Abstract
Purpose: The configuration of the 6-minute walk test (6MWT) may influence the distance walked and comparability of results among subjects and across programmes. The purpose of this study was to evaluate the relative and absolute test–retest reliability of two 6MWT configurations and to evaluate the agreement between these two configurations in users of lower extremity prosthetics. Methods: A cross-sectional design was used to analyze data from 25 subjects completing in-patient prosthetic rehabilitation (mean age 63.12 [SD 13.77] y; 72% male). Two configurations of the 6MWT were examined, and relative and absolute test–retest reliabilities were calculated. Bland–Altman plots were constructed to evaluate agreement between configurations. Results: The relative test–retest reliability was excellent for both Configuration 1 and Configuration 2: ICC 0.97, 95% CI: 0.93, 0.98, and ICC 0.97, 95% CI: 0.94, 0.99, respectively. Comparable values for absolute test–retest reliability were also found. The Bland–Altman plot demonstrated a difference of ±63.92 meters between configurations. Conclusions: The two 6MWT configurations had excellent relative and absolute test–retest reliability, but the results from each configuration do not agree sufficiently to make them interchangeable or directly comparable. This highlights the importance of explicitly indicating the test configuration for the 6MWT when reporting results.
Key Words: amputees, exercise test, lower extremity, prostheses
Abstract
Objectif : la configuration du test de marche de 6 minutes (TM6M) peut influencer la distance marchée et la comparabilité des résultats entre sujets et entre programmes. L'objectif de cette étude était d'évaluer la fiabilité relative et absolue test–retest de deux configurations de TM6M et d'évaluer la concordance de ces deux configurations chez des personnes portant une prothèse à un membre inférieur. Méthodologie : les chercheurs ont analysé les données de 25 sujets suivant une réadaptation prothétique à l'hôpital à l'aide d'une méthodologie transversale (âge moyen de 63,12 [ÉT 13,77] ans; 72 % d'hommes). Ils ont examiné les deux configurations du TM6M et calculé la fiabilité relative et absolue test–retest. Ils ont créé un graphique Bland–Altman pour évaluer la concordance entre les configurations. Résultats : la fiabilité relative test–retest était excellente pour les deux configurations. CIC 0,97; IC à 95 % (0,93; 0,98) et CIC 0,97; IC à 95 % (0,94; 0,99), respectivement. Ils ont aussi observé des valeurs comparables pour la fiabilité absolue test–retest. Le graphique Bland–Altman a révélé une différence de±63,92 m entre les deux configurations. Conclusions : les deux configurations du TM6M ont obtenu une excellente fiabilité relative et absolue test–retest. Cependant, les résultats de chaque configuration ne concordent pas suffisamment pour les rendre interchangeables ou directement comparables. Cette constatation fait ressortir l'importance d'indiquer explicitement la configuration du test pour le TM6M au moment de rendre compte des résultats.
Mots clés : amputés, membre inférieur, prothèses, test d'exercice
Outcome measures are important tools that clinicians use to measure functional performance, identify limitations or impairments, and assess whether treatment programmes are providing benefit. For the population with lower extremity amputation (LEA), measures of functional ability and performance are particularly important because they provide information about the rehabilitation goals of improved mobility and independence. Walk tests are a subset of outcome measures that provide crucial information about mobility with prosthetic devices during rehabilitation and follow-up.1 A variety of walk tests exist, including those based on walking time for a set distance and those based on walking distance achieved in a set time.1–5 These tests are useful tools because they are able to predict future outcomes as well as functional mobility and endurance.6,7
The 6-minute walk test (6MWT) is a measure based on walking a distance in a set time,2 and it has demonstrated good to excellent test–retest reliability as a measure of functional capacity in the population with LEA.8,9 It may be preferred to the 12- and 2-minute walk tests because it is short and easy to administer2 while still involving a moderate degree of exercise intensity.9 It is also useful as a test of community-walking capacity because requirements for typical community ambulation involve distances between 132 and 342 metres,10 and comparable 6-minute walk distances have been reported in multiple populations.7,9,11,12
Originally developed as a measure of functional exercise capacity for people with chronic heart failure, the 6MWT has been studied extensively in many patient populations,11 and it has garnered excellent reviews for patients with cardiovascular, respiratory, and other medical conditions.6,12–14 In the LEA population specifically, the 6MWT has been shown to have excellent test–retest reliability9 and good intra- and interrater reliability.15 However, non-standardized configurations of the test limit the comparability of this outcome measure from one programme to another.
