Abstract
There is a well-established socioeconomic gradient in smoking behaviour: those with lower socioeconomic status smoke more. However, much less is known the mechanisms explaining how SES is linked to smoking. This study takes a social-ecological perspective by examining whether socioeconomic status affects smoking behaviour by differential exposure to places where smoking is allowed. Exposure to smoking restrictions was assessed in real-time using Ecological Momentary Assessment methods. A sample of 194 daily smokers, who were not attempting to quit, recorded their smoking and information about situational and contextual factors for three weeks using an electronic diary. We tested whether a smoker’s momentary context mediated the relationship between socioeconomic status (educational attainment) and cigarettes smoked per day (CPD). Momentary context was operationalized as the proportion of random assessments answered in locations where smoking was allowed versus where smoking was not allowed. Data were analysed using multilevel regression (measurements nested within participants) with a lower level mediation model (2-1-1 mediation). Although no significant direct effect of SES on CPD were observed, there was a significant indirect effect of SES on CPD via the momentary context. Compared to participants with higher education, lower educated participants were more likely to encounter places where smoking was allowed, and this in turn, was associated with a higher number of CPD. These findings suggest that SES is associated with smoking at least partially via differential exposure to smoking- friendly environments, with smokers from lower SES backgrounds accessing more places where smoking is allowed. Implications for current smoke-free legislation are discussed.
Keywords: smoking, EMA, socioeconomic status, smoking bans
1 Introduction
Smoking remains one of the leading causes of preventable disease and death in the developed world (Ng et al, 2014), and what is more important, it is unequally distributed between groups of different socioeconomic status (SES; often indicated by differential resources such as education, income, or occupational status): groups and individuals with lower SES smoke more (Fidler, Jarvis, Mindell, & West, 2008; Hiscock, Bauld, Amos, Fidler, & Munafo, 2012; Pisinger, Aadahl, Toft, & Jorgensen, 2011). While the associations between SES and tobacco use are well established, much less is known about the processes and mechanisms linking SES to smoking behaviour. One potential mechanism this paper explores is differential exposure to physical contexts and their corresponding behavioural implications for smoking according to SES: Poland et al. (2006) suggest that, depending on SES, smokers are exposed to environments that are more or less permissive of smoking, which in turn influences smoking.
Exploring the relationship between SES and smoking is challenging, as SES can affect health-related behaviours such as smoking via influences on different environmental levels, ranging from individual factors over proximal- level factors such as one’s neighbourhood to macro-level or societal factors (Schüz, 2017). Previous studies have looked at these indicators in isolation: When looking at the community level as contextual unit, smoking rates are significantly higher in more disadvantaged areas (Bernard et al., 2007; Bobak, Jarvis, Skodova, & Marmot, 2000) compared to more affluent areas. For example, prior to the smoke-free legislation in Scotland in 2006, smoking was not only more prevalent among socioeconomically disadvantaged communities, those communities were also less likely to have tobacco control policies and were more likely to permit smoking rather than more affluent communities (Eadie et al., 2008; Plunkett, Haw, Cassels, Moore, & O’Connor, 2000). The idea underlying such studies is that the neighbourhood comprises of built and social environment features that provide resources such as access to libraries, playgrounds or the presence of environments that support healthy lifestyles. However, such measures do not take individual socioeconomic characteristics into account, thus potentially falling prone to the ecological fallacy (Spicker, 2001). On the other hand, only considering individual characteristics such as education might lead to false conclusions (atomistic fallacy) as the environment people are embedded in features socioeconomic inequalities that can facilitate or constrain health behaviour (Diez-Roux, 1998).
In addition to these considerations, it has been argued that context is less a fixed geographical location, but the entirety of varying physical and social environments that people are being exposed to – that is, both their place of residence, but also environments they encounter at work or on the way to work (Barnett, Moon, Pearce, Thompson, & Twigg, 2017). This highlights that in order to understand the effects of context on smoking, we need to take into account that contexts vary over time, and that these contexts can vary as a function of SES. Supporting this idea, a previous qualitative study (Paul et al., 2010) found that smokers of lower SES not only reported higher smoking prevalence, but also perceived a more smoke-permitting social context than smokers of high SES. Furthermore, smokers with lower SES encountered more environments that were more permissive towards smoking, in particular via workplaces that were more conducive to smoking by enforcing less anti-smoking regulations, and with more access to smoking breaks. Conversely, high SES smokers encountered more anti-smoking factors in their everyday environment. In terms of perceptions of social acceptance, smokers in lower SES neighbourhoods reported smoking in public to be more acceptable compared to those in high SES neighbourhoods. Moreover, while government regulations, such as bans on cigarette sales tend to empower high SES smokers to quit smoking, low SES smokers are more likely to circumvent those regulations by seeking alternative, illegal sources of cigarettes (Paul et al., 2010).
