Abstract
The objective of this study was to describe a multilevel conceptual framework to understand the role of food insecurity on antiretroviral therapy adherence. The authors illustrated an example of how they used the multilevel framework to develop an intervention for poor people living with HIV in a rural and low-resource community. The framework incorporates intra-personal, interpersonal, and structural-level theories of understanding and changing health behaviors. The framework recognizes the role of personal, social, and environmental factors on cognition and behavior, with particular attention to ways in which treatment adherence is enabled or prevented by structural conditions, such as food insecurity.
Keywords: Food insecurity, antiretroviral therapy adherence, HIV, theory, intrapersonal, interpersonal, structural
Food insecurity and HIV/AIDS remain global, social, and public health challenges. The reciprocal relationship between food insecurity and HIV/AIDS has been well documented in the literature (Gillespie & Kadiyala, 2005; Weiser et al., 2011). On the one hand, food insecurity increases risk of HIV (Rollins, 2007; Weiser et al., 2011) and elevates risk of adverse outcomes among people living with HIV (PLHIV; de Pee & Semba, 2010; Kadiyala & Rawat, 2013; Rawat, McCoy, & Kadiyala, 2013). On the other hand, HIV heightens vulnerability to food insecurity by limiting household income and food production (de Waal & Whiteside, 2003; Donovan & Massingue, 2007; Larson et al., 2013). Additionally, expansion of access to antiretroviral therapy (ART), particularly in low-resource countries, has exacerbated the relationship between food insecurity and HIV/AIDS. A growing body of literature has shown that food insecurity acts as a barrier to ART adherence (Singer, Weiser, & McCoy, 2015; Young, Wheeler, McCoy, & Weiser, 2014). Evidence indicates that food-insecure PLHIV are more likely to miss or skip taking their medications as prescribed by their healthcare providers (Hong et al., 2014; Musumari et al., 2014; Sanjobo, Frich, & Fretheim, 2008; Weiser et al., 2014). In turn, the compounded effect of food insecurity and nonadherence to ART elevates the risk of adverse health outcomes, including mortality (Chi et al., 2009; Koethe et al., 2013; Rawat et al., 2013; Stringer et al., 2006).
Although prior studies have described how and why food insecurity affects adherence (Kalofonos, 2010; Musumari et al., 2013; Weiser et al., 2010; Young et al., 2014), fewer studies have explained the relationship using a multilevel conceptual framework that takes into account individual and structural factors. In turn, this conceptual framework may guide development of more holistic and appropriate programs that tackle underlying predictors and mediating factors that heighten risk of nonadherence among ART patients who are food insecure in low-resource settings. Accordingly, the objective of this article is threefold: (1) to describe a multilevel conceptual framework (that is referred to as “framework”), which is based on theories that explain human behavior at the individual, interpersonal, and societal or structural level; (2) to expand our understanding of the association between food insecurity and ART adherence; and (3) to illustrate how the framework can inform development of a holistic program designed to increase food security and ART adherence among PLHIV in low-resource communities. This article proceeds as follows. First, we clarify the definition of food insecurity and ART adherence that we used in conceptualizing the framework. Second, we identify four theories that explain the relationship between food insecurity and ART adherence. In addition, we describe an adaptation of an integrated treatment adherence model that encapsulates key propositions from the four theories. Third, we propose a multilevel conceptual framework informed by the four behavioral theories and the integrated adherence model. Fourth, we illustrate how the framework can be translated into practice by informing program development. We provide an example of an existing program designed to improve access to food and ART adherence in a low-resource community in eastern Zambia. Lastly, we discuss the framework and its implications for social work practice.
Definition of food insecurity and antiretroviral therapy adherence
Food insecurity
The definition of food insecurity has seen significant changes, including the shift to individual and household experiences of food insecurity and use of objective indicators and subjective perception of food insecurity (Maxwell, 1996). Consistent with these changes, we define food insecurity as the inability of individuals and households to access and maintain at all times adequate, safe, and nutritious food that meet dietary needs (Food and Agriculture Organization of the United Nations, 1996). We focused on access to food because access is more closely associated with social and economic status compared to other dimensions such as availability and utilization (Barrett, 2010; Sen, 1981). Additionally, access reflects the demand side of food security and is generally predicted by the amount of economic and social resources. Our focus on access is also motivated by the type of programs (e.g., economic strengthening) that can be developed to improve access to food.
ART adherence
The World Health Organization defines adherence as the extent to which a person’s behavior corresponds with agreed recommendations from a healthcare provider (Sabaté, 2003). Consistent with food insecurity, adherence can be viewed as a multidimensional phenomenon that includes a broad range of health behaviors such as seeking medical attention, taking medications as prescribed, attending followup appointments, and filling prescriptions. However, we define adherence as medication adherence or taking drugs as prescribed. This definition is consistent with one of the more common definitions of adherence in the HIV literature (Liu et al., 2001; Llabre et al., 2006; Weiser et al., 2014). Within the narrower concept of medication adherence, we focused on dose adherence, defined as the amount or proportion of medications taken by a patient relative to the amount or proportion of medications prescribed (Cramer et al., 2008). We used this definition of medication adherence because it is more commonly used in the HIV and ART adherence literature than other dimensions such as timing and frequency. In summary, clarity of our definition of food insecurity and ART adherence guided our selection of theories and conceptualization of the multilevel framework.
Why food insecurity affects adherence: Theories of health behavior at the intrapersonal, interpersonal, and structural level
Intrapersonal level
Health belief model
Although the health belief model (HBM) has been used to explain ART adherence in resource-adequate (Malcolm, Ng, Rosen, & Stone, 2003) and resource-limited settings (Roura et al., 2009; Wringe et al., 2009), to our knowledge, we are not aware of prior published studies that applied the HBM to explain the association between food insecurity (a particular barrier to treatment adherence) and ART. The role of individual beliefs about food insecurity as a barrier to ART adherence is exemplified in the HBM using the concepts of perceived barriers and perceived self-efficacy (Rosenstock, Strecher, & Becker, 1988). People’s perception of the barriers to performing a health behavior has been shown to be a strong predictor of the actual behavior (Asare, Sharma, Bernard, Rojas-Guyler, & Wang, 2013; Volk & Koopman, 2001). Perceived barriers refer to costs (monetary and nonmonetary) that must be overcome for an individual to perform and maintain a particular health behavior (Janz, Champion, & Strecher, 2002). In the case of ART adherence, a major cost or perceived barrier, particularly in low-resource settings, is inadequate access to food. If PLHIV with treatment experience are food insecure, they may not be able to adhere to treatment because lack of access to food may compel them to skip taking medications as prescribed or to take medications only when they have food. Patients who are food insecure and taking ART may weigh expected effectiveness or benefits of taking their medications against beliefs that taking antiretroviral (ARV) drugs without food may be less efficacious and creates intolerable side effects. Additionally, patients taking ART may weigh expected benefits of treatment and its ancillary costs against other competing demands, such as urgency of paying for other household needs. Evidence suggests that actual experience or fear of experiencing food insecurity influences the decision of patients taking ART to skip doses and only take medications when they have food (Young et al., 2014).
Furthermore, food insecurity as a perceived barrier may affect PLHIVs’ perception of their ability to achieve and maintain optimal adherence levels. If PLHIV do not have access to adequate food to optimize treatment efficacy and prevent severe side effects, they may believe that they are not capable of adhering and less likely to benefit from treatment. ART adherence requires a good deal of confidence to initiate and maintain because it requires lifetime adherence. Consistent with perceived barriers, people’s perception of their efficacy to perform a particular health behavior has been shown to be a strong predictor of engaging in that same behavior (Hounton, Carabin, & Henderson, 2005; Zak-Place & Stern, 2004). In other words, food insecurity acts as a barrier, which, in turn, may influence one’s perceived self-efficacy to adhere to ART. In turn, perceived self-efficacy predicts actual adherence or nonadherence to treatment.
