Abstract
Background
Data on the association between HIV stigma and drug use are scarce, but some research suggests that internalized HIV stigma may be associated with increased drug use and that this association may be at least partially mediated by emotion dysregulation. We sought to test this hypothesis with event-level data to more accurately tease out the co-occurrence of these phenomena.
Methods
We utilized multivariate multilevel analysis to test an autoregressive cross-lagged path model of the direct and indirect effects of internalized HIV stigma and emotion dysregulation on non-prescription stimulant drug use in a sample of 52 HIV-positive gay and bisexual men who completed a 21-day, twice-daily ecological momentary assessment study.
Results
As hypothesized, we observed significant concurrent effects of internalized HIV stigma on emotion dysregulation as well as autoregressive associations of internalized HIV stigma and emotion dysregulation with themselves across the day. Furthermore, findings revealed direct effects of internalized HIV stigma on later emotion dysregulation and increased likelihood of stimulant use, but no direct effect of emotion dysregulation on stimulant use.
Conclusions
Internalized HIV stigma appears to exert a direct risk-enhancing effect on the likelihood of stimulant drug use and does not appear to do so through emotion dysregulation. Future research is needed to more carefully examine distinct affective experiences and regulation strategies to better understand what mechanism links internalized HIV stigma with drug use behaviors.
Keywords: Minority stress, emotion dysregulation, gay and bisexual men, ecological momentary assessment, stimulant use, drug use
1. Introduction
HIV stigma has several well-documented associations with adverse mental health outcomes for people living with HIV, including depression,1–3 anxiety,4,5 general distress,6 and low self-esteem.7 Internalized HIV stigma, whereby negative societal attitudes become directed towards oneself, has been shown to be particularly problematic for its effects on mental health and health behaviors among both general samples of HIV-positive individuals 7–12 and among HIV-positive gay and bisexual men (GBM), specifically.13–18 In particular, rates of drug use and related problems are disproportionately higher for GBM in general as compared to their heterosexual peers19,20 and, among GBM, disproportionately higher among HIV-positive compared to HIV-negative GBM.21 Among GBM, stimulant drugs such as cocaine/crack and crystal methamphetamine are among the most frequently reported illicit drugs used,22–26 and consequences of their use have included greater HIV transmission risk behavior and lower antiretroviral medication adherence.27–30 Furthermore, stimulants such as cocaine/crack and crystal methamphetamine are known to have significant HIV-related health consequences, such as increased viral replication,31–33 inflammation,34 and quickened progression to AIDS.35
One prominent model for understanding the disproportionate burden of negative health outcomes observed among GBM is the minority stress model.36–39 In both theoretical and empirical work, the link between sexual minority stress and behavioral outcomes such as drug use among GBM has been posited to operate through the mediating factor of emotion dysregulation.30,36,40,41 Prior research has shown consistent effects of both sexual minority and HIV-related stigma on emotion dysregulation for HIV-positive GBM,18 and that emotion dysregulation mediates the effect of these forms of stigma on negative mental health, sexual risk behavior, and substance use outcomes.18,37,42 As such, there is a growing empirical basis for theorizing that stigma may lead to behaviors such as drug use through emotion dysregulation, whereby an individual experiences both behavioral disinhibition as well as a drive to seek such behavioral experiences in order to improve positive mood or distract from negative mood.
While a growing body of evidence has shown the links between HIV stigma and emotion dysregulation as cited above, research on HIV stigma’s direct association with substance use has been relatively scarce and has focused mostly on heterosexual samples.2,43–45 We are aware of only two studies looking at the association between HIV stigma and substance use in GBM: one which observed a non-significant association between HIV stigma and alcohol dependency,16 and another study which found that, among young Black GBM, those with greater HIV stigma reported higher odds of having sex while high or intoxicated.46 Further investigation in this area is therefore needed, especially given the elevated rates of drug use among HIV-positive GBM, the link between emotion dysregulation and stimulant use,25 and the detrimental effects of use on various HIV-related health outcomes.25,47
Most of the aforementioned research on the mental and behavioral health effects of HIV stigma has focused on links between global or enduring levels of HIV stigma and aggregate outcomes (e.g., depression, substance use dependency). However, a more temporally-precise understanding of the co-occurrence of HIV stigma and health outcomes has been provided by two recent studies looking at day-level associations. In the first study, Fazeli et al. showed a positive association between enacted and internalized HIV stigma using a 7-day experience sampling design.48 In the second study, Rendina et al. showed a positive effect of situationally-fluctuating levels of internalized HIV stigma measured once daily on negative affect and emotion dysregulation using a 21-day ecological momentary assessment (EMA) design.49 No study of which we aware has yet looked at event-level associations between HIV stigma and drug use, though three recent daily diary studies on sexual minority stigma among GBM—one showing that daily sexual minority stigma was associated with increased negative affect,50 one showing that individual- level sexual minority stigma was associated with increased odds of alcohol and tobacco use on a given day,51 and another showing that daily sexuality-based discrimination was associated with both daily nicotine and substance use52—further support the possibility that daily fluctuations in levels of internalized HIV stigma may be associated at an event-level with the experience of emotion dysregulation and drug use.