Walk tests, and particularly the 6MWT, can be influenced by several factors, including encouragement,16 practice,3,17 and course configuration.18–22 The original description of the 6MWT used a 33-metre straight corridor, and patients were instructed to walk repeatedly from end to end.11 This is similar to the most frequently used guidelines from the American Thoracic Society (ATS), which recommend a 30-metre straight corridor.3 No changes have been found between indoor and outdoor 6MWTs using a 30-metre straight course for those with chronic obstructive pulmonary disease (COPD), indicating that similar test configurations are transferable to the outdoors.23
Configuration does seem to matter in certain populations, however, and it can affect the distance walked by as much as 10%.18 Studies have shown that the number of turns made during the 6-minute time frame also affects the distance walked.19–22 The issue of 6MWT configuration is of particular relevance for amputee rehabilitation programmes that use this outcome measure because unilateral amputations are structurally asymmetrical, something that can predispose patients to differences in performance caused by the number of turns; stroke patients can also experience this.20 Using a gait aid may further impair the distance a patient travels on a course with more turns, although this has not specifically been studied.
Despite the impact that configuration has on distance walked, some rehabilitation programmes must rely on altered configurations for patients to complete the 6MWT. In many cases, there may be practical limitations to finding and using a 30-metre stretch of hallway that is free of objects and likely to remain free of distractions for more than 6 minutes. Some studies have intentionally changed the configuration to suit the population of interest, such as amputees,7 and others have used non-standard configurations without stating why they were selected.14
For this reason, the effect of 6MWT course configuration should be established among people with LEAs who use a prosthesis or prostheses for ambulation. The purpose of this study was (1) to evaluate the relative and absolute test–retest reliability of the 6MWT using two different configurations and (2) to evaluate whether the two testing configurations for the 6MWT agreed sufficiently so that one could be used in place of the other.
Methods
Sample
All patients admitted to Parkwood Institute's lower extremity prosthetic training programme between February and August 2012 were informed of the study and invited to participate. Those who consented to participate had to meet the following inclusion criteria: They were aged 18 years or older; they had been admitted for initial prosthetic training after their first LEA (unilateral or bilateral transtibial amputation, unilateral transfemoral amputation); and they had no cognitive or language deficits that would affect their ability to understand the study and to provide consent. Exclusion criteria were that the subject was unable or unwilling to comply with the study protocol or that the subject had prosthetic or residual limb or medical instability that, in the opinion of a physiotherapist, physician, or both, made it unsafe to complete the tests.
The study was approved by the Health Sciences Ethics Review Board of the University of Western Ontario and by the Clinical Resources Impact Committee of Lawson Health Research Institute.
Data collection
Demographic data were collected, including age, gender, date and level of amputation, etiology of amputation, comorbidities, smoking history, domestic (at discharge) living arrangements, and gait aid used. In accordance with usual discharge procedures, scores from the following measures were also obtained: timed up-and-go test, L Test, 2-minute walk test, and Activities-Specific Balance Confidence Scale.
Subjects completed four 6MWTs in the last 3 days of their in-patient admission. To avoid any effects of encouragement, verbal instruction was standardized across participants, based on the 2002 statement issued by the ATS.3 During each walk test, subjects were informed as each minute passed, were asked how they were doing, and were informed that they could rest or stop at any time. To ensure their safety, each subject was tested by one of the two physiotherapists on the team with whom he or she had undergone his or her prosthetic rehabilitation and who had the best understanding of the subject's capabilities and limitations in ambulating.