Interpersonal level
Social cognitive theory
Social cognitive theory (SCT) is a theoretical model of behavior that recognizes the influence of interpersonal dynamics on health behaviors. Based on SCT, PLHIVs’ ability to adhere to ART is explained through a triadic, dynamic, and reciprocal relationship in which medication adherence, individual factors (such as personal expectancies), and environmental influences (primarily from social relationships) are continuously interacting and reinforcing each other (Bandura, 1977, 1986). Personal expectancies can be outcome related (e.g., beliefs about the benefits of ART adherence) or about individual competence (or personal efficacy to adhere to ART). In turn, personal expectancies are strong predictors of behaviors (Bandura, 1997, 1998).
PLHIVs’ beliefs about outcomes and beliefs of personal efficacy within the context of food insecurity can be influenced by interpersonal relationships through vicarious experiences (or learning by observation) and social persuasion. For instance, witnessing other patients who are food insecure and taking ART adhere to treatment may enhance observers’ beliefs that they, too, possess the ability to adhere to treatment. Alternatively, seeing other PLHIV who are food insecure struggle to adhere to ART may diminish observers’ beliefs that they can follow treatment as prescribed. Seeing other food-insecure ART patients suffer from severe side effects exacerbated by the absence of food may influence others’ decision to skip doses or only take medications when there is food to avoid adverse reactions. Empirical evidence supports the role of observational learning on ART adherence among PLHIV who are food insecure in low-resource settings (Grant, Logie, Masura, Gorman, & Murray, 2008; Kalofonos, 2010; Weiser et al., 2010). For example, in Mozambique, PLHIV who knew family or other community members who experienced severe hunger while on ART were discouraged to continue treatment because of fear that acute hunger might occur when ARV drugs are taken without food (Kalofonos, 2010).
In addition to observational learning, social persuasion can influence PLHIVs’ beliefs about outcomes and beliefs of personal efficacy. In many communities in sub-Saharan Africa (SSA), high rates of ART adherence in spite of economic barriers such as food insecurity have been attributed to social persuasion. Social persuasion refers to explicit expectations from PLHIVs’ essential relationships (e.g., family members, friends, and healthcare providers) that they can adhere to treatment (Ware et al., 2009). Social persuasion may enable PLHIV to muster greater effort to succeed, fulfill social responsibilities, and preserve social relationships, which in turn, may ensure assistance will be available when future needs arise. However, the reverse is also possible. For example, PLHIV who are food insecure may not have a wider network of social support or role models that can encourage them to adhere to treatment. HIV/AIDS remains highly stigmatized (Abrahams & Jewkes, 2012; Kidia et al., 2015), which in turn, may result in a weakening or dissolution of a social support system. Further, dissolution of a social network may discourage patients taking ART to adhere to treatment.
Structural level: Role of resources
Conservation of resources theory
Conservation of resources theory (CoRT) emphasizes the role of resources as predictors of health behaviors. People accumulate resources, which can be personal or material, that they can use to accommodate, withstand, or overcome threats (Hobfoll, 1989). These resources are valued because they satisfy the survival needs of individuals. Consequently, individuals thrive when they gain, maintain, and conserve their resources (Hobfoll & Lilly, 1993). However, PLHIV may encounter more challenges accumulating resources because of their chronic health condition. For instance, PLHIV are more likely to miss work and earn less income (Donovan & Massingue, 2007; Fox et al., 2004), to incur higher healthcare expenses (Gregson, Mushati, & Nyamukapa, 2007; Ngalula, Urassa, Mwaluko, Isingo, & Ties Boerma, 2002), and to experience diminishing social support due to HIV-related stigma (Dawson, 2013; Kaschula, 2011) than people who are not living with HIV. In turn, these events are less likely to provide PLHIV with opportunities to accumulate resources. Instead, missing work, paying for higher healthcare costs, and losing social support are more likely to drain existing resources and deprive PLHIV of the means to replace expended resources.
A critical and material resource for survival is food. When food is limited or depleted, PLHIVs’ ability to address needs and demands (e.g., optimize treatment benefits and avoid adverse ARV side effects) becomes insufficient. Consequently, inability to access adequate food restricts the ability of PLHIV to adhere to ART (Singer et al., 2015; Young et al., 2014). Additionally, CoRT postulates that when PLHIV cannot satisfy needs or meet demands because of inadequate resources, they experience stress (Hobfoll, 1989). Higher levels of stress, in turn, influence a range of undesirable health outcomes (Cohen & Williamson, 1991; Steptoe, 1991). For example, when PLHIV do not have adequate food, they may experience stress and anxiety that negatively affect their ability to adhere to treatment. Empirical evidence indicates that food insecurity heightens stress levels of PLHIV (Addo et al., 2011; Garcia et al., 2013). Moreover, higher stress levels (or poor psychosocial functioning) predicts nonadherence to ART (Kidia et al., 2015; Langebeek et al., 2014).
CoRT also posits that stress can occur when resources may be at lost or are at risk of being lost. When resources are at risk of being lost, individuals experience anticipatory stress (Hobfoll, 1989). The effects of anticipatory stress can be as severe as actual stress (Hobfoll, 2001). The concept of anticipatory stress is germane to understanding why the fear of running out of food or the possibility of not having enough food may lead to stress at levels that are consistent with actual loss of resources. Accordingly, research has shown that fear of experiencing food insecurity is associated with ART nonadherence (Young et al., 2014).
Structural level: Role of group memberships
Memberships theory of poverty
Memberships theory of poverty (MTP) emphasizes the role of group memberships as predictors of social, economic, and health outcomes (Durlauf, 2001). Although primarily developed as an economic model, MTP posits that structural barriers and group memberships influence individual behaviors. Based on MTP, the ability to engage in a particular behavior depends on the composition of the various groups over the life course of which an individual is a member (Durlauf, 1999, 2001). The groups can be exogenous (such as gender or ethnicity) or endogenous (such as education, employment, or income level). In turn, the groups influence individual outcomes through several mechanisms such as peer group effects, role model effects, social learning, social complementarities, social network effects, and social norms (Durlauf, 2001).
One salient group membership that may strengthen our understanding of the relationship between food insecurity and ART adherence is membership related to health conditions, more specifically being HIV positive. Being HIV positive presents unique opportunities and challenges. For example, HIV infection heightens vulnerability to food insecurity by limiting income and food production (Gillespie & Kadiyala, 2005; Weiser et al., 2011). Furthermore, stigma and discrimination against PLHIV may exacerbate food insecurity as PLHIV may find it more difficult to work and maintain a livelihood or rely on their social networks for assistance. Additionally, PLHIV who live in resource-poor communities with limited employment opportunities, poor healthcare access and quality, and shortage of social assistance programs may be more likely to experience food insecurity than PLHIV who live in resource-rich communities with more economic opportunities and targeted social assistance programs. Because of the role of group memberships on health behavior, HIV care and treatment providers have been employing a group-membership framework (i.e., a group defined by HIV status) to address more effectively the distinct causes and effects of food insecurity on physical and mental health of PLHIV (Roopnaraine, Rawat, Babirye, Ochai, & Kadiyala, 2012). The group-based model is consistent with MTP and its key propositions. For instance, participation in a group-based program may enable participants to build social networks, observe and learn from others, and create social norms to be respected and enforced by group members. As a result, these mechanisms (social networks, social norms, social learning, and role models) may influence an individual’s ability to perform a particular behavior (in this case, ART adherence).
Integrated adherence model: Combining intrapersonal, interpersonal, and structural factors
Information-motivation-strategy model
Although key concepts from HBM, SCT, CoRT, and MTP appear distinct, these same concepts can be integrated to illustrate their interrelatedness and combined influence on ART adherence. The information-motivation-strategy model (IMSM) is an appropriate adherence-focused model of behavior change that combines the four theories of health behavior. IMSM is distinct from the intrapersonal-, interpersonal-, and structural-level theories because IMSM represents a model of behavior change. In contrast, HBM, SCT, CoRT, and MTP, in varying degrees, exemplify models of behavior or explaining health behaviors. IMSM refines the key propositions (from HBM, SCT, CoRT, and MTP) that explain the association between food insecurity and ART adherence into three discrete but interrelated mechanisms that can be targeted and modified through an intervention.
