Abstract
Background
Coronary computed tomography angiography (coronary CTA) allows efficient triage of low to intermediate risk patients with suspected acute coronary syndrome (ACS) in the emergency department (ED). Techniques for coronary CTA acquisition in the ED continue to evolve with the establishment of standardized scan protocols and the introduction of newer generations of CT hardware.
Objectives
To evaluate qualitative and quantitative image quality and radiation dose exposure of coronary CTA acquired on 2nd versus 3rd generation dual source CT (DSCT) scanners using a standardized institutional scan protocol designed for the ED.
Methods
A retrospective observational case-control study was performed of 246 ED patients referred to coronary CTA with suspicion of ACS (56.5% male; mean age 53.3 ±11.6 years) between October 2013 and August 2015. 123 consecutive patients were scanned on 3rd generation DSCT, and a cohort of 123 patients matched by age, BMI and heart rate were identified who had undergone 2nd generation DSCT imaging utilizing the same standard clinical protocol. Qualitative and quantitative image quality parameters and radiation exposures were evaluated.
Results
Qualitative image quality was significantly higher using 3rd generation DSCT as compared to 2nd generation (p<0.001). Mean attenuation in the proximal coronary arteries was also significantly higher on 3rd generation DSCT than for 2nd generation (586 HU vs. 426 HU in the left main coronary artery (LM), p<0.001). Signal-to-noise ratio (SNR) and contrast-to-noise ratio (CNR) values, however, were lower in 3rd generation DSCT than 2nd generation (SNR 11.2 [9.9–13.4] vs 13.5 [11.0–15.5] and CNR 12.4 [10.9–14.8] vs 15.2 [12.8–17.9] in the LM, p<0.001). Median effective dose was also lower for 3rd generation DSCT than for 2nd generation (2.9 [2.3–5.0] mSv and 3.7 mSv [2.5–5.7], respectively) although this trend did not reach statistical significance (p=0.065).
Conclusion
Qualitative image quality and mean CT attenuation values of the assessed coronary segments were significantly higher using 3rd generation DSCT. SNR and CNR were lower on 3rd generation DSCT, however this was accompanied by a trend toward lower radiation dose exposure when using the same standard institutional protocol.
Keywords: Coronary CT angiography, Coronary artery disease, Dual source CT, Image quality, Acute coronary syndrome
1. INTRODUCTION
Coronary computed tomography angiography (coronary CTA) has been established in multiple large randomized trials to allow efficient and safe triage of low to intermediate risk patients with suspected acute coronary syndrome (ACS).1–5 The utilization of coronary CTA has increased rapidly in recent years in the emergency department (ED) setting, facilitated by advancements in CT scanner technology.6–8 Dual source CT (DSCT) scanners are equipped with two x-ray tubes and two corresponding detector arrays, improving temporal resolution as compared to single source CT systems and allowing for diagnostic image acquisition of the coronary arteries at higher heart rates.9 Compared to earlier generations, the most recent 3rd generation DSCT scanner features a more powerful generator with higher peak tube current settings, thus enhancing the ability for low kilovoltage scanning with sufficient photon flux in larger patients; per the respective scanner system owner manuals, the 3rd generation DSCT can generate 520 mAs/rot (mAs per rotation) at 70 kVp while the 2nd generation can generate 285 mAs/rot at 70 kVp (SOMATOM Definition Flash or SOMATOM Force; Siemens Healthineers, Forchheim, Germany). In addition, the 3rd generation DSCT has increased z-axis coverage in axial-sequential scan mode (192 simultaneous slices with an option for half-detector-width coverage versus 128 simultaneous slices and no partial-detector width acquisitions), improved temporal and spatial resolution, newer raw data based iterative reconstruction algorithms, and improved detector efficiency. Initial studies have suggested lower radiation dose exposure with 3rd generation DSCT as compared to prior generations in the controlled setting of a research trial.10–12 The increasingly widespread use of clinical coronary CTA has led to technical questions regarding diagnostic image acquisition in patients with a wide spectrum of body mass indices (BMI) and heart rates as well as concerns regarding patient radiation dose exposure in actual clinical practice.13,14
In this study, our aim is to elucidate our standardized clinical protocol for emergency department (ED) coronary CTA based on over 10 years of institutional experience, and to compare quantitative and qualitative image quality and radiation exposure utilizing this standard protocol on 2nd and 3rd generation DSCT systems.
2. METHODS
2.1 Study Design and Patient Selection
A retrospective observational case-control study was performed using a clinical registry of all ED patients undergoing coronary CTA at a single tertiary academic medical center between October 2013 and August 2015 after presenting to the ED with symptoms concerning for ACS. All consecutive patients who underwent coronary CTA on a 3rd generation DSCT installed in the ED between September 2014 and January 2015 were identified; the scanner was only present during these months and subsequently removed due to unrelated technical issues. A cohort of patients matched by age, BMI and heart rate strata were then identified from the clinical registry who underwent coronary CTA on a 2nd generation DSCT scanner between October 2013 and August 2015.
Eligibility criteria were standard for coronary CTA at our institution, and did not exclude patients based on heart rhythm, heart rate, weight, or body mass index.15 Relative contraindications to coronary CTA included known coronary artery disease, prior revascularization, positive serum biomarker levels, ischemic ECG changes, impaired renal function (eGFR<60 mL/min/1.73m2) and prior anaphylactoid reaction to iodinated contrast. If relative contraindications were present, patients were only scanned only after consultation with the cardiology service.