To date, research on the SES gradient in smoking has largely ignored the impact of differential environments on smoking. For example, individuals with higher educational attainment are more likely to work in ‘white collar’ environments (offices with a higher likelihood of smoking bans) than individuals with lower educational attainment, who are more likely to work in service or outdoors environments where smoking bans are less prevalent and easier to circumvent (Barnett et al., 2017). The interaction between personal and contextual factors, and their influence on behaviour, suggests that more in-depth investigation in real-time and real-world is necessary. Consequently, this study aimed to investigate the relevance of contextual factors—specially the prevalence of environments where smoking is allowed—using Ecological Momentary Assessment (EMA: Shiffman, Stone, & Hufford, 2008) methods. The relative exposure to particular smoking environments represents opportunities or barriers to smoking, which in turn are believed to have an influence on smoking behaviour (Bancroft, Wiltshire, Parry, & Amos, 2003). More exposure to smoking-permissive environments therefore poses less barriers and more opportunities to smoke, whereas fewer encounters of pro smoking environments increases barriers and provides less opportunities. These opportunities and barriers facilitate or constrain behaviour, resulting in the final number of cigarettes smoked on any given day (Twyman, Bonevski, Paul, & Bryant, 2014; Wiltshire, Bancroft, Parry, & Amos, 2003).
The goal of this study was to gain a better understanding of whether and how individual SES is associated with exposure to smoking-related environments, and how these environments in turn facilitate or impede smoking behaviour. This could identify intervention options, in particular for people with lower SES. In this study, we investigate whether individual SES is associated with the degree of smoking permissiveness of the environments that smokers encounter during the day, and whether this differential context exposure mediates the relationship between SES and cigarettes smoked per day. We hypothesize that the momentary context (partially) mediates the relationship between SES and CPD in a way that smokers from low SES backgrounds are exposed to more places where smoking is allowed, and that greater exposure is in turn associated with more cigarettes smoked.
2 Method
2.1 Participants
The sample used in this analysis is a sub-set of a larger study examining differences between daily and non-daily smokers and details on the recruitment methods have been reported elsewhere (Shiffman et al., 2014a, 2014b). Briefly, 194 daily smokers were recruited in the Pittsburgh area between November 2007 and January 2010. The study was introduced as a naturalistic study of smoking patterns. To be eligible, participants had to be daily smokers (defined as smoking 5 to 30 cigarettes per day) for at least the last 3 months, not planning to quit, and be ≥21 years old.
2.2 Procedure
The study procedures have been described in detail elsewhere (Shiffman et al., 2014a, 2014b). Briefly, participants were required to monitor their smoking, activities and social setting over 21 days (M=22.5, SD=4.12) using an electronic diary (ED). To monitor real-time smoking, participants were provided with an ED and received hands-on individual training. Participants were asked to carry the ED at all times during the waking day. Participants were instructed to report each time they smoked a cigarette and a subset of these reports (approximately 4-5 a day) was randomly selected for assessment of the situation they were in (Shiffman et al., 2014a). To be able to compare the situations when participants were not smoking, participants were also “beeped” 3-4 times a day (M = 3.52) at randomly selected times (but never within 15 minutes of a smoking occasion) and asked to answer a series of questions concerning non-smoking situations. Compliance was monitored at each study visit and participants received feedback and were given additional training if needed. Over the course of the EMA monitoring there were three visits, each at the end of the first, second and third week of the study. Compliance was based on the percentage of random prompts that were answered within two minutes of prompting. Compensation was provided at the end of each week of monitoring with progressively larger increments ($15, $30, $75). Finally, participants were asked to complete an evening and waking report where they were asked to enter the number of additional cigarettes they smoked on that given day, which they had not reported during the assessments. Data consisted of 13,761 smoking and 11,640 non-smoking assessments. Each participant contributed an average of 70.9 (SD=25.14) smoking assessments and 59.94 (SD= 19.42) non-smoking assessments.
2.3 Measures
Participants’ highest educational achievement (assessed during the baseline visit) was used as indicator for socioeconomic status. Education was dichotomized as lower education (“8th grade or less”, some high school, no graduation/ GED”, “high school graduate/ GED”) and higher education (“some college”, “college graduate/ degree”, “some graduate work”, “graduate degree”). SES was operationalized via education because of several potential mechanisms through which educational attainment might influence health behaviour (Wetter et al., 2005): Higher educated persons might have developed better critical thinking skills or information processing, and abilities required to interact with health care providers (Ross & Wu, 1995). Furthermore, higher educated individuals are more likely to be socialized to health-promoting behaviour and lifestyles, and are more likely to have better work and economic conditions (Shavers, 2007). Additionally, using educational attainment as an indicator for SES has the advantage of being available for both, men and women, generally does not change throughout the life course, and has a high validity and reliability (Galobardes, Shaw, Lawlor, Lynch, & Davey Smith, 2006)1.
