al. 2015). A number of randomized controlled trials have demonstrated long-term crossover effects on emerging adult HRSBs (Botvin & Griffin, 2014b; Kellam et al. 2014; Spoth et al. 2014a; Perrino et al. 2016).
The use of community-based delivery systems guided by key stakeholders in a community can create high quality implementation and sustainability of universal preventive interventions. In addition to the PROSPER model, Communities That Care is a well-recognized community-based decision-making and program delivery model (CTC: Hawkins & Catalano, 1992). In a multi-state study of 24 small to moderate sized communities focused on prevention targeting youth ages 10–14, their families, and their schools, outcomes evaluated at age 19 showed a significant overall effect across lifetime measures of substance use for males but not for females, nor for the full sample. “Lifetime abstinence” from delinquency in the full sample was significantly higher in CTC communities; however, significant intervention effects were not found for specific delinquent or violent behaviors, nor for recent substance misuse, substance use disorders or sexual risk behaviors (Oesterle et al. 2015).
Here we examine long-term emerging adult outcomes of PROSPER, a delivery system that utilizes the outreach arm of the land grant university, the Cooperative Extension System (CES), to catalyze community teams to deliver school-based and family-focused interventions targeting middle school students. The PROSPER delivery system model (described in detail elsewhere; Spoth et al. 2004) consists of: (1) teams of community stakeholders linked with public schools and led by local CES staff, (2) Prevention Coordinators (PCs) connected with the land grant university’s CES, and (3) a team of state-level university researchers and CES faculty. Prevention Coordinators serve as liaisons between the community and university teams, providing ongoing, proactive technical assistance to community teams to optimize team functioning and program delivery. (See online supplement for more detail about the PROSPER model).
Effectiveness of the PROSPER model (Spoth et al. 2004, 2007c) throughout middle and high school has been documented in earlier reports on this cluster randomized controlled trial, which began in 2001. Previously reported findings include effective participant recruitment (Spoth et al. 2007a), maintenance of high quality implementation (Spoth et al. 2007b), and sustainability of intervention delivery (Welsh et al. 2016). Earlier analyses of program impact on youth, parent, and family skills and behaviors–hypothesized to mediate impact on longer-term substance misuse–have shown significant effects on a range of outcomes. These include parenting and family outcomes (e.g., general child management, parent-child affective quality, parent-child activities, family environment), and youth outcomes (e.g., problem solving, assertiveness, association with antisocial peers, perceived substance use norms; see Redmond et al. 2009). Analyses have demonstrated significantly lower levels of substance misuse for the intervention group, relative to controls, for past month, past year, and growth trajectory slopes, especially for potentially more serious illicit substance misuse (e.g., marijuana, methamphetamine, prescription drug misuse), at both 4.5 and 6.5 years past baseline (grades 10 and 12, Spoth et al. 2011 grades 10 and 12, Spoth et al. 2013a). Further, these analyses showed that intervention effects for higher risk youth were comparable to or stronger than effects for lower risk youth. Finally, effects also were demonstrated on associated adolescent conduct problem behaviors through 6.5 years past baseline, with positive effects through 12th grade (Spoth et al. 2015).
Since youth have left high school our research focus has shifted to examining whether effects are sustained. Although a failure to sustain effects during the post-secondary follow up period would not negate beneficial effects at earlier ages (given the detrimental impact of adolescent substance misuse on relationships, disruptive behaviors, and academic functioning–as well as potential long-term brain and health effects of use during adolescent development), findings supporting sustained effects would provide further evidence of long-term benefits of universal prevention initiated during early adolescence. We also further explore whether intervention effects for higher-risk participants differ from lower-risk participants, as has been found in earlier reports.
Based on the literature cited above and the demonstrated PROSPER effects on proximal mediators and adolescent substance misuse, we hypothesized that effects on substance misuse would be sustained as study participants progress into emerging adulthood, during their first post-high school year, with additional intervention effects hypothesized for ancillary outcomes, including associated risk behaviors (antisocial behavior, HRSBs) and their consequences (STIs).
METHODS
Community Selection and Assignment
Twenty-eight rural communities were recruited from Iowa and Pennsylvania (14 in each state). Eligibility requirements included a community school district enrollment of 1,300 to 5,200 students and relevant stakeholder (extension and school district) agreement to random assignment, as well as a willingness and capacity to support PROSPER model implementation if assigned to the intervention condition. Following their enrollment, school districts were blocked on the basis of size and location, then randomized and informed of their assignment to the intervention condition. The participating universities’ Institutional Review Boards approved the study procedures. Additional details related to recruitment procedures are available in Spoth et al. (2007a).
Sample and Data collection
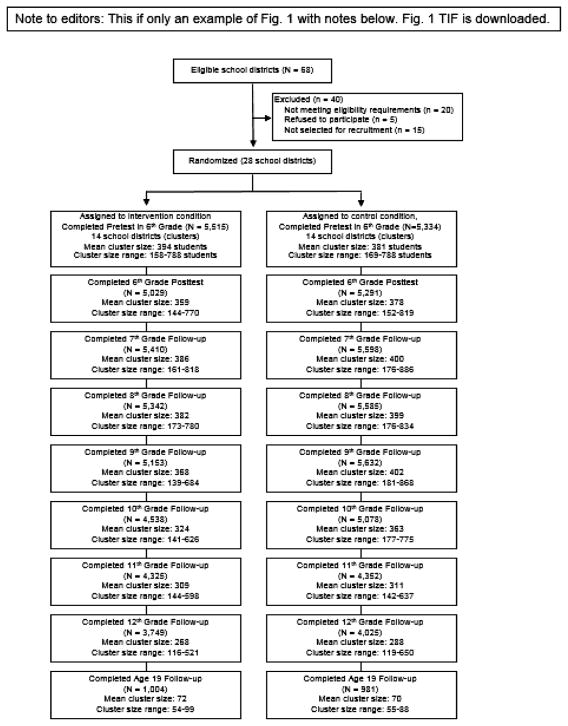
The study began with two successive cohorts of 6th graders enrolled in the 28 participating school districts. Fig. 1 summarizes sample tracking over the waves of data collection. All enrolled 6th graders from the two cohorts were recruited for participation. Approximately 90% of the eligible sample provided baseline data. Most students were White (85%), 51% were female, 64% lived with both biological parents, and 31% received free or reduced-cost school lunchesa. The average age of participants was 11.8 years at baseline and 19.5 years for the current report.
Fig. 1.