IMSM hypothesizes that before an individual can change health behavior, that individual must (1) know what change is necessary (information component), (2) have the desire to change (motivation component), and (3) have the necessary tools, whether economic, financial, or social, to achieve and maintain health behavior change (strategy component; DiMatteo & Nicola, 1982; Martin, Haskard-Zolnierek, & DiMatteo, 2010; Skovdal, Campbell, Nhongo, Nyamukapa, & Gregson, 2011). To explain the relationship between food insecurity and ART adherence, IMSM posits that adherence will be achieved when PLHIV (1) know and believe that food is important to manage their HIV infection and maximize the benefits of ART, (2) are confident and competent to adhere to ART, and (3) have tangible tools, such as adequate food and financial resources to overcome barriers and carry out the health behavior change.
The flexible nature of IMSM enables the model to incorporate evidence from empirical research, while remaining in line with HBM, SCT, CoRT, and MTP. Consistent with IMSM, food and nutrition counseling provides information about the importance of adequate food and a nutritious diet to optimize treatment outcomes, satisfy increased appetite, and avoid severe side effects. Furthermore, essential social relationships and their influences (either through observational learning or social persuasion) on personal efficacy create motivation to adhere to ART. Social relationships may create powerful channels to encourage PLHIV to adhere to ART in spite of food insecurity. In addition, income from employment or other livelihood activities, or instrumental support in the form of food assistance from social networks, are tangible strategies that are necessary to achieve and maintain ART adherence.
A multilevel conceptual framework for food insecurity and art adherence
Building on the key concepts and propositions outlined in the four theoretical models of behavior and the integrated adherence model, we propose a multilevel conceptual framework for food insecurity and ART adherence in low-resource settings. Figure 1 illustrates the multilevel framework. This framework has two objectives: (1) to explain the relationship between food insecurity and adherence at the intrapersonal, interpersonal, and structural levels and (2) to inform intervention development through synthesis and application of multilevel theories into interrelated and alterable mechanisms. The multilevel framework recognizes that an interaction of intrapersonal, interpersonal, and structural factors may provide a more holistic explanation of why food-insecure ART patients are less likely to adhere to treatment compared with their food-secure counterparts. Alternatively, the framework emphasizes that an incomplete construction of the relationship may lead to development of interventions that fail to recognize and address the combined effects of intrapersonal, interpersonal, and structural factors on health behaviors such as ART adherence.
Figure 1.
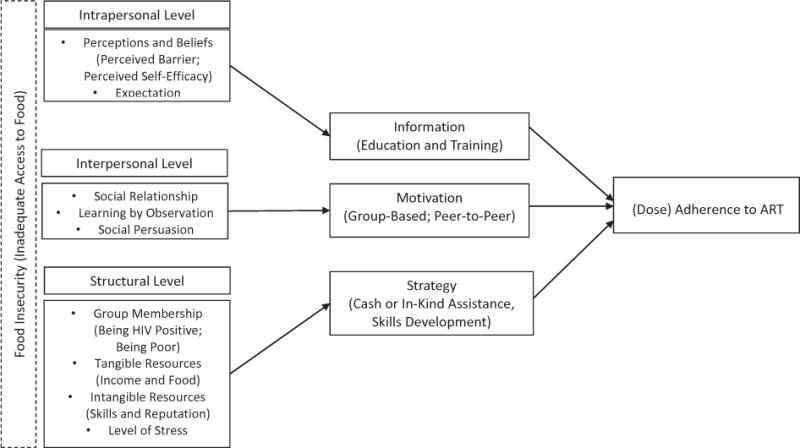
Multilevel conceptual framework for understanding the role of food insecurity on antiretroviral therapy (ART) adherence.
The multilevel framework expands the integrated adherence model by identifying malleable constructs (or intervention “entry points”) that are consistent with the three domains of IMSM. These malleable constructs are also consistent with the four theories of behavior. Each theory represents one of the three domains of IMSM: information, motivation, and strategy. First, intrapersonal level comprises key HBM concepts, such as beliefs, perceptions, and expectations, which in turn, form the information component of IMSM. The HBM and the information component of IMSM acknowledge that PLHIV must have access to information that helps them to create positive beliefs about the importance of food and nutrition on their health and well-being, including treatment adherence. Second, the interpersonal component is adapted primarily from SCT. Interpersonal level translates into motivation through key SCT concepts such as social relationship, learning by observation, and social persuasion. Social relationships remain an important source of motivation. Through observational learning and social persuasion, PLHIV may increase their self-efficacy. SCT and the motivation component of IMSM postulate that social relationships and their effects on individual cognitions and group dynamics strongly influence ART adherence within the context of food insecurity. The third component pertains to structural factors that predict access to food and its effect on ART adherence. These factors consist of tangible and intangible resources that are consistent with MTP and CoRT. In turn, these resources build the strategy component of IMSM. These strategies include group membership, and tangible and intangible assets. In addition, stress is considered a structural factor given its underlying predictors, such as loss of resources and stigma and discrimination against PLHIV. CoRT, MTP, and the strategy element of IMSM emphasize the importance of resources in predicting access to food and adherence to ART.
Another contribution of the framework is its recognition of the interaction of information, motivation, and strategy. Unlike other social-ecological models, IMSM does not specify an interrelationship of the three components. The multilevel framework recognizes that the ability to obtain information may be influenced by a person’s motivation and social relationships, which in turn, may be shaped by the availability of tangible resources. In sum, this multilevel conceptual framework explicitly takes into account the influence of personal, social, and environmental factors on cognition and behavior, with particular attention to mechanisms in which ART adherence is enabled or limited by larger structural conditions, such as poverty, food insecurity, and stigma, which remain widespread in many resource-limited countries.
From theory to practice: Using the multilevel framework to develop an intervention
To move from theory to practice, we describe an example of how we used the multilevel framework to inform a programmatic response. The intervention is based on a promising approach that combines HIV treatment with household-economic-strengthening programs to improve economic and health well-being of patients who are taking ART and resource poor, including their food security and adherence. We developed and implemented the Chuma na Uchzi intervention (or Health and Wealth) in a rural, low-resource community in Zambia. The intervention is an integrated HIV and livelihood program (IHLP) that combined cash transfers, skills training, and financial capability (Masa, 2016). Although the project aims to improve the overall economic and health welfare of PLHIV, we focus on food security and ART adherence because these are the key constructs in the multilevel framework.
As presented in Figure 1, the information component in the framework is operationalized by constructs based on HBM. These constructs can be changed through health education. In Chuma na Uchizi, information or knowledge transfer may be achieved by including a health education component. This component covers topics, such as adequate food and proper nutrition, diet improvement to enhance drug efficacy, management of treatment side effects, and proper sanitation (e.g., handwashing, water safety, and personal hygiene). These health subjects were tailored to the needs of PLHIV with experience in treatment. In other words, the health education component provides the necessary information about food and ART that may help participants assess the benefits and barriers to adherence, as well as their personal efficacy to adhere to treatment.