2.2 Clinical coronary CTA scan protocol
Examinations were performed using a second- or third-generation DSCT scanner (SOMATOM Definition Flash or SOMATOM Force; Siemens Healthineers, Forchheim, Germany) using ECG synchronization. A combined automated tube potential selection software (CAREkV, Siemens Healthineers) and automatic tube current selection algorithm (CAREDose 4D, Siemens Healthineers) was utilized using a reference peak tube current of 280 mA and “Vascular” weighting of the automatic algorithm.16 Table 1 describes in detail the clinical scan protocol on each scanner, which were identical from the perspective of protocol building. Breast displacement was performed in all females using the bed positioning strap as per department policy, in a method previously published.17 Clinical criteria for exclusion included impaired renal function, allergy to iodinated contrast media, and inability to lie flat and breath-hold for 10 seconds. All heart rates and rhythms were accepted for scanning, provided patients were hemodynamically stable. Beta-blocker administration was not standard in the CT suite, but occasionally occurred on the ward at the discretion of the referring clinical team or by supervising physician’s choice in the CT suite early in our experience.
Table 1.
Clinical coronary CTA scan protocol on 2nd and 3rd generation DSCT
| 2nd generation DSCT | 3rd generation DSCT | |
|---|---|---|
| Topogram – Lateral and PA | ||
| Tube voltage/tube current | 120 kVp/30 mA | 120 kVp/30 mA |
| Noncontrast scan for calcium scoring and range planning | ||
| Tube voltage | 120 kV (fixed) | 120 kV (fixed) |
| Tube current | reference mA 80 (CareDose 4D enabled) | reference mA 80 (CareDose 4D enabled) |
| Triggering/gating | Prospectively ECG-triggered axial-sequential, single phase at absolute delay of 280 msec | Prospectively ECG-triggered axial-sequential, single phase at absolute delay of 280 msec |
| Kernel | Filtered back projection B35f | Filtered back projection Qr36 |
| Rotation time | 0.28 sec | 0.25 sec |
| Coronary CTA | ||
| Tube voltage | reference kV 120 (Care kV enabled) | reference kV 120 (Care kV enabled) |
| Tube current | reference mA 280 (CareDose 4D enabled) | reference mA 280 (CareDose 4D enabled) |
| ECG synchronization | ||
| Prospectively ECG triggered (heart rate < approximately 75 beats per min or arrhythmia) |
|
|
| Retrospectively ECG gated (heart rate > approximately 75 beats per min and regular; or difficulty breath holding) |
|
|
| Tube current modulation |
|
|
| Contrast timing | Isovue 370, bolus timing method with 20cc test bolus | Isovue 370, bolus timing method with 20cc test bolus |
| Contrast injection | Power injector with mixed contrast injection weight-based software | Power injector with mixed contrast injection weight-based software |
| Kernel/Data Reconstruction | I131F SAFIRE strength 3 (out of 5) | Bv40 ADMIRE strength 3 (out of 5) |
| Rotation time | 0.28 sec | 0.25 sec |
| Slice thickness | 0.6 mm | 0.6 mm |
| Slice increment | 0.3 mm | 0.3 mm |
Scan acquisitions were performed during a single end-inspiratory breath-hold with scan range from the level of the carina to the diaphragm. Non-contrast coronary calcium scan was obtained in all patients and contrast-enhanced scans were performed regardless of coronary calcium burden. Unless contraindicated, 600 mcg of sublingual nitroglycerin was administered by the supervising physician to all patients at least 5 minutes prior to the contrast-enhanced scan. A 20 cc test bolus of iopamidol 370 g/cm3 (Isovue 370; Bracco Diagnostics, Princeton, NJ, USA) was used to determine contrast bolus timing via a region of interest placed on the ascending aorta. A power injector with mixed contrast injection weight-based software was utilized for the diagnostic contrast injection (Certegra/P3T and Stellant, MedRad, Indianola, PA). In patients with heart rates below approximately 75 beats/min or arrhythmias including atrial fibrillation, prospectively ECG-triggered axial-sequential scans with arrhythmia rejection (Adaptive Cardio Sequential, Siemens) were acquired with peak tube current in systole (200–440ms) and pulsed tube current in a widened acquisition window (200–950ms). Alternatively, in patients with regular heart rates above approximately 75 beats/min, or in patients who were unable to reliably breath hold, retrospectively ECG-gated helical acquisition was available in order to shorten acquisition time with peak tube current in systole (200–440ms) and aggressive tube current modulation (MinDose, Siemens Healthcare) in the remainder of the R-R interval. All scans were supervised by a physician with subspecialty training in cardiovascular imaging.
2.3 Image Reconstruction
2nd generation DSCT coronary CTA images were reconstructed with SAFIRE strength 3 (Sinogram Affirmed Iterative Reconstruction, Siemens Healthineers) and 3rd generation DSCT images were reconstructed with ADMIRE strength 3 (Advanced Modeled Iterative Reconstruction, Siemens Healthineers).18,19 Diagnostic coronary CTA images were reconstructed with 0.75mm slice thickness at 0.4mm increments using a medium-smooth dedicated heart kernel (I31F kernel on the 2nd generation scanner and Bv40d kernel on the 3rd generation) in the available phase of the R-R interval demonstrating the least motion artifact. Multiphase images were reconstructed with 1.5mm slice thickness at 1.5mm increments using 50 msec intervals for the prospectively ECG-triggered scans throughout the imaged portion of the cardiac cycle and at 5% intervals for the retrospectively ECG-gated scans throughout the entire R-R interval, thus allowing for evaluation of ventricular function at the time of interpretation in all patients. Additional multiphase images were reconstructed at 20 msec intervals through systole (defined as 200–440 msec) to allow for selection of the phase with least motion artifact.20 Radiation dose was recorded as dose length product (mGy-cm) and effective dose (mSv) utilizing a conversion factor of 0.014.21
2.4 Image Quality Analysis
Two cardiac imaging fellows, each with two years of experience and dedicated training in coronary CTA, evaluated qualitative and quantitative image quality independently blinded to scanner type. All images were analyzed on a dedicated CT workstation (Aquarius version 4.4.8, TeraRecon Inc., San Mateo, CA, USA).