In-school survey and emerging adult follow up assessment: total participation by wave.*
*Reported participation rates include all students in both study cohorts completing the in-school survey at the indicated wave through 12th grade. All students enrolled in the project school districts and in the targeted grades were eligible for participation, regardless of their participation in earlier survey waves, as a result, participation at later waves may exceed participation at pretest. Emerging adult assessments were conducted with randomly selected participants from the in-school assessment sample that completed 6th grade pretest assessments and were still enrolled in their baseline school district in the 9th grade.
In-class pretest self-report assessments were conducted with 6th graders during the fall semesters of 2002 (for Cohort 1) and 2003 (for Cohort 2). Follow-up assessments through high school were conducted annually in the springs of 6th to 12th grade (i.e., from 0.5 years to 6.5 years past baseline). On average, 88% of all eligible students completed in-school surveys across the eight data points, with slightly higher rates of participation at earlier data collection points.
Because of the high cost of following the entire sample into adulthood, after the spring of 12th grade, a randomly selected subsample of 1,985 youth were recruited for continued follow-up. Participants who completed the 6th grade baseline assessment and were still enrolled in the same school district in the 9th grade were eligible for participation. Subsample selection was stratified by school district, gender, and risk status. Risk status was based on how many of the following five factors were reported by participants at baseline: lifetime gateway substance use (alcohol, cigarettes, or marijuana); conduct problem behaviors (at least 2 of 12); eligibility for the free/reduced cost school lunch program; lower family cohesion (dichotomized); and living with only one or no biological parents. Students were classified as higher-risk if they reported (a) any three or more of the five risk factors or (b) two risk factors, if gateway substance use and/or conduct problems were among the two. In order to have sufficient statistical power to investigate risk-related moderation effects when applying multilevel analytic models, higher-risk participants were oversampled. They comprised 37.4% of the participating subsample, versus 29.2% of the eligible sample. At age 19, participants could complete assessments either through a computer-assisted telephone interview or a web-based survey (16% and 84%, respectively). Sample and survey participation by school district and risk level is available online.
PROSPER Partnership Delivery System
In the communities assigned to the intervention condition, stakeholder teams of 8–12 individuals were formed, including the local CES-based team leader, a public school co-leader, representatives of local human service agencies (e.g., mental health, substance abuse), and parent and youth representatives. Teams selected a sequence of two interventions from a menu of evidence-based programs to be delivered, beginning with a family-focused intervention for 6th graders and their parents, followed by a school-based intervention implemented for the same cohort of youth in 7th grade. As part of the trial, communities administered these programs for two successive cohorts of students. (See the detailed description online.)
For their family-focused intervention, all 14 community teams selected the Strengthening Families Program: For Parents and Youth 10–14 (SFP 10–14). For their school-based intervention, four community teams selected Life Skills Training (LST), four selected Project Alert, and six selected the All Stars curriculum. Brief information on each program is in Table 1 (for more detail, see Spoth et al. 2007c).
Table 1.
Brief description of PROSPER universal preventive interventions
| Family Intervention for 6th Graders | |||
|---|---|---|---|
| Intervention | Description | Implementation Adherence Rate | Key Citations |
| Strengthening Families Program: For Parents and Youth 10–14 (SFP 10–14) | 7-session program that focuses on enhancing parenting skills (e.g., nurturance, limit setting, and communication), as well as youth substance refusal and other prosocial skills | >90% | Molgaard et al. 1997; Spoth et al. 2011 |
| School Interventions for 7th Graders | |||
| Life Skills Training (LST) | 15-lesson universal preventive intervention designed to promote skills, such as peer resistance and self-management, and strategies for avoiding the use of substances | 89% | Botvin et al. 1996; 2000 |
| Project ALERT | 11-session social influence-focused intervention intended to change students’ beliefs about substance use norms, help students identify and resist pro-substance use pressures from peers and the media, and strengthen their refusal self-efficacy | 89% | Rosenstock et al. 1988 |
| All Stars | 13-session intervention intended to influence students’ perceptions about substance use and violence, increase accuracy of their beliefs about peer norms, have students make a personal commitment to avoid negative behaviors, and increase their bonding to school | 91% | Hansen, 1996 |
Family intervention for 6th graders
Across the two successive cohorts of families of 6th graders, there were 142 SFP 10–14 program groups offered in the 14 intervention communities. A total of 1,064 families attended at least one session, representing 17% of all eligible families. Of these, 90% attended at least four of the seven sessions and 63% attended at least six.
School interventions for 7th graders
The school-based program was implemented with Cohort 1 7th grade students in the second year of model implementation and with the Cohort 2 7th grade students the following year. Each school-based program was delivered in a class normally taken by all 7th grade students, generally by a trained classroom teacher (Spoth et al. 2007b).
Measures
Outcomes evaluated at age 19 were selected to (a) provide continuity with prior outcome reports, and (b) encompass developmentally-relevant young adult problem behaviors that have the potential for significant social-, health-, and economic-related harm. Measures were informed by those reported in previous studies (e.g., Spoth et al. 2001) and included self-reported substance misuse, conduct problems in the form of antisocial behavior, HRSBs, and STIs. Substance misuse outcomes include lifetime use of illicit or non-prescribed drugs, drug- and alcohol-related problems, along with current use and frequency of use of more commonly used substances. Substance misuse questions were adapted from Monitoring the Future items (Johnston et al. 2015a); items assessing antisocial behaviors were adapted from Elliot and colleagues (Elliott et al. 1985). Multi-item measures in the current report are count indices designed to assess cumulative numbers of risk behaviors or negative outcomes (in contrast to scales representing latent constructs assessed via multiple indicators); as such, alpha reliabilities were not calculated.
Lifetime Substance Misuse and Related Problems
Lifetime substance misuse measures included use of marijuana, cocaine, ecstasy, methamphetamine, LSD, non-prescribed narcotics, and amphetamines, scored as any use (1) versus no use (0). The Illicit Substance Use Index includes lifetime use of five substances (dichotomized and summed); methamphetamine, ecstasy, LSD (or other hallucinogens, including mushrooms), cocaine, and GHB or Rohypnol. The Prescription Drug Misuse Index measured “overall” prescription drug misuse and included three items (dichotomized and summed) addressing lifetime non-prescribed use of narcotics (e.g., Vicodin, Oxycontin, Percocet), amphetamines, and barbiturates.
Current use and frequency
More commonly used substances were measured with a current, one-month time frame; a one-year time frame was applied for those substances less frequently used. These dichotomous measures indicated past-month drunkenness, past-month cigarette smoking, past-year marijuana use, and past-year use of narcotics not prescribed by a doctor. Past-year frequency of use was assessed for cigarette use, drinking, drunkenness, driving after drinking, marijuana use, and narcotic use. Frequencies were truncated at 150 times in the past year to prevent undue influence of outliers.