The walk tests were based on two different configurations. Configuration 1 used instructions from the 2002 ATS statement3 but consisted of a 20-metre path rather than a 30-metre path. Cross marks were taped every 1 metre along the 20-metre path. Subjects made 180-degree turns at each end of the path, essentially traversing a very narrow, 40-metre loop with sharp turns in the same direction every 20 metres. A stopwatch was used to record the distance to the nearest 0.1 metre at 2 and 6 minutes, using the cross marks as a reference.
Configuration 2 was defined by the placement of four prominent red dots on a gymnasium floor, which created a rectangle measuring 6 metres by 4 metres (20 m perimeter). Subjects were asked to walk over the dots (not around them using 90-degree turns), so that they traversed a wide, oval loop of approximately 20 metres, always walking on a gradual turn in one direction. A stopwatch and a measuring wheel (Precimeter 305; Sentech, Tempe, Arizona) were used to record the time and distance to the nearest 0.1 metre at 2 and 6 minutes; the recorder walked on the inside of the loop and measured beside the subject's inside foot.
On the first day of testing, the order of the walk tests was established using a coin toss, and the order was reversed on the second day. There was a 30-minute rest period between the two tests each day, some of which was taken up by the recorder transporting the subjects between test sites using a wheelchair.
While sitting before the start of each test, subjects were informed that they could self-select the direction in which they wanted to proceed up and down the hallway or around the gym. Once standing, subjects were asked to step up to the start of the 20-metre line or to one of the red dots on the gym floor. Once they had established that they were ready, the walk test proceeded.
During inpatient rehabilitation, the choice of gait aid was made by a physiotherapist on the basis of his or her opinion of which aid would provide the usual, safest household and community mobility for each subject. This was the gait aid used to perform the walking tests. Each subject used the same gait aid for all four tests. Furthermore, if the gait aid of choice was a rollator (rolling walker) with a seat, subjects were informed that they could rest either by standing at the rollator or by turning to sit on the seat, as they might do in the community. (The timer would continue to run.) Anyone using a rollator could also indicate that they wanted to stop the test, while sitting on the seat, at which point their wheelchair was brought to them.
If any other gait aid was used (e.g., two-wheeled walker, forearm crutches, cane or canes), subjects were informed that they could rest in standing only; the timer would continue to run. If a subject needed to sit while using a gait aid, the walk test was ended. Other than sitting on the rollator seat, subjects could sit in their own wheelchair, on plinths around the gym, or on a chair in the hallway or nearby auditorium; in this case, the test was ended, and the time at which subjects stopped was recorded. This was done to reflect what occurs during ambulation in a community setting; those with seats on their walkers are able to stop and sit when needed, but other gait aid users do not have this ability.
Data analysis
Baseline characteristics and scores on tests of balance confidence and physical function were summarized using either means and SDs or frequencies and percentages, as appropriate.
Relative reliability is the degree to which individuals maintain their position in a sample when repeated measurements are performed.24 One measure of relative reliability was calculated for the two 6MWT protocols: test–retest reliability (the degree to which a result with one instrument is equivalent to the result with the same instrument across days). The relative test–retest reliability was quantified using the intra-class correlation coefficient (ICC). An ICC value of more than 0.9 was considered excellent, values between 0.8 and 0.9 were considered good, values between 0.7 and 0.8 were considered fair, and values less than 0.7 were considered of questionable clinical value.25