Qualitative image quality of the diagnostic phase axial coronary CTA images was evaluated by these two readers using a 4-point Likert scale (3: very good image quality, no artifacts; 2: fully diagnostic image quality, minor artifacts; 1: poor image quality; severe artifacts; 0: nondiagnostic segment) for each coronary artery segment. An 18-segment coronary artery tree was evaluated, according to previously described methods.22–24 Discrepancies in visual scores were resolved in a consensus read by a third observer, a subspecialty trained cardiovascular radiologist with 3 years experience.
Quantitative image quality was evaluated according to previously described methods, with circular regions of interest (ROIs) drawn in the arteries and adjacent perivascular fat to measure mean attenuation values on axial images, avoiding plaque and obvious motion artifact.20 Measurements were performed in the left main (LM), proximal right coronary artery (RCA) and distal left anterior descending artery (LAD). Based on coronary dominance, measurement was also performed in either the distal RCA or distal left circumflex artery (LCx) at 8 cm from the coronary ostium; in patients with a co-dominant circulation, the distal RCA was measured. Mean image noise was defined as the standard deviation (SD) of the CT attenuation of the aortic lumen at the level of the LM ostium. Signal-to-noise ratio (SNR) was calculated for all assessed segments dividing the mean attenuation value of the given ROI by the image noise. Contrast-to-noise ratio (CNR) was calculated as the difference of the mean attenuation of the coronary lumen and pericoronary adipose tissue, divided by the image noise.
2.5 Statistical analysis
Continuous variables were expressed as mean ± standard deviation (SD) or median with interquartile range based on normality. Categorical variables were expressed as percentage and were compared using the chi2 test. Image quality parameters (image noise, SNR, CNR) between the 2 scanner systems were compared by using Mann-Whitney tests. Inter-observer reproducibility of quantitative measurements was calculated using intraclass correlation coefficients (ICC). P<0.05 was considered statistically significant. Statistical analysis was performed using SPSS (IBM Corp, version 22.0, Armonk, NY, USA).
3. RESULTS
3.1 Study population
All 123 consecutive patients scanned on 3rd generation DSCT while it was installed in the ED between 9/2014 – 1/2015 were included. 123 matched patients were identified who were scanned on a 2nd generation DSCT scanner between 2013 and 2015. Datasets from a total of 246 patients were evaluated. The patients were 57% male with mean age 53.3±11.6 years and median BMI 28.0 [24.5–31.0] kg/m2 (Table 1). Heart rate in the 2nd generation DSCT group was 73.8±14.2 beats per minute and in the 3rd generation DSCT group was 74.1±14.2 beats per minute, which was not a statistically significant difference. Of the 123 patients scanned on the 2nd generation DSCT, 60 were scanned prior to September 2014 and of this group, 28 (23%) were administered beta-blockers; no 3rd generation DSCT patients were administered beta-blockers. Nitroglycerin was administered to 120 (98%) of the patients scanned on the 2nd generation DSCT and 119 (97%) of the patients scanned on the 3rd generation DSCT.
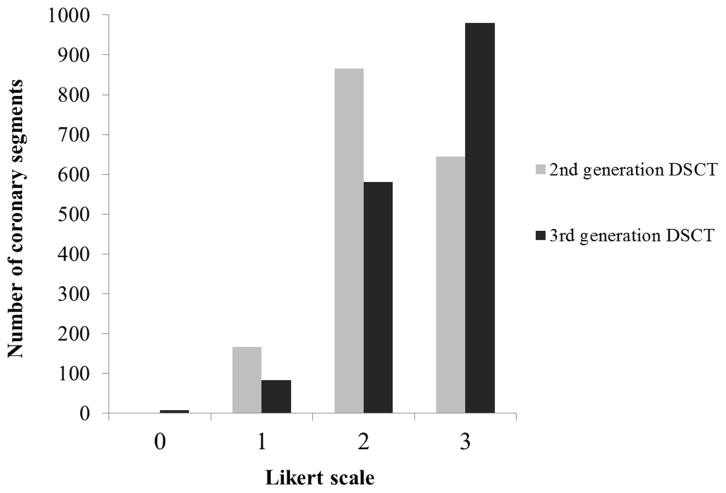
3.2 Image Quality
Qualitative image quality was significantly higher with 3rd generation DSCT as compared to 2nd generation, (2.5 ± 0.6 vs. 2.3 ± 0.6 points on Likert scale, p<0.001). (Fig. 3). Out of 3446 total assessed coronary segments, 249 (7%) were identified with significantly limited image quality (1 on Likert scale) and 9 (0.3%) were identified with nondiagnostic quality (0 on Likert scale). Of the 258 total segments graded as significantly limited or nondiagnostic quality, 91 (35%) were from scans on the 3rd generation DSCT and 167 (65%) were from scans on the 2nd generation DSCT. Mean attenuation, SNR and CNR values are summarized in Table 3. Mean CT attenuation in the left main and proximal right coronary artery were significantly higher on 3rd generation DSCT as compared to 2nd generation (p<0.001). 2nd generation DSCT yielded significantly lower image noise by quantitative assessment as compared to 3rd generation (31.9 HU vs. 55.9 HU, respectively, p<0.001). SNR and CNR values of both proximal and distal coronary segments were significantly higher on 2nd generation DSCT as compared to 3rd generation (p<0.001).
