Abstract
Although it is widely thought that childhood levels of cardiovascular (CV) risk factors are related to adult CV disease, longitudinal data directly linking the two are lacking. This paper describes the design and organization of the International Childhood Cardiovascular Cohort Consortium Outcomes Study (i3C Outcomes), the first longitudinal cohort study designed to locate adults with detailed, repeated, childhood biological, physical, and socioeconomic measurements and a harmonized database. I3C Outcomes uses a Heart Health Survey (HHS) to obtain information on adult CV endpoints, using mail, email, telephone, and clinic visits in the United States (U.S.) and a national health database in Finland. Microsoft Access, REsearch Data Capture (REDCap) (U.S.), LimeSurvey (Australia), and Medidata Rave data systems are used to collect, transfer and organize data. Self-reported CV events are adjudicated via hospital and doctor-released medical records. After the first two study years, participants (N=10,968) were more likely to be female (56% vs. 48%), non-Hispanic white (90% vs. 80%), and older (10.4 ± 3.8 years vs. 9.4 ± 3.3 years) at their initial childhood study visit than the currently non-recruited cohort members. Over 48% of cohort members seen during both adulthood and childhood have been found and recruited, to date, vs. 5% of those not seen since childhood. Self-reported prevalences were 0.7% Type 1 Diabetes, 7.5% Type 2 Diabetes, 33% hypertension, and 12.8% CV event. 32% of CV events were judged to be true. I3C Outcomes is uniquely able to establish evidence-based guidelines for child health care and to clarify relations to adult CV disease.
Keywords: Longitudinal cardiovascular risk study, Childhood cardiovascular risk factors, Adult Cardiovascular disease, Collaborative cohort study, Heart health survey
1. Introduction
It is generally accepted that cardiovascular (CV) and metabolic disease risk factors in childhood are related to development of adult CV disease [1–9]. While the main focus has been on obesity, other childhood CV risk factors, such as lipids and blood pressure (BP) (10–16), in addition to increases in body mass index (BMI) (17,18) have been shown to be significantly related to adult risk factor levels.
Although children virtually never suffer the adverse CV events experienced by adults, the importance of exposure to CV risk factors during childhood and early adulthood is emphasized by post-mortem examinations in the Bogalusa Heart Study (19) and the Pathobiologic Determinants of Atherosclerosis in Youth Study (20). These studies found that ante-mortem levels of CV risk factors in individuals dying during their teenage years are directly associated with the degree of atherosclerosis found in their arteries. Moreover, the Muscatine Study, the Bogalusa Heart Study and the Cardiovascular Risk in Young Finns Study have shown that exposure to CV risk factors in childhood is related to increased carotid artery intima media thickness (cIMT) and coronary artery calcification (21–25) in adulthood.
Despite evidence that CV risk factors track through childhood into early adulthood and that CV risk factors in youth are associated with early subclinical disease, there are no longitudinal data linking CV risk factors in childhood to adult CV disease outcomes. This is due, in part, to 1) a lack of childhood cohorts large enough or with adequate numbers of longitudinal observations of CV risk factors (beyond BMI) to assess an effect on adult CV endpoints; and 2) a lack of evidence-based childhood definitions for elevated levels of CV risk factors (26–31).
The National Heart, Lung and Blood Institute (NHLBI) Pediatric CV Risk Reduction Initiative (26) noted that the lack of longitudinal studies linking CV risk factor levels in childhood to CV endpoints in adulthood is a major clinical research gap that needs to be spanned. To that end, the International Childhood Cardiovascular Cohort (i3C) Consortium, consisting of seven major U.S. and international longitudinal studies, was formed in 2009 to close that research gap (32). Each of these studies was a primary contributor to development of the earliest standards for CV risk factors in children and provided early evidence for tracking of CV risk factors from childhood to young adulthood.
The purpose of this paper is to describe the design, organizational structure, data systems and management of the National Institutes of Health (NIH) funded i3C Outcomes Study, the first longitudinal cohort study designed to locate large numbers of adults with detailed biological, physical, and socioeconomic measurements obtained in childhood and with a longitudinally focused harmonized data base. This study has significant potential for clarifying the relation between childhood levels of CV risk factors and development of adult CV disease, with an acknowledged public health goal of establishing evidence-based preventive guidelines that can be introduced during childhood.
2. Methods
2.1. The I3C Consortium Cohorts
The seven cohorts participating in this Outcomes Study previously have been described in detail (32); a brief description follows, and a summary of the cohorts with respect to study design and follow-up is shown in Table 1.