Drug- and alcohol-related problems
Indices were constructed to assess problems resulting from drug use and from alcohol use. Each index consisted of 15 dichotomous items adapted from the Short Inventory of Problems: Alcohol and Drugs (Blanchard et al. 2013) and addressed a range of substance-related problems and issues. Adaptation for the current study involved constructing measures to address drug- and alcohol-related problems separately, in contrast to the original measure, which assessed drug and alcohol problems jointly. Examples include: “You have failed to do what’s expected of you because of your [drug/alcohol] use,” and “You have had money problems because of your [drug/alcohol] use.”
Health-Risking Sexual Behaviors (HRSBs) and Sexually Transmitted Infections (STIs)
HRSBs were assessed as an index of 11 dichotomously scored items. Examples include: lifetime intercourse, lifetime anal intercourse, number of intercourse partners (three or more), number of anal intercourse partners (more than one), past-year intercourse with someone they did not know well, and early onset of first intercourse (before age 14). STIs were assessed as an index of seven dichotomous items assessing lifetime diagnoses of gonorrhea, syphilis, herpes or warts, chlamydia, Hepatitis B, AIDS/HIV, and any other STI.
Antisocial behaviors
A count of antisocial and delinquent or illegal behaviors, adapted from Elliott et al. (1985), was constructed using 13 dichotomously-scored self-report items concerning past-year behaviors (behavior present versus absent). Example behaviors include: “Steal money or take something that did not belong to you,” “Beat up or fight with someone because you were mad at them,” “Drive a car recklessly,” and “Sell stolen goods.”
Analyses
Multi-level ANCOVAs were conducted to test for intervention effects on outcomes. Binary outcomes were analyzed using SAS PROC GLIMMIX; other outcomes were analyzed using SAS PROC MIXED. These analytic procedures were selected to accommodate this study’s cluster-randomized design and address relevant variance components across model levels. Analyzed models included the design factors of block (school district size and location), experimental condition, cohort, and state. An intent-to-treat approach was applied for all analyses. Effect size estimates are based on Cohen’s d. In the last report on PROSPER high school outcomes, one-tailed significance levels and related p-values were applied because all intervention-control differences were in the expected direction at each earlier wave of data collection. For the current report, because less evidence was available to definitively support unidirectional hypotheses of effects at this developmental stage and for new measures of health-risking and other behaviors not previously tested with this sample, two-tailed p-values are reported. Risk status was included as a post-hoc factor; Risk × Condition was included in order to assess risk moderation effects (conducted using the CONTRAST statement in SAS PROC MIXED and GLIMMIX). Risk-related moderation analyses were conducted to evaluate whether intervention effects for higher-risk youth were comparable to or stronger than effects for lower risk youth, as has been found in earlier analyses of PROSPER data. Although this risk measure is slightly different than the one used in earlier reports (Spoth et al. 2011,Spoth et al. 2013a), it was selected because it is the measure that was used to stratify the young adult sample. Notably, 85% of those classified as higher- or lower-risk using this measure would be in the same risk classification category using the prior measure (which was based exclusively on gateway substance initiation at the baseline assessment).
Model-based relative reduction rates (RRRs) were calculated for binary outcomes to illustrate the practical significance of findings; they indicate the proportional reduction in behaviors in the intervention group relative to controls; that is, how much lower the estimated prevalence of a behavior is for those in the intervention group than in the control group, expressed as a percentage of the control group prevalence (e.g., if the estimated prevalences in the intervention and control groups were 40% and 50%, respectively, the RRR for the intervention group would be 20% (i.e.: [50% – 40%] ÷ 50% = 20%).
RESULTS
Sample Quality
Pretest equivalence of the two conditions was assessed; there were no significant differences on any sociodemographic measure (e.g., gender, age, race, school lunch status) or on any outcomes. Differential representation in the age 19 sample was assessed by examining whether the two-way interaction of Condition × Outcome pretest score predicted participation at age 19. No significant interactions were found.
Intervention Effect Estimates
Intervention main effect estimates (IMEE)
IMEEs are reported in Table 2. Results show significant IMEEs indicating lower levels of substance misuse in the intervention group across a range of substance use outcomes: Significant IMEEs were found for lifetime use of most individual illicit drugs (marijuana, cocaine, ecstasy, methamphetamine, LSD, non-prescription narcotics), as well as for the illicit and prescription drug misuse indices. In addition, significant IMEEs were found for the drug-related problems index and for the frequencies of cigarette and marijuana use. RRRs for significant binary outcomes favored the intervention group in all instances, and ranged from 9.4% (lifetime marijuana use) to 41.0% (lifetime methamphetamine use). There were no significant findings for current use measures, nor for HRSB or STI indices, or for the antisocial behavior index.
Table 2.