The primary outcome, “number of cigarettes smoked per day” (CPD) was operationalized by cross-referencing ED logs and daily retrospective reports assessed at the end of the day (Shiffman, Dunbar, & Ferguson, 2015). Here, participants were asked to report any additional cigarettes they had smoked but not reported during the day. This number was then added to the number of cigarettes reported by participants over the day.
The mediator variable (momentary context) was operationalized by computing, for every participant and every day, the ratio of random prompts answered in environments where smoking was allowed divided by the sum of all random prompts answered where smoking was allowed or forbidden. Situations in which smoking was discouraged were not included in the analysis. For example, a person who responded to 4 random prompts per day, 3 of these were answered in environments where smoking was allowed, and none in an environment where smoking was discouraged, would be assigned a value of 0.75 for this day. Smoking regulations at the current location was assessed during the random prompts (“Smoking allowed?” with following possible responses: “Forbidden”, “Discouraged”, or “Allowed”). These assessments represent a random sample of non-smoking times during the day.
2.4 Analysis
In this study, we were interested in examining indirect effects of SES (independent variable) on smoking (dependent variable) via momentary context exposure (mediating variable). Such mediation models allow exploring an underlying process by which an independent variable influences a dependent variable through a third variable (mediator: Krull & MacKinnon, 2001). In our case, this means exploring the proportions to which the total effect of SES on smoking consists of the direct effect of SES (estimated while the mediating variable remains unaltered) and the indirect effect via exposure (operationalised as the product of the effects of SES on exposure and the effect of exposure on smoking). No covariates were included in this analysis.
By nature, EMA data has a hierarchical structure with multiple daily assessments nested within participants (cigarette reports, random assessments), which requires analyses that accommodate the hierarchical non-independency of observations. The independent variable, SES, was measured on the level of the participant, and the mediating variable (exposure per day) and dependent variable (cigarettes per day) were measured on the level of days (level-1) nested under persons (level-2; Figure 1).
Fig. 1.
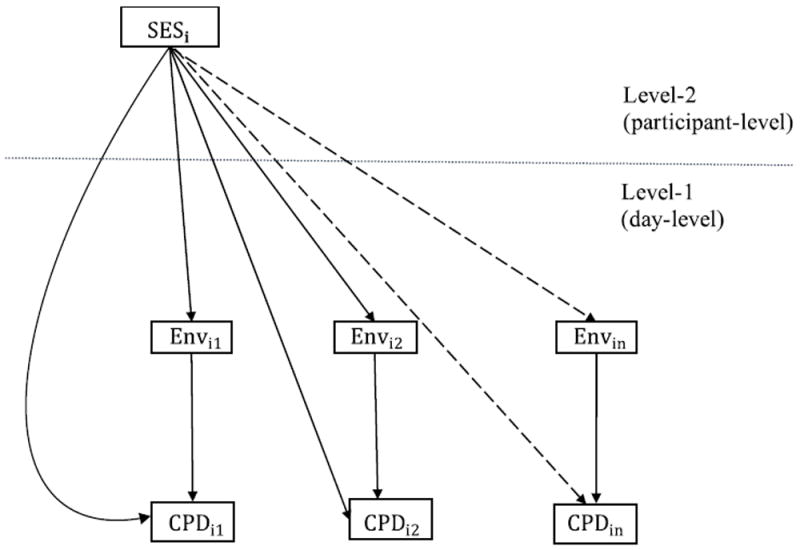
Conceptual diagram of 2-1-1 mediation model
Note: SESi: = Highest educational attainment for participant i; Envin:= Smoking environment for participant i on day n; CPDin:= Cigarettes smoked per day for participant i on day n
Therefore, a 2-1-1 mediation model (Preacher, Zyphur, & Zhang, 2010) with random intercepts and random slopes was estimated. To estimate these models MPlus (TYPE = TWOLEVEL RANDOM; Muthén & Muthén, 2012) was used.
3 Results
Participants smoked on average 15 cigarettes per day (SD=5.86), 58.25% had an education beyond high school, were 41 years old (SD=11.18), 55% were male, and had been smoking for 26 years (SD=11.83) on average. The demographic characteristics of the sample in relation to SES are presented in Table 1. Lower SES participants were older and significantly more likely to be African American. Compared to higher SES participants, they did not significantly differ by gender, or annual household income.
Table 1.