Table 1.
Summary of the i3C Outcomes Study cohorts at enrollment, number of childhood visits, and mean age in 2017, the midpoint of when Heart Health Surveys will be completed.
| Cohort* | Sampling Source | First Visit Year | Total Enrolled | Initial Ages | Race (%White) | Max Number Childhood Visits | Mean (SD) Age in 2017 |
|---|---|---|---|---|---|---|---|
| BHS | Schools | 1973 | 11,961 | 3–18 | 65% | 9 | 45 (8.3) |
| MN | |||||||
| PHBPC | Schools | 1977 | 2,694 | 6–8 | 80% | 20 | 47 (0.8) |
| NaKS | Schools | 1985 | 283 | 11–14 | 86% | 16 | 44 (1.4) |
| INS | Schools | 1995 | 586 | 11–19 | 80% | 3 | 33 (3.3) |
| MUSC | Schools | 1970 | 11,377 | 5–18 | 95% | 6 | 57 (5.8) |
| NGHS | Schools | 1987 | 870 | 9–10 | 50% | 10 | 40 (0.7) |
| PLRS | Schools | 1973 | 2,324 | 5–19 | 73% | 3 | 55 (3.6) |
| CDAH | Schools | 1985 | 8,498 | 7–15 | 97% | 1 | 43 (2.6) |
| YFS | Random | 1980 | 3,596 | 3–18 | 100% | 5 | 48 (5.0) |
BHS=Bogalusa Heart Study (Louisiana); MN=Minnesota Childhood Cohort Studies (PHBPC=Prevention of High Blood Pressure in Children; NaKs=Sodium-Potassium BP Trial in Children; INS=Obesity/Insulin Resistance Study); MUSC=Muscatine Study (Iowa); NGHS=NHLBI Growth and Health Study (Ohio); PLRS=Princeton Lipid Research Study (Ohio); CDAH=Childhood Determinants of Adult Health Study (Australia); YFS=Cardiovascular Risk in Young Finns Study (Finland)
Only the Cincinnati clinic of NGHS is included
2.1.1. The Bogalusa Heart Study
The Bogalusa Heart Study (BHS) began in 1973, with nine subsequent cross-sectional screenings of children aged 3 to 18 years and participation rates of 80 to 93%. An additional 11 cross-sectional screenings at ages 19–62 years were conducted, with participation rates of 72 to 93%. Linking the 20 surveys provides 39,647 observations on 11,961 cohort members. In the most recent contact 1,298 of a sub-sample of recruited participants was examined between 2013–2016.
2.1.2. Minneapolis Childhood Cohort Studies
The Minneapolis Childhood Cohort Studies (MPLS) consist of three separate cohorts (ages 6–19 years), all randomly sampled after school screenings. The Prevention of High BP in Children study (PHBPC) was initiated in 1977–78 with BP screening of 10,423 6–8 year olds. A cohort of 1,207 was selected for long-term evaluation, with stratification for age and race. They were seen twice yearly through grade school, once yearly through high school, and at ages 19, 24. At age 40 81% of a limited group of 872 individuals with children were found for a comprehensive anthropometric and metabolic screening.
The Sodium Potassium BP trial (NaKs) was initiated in 1985–86. After BP screening of 19,452 11–14 year olds, 283, stratified by BP, were entered into a sodium-potassium clinical trial and seen four times/year for three years. At age 26 years 174 of 278 (63%) participated in an anthropometric and metabolic screening.
The Obesity/Insulin Resistance study (INS) began in 1995. After school screening of 12,000 10–14 year olds, a cohort of 586, consisting of randomly recruited students and their siblings, had repeated measures of detailed CV risk factors and insulin clamp studies. In a study conducted between 2004–2008 466 of 817 (57%) completed an anthropometric and metabolic screening.
2.1.3. The Muscatine Study
The Muscatine Study (MUSC) was initiated in 1970 in the schools of Muscatine, Iowa. Approximately 70% of the eligible school population (11,377 students, 5–18 years at baseline) had data collected over the following 12 years. During 1982–91, a representative subset of 2,547 (age 20–39) was re-examined, and a subsample of those (n=906) was followed longitudinally between 1992–08. A representative subset (N=594) of the childhood cohort was recruited in 1999–2001 for an examination, and a follow-up examination of this subset was conducted in 2007–2008 with 82% participation.