Absolute test–retest reliability is the degree to which repeated measurements using the same tool vary for an individual; a smaller variation indicates a higher reliability.24 Two measures of absolute reliability were quantified from each 6MWT protocol. The first measure calculated was the standard error of measurement (SEM), for which an expression of measurement error is in the same units as the scale. This was calculated as follows: SEM=SD √(1—ICC).26 The second measure calculated was the minimum detectable change (MDC), with a 95% CI (MDC95), which is an estimate of the smallest change in the score that can be detected beyond measurement error: MDC95=SEM×√2×1.96.26
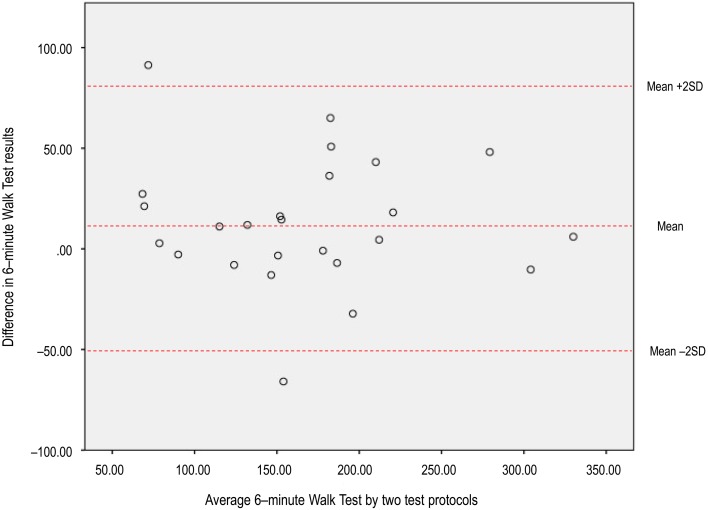
Finally, Bland–Altman plots were constructed to measure the agreement between the two 6MWT protocols, evaluating whether they agreed sufficiently so that one could be replaced by the other.27 We created a Bland–Altman plot by graphing the difference in the scores between the two testing methods against the mean of the sample scores; we used the scores from the first day of testing.
A sample size of 19 people, determined using the method described by Walter and colleagues,28 was calculated to identify a desired ICC of 0.90, with a lower bound of 0.70, given α=0.05 and β=0.20. All statistical analyses were performed using the IBM SPSS Statistics, version 22.0 (IBM Corporation, Armonk, NY).
Results
Summary demographic and other data are displayed in Table 1. A total of 52 people consented to be in the study, but only 25 people completed all testing on each of the two testing days. On the first testing day, rest stops during testing were required by 48% (n=12) of the sample for Configuration 1 and 40% (n=10) of the sample for Configuration 2. The distances walked for the two protocols were not statistically significantly different on the first day of testing (p=0.09) but were significantly different on the second day (p<0.001). The results from the second testing session for each 6MWT protocol were greater than the first, indicating a potential learning effect with repetition. The mean differences for Configurations 1 and 2 were −19.71 (SD 25.94) metres and −4.44 (SD 24.26) metres, respectively. The variables for mean difference were normally distributed.
Table 1.
Characteristics of Study Sample (n=25)
| Characteristic | No. (%)* |
| Mean (SD) age, y | 63.1 (13.8) |
| Female | 7 (28.0) |
| Etiology of amputation | |
| Diabetic | 9 (36.0) |
| Vascular | 7 (28.0) |
| Trauma | 4 (16.0) |
| Other | 5 (20.0) |
| Gait aid at discharge from in-patient rehabilitation | |
| Walker | 16 (64.0) |
| Cane or crutches | 9 (36.0) |
| No aid | 0 (0.0) |
| Discharge destination from rehabilitation | |
| Community, alone | 3 (12.0) |
| Community, with another person | 19 (76.0) |
| Assisted living | 0 (0.0) |
| Nursing home or hospital | 3 (12.0) |
| Mean (SD) BMI, kg/m2 | 24.9 (4.3) |
| Smoking status | |
| Current | 5 (20.0) |
| Recent cessation (within past 6 mo) | 1 (4.0) |
| Former smoker | 14 (56.0) |
| Never smoked | 5 (20.0) |
| Mean (SD) length of stay in rehabilitation, d | 32.3 (11.1) |
| Outcome measure of ambulation status at discharge from in-patient rehabilitation; mean (SD) | |
| Timed up-and-go test, s | 29.2 (14.9) |
| L Test, s | 55.3 (22.7) |
| 2-minute walk test, m | 62.5 (19.5) |
| Activity-Specific Balance Confidence Scale score at discharge | 73.0 (18.9) |
Except where otherwise indicated.
The test–retest reliability was excellent for Configuration 1, as well as for Configuration 2: ICC 0.97, 95% CI: 0.93, 0.98, and ICC 0.97, 95% CI: 0.94, 0.99, respectively, and the SEM and MDC95 for both test protocols were very similar. The results of the relative and absolute test–retest reliability analyses are presented in Table 2.