Furthermore, the motivation component is operationalized using constructs that are consistent with SCT. These constructs can be enhanced by social relationships. In Chuma na Uchizi, social relationships are nurtured through the concept of group membership, particularly as people living with HIV. Recognizing that being HIV positive presents unique strengths and challenges, Chuma na Uchizi, purposefully selected group-based training to create opportunities for observational learning and social persuasion. Our assumption is that interaction with other PLHIV who are more likely to understand the daily challenges of adhering to treatment (particularly while being food insecure) may act as examples, which in turn, may motivate participants to adhere to ART. In addition, other PLHIV may become role models and a source of social support. Chuma na Uchizi offer several opportunities for group-based learning and interaction. For example, skills training, which consist of sessions on financial literacy, business management, and health education, may enable opportunities for classroom and group-based techniques that allow peer-to-peer interaction and learning. Other programs have also facilitated formation of self-help groups that function as a support network to assist in carrying out livelihood activities and to encourage healthy behaviors (Datta & Njuguna, 2008). Through contact with other PLHIV, participants can learn (through observations, role modeling, or social persuasions) how to manage food insecurity, while adhering to ART. Beyond participants’ family members and relatives, an IHLP may also expand PLHIVs’ social support network to include other PLHIV, healthcare providers, and livelihood experts who are trained to be respectful and sensitive to PLHIVs’ situation. In sum, being part of a group that empathizes or shares similar experiences may motivate PLHIV to perform desirable health behaviors.
Additionally, the strategy component is operationalized using key constructs and propositions from CoRT and MTP. Because of its multifaceted nature, Chuma na Uchizi (and other IHLP) provide opportunities for participants to accumulate different types of resources. These resources can be intrapersonal (such as optimism and self-efficacy) or interpersonal (such as motivation and social support). In addition to intangible assets, tangible resources are provided. In Chuma na Uchizi, tangible resources include cash transfers and a low-cost savings account. The cash transfers are given to help participants accumulate productive assets. The savings account is designed to provide a safe and secure way to set aside money for future use. Furthermore, in Chuma na Uchizi, intangible resources include development and acquisition of life skills. These life skills represent a range of topics, such as small business management, financial literacy, and health competency. The combination of intangible and tangible resources provides experiential learning, which enables participants to learn new skills and to use those skills. For example, Chuma na Uchizi offers training sessions on how to start or manage income-generating activities, from separating personal and business income to pricing and marketing products. In addition, the program provides cash and other material assistance to help participants use their new skills. These opportunities and activities are strategies that may help PLHIV earn income and obtain money to buy food or may increase their capacity to produce food. In turn, these resources become necessary tools to achieve and maintain ART adherence. Furthermore, these material resources, in addition to personal and social assets, may make it less stressful to follow treatment guidelines and sustain adherence for a longer period of time.
Lastly, the selection of the project district is purposeful. Consistent with MTP, PLHIV in resource-poor communities with limited livelihood opportunities are more likely to encounter additional barriers than their peers in resource-rich communities with more economic opportunities and better services. Accordingly, Chuma na Uchizi is implemented in Lundazi District in Eastern Province, Zambia. Lundazi District is a rural and poor district with a high prevalence of HIV. Lundazi District has an estimated HIV prevalence rate of 15%, which is higher than the prevalence rates for Eastern Province (9.3%) and Zambia (13.3%; Central Statistical Office, Ministry of Health, & ICF International, 2015). Lundazi District is predominantly rural with more than 90% of the population living in rural areas (Central Statistical Office, 2012b). At the provincial level, an estimated 78% of the population is living in poverty, which is the third highest in the country. Further, 59% of the population is estimated to be living in extreme poverty, which is also the third highest in Zambia (Central Statistical Office, 2012a).
Hypothesized effects and empirical support
Figure 2 illustrates the proposed effects of Chuma na Uchizi. The intervention is hypothesized to have direct and indirect effects on ART adherence. The indirect effect is mediated by food security or psychosocial functioning, which, in turn, directly affects adherence. Chuma na Uchizi is also hypothesized to directly affect food security and psychosocial functioning, such as perceived stress and treatment self-efficacy. Using the multilevel framework, the proposed relationships identify the variables that are to be targeted, affected, and improved by the intervention. The hypothesized relationships also represent how the intervention attempts to change or improve outcomes by incorporating and manipulating mechanisms that are consistent with the multilevel conceptual framework for food insecurity and ART adherence.
Figure 2.
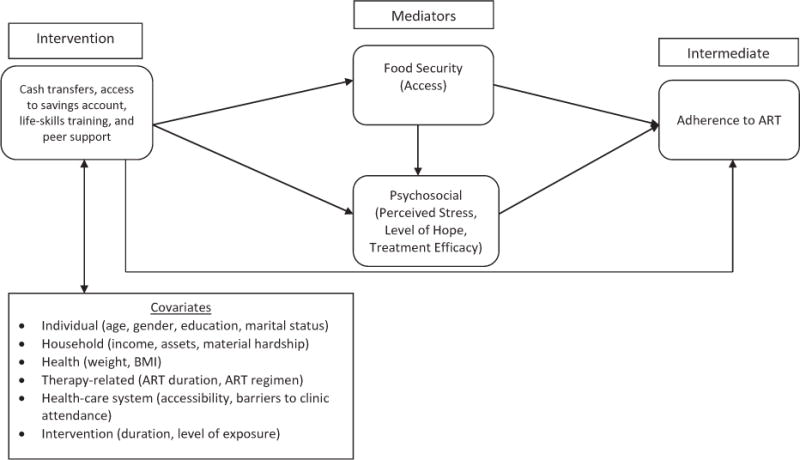
Hypothesized relationships that are represented in a program designed to address food security and antiretroviral therapy (ART) adherence.
The proposed relationships outlined in Figure 2 are not only informed by theoretical evidence but also supported by empirical research. For instance, the model’s mediators and covariates are known facilitators and barriers to ART adherence in resource-limited countries (Langebeek et al., 2014; Lankowski, Siedner, Bangsberg, & Tsai, 2014; Mills et al., 2006; Reda & Biadgilign, 2012; Weiser et al., 2014). Financial constraints, including income sufficiency, are negatively associated with ART adherence (Bezabhe et al., 2014; Sanjobo et al., 2008; Weiser et al., 2003). Also, food insecurity is emerging as a major barrier to treatment adherence (Singer et al., 2015; Young et al., 2014). Similarly, adequate access to food improves ART adherence (de Pee, Grede, Mehra, & Bloem, 2014; Tirivayi & Groot, 2011). At the most basic level, higher and regular incomes make it easier to put food on the table every day. Poor mental status, such as higher levels of stress and feelings of hopelessness predict lower ART adherence rates (Kidia et al., 2015; Langebeek et al., 2014; Mills et al., 2006). Food insecurity is also associated with higher levels of mental distress among PLHIV in low-resource communities (Addo et al., 2011; Palermo, Rawat, Weiser, & Kadiyala, 2013).
In addition to correlational studies, several examples of intervention research support Chuma na Uchizi’s hypothesized relationships. For instance, food assistance programs in low-resource communities have improved ART adherence (Cantrell et al., 2008; Palar et al., 2015; Tirivayi, Koethe, & Groot, 2012). Similarly, these programs have increased food security of PLHIV and their households (de Pee et al., 2014; Rawat, Faust, Maluccio, & Kadiyala, 2014). In addition, evaluation of livelihood programs for PLHIV has shown promising effects on household income and food security (Pandit et al., 2010; Weiser et al., 2015). Similarly, evaluation of livelihood interventions for the general population has found positive impacts on economic and health outcomes (Boccia et al., 2011; Chowa, Masa, & Sherraden, 2012; Dunbar et al., 2014; Nsabuwera et al., 2015). For instance, a randomized multifaceted livelihood program implemented in six resource-poor countries, including Ethiopia and Ghana, had long-term positive impacts on household income, food security, and mental health status, including lower stress level (Banerjee et al., 2015).
Discussion
In recent years, household-economic-strengthening strategies have been integrated with HIV treatment and care programs in low-resource settings globally. This integration is motivated by a growing recognition that purely biomedical interventions may not result in optimal outcomes when patients’ socioeconomic needs are not fully met, particularly for PLHIV in low-resource countries. Furthermore, the expansion of ART, which has expanded the number of low-income PLHIV with access to lifesaving HIV treatment, has heightened the need to address social and economic barriers to ART adherence. Similarly, the expansion of access to ART has increased the proportion of PLHIV without resources to pay for treatment-related needs and costs, such as adequate food. This overlap of poverty, food insecurity, and access to HIV treatment may undermine progress in increasing survival of PLHIV and eliminating HIV/AIDS. In turn, this increasing trend has led to development and testing of various strategies, such as food assistance and livelihood support, to tackle inadequate access to food and its adverse effects on ART adherence.