2.1.4. The NHLBI Growth and Health Study
The NHLBI Growth and Health Study (NGHS) was started in 1987 as a longitudinal fixed-cohort study of girls (9–10 years at baseline and followed annually for 10 years to age 19) at three clinical centers (Richmond, CA, Cincinnati, OH, and Washington, DC). Only the Cincinnati center (N=870) is participating in this i3C Outcomes study. Yearly examinations were conducted between ages 19–24, and there were two visits between ages 25–29. The last in-person examination was conducted between 2003–2006, with recruitment of 535 participants, 70% of those eligible.
2.1.5. The Princeton Lipid Research Clinics Follow-up Study
The Princeton Lipid Research Clinics Follow-up Study (PLRS) began in 1973 as part of the NHLBI Lipid Research Clinics (LRC) Prevalence Study with enrollment of 6,775 6–19 year old children from the Princeton City School District (Cincinnati, OH). A random subset of 2,324 were selected for two childhood visits, and a family-based subset of those were seen between 1998–03 and participated in a heath-status questionnaire in 2010–12. The last in-person examination was conducted between 1998–2001 on 911 participants, 70% of those eligible for recruitment.
2.1.6. The Childhood Determinants of Adult Health Study
The Childhood Determinants of Adult Health (CDAH) Study started in 1985 with recruitment across Australia of 8,498 school children aged 7–15. Technical tests and blood samples were collected on 9, 12, and 15 year olds. A follow-up field clinic was conducted in 2004–06 at ages 26–36, and in 2009–10 a questionnaire-based assessment of health status was obtained. CDAH is currently attempting to examine all participants previously seen during young adulthood (N=4,947) and expects to see 1800 (36.4%).
2.1.7 The Cardiovascular Risk in Young Finns Study
The Cardiovascular Risk in Young Finns Study (YFS) is a population-based multicenter study in Finland and the largest European CV risk factor follow-up study from childhood to adulthood. Participants aged 3–18 years (N=3,596) were recruited in 1980, and this cohort has been followed-up every 3–6 years. The most recent in-person examination was in 2011 with participation of 2,041 individuals (62% of the 3,318 invited).
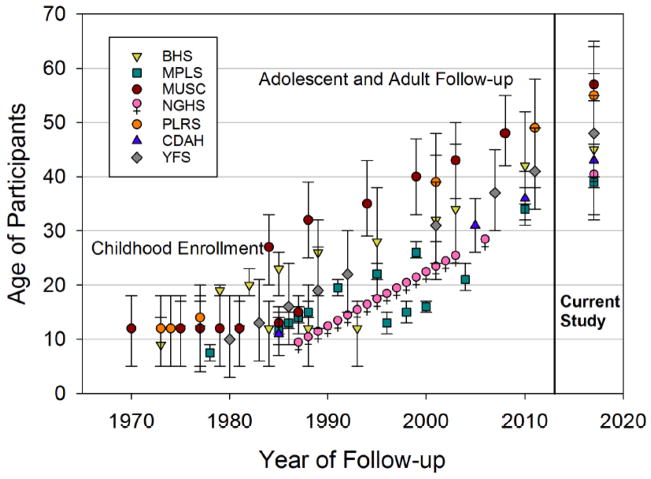
Members of these seven cohorts were enrolled at ages 3–19 in the 1970s and 1980s and at the midpoint of the current study (January 1, 2017) they were 32–65 years old, the age when CV events begin to significantly increase (33). Figure 1 shows the frequency and ages of repeat visits by cohort.
Figure 1.
Cohort ages by years of longitudinal visits
3. Study Design
The Specific Aims and Hypotheses for the Outcomes Study are as follows:
Specific Aim 1
To locate the childhood participants of five NIH-funded longitudinal studies in the U.S. (BHS, MUSC, PFS, MPLS, and NGHS) and two international studies (YFS and CDAH) in order to: 1) identify incident CV endpoints using self-reported morbidity validated by adjudication of medical records; and 2) identify decedents using the National Death Index and adjudicate cause of death for deceased participants.
Specific Aim 2
To evaluate relationships between childhood CV risk factors and adult CV endpoints.
Hypothesis 1
Adverse childhood/adolescent (age 3–19) CV risk factor levels (BMI, lipids [total cholesterol, LDL cholesterol, HDL cholesterol, and triglycerides], BP) are related to increased incidence of CV endpoints in adulthood.