Intervention-control differences for emerging adult outcomes
| Control | Intervention | F-value (1,12) | p-value (two-tailed) | RRR (ES) | Confidence Interval of Difference in LS Means (C-I) | |||
|---|---|---|---|---|---|---|---|---|
| N | LS Mean (SE) | N | LS Mean (SE) | |||||
| Lifetime Illicit and Non-Prescribed Substance Use | ||||||||
| Marijuana | 974 | 0.618 (0.022) | 994 | 0.560 (0.022) | 5.27 | 0.040 | 9.4% | (0.002, 0.113) |
| Cocaine | 978 | 0.132 (0.013) | 1,001 | 0.092 (0.011) | 5.48 | 0.037 | 30.3% | (0.006, 0.073) |
| Ecstasy | 976 | 0.169 (0.014) | 1,000 | 0.113 (0.012) | 8.99 | 0.011 | 33.1% | (0.020, 0.092) |
| Methamphetamine | 975 | 0.105 (0.011) | 1,000 | 0.062 (0.008) | 9.59 | 0.009 | 41.0% | (0.015, 0.070) |
| LSD | 976 | 0.114 (0.014) | 999 | 0.074 (0.011) | 5.82 | 0.033 | 35.1% | (0.006, 0.074) |
| Narcotics (non-prescription) | 977 | 0.299 (0.024) | 1,000 | 0.222 (0.020) | 6.01 | 0.031 | 25.8% | (0.015, 0.138) |
| Amphetamine (non-prescription) | 976 | 0.130 (0.014) | 1,000 | 0.120 (0.013) | 0.30 | 0.594 | 7.7% | (−0.028,0.048) |
| Illicit Substance Use Index | 979 | 0.253 (0.015) | 1,002 | 0.189 (0.013) | 10.15 | 0.008 | 25.3% | (0.025, 0.103) |
| Prescription Drug Misuse Index | 979 | 0.347 (0.023) | 1,002 | 0.278 (0.021) | 5.11 | 0.043 | 19.9% | (0.009, 0.129) |
| Current Substance Use | ||||||||
| Past Month Cigarette | 972 | 0.324 (0.019) | 996 | 0.288 (0.018) | 2.18 | 0.166 | 11.1% | (−0.015, 0.088) |
| Past Month Drunkenness | 749 | 0.501 (0.023) | 776 | 0.489 (0.023) | 0.15 | 0.703 | 2.4% | (−0.052, 0.076) |
| Past Year Marijuana | 913 | 0.315 (0.019) | 951 | 0.281 (0.018) | 2.08 | 0.175 | 10.8% | (−0.018, 0.086) |
| Past Year Narcotics | 959 | 0.075 (0.012) | 995 | 0.060 (0.011) | 0.85 | 0.374 | 20.0% | (−0.017, 0.048) |
| Frequency of Substance Use | ||||||||
| Cigarettes | 969 | 2.000 (0.052) | 989 | 1.824 (0.052) | 7.09 | 0.021 | (0.15) | (0.032, 0.320) |
| Drinking | 715 | 24.64 (1.72) | 730 | 23.60 (1.71) | 0.19 | 0.668 | (0.03) | (−4.118, 6.200) |
| Drunkenness | 749 | 14.43 (1.07) | 776 | 13.41 (1.05) | 0.46 | 0.510 | (0.04) | (−2.247, 4.282) |
| Drinking and driving | 836 | 1.06 (0.14) | 873 | 0.88 (0.13) | 0.85 | 0.375 | (0.05) | (−0.239, 0.588) |
| Marijuana | 913 | 15.32 (1.62) | 951 | 10.80 (1.60) | 5.37 | 0.039 | (0.13) | (0.270, 8.767) |
| Narcotics (non-prescription) | 959 | 2.27 (0.52) | 995 | 0.82 (0.51) | 3.98 | 0.069 | (0.14) | (−0.139, 3.042) |
| Drug/Alcohol-related Problems | ||||||||
| Drug-related Problems | 865 | 1.275 (0.086) | 901 | 0.925 (0.086) | 8.42 | 0.013 | (0.14) | (0.120, 0.579) |
| Alcohol-related Problems | 980 | 1.885 (0.097) | 1,004 | 1.725 (0.096) | 1.37 | 0.264 | (0.06) | (−0.098, 0.417) |
| Health-Risking Sexual Behavior/STIs | ||||||||
| HRSB Index | 966 | 2.539 (0.070) | 989 | 2.492 (0.069) | 0.23 | 0.641 | (0.02) | (−0.617, 0.262) |
| Lifetime STI | 981 | 0.036 (0.007) | 1,004 | 0.025 (0.006) | 1.59 | 0.231 | 30.6% | (−0.005, 0.028) |
| Antisocial/Delinquent Behaviors | 976 | 0.622 (0.040) | 998 | 0.632 (0.040) | 0.03 | 0.862 | (0.01) | (−0.132, 0.112) |
LS Means are model-based means. Analytic models include Block (school district size and location), State, Intervention Condition, and Cohort as design factors and Risk Status as a post-hoc factor. Analyses of binary outcomes were conducted using SAS PROC GLIMMIX; Relative Reduction Rates (RRRs) were calculated for binary outcomes. Analyses of continuous outcomes were conducted using PROC MIXED; Cohen’s d was employed for effect size calculations.
To evaluate the sensitivity of results to the factors included the analytic model, we conducted analyses utilizing a simpler analytic model. Results were similar to those reported above.b In addition, to further evaluate whether effects observed during high school were sustaining, diminishing or increasing, post hoc analyses also were conducted to examine substance new user rates after the post high school time point. Results showed those rates were lower for the intervention group for all outcomes, with one exception, but that they did not attain statistical significance (two-tailed).c These supplemental analyses are consistent with the suggestion of sustaining effects evidenced when applying the full analytic model based on the experimental design.
Risk moderation of intervention effect estimates
Risk moderation analyses found a significant Condition by Risk effect only for drug-related problems—the intervention effect estimate in this case was larger for the higher risk participants. However, that noted, the intervention-control difference was larger for the higher-risk participants than the lower-risk participants for most outcome variables (see online supplement for the table of risk moderation results). To illustrate the observed patterns of findings across study sites (school districts) by treatment condition and risk level, scatterplots for representative outcomes are provided in Fig. 2.
Fig. 2.
Illustrative outcomes (lifetime substance prevalence) for each school district by intervention condition and risk level.
DISCUSSION
Results indicated that a robust pattern of statistically significant PROSPER intervention effect estimates on primary substance misuse outcomes, previously found through the 12th grade, was still in evidence at age 19. These findings provide support for the utility of the PROSPER delivery system to provide preventive health benefits into emerging adulthood. It is noteworthy that, despite the changes occurring in participants’ social environments following high school, evidence of positive intervention impact remained.
Overall, evidence for positive intervention effects was most pronounced for the primary substance misuse outcomes targeted by PROSPER, particularly lifetime misuse of illicit substances and non-prescribed narcotics, drug use problems, and non-alcohol-related frequency measures. The reasons for the lack of significant results for current use outcomes are not entirely clear; in all cases the mean scores favored the intervention group, and the RRRs were in the 10–20% range in three of four cases. In the case of marijuana use, intervention effect tests were statistically significant for both lifetime and frequency outcomes, suggesting that the dichotomous, current use measures might have been less sensitive to intervention-control differences. There also may be different patterns of current use among subgroups of participants defined by college enrollment or other changes in physical and social environments (e.g., change to a non-rural residence). Following the next wave of data collection, when participants will be completing their college years, we will examine this possibility. Alcohol-related effects were non-significant at age 19. Current alcohol use and frequency outcomes continued to reflect the general pattern of findings in the high school waves of data collection; that is, outcomes were weaker than those concerning illicit or non-prescription drug use.
Although significant intervention effect estimates for antisocial behaviors were found through high school (Spoth et al. 2015), effect estimates for antisocial and illegal behaviors were non-significant at age 19, when developmental trends indicate that these behaviors in general populations begin to decline (Sameroff et al. 2004). The lack of significant intervention-control differences could be the result of a combination of factors, including developmental epidemiological trends toward lower prevalence of the types of behaviors assessed. The types of items included in the antisocial behavior index are representative of the behaviors that are prevalent during late adolescence; more serious forms of young adult antisocial or offending behaviors (e.g., arrest records) will be obtained and reported for a subsequent wave of data collection.