However, the theoretical foundation for these programmatic responses, particularly livelihood support combined with HIV treatment, has not been sufficiently explained. The use of theories to explain a problem (in this case, the relationship between food insecurity and ART adherence) is valuable from a basic and applied research perspective. Theories are useful to guide our understanding of why and how a particular issue occurs. We identified appropriate theories from public health (HBM and IMSM), social psychology (CoRT and SCT), and economics (MTP) to inform a multilevel conceptual framework that takes into account the role of intrapersonal, interpersonal, and environmental factors in predicting behaviors. In particular, these theories were applied to illustrate how and why food insecurity contribute to nonadherence among patients taking ART in low-resource communities. Each theory represents a particular level of understanding health behaviors. HBM explains the influence of individual beliefs as motivators of adherence (intrapersonal). SCT describes the role of psychosocial (or interpersonal) dynamics on adherence. CoRT clarifies the role of environmental factors (in particular, presence or absence of tangible and intangible resources) on an individual’s mental health. In particular, CoRT highlights the effect of stress (real or anticipatory) on adherence. MTP illustrates the influence of unique group-level factors and structural constraints on health outcomes. Being HIV positive and living in a low-resource community are two salient group memberships that may negatively affect various outcomes, such as the ability to earn income, buy food, and adhere to treatment. Lastly, IMSM, which is also an integrated adherence model, combines key propositions from the four theories and identifies three distinct and alterable mechanisms that predict adherence in the context of food insecurity.
These theories may guide not only our understanding of the problem but also, more importantly, the development of appropriate interventions. The multilevel framework was created to operationalize relevant constructs and propositions from the five theoretical models into mechanisms that can be targeted and altered through an intervention. In turn, the multilevel conceptual framework informed the development of Chuma na Uchizi, an economic-strengthening intervention for treatment-experienced PLHIV in a low-resource and rural community in Eastern Province, Zambia. The framework is unique because it recognizes the different layers of factors (intrapersonal, interpersonal, and structural) affecting health behavior change (i.e., ART adherence). The framework also considers the limitations of using only a single level of understanding behavior. For instance, HBM has been critiqued for focusing primarily on individual decision making and thus may have limited relevance when addressing HIV and food insecurity in non-Western societies and resource-limited countries (Campbell, 2003; Tomlinson, Rohleder, Swartz, Drimie, & Kagee, 2010). Similarly, SCT does not consider that individual cognitions are shaped by larger contextual realities and structural issues that are beyond the immediate social networks of PLHIV (Kagee et al., 2011; Skovdal et al., 2011).
Theoretical models that rely on rational choice ignore broader factors that operate outside individuals’ ability to weigh costs and benefits and beyond their immediate social relationships. However, these nonindividual factors may have substantial influence on how patients who are food-insecure and taking ART in low-resource settings make adherence decisions. Addressing the limitations of purely individual theories of behavior change, our multilevel framework acknowledges that larger economic and social factors may be more constraining on individual behaviors among marginalized populations in low-resource communities than their less-stigmatized counterparts in resource-adequate settings. In sum, the multilevel framework explicitly recognizes the role of personal, social, and environmental factors on cognition and behavior, with particular attention to ways in which ART adherence is enabled or prevented by structural conditions, such as poverty, food insecurity, and stigma.
The framework has implications for social work practice, particularly public health social work. ART has transformed HIV from a life-threatening illness to a more chronic, manageable condition. This advancement in HIV therapy means that PLHIV can now live longer and healthier. However, access to ART alone is not sufficient to fulfill its benefits on survival and better health. PLHIV are required to remain in treatment and care, including long-term adherence to ART. To ensure that patients taking ART adhere to treatment, barriers must be identified and addressed. Social workers working with PLHIV should be aware of known barriers and corresponding tools to mitigate adverse effects. One critical barrier, particularly for poor PLHIV, is inadequate access to food.
At the same time, practitioners must understand why and how food insecurity negatively influences treatment adherence. Social workers should be familiar with coping strategies (positive and negative) and recognize how various strategies affect the well-being of PLHIV. If coping mechanisms are desirable, social workers should be trained on how to strengthen these strategies. If coping techniques are harmful, social workers should be equipped to minimize risky coping strategies without stigmatizing PLHIV. Similarly, social workers should be trained to address fears of PLHIV about hunger and adverse effects of ART when food is not sufficient. Counseling sessions should include concrete strategies to tackle and overcome various mechanisms, as illustrated in the multilevel framework in which food insecurity can interfere with treatment adherence. Additionally, social workers and other allied health practitioners should be knowledgeable of readily available services that provide food to PLHIV who are food insecure or be able to issue referrals for food assistance. These practice implications are consistent with the social work profession, which requires practitioners to have accurate and up-to-date knowledge of economic and health factors that facilitate human development and individual capacity for better social functioning, particularly among the most vulnerable populations. Lastly, these practice recommendations may help social workers to be more effective social service providers and advocate for PLHIV.
Conclusions
A single level of understanding health behavior may not adequately explain the relationship between ART adherence and food insecurity in low-resource communities. However, a combination of cognitive, psychosocial, material, and structural factors may explain more convincingly why and how PLHIV who are food insecure are less likely to adhere to ART than their food-secure counterparts. A multilevel conceptual framework that considers the influence of intrapersonal, interpersonal, and environmental factors on cognition and behavior, with particular attention to mechanisms in which treatment adherence is enabled or limited by a larger structural background, may be more salient in understanding why food insecurity acts as a barrier to treatment adherence. A broader perspective on understanding the association between food insecurity and ART adherence beyond an “individualistic” or “structuralist” perspective only may be required if substantial contributions to the betterment of PLHIV who are food insecure is to be achieved. A multilevel conceptual framework that incorporates intrapersonal, interpersonal and environmental factors may help identify holistic, feasible, and appropriate “entry points” for interventions that promote food security as a strategy to improve ART adherence.