Hypothesis 2
A CV risk score weighting childhood/adolescent risk factors (BMI, lipids, BP, age, sex and race/ethnicity) is a stronger predictor of adult CV endpoints than any individual risk factor.
Hypothesis 3
The relationship of individual risk factors or CV risk score with adult CV endpoints becomes stronger with increasing age from childhood (age 3–11) to adolescence (age 11–19).
Specific Aim 3
To evaluate the association of CV risk score trajectories on adult CV endpoints.
Hypothesis 4
Trajectories in the CV risk score from childhood (age 3–11) through adolescence (age 11–19) (i.e., high-high, high-low, low-high, low-low) are better predictors of adult CV endpoints than risk scores in either childhood (age 3–11) or adolescence (age 11–19) alone.
Hypothesis 5
Extension of trajectories in the CV risk score from childhood/adolescence (age 3–19) through adulthood (age>25) increases prediction of adult CV endpoints beyond the childhood/adolescence (age 3–19) risk scores or trajectories alone.
The i3C Outcomes Study is using a Heart Health Survey (HHS) developed by the i3C investigators to obtain information on adult CV endpoints (coronary heart disease, myocardial infarction, angina pectoris, heart failure, peripheral artery disease, stroke, transient ischemic attack, and abdominal aortic aneurysm); diagnostic tests for cardiovascular disease; related and other diseases (e.g., diabetes, hypertension, cancer); smoking; and use of pharmacologic agents. Initial contact is made by mail, email and/or telephone in the five United States cohorts, additionally by contact at a local dedicated clinic in the BHS, and by data obtained from the Finland national medical data base in the YFS study. The HHS is completed on paper forms returned to the respective cohort clinics or on-line by cohort members, or completed on-line by study coordinators during telephone interviews, except for YFS. Self-reports of CV endpoints identified during completion of the HHS forms are confirmed by review of medical records and expert adjudication.
This study was approved by the Institutional Review Boards (IRB) at each of the seven cohort sites. IRB approval was given to waive documentation of consent, and consent was obtained verbally over the phone. Coordinators explained the study to the participants using standardized language, addressed participant questions, and verified the participant’s willingness to participate prior to conducting the Heart Health Survey.
4. Data Collection
The Outcomes Study includes two Data Centers. The Finland data center, housed at the Research Centre of Applied and Preventive Cardiovascular Medicine at the University of Turku, Finland, has had the primary responsibility for organizing and harmonizing historical data beginning with the initial collaboration of the i3C Consortium cohorts. It will continue to be the primary center for current and future harmonized data.
The Cincinnati data center, housed at Cincinnati Children’s Hospital Medical Center (CCHMC) has responsibility for: 1) designing, implementing and maintaining data systems for collection of data related to current contact information, the HHS and adjudication; 2) ensuring quality control of data; 3) developing and implementing procedures for database lock and creation of analysis datasets; and 4) providing monitoring reports on progress of the study to the Outcomes Study Executive Committee.
Personally identifiable data, with the exception of birthdate and exam dates, are retained at each study site. Data on the recruitment progress and from the HHS are entered at each site either directly into the main study database or uploaded monthly to an Outcomes Study specific SharePoint site at CCHMC. The data are then incorporated into the main study database at the Cincinnati Data Center to ensure uniform and timely data cleaning and monitoring. After ensuring completeness and cleaning of HHS data, including sending queries to the sites for clarification about missing or questionable data, the data are placed in a data analysis file for merger with the harmonized database in Finland.
5. Data Systems
A Microsoft Access database is used to track recruitment status of participants and the acquisition of consent forms and death certificates. The database is constructed to maintain confidentiality of personal health information (PHI). All contact data from existing cohort databases were uploaded into the tracking system at the beginning of the study and are updated during the recruitment process. Tracking data are downloaded monthly by the sites to Excel spreadsheets and sent to the Cincinnati Data Center for quality control check and production of monitoring reports for the Executive Committee.
REsearch Data Capture (REDCap) (United States) and LimeSurvey (Australia) databases are used for completion of the HHS questionnaires by participant self-administration and/or direct entry of data by an interviewer during a telephone conversations with cohort members. Data from REDCap and LimeSurvey are downloaded on a monthly basis and sent to the Cincinnati Data Center, using a program designed to maintain confidentiality of PHI.
Medidata™ Rave is used for central (at CCHMC) organization and storage of data collected on the HHS forms, with scheduled incremental and full backups. Data either are entered by site personnel directly into the Rave system after collection on paper forms or are entered into REDCap or LimeSurvey by participants or by site interviewers during telephone interviews and forwarded to the Cincinnati data center for uploading into RAVE.