Because the low overall rates of both lifetime STIs (approximately 3%), and HRSBs (approximately 3%, with an approximate mean of 2.5 of 11 potential risk behaviors) constrained variability, our ability to detect intervention-control differences was limited; intervention effect estimates were non-significant for both outcomes. HRSBs were examined as a possible “crossover” outcome of the interventions delivered, given that there was no instructional content directly addressing these behaviors.
In contrast to findings during the 11th and 12th grades (Spoth et al. 2015), risk moderation results at age 19 were considerably more limited. In part, this may be due to the smaller sample selected for longer follow-up. Nonetheless, the pattern showing generally stronger intervention effect estimates for the higher-risk group was consistent with the pattern in earlier analyses described in the introduction. One consideration is that, despite the originally large sample size, due to the modest number of clusters in the analysis (at level 2), this follow-up study was potentially underpowered. Analyses of main effects were likely underpowered in some cases, and the analyses of risk-related moderation effects, were likely underpowered in most cases.
The most recent major reports on the prevention of behavioral health-related disorders by the National Research Council and the Institute of Medicine (NRC-IOM, 2009), and on addiction prevention by the US Surgeon General (US Department of Health and Human Services, Office of the Surgeon General, 2016) noted the important knowledge gap concerning the effects of adolescent-stage preventive interventions on young adult outcomes. The current findings add to a growing literature addressing this gap and indicate the potential benefits of developmentally well-timed interventions in early adolescence for substance-related outcomes during emerging adulthood, further substantiating results concerning substance misuse presented in our earlier reports from other projects (Spoth et al. 2009b, 2014a, 2014b), and from other research groups that have reported results into young adulthood (Oesterle et al. 2015).
As described in the introduction, we hypothesized that intervention effects on putative proximal mediators of externalizing behaviors, including enhanced young adolescent skills, parenting, and family environment would lead to subsequent effects on substance misuse and associated, health-risking behaviors. Results from prior PROSPER reports on proximal mediators, including positive effects on peer social networks (Osgood et al. 2013) and crossover effects on non-targeted behaviors, are consistent with these mechanisms of effects. Moreover, early initiation is one of the most powerful predictors of later substance misuse. In earlier reports, we found delayed initiation among intervention group youth; such delays typically are associated with reduced substance misuse in late adolescence and emerging adulthood (Grant & Dawson, 1998; Grant et al. 2001). This point highlights the critical importance of the developmental timing of preventive intervention. PROSPER community teams delivered the interventions when some students were beginning to experiment with substance use, but before they moved to more frequent or serious use. Nonetheless, prior reports also indicate that, for adolescents who began substance experimentation early, the progression to more serious use was dampened by the interventions (e.g., Spoth et al. 2009b, 2014b).
The reported relative reduction rates (RRRs) provide one metric with which to gauge the potential public health significance of PROSPER. RRRs for the dichotomous outcomes significantly affected by the interventions ranged from 9.4% to 41.0%. To illustrate, the RRR for lifetime non-prescribed narcotics use (25.8%) suggests that, for every 100 general population young adults (i.e., from non-PROSPER communities/school districts) who have ever misused narcotics, approximately 74 young adults from PROSPER sites would have misused narcotics. The combination of positive outcomes and cost-efficiency of the PROSPER partnership model (Spoth & Greenberg, 2011; Crowley et al. 2012) suggests its potential public health benefit, particularly in light of the likely long-term effects of reduced young adult substance misuse (e.g., Hawkins et al. 2005, 2008b; Spoth et al. 2014a;Trudeau et al. 2016). The National Research Council and Institute of Medicine Report (2009) and the recent US Surgeon General Report (2016), along with other literature (Hawkins et al. 2008a; 2012), note the practical benefits of community-based prevention delivery systems for EBIs, particularly those embedded in national delivery systems and/or those supporting practitioner-scientist partnerships (Grumbach & Mold, 2009; Spoth & Greenberg, 2011).
There are important limitations to keep in mind when considering the findings reported here. First, the sample was drawn from rural and small town populations; generalization to urban settings and/or populations that differ in relevant characteristics, such as ethnicity or geographic location, has not yet been established and will require additional research. Second, our outcome measures were based on self-reports. Self-reports may be susceptible to social desirability biases, although youth and young adult self-reports have been found to be valid in other studies (Murray et al. 1987; Smith et al. 1995). In this regard, it should also be noted that such biases, if present, would likely affect both the intervention and control groups in a similar manner, especially given the number of years that had elapsed between intervention delivery (in the 6th and 7th grades) and the age 19 assessments. Third, readers should be cognizant of the number of statistical tests conducted independently with similar types of outcomes; significance level adjustments to account for multiple tests are left to the discretion of the reader. Finally, this study is subject to the universally applicable threats to validity in experimental studies associated with the potential omission of relevant variables and the failure of randomization to balance all pertinent factors.
In conclusion, these findings support the hypothesis that implementation of the PROSPER delivery system reduces levels of substance misuse through age 19, sustaining the positive results found during adolescence, and thus further enhancing its potential public health value and supporting its evaluation and dissemination in additional communities. The practical benefits of community-based prevention delivery systems have been documented and supported in the literature (Grumbach & Mold, 2009; Office of the US Surgeon General, 2016). The PROSPER partnership model has potential to facilitate effective and efficient translation of preventive health interventions into community practice.
Acknowledgments
Work on this paper was supported by research grant DA13709 from the National Institute on Drug Abuse and co-funding from the National Institute on Alcohol Abuse and Alcoholism (R01 AA14702).
Footnotes
In the US, school children are eligible for free school lunches if their family’s income is at or below 130% of the poverty-level; if a family’s income is more than 130% of the poverty-level, but not but not more than 185% of that level, their child is eligible for reduced-cost lunches.
Specifically, we tested a school-district level model that included only intervention condition and risk-level as factors. Results yielded similar levels of significance for 19 of 22 outcomes examined. In two instances, results became less significant–the intervention effect test for lifetime marijuana use changed from significant at the .05 level to non-significant and the intervention effect test for the lifetime prescription drug index changed from significant at the .05 level to significant at the .10 level. The intervention effect test for past month cigarette use changed from not approaching significance to significant at the .10 level.
Post high school new user rates were examined for seven substance outcomes (marijuana, cocaine, ecstasy, methamphetamine, LSD, non-prescription narcotics, and non-prescription amphetamine). With the exception of marijuana use, post high school new user rates were lower for the intervention group than for the control group, albeit not significantly so at the.05 level (two-tailed test); similarly, new user rate differences for marijuana use also were non-significant. Findings concerning marijuana use are characteristic of those for other gateway substances (e.g., alcohol, cigarettes) in which lifetime rates tend to approach ceiling levels that are eventually observed for both intervention and control groups (although those levels may be reached at different ages).