Table 2.
Measures of Two Protocols for the 6-Minute Walk Test (n=25)
| Protocol (m) |
|||
| Measurement | Configuration 1 (Straight Path) | Configuration 2 (Oval Path) | Compared |
| Trial 1, mean (SD) | 173.3 (70.1) | 160.3 (72.5) | |
| Trial 2, mean (SD) | 193.0 (75.0)* | 166.1 (73.5)* | |
| Test–retest reliability, ICC (95% CI) | 0.97 (0.93, 0.98) | 0.97 (0.94, 0.99) | |
| SEM | 12.6 | 12.5 | |
| MDC95 | 34.8 | 34.7 | |
| Agreement (Bland–Altman plot) | 63.9 | ||
Difference is statistically significant (p<0.001).
ICC=intra-class correlation coefficient; SEM=standard error of measurement; MDC95=minimal detectable change with 95% CI.
The Bland–Altman plot (shown in Figure 1) indicated that the differences between the protocols did not seem to vary in any systematic way over the range of measurements. The plot also demonstrated that the disagreement was of a magnitude such that differences between values would be clinically important (±63.92 m) because this value exceeds the SEM for each test protocol. Overall, the plot indicates that there would be problems interpreting the results between the two test protocols and that they could not be used interchangeably.
Figure 1.
Bland–Altman plot for Configurations 1 and 2 of the 6-minute walk test.
Discussion
This study demonstrated that the two configurations of the 6MWT investigated have excellent relative test–retest reliability and comparable values for absolute test–retest reliability. Quantification of the MDC95 for both test protocols was needed to establish whether the agreement between the protocols was of an acceptable value or would lead to difficulties in interpreting the tests. It was determined that results from each of the test protocols did not agree sufficiently to allow one measure to be used in place of the other; therefore, results from the different configurations could not be directly compared with each other.
It has previously been established that the 6MWT demonstrates excellent test–retest reliability in people with transtibial amputation.9 However, no prior study has examined the reliability of altered configurations of the 6MWT in users of lower extremity prosthetics. The 6MWT distances walked by the participants in this study were shorter than those walked by healthy adults without amputations,29 but they were well within the distances required for community ambulation.30 These distances are thought to be an appropriate measure of functional capacity in community-dwelling people with LEA. The distances reported were also lower than the distances previously reported for those with transtibial amputation of at least 2 years who had been using their current prosthesis for at least 6 months.8,9 However, it is expected that 6MWT distance will continue to improve after the participants are discharged,31 so the distances recorded in this study may not accurately reflect the participants' full ambulatory potential.
A previous study of course configuration in patients with COPD found that they could walk significantly longer distances on oval or circular courses than on straight-path courses but that course length had no impact.18 Differing from these results, the current study found that individuals with LEA walked longer distances on the straight course (Configuration 1) than on the oval one (Configuration 2). There are a couple of reasons that may have caused individuals with an LEA to traverse shorter distances when walking on an oval path. First, the continuous turn of the oval path may have limited their ability to accelerate to and maintain a top speed, as they were able to do on the straight path. Second, as a result of the limitations of artificial ankle joints, a subject walking on a continuous turn may be affected by the eversion, inversion, and torque limitations of the ankle, which may in turn affect socket comfort while walking. However, this would need to be further assessed by investigating the differences in distance walked by individuals with different prosthetic ankles, feet, or both, which is beyond the scope of this study.
In a 2011 study, Resnik and Borgia8 reported the MDC90 for the 6MWT to be 45.0 metres for participants who had been using their prosthesis for 6 months. In the current study, the MDC95 for the 6MWT was calculated to be 34.81 metres for Configuration 1 and 34.70 metres for Configuration 2. An MDC95 should be a more generous value than an MDC90, but both methods of reporting MDC are seen in the literature. The differences in reported MDC values may be due in part to differences in the stage of prosthesis use. The average length of stay in rehabilitation in this study was a mean 32.32 (SD 11.05) days, so participants were still learning to use their prosthesis, compared with individuals who had been using their prosthesis for 6 months.8 Also, Resnik and Borgia8 did not report the configuration of the 6MWT that was used, so no comparisons can be drawn with their results.