6. Recruitment Plan
6.1. Participant Contact
The initial contact with a participant is made via a mailed packet, including a letter introducing the study and linking it to their prior participation, an explanation of participant rights related to Institutional Review Board and HIPAA regulations, a contact update form, and a stamped, self-addressed envelope. The letter also offers the participant an opportunity to respond by email or by completion of a web-based (REDCap in the U.S. and LimeSurvey in Australia) contact update form. If no response is received after the initial mailing, attempts are made to reach the participant by repeated mailings, phone calls or email. The primary goal of the contact is completion of the Heart Health Survey (HHS) detailing CV diseases, related conditions (e.g., diabetes, hypertension), smoking history, and past and current medication use.
6.2. Data Collection in Finland
Medical data for Finnish individuals are available in a national medical database that includes information on all hospital discharges, outpatient visits, and surgical procedures. These data are linked to the existing YFS database by using a national social security number. Thus, data from childhood through adult life, are available without the need to locate and recruit participants. Finnish authorities update the data for hospital discharge and outpatient diagnoses annually. The data (ICD codes) include all diagnoses and procedures for each of the original 3,596 YFS participants during their life-course while they remain in Finland.
6.3. Search for Deceased Cohort Members
Active searches for deceased cohort members and causes of death are planned for all cohorts. In the U.S. searches will be conducted via the U.S. National Death Index (NDI), a database of all deaths in the U.S. since 1979. The NDI provides information on date, location and cause of death, matched by combinations of name, social security number, birthdate and other identifiable information submitted by the individual sites. Decedents’ death certificates will be obtained, and an attempt will be made to locate medical records and/or contact close relatives to confirm the cause and circumstances of death.
The YFS study has access to the Finnish NDI to search for deceased participants and cause of death.
The CDAH study has linked their cohort database with the Australia NDI on two previous occasions, most recently in 2012, and further linkage is planned.
6.4. Adjudication of CV Events
All CV events self-reported on the HHS will be adjudicated including fatal or non-fatal coronary heart disease, myocardial infarction, peripheral artery disease, stroke, aneurysm, angina pectoris, transient ischemic attack, and heart failure; we recognize the latter three may be more subjective and difficult to diagnose. Verification for all events will require review of hospital records. Heart failure due to non-CV disease (e.g., cardiomyopathy, cocaine use) will be excluded. All-cause and cause-specific non-CV mortality (based on ICD codes) will be secondary outcomes.
A signed consent is required from each participant reporting a CV event in order to request hospital or physician office records needed to confirm the event. We have found the hospital discharge data in the Finnish national registry to be highly accurate, based on adjudication of medical records from a randomly selected group of Finnish participants in which the adjudicated CV result matched the data obtained from the registry.
The adjudication staff includes two cardiologists, two stroke neurologists and one non-specialist with significant experience adjudicating outcomes for epidemiologic studies, with all adjudicators, except Dr. Prineas, at the Cincinnati site. Adjudications are being conducted with the adjudicators randomly selected and blinded to subject ID and site, using an acrostic generated by the sites. Two adjudicators are assigned per event to review the available medical records and determine whether the self-reported event meets the definition of a study outcome. Discrepancies between adjudicators are resolved through discussion and consensus.
A centralized medical records adjudication portal was designed to enable blinded adjudication of medical records and supporting documentation to determine the validity of self-reported CV outcomes for the study. Sites are required to redact medical records of any PHI or site-specific information (e.g., hospital name or city) and develop a novel acrostic for the participant which, unlike the study ID, does not include an indication of which site submitted the record. The sites are not involved in assessing the adjudication.
To estimate the expected number of true CV endpoints, we used data from the CARDIA study (34), which has followed a population-based sample of 18–30 year olds for over 30 years, identifying and adjudicating CV events and using a definitional framework similar to the framework in the current study. Using observed CARDIA age-specific adjudicated event rates (age 35 0.29%; age 40 1.06%; age 45 1.99%; and age 50 3.46%, and interpolated for intermediate ages), we project 665 adjudicated fatal/non-fatal CV events (Table 2).
Table 2.