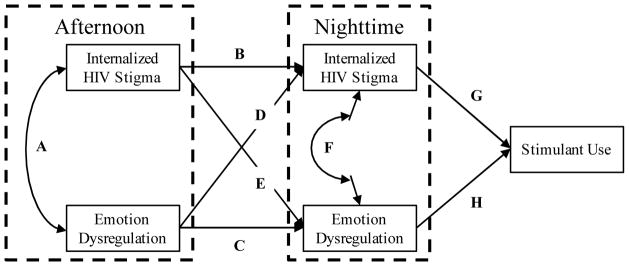
Building upon the existing data, the purpose of the present study was to examine an event-level, autoregressive cross-lagged path model of internalized HIV stigma, emotion dysregulation, and use of non-prescription stimulant drugs among HIV-positive GBM participating in a twice-daily, 21-day EMA study. As depicted in Figure 1, we hypothesized the following: (1) concurrent effects whereby afternoon levels of internalized HIV stigma would be positively associated with afternoon levels of emotion dysregulation (Path A) and the same would be true for the nighttime measurements (Path F); (2) autoregressive effects whereby afternoon levels of internalized HIV stigma would be positively associated with nighttime levels of internalized HIV stigma (Path B) and the same would be true for emotion dysregulation (Path C); (3) a positive cross-lagged effect of afternoon levels of internalized HIV stigma on nighttime levels of emotion dysregulation (Path E); (4) a positive direct effect of nighttime levels of emotion dysregulation on subsequent stimulant drug use (Path H); and (5) positive indirect effects (i.e., mediation) of afternoon internalized HIV stigma on stimulant drug use through nighttime emotion dysregulation (Path E–H). Based on the proposed theoretical model, we expected that internalized HIV stigma would be associated with higher levels of subsequent emotion dysregulation, but that the reverse would not be true—that is, that earlier experiences of emotion dysregulation would not be associated with later experiences of internalized HIV stigma (Path D). Similarly, based on prior work, we expected the effect of internalized HIV stigma on stimulant drug use would be through emotion dysregulation, so we expected no direct effect of internalized HIV stigma on stimulant drug use (Path G). However, this was not tested as formal hypotheses due to the fact that a null hypothesis cannot be supported.
Figure 1.
This figure displays the specific paths being tested within the autoregressive path model that are used in text to reference specific hypotheses regarding concurrent associations (curved paths A and F), autoregressive effects (paths B and C), cross-lagged effects (paths D and E), and the direct effects on subsequent stimulant use (paths G and H).
2. Method
Data for this paper were drawn from 52 participants enrolled in day2day, a 21-day twice-daily EMA study of HIV-positive GBM in New York City that was conducted in late 2015 and early 2016.
2.1 Participants and Procedures
Men were recruited using several online methods, including advertisements on social media websites and sexual networking apps. Eligibility for the study was assessed preliminarily over the phone and was confirmed during the in-person appointment. Participants were deemed eligible if they: (1) were aged 18 or older; (2) were cisgender male; (3) were HIV-positive and able to verify both their HIV status and an active prescription for antiretroviral therapy; (4) identified as gay or bisexual; (5) reported 2 or more days of club drug (i.e., crack, crystal meth, cocaine, ecstasy, ketamine, or GHB) in the prior 30 days; (6) reported 1 or more acts of HIV transmission risk behavior (i.e., condomless anal sex with an HIV-negative/unknown partner, excluding main partners who were on PrEP) in the prior 30 days; and (7) had daily access to the internet via smartphone.
Eligible participants were sent a link to complete an online survey from home that lasted approximately one hour, after which participants completed an in-person assessment at our research center. During this visit, participants were trained on how to use the twice-daily EMA system. Beginning the day after the baseline assessment and continuing for 21 days, participants were sent unique links twice a day—one at 12pm that expired at 4pm (i.e., the ‘afternoon’ measurement) and one at 8pm that expired at midnight (i.e., the ‘nighttime’ measurement)—that took them to the online EMA system within Qualtrics. Both the afternoon and nighttime surveys contained the emotion dysregulation and HIV stigma measures, providing two time points of measurement for each; because it often occurs in the late night and early morning, drug use was captured in the subsequent day’s afternoon survey and the data were later lagged back to the previous day. Participants were compensated $50 for the in-person assessment and could earn up to $42 dollars for completion of the EMA. All protocols were approved by the Institutional Review Board of The City University of New York (CUNY).
2.2 Measures
During each EMA survey, participants began by reporting on their emotiondysregulation, after which they reported on experiences of HIV-related stress.
2.2.1 Situational HIV Stigma
Participants were asked to complete a total of nine items that were adapted from several published measures on HIV-related stressors.53–56 Five items were used to capture situational experiences of internalized HIV stigma (e.g., “I’ve been feeling guilty because of my HIV status” and “I’ve been feeling emotionally upset or overwhelmed by my status”) as described in more detail elsewhere.49 Participants were asked to rate the extent to which they had experienced each in the past few hours on a scale from 1 (not at all) to 4 (completely). The order of the items was randomly displayed during each survey and the average across items was taken to calculate a score at each time point.
2.2.2 Situational Emotion Dysregulation
Situational experiences of emotion dysregulation were measured by responses to four items adapted from the Difficulties with Emotion Regulation Scale57 (e.g., “I’ve been experiencing my emotions as overwhelming,” “I’ve been having difficulty making sense of my feelings”). Participants were asked to rate the extent to which they had been experiencing each in the past few hours on a scale from 1 (not at all) to 4 (completely). The order of the items was randomly displayed during each survey and the average across items was taken to calculate a score at each time point. The scale has previously been shown to be significantly positively associated with validated measures of situational negative affect.49
2.2.3 Daily Drug Use
In each day’s afternoon survey, participants were asked about any substance use they had engaged in the prior day. Participants were provided with a list of drugs that included non-prescription stimulants (cocaine/crack and crystal meth), and were asked to respond to whether or not they had used these. When participants reported use of any drugs, they were asked at what time they first began using them—because we are focused on drug use as an outcome of nighttime reports of internalized HIV stigma and emotion dysregulation, we excluded reports of drug use prior to 8:00 p.m.