Therefore, the current study adds important information about the test properties of the 6MWT for people with LEAs using a prosthesis at discharge from in-patient rehabilitation. This study makes additional novel contributions to the literature on the SEM of 6MWT performance for people with LEAs.
The standardization of the verbal instructions for the testing protocols, and the encouragement given to the participants, is a strength of this study. This standardization allows us to be confident that the differences observed between the configuration protocols are not due to other factors that are known to influence walk test results. Although this was a small study, it identified important considerations for future research with regard to interpreting results and reporting configuration and instructions when using rehabilitation outcome measures.
One limitation of this study can be found in the type of rest we allowed the participants, depending on the gait aid they used. Those using rollators were able to rest in standing or by sitting on the seat, whereas those using other aids were able to rest only in standing. (If they needed to sit, the test was stopped.) Although this was done to mimic a community setting, the variation in resting protocol may have affected the results because some individuals might not have walked for the complete 6 minutes. In future studies, the type of rest permitted across all gait aids should be the same.
A second limitation of the study is that no practice performances were allowed, even though the literature has established that a learning effect is seen in the 6MWT across the first two performances.2,16,32 As noted previously, a learning effect could have accounted, in part, for the larger result seen on the second test day. Future testing with the 6MWT should allow practice sessions to eliminate any questions regarding learning effects.
Conclusions
This study has confirmed that the 6MWT has excellent test–retest reliability for both configuration protocols in the LEA population. It has also established that both configurations have comparable values for absolute test–retest reliability, making novel contributions to the LEA literature regarding MCD95 and the SEM. No previous study has investigated the impact of configuration on the distance walked in the 6MWT in those with LEA. This study has added further evidence that configuration affects the distance walked in the 6MWT: Bland–Altman plots showed that test protocols do not sufficiently agree to allow one to be used in place of the other in this population. This result highlights the importance of explicitly indicating the test configuration for the 6MWT in reporting results to allow for comparability across locations and patients.
Key Messages
What is already known on this topic
It has previously been established that the 6-minute walk test (6MWT) is a measure of functional capacity in the population with lower extremity amputation that has excellent test–retest reliability. However, the configuration of the 6MWT is not always reported, which may be problematic because research in other populations has shown that configuration may affect the distance walked.
What this study adds
This study is the first to report minimum detectable change with a 95% confidence interval values for two configurations of the 6MWT for people with amputations who use a prosthesis. It makes additional novel contributions to the literature regarding the standard error of measurement. The findings also show that results from the different configurations cannot be compared directly with each other; this highlights the importance of reporting configurations in research and when comparing results across patients or rehabilitation programmes.
References
- 1. Deathe AB, Miller WC. The L test of functional mobility: measurement properties of a modified version of the timed “up & go” test designed for people with lower-limb amputations. Phys Ther. 2005;85(7):626–35. Medline:15982169 [PubMed] [Google Scholar]
