Abstract
PURPOSE
To compare the visual, refractive, keratometric, topographic, and pachymetric outcomes of corneal collagen cross-linking (CXL) for progressive keratoconus following epithelial removal by transepithelial phototherapeutic keratectomy (PTK) or manual debridement.
METHODS
In this analysis, 339 eyes (78% male, 22% female) that had undergone CXL following manual epithelial debridement (n = 180) or ablation via PTK (n = 159) were evaluated preoperatively and at 6, 12, and 24 months postoperatively for uncorrected distance visual acuity (UDVA), corrected distance visual acuity (CDVA), maximum corneal keratometry, pachymetry, and spherical equivalent. The data were analyzed in a t test to evaluate the relative efficacy of each epithelial removal procedure.
RESULTS
Manual epithelial debridement and ablation via PTK produce equivalent changes for all variables at each time interval with the exception of maximum corneal keratometry at 6 months postoperatively, for which PTK exhibited a significantly improved (flatter) result. This difference was present but not statistically significant at 12 and 24 months postoperatively.
CONCLUSIONS
Prior to CXL, both manual epithelial debridement and ablation via PTK result in equivalent visual, refractive, and keratometric outcomes up to 24 months postoperatively.
The efficacy of corneal collagen cross-linking (CXL) is highly dependent on the ability of the riboflavin solution to saturate the corneal stroma.1 In the past, epithelial debridement has been performed using various methods (eg, scalpel or rotating brush) or by briefly exposing the epithelium to ethyl alcohol, followed by gentle rubbing by a cellulose sponge. The success of manual debridement is dependent on the ability of the surgeon to completely remove the epithelium while leaving Bowman’s membrane undamaged. The use of sharp instruments has been reported to debride unevenly and damage Bowman’s membrane.2 In contrast, the use of alcohol has been shown to allow for even debridement of the epithelium without compromising Bowman’s membrane. However, it has also been reported that alcohol may have cytotoxic effects on keratocytes,3 which subsequently would be reduced in number following the exposure to ultraviolet-A (UVA) light.1 Although CXL can be performed without epithelial removal, the procedure requires a longer time for the riboflavin to fully saturate the cornea and has been shown to be significantly less effective.1,4
Excimer laser transepithelial phototherapeutic keratectomy (PTK), which is frequently used as a method for eliminating superficial corneal pathology, has also been employed as a method for removing the epithelial layer prior to CXL.5 In addition to being used to ablate keratoconic nodules,6 employing PTK for epithelial ablation may result in better visual acuity. A directional but not significant improvement in visual outcomes following CXL with PTK has been reported,7 and other research has shown a statistically significant improvement in uncorrected distance visual acuity (UDVA) and corrected distance visual acuity (CDVA) and reduction in astigmatism.8
The current study was a retrospective analysis of outcomes for patients who underwent CXL following epithelial debridement via manual removal versus PTK for progressive keratoconus.
PATIENTS AND METHODS
This retrospective analysis included 339 eyes (78% male, 22% female) with an average age of 24.4 years (range: 10 to 70 years) who were diagnosed as having progressive keratoconus. All patients were informed about CXL and consented to enroll in a clinical trial (NCT01081561). The procedures occurred between February 2010 and May 2015. The protocol followed for treatment of these patients was the Dresden technique. This was approved by the Western Institutional Review Board.
The inclusion criteria for the study were as follows: diagnosis of progressive keratoconus, CDVA worse than 20/20, and minimum corneal thickness greater than 400 μm. In determining progression of keratoconus, it is important to evaluate the entire clinical status of the cornea. For this research study, we defined progression of keratoconus as one or more of the following: a 1.00 diopter (D) increase in maximum keratometry (K), a reduction in the thinnest point on anterior chamber optical coherence tomography corneal thickness of 10 μm or greater, and/or a 1.00 D increase in refractive sphere or cylinder over 12 months. Patients were excluded if there were any of the following: no evidence of progression over a 1-year period, central corneal scarring causing reduced vision, history of herpetic eye disease, or the patient was pregnant or nursing.
A complete preoperative work-up was performed, including review of medical and ophthalmologic history with prior corneal records, slit-lamp examination, dilated ophthalmoscopy, and intraocular pressure. Measurement of the following variables was recorded: UDVA, CDVA, maximum K via videokeratography (TMS 4; Tomey, Nagoya, Japan), and corneal pachymetry as measured by optical coherence tomography (Optovue, Fremont, CA). UDVA and CDVA were converted into logMAR scale values for analytic feasibility and reported as such.9 All eyes were anesthetized with instillation of proparacaine hydrochloride 0.5% (Bausch & Lomb, Rochester, NY).