Participant demographics
| Overall (n=194) | Low SES (n=81) | High SES (n=113) | |
|---|---|---|---|
| Age | 41.2 (11.18) | 42.6 (10.6) *** | 40.1 (11.5) |
| Gender Male | 55.2% (n=107) | 56.8% (n=46) | 54.0% (n=61) |
| Household income below $30,000 | 75.8% (n=147) | 82.7% (n=67) | 70.8% (n=80) |
| African American | 37.6% (n=73) | 45.7% (n=37) * | 31.9% (n=36) |
Note: Entries are M (SD), unless % is specified. M = mean, SD = standard deviation.
p < .05,
p < .01,
p < .001
Overall, lower SES participants responded to 9539 random prompts, whereas higher SES participants answered 2101 prompts2. Smoking was allowed in 79.2% of the prompts answered by lower SES participants and 59% of the prompts answered by higher SES participants. Overall, smoking was forbidden in the locations where 14.6% of prompts were answered by lower SES participants (62.5% forbidden by law), and 30.5% for higher SES participants (69.2% forbidden by law). With regards to locations where smoking was forbidden, 37.1% of these were at work in the low SES group, and 53.5% were at work in the higher SES group.
The results for the multilevel mediation analysis are shown in Table 2.
Table 2.
Coefficient Estimates for parameters in 2-1-1 mediation model predicting CPD
| Coefficient Estimates | B (SD) |
|---|---|
| Fixed Effects (Measurement occasion level) | |
| Intercept CPD | 6.908 (1.383) *** |
| Intercept Environment | 0.845 (0.017) *** |
| SES → Environment | -0.188 (0.056) *** |
| Environment → CPD (Level-2 component) | 4.963 (1.782) ** |
| Environment → CPD (average Level-1 component) | 0.187 (0.418) |
| Environment → CPD (total effect) | 5.150 (1.646) ** |
| Direct Effect SES → CPD | 1.262 (1.186) |
| Indirect Effect | -0.966 (0.45) * |
| Total Effect | 0.269 (1.202) |
|
| |
| Random Effects (Participant level) | |
| Residual Variance Intercept Environment | 0.049 (0.008) *** |
| Residual Variance Intercept CPD | 25.636 (4.176) *** |
| Residual Variance Slopes | 6.546 (2.812) * |
| Covariance Environment CPD | 15.739 (1.019) *** |
Note: B = coefficient estimates, SD = standard deviation.
p < .05,
p < .01,
p < .001
Compared to lower educated participants, participants with higher SES (education) were significantly less likely to encounter places where smoking was allowed (B=-0.188, SD=0.056, p <.001). Participants who encountered relatively more smoking-permissive environments relative to other participants, smoked more cigarettes per day (B=4.963, SD=1.782, p <.01). This resulted in a significant indirect effect (B=-0.966, SD=0.45, p<.05) of educational achievement via the environment on CPD, which means that socioeconomic status was indirectly associated with smoking behaviour via the environments encountered throughout the day (Figure 2).
Fig. 2.
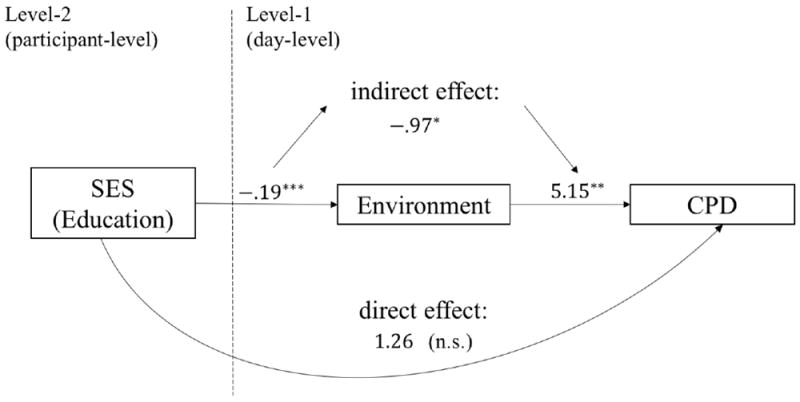
Final 2-1-1 Mediation Model
Note: * p < .05, ** p < .01, *** p < .001
4 Discussion
In this study, we showed that the association between smokers’ individual SES and their everyday smoking was partially mediated via their exposure to smoking-permissive environments. Compared to smokers with higher SES, low SES smokers encountered proportionally more locations per day in which smoking was allowed. This greater exposure to smoking-friendly environment was in turn associated with a higher number of cigarettes smoked, suggesting an indirect effect of education via environmental exposure.
This underpins the importance of a perspective that conceptualises SES both as a person-and a location-related construct that facilitates or constrains behaviour depending on individual and momentary characteristics. This is in line with previous findings: Paul et al. (2010) showed that low SES smokers experience more everyday encounters in which smoking is acceptable. In addition, Wiltshire et al. (2003) argued that smoking is deeply embedded in low SES smokers’ lives, as they might encounter fewer contexts in which smoking is explicitly disallowed. This is also supported on a community level: Eadie et al. (2008) showed that compliance in enforcing the 2006 smoking ban in Scottish bars was greater for bars serving more affluent communities, whereas more violations were found in bars serving more deprived communities.