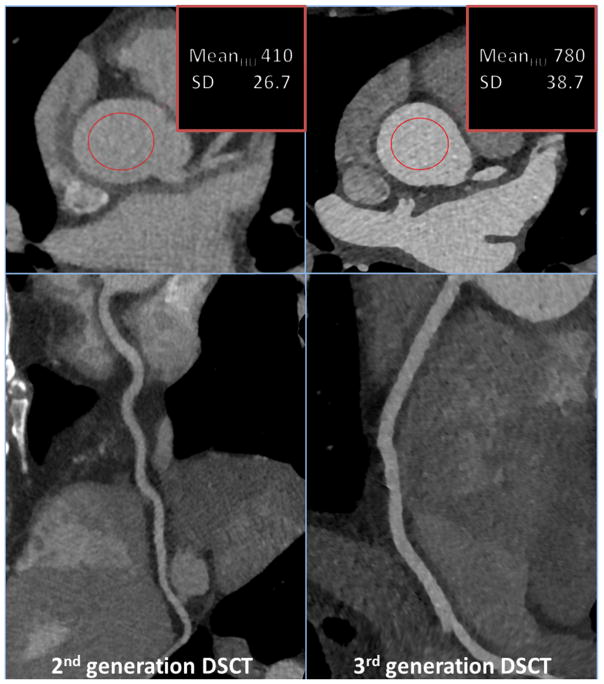
Fig 3.
Representative clinical cases of quantitative image noise measurements. Images from patients matched by body mass index and heart rate demonstrate higher attenuation accompanied by higher noise (SD) using 3rd generation DSCT. Novel image reconstruction algorithm (ADMIRE) provides sharp contours for the evaluation of the lumen and vessel structure on visual assessment. Applied tube voltage was 100 kV for both images.
Table 3.
Scan parameters and dose estimates
| Scan parameters and dose estimates | Total | 2nd generation DSCT | 3rd generation DSCT | p value |
|---|---|---|---|---|
| (N=246) | (N=123) | (N=123) | ||
| Tube voltage, n (%) | <0.001 | |||
| 70 kV | 52 (21.1) | - | 52 (42.3) | |
| 80 kV | 48 (19.5) | 30 (24.4) | 18 (14.6) | |
| 90 kV | 15 (6.1) | - | 15 (12.2) | |
| 100 kV | 82 (33.3) | 60 (48.8) | 22 (17.9) | |
| 110 kV | 3 (1.2) | - | 3 (2.4) | |
| 120 kV | 43 (17.5) | 30 (24.4) | 13 (10.6) | |
| 140 kV | 3 (1.2) | 3 (2.4) | - | |
| Tube current (mAs) (mean [range]) | 196.5 [160.8–265.3] | 174.0 [140.5–214.0] | 239.0 [179.8–279.0] | <0.001 |
| Contrast agent (ml) | 101.0 [92.0–107.3] | 101.0 [93.0–110.0] | 101.0 [91.0–106.0] | 0.618 |
| Gating, n (%) | <0.001 | |||
| Prospective | 217 (88.2) | 96 (78.0) | 121 (98.4) | |
| Retrospective | 29 (11.8) | 27 (22.0) | 2 (1.6) | |
| DLP (mGy*cm) | 242.5 [169.0–376.5] | 264.0 [176.0–406.0] | 210.0 [164.0–356.0] | 0.065 |
| Effective dose (mSv) (mean [range]) | 3.4 [2.4–5.2] | 3.7 [2.5–5.7] | 2.9 [2.3–5.0] | 0.064 |
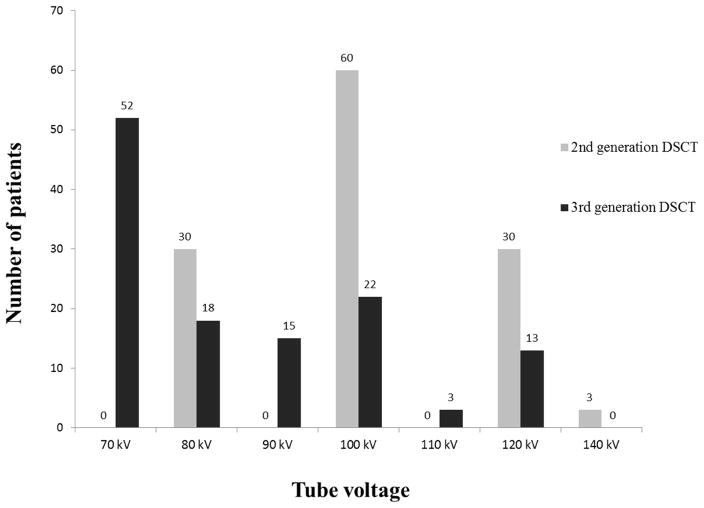
3.3 Radiation dose
Median effective dose was 3.7 mSv [2.5–5.7] for 2nd generation DSCT and 2.9 mSv [2.3–5.0] for 3rd generation DSCT. Although the trend was for lower median effective dose with 3rd generation DSCT, this difference was not statistically significant (p=0.065). No difference was found in the dosage of contrast media between the two cohorts (p=0.384). The majority of patients were scanned using prospectively ECG-triggered axial-sequential technique on both 2nd and 3rd generation scanners, although there was a significant trend towards higher use of prospective ECG-triggering on the 3rd generation scanner vs. the 2nd generation (98.4% and 78.0%, respectively, p<0.001). Mean tube voltage was significantly lower for 3rd generation DSCT scanner as compared to 2nd generation DSCT (85.5 kV vs. 101.0, respectively p<0.001).