2.3 Statistical Analyses
Reports of HIV stigma and emotion dysregulation from each survey were disaggregated into a Level 2, grand-mean centered score corresponding to the individual’s average across all time points and a Level 1, person-centered score corresponding to the individual’s fluctuation from that average at each time point. We restructured the data by taking the “long” data (i.e., one row for each survey) and transposing the data such that the afternoon and nighttime reports for the same day were within the same row. We subsequently created a dichotomous indicator of daily stimulant use collected during the following day’s afternoon survey and lagged this variable back to the prior day’s reports of HIV stigma and emotion dysregulation. Multilevel modeling was conducted in Mplus Version 8.0 using random intercepts (i.e., TYPE = TWOLEVEL) with Bayesian estimation (i.e., ESTIMATOR = BAYES). The drug use outcome was specified as a categorical (i.e., dichotomous) outcome and modeled using the default probit regression. The use of Bayesian estimation allowed for the inclusion of all days where the afternoon survey was completed, even when the nighttime survey or the drug use report on the subsequent day were missing. Unlike standard multilevel modeling in which a single outcome is specified, the use of Mplus allowed for testing of a multivariate model in which all specified paths were estimated simultaneously. Level 1 effects were adjusted for the day of the EMA cycle centered at the middle day and whether or not the report was on a weekend (i.e., Friday, Saturday, or Sunday); Level 2 effects were adjusted for Black race, relationship status, and grand mean-centered age. We utilized model constraints to calculate coefficients and standard errors for indirect effects (i.e., the product of sequential direct paths). Mplus does not produce standard model fit statistics for multilevel models of this kind, and as such we rely solely on reporting the parameter estimates of the path coefficients.
3. Results
One of the 53 men in the study was missing demographic data and excluded from analyses, resulting in an analytic sample of 52 participants. The median number of surveys completed per participant was 35 (83.3% of sent)—median completion for both the afternoon and nighttime surveys was 17, and we analyzed a total of 784 days’ worth of data. Table 1 reports on the demographic characteristics of the sample, showing that most were men of color, gay-identified, single, and unemployed, and had completed some college but not a 4-year degree. The mean age was 38.6 and the average amount of time living with HIV was 10.6 years.
Table 1.
Demographic characteristics of the sample.
| n | % | |
|---|---|---|
| Race/Ethnicity | ||
| Black | 18 | 34.6 |
| Latino | 15 | 28.8 |
| White | 11 | 21.2 |
| Multiracial/Other | 8 | 15.4 |
| Sexual Orientation | ||
| Gay, queer, or homosexual | 46 | 88.5 |
| Bisexual | 6 | 11.5 |
| Employment Status | ||
| Full-time | 15 | 28.8 |
| Part-time | 7 | 13.5 |
| Unemployed | 30 | 57.7 |
| Highest Educational Attainment | ||
| High school diploma/GED or less | 9 | 17.3 |
| Some college or Associate’s degree | 29 | 55.8 |
| Bachelor’s or other 4-year degree | 9 | 17.3 |
| Graduate degree | 5 | 9.6 |
| Relationship Status | ||
| Single | 39 | 75.0 |
| Partnered | 13 | 25.0 |
| M | SD | |
|
|
||
| Age (Mdn = 35.0) | 38.6 | 10.3 |
| Years since HIV diagnosis (Mdn = 10.0) | 10.6 | 6.8 |
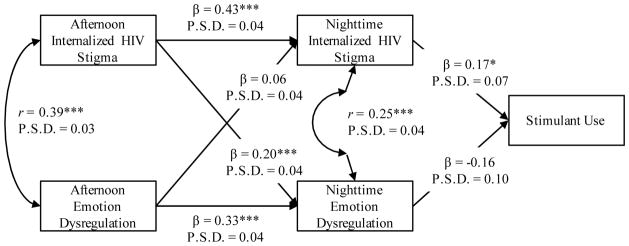
The unstandardized results of the model are presented within Table 2 and the Level 1 autoregressive cross-lagged portion of the model is represented graphically with standardized coefficients in Figure 2. Results confirmed our first set of hypotheses that there would be significant concurrent associations (curved paths A and F), with internalized HIV stigma and emotion dysregulation measured at the same time being significantly, positively correlated in both the afternoon and nighttime measurements. The findings also supported the second hypothesis regarding the autoregressive effects (paths B and C)—afternoon levels of internalized HIV stigma were significantly and positively associated with nighttime levels of internalized HIV stigma and the same was true for emotion dysregulation. The third hypothesis was supported (path E)—there was a significant cross-lagged effect of afternoon internalized HIV stigma on nighttime internalized HIV stigma. Although not a formal hypothesis, there was no cross-lagged association from afternoon emotion dysregulation to nighttime internalized HIV stigma (path D), as expected. We did not find support for our fourth hypothesis regarding a direct effect of nighttime emotion dysregulation on stimulant drug use (path H); contrary to our expectations, we did find a significant direct effect of nighttime internalized HIV stigma on stimulant drug use (path G). Given the lack of direct effect of nighttime emotion dysregulation on stimulant drug use, it was not surprising that we also did not find evidence for our fifth hypothesis regarding a significant indirect effect of afternoon internalized HIV stigma on stimulant drug use through nighttime emotion dysregulation (path E–H), B = −0.02, 95%CI[−0.10, 0.01].
Table 2.
Model results for the multilevel path analysis.
| Nighttime Internalized HIV Stigma | Nighttime Emotion Dysregulation | |||
|---|---|---|---|---|
|
|
|
|||
| B | 95%CI | B | 95%CI | |
| Fixed Components | ||||
| Level 1: Situational Level | ||||
| Intercept | −0.02 | [−0.04, 0.01] | −0.01 | [−0.03, 0.02] |
| Afternoon Internalized HIV Stigma | 0.42*** | [0.35, 0.49] | 0.23*** | [0.15, 0.31] |
| Afternoon Emotion dysregulation | 0.05 | [−0.01, 0.11] | 0.32*** | [0.25, 0.39] |
| Day of EMA cycle | 0.00 | [0.00, 0.00] | 0.00 | [−0.01, 0.00] |
| Weekend report (1 = yes) | 0.01 | [−0.03, 0.05] | −0.01 | [−0.05, 0.04] |
| Stimulant Use | ||||
|
|
||||
| B | 95%CI | |||
|
|
||||
| Fixed Components | ||||
| Level 1: Situational Level | ||||
| Intercept | −1.80*** | [−2.51, −1.28] | ||
| Nighttime Internalized HIV Stigma | 0.62* | [0.10, 1.19] | ||
| Nighttime Emotion dysregulation | −0.52 | [−1.18, 0.06] | ||
| Day of EMA cycle | −0.02 | [−0.05, 0.01] | ||
| Weekend report (1 = yes) | 0.02 | [−0.31, 0.36] | ||
| Level 2: Individual Level | ||||
| Average Internalized HIV Stigma | −0.02 | [−1.19, 1.15] | ||
| Average Emotion Dysregulation | −0.06 | [−1.48, 1.44] | ||
| Black race (1 = yes) | 0.36 | [−0.42, 1.14] | ||
| Relationship status (1 = partnered) | −0.15 | [−1.18, 0.83] | ||
| Age | 0.00 | [−0.03, 0.04] | ||
| Random Components | ||||
| Intercept Variance | 0.92*** | [0.33, 2.72] | ||
Note. N = 52, Ndays = 784.