Through the process of socialisation and the harmonization of individual’s attitudes and behaviour with that of their socioeconomic status, individuals are provided with status dependant lifestyles and ways of acting (Singh-Manoux & Marmot, 2005). Thus, bound to social and environmental structures, individuals carry out status dependant behaviour. Using Ecological Momentary Assessment (EMA) methods, we could show that via multiple everyday encounters, the environment was significantly associated with how much participants smoked over the day and that this was a function of SES.
4.1 Strengths and Limitations
The study’s strengths included the use of real-time EMA methods, which allow for detailed characterization of environmental context and smoking behaviour without relying on participants’ memory and, more importantly, assessing the time- and location-varying nature of smoking regulations. The assessment of exposure to smoking-permissive environments via a random sampling of non-smoking occasions allowed for a sample of places participants encountered over the day, specifically in non-smoking situations. However, there are some limitations to the study that need to be taken into account when interpreting the findings. First, EMA data is essentially correlational in nature, which makes causal interpretations difficult. For example, low SES smokers who tend to be heavier smokers could deliberately apply for jobs in smoking friendly workplaces. Second, as with other self-reported measures, using EMA, participants could have deliberately or unintentionally misrepresented their behaviour (Furnham & Henderson, 1982). Third, self-reports and situational characteristics have the potential to induce reactivity, which means that the monitoring itself might change participant’s behaviour. However, results on the potential behavioural reactivity of EMA methods on behaviour to date are mixed (Hufford, Shields, Shiffman, Paty, & Balabanis, 2002; Rowan et al., 2007). Nevertheless, EMA methods represent a substantial improvement over more common retrospective methods, by maximising ecological validity, while avoiding recall bias (Schwarz, 2007).
Further, the data comprised of fewer assessments from higher SES participants than from low SES participants. While we do not know the reason for this discrepancy, overall compliance with answering random prompts was excellent—with participants completing >87% of prompts—and, consistent with a previous study, we did not observe differences in compliance based on SES (Schüz, Walters, Frandsen, Bower & Ferguson, 2014). As such, we do not think this imbalance influenced our findings. Here we presented educational attainment as the sole indicator of participants’ SES, which does not adequately reflect individuals relative position on a hierarchical social structure, which may also significantly differ across income and racial/ ethnic or gender groups. Additional analyses (see Supplementary files) with income as individual SES indicator show smaller effects of income on the momentary environment and non-significant indirect effects, which suggests that education and income might differentially affect where people spend their time – most notably through differences in jobs and professions according to education. Nevertheless, education is the strongest sociodemographic correlate of smoking (Pierce, 1989) and perhaps the most widely used indicator of SES, because of its potential influence on future occupational opportunities. Furthermore, caution needs to be taken when interpreting the findings, as the analysis did not take into consideration whether smoking was forbidden by law, own rule or others’ rule and the type of location participants inhabited during random prompts. This can have implications for the effectiveness of additional smokefree legislations. Both SES groups reported being at home for the vast majority of prompts where smoking was allowed. Further research considering the type of locations is needed to examine potential additional benefits through smokefree policies. In addition, smokefree policies were introduced within the duration of the study. The Pennsylvania Clean Indoor Air Act (2008) requires that public places and workplaces must be smoke-free. However, no information about the stringency of policy enforcement within and between the municipalities relevant for this study was available.
4.2 Implications
While it has been widely accepted that socioeconomic differences drive the uptake of smoking in adolescents and its persistence across adulthood, tobacco control policies still focus on changing behaviour, not individuals’ life circumstances. It has been suggested that these tobacco control policies have had differential impact according to social status, tending to rather increase than narrow the gap in health inequalities (Mackenbach, 2012). The approaches to narrow down the gap in smoking rates between high and low SES smokers so far have mainly focused on encouraging the de-normalisation of smoking and have found mixed results (Giskes et al., 2007; Hill, Amos, Clifford, & Platt, 2014; Thomas et al., 2008). As our findings suggest that SES is associated with smoking at least partially via differential exposure to smoking- friendly environments, with smokers from lower SES backgrounds accessing more places where smoking is allowed, current smoke-free legislation might need to be extended in order to benefit smokers regardless of their SES. Tailored policy responses reflecting different patterns of places smokers with low SES inhabit on a daily basis could help narrowing the SES gap in smoking behaviour (Graham, Inskip, Francis, & Harman, 2006). Enforcing smoking restrictions on a mutual level across all workplaces, regardless of outdoor or indoor workplaces, could benefit especially those smokers who are prone to encounter more places where smoking is allowed or restrictions are not strictly enforced, such as outdoor working places (Blue-collar workers).