3.4 Reproducibility
Inter-observer reproducibility of quantitative image quality was evaluated based on 20 patients and was excellent between the two readers for all assessed coronary segments (ICC 0.615–0.988).
4. DISCUSSION
In this study we evaluated our clinical experience with coronary CTA in the ED to compare quantitative and qualitative image quality as well as radiation exposure on 2nd and 3rd generation DSCT. Overall, utilizing a standardized institutional protocol imaging targeted to end-systole for both prospectively ECG-triggered and retrospectively ECG-gated acquisitions allowed for consistently high diagnostic-quality imaging of ED patients on both scanner generations. Of note, scan acquisitions remained of high diagnostic quality regardless of heart rate and rhythm with low rates of beta-blocker administration, which in clinical practice increased patient throughput. In addition, radiation dose utilizing this standard protocol was significantly lower than values from previous large published trials, even with the addition of a widened acquisition window for prospectively ECG-triggered scans to allow for ventricular function analysis in all patients.
Mean vessel attenuation values were higher on 3rd generation DSCT, likely because scanner ability to generate higher tube current at lower tube potentials as well as improved detector efficiency led to imaging at lower tube voltages (kV).13 Low kV imaging increases contrast conspicuity due to the photoelectric effect when imaging with a spectrum centered closer to the k-edge of iodine, resulting in higher attenuation values, which tends to the contrast-to-noise ratio, despite overall higher image noise. Qualitative image quality based on segmental analysis was also higher on 3rd generation DSCT, presumably due to improved temporal resolution secondary to increased gantry rotation speed resulting in reduced motion artifact, as well as improved CNR. Additionally, the larger z-axis coverage yields fewer potential slab-to-slab misregistration and banding artifacts. Quantitative image quality as measured by SNR was lower on 3rd generation DSCT compared to 2nd generation, as was CNR, secondary to an increase in quantitative image noise. Our experience, however, was that advancements in iterative reconstruction software algorithms rendered this decrease in absolute CNR and SNR values nearly indiscernible to the reader, perhaps aided by the decrease in motion artifacts (Figures 3–7).
Fig 7.
Example clinical cases demonstrating representative image quality on the 3rd generation DSCT (above) and 2nd generation DSCT (below) on patients with similar BMI. Curved planar reformat images demonstrate partially calcified plaque resulting in moderate luminal narrowing of the left anterior descending coronary artery (right, white arrows). A shallow myocardial bridge is also present in the lower image which should not be mistaken for atherosclerotic disease (right, gray arrow).
Although CNR and SNR were lower on 3rd generation DSCT, there was an expected concomitant trend toward decreased radiation exposure. Given that the images remained of high diagnostic quality, the decreased quantitative image quality values were deemed as an acceptable clinical tradeoff for decreased radiation exposure. The increased use of low tube voltage scanning at 70 kVp on the 3rd generation DSCT likely contributed to the lower radiation dose trend, facilitated by the ability to generate a maximum of 520 mAs per rotation rather than 285 mAs per rotation for the 2nd generation DSCT. While 70 kVp scanning is possible on the 2nd generation DSCT, this has never been utilized clinically in adults at our institution due to the low maximum mAs achievable and resultant unacceptable image noise.
A proportion of the lower radiation dose trend in 3rd generation DSCT in our cohort may also be attributed to higher utilization of prospectively ECG-triggered acquisition, despite matched heart rates in both groups.25 The increase in utilization was likely due to increased supervising physician confidence over time in this mode of acquisition at “borderline” heart rates near 75 beats per minute. This increase in confidence is thought to be due to increasing familiarity with the prospectively ECG-triggered institutional protocol as well as increasing knowledge of the superior temporal resolution and detector array width of the 3rd generation DSCT, both of which manifest as lower overall CTA acquisition time thereby improving bolus geometry and leading to better coronary enhancement. The decrease in radiation dose with prospectively ECG-triggered acquisitions on the 3rd generation DSCT was likely amplified by shortened acquisition durations due to improved z-axis coverage, as well as avoiding the susceptibility of retrospectively ECG gated exams to radiation dose increases due to pitch and ECG-based tube current variability in the face of arrhythmia.
4.1 Limitations
All results are from a single site and are therefore site-specific. Given the clear nature of our standardized protocol, however, the results remain relevant to other sites who could adopt similar protocols with either of these scanner technologies. Another limitation is that early on in the adoption process for the standardized protocol, multiple considerations may have affected physician choice of acquisition mode in borderline heart rate cases near the prescribed cutoff of 75 beats per minute including arrhythmia and breath-holding capacity. Earlier on in our experience, in order to provide the best patient care based on understanding of scanner technology at the time, the acquiring physician may have been more likely to choose retrospectively ECG-gated acquisition at these borderline heart rates; this tendency is likely reflected in the increased rates of prospective acquisition on the 3rd generation DSCT. Overall, a minority of cases was scanned with retrospectively ECG-gated acquisition on both scanners: 22 (15%) for the 2nd generation DSCT and 2 (1%) for the 3rd generation DSCT.