- 2. Butland RJ, Pang J, Gross ER, et al. Two-, six-, and 12-minute walking tests in respiratory disease. Br Med J (Clin Res Ed). 1982;284(6329):1607–8. Medline:6805625 http://dx.doi.org/10.1136/bmj.284.6329.1607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. American Thoracic Society Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166(1):111–7. Medline:12091180 http://dx.doi.org/10.1164/ajrccm.166.1.at1102 [DOI] [PubMed] [Google Scholar]
- 4. Schoppen T, Boonstra A, Groothoff JW, et al. The timed “up and go” test: reliability and validity in persons with unilateral lower limb amputation. Arch Phys Med Rehabil. 1999;80(7):825–8. Medline:10414769 http://dx.doi.org/10.1016/S0003-9993(99)90234-4 [DOI] [PubMed] [Google Scholar]
- 5. Datta D, Ariyaratnam R, Hilton S. Timed walking test—an all-embracing outcome measure for lower-limb amputees? Clin Rehabil. 1996;10(3):227–32. http://dx.doi.org/10.1177/026921559601000307 [Google Scholar]
- 6. Bellet RN, Adams L, Morris NR. The 6-minute walk test in outpatient cardiac rehabilitation: validity, reliability and responsiveness—a systematic review. Physiotherapy. 2012;98(4):277–86. Medline:23122432 http://dx.doi.org/10.1016/j.physio.2011.11.003 [DOI] [PubMed] [Google Scholar]
- 7. Linberg AA, Roach KE, Campbell SM, et al. Comparison of 6-minute walk test performance between male active duty soldiers and servicemembers with and without traumatic lower-limb loss. J Rehabil Res Dev. 2013;50(7):931–40. Medline:24301430 http://dx.doi.org/10.1682/JRRD.2012.05.0098 [DOI] [PubMed] [Google Scholar]
- 8. Resnik L, Borgia M. Reliability of outcome measures for people with lower-limb amputations: distinguishing true change from statistical error. Phys Ther. 2011;91(4):555–65. Medline:21310896 http://dx.doi.org/10.2522/ptj.20100287 [DOI] [PubMed] [Google Scholar]
- 9. Lin S-J, Bose NH. Six-minute walk test in persons with transtibial amputation. Arch Phys Med Rehabil. 2008;89(12):2354–9. Medline:18976979 http://dx.doi.org/10.1016/j.apmr.2008.05.021 [DOI] [PubMed] [Google Scholar]
- 10. Robinett CS, Vondran MA. Functional ambulation velocity and distance requirements in rural and urban communities. A clinical report. Phys Ther. 1988;68(9):1371–3. http://ptjournal.apta.org/content/68/9/1371.short. Medline:3420171 [DOI] [PubMed] [Google Scholar]
- 11. Guyatt GH, Sullivan MJ, Thompson PJ, et al. The 6-minute walk: a new measure of exercise capacity in patients with chronic heart failure. Can Med Assoc J. 1985;132(8):919–23. Medline:3978515 [PMC free article] [PubMed] [Google Scholar]
- 12. Pilutti LA, Dlugonski D, Sandroff BM, et al. Gait and six-minute walk performance in persons with multiple sclerosis. J Neurol Sci. 2013;334(1–2):72–6. Medline:23962697 http://dx.doi.org/10.1016/j.jns.2013.07.2511 [DOI] [PubMed] [Google Scholar]
- 13. Bartels B, de Groot JF, Terwee CB. The six-minute walk test in chronic pediatric conditions: a systematic review of measurement properties. Phys Ther. 2013;93(4):529–41. Medline:23162042 http://dx.doi.org/10.2522/ptj.20120210 [DOI] [PubMed] [Google Scholar]
- 14. Mossberg KA, Fortini E. Responsiveness and validity of the six-minute walk test in individuals with traumatic brain injury. Phys Ther. 2012;92(5):726–33. Medline:22282772 http://dx.doi.org/10.2522/ptj.20110157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lahiri S, Das PG. Reliability of the six-minute walk test in individuals with transtibial amputation. Indian J Physiother Occup Ther [serial on the Internet]. 2012. [cited 2016 May 25];6(2):100–2. Available from: http://www.indianjournals.com/ijor.aspx?target=ijor:ijpot&volume=6&issue=2&article=024 [Google Scholar]