p < 0.08;
p < 0.05;
p < 0.01;
p < 0.001. 95%CI = 95% credibility interval. Unstandardized model coefficients are presented. Continuous Level 1 variables were person mean -centered; continuous Level 2 variables were grand mean-centered. The modeled covariances between emotion dysregulation and internalized HIV stigma at each time point are excluded from this table and can be found presented within Figure 1.
Figure 2.
This figure displays the standardized results of the Level 1 autoregressive cross-lagged path model whereby afternoon levels of internalized HIV stigma and emotion dysregulation predict nighttime levels of each, which subsequently predict stimulant use. At Level 1, the model was adjusted for the day of data collection and whether or not the report was on a weekend; at Level 2, the model was adjusted for cross-time average levels of internalized HIV stigma and emotion dysregulation, age, Black race, and relationship status. Standardized effects are reported. *p < 0.05; **p < 0.01; ***p < 0.001. P.S.D. = posterior standard deviation.
Finally, it is worth noting that individual- level (i.e., Level 2) average scores for internalized HIV stigma and emotion dysregulation displayed in Table 2 were not significantly associated with the likelihood of daily stimulant drug use, suggesting these are primarily within-person rather than between-person associations.
4. Discussion
We examined an autoregressive cross-lagged path model of internalized HIV stigma, emotion dysregulation, and drug use within a twice-daily EMA study with HIV-positive GBM. In doing so, we found the following: (1) there were significant and positive concurrent associations between internalized HIV stigma and levels of emotion dysregulation measured at the same time, which was true at both time points examined; (2) there were significant autoregressive effects of internalized HIV stigma in the afternoon on levels of internalized HIV stigma in the nighttime and of emotion dysregulation in the afternoon on emotion dysregulation in the nighttime; (3) there was a significant cross-lagged effect of afternoon internalized HIV stigma on nighttime emotion dysregulation, but not for afternoon emotion dysregulation on nighttime internalized HIV stigma; and (4) contrary to expectations, nighttime emotion dysregulation was not significantly associated with subsequent stimulant drug use whereas nighttime internalized HIV stigma was significantly associated. Taken together, these findings suggest a complex interplay between daily experiences of internalized HIV stigma, emotion dysregulation, and the daily use of both non-prescription stimulant drugs.
The first set of findings that is notable has to do with the association between internalized HIV stigma and emotion dysregulation. Taken together, the concurrent and crossed-lagged effects suggest that heightened internalized HIV stigma at earlier times may be associated with increases in emotion dysregulation at later times, but the opposite is not true—this is consistent with existing individual- level models establishing emotion dysregulation as one of the primary sequelae of minority stress experiences.18,36,42 In addition to these findings suggesting a coupling of and downstream effects of internalized HIV stigma onto emotion dysregulation, autoregressive effects of these variables on themselves from one time point to the next suggests a mechanism through which these may be perpetuated. Together, these two findings highlight the three routes through which an experience of internalized HIV stigma can lead to a sustained increase in later emotion dysregulation: (1) the autoregressive “spill-over” of earlier stigma onto later stigma followed by the concurrent impact of stigma on emotion dysregulation; (2) the concurrent impact of stigma on emotion dysregulation followed by the autoregressive “spill-over” of earlier emotion dysregulation onto later emotion dysregulation; and (3) the direct cross-lagged effect of earlier internalized HIV stigma on later emotion dysregulation. Whereas internalized HIV stigma may be relatively domain-specific and avoided by shifting contexts or mindsets, its spill-over into the more global process of emotion dysregulation suggests its negative effects may nonetheless be sustained, at least within the span of several hours. Future research is needed to better understand these effects and the extent to which drug use—which appears to be more likely as a result of increased stigma—may itself further exacerbate the experience of stigma and emotion dysregulation, further propagating these negative minority stress effects over longer periods of time.
The second noteworthy set of findings has to do with the impact of internalized HIV stigma and emotion dysregulation on the use of non-prescription stimulant drugs later that day. The findings contradicted both of our original expectations—instead of direct effects of emotion dysregulation and no direct effects of internalized HIV stigma, we found the opposite. Nighttime internalized HIV stigma was significantly associated with increased likelihood of subsequent stimulant drug use, whereas nighttime emotion dysregulation was not associated. We posited that emotion dysregulation is the mechanism through which internalized HIV stigma acts to increase drug use, but instead found that HIV stigma itself was directly associated. These findings further underscore the negative impact of situational experiences of internalized HIV stigma—not only is it associated with increased and sustained emotion dysregulation, it is also directly associated with greater likelihood of recreational stimulant drug use. However, the exact process linking internalized HIV stigma to stimulant drug use is as yet undetermined, and examining additional affective experiences may help to better understand these results.