References
- Abrahams N, Jewkes R. Managing and resisting stigma: A qualitative study among people living with HIV in South Africa. Journal of the International AIDS Society. 2012;15(2):17330. doi: 10.7448/IAS.15.2.17330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Addo AA, Marquis GS, Lartey AA, Perez-Escamilla R, Mazur RE, Harding KB. Food insecurity and perceived stress but not HIV infection are independently associated with lower energy intakes among lactating Ghanaian women. Maternal & Child Nutrition. 2011;7(1):80–91. doi: 10.1111/j.1740-8709.2009.00229.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asare M, Sharma M, Bernard AL, Rojas-Guyler L, Wang LL. Using the health belief model to determine safer sexual behavior among African immigrants. Journal of Health Care for the Poor and Underserved. 2013;24(1):120–134. doi: 10.1353/hpu.2013.0020. [DOI] [PubMed] [Google Scholar]
- Bandura A. Self-efficacy: Toward a unifying theory of behavioral change. Psychological Review. 1977;84(2):191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- Bandura A. Social foundations of thought and action: A social cognitive theory. Englewood Cliffs, NJ: Prentice Hall; 1986. [Google Scholar]
- Bandura A. Self-efficacy: The exercise of control. New York, NY: W. H. Freeman; 1997. [Google Scholar]
- Bandura A. Health promotion from the perspective of social cognitive theory. Psychology and Health. 1998;13(4):623–649. [Google Scholar]
- Banerjee A, Duflo E, Goldberg N, Karlan D, Osei R, Parienté W, Udry C. A multifaceted program causes lasting progress for the very poor: Evidence from six countries. Science. 2015;348(6236):1260799. doi: 10.1126/science.1260799. [DOI] [PubMed] [Google Scholar]
- Barrett CB. Measuring food insecurity. Science. 2010;327(5967):825–828. doi: 10.1126/science.1182768. [DOI] [PubMed] [Google Scholar]
- Bezabhe WM, Chalmers L, Bereznicki LR, Peterson GM, Bimirew MA, Kassie DM. Barriers and facilitators of adherence to antiretroviral drug therapy and retention in care among adult HIV-positive patients: A qualitative study from Ethiopia. PloS ONE. 2014;9(5):e97353. doi: 10.1371/journal.pone.0097353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boccia D, Hargreaves J, Lönnroth K, Jaramillo E, Weiss J, Uplekar M, Evans CA. Cash transfer and microfinance interventions for tuberculosis control: Review of the impact evidence and policy implications. International Journal of Tuberculosis and Lung Disease. 2011;15(2):S37–S49. doi: 10.5588/ijtld.10.0438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell C. Letting them die: Why HIV/AIDS intervention programmes fail. Bloomington, IN: Indiana University Press; 2003. [Google Scholar]
- Cantrell RA, Sinkala M, Megazinni K, Lawson-Marriott S, Washington S, Chi BH, Stringer JS. A pilot study of food supplementation to improve adherence to antiretroviral therapy among food-insecure adults in Lusaka, Zambia. Journal of Acquired Immune Deficiency Syndromes. 2008;49(2):190–195. doi: 10.1097/QAI.0b013e31818455d2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Central Statistical Office. 2010 census of population and housing. Population summary report. Lusaka, Zambia: Author; 2012a. [Google Scholar]
- Central Statistical Office. 2010 census of population and housing. Volume 11 national descriptive tables. Lusaka, Zambia: Author; 2012b. [Google Scholar]
- Central Statistical Office, Ministry of Health, & ICF International. Zambia demographic and health survey 2013–2014. Lusaka, Zambia: Central Statistical Office; 2015. [Google Scholar]
- Chi BH, Cantrell RA, Zulu I, Mulenga LB, Levy JW, Tambatamba BC, Stringer JS. Adherence to first-line antiretroviral therapy affects non-virologic outcomes among patients on treatment for more than 12 months in Lusaka, Zambia. International Journal of Epidemiology. 2009;38(3):746–756. doi: 10.1093/ije/dyp004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chowa G, Masa R, Sherraden M. Wealth effects of an asset-building intervention among rural households in sub-Saharan Africa. Journal of the Society for Social Work and Research. 2012;3:329–345. doi: 10.5243/jsswr.2012.20. [DOI] [Google Scholar]
- Cohen S, Williamson GM. Stress and infectious disease in humans. Psychological Bulletin. 1991;109:5–24. doi: 10.1037/0033-2909.109.1.5. [DOI] [PubMed] [Google Scholar]
- Cramer JA, Roy A, Burrell A, Fairchild CJ, Fuldeore MJ, Ollendorf DA, Wong PK. Medication compliance and persistence: Terminology and definitions. Value in Health. 2008;11(1):44–47. doi: 10.1111/j.1524-4733.2007.00213.x. [DOI] [PubMed] [Google Scholar]
- Datta D, Njuguna J. Microcredit for people affected by HIV and AIDS: Insights from Kenya. SAHARA J: Journal of Social Aspects of HIV/AIDS Research Alliance. 2008;5(2):94–102. doi: 10.1080/17290376.2008.9724906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson H. HIV/AIDS, the erosion of social capital and the collapse of rural livelihoods in the Nkomazi District of South Africa. African Journal of AIDS Research. 2013;12(4):185–194. doi: 10.2989/16085906.2013.863218. [DOI] [PubMed] [Google Scholar]
- de Pee S, Grede N, Mehra D, Bloem MW. The enabling effect of food assistance in improving adherence and/or treatment completion for antiretroviral therapy and tuberculosis treatment: A literature review. AIDS and Behavior. 2014;18(Suppl 5):S531–S541. doi: 10.1007/s10461-014-0730-2. [DOI] [PubMed] [Google Scholar]
- de Pee S, Semba RD. Role of nutrition in HIV infection: Review of evidence for more effective programming in resource-limited settings. Food and Nutrition Bulletin. 2010;31(4):S313–S344. [PubMed] [Google Scholar]
- de Waal A, Whiteside A. New variant famine: AIDS and food crisis in Southern Africa. Lancet. 2003;362(9391):1234–1237. doi: 10.1016/S0140-6736(03)14548-5. doi:S0140-6736(03)14548-5. [DOI] [PubMed] [Google Scholar]
- DiMatteo MR, Nicola DD. Achieving patient compliance. New York, NY: Pergamon Press; 1982. [Google Scholar]
- Donovan C, Massingue J. Illness, death, and macronutrients: Adequacy of rural Mozambican household production of macronutrients in the face of HIV/AIDS. Food and Nutrition Bulletin. 2007;28(2 Suppl):S331–S338. doi: 10.1177/15648265070282S212. [DOI] [PubMed] [Google Scholar]
- Dunbar MS, Kang Dufour MS, Lambdin B, Mudekunye-Mahaka I, Nhamo D, Padian NS. The SHAZ! project: Results from a pilot randomized trial of a structural intervention to prevent HIV among adolescent women in Zimbabwe. PLoS ONE. 2014;9(11):e113621. doi: 10.1371/journal.pone.0113621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durlauf SN. The memberships theory of inequality: Ideas and implications. In: Brezis ES, Temin P, editors. Elites, minorities and economic growth. Amsterdam, The Netherlands: Elsevier; 1999. pp. 161–177. [Google Scholar]
- Durlauf SN. The memberships theory of poverty: The role of group affiliations in determining socioeconomic outcomes. In: Danziger SH, Haveman RH, editors. Understanding poverty. New York, NY: Russell Sage Foundation; 2001. pp. 392–416. [Google Scholar]
- Food and Agriculture Organization of the United Nations. Rome declaration on world food security. 1996 Retrieved from http://www.fao.org/docrep/003/w3613e/w3613e00.HTM.