- 16. Guyatt GH, Pugsley SO, Sullivan MJ, et al. Effect of encouragement on walking test performance. Thorax. 1984;39(11):818–22. Medline:6505988 http://dx.doi.org/10.1136/thx.39.11.818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Wise RA, Brown CD. Minimal clinically important differences in the six-minute walk test and the incremental shuttle walking test. COPD. 2005;2(1):125–9. Medline:17136972 http://dx.doi.org/10.1081/COPD-200050527 [DOI] [PubMed] [Google Scholar]
- 18. Sciurba F, Criner GJ, Lee SM, et al. ; National Emphysema Treatment Trial Research Group. Six-minute walk distance in chronic obstructive pulmonary disease: reproducibility and effect of walking course layout and length. Am J Respir Crit Care Med. 2003;167(11):1522–7. Medline:12615634 http://dx.doi.org/10.1164/rccm.200203-166OC [DOI] [PubMed] [Google Scholar]
- 19. Ng SS, Yu PC, To FP, et al. Effect of walkway length and turning direction on the distance covered in the 6-minute walk test among adults over 50 years of age: a cross-sectional study. Physiotherapy. 2013;99(1):63–70. Medline:23219645 http://dx.doi.org/10.1016/j.physio.2011.11.005 [DOI] [PubMed] [Google Scholar]
- 20. Dunn A, Marsden DL, Nugent E, et al. Protocol variations and six-minute walk test performance in stroke survivors: a systematic review with meta-analysis. . 2015;484813 http://dx.doi.org/10.1155/2015/484813 [DOI] [PMC free article] [PubMed]
- 21. Kosak M, Smith T. Comparison of the 2-, 6-, and 12-minute walk tests in patients with stroke. J Rehabil Res Dev. 2005;42(1):103–7. Medline:15742254 [DOI] [PubMed] [Google Scholar]
- 22. Enright PL. The six-minute walk test. Respir Care. 2003;48(8):783–5. Medline:12890299 [PubMed] [Google Scholar]
- 23. Brooks D, Solway S, Weinacht K, et al. Comparison between an indoor and an outdoor 6-minute walk test among individuals with chronic obstructive pulmonary disease. Arch Phys Med Rehabil. 2003;84(6):873–6. Medline:12808541 http://dx.doi.org/10.1016/S0003-9993(03)00011-X [DOI] [PubMed] [Google Scholar]
- 24. Bruton A, Conway JH, Holgate ST. Reliability: What is it, and how is it measured? Physiotherapy. 2000;86(2):94–9. http://dx.doi.org/10.1016/S0031-9406(05)61211-4 [Google Scholar]
- 25. Streiner DL, Norman GR. Health Measurement scales: a practical guide to their development and use. New York: Oxford University Press; 2003. [Google Scholar]
- 26. Stratford PW. Getting more from the literature: estimating the standard error of measurement from reliability studies. Physiother Can. 2004;56(1):27–30. http://dx.doi.org/10.2310/6640.2004.15377 [Google Scholar]
- 27. Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;327(8476):307–10. Medline:2868172 http://dx.doi.org/10.1016/S0140-6736(86)90837-8 [PubMed] [Google Scholar]
- 28. Walter SD, Eliasziw M, Donner A. Sample size and optimal designs for reliability studies. Stat Med. 1998;17(1):101–10. Medline:9463853 http://dx.doi.org/10.1002/(SICI)1097-0258(19980115)17:1<101::AID-SIM727>3.0.CO;2-E [DOI] [PubMed] [Google Scholar]
- 29. Rasekaba T, Lee AL, Naughton MT, et al. The six-minute walk test: a useful metric for the cardiopulmonary patient. Intern Med J. 2009;39(8):495–501. Medline:19732197 http://dx.doi.org/10.1111/j.1445-5994.2008.01880.x [DOI] [PubMed] [Google Scholar]
- 30. Salbach NM, O'Brien KK, Brooks D, et al. Reference values for standardized tests of walking speed and distance: a systematic review. Gait Posture. 2015;41(2):341–60. Medline:25542397 http://dx.doi.org/10.1016/j.gaitpost.2014.10.002 [DOI] [PubMed] [Google Scholar]
- 31. Czerniecki JM, Turner AP, Williams RM, et al. Mobility changes in individuals with dysvascular amputation from the presurgical period to 12 months postamputation. Arch Phys Med Rehabil. 2012;93(10):1766–73. Medline:22543258 http://dx.doi.org/10.1016/j.apmr.2012.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Mungall IP, Hainsworth R. Assessment of respiratory function in patients with chronic obstructive airways disease. Thorax. 1979;34(2):254–8. Medline:483195 http://dx.doi.org/10.1136/thx.34.2.254 [DOI] [PMC free article] [PubMed] [Google Scholar]