With one notable exception in which researchers found a positive association between aggregate (i.e., individual-level) emotion dysregulation and stimulant use,25 there is little existing research with which to compare these findings. In fact, when examined simultaneously, we found that situational variability in internalized HIV stigma was associated with stimulant drug use whereas individual differences in internalized HIV stigma were not. This suggests that individual differences observed in prior research may operate at a within-person level and more research using intensive longitudinal designs is warranted to better understand the mechanisms linking minority stress processes to health outcomes. Future research looking at subtypes of emotion dysregulation—or perhaps the use of specific emotion regulation strategies and/or one’s flexibility in choosing adaptive strategies in a given situation58—is needed to better contextualize these results. Furthermore, our findings pertaining to the nighttime effects of stigma and stimulant use may also have implications for sleep health. Recent research has observed links between experiences of stigma with subsequent sleep disruption,59 increased problems regulating emotions and behavior late at night,60 and the protective or buffering role of good sleep on the effects of discrimination on mental health.61 These links become even more important given that people living with HIV more commonly experience poor sleep health.62
Although preliminary in nature, if replicated these findings might hint at the potential utility of mobile health (i.e., mHealth) interventions that can be delivered “on-demand” during times when individuals are experiencing increased levels of internalized HIV stigma as a means of reducing both emotion dysregulation and the use of stimulants. Given that one of the defining features of internalized stigma is its negative, self-evaluative component,63,64 interventions that bolster against self-evaluative threat may be particularly promising. Self-affirmation exercises—which often involve writing briefly about one’s personal values or positive attributes—have received considerable attention in the social and health literature within the past decade as a means of bolstering against the very types of self-evaluative threats posed by internalized HIV stigma (for a review, see Cohen & Sherman, 2014). This technique may be particularly promising because, like the autoregressive pathways found for internalized HIV stigma and emotion dysregulation over time within the present study, self-affirmation interventions have been found to have self-propagating effects over time and a significant impact on health behavior.66 Moreover, because self-affirmation exercises involve a simple writing task, they can be easily implemented within mobile delivery platforms such as those already being used to collect EMA data.
4.1 Study Strengths and Limitations
The present study has numerous strengths as well as limitations. Although this is the first study of which we are aware to utilize an EMA design to examine situational experiences of HIV stigma and emotion dysregulation and their impact on drug use, this was a pilot study of 52 men. Having found several significant effects suggests that we were adequately powered for many, but others may have also reached significance with a larger sample and strengthened the conclusions. Although we considered it a strength of the study to focus on a population in great need of intervention, this was nonetheless a sample of high-risk HIV-positive GBM living in New York City, all of whom reported drug use and sexual HIV transmission risk behavior at baseline. As such, the findings should be interpreted with caution and future research should focus on replicating these findings with larger and more diverse samples. Participants were not asked about the mode of administration of stimulants, and this is something useful to capture in future research. Finally, the twice-daily diaries provided critical insights and allowed for the testing of a cross-lagged autoregressive path model, but such a design may be less feasible in larger studies, as it is resource-intensive for researchers and somewhat burdensome for participants. Future studies may consider less frequent reporting or other reporting schedules (e.g., event-contingent or random sampling) over a longer period.
4.2 Conclusions
The present study revealed that situational increases in internalized HIV stigma are positively associated with increases in emotion dysregulation and this occurs both directly through concurrent and cross-lagged increases as well as indirectly over time through autoregressive increases whereby internalized HIV stigma or emotion dysregulation at one time point has a “spill-over” effect on the level of the same variable at a later time point. Although we expected that internalized HIV stigma would increase the likelihood of drug use through emotion dysregulation, we instead found that increased internalized HIV stigma was directly associated with a significant increase in the likelihood of non-prescription stimulant drug use later in the day. Contrary to hypotheses, increases in emotion dysregulation were unassociated with the likelihood of stimulant use later in the day. Given that we found significant situational but not individual- level effects of internalized HIV stigma on substance use, it is important to note that aggregate and individual- level research may obscure the processes through which this operates. Further research is needed to replicate these findings in larger and more diverse samples as well as to better characterize the role that emotion dysregulation—and perhaps specific emotion regulation strategies—play in drug use behavior for this population. Given the event-level nature of drug use, intensive longitudinal designs represent an important methodolo gy for better understanding these behaviors and the present findings highlight that minority stress research can and should continue to be conducted within such a paradigm.
Research Highlights.
Internalized HIV stigma is associated with subsequent increases in emotion dysregulation
Internalized HIV stigma is associated with later use of stimulant drugs
Emotion dysregulation was not associated with stimulant use
Emotion dysregulation did not explain the link between internalized stigma and drugs
Acknowledgments
Role of Funding Sources:
This work was funded by a career development award from the National Institute on Drug Abuse (K01-DA039030, PI: Rendina). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
The authors would like to acknowledge the mentorship provided to the first author by the mentors and collaborators on his K01 award: Dr. John Pachankis, Dr. Steven Safren, Dr. Sarah Feldstein Ewing, Dr. Christina Meade, and Dr. Brian Mustanski. The authors also acknowledge the contributions of the day2day Research Team: Sitaji Gurung, Ruben Jimenez, Douglas Keeler, Jonathan Lopez Matos, Chloe Mirzayi, and Laurie Spacek. Finally, the authors would like to thank the CHEST staff, particularly those who played important roles in the implementation of the project: Darren Agboh, Evie Arroyo, Juan Castiblanco, and Brian Salfas, as well as our team of recruiters and interns.
Footnotes
Contributors:
HJR was responsible for study design, data collection, data analysis, interpreting the results, and drafting of the manuscript. BMM was responsible for drafting of the manuscript. JTP was responsible for study design and revising the manuscript. All three authors read, revised, and approved a final version of the manuscript.