In the PTK group (180 eyes), epithelial removal was performed via PTK set at 50 μm with a 6.5-mm diameter using the VISX Star S4 excimer laser (Advanced Medical Optics, Santa Ana, CA), which was additionally blended out by 2.7 mm. Afterward, the diameter was manually extended to 9 mm using a Maloney spatula.
In the manual debridement group (159 eyes), manual epithelial debridement was performed by exposing the eye to 20% ethyl alcohol in a 9-mm ring for 40 seconds, after which the alcohol was washed away and a cellulose sponge or blunt spatula was used to remove the epithelial tissue.
The CXL protocol followed was similar to the initial in vivo research results from 2003.10 Following debridement, the cornea was saturated with topical riboflavin (0.1% riboflavin, 1.1% hydroxymethylcellulose in solution; PeschkeMeditrade GmbH, Huenenberg, Switzerland) instilled every 2 minutes for 30 minutes. Corneal pachymetry was used to ensure a thickness of at least 400 μm. All patients were taken to the slit lamp to verify corneal saturation with riboflavin and anterior chamber flare. Patients then underwent CXL with continued instillation of riboflavin every 2 minutes and exposure to UVA irradiation (PeschkeMeditrade GmbH) at 3 mW/cm2 for 30 minutes.
Postoperatively, patients were treated with a topical antibiotic and bandaged with a soft contact lens, which they were instructed to wear until the epithelium healed, usually from 4 to 7 days. The patient was also given nonsteroidal anti-inflammatory drops, non-preserved artificial tears, and oral pain medication (if necessary). Patients were instructed to begin a course of prednisolone acetate at day 5. Postoperative examinations were conducted at day 1, week 1, and at months 1, 3, 6, 12, and 24 and included UDVA, CDVA, videokeratography, corneal pachymetry, manifest refraction, and slit-lamp examination.
Data from each examination at each time period were tabulated in Microsoft Excel (Microsoft Corporation, Redmond, WA) and later processed with SAS (SAS Institute, Cary, NC) software. Differences between each examination measurement and the corresponding preoperative measurement were calculated. Those differences were then compared using a Student’s t test for variables that were normally distributed and a Wilcoxon test for variables that were not normally distributed.
RESULTS
Table A (available in the online version of this article) lists the preoperative demographics of the patients. Prior to CXL, patients in both groups showed equivalent UDVA, CDVA, pachymetry, and spherical equivalent. However, the patient groups differed on maximum corneal K: the PTK group averaged 51.5 ± 5.0 D, whereas the manual debridement group averaged 50.5 ± 5.4 D (P = .05). All patients exhibited improvement in all measured variables after CXL.
With regard to the PTK group, patients improved on each measured variable at all follow-up examinations compared to the average preoperative measurement. At the preoperative examination, the average UDVA for this group was 0.87 ± 0.52 logMAR (20/148 Snellen), and this value improved to 0.67 ± 0.49 logMAR (20/94 Snellen) at 6 months (P < .001), 0.65 ± 0.42 logMAR (20/89 Snellen) at 12 months (P < .001), and 0.65 ± 0.41 logMAR (20/89 Snellen) at 24 months (P < .01) (Figure 1). There was a corresponding improvement in average CDVA: 0.33 ± 0.25 logMAR (20/43 Snellen) preoperatively, 0.27 ± 0.19 logMAR (20/37 Snellen) at 6 months (P < .001), 0.22 ± 0.18 logMAR (20/30 Snellen) at 12 months (P < .001), and 0.23 ± 0.20 logMAR (20/34 Snellen) at 24 months (P < .05) (Figure 2). Maximum K improved significantly over the course of the study by decreasing from 51.5 ± 5.0 D preoperatively to 50.0 ± 5.3 D at 24 months postoperatively (P < .05) (Figure 3). The corneas initially thinned following the procedure and eventually thickened to 11 μm less than their preoperative thickness, from 451 ± 45 to 440 ± 4 μm at 24 months (P < .001) (Figure 4). Spherical equivalent also improved significantly over the course of the study, from −3.80 ± 3.90 to −2.50 ± 3.10 D at 24 months (P < .05) (Figure 5).