All images were reconstructed with iterative reconstruction at the time of the clinical scan due to the superior image quality as compared to filtered back projection. As the raw data was not stored on the scanners, images cannot retrospectively be reconstructed with filtered back projection for further analysis of image quality removing the variation inherent in different iterative reconstruction algorithms. The same automated tube potential/current selection algorithm was used for both scanners as described, however any changes that may have been made to the algorithm between scanners are unaccounted for as they are proprietary to the vendor and not made available to the scanner user. Lastly, many important areas of future research remain regarding clinical outcomes after coronary CTA including effects on downstream testing; for reference, initial results on additional testing in this clinical coronary CTA registry have recently been published.15
5. CONCLUSION
Excellent image quality with low radiation exposure was obtained on both generations of DSCT utilizing our institutional protocol. Potential exists for greater radiation dose and contrast reduction in the future with more consistent use of low tube voltage imaging and prospectively ECG-triggered acquisition as clinician familiarity with these concepts continues to grow.
Fig 1.
Tube potential settings by DSCT generation used in study cohort of clinical coronary CTA. Data acquisition with 70 kV provides increased contrast conspicuity due to the photoelectric effect when imaging closer to the k-edge of iodine on 3rd generation DSCT.
Fig 2.
Qualitative image quality assessment demonstrated higher scores for 3rd generation DSCT: 2.3 ± 0.6 for 2nd generation vs. 2.5 ± 0.6 for 3rd generation DSCT (p<0.001).
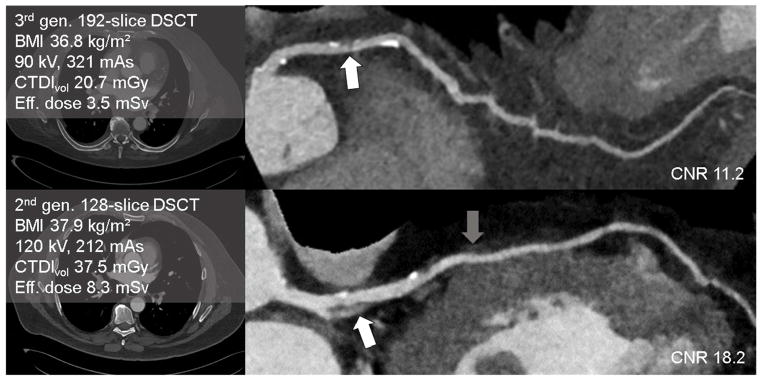
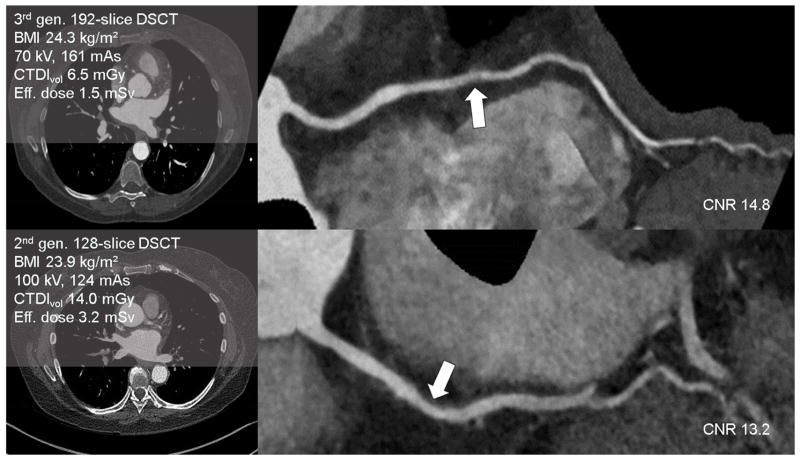
Fig 4.
Example clinical cases of quantitative contrast-to-noise ratio measurements demonstrating representative image quality on the 3rd generation DSCT (above) and 2nd generation DSCT (below) on patients with similar BMI. Curved planar reformat images demonstrate noncalcified plaque resulting in mild stenosis of the right coronary artery (right, arrows).
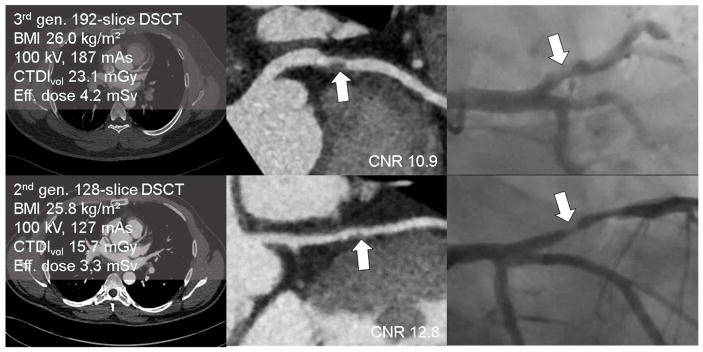
Fig 5.
Example clinical cases demonstrating representative image quality on the 3rd generation DSCT (above) and 2nd generation DSCT (below) on patients with similar BMI. Curved planar reformat images demonstrate partially calcified plaque resulting in severe stenoses of the left anterior descending coronary artery (center, arrows) confirmed by invasive coronary angiography (right, arrows).