Estimated recruitment (i.e. completion of Heart Health Survey) and number of CV events
| Recruitment* | Estimated number of CV Events** | |||
|---|---|---|---|---|
| Cohort | Targeted for Recruitment | Expected Recruitment (%) | CV Event rate (%) | Expected CV Events |
| BHS | 6,000 | 3,900 (65%) | 2.0% | 78 |
| MPLS | 2,171 | 1,412 (65%) | 1.8% | 25 |
| MUSC | 11,377 | 8,533 (75%) | 4.3% | 371 |
| NGHS | 870 | 566 (65%) | 1.1% | 6 |
| PLRS | 2,330 | 1,515 (65%) | 4.6% | 70 |
| CDAH | 5,170 | 3,361 (65%) | 1.6% | 54 |
| YFS | 3,596 | 3,480 (97%) | 1.7% | 61 |
| TOTAL | 31,514 | 22,833 (73%) | 665 | |
See Table 1 for cohort names
Targeted and expected recruitment are based on estimates from each site’s PI, with a total Study expectation that 31,514 of the 40,000 cohort members would be found and 22,833 would agree to participate in this study.
Estimated number of CV events was based on data from the CARDIA study (37).
7. Statistical Methods
For this paper statistical analyses were performed to describe the data obtained from the original cohorts, with data presented as mean ± SD or percent among all cohort members ever seen in the cohorts and in those who have been successfully recruited into the Outcomes study, as of December 31, 2016. The difference between first measurement of childhood variables in those who have been successfully recruited so far vs those in the full dataset not yet recruited were tested using 2 sample t-tests. We defined recruitment success as the number of people who have so far completed the HHS divided by the number of people in the harmonized data base, according to number of visits in childhood, adolescence and adulthood, counting the YFS 2010–2012 survey participants as recruited.
8. Results
Most of the historic cohort data transfer from each of the seven cohort sites to the harmonized database in the Finland data center was completed within one year of initiation of the i3c Outcomes Study. Harmonization of the childhood smoking and socioeconomic status variables is ongoing, while harmonization has not been attempted for the complex diet and physical activity variables. Table 3 shows the clinical and laboratory data by cohort at the participants’ first childhood measurement.
Table 3.
Characteristics at the first childhood measure for the seven cohorts in the i3C Outcomes Study and overall, (N=42,189).
| BHS | CDAH | MN | MUSC | NGHS | PLRS | YFS | P for diff betwee n studies |
Total | ||
|---|---|---|---|---|---|---|---|---|---|---|
| N total | 11,961 | 8,498 | 3,563 | 11,377 | 870 | 2,324 | 3,596 | - | 42,189 | |
| Age, years* | Mean (SD) | 8.7 (3.3) | 10.9 (2.5) | 8.7 (2.8) | 9.5 (3.5) | 9.5 (0.5) | 12.0 (3.4) | 10.4 (5) | <0.001 | 9.7 (3.5) |
| Range | 3–19 | 7–15 | 6–12 | 5–19 | 9–11 | 4–19 | 3–18 | 3–19 | ||
| Childhood stage | <0.001 | |||||||||
| Early childhood (3–11 years) | N (%) | 9,307 (77.8) | 4,872 (57.3) | 2,802(78.6) | 8,175 (71.9) | 870 (100) | 1,043 (44. 9) | 1806 (50.2) | 28,875 (68.4) | |