Figure 1.
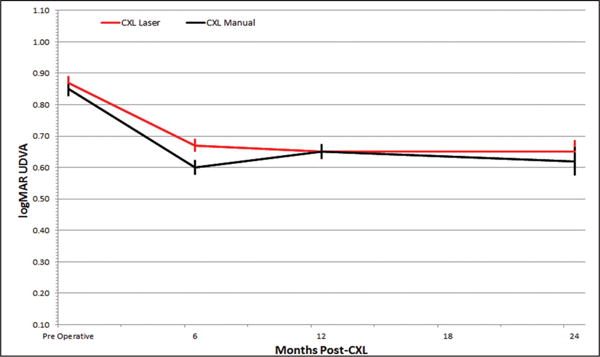
The improvement in logMAR uncorrected distance visual acuity (UDVA) for all patients was significant for both groups at each time interval compared to the respective preoperative average. The difference between the groups remained non-significant. CXL = corneal collagen cross-linking
Figure 2.
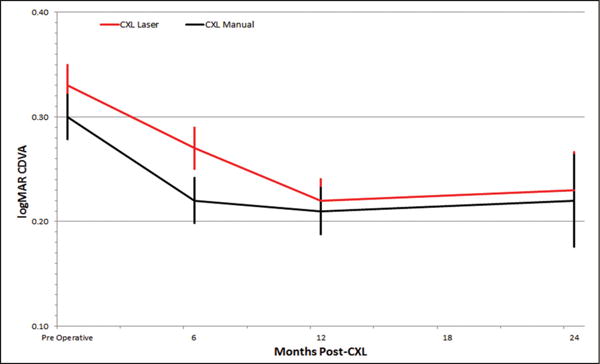
The improvement in logMAR corrected distance visual acuity (CDVA) follows a similar trajectory as uncorrected distance visual acuity. Improvement for both groups was significant at each time interval, and the groups never exhibited significant differences with respect to each other. CXL = corneal collagen cross-linking
Figure 3.
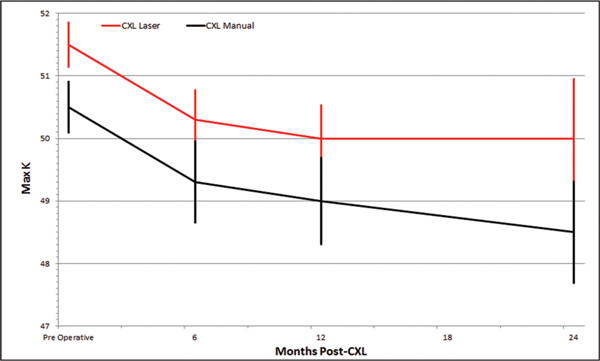
Maximum corneal keratometry (K) decreased significantly over the course of the study, but this decrease was only significant for the phototherapeutic keratectomy group at the 6-month time interval. CXL = corneal collagen cross-linking
Figure 4.

Corneal pachymetry decreased significantly over the course of the study despite a slight increase in the second half of the study. CXL = corneal collagen cross-linking
Figure 5.
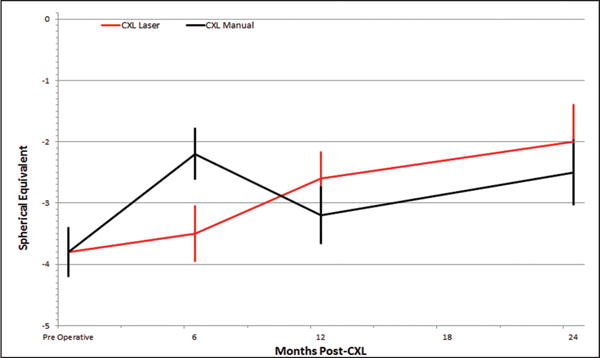
Spherical equivalent improved significantly for both groups at each time interval with respect to their average preoperative values. At no time interval did one group vary significantly on this value. CXL = corneal collagen cross-linking
As with the PTK group, the manual debridement group exhibited similar improvement in UDVA, from 0.85 ± 0.52 logMAR (20/142 Snellen) to 0.62 ± 0.51 logMAR (20/83 Snellen) at 24 months (P = .004). The CDVA also improved, but nonsignificantly from 0.30 ± 0.026 logMAR (20/40 Snellen) to 0.22 ± 0.25 logMAR (20/33 Snellen) at 24 months (P > .10). Maximum K for these patients improved by decreasing from 50.5 ± 5.4 D preoperatively to 48.5 ± 5.4 D at 24 months postoperatively (P < .05). Pachymetric values also followed a similar trend by first thinning from 455 ± 58 to 440 ± 53 μm at 12 months (P < .001) and later thickening to 449 ± 57 μm (P < .001) by 24 months postoperatively. Spherical equivalent improved significantly over the course of the study, from −3.80 ± 3.90 to −2.50 ± 3.10 D at 24 months (P = .026).