As a strategy that is less dependent on SES, so-called choice architecture interventions that aim to alter the environment by changing properties or placement of objects or stimuli within micro-environments (Hollands et al., 2013) might be promising. Being less dependent on literacy and self-regulatory skills, which are generally lower in those with lower SES, these interventions have the potential to reduce the social gradient in smoking. Reducing the proximity and density of tobacco retail outlets or the size and number of cigarettes sold per packet for example may influence the number of consumed cigarettes.
4.3 Conclusion
Our study suggests that place matters in terms of health behaviours such as smoking (Ellen, Mijanovich, & Dillman, 2001; Frohlich, Corin, & Potvin, 2001). Our study extends previous work on environmental effects on smoking by taking a decidedly within-participant and time-varying perspective, which for the first time allows examining whether people are, as a function of SES, exposed to different places, which in turn affect smoking differentially. Our findings suggest that current smoke-free legislation might need to be extended in order to target particularly those places frequented by smokers of lower SES in order to benefit smokers regardless of their SES.
Highlights.
SES affects smoking partially via differential exposure to smoking-friendly environments
Research needs to account for differential variability of everyday environments
To benefit smokers regardless of SES, smokefree-legislation might need extension
Acknowledgments
The authors acknowledge that this research was conducted with the support of an Australian Government Research Training Program Scholarship. The authors are grateful to Thomas Kirchner, Deborah Scharf and Sarah M. Scholl for help launching this study and for input on study design; and to Anna Tsivina, Joe Stafura, Rachelle Gish, and Aileen Butera for their work conducting research sessions.
Role of Funding Sources
Data collection was supported by Grant R01-DA020742 (PI: Shiffman) from the U.S. National Institutes of Health, National Institute on Drug Abuse. National Institute on Drug Abuse had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
Footnotes
Additional analyses using income as indicator of SES were conducted. While a similar direction of effects was found, effects of income on environment were smaller, and indirect effects were not significant. Results of the analyses using income as SES indicator can be found in the supplementary material.
More information on the characteristics of encountered environments with regard to SES can be found in the supplementary material (Table. 4)
Contributors
Stuart G Ferguson and Saul Shiffman designed the study and wrote the protocol. Johannes Thrul conducted literature searches and provided summaries of previous research studies. Benjamin Schüz conducted the statistical analysis. Tina Jahnel wrote the first draft of the manuscript and all authors contributed to and have approved the final manuscript.
Conflict of Interest
Dr. Shiffman provides consulting services on tobacco harm minimization (including nicotine replacement therapy and digital vapor products) to subsidiaries of Reynolds American Inc. Stuart G Ferguson has worked as a consultant for pharmaceutical companies on matters relating to smoking cessation. All other authors declare that they have no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Bancroft A, Wiltshire S, Parry O, Amos A. It’s like an addiction first thing… afterwards it’s like a habit”: daily smoking behaviour among people living in areas of deprivation. Social Science and Medicine. 2003;56(6):1261–1267. doi: 10.1016/S0277-9536(02)00124-7. [DOI] [PubMed] [Google Scholar]
- Barnett R, Moon G, Pearce J, Thompson L, Twigg L. Smoking Geographies, Space, Place, Tobacco. Sussex: John Wiley & Sons; 2017. [Google Scholar]
- Bernard P, Charafeddine R, Frohlich KL, Daniel M, Kestens Y, Potvin L. Health inequalities and place: a theoretical conception of neighbourhood. Soc Sci Med. 2007;65(9):1839–1852. doi: 10.1016/j.socscimed.2007.05.037. [DOI] [PubMed] [Google Scholar]