| Adolescence (12–19 years) | N (%) | 2,654 (22.2) | 3,626 (42.7) | 761 (21.4) | 3,202 (28.1) | 0 (0) | 1,281 (55.1) | 1790 (49.8) | 13,314 (31.6) | |
| Sex | <0.001 | |||||||||
| Male | N (%) | 6,142 (51.4) | 4,307 (50.7) | 1,844 (51.8) | 5,754 (50.6) | 0 (0) | 1,170 (50.3) | 1,764 (49.1) | 20,981 (49.7) | |
| Female | N (%) | 5,819 (48.6) | 4,191 (49.3) | 1,719 (48.2) | 5,623 (49.4) | 870 (100) | 1,154 (49.7) | 1,832 (50.9) | 21,208 (50.3) | |
| Race | <0.001 | |||||||||
| White | N (%) | 7,671 (64.1) | 8,207 (96.6) | 2,071 (58.1) | 11,272 (99.1) | 431 (49.5) | 1,621 (69.8) | 3,596 (100) | 34,869 (82.6) | |
| Black | N (%) | 4,290 (35.9) | 51 (0.6) | 1,071 (30.1) | 14 (0.1) | 439 (50.5) | 689 (29.6) | 0 (0) | 6,554 (15.5) | |
| Other | N (%) | 0 (0) | 240 (2.8) | 421 (11.8) | 91 (0.8) | 0 (0) | 14 (0.6) | 0 (0) | 766 (1.8) | |
| Body mass index, kg/m2 | N | 11,945 | 8,492 | 3,563 | 11,377 | 870 | 2,196 | 3,592 | 42,035 | |
| Mean (SD) | 17.6 (3.5) | 18.2 (2.9) | 18.0 (4.1) | 18.2 (3.6) | 18.4 (3.8) | 19.4 (4.1) | 17.8 (3.1) | <0.001 | 18.0 (3.5) | |
| Median (25th,75th) | 16.5 (15.2, 18.9) | 17.7 (16.1, 19.8) | 16.7 (15.4, 19.5) | 17.2 (15.8, 19.8) | 17.5 (15.7, 20.2) | 18.6 (16.4, 21.5) | 17.1 (15.5, 19.8) | 17.1 (15.6, 19.7) | ||
| Weight, kg | N | 11,949 | 8496 | 3,563 | 11,377 | 870 | 2,200 | 3,594 | 42,049 | |
| Mean (SD) | 32.8 (15.2) | 39.9 (13) | 34.7 (17.3) | 36.2 (16.5) | 36.7 (10) | 46.2 (17.9) | 38.3 (18.3) | <0.001 | 36.6 (16) | |
| Median (25th,75th) | 27.6 (21.5, 40.7) | 37.5 (29.5, 49.0) | 27.4 (23.6, 41.1) | 30.5 (23.5, 45.9) | 34.7 (29.6, 41.6) | 44.7 (31.6, 57.7) | 35.3 (22.2, 52.8) | 31.9 (24.0, 46.7) | ||
| Height, cm | N | 11,955 | 8493 | 3,563 | 11,377 | 870 | 2,198 | 3,592 | 42,048 | |
| Mean (SD) | 133.1 (19.2) | 145.8 (15.4) | 134.8 (17.6) | 137.2 (19.5) | 140.7 (7.6) | 151.4 (17.9) | 141.2 (25.9) | <0.001 | 138.7 (19.7) | |
| Median (25th,75th) | 129.1 (117.7, 146.9) | 145.2 (133.4, 157.9) | 129.0 (123.0, 142.5) | 133.3 (120.8, 152.7) | 140.0 (135.6, 145.5) | 154.0 (137.5, 165) | 143.5 (120.4, 163.4) | 136.2 (123, 154.7) | ||
| Total cholesterol, mmol/L | N | 11,767 | 1,770 | 832 | 10,074 | 804 | 2,316 | 3,585 | 31,148 | |
| Mean (SD) | 4.25 (0.74) | 4.50 (0.75) | 3.97 (0.73) | 4.06 (0.70) | 4.39 (0.77) | 4.43 (0.82) | 5.29 (0.92) | <0.001 | 4.33 (0.84) | |
| Median (25th,75th) | 4.19 (3.75, 4.68) | 4.48 (3.99, 4.95) | 3.88 (3.47, 4.40) | 4.03 (3.59, 4.47) | 4.34 (3.83, 4.87) | 4.34 (3.83, 4.93) | 5.23 (4.68, 5.84) | 4.24 (3.75, 4.81) | ||
| Low-density lipoprotein cholesterol, mmol/L | N | 11,762 | 1,746 | 558 | 2,249 | 803 | 2,180 | 3,584 | 22,882 | |
| Mean (SD) | 2.44 (0.65) | 2.73 (0.68) | 2.32 (0.65) | 2.36 (0.60) | 2.66 (0.73) | 2.69 (0.72) | 3.43 (0.84) | <0.001 | 2.63 (0.78) | |
| Median (25th,75th) | 2.36 (1.98, 2.81) | 2.68 (2.28, 3.13) | 2.21 (1.89, 2.69) | 2.31 (1.96, 2.71) | 2.61 (2.17, 3.10) | 2.61 (2.20, 3.10) | 3.37 (2.87, 3.92) | 2.53 (2.09, 3.07) | ||