In comparing between the groups, the data reflect that both procedures yield equivalent refractive and topographic outcomes, with the exception of maximum K at 6 months postoperatively. When analyzed in a t test, the PTK group had decreased maximum K significantly more than the manual debridement group (1.3 ± 3.5 compared to 0.5 ± 3.3 mm) at the 6-month interval (P = .03) (Table 1). Although our initial study, which was published in 2013 and contained 77 eyes, showed that there was a significant flattening of maximum K for the PTK group compared to the manual debridement group at 12 months, in the current study of 339 eyes, the data suggest no such difference at 12 or 24 months.11 The changes for each other recorded variable at every other time interval were not significantly different.
TABLE 1.
Comparisons of the Change at 6, 12, and 24 Months Between the Two Groups
| Parameter | 6 Months | 12 Months | 24 Months |
|---|---|---|---|
| UDVA (logMAR) | |||
| PTK | 0.18 ± 0.37 | 0.19 ± 0.40 | 0.17 ± 0.33 |
| Manual debridement | 0.14 ± 0.42 | 0.21 ± 0.37 | 0.19 ± 0.38 |
| P | > .10 | > .10 | > .10 |
| CDVA (logMAR) | |||
| PTK | 0.10 ± 0.20 | 0.08 ± 0.16 | 0.05 ± 0.12 |
| Manual debridement | 0.04 ± 0.18 | 0.06 ± 0.20 | 0.02 ± 0.16 |
| P | > .10 | > .10 | > .10 |
| Pachymetry (μm) | |||
| PTK | 17 ± 25 | 24 ± 42 | 22 ± 29 |
| Manual debridement | 18 ± 28 | 24 ± 42 | 22 ± 29 |
| P | > .10 | > .10 | > .10 |
| Spherical equivalent (D) | |||
| PTK | −1.10 ± 3.30 | −1.20 ± 2.90 | −1.10 ± 3.40 |
| Manual debridement | −1.40 ± 4.20 | −1.30 ± 2.70 | −1.00 ± 2.20 |
| P | > .10 | > .10 | > .10 |
| Maximum K (D) | |||
| PTK | 1.30 ± 3.50 | 1.20 ± 2.60 | 1.10 ± 2.70 |
| Manual debridement | 0.50 ± 3.30 | 1.00 ± 3.20 | 1.70 ± 3.10 |
| P | > .003 | > .10 | > .10 |
UDVA = uncorrected distance visual acuity; PTK = phototherapeutic keratectomy; CDVA = corrected distance visual acuity; D = diopters; K = keratometry
DISCUSSION
This research investigated the comparison of visual, keratometric, topographic, pachymetric, and spherical equivalent outcomes of CXL for progressive keratoconus performed with epithelial ablation via PTK versus manual debridement. Our results indicate that epithelial ablation via PTK yields similar outcomes to manual debridement. For almost every data point at every time interval, corneas that had been deepithelialized via PTK underwent a similar degree of topographic and refractive change compared to those that underwent manual debridement. Further, there is some evidence to suggest that PTK may reduce astigmatism by smoothing the corneal surface: at the 6-month postoperative examination, the PTK group had reduced corneal steepness compared to the manual debridement group. In this case, consistent with a doughnut-shaped model of the epithelium,7,12 we concur with the hypothesis that epithelial ablation via PTK removes more stromal tissue from the central cone of the keratoconic cornea, thereby implying that PTK initially flattens the cornea more than manual debridement, but that change was not demonstrated after the 6-month visit. This is likely because even though the keratoconic cornea has a thinner epithelium (usually < 50 μm), the PTK ablation only removes a negligible amount of stromal tissue and the consequent decrease in maximum K is slight. If removal of corneal stroma were a significant concern, this risk could potentially be mitigated by combining PTK with optical coherence tomography pachymetry maps to customize the epithelial ablation so that minimal stromal tissue is ablated.12–14
Therefore, the results of the current study add to previously published research from Kymionis et al.8 and Kapasi et al.7,15 by suggesting that, although PTK is as effective as manual debridement preceding CXL, it induces no significant and lasting visual, topographic, or refractive benefits (Table 2). Although this difference may be accounted for to some degree by a difference in methodology, it may also be possible that the increased number of eyes in the current study allowed for the trend to be elucidated. Regardless, all studies support the conclusion that PTK is effective at ablating epithelial tissue prior to CXL without inducing adverse events, a finding that has been found in 11 eyes at 3 years postoperatively and 7 eyes at 4 years postoperatively.16
TABLE 2.