Conflict of interest: None.
Ethical standards: The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
References
- Anthony J. Selected issued pertinent to epidemiology of adolescent drug use and dependence. Invited presentation to the Annenberg Commission on Adolescent Substance Abuse meeting; Philadelphia, PA. 2003. Aug 1, [Google Scholar]
- Blanchard KA, Morgenstern J, Morgan TJ, Lobouvie EW, Bux DA. Assessing Consequences of Substance Use: Psychometric properties of the inventory of drug use consequences. Psychology of Addictive Behaviors. 2013;17:328–331. doi: 10.1037/0893-164X.17.4.328. [DOI] [PubMed] [Google Scholar]
- Botvin GJ. Life Skills Training and the prevention of adolescent drug abuse. In: Clark D, editor. Preparing Youth for the 21st Century. Washington, DC: The Aspen Institute; 1996. [Google Scholar]
- Botvin GJ. Life Skills Training. Princeton NJ: Princeton Health Press; 2000. [Google Scholar]
- Botvin GJ, Griffin KW. Life skills training: preventing substance misuse by enhancing individual and social competence. New Directions for Youth Development. 2014a;141:57–65. doi: 10.1002/yd.20086. [DOI] [PubMed] [Google Scholar]
- Botvin GJ, Griffin KW. Toward the development of preventive interventions to reduce HRSB, HIV/AIDS, and multiple problem behaviors. Prevention Science. 2014b;15(S1):S81–83. doi: 10.1007/s11121-014-0461-7. [DOI] [PubMed] [Google Scholar]
- Chen C-Y, Dormitzer CM, Gutierrez U, Vittetoe K, Gonzalez GB, Anthony JC. The adolescent behavioral repertoire as a context for drug exposrure: Behavioral autarcesis at play. Addiction. 2004;99:897–906. doi: 10.1111/j.1360-0443.2004.00774.x. [DOI] [PubMed] [Google Scholar]
- Coffey C, Patton G. Cannabis use in adolescence and young adulthood: A review of findings from the Victorian Adolescent Health Cohort Study. Canadian Journal of Psychiatry-Revue. 2016;61:318–327. doi: 10.1177/0706743716645289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crowley DM, Jones DE, Greenberg MT, Feinberg ME, Spoth RL. Resource consumption of a dissemination model for prevention programs: The PROSPER delivery system. Journal of Adolescent Health. 2012;50:256–263. doi: 10.1016/j.jadohealth.2011.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degenhardt L, Chiu W-T, Sampson N, Kessler RC, Anthony JC, Angermeyer M, Bruffaerts R, de Girolamo G, Gureje O, Huang Y, Karam A, Kostyuchenko S, Lepine JP, Mora ME, Neumark Y, Ormel JH, Pinto-Meza A, Posada-Villa J, Stein DJ, Takeshima T, Wells JE. Toward a global view of alcohol, tobacco, cannabis, and cocaine use: findings from the WHO World Mental Health Surveys. PLoS Medicine. 2008;5:e141. doi: 10.1371/journal.pmed.0050141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliott DS, Huizinga D, Ageton SS. Explaining delinquency and drug use. Beverly Hills: Sage; 1985. [Google Scholar]
- Fergusson DM, Boden JM. Cannabis use and later life outcomes. Addiction. 2008;103:969–976. doi: 10.1111/j.1360-0443.2008.02221.x. [DOI] [PubMed] [Google Scholar]
- Fischer JA, Clavarino AM, Plotnikova M, Najman JM. Cannabis use and quality of life of adolescents and young adults: Findings from an Australian birth cohort. Journal of Psychoactive Drugs. 2015;47:107–116. doi: 10.1080/02791072.2015.1014121. [DOI] [PubMed] [Google Scholar]
- Grant BF, Dawson DA. Age of onset of drug use and its association with DSM-IV drug abuse and dependence: Results from the national longitudinal alcohol epidemiologic survey. Journal of Substance Abuse. 1998;10:163–173. doi: 10.1016/s0899-3289(99)80131-x. [DOI] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Harford TC. Age at onset of alcohol use and DSM-IV alcohol abuse and dependence: A 12-year follow-up. Journal of Substance Abuse. 2001;13:493–504. doi: 10.1016/s0899-3289(01)00096-7. [DOI] [PubMed] [Google Scholar]
- Grumbach K, Mold JW. A health care cooperative extension service: Transforming primary care and community health. Journal of the American Medical Association. 2009;301:2589–2591. doi: 10.1001/jama.2009.923. [DOI] [PubMed] [Google Scholar]
- Hansen WB. Pilot test results comparing the All Stars program with seventh grade D.A.R.E. program integrity and mediating variable analysis. Substance Use and Misuse. 1996;31:1359–77. doi: 10.3109/10826089609063981. [DOI] [PubMed] [Google Scholar]
- Hawkins JD, Catalano RF, Jr, et al. Communities That Care: Action for drug abuse prevention. 1. San Francisco: Jossey-Bass; 1992. [Google Scholar]
- Hawkins JD, Catalano RF, Arthur MW, Egan E, Brown EC, Abbott RD, Murray DM. Testing Communities That Care: The rationale, design and behavioral baseline equivalence of the community youth development study. Prevention Science. 2008a;9:178–190. doi: 10.1007/s11121-008-0092-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkins JD, Kosterman R, Catalano RF, Hill KG, Abbott RD. Promoting positive adult functioning through social development intervention in childhood: Long term effects from the Seattle Social Development Project. Archives of Pediatrics and Adolescent Medicine. 2005;159:25–31. doi: 10.1001/archpedi.159.1.25. [DOI] [PubMed] [Google Scholar]
- Hawkins JD, Kosterman R, Catalano RF, Hill KG, Abbott RD. Effects of social development intervention in childhood fifteen years later. Archives of Pediatrics and Adolescent Medicine. 2008b;162:1133–1141. doi: 10.1001/archpedi.162.12.1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkins JD, Oesterle S, Brown EC, Monahan KC, Abbott RD, Arthur MW. Sustained decreases in risk exposure and youth problem behaviors after installation of the Communities That Care prevention system in a randomized trial. Archives of Pediatrics & Adolescent Medicine. 2012;166:141–148. doi: 10.1001/archpediatrics.2011.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE, Miech RA. Monitoring the Future national survey results on drug use, 1975–2104: Volume 2, college students and adults ages 19–55. Ann Arbor: Institute for Social Research, The University of Michigan; 2015a. [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE, Patrick ME, Miech RA. HIV/AIDS: Risk & protective behaviors among adults ages 21 to 40 in the U.S., 2004–2014. Ann Arbor: Institute for Social Research, The University of Michigan; 2015b. [Google Scholar]