- Fox MP, Rosen S, MacLeod WB, Wasunna M, Bii M, Foglia G, Simon JL. The impact of HIV/AIDS on labour productivity in Kenya. Tropical Medicine and International Health. 2004;9(3):318–324. doi: 10.1111/j.1365-3156.2004.01207.x. [DOI] [PubMed] [Google Scholar]
- Garcia J, Hromi-Fiedler A, Mazur RE, Marquis G, Sellen D, Lartey A, Perez-Escamilla R. Persistent household food insecurity, HIV, and maternal stress in peri-urban Ghana. BMC Public Health. 2013;13:215. doi: 10.1186/1471-2458-13-215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillespie S, Kadiyala S. HIV/AIDS and food and nutrition security: From evidence to action. Washington, DC: International Food Policy Research Institute; 2005. [Google Scholar]
- Grant E, Logie D, Masura M, Gorman D, Murray SA. Factors facilitating and challenging access and adherence to antiretroviral therapy in a township in the Zambian Copperbelt: A qualitative study. AIDS Care. 2008;20(10):1155–1160. doi: 10.1080/09540120701854634. [DOI] [PubMed] [Google Scholar]
- Gregson S, Mushati P, Nyamukapa C. Adult mortality and erosion of household viability in AIDS-afflicted towns, estates, and villages in Eastern Zimbabwe. Journal of Acquired Immune Deficiency Syndromes. 2007;44(2):188–195. doi: 10.1097/01.qai.0000247230.68246.13. [DOI] [PubMed] [Google Scholar]
- Hobfoll SE. Conservation of resources. A new attempt at conceptualizing stress. American Psychologist. 1989;44(3):513–524. doi: 10.1037//0003-066x.44.3.513. [DOI] [PubMed] [Google Scholar]
- Hobfoll SE. The influence of culture, community, and the nested-self in the stress process: Advancing conservation of resources theory. Applied Psychology. 2001;50(3):337–421. doi: 10.1111/1464-0597.00062. [DOI] [Google Scholar]
- Hobfoll SE, Lilly RS. Resource conservation as a strategy for community psychology. Journal of Community Psychology. 1993;21(2):128–148. doi: 10.1002/1520-6629(199304)21:23.0.CO;2-5. [DOI] [Google Scholar]
- Hong SY, Fanelli TJ, Jonas A, Gweshe J, Tjituka F, Sheehan HM, Tang AM. Household food insecurity associated with antiretroviral therapy adherence among HIV-infected patients in Windhoek, Namibia. Journal of Acquired Immune Deficiency Syndromes. 2014;67(4):e115–122. doi: 10.1097/QAI.0000000000000308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hounton SH, Carabin H, Henderson NJ. Towards an understanding of barriers to condom use in rural Benin using the health belief model: A cross sectional survey. BMC Public Health. 2005;5:8. doi: 10.1186/1471-2458-5-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janz NK, Champion VL, Strecher VJ. The health belief model. In: Glanz K, Rimer BK, Lewis FM, editors. Health behavior and health education: Theory, research, and practice. San Francisco, CA: Jossey-Bass; 2002. pp. 45–66. [Google Scholar]
- Kadiyala S, Rawat R. Food access and diet quality independently predict nutritional status among people living with HIV in Uganda. Public Health Nutrition. 2013;16(1):164–170. doi: 10.1017/S136898001200050X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kagee A, Remien RH, Berkman A, Hoffman S, Campos L, Swartz L. Structural barriers to ART adherence in Southern Africa: Challenges and potential ways forward. Global Public Health. 2011;6(1):83–97. doi: 10.1080/17441691003796387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalofonos IA. “All I eat is ARVs”: The paradox of AIDS treatment interventions in Central Mozambique. Medical Anthropology Quarterly. 2010;24(3):363–380. doi: 10.1111/j.1548-1387.2010.01109.x. [DOI] [PubMed] [Google Scholar]
- Kaschula S. Using people to cope with the hunger: Social networks and food transfers amongst HIV/AIDS afflicted households in KwaZulu-Natal, South Africa. AIDS and Behavior. 2011;15(7):1490–1502. doi: 10.1007/s10461-011-0006-z. [DOI] [PubMed] [Google Scholar]
- Kidia K, Machando D, Bere T, Macpherson K, Nyamayaro P, Potter L, Abas M. ‘I was thinking too much’: Experiences of HIV-positive adults with common mental disorders and poor adherence to antiretroviral therapy in Zimbabwe. Tropical Medicine and International Health. 2015;20(7):903–913. doi: 10.1111/tmi.12502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koethe JR, Blevins M, Bosire C, Nyirenda C, Kabagambe EK, Mwango A, Heimburger DC. Self-reported dietary intake and appetite predict early treatment outcome among low-BMI adults initiating HIV treatment in Sub-Saharan Africa. Public Health Nutrition. 2013;16(3):549–558. doi: 10.1017/S1368980012002960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langebeek N, Gisolf EH, Reiss P, Vervoort SC, Hafsteinsdottir TB, Richter C, Nieuwkerk PT. Predictors and correlates of adherence to combination antiretroviral therapy (ART) for chronic HIV infection: A meta-analysis. BMC Medicine. 2014;12:142. doi: 10.1186/PREACCEPT-1453408941291432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lankowski AJ, Siedner MJ, Bangsberg DR, Tsai AC. Impact of geographic and transportation-related barriers on HIV outcomes in Sub-Saharan Africa: A systematic review. AIDS and Behavior. 2014;18(7):1199–1223. doi: 10.1007/s10461-014-0729-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larson BA, Fox MP, Bii M, Rosen S, Rohr J, Shaffer D, Simon JL. Antiretroviral therapy, labor productivity, and sex: A longitudinal cohort study of tea pluckers in Kenya. AIDS. 2013;27(1):115–123. doi: 10.1097/QAD.0b013e32835a5b12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu H, Golin CE, Miller LG, Hays RD, Beck CK, Sanandaji S, Wenger NS. A comparison study of multiple measures of adherence to HIV protease inhibitors. Annals of Internal Medicine. 2001;134(10):968–977. doi: 10.7326/0003-4819-134-10-200105150-00011. doi:200105150-00011. [DOI] [PubMed] [Google Scholar]
- Llabre MM, Weaver KE, Duran RE, Antoni MH, McPherson-Baker S, Schneiderman N. A measurement model of medication adherence to highly active antiretroviral therapy and its relation to viral load in HIV-positive adults. AIDS Patient Care and STDs. 2006;20(10):701–711. doi: 10.1089/apc.2006.20.701. [DOI] [PubMed] [Google Scholar]
- Malcolm S, Ng J, Rosen R, Stone V. An examination of HIV/AIDS patients who have excellent adherence to HAART. AIDS Care. 2003;15(2):251–261. doi: 10.1080/0954012031000068399. [DOI] [PubMed] [Google Scholar]
- Martin LR, Haskard-Zolnierek KB, DiMatteo MR. Health behavior change and treatment adherence: Evidence-based guidelines for improving healthcare. New York, NY: Oxford University Press; 2010. [Google Scholar]
- Masa RD. Food security and antiretroviral therapy adherence among people living with HIV in Lundazi District. Zambia: A pilot study. 2016 (Unpublished doctoral dissertation). Retrieved from ProQuest. (ProQuest No. 10119827) [Google Scholar]
- Maxwell S. Food security: A post-modern perspective. Food Policy. 1996;21(2):155–170. [Google Scholar]
- Mills EJ, Nachega JB, Buchan I, Orbinski J, Attaran A, Singh S, Bangsberg DR. Adherence to antiretroviral therapy in sub-Saharan Africa and North America: A meta-analysis. Journal of the American Medical Association. 2006;296(6):679–690. doi: 10.1001/jama.296.6.679. [DOI] [PubMed] [Google Scholar]
- Musumari PM, Feldman MD, Techasrivichien T, Wouters E, Ono-Kihara M, Kihara M. If I have nothing to eat, I get angry and push the pills bottle away from me”: A qualitative study of patient determinants of adherence to antiretroviral therapy in the Democratic Republic of Congo. AIDS Care. 2013;25(10):1271–1277. doi: 10.1080/09540121.2013.764391. [DOI] [PubMed] [Google Scholar]
- Musumari PM, Wouters E, Kayembe PK, Kiumbu Nzita M, Mbikayi SM, Suguimoto SP, Kihara M. Food insecurity is associated with increased risk of non-adherence to antiretroviral therapy among HIV-infected adults in the Democratic Republic of Congo: A cross-sectional study. PloS ONE. 2014;9(1):e85327. doi: 10.1371/journal.pone.0085327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ngalula J, Urassa M, Mwaluko G, Isingo R, Ties Boerma J. Health service use and household expenditure during terminal illness due to AIDS in rural Tanzania. Tropical Medicine and International Health. 2002;7(10):873–877. doi: 10.1046/j.1365-3156.2002.00922.x. [DOI] [PubMed] [Google Scholar]