Comparison of Study Outcomes for PTK vs Manual Debridement
| PTK
|
Manual Debridement
|
|||||
|---|---|---|---|---|---|---|
| Parameter | 6 Months | 12 Months | 24 Months | 6 Months | 12 Months | 24 Months |
| UDVA (logMAR) | < .001 | < .001 | .008 | .002 | < .001 | .004 |
| CDVA (logMAR) | < .001 | < .001 | .032 | .060 | .014 | > .10 |
| Pachymetry (μm) | < .001 | < .001 | < .001 | < .001 | < .001 | < .001 |
| Spherical equivalent (D) | .003 | < .001 | .007 | .022 | .001 | .026 |
| Maximum K (D) | < .001 | < .001 | .038 | > .10 | .022 | .003 |
PTK = phototherapeutic keratectomy; UDVA = uncorrected distance visual acuity; CDVA = corrected distance visual acuity; D = diopters; K = keratometry
The study is limited in its power because it is a retrospective analysis. Although both groups had similar preoperative UDVA, CDVA, pachymetry, and spherical equivalent, by chance, the PTK group had a higher preoperative corneal curvature than did the manual debridement group (P = .05). Although unlikely, it could be that the procedure is more effective for those patients with steeper corneas, thereby possibly influencing our interpretation. Furthermore, another potential limitation of the PTK procedure could be that increased ablation of the cornea, specifically of Bowman’s membrane, could result in a higher intensity CXL treatment,17 or damage to the cornea from UVA exposure.5 If this were established by later research, the Dresden CXL protocol could be amended by decreasing the length of exposure to UVA light.
Supplementary Material
Acknowledgments
Supported in part by The Eye Defects Research Foundation, Inc., Los Angeles, CA.
Footnotes
National Institutes of Health Clinical Trial NCT01081561.
The authors have no financial or proprietary interest in the materials presented herein.
AUTHOR CONTRIBUTIONS
Study concept and design (RNG, XL, YSR); data collection (RNG, YSR); analysis and interpretation of data (RNG, JBM, DNG, XL, YSR); writing the manuscript (RNG, JBM, DNG); critical revision of the manuscript (RNG, XL, YSR); statistical expertise (DNG, XL); administrative, technical, or material support (RNG); supervision (RNG, XL, YSR)
Contributor Information
Ronald N. Gaster, Cornea Eye Institute, Beverly Hills, California.
J. Ben Margines, Cornea Eye Institute, Beverly Hills, California.
David N. Gaster, Cornea Eye Institute, Beverly Hills, California
Xiaohui Li, Institute for Translational Genomics and Population Sciences, Los Angeles Biomedical Research Institute at Harbor-UCLA Medical Center, Torrance, California.
Yaron S. Rabinowitz, Cornea Eye Institute, Beverly Hills, California (RNG, JBM, DNG, YSR).