Conflict of Interest:
None.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Chaudoir SR, Norton WE, Earnshaw VA, Moneyham L, Mugavero MJ, Hiers KM. Coping with HIV stigma: do proactive coping and spiritual peace buffer the effect of stigma on depression? AIDS and Behavior. 2012;16(8):2382–2391. doi: 10.1007/s10461-011-0039-3. [DOI] [PubMed] [Google Scholar]
- 2.Wright K, Naar-King S, Lam P, Templin T, Frey M. Stigma scale revised: reliability and validity of a brief measure of stigma for HIV+ youth. Journal of Adolescent Health. 2007;40(1):96–98. doi: 10.1016/j.jadohealth.2006.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rao D, Feldman BJ, Fredericksen RJ, et al. A structural equation model of HIV-related stigma, depressive symptoms, and medication adherence. AIDS Behav. 2012;16(3):711–716. doi: 10.1007/s10461-011-9915-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Varni SE, Miller CT, McCuin T, Solomon SE. Disengagement and engagement coping with HIV/AIDS stigma and psychological well-being of people with HIV/AIDS. Journal of Social and Clinical Psychology. 2012;31(2):123–150. doi: 10.1521/jscp.2012.31.2.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tomassilli JC, Parsons JT, Golub SA. What’s sex got to do with it? The role of sexual affect in the relationship between HIV stigma and mental health. AIDS Behav. 2013;17(5):1770–1774. doi: 10.1007/s10461-012-0389-5. [DOI] [PubMed] [Google Scholar]
- 6.Miller CT, Solomon SE, Varni SE, Hodge JJ, Knapp FA, Bunn JY. A transactional approach to relationships over time between perceived HIV stigma and the psychological and physical well-being of people with HIV. Social Science & Medicine. 2016;162:97–105. doi: 10.1016/j.socscimed.2016.06.025. [DOI] [PubMed] [Google Scholar]
- 7.Turan B, Budhwani H, Fazeli PL, et al. How does stigma affect people living with HIV? The mediating roles of internalized and anticipated HIV stigma in the effects of perceived community stigma on health and psychosocial outcomes. AIDS and Behavior. 2017;21(1):283–291. doi: 10.1007/s10461-016-1451-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Turan B, Smith W, Cohen MH, et al. Mechanisms for the negative effects of internalized HIV-related stigma on antiretroviral therapy adherence in women: The mediating roles of social isolation and depression. Journal of Acquired Immune Deficiency Syndromes. 2016;72(2):198–205. doi: 10.1097/QAI.0000000000000948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sayles JN, Hays RD, Sarkisian CA, Mahajan AP, Spritzer KL, Cunningham WE. Development and psychometric assessment of a multidimensional measure of internalized HIV stigma in a sample of HIV-positive adults. AIDS and Behavior. 2008;12(5):748–758. doi: 10.1007/s10461-008-9375-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rueda S, Mitra S, Chen S, et al. Examining the associations between HIV-related stigma and health outcomes in people living with HIV/AIDS: a series of meta-analyses. BMJ open. 2016;6(7):e011453. doi: 10.1136/bmjopen-2016-011453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sweeney SM, Vanable PA. The Association of HIV-Related Stigma to HIV Medication Adherence: A Systematic Review and Synthesis of the Literature. AIDS and Behavior. 2016;20(1):29–50. doi: 10.1007/s10461-015-1164-1. [DOI] [PubMed] [Google Scholar]
- 12.Katz IT, Ryu AE, Onuegbu AG, et al. Impact of HIV-related stigma on treatment adherence: systematic review and meta-synthesis. J Int AIDS Soc. 2013;16(3 Suppl 2):18640. doi: 10.7448/IAS.16.3.18640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dowshen N, Binns HJ, Garofalo R. Experiences of HIV-related stigma among young men who have sex with men. AIDS Patient Care and STDs. 2009;23(5):371–376. doi: 10.1089/apc.2008.0256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hatzenbuehler ML, O’Cleirigh C, Mayer KH, Mimiaga MJ, Safren SA. Prospective associations between HIV-related stigma, transmission risk behaviors, and adverse mental health outcomes in men who have sex with men. Ann Behav Med. 2011;42(2):227–234. doi: 10.1007/s12160-011-9275-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wohl AR, Galvan FH, Carlos JA, et al. A comparison of MSM stigma, HIV stigma and depression in HIV-positive Latino and African American men who have sex with men (MSM) AIDS Behav. 2013;17(4):1454–1464. doi: 10.1007/s10461-012-0385-9. [DOI] [PubMed] [Google Scholar]
- 16.Berg RC, Carter D, Ross MW. A Mixed-Method Study on Correlates of HIV-Related Stigma Among Gay and Bisexual Men in the Southern United States. Journal of the Association of Nurses in AIDS Care. 2017;28(4):532–544. doi: 10.1016/j.jana.2017.02.004. [DOI] [PubMed] [Google Scholar]
- 17.Rendina HJ, Golub SA, Grov C, Parsons JT. Stigma and sexual compulsivity in a community-based sample of HIV-positive gay and bisexual men. AIDS and Behavior. 2012;16(3):741–750. doi: 10.1007/s10461-011-0048-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rendina HJ, Gamarel KE, Pachankis JE, Ventuneac A, Grov C, Parsons JT. Extending the minority stress model to incorporate HIV-positive gay and bisexual men’s experiences: A longitudinal examination of mental health and sexual risk behavior. Annals of Behavioral Medicine. 2017;51(2):147–158. doi: 10.1007/s12160-016-9822-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McCabe SE, West BT, Hughes TL, Boyd CJ. Sexual orientation and substance abuse treatment utilization in the United States: Results from a national survey. Journal of substance abuse treatment. 2013;44(1):4–12. doi: 10.1016/j.jsat.2012.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Green KE, Feinstein BA. Substance use in lesbian, gay, and bisexual populations: An update on empirical research and implications for treatment. Psychology of Addictive Behaviors. 2012;26(2):265. doi: 10.1037/a0025424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schmidt AJ, Bourne A, Weatherburn P, et al. Illicit drug use among gay and bisexual men in 44 cities: findings from the European MSM Internet Survey (EMIS) International Journal of Drug Policy. 2016;38:4–12. doi: 10.1016/j.drugpo.2016.09.007. [DOI] [PubMed] [Google Scholar]