- Nsabuwera V, Hedt-Gauthier B, Khogali M, Edginton M, Hinderaker SG, Nisingizwe MP, Drobac P. Making progress towards food security: Evidence from an intervention in three rural districts of Rwanda. Public Health Nutrition. 2015;19(7):1296–1304. doi: 10.1017/S1368980015002207. doi:S1368980015002207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palar K, Derose KP, Linnemayr S, Smith A, Farias H, Wagner G, Martinez H. Impact of food support on food security and body weight among HIV antiretroviral therapy recipients in Honduras: A pilot intervention trial. AIDS Care. 2015;27(4):409–415. doi: 10.1080/09540121.2014.983041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palermo T, Rawat R, Weiser SD, Kadiyala S. Food access and diet quality are associated with quality of life outcomes among HIV-infected individuals in Uganda. PloS ONE. 2013;8(4):e62353. doi: 10.1371/journal.pone.0062353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pandit JA, Sirotin N, Tittle R, Onjolo E, Bukusi EA, Cohen CR. Shamba maisha: A pilot study assessing impacts of a micro-irrigation intervention on the health and economic wellbeing of HIV patients. BMC Public Health. 2010;10:245. doi: 10.1186/1471-2458-10-245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rawat R, Faust E, Maluccio JA, Kadiyala S. The impact of a food assistance program on nutritional status, disease progression, and food security among people living with HIV in Uganda. Journal of Acquired Immune Deficiency Syndromes. 2014;66(1):e15–22. doi: 10.1097/QAI.0000000000000079. [DOI] [PubMed] [Google Scholar]
- Rawat R, McCoy SI, Kadiyala S. Poor diet quality is associated with low CD4 count and anemia and predicts mortality among antiretroviral therapy-naive HIV-positive adults in Uganda. Journal of Acquired Immune Deficiency Syndromes. 2013;62(2):246–253. doi: 10.1097/QAI.0b013e3182797363. [DOI] [PubMed] [Google Scholar]
- Reda AA, Biadgilign S. Determinants of adherence to antiretroviral therapy among HIV-infected patients in Africa. AIDS Research and Treatment. 2012;2012:574656. doi: 10.1155/2012/574656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rollins N. Food insecurity—A risk factor for HIV infection. PLoS Medicine. 2007;4(10):1576–1577. doi: 10.1371/journal.pmed.0040301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roopnaraine T, Rawat R, Babirye F, Ochai R, Kadiyala S. “The group” in integrated HIV and livelihoods programming: Opportunity or challenge? AIDS Care. 2012;24(5):649–657. doi: 10.1080/09540121.2011.630349. [DOI] [PubMed] [Google Scholar]
- Rosenstock IM, Strecher VJ, Becker MH. Social learning theory and the health belief model. Health Education Quarterly. 1988;15(2):175–183. doi: 10.1177/109019818801500203. [DOI] [PubMed] [Google Scholar]
- Roura M, Busza J, Wringe A, Mbata D, Urassa M, Zaba B. Barriers to sustaining antiretroviral treatment in Kisesa, Tanzania: A follow-up study to understand attrition from the antiretroviral program. AIDS Patient Care and STDs. 2009;23(3):203–210. doi: 10.1089/apc.2008.0129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabaté E. Adherence to long-term therapies: Evidence for action. Geneva, Switzerland: World Health Organization; 2003. [Google Scholar]
- Sanjobo N, Frich JC, Fretheim A. Barriers and facilitators to patients’ adherence to antiretroviral treatment in Zambia: A qualitative study. SAHARA J: Journal of Social Aspects of HIV/AIDS Research Alliance. 2008;5(3):136–143. doi: 10.1080/17290376.2008.9724912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sen A. Poverty and famines: An essay on entitlement and deprivation. New York, NY: Oxford University Press; 1981. [Google Scholar]
- Singer AW, Weiser SD, McCoy SI. Does food insecurity undermine adherence to antiretroviral therapy? A systematic review. AIDS and Behavior. 2015;19(8):1510–1526. doi: 10.1007/s10461-014-0873-1. [DOI] [PubMed] [Google Scholar]
- Skovdal M, Campbell C, Nhongo K, Nyamukapa C, Gregson S. Contextual and psychosocial influences on antiretroviral therapy adherence in rural Zimbabwe: Towards a systematic framework for programme planners. International Journal of Health Planning and Management. 2011;26(3):296–318. doi: 10.1002/hpm.1082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steptoe A. The links between stress and illness. Journal of Psychosomatic Research. 1991;35(6):633–644. doi: 10.1016/0022-3999(91)90113-3. [DOI] [PubMed] [Google Scholar]
- Stringer JS, Zulu I, Levy J, Stringer EM, Mwango A, Chi BH, Sinkala M. Rapid scale-up of antiretroviral therapy at primary care sites in Zambia: Feasibility and early outcomes. Journal of American Medical Association. 2006;296(7):782–793. doi: 10.1001/jama.296.7.782. doi:296/7/782. [DOI] [PubMed] [Google Scholar]
- Tirivayi N, Groot W. Health and welfare effects of integrating AIDS treatment with food assistance in resource constrained settings: A systematic review of theory and evidence. Social Science and Medicine. 2011;73(5):685–692. doi: 10.1016/j.socscimed.2011.06.056. [DOI] [PubMed] [Google Scholar]
- Tirivayi N, Koethe JR, Groot W. Clinic-based food assistance is associated with increased medication adherence among HIV-infected adults on long-term antiretroviral therapy in Zambia. Journal of AIDS & Clinical Research. 2012;3(7):171. doi: 10.4172/2155-6113.1000171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomlinson M, Rohleder P, Swartz L, Drimie S, Kagee A. Broadening psychology’s contribution to addressing issues of HIV/AIDS, poverty and nutrition: Structural issues as constraints and opportunities. Journal of Health Psychology. 2010;15(7):972–981. doi: 10.1177/1359105310371399. [DOI] [PubMed] [Google Scholar]
- Volk JE, Koopman C. Factors associated with condom use in Kenya: A test of the health belief model. AIDS Education and Prevention. 2001;13(6):495–508. doi: 10.1521/aeap.13.6.495.21438. [DOI] [PubMed] [Google Scholar]
- Ware NC, Idoko J, Kaaya S, Biraro IA, Wyatt MA, Agbaji O, Bangsberg DR. Explaining adherence success in sub-Saharan Africa: An ethnographic study. PLoS Medicine. 2009;6(1):e11. doi: 10.1371/journal.pmed.1000011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiser S, Wolfe W, Bangsberg D, Thior I, Gilbert P, Makhema J, Marlink R. Barriers to antiretroviral adherence for patients living with HIV infection and AIDS in Botswana. Journal of Acquired Immune Deficiency Syndromes. 2003;34(3):281–288. doi: 10.1097/00126334-200311010-00004. [DOI] [PubMed] [Google Scholar]
- Weiser SD, Bukusi EA, Steinfeld RL, Frongillo EA, Weke E, Dworkin SL, Cohen CR. Shamba maisha: Randomized controlled trial of an agricultural and finance intervention to improve HIV health outcomes. AIDS. 2015;29(14):1889–1894. doi: 10.1097/QAD.0000000000000781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiser SD, Palar K, Frongillo EA, Tsai AC, Kumbakumba E, Depee S, Bangsberg DR. Longitudinal assessment of associations between food insecurity, antiretroviral adherence and HIV treatment outcomes in rural Uganda. AIDS. 2014;28(1):115–120. doi: 10.1097/01.aids.0000433238.93986.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiser SD, Tuller DM, Frongillo EA, Senkungu J, Mukiibi N, Bangsberg DR. Food insecurity as a barrier to sustained antiretroviral therapy adherence in uganda. PloS ONE. 2010;5(4):e10340. doi: 10.1371/journal.pone.0010340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiser SD, Young SL, Cohen CR, Kushel MB, Tsai AC, Tien PC, Bangsberg DR. Conceptual framework for understanding the bidirectional links between food insecurity and HIV/AIDS. American Journal of Clinical Nutrition. 2011;94(6):1729S–1739S. doi: 10.3945/ajcn.111.012070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wringe A, Roura M, Urassa M, Busza J, Athanas V, Zaba B. Doubts, denial and divine intervention: Understanding delayed attendance and poor retention rates at a HIV treatment programme in rural Tanzania. AIDS Care. 2009;21(5):632–637. doi: 10.1080/09540120802385629. [DOI] [PubMed] [Google Scholar]
- Young S, Wheeler AC, McCoy SI, Weiser SD. A review of the role of food insecurity in adherence to care and treatment among adult and pediatric populations living with HIV and AIDS. AIDS and Behavior. 2014;18(Suppl 5):S505–S515. doi: 10.1007/s10461-013-0547-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zak-Place J, Stern M. Health belief factors and dispositional optimism as predictors of STD and HIV preventive behavior. Journal of American College Health. 2004;52(5):229–236. doi: 10.3200/JACH.52.5.229-236. [DOI] [PubMed] [Google Scholar]