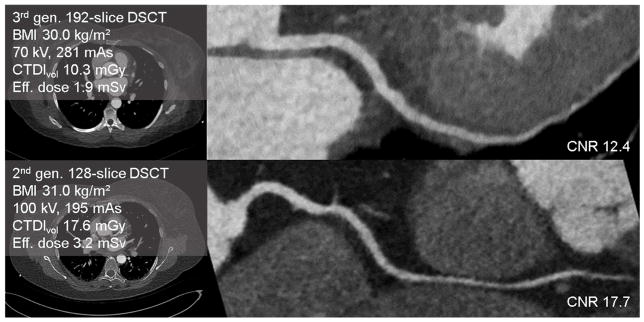
Fig 6.
Example clinical cases demonstrating representative image quality on the 3rd generation DSCT (above) and 2nd generation DSCT (below) on patients with similar BMI. Curved planar reformat images demonstrate no plaque in the right coronary artery.
Table 2.
Patient characteristics
| Patient characteristics | Total | 2nd generation DSCT | 3rd generation DSCT | p value |
|---|---|---|---|---|
| (N=246) | (N=123) | (N=123) | ||
| Age (years) | 53.3 ± 11.6 | 53.0 ± 10.6 | 53.5 ± 12.5 | 0.762 |
| BMI (kg/m2) | 28.0 [24.5–31.0] | 27.9 [24.6–31.6] | 28.0 [24.3–30.6] | 0.764 |
| Male gender, n (%) | 139 (57) | 74 (60) | 65 (53) | 0.247 |
| Heart rate (beats/min) [Min-Max] | 73.9 ± 14.1 [48–119] | 73.8 ± 14.2 [49–119] | 74.1 ± 14.2 [48–116] | 0.929 |
| Sinus rhythm, n (%) | 246 (98) | 118 (96) | 122 (99) | 0.213 |
| Nitroglycerin administration, n (%) | 239 (97) | 120 (98) | 119 (97) | - |
| Beta-blocker administration, n (%) | 28 (11) | 28 (23) | 0 (0) | - |
Data are presented as mean ± SD or median and IQR.
Table 4.
Comparative quantitative image quality of 2nd and 3rd generation DSCT.
| 2nd generation DSCT (N=123) | 3rd generation DSCT (N=123) | p-value | |
|---|---|---|---|
| Image noise (HU) | 31.9 [27.0–42.4] | 55.9 [46.6–61.4] | <0.001 |
| pRCA signal (HU) | 431.0 [350.0–547.0] | 599.0 [441.0–726.0] | <0.001 |
| pRCA SNR | 13.3 [11.0–15.8] | 10.9 [9.5–12.6] | <0.001 |
| pRCA CNR | 15.2 [13.2–18.3] | 12.5 [11.1–14.3] | <0.001 |
| LM signal (HU) | 426.0 [362.0–535.0] | 586.0 [465.0–764.0] | <0.001 |
| LM SNR | 13.5 [11.0–15.5] | 11.2 [9.9–13.4] | <0.001 |
| LM CNR | 15.2 [12.8–17.9] | 12.4 [10.9–14.8] | <0.001 |
| Distal LAD SNR | 10.7 [8.7–13.1] | 8.8 [7.2–10.6] | <0.001 |
| Distal RCA/LCX SNR | 12.0 [9.9–14.9] | 10.7 [8.6–12.7] | <0.001 |
Acknowledgments
Nandini M. Meyersohn MD was supported by the NIH Heart, Lung, and Blood Institute T32 grant number HL076136.
Abbreviations
- Coronary CTA
Coronary computed tomography angiography
- ED
Emergency department
- ACS
Acute coronary syndrome
- DSCT
Dual source computed tomography
- FBP
Filtered back projection
- HU
Hounsfield units
- SNR
Signal-to-noise ratio
- CNR
Contrast-to-noise ratio
- LM
Left main coronary artery
- LAD
Left anterior descending coronary artery
- LCx
Left circumflex coronary artery
- RCA
Right coronary artery
Footnotes
Conflicts of Interest: The authors report no conflicts of interest (disclosure forms attached).
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Litt HI, et al. CT angiography for safe discharge of patients with possible acute coronary syndromes. N Engl J Med. 2012;366(15):1393–403. doi: 10.1056/NEJMoa1201163. [DOI] [PubMed] [Google Scholar]
- 2.Hoffmann U, et al. Coronary CT angiography versus standard evaluation in acute chest pain. N Engl J Med. 2012;367(4):299–308. doi: 10.1056/NEJMoa1201161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goldstein JA, et al. The CT-STAT (Coronary Computed Tomographic Angiography for Systematic Triage of Acute Chest Pain Patients to Treatment) trial. J Am Coll Cardiol. 2011;58(14):1414–22. doi: 10.1016/j.jacc.2011.03.068. [DOI] [PubMed] [Google Scholar]
- 4.Bittencourt MS, et al. Prognostic value of nonobstructive and obstructive coronary artery disease detected by coronary computed tomography angiography to identify cardiovascular events. Circ Cardiovasc Imaging. 2014;7(2):282–91. doi: 10.1161/CIRCIMAGING.113.001047. [DOI] [PubMed] [Google Scholar]
- 5.Rubinshtein R, et al. Usefulness of 64-slice cardiac computed tomographic angiography for diagnosing acute coronary syndromes and predicting clinical outcome in emergency department patients with chest pain of uncertain origin. Circulation. 2007;115(13):1762–8. doi: 10.1161/CIRCULATIONAHA.106.618389. [DOI] [PubMed] [Google Scholar]
- 6.Galperin-Aizenberg M, et al. Cardiac CT angiography in the emergency department. AJR Am J Roentgenol. 2015;204(3):463–74. doi: 10.2214/AJR.14.12657. [DOI] [PubMed] [Google Scholar]
- 7.Raff GL, et al. SCCT guidelines on the use of coronary computed tomographic angiography for patients presenting with acute chest pain to the emergency department: a report of the Society of Cardiovascular Computed Tomography Guidelines Committee. J Cardiovasc Comput Tomogr. 2014;8(4):254–71. doi: 10.1016/j.jcct.2014.06.002. [DOI] [PubMed] [Google Scholar]
- 8.Cury RC, et al. Triage of patients presenting with chest pain to the emergency department: implementation of coronary CT angiography in a large urban health care system. AJR Am J Roentgenol. 2013;200(1):57–65. doi: 10.2214/AJR.12.8808. [DOI] [PubMed] [Google Scholar]