- Kellam SG, Wang W, Mackenzie AC, Brown CH, Ompad DC, Or F, Ialongo NS, Poduska JM, Windham A. The impact of the Good Behavior Game, a universal classroom-based preventive intervention in first and second grades, on high-risk sexual behaviors and drug abuse and dependence disorders into young adulthood. Prevention Science. 2014;15(S1):S6–18. doi: 10.1007/s11121-012-0296-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loeber R, Farrington DP, Stouthamer-Loeber M, White HR. Violence and serious theft: Development and prediction from childhood to adulthood. Mahwah, NJ: Lawrence Erlbaum; 2008. [Google Scholar]
- Molgaard VM, Kumpfer KK, Fleming E. Strengthening Families Program for Parents and Youth 10–14: A video-based curriculum. Ames, IA: Institute for Social and Behavioral Research; 1997. [Google Scholar]
- Murray DM, O’Connell CM, Schmid LA, Perry CI. The validity of smoking self-reports by adolescents: A reexamination of the bogus pipeline procedure. Addictive Behavior. 1987;12:7–15. doi: 10.1016/0306-4603(87)90003-7. [DOI] [PubMed] [Google Scholar]
- Murray J, Farrington DP. Risk factors for conduct disorder and delinquency: key findings from longitudinal studies. Canadian Journal of Psychiatry. 2010;55:633–642. doi: 10.1177/070674371005501003. [DOI] [PubMed] [Google Scholar]
- National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention. Incidence, prevalence, and cost of sexually transmitted infections in the United States. Center for Disease Control and Prevention; Feb, 2013. [Accessed 02, 24-2016]. ( http://www.cdc.gov/std/stats/sti-estimates-fact-sheet-feb-2013.pdf) [Google Scholar]
- National Institute on Drug Abuse. [Accessed 02, 24-2016];Abuse of prescription (Rx) drugs affects young adults most. 2016a Feb; ( https://www.drugabuse.gov/related-topics/trends-statistics/infographics/abuse-prescription-rx-drugs-affects-young-adults-most)
- National Institute on Drug Abuse. [Accessed 02, 24-2016];Trends & Statistics. 2016b Feb; ( https://www.drugabuse.gov/related-topics/trends-statistics)
- National Research Council and Institute of Medicine. Preventing mental, emotional, and behavioral disorders among young people: Progress and possibilities (ed M E O’Connell, T Boat, K E Warner) Committee on the prevention of Mental Disorders and Substance Abuse Among Children, Youth and Young Adults; Research Advances and Promising Interventions; Board on Children, Youth and Families, Division of Behavioral and Social Sciences and Education. Washington, DC: The National Academies Press; 2009. [Accessed 5, 5-2016]. ( http://www.nap.edu/catalog/12480/preventing-mental-emotional-and-behavioral-disorders-among-young-people-progress) [Google Scholar]
- Oesterle S, Hawkins JD, Kuklinski MR, Fagan AA, Fleming C, Rhew IC, Brown EC, Abbott RD, Catalano RF. Effects of Communities That Care on males’ and females’ drug use and delinquency 9 years after baseline in a community-randomized trial. American Journal of Community Psychology. 2015;56:217–228. doi: 10.1007/s10464-015-9749-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Offord DR, Bennett KJ. Prevention. In: Rutter M, Taylor E, editors. Child and adolescent psychiatry. 4. Oxford, England: Blackwell Scientific; 2002. pp. 881–889. [Google Scholar]
- Osgood DW, Feinberg ME, Gest SD, Moody J, Ragan DT, Spoth R, Greenberg M, Redmond C. Effects of PROSPER on the influence potential of prosocial versus antisocial youth in adolescent friendship networks. Journal of Adolescent Health. 2013;53:174–179. doi: 10.1016/j.jadohealth.2013.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perrino T, Pantin H, Huang S, Brincks A, Brown CH, Prado G. Reducing the risk of internalizing symptoms among high-risk Hispanic youth through a family intervention: A randomized controlled trial. Family Process. 2016;55:91–106. doi: 10.1111/famp.12132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piquero AF, Farrington D, Blumstein A. Key issues in criminal career research. New York: Cambridge University Press; 2007. [Google Scholar]
- Poduska JM, Kellam SG, Wang W, Brown CH, Ialongo NS, Toyinbo P. Impact of the Good Behavior Game, a universal classroom-based behavior intervention, on young adult service use for problems with emotions, behavior, or drugs or alcohol. Drug and Alcohol Dependence. 2008;95:S29–44. doi: 10.1016/j.drugalcdep.2007.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Redmond C, Spoth RL, Shin C, Schainker L, Greenberg M, Feinberg M. Long-term protective factor outcomes of evidence-based interventions implemented by community teams through a community-university partnership. Journal of Primary Prevention. 2009;30:513–530. doi: 10.1007/s10935-009-0189-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehm J. The risks associated with alcohol use and alcoholism. Alcohol Research & Health. 2011;34:135–143. [PMC free article] [PubMed] [Google Scholar]
- Riggs N, Chou C, Pentz M. Preventing growth in amphetamine use: long term effects of the Midwestern Prevention Project (MPP) from early adolescence to early adulthood. Addiction. 2009;104:1691–1699. doi: 10.1111/j.1360-0443.2009.02666.x. [DOI] [PubMed] [Google Scholar]
- Rosenstock IM, Strecher VJ, Becker MH. Social learning theory and the Health Belief Model. Health Education Quarterly. 1988;88:175–183. doi: 10.1177/109019818801500203. [DOI] [PubMed] [Google Scholar]
- Sameroff AJ, Peck SC, Eccles JS. Changing econolgical determinants of conduct problems from early adolescence to early adulthood. Development and Psychopathology. 2004;16:873–896. doi: 10.1017/s0954579404040052. [DOI] [PubMed] [Google Scholar]
- Smith GT, McCarthy DM, Goldman MS. Self-reported drinking and alcohol-related problems among early adolescents: Dimensionality and validity over 24 months. Journal of Studies on Alcohol and Drugs. 1995;36:383–394. doi: 10.15288/jsa.1995.56.383. [DOI] [PubMed] [Google Scholar]
- Spoth R, Clair S, Trudeau L. Universal family-focused intervention with young adolescents: Effects on health-risking sexual behaviors and STDs among young adults. Prevention Science. 2014a;15:S47–S58. doi: 10.1007/s11121-012-0321-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spoth R, Clair S, Greenberg M, Redmond C, Shin C. Toward dissemination of evidence-based family interventions: Maintenance of community-based partnership recruitment results and associated factors. Journal of Family Psychology. 2007a;21:137–146. doi: 10.1037/0893-3200.21.2.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spoth R, Greenberg M. Impact challenges in community science-with-practice: Lessons from PROSPER on transformative practitioner-scientist partnerships and prevention infrastructure development. American Journal of Community Psychology. 2011;48:106–119. doi: 10.1007/s10464-010-9417-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spoth R, Greenberg M, Bierman K, Redmond C. PROSPER community-university partnership model for public education systems: Capacity-building for evidence-based, competence-building prevention. Prevention Science. 2004;5:31–39. doi: 10.1023/b:prev.0000013979.52796.8b. [DOI] [PubMed] [Google Scholar]