- Bobak M, Jarvis MJ, Skodova Z, Marmot M. Smoke intake among smokers is higher in lower socioeconomic groups. Tobacco Control. 2000;9(3):310–312. doi: 10.1136/tc.9.3.310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diez-Roux AV. Bringing context back into epidemiology: Variables and fallacies in multilevel analysis. American Journal of Public Health. 1998;88(2):216–222. doi: 10.2105/Ajph.88.2.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eadie D, Heim D, Macaskill S, Ross A, Hastings G, Davies J. A qualitative analysis of compliance with smoke-free legislation in community bars in Scotland: implications for public health. Addiction. 2008;103(6):1019–1026. doi: 10.1111/j.1360-0443.2008.02217.x. [DOI] [PubMed] [Google Scholar]
- Ellen IG, Mijanovich T, Dillman KN. Neighborhood effects on health: Exploring the links and assessing the evidence. Journal of Urban Affairs. 2001;23(3-4):391–408. doi: 10.1111/0735-2166.00096. [DOI] [Google Scholar]
- Fidler JA, Jarvis MJ, Mindell J, West R. Nicotine intake in cigarette smokers in England: distribution and demographic correlates. Cancer Epidemiol Biomarkers Prev. 2008;17(12):3331–3336. doi: 10.1158/1055-9965.EPI-08-0296. [DOI] [PubMed] [Google Scholar]
- Frohlich KL, Corin E, Potvin L. A theoretical proposal for the relationship between context and disease. Sociology of Health & Illness. 2001;23(6):776–797. doi: 10.1111/1467-9566.00275. [DOI] [Google Scholar]
- Furnham A, Henderson M. The Good, the Bad and the Mad - Response Bias in Self-Report Measures. Personality and Individual Differences. 1982;3(3):311–320. doi: 10.1016/0191-8869(82)90051-4. [DOI] [Google Scholar]
- Galobardes B, Shaw M, Lawlor DA, Lynch JW, Davey Smith G. Indicators of socioeconomic position (part 1) J Epidemiol Community Health. 2006;60(1):7–12. doi: 10.1136/jech.2004.023531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giskes K, Kunst AE, Ariza C, Benach J, Borrell C, Helmert U, Mackenbach JP, et al. Applying an equity lens to tobacco-control policies and their uptake in six Western-European countries. J Public Health Policy. 2007;28(2):261–280. doi: 10.1057/palgrave.jphp.3200132. [DOI] [PubMed] [Google Scholar]
- Graham H, Inskip HM, Francis B, Harman J. Pathways of disadvantage and smoking careers: evidence and policy implications. J Epidemiol Community Health. 2006;60(Suppl 2(Supl II)):7–12. doi: 10.1136/jech.2005.045583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill S, Amos A, Clifford D, Platt S. Impact of tobacco control interventions on socioeconomic inequalities in smoking: review of the evidence. Tob Control. 2014;23(e2):e89–97. doi: 10.1136/tobaccocontrol-2013-051110. [DOI] [PubMed] [Google Scholar]
- Hiscock R, Bauld L, Amos A, Fidler JA, Munafo M. Socioeconomic status and smoking: a review. Ann N Y Acad Sci. 2012;1248:107–123. doi: 10.1111/j.1749-6632.2011.06202.x. [DOI] [PubMed] [Google Scholar]
- Hollands GJ, Shemilt I, Marteau TM, Jebb SA, Kelly MP, Nakamura R, Ogilvie D, et al. Altering micro-environments to change population health behaviour: towards an evidence base for choice architecture interventions. BMC Public Health. 2013;13:1218. doi: 10.1186/1471-2458-13-1218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hufford MR, Shields AL, Shiffman S, Paty J, Balabanis M. Reactivity to ecological momentary assessment: An example using undergraduate problem drinkers. Psychology of Addictive Behaviors. 2002;16(3):205–211. doi: 10.1037//0893-164x.16.3.205. [DOI] [PubMed] [Google Scholar]
- Krull JL, MacKinnon DP. Multilevel modeling of individual and group level mediated effects. Multivariate Behavioral Research. 2001;36(2):249–277. doi: 10.1207/S15327906mbr3602_06. [DOI] [PubMed] [Google Scholar]
- Mackenbach JP. The persistence of health inequalities in modern welfare states: The explanation of a paradox. Social Science and Medicine. 2012;75:761–769. doi: 10.1016/j.socscimed.2012.02.031. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. MPlus User’s Guide. 7. Los Angeles: Muthén & Muthén; 2012. [Google Scholar]
- Ng M, Freeman MK, Fleming TD, Robinson M, Dwyer-Lindgren L, Thomson B, Gakidou E, et al. Smoking prevalence and cigarette consumption in 187 countries, 1980-2012. JAMA. 2014;311(2):183–192. doi: 10.1001/jama.2013.284692. [DOI] [PubMed] [Google Scholar]
- Paul CL, Ross S, Bryant J, Hill W, Bonevski B, Keevy N. The social context of smoking: A qualitative study comparing smokers of high versus low socioeconomic position. BMC Public Health. 2010;10(211):211. doi: 10.1186/1471-2458-10-211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce JP. Trends in Cigarette Smoking in the United States. Jama. 1989;261(1):61. doi: 10.1001/jama.1989.03420010071035. [DOI] [PubMed] [Google Scholar]