References
- 1.Wollensak G, Iomdina E. Biomechanical and histological changes after corneal crosslinking with and without epithelial debridement. J Cataract Refract Surg. 2009;35:540–546. doi: 10.1016/j.jcrs.2008.11.036. [DOI] [PubMed] [Google Scholar]
- 2.Ghoreishi M, Attarzadeh H, Tavakoli M, et al. Alcohol-assisted versus mechanical epithelium removal in photorefractive keratectomy. J Ophthalmic Vis Res. 2010;5:223–227. [PMC free article] [PubMed] [Google Scholar]
- 3.Campos M, Raman S, Lee M, McDonnell P. Keratocyte loss after different methods of de-epithelialization. Ophthalmology. 1994;101:890–894. doi: 10.1016/s0161-6420(94)31242-5. [DOI] [PubMed] [Google Scholar]
- 4.Leccisotti A, Islam T. Transepithelial corneal collagen cross-linking in keratoconus. J Refract Surg. 2010;26:942–948. doi: 10.3928/1081597X-20100212-09. [DOI] [PubMed] [Google Scholar]
- 5.Kymionis G, Grentzelos M, Karavitaki A, et al. Transepithelial phototherapeutic keratectomy using a 213-nm solid-state laser system followed by corneal collagen cross-linking with riboflavin and UVA Iiradiation. J Ophthalmol. 2010;2010:146543. doi: 10.1155/2010/146543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Elsahn A, Rapuano C, Antunes V, Abdalla Y, Cohen E. Excimer laser phototherapeutic keratectomy for keratoconus nodules. Cornea. 2009;28:144–147. doi: 10.1097/ICO.0b013e31818526b8. [DOI] [PubMed] [Google Scholar]
- 7.Kapasi M, Baath J, Mintsioulis G, Jackson W, Baig K. Phototherapeutic keratectomy versus mechanical epithelial removal followed by corneal collagen crosslinking for keratoconus. Can J Ophthalmol. 2012;47:344–347. doi: 10.1016/j.jcjo.2012.03.046. [DOI] [PubMed] [Google Scholar]
- 8.Kymionis G, Grentzelos M, Kounis G, Diakonis V, Limnopoulou A, Panagopoulou S. Combined transepithelial phototherapeutic keratectomy and corneal collagen cross-linking for progressive keratoconus. Ophthalmology. 2012;119:1777–1784. doi: 10.1016/j.ophtha.2012.03.038. [DOI] [PubMed] [Google Scholar]
- 9.Bailey I, Lovie J. New design principles for visual acuity letter charts. Optom Vis Sci. 1976;53:740–745. doi: 10.1097/00006324-197611000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Wollensak G, Spoerl E, Seiler T. Riboflavin/ultraviolet-a–induced collagen crosslinking for the treatment of keratoconus. Am J Ophthalmol. 2003;135:620–627. doi: 10.1016/s0002-9394(02)02220-1. [DOI] [PubMed] [Google Scholar]
- 11.Canedo A, Gaster R, Rabinowitz Y. Comparison of laser-assisted removal of epithelium to mechanical debridement in corneal cross-linking for progressive keratoconus: 12-months results. Invest Ophthalmol Vis Sci. 2013;54:3112. [Google Scholar]
- 12.Reinstein D, Archer T, Gobbe M. Corneal epithelial thickness profile in the diagnosis of keratoconus. J Refract Surg. 2009;25:604–610. doi: 10.3928/1081597X-20090610-06. [DOI] [PubMed] [Google Scholar]
- 13.Rocha KM, Perez-Straziota CP, Stulting RD, Randleman JB. Epithelial and stromal remodeling after corneal collagen cross-linking evaluated by spectral-domain OCT. J Refract Surg. 2014;30:122–127. doi: 10.3928/1081597X-20140120-08. [DOI] [PubMed] [Google Scholar]
- 14.Rocha KM, Perez-Straziota CE, Stulting RD, Randleman JB. Spectral-domain OCT analysis of regional epithelial thickness profiles in keratoconus, postoperative corneal ectasia, and normal eyes. J Refract Surg. 2013;29:173–179. doi: 10.3928/1081597X-20130129-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kapasi M, Dhaliwal A, Mintsioulis G, Jackson W, Baig K. Long-term results of phototherapeutic keratectomy versus mechanical epithelial removal followed by corneal collagen cross-linking for keratoconus. Cornea. 2016;35:157–161. doi: 10.1097/ICO.0000000000000679. [DOI] [PubMed] [Google Scholar]
- 16.Kymionis G, Grentzelos M, Kankariya V, et al. Long-term results of combined transepithelial phototherapeutic keratectomy and corneal collagen crosslinking for keratoconus: Cretan protocol. J Cataract Refract Surg. 2014;40:1439–1445. doi: 10.1016/j.jcrs.2014.01.040. [DOI] [PubMed] [Google Scholar]
- 17.Alessio G, L’Abbate M, Furino C, Sborgia C, La Tegola M. Confocal microscopy analysis of corneal changes after photorefractive keratectomy plus cross-linking for keratoconus: 4-year follow-up. Am J Ophthalmol. 2014;158:476–484. doi: 10.1016/j.ajo.2014.05.024. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