- 22.Skinner WF. The prevalence and demographic predictors of illicit and licit drug use among lesbians and gay men. American Journal of Public Health. 1994;84(8):1307–1310. doi: 10.2105/ajph.84.8.1307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McCabe SE, Hughes TL, Bostwick WB, West BT, Boyd CJ. Sexual orientation, substance use behaviors and substance dependence in the United States. Addiction. 2009;104(8):1333–1345. doi: 10.1111/j.1360-0443.2009.02596.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lea T, Prestage G, Mao L, Zablotska I, Wit J, Holt M. Trends in drug use among gay and bisexual men in Sydney, Melbourne and Queensland, Australia. Drug and alcohol review. 2013;32(1):39–46. doi: 10.1111/j.1465-3362.2012.00494.x. [DOI] [PubMed] [Google Scholar]
- 25.Carrico AW, Johnson MO, Moskowitz JT, et al. Affect regulation, stimulant use, and viral load among HIV-positive persons on anti-retroviral therapy. Psychosomatic medicine. 2007;69(8):785–792. doi: 10.1097/PSY.0b013e318157b142. [DOI] [PubMed] [Google Scholar]
- 26.Grov C, Bimbi DS, Bimbi JE, Parsons JT. Exploring racial and ethnic differences in recreational drug use among gay and bisexual men in New York City and Los Angeles. Journal of drug education. 2006;36(2):105–123. doi: 10.2190/1G84-ENA1-UAD5-U8VJ. [DOI] [PubMed] [Google Scholar]
- 27.Rendina HJ, Moody RL, Ventuneac A, Grov C, Parsons JT. Aggregate and event-level associations between substance use and sexual behavior among gay and bisexual men: Comparing retrospective and prospective data. Drug and alcohol dependence. 2015;154:199–207. doi: 10.1016/j.drugalcdep.2015.06.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Li J, McDaid LM. Alcohol and drug use during unprotected anal intercourse among gay and bisexual men in Scotland: what are the implications for HIV prevention? Sex Transm Infect. 2014;90(2):125–132. doi: 10.1136/sextrans-2013-051195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Parsons JT, Kowalczyk WJ, Botsko M, Tomassilli J, Golub SA. Aggregate versus day level association between methamphetamine use and HIV medication non-adherence among gay and bisexual men. AIDS and Behavior. 2013;17(4):1478–1487. doi: 10.1007/s10461-013-0463-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lelutiu-Weinberger C, Pachankis JE, Golub SA, Ja’Nina JW, Bamonte AJ, Parsons JT. Age cohort differences in the effects of gay-related stigma, anxiety and identification with the gay community on sexual risk and substance use. AIDS and Behavior. 2013;17(1):340–349. doi: 10.1007/s10461-011-0070-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Baum MK, Rafie C, Lai S, Sales S, Page B, Campa A. Crack-cocaine use accelerates HIV disease progression in a cohort of HIV-positive drug users. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2009;50(1):93–99. doi: 10.1097/QAI.0b013e3181900129. [DOI] [PubMed] [Google Scholar]
- 32.Shoptaw S, Stall R, Bordon J, et al. Cumulative exposure to stimulants and immune function outcomes among HIV-positive and HIV-negative men in the Multicenter AIDS Cohort Study. International journal of STD & AIDS. 2012;23(8):576–580. doi: 10.1258/ijsa.2012.011322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Massanella M, Gianella S, Schrier R, et al. Methamphetamine use in HIV-infected individuals affects T-cell function and viral outcome during suppressive antiretroviral therapy. Scientific reports. 2015;5:13179. doi: 10.1038/srep13179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Roth MD, Whittaker KM, Choi R, Tashkin DP, Baldwin GC. Cocaine and σ-1 receptors modulate HIV infection, chemokine receptors, and the HPA axis in the huPBL-SCID model. Journal of leukocyte biology. 2005;78(6):1198–1203. doi: 10.1189/jlb.0405219. [DOI] [PubMed] [Google Scholar]
- 35.Carrico AW, Shoptaw S, Cox C, et al. Stimulant use and progression to Aids or mortality after the initiation of highly active antiretroviral therapy. Journal of acquired immune deficiency syndromes (1999) 2014;67(5):508–513. doi: 10.1097/QAI.0000000000000364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hatzenbuehler ML. How does sexual minority stigma “get under the skin”? A psychological mediation framework. Psychological bulletin. 2009;135(5):707. doi: 10.1037/a0016441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hatzenbuehler ML, Nolen-Hoeksema S, Erickson SJ. Minority stress predictors of HIV risk behavior, substance use, and depressive symptoms: results from a prospective study of bereaved gay men. Health Psychology. 2008;27(4):455. doi: 10.1037/0278-6133.27.4.455. [DOI] [PubMed] [Google Scholar]
- 38.Meyer IH. Minority stress and mental health in gay men. Journal of health and social behavior. 1995:38–56. [PubMed] [Google Scholar]
- 39.Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychological bulletin. 2003;129(5):674. doi: 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.McCabe SE, Bostwick WB, Hughes TL, West BT, Boyd CJ. The relationship between discrimination and substance use disorders among lesbian, gay, and bisexual adults in the United States. American journal of public health. 2010;100(10):1946–1952. doi: 10.2105/AJPH.2009.163147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Feinstein BA, Newcomb ME. The role of substance use motives in the associations between minority stressors and substance use problems among young men who have sex with men. Psychology of sexual orientation and gender diversity. 2016;3(3):357–266. doi: 10.1037/sgd0000185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pachankis JE, Rendina HJ, Restar A, Ventuneac A, Grov C, Parsons JT. A minority stress—emotion regulation model of sexual compulsivity among highly sexually active gay and bisexual men. Health Psychology. 2015;34(8):829. doi: 10.1037/hea0000180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wolitski RJ, Pals SL, Kidder DP, Courtenay-Quirk C, Holtgrave DR. The effects of HIV stigma on health, disclosure of HIV status, and risk behavior of homeless and unstably housed persons living with HIV. AIDS and Behavior. 2009;13(6):1222–1232. doi: 10.1007/s10461-008-9455-4. [DOI] [PubMed] [Google Scholar]