- 9.Hell MM, et al. Prospectively ECG-triggered high-pitch coronary angiography with third-generation dual-source CT at 70 kVp tube voltage: feasibility, image quality, radiation dose, and effect of iterative reconstruction. J Cardiovasc Comput Tomogr. 2014;8(6):418–25. doi: 10.1016/j.jcct.2014.09.003. [DOI] [PubMed] [Google Scholar]
- 10.Meyer M, et al. Closing in on the K Edge: Coronary CT Angiography at 100, 80, and 70 kV—Initial Comparison of a Second- versus a Third-Generation Dual-Source CT System. Radiology. 2014;273(2):373–382. doi: 10.1148/radiol.14140244. [DOI] [PubMed] [Google Scholar]
- 11.Meinel FG, et al. Image quality and radiation dose of low tube voltage 3rd generation dual-source coronary CT angiography in obese patients: a phantom study. Eur Radiol. 2014;24(7):1643–50. doi: 10.1007/s00330-014-3194-x. [DOI] [PubMed] [Google Scholar]
- 12.Mangold S, et al. Automated tube voltage selection for radiation dose and contrast medium reduction at coronary CT angiography using 3rd generation dual-source CT. Eur Radiol. 2016 doi: 10.1007/s00330-015-4191-4. (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 13.Einstein AJ. Effects of radiation exposure from cardiac imaging: how good are the data? J Am Coll Cardiol. 2012;59(6):553–65. doi: 10.1016/j.jacc.2011.08.079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cook TS, Galperin-Aizenberg M, Litt HI. Coronary and cardiac computed tomography in the emergency room: current status and future directions. J Thorac Imaging. 2013;28(4):204–16. doi: 10.1097/RTI.0b013e3182956bbf. [DOI] [PubMed] [Google Scholar]
- 15.Ghoshhajra BB, et al. Clinical Implementation of an Emergency Department Coronary Computed Tomographic Angiography Protocol for Triage of Patients with Suspected Acute Coronary Syndrome. Eur Radiol. doi: 10.1007/s00330-016-4562-5. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ghoshhajra BB, et al. Cardiac computed tomography angiography with automatic tube potential selection: effects on radiation dose and image quality. J Thorac Imaging. 2013;28(1):40–8. doi: 10.1097/RTI.0b013e3182631e8a. [DOI] [PubMed] [Google Scholar]
- 17.Vadvala H, et al. Coronary CTA using scout-based automated tube potential and current selection algorithm, with breast displacement results in lower radiation exposure in females compared to males. Cardiovasc Diagn Ther. 2014;4(6):470–9. doi: 10.3978/j.issn.2223-3652.2014.12.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yin WH, et al. Iterative reconstruction to preserve image quality and diagnostic accuracy at reduced radiation dose in coronary CT angiography: an intraindividual comparison. JACC Cardiovasc Imaging. 2013;6(12):1239–49. doi: 10.1016/j.jcmg.2013.08.008. [DOI] [PubMed] [Google Scholar]
- 19.Layritz C, et al. Accuracy of prospectively ECG-triggered very low-dose coronary dual-source CT angiography using iterative reconstruction for the detection of coronary artery stenosis: comparison with invasive catheterization. Eur Heart J Cardiovasc Imaging. 2014;15(11):1238–45. doi: 10.1093/ehjci/jeu113. [DOI] [PubMed] [Google Scholar]
- 20.Celeng C, et al. Defining the optimal systolic phase targets using absolute delay time for reconstructions in dual-source coronary CT angiography. Int J Cardiovasc Imaging. 2016;32(1):91–100. doi: 10.1007/s10554-015-0755-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.The 2007 Recommendations of the International Commission on Radiological Protection. ICRP publication 103. Ann ICRP. 2007;37(2–4):1–332. doi: 10.1016/j.icrp.2007.10.003. [DOI] [PubMed] [Google Scholar]
- 22.Achenbach S, et al. Comparison of image quality in contrast-enhanced coronary-artery visualization by electron beam tomography and retrospectively electrocardiogram-gated multislice spiral computed tomography. Invest Radiol. 2003;38(2):119–28. doi: 10.1097/00004424-200302000-00007. [DOI] [PubMed] [Google Scholar]
- 23.Bittencourt MS, et al. Iterative reconstruction in image space (IRIS) in cardiac computed tomography: initial experience. Int J Cardiovasc Imaging. 2011;27(7):1081–7. doi: 10.1007/s10554-010-9756-3. [DOI] [PubMed] [Google Scholar]
- 24.Commission., E. European guidelines on quality criteria for computed tomography. Luxembourg: European Commission; 1998. [Google Scholar]
- 25.Stolzmann P, et al. Dual-source CT in step-and-shoot mode: noninvasive coronary angiography with low radiation dose. Radiology. 2008;249(1):71–80. doi: 10.1148/radiol.2483072032. [DOI] [PubMed] [Google Scholar]