- Spoth R, Guyll M, Lillehoj CJ, Redmond C, Greenberg M. PROSPER study of evidence-based intervention implementation quality by community-university partnerships. Journal of Community Psychology. 2007b;35:981–999. doi: 10.1002/jcop.20207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spoth R, Guyll M, Shin C. Universal intervention as a protective shield against exposure to substance use: Long-term outcomes and public health significance. American Journal of Public Health. 2009a;99:2026–2033. doi: 10.2105/AJPH.2007.133298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spoth R, Redmond C, Clair S, Shin C, Greenberg M, Feinberg M. Preventing substance misuse through community-university partnerships: Randomized controlled trial outcomes 4.5 years past baseline. American Journal of Preventive Medicine. 2011;40:440–447. doi: 10.1016/j.amepre.2010.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spoth R, Redmond C, Shin C. Randomized trial of brief family interventions for general populations: Adolescent substance use outcomes four years following baseline. Journal of Consulting and Clinical Psychology. 2001;69:627–642. doi: 10.1037//0022-006x.69.4.627. [DOI] [PubMed] [Google Scholar]
- Spoth R, Redmond C, Shin C, Greenberg M, Clair S, Feinberg M. Substance use outcomes at 18 months past baseline: The PROSPER community-university partnership trial. American Journal of Preventive Medicine. 2007c;32:395–402. doi: 10.1016/j.amepre.2007.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spoth R, Redmond C, Shin C, Greenberg M, Feinberg M, Schainker L. PROSPER community-university partnership delivery system effects on substance misuse through 6½ years past baseline from a cluster randomized controlled intervention trial. Preventive Medicine. 2013a;56:190–196. doi: 10.1016/j.ypmed.2012.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spoth R, Trudeau L, Guyll M, Shin C, Redmond C. Universal intervention effects on substance use among young adults mediated by delayed adolescent substance initiation. Journal of Consulting and Clinical Psychology. 2009b;77:620–632. doi: 10.1037/a0016029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spoth R, Trudeau L, Redmond C, Shin C. Replication RCT of early universal prevention effects on young adult substance misuse. Journal of Consulting and Clinical Psychology. 2014b;82:949–963. doi: 10.1037/a0036840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spoth R, Trudeau L, Redmond C, Shin C. Replicating and extending a model of effects of universal preventive intervention during early adolescence on young adult substance misuse. Journal of Consulting and Clinical Psychology. 2016;84:913–921. doi: 10.1037/ccp0000131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spoth R, Trudeau L, Shin C, Ralston E, Redmond C, Greenberg M, Feinberg M. Longitudinal effects of universal preventive intervention on prescription drug misuse: Three randomized controlled trials with late adolescents and young adults. American Journal of Public Health. 2013b;103:665–672. doi: 10.2105/AJPH.2012.301209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spoth RL, Trudeau LS, Redmond C, Shin C, Greenberg MT, Feinberg ME, Hyun GH. PROSPER partnership delivery system: Effects on conduct problem behavior outcomes through 6.5 years past baseline. Journal of Adolescence. 2015;45:44–55. doi: 10.1016/j.adolescence.2015.08.008. http://dx.doi.org/10.1016/j.adolescence.2015.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone AL, Becker LG, Huber AM, Catalano RF. Review of risk and protective factors of substance use and problem use in emerging adulthood. Addictive Behaviors. 2012;37:747–775. doi: 10.1016/j.addbeh.2012.02.014. [DOI] [PubMed] [Google Scholar]
- Sussman S. A lifespan developmental-stage approach to tobacco and other drug abuse prevention. [Accessed 5, 5-2016];ISRN Addiction. 2013 2013 doi: 10.1155/2013/745783. Article ID 745783. ( http://dx.doi.org/10.1155/2013/745783) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swendsen J, Conway KP, Degenhardt L, Glantz M, Jin R, Merikangas KR, Sampson N, Kessler RC. Mental disorders as risk factors for substance use, abuse and dependence: Results from the 10-year follow-up of the National Comorbidity Survey. Addiction. 2010;105:1117–1128. doi: 10.1111/j.1360-0443.2010.02902.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trudeau L, Spoth R, Mason WA, Randall GK, Redmond C, Schainker L. Effects of an adolescent universal substance misuse preventive intervention on young adult depression symptoms: Mediational modeling. Journal of Abnormal Child Psychology. 2016;44:257–268. doi: 10.1007/s10802-015-9995-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trudeau L, Spoth R, Randall K, Mason WA, Shin C. Internalizing symptoms: Effects of a preventive intervention on developmental pathways from early adolescence to young adulthood. Journal of Youth & Adolescence. 2012;41:788–801. doi: 10.1007/s10964-011-9735-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- US Department of Justice, Drug Enforcement Administration. [Accessed 02, 24-2016];The dangers and consequences of marijuana abuse. 2014 May; ( http://www.dea.gov/docs/dangers-consequences-marijuana-abuse.pdf)
- US Department of Health and Human Services (HHS), Office of the Surgeon General. Facing Addiction in America: The Surgeon General’s Report on Alcohol, Drugs, and Health. Washington, DC: HHS; 2016. Nov, [PubMed] [Google Scholar]
- Van Ryzin MJ, Johnson AB, Leve LD, Kim HK. The number of sexual partners and health-risking sexual behavior: Prediction from high school entry to high school exit. Archives of Sexual Behavio. 2011;40:939–949. doi: 10.1007/s10508-010-9649-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow ND, Compton WM, Weiss SRB. Adverse health effects of marijuana use REPLY. New England Journal of Medicine. 2014;371(9):879–879. doi: 10.1056/NEJMc1407928. [DOI] [PubMed] [Google Scholar]
- Welsh J, Chilenski SM, Johnson L, Greenberg MT, Spoth RL. Pathways to sustainability: 8-year outcomes from the PROSPER project. Journal of Primary Prevention. 2016;37(3):263–286. doi: 10.1007/s10935-016-0421-z. [DOI] [PMC free article] [PubMed] [Google Scholar]