- 44.Lunze K, Lioznov D, Cheng DM, et al. HIV Stigma and Unhealthy Alcohol Use Among People Living with HIV in Russia. AIDS and Behavior. 2017:1–9. doi: 10.1007/s10461-017-1820-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Edelman EJ, Lunze K, Cheng DM, et al. HIV Stigma and Substance Use Among HIV-Positive Russians with Risky Drinking. AIDS and Behavior. 2017 doi: 10.1007/s10461-10017-11832-10464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Radcliffe J, Doty N, Hawkins LA, Gaskins CS, Beidas R, Rudy BJ. Stigma and sexual health risk in HIV-positive African American young men who have sex with men. AIDS patient care and STDs. 2010;24(8):493–499. doi: 10.1089/apc.2010.0020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tucker JS, Burnam MA, Sherbourne CD, Kung F-Y, Gifford AL. Substance use and mental health correlates of nonadherence to antiretroviral medications in a sample of patients with human immunodeficiency virus infection. The American journal of medicine. 2003;114(7):573–580. doi: 10.1016/s0002-9343(03)00093-7. [DOI] [PubMed] [Google Scholar]
- 48.Fazeli PL, Turan JM, Budhwani H, et al. Moment-to-Moment Within-Person Associations Between Acts of Discrimination and Internalized Stigma in People Living With HIV: An Experience Sampling Study. 2016 doi: 10.1037/sah0000051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rendina HJ, Millar BM, Parsons JT. The critical role of internalized HIV-related stigma in the daily negative affective: Experiences of HIV-positive gay and bisexual men. doi: 10.1016/j.jad.2017.11.005. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Eldahan AI, Pachankis JE, Rendina HJ, Ventuneac A, Grov C, Parsons JT. Daily minority stress and affect among gay and bisexual men: A 30-day diary study. Journal of affective disorders. 2016;190:828–835. doi: 10.1016/j.jad.2015.10.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Pachankis JE, Hatzenbuehler ML, Starks TJ. The influence of structural stigma and rejection sensitivity on young sexual minority men’s daily tobacco and alcohol use. Social Science & Medicine. 2014;103:67–75. doi: 10.1016/j.socscimed.2013.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Livingston NA, Flentje A, Heck NC, Szalda-Petree A, Cochran BN. Ecological momentary assessment of daily discrimination experiences and nicotine, alcohol, and drug use among sexual and gender minority individuals. Journal of consulting and clinical psychology. 2017;85(12):1131–1143. doi: 10.1037/ccp0000252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Berger BE, Ferrans CE, Lashley FR. Measuring stigma in people with HIV: Psychometric assessment of the HIV stigma scale. Research in nursing & health. 2001;24(6):518–529. doi: 10.1002/nur.10011. [DOI] [PubMed] [Google Scholar]
- 54.Pakenham K, Rinaldis M. Development of the HIV/AIDS stress scale. Psychology and Health. 2002;17(2):203–219. [Google Scholar]
- 55.Golub SA, Rendina HJ, Gamarel KE. Identity-related growth and loss in a sample of HIV-positive gay and bisexual men: Initial scale development and psychometric evaluation. AIDS and Behavior. 2013;17:748–759. doi: 10.1007/s10461-012-0338-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Golub SA, Rendina HJ, Gamarel KE. Loss and growth: Identity processes with distinct and complementary impacts on wellbeing among those living with chronic illness. Psychology, Health, and Medicine. 2013 doi: 10.1080/13548506.2013.855318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of psychopathology and behavioral assessment. 2004;26(1):41–54. [Google Scholar]
- 58.Bonanno GA, Burton CL. Regulatory flexibility: An individual differences perspective on coping and emotion regulation. Perspectives on Psychological Science. 2013;8(6):591–612. doi: 10.1177/1745691613504116. [DOI] [PubMed] [Google Scholar]
- 59.Ong AD, Cerrada C, Lee RA, Williams DR. Stigma consciousness, racial microaggressions, and sleep disturbance among Asian Americans. Asian American Journal of Psychology. 2017;8(1):72–81s. [Google Scholar]
- 60.Kroese FM, Evers C, Adriaanse MA, de Ridder DT. Bedtime procrastination: A self-regulation perspective on sleep insufficiency in the general population. Journal of Health Psychology. 2016;21(5):853–862. doi: 10.1177/1359105314540014. [DOI] [PubMed] [Google Scholar]
- 61.Yip T. The effects of ethnic/racial discrimination and sleep quality on depressive symptoms and self-esteem trajectories among diverse adolescents. Journal of youth and adolescence. 2015;44(2):419–430. doi: 10.1007/s10964-014-0123-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wu J, Wu H, Lu C, Guo L, Li P. Self-reported sleep disturbances in HIV-infected people: a meta-analysis of prevalence and moderators. Sleep medicine. 2015;16(8):901–907. doi: 10.1016/j.sleep.2015.03.027. [DOI] [PubMed] [Google Scholar]
- 63.Earnshaw VA, Chaudoir SR. From conceptualizing to measuring HIV stigma: A review of HIV stigma mechanism measures. AIDS and Behavior. 2009;13(6):1160–1177. doi: 10.1007/s10461-009-9593-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Earnshaw VA, Smith LR, Chaudoir SR, Amico KR, Copenhaver MM. HIV stigma mechanisms and well-being among PLWH: a test of the HIV stigma framework. AIDS Behav. 2013;17(5):1785–1795. doi: 10.1007/s10461-013-0437-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Cohen GL, Sherman DK. The psychology of change: Self-affirmation and social psychological intervention. Annual review of psychology. 2014;65:333–371. doi: 10.1146/annurev-psych-010213-115137. [DOI] [PubMed] [Google Scholar]
- 66.Epton T, Harris PR, Kane R, van Koningsbruggen GM, Sheeran P. The impact of self-affirmation on health-behavior change: a meta-analysis. Health Psychology. 2015;34(3):187. doi: 10.1037/hea0000116. [DOI] [PubMed] [Google Scholar]