- Pisinger C, Aadahl M, Toft U, Jorgensen T. Motives to quit smoking and reasons to relapse differ by socioeconomic status. Prev Med. 2011;52(1):48–52. doi: 10.1016/j.ypmed.2010.10.007. [DOI] [PubMed] [Google Scholar]
- Plunkett M, Haw S, Cassels J, Moore M, O’Connor M. Smoking in Public Places—A Survey of the Scottish Leisure Industry. Edinburgh: ASH Scotland/HEBS; 2000. [Google Scholar]
- Poland B, Frohlich K, Haines RJ, Mykhalovskiy E, Rock M, Sparks R. The social context of smoking: the next frontier in tobacco control? Tob Control. 2006;15(1):59–63. doi: 10.1136/tc.2004.009886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, Zyphur MJ, Zhang Z. A General Multilevel SEM Framework for Assessing Multilevel Mediation. American Psychological Association. 2010;15(3):209–233. doi: 10.1037/a0020141. [DOI] [PubMed] [Google Scholar]
- Ross CE, Wu CL. The Links between Education and Health. American Sociological Review. 1995;60(5):719–745. doi: 10.2307/2096319. [DOI] [Google Scholar]
- Rowan PJ, Cofta-Woerpel L, Mazas CA, Vidrine JI, Reitzel LR, Cinciripini PM, Wetter DW. Evaluating Reactivity to ecological momentary assessment during smoking cessation. Experimental and Clinical Psychopathology. 2007;15(4):382–389. doi: 10.1037/1064-1297.15.4.382. [DOI] [PubMed] [Google Scholar]
- Schüz B. Socio-economic status and theories of health behaviour: Time to upgrade a control variable. Br J Health Psychol. 2017;22(1):1–7. doi: 10.1111/bjhp.12205. [DOI] [PubMed] [Google Scholar]
- Schüz N, Walters JA, Frandsen M, Bower J, Ferguson SG. Compliance with an EMA monitoring protocol and its relationship with participant and smoking characteristics. Nicotine Tob Res. 2014;16(Suppl 2):S88–92. doi: 10.1093/ntr/ntt142. [DOI] [PubMed] [Google Scholar]
- Schwarz N. Retrospective and Concurrent Self-Reports: The Rationale for Real-Time Data Capture. In: Stone AA, Shiffman S, Atienza A, Nebeling L, editors. The science of real-time data capture: Self-reports in health research. New York: Oxford University Press; 2007. pp. 11–26. [Google Scholar]
- Shavers VL. Measurement of socioeconomic status in health disparities research. J Natl Med Assoc. 2007;99(9):1013–1023. [PMC free article] [PubMed] [Google Scholar]
- Shiffman S, Dunbar MS, Ferguson SG. Stimulus control in intermittent and daily smokers. Psychol Addict Behav. 2015;29(4):847–855. doi: 10.1037/adb0000052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S, Dunbar MS, Li X, Scholl SM, Tindle HA, Anderson SJ, Ferguson SG. Craving in intermittent and daily smokers during ad libitum smoking. Nicotine Tob Res. 2014a;16(8):1063–1069. doi: 10.1093/ntr/ntu023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S, Dunbar MS, Li X, Scholl SM, Tindle HA, Anderson SJ, Ferguson SG. Smoking patterns and stimulus control in intermittent and daily smokers. PLOS ONE. 2014b;9(3):e89911. doi: 10.1371/journal.pone.0089911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S, Stone AA, Hufford MR. Ecological momentary assessment. Annu Rev Clin Psychol. 2008;4:1–32. doi: 10.1146/annurev.clinpsy.3.022806.091415. [DOI] [PubMed] [Google Scholar]
- Singh-Manoux A, Marmot M. Role of socialization in explaining social inequalities in health. Soc Sci Med. 2005;60(9):2129–2133. doi: 10.1016/j.socscimed.2004.08.070. [DOI] [PubMed] [Google Scholar]
- Spicker P. Poor areas and the ‘ecological fallacy’. Radical Statistics. 2001;76:38–49. [Google Scholar]
- Thomas S, Fayter D, Misso K, Ogilvie D, Petticrew M, Sowden A, Worthy G, et al. Population tobacco control interventions and their effects on social inequalities in smoking: systematic review. Tob Control. 2008;17(4):230–237. doi: 10.1136/tc.2007.023911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Twyman L, Bonevski B, Paul C, Bryant J. Perceived barriers to smoking cessation in selected vulnerable groups: a systematic review of the qualitative and quantitative literature. BMJ Open. 2014;4(12):e006414. doi: 10.1136/bmjopen-2014-006414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wetter DW, Cofta-Gunn L, Irvin JE, Fouladi RT, Wright K, Daza P, Gritz ER, et al. What accounts for the association of education and smoking cessation? Prev Med. 2005;40(4):452–460. doi: 10.1016/j.ypmed.2004.07.001. [DOI] [PubMed] [Google Scholar]
- Wiltshire S, Bancroft A, Parry O, Amos A. ‘I came back here and started smoking again’: perceptions and experiences of quitting among disadvantaged smokers. Health Education Research. 2003;18(3):292–303. doi: 10.1093/her/cyf031. [DOI] [PubMed] [Google Scholar]