| High-density lipoprotein cholesterol, mmol/L | N | 11,751 | 1,750 | 832 | 2,252 | 803 | 2,167 | 3,584 | 23,139 | |
| Mean (SD) | 1.60 (0.49) | 1.44 (0.30) | 1.20 (0.28) | 1.30 (0.29) | 1.41 (0.31) | 1.41 (0.32) | 1.56 (0.31) | <0.001 | 1.51 (0.43) | |
| Median (25th,75th) | 1.57 (1.28, 1.89) | 1.43 (1.23, 1.63) | 1.16 (1.01, 1.37) | 1.27 (1.11, 1.47) | 1.40 (1.19, 1.60) | 1.37 (1.19, 1.60) | 1.54 (1.35, 1.75) | 1.47 (1.23, 1.76) | ||
| Triglycerides, mmol/L | N | 11,193 | 1,770 | 558 | 10,071 | 804 | 2,316 | 3,585 | 30,297 | |
| Mean (SD) | 0.75 (0.38) | 0.74 (0.38) | 1.03 (0.61) | 0.85 (0.43) | 0.90 (0.38) | 0.87 (0.44) | 0.66 (0.32) | <0.001 | 0.79 (0.41) | |
| Median (25th,75th) | 0.67 (0.51, 0.89) | 0.65 (0.50, 0.88) | 0.86 (0.62, 1.26) | 0.75 (0.55, 1.03) | 0.79 (0.64, 1.07) | 0.76 (0.58, 1.02) | 0.59 (0.45, 0.79) | 0.69 (0.52, 0.95) | ||
| Systolic blood pressure, mmHg | N | 11,961 | 2,737 | 3,563 | 11,374 | 870 | 1,729 | 3,587 | 35,821 | |
| Mean (SD) | 98.6 (10.1) | 109.6 (13.3) | 105.6 (11.4) | 106.3 (14.4) | 101.0 (8.6) | 103.0 (12.9) | 112.5 (12.2) | <0.001 | 104.2 (13.1) | |
| Median (25th,75th) | 97.7 (91.7, 104.7) | 109.0 (100.0, 118.0) | 105.0 (98.0, 113.0) | 105.0 (96.0, 115.0) | 100.0 (95.0, 107.0) | 102.0 (94.0, 110.7) | 111.3 (104.0, 120.0) | 103.0 (94.7, 112.0) | ||
| Diastolic blood pressure phase V, mmHg | N | 11,958 | 2,722 | 3,563 | 11,361 | 870 | 1,638 | 3,530 | 35,642 | |
| Mean (SD) | 44.9 (12.7) | 66.0 (12.3) | 56.8 (14.6) | 62.6 (11.6) | 59.3 (10.4) | 62.4 (11.2) | 67.9 (9.9) | <0.001 | 56.8 (15.0) | |
| Median (25th,75th) | 45.7 (37.3, 53.3) | 67.0 (59.0, 74.0) | 59.0 (50.0, 66.0) | 62.0 (55.0, 70.0) | 60.0 (53.0, 66.0) | 62.0 (55.3, 70.0) | 68.0 (61.3, 74.7) | 58.0 (47.7, 68.0) | ||
| Glucose, mmol/L | N | 10,116 | 0 | 838 | 0 | 614 | 2,129 | 1,808 | 15,505 | |
| Mean (SD) | 4.64 (0.54) | 4.96 (0.51) | 4.09 (1.27) | 4.76 (0.5) | 4.73 (0.89) | <0.001 | 4.66 (0.65) | |||
| Median (25th,75th) | 4.61 (4.33, 4.94) | 4.93 (4.64, 5.22) | 4.16 (3.55, 4.66) | 4.77 (4.50, 5.00) | 4.66 (4.35, 4.97) | 4.66 (4.33, 5.00) | ||||
| Insulin, umol/l | N | 8,014 | 0 | 557 | 0 | 625 | 0 | 3,581 | 12,777 | |
| Mean (SD) | 9.94 (7.76) 8.00 | 11.21 (9.20) | 15.04 (16.99) | 9.57 (5.95) | <0.001 | 10.14 (8.17) | ||||
| Median (25th,75t h) | (5.60, 12.00) | 9.00 (5.50, 13.70) | 11.10 (7.80, 16.50) | 8.50 (5.00, 12.50) | 8.00 (5.50, 12.00) |
See Table 1 for cohort names.
Age represents age when a participant entered the study.
The values for each variable represent the first clinic visit where this variable was measured; not all variables for an individual cohort member were necessarily measured at the same clinic visit.
Statistical comparisons across cohorts were done using Chi-square for categorical variables and analysis of variance for continuous variables.
The mean age at entry was 9.7 ± 3.5 years, with 28,875 (68%) initially recruited during childhood (3–11 years) and 13,314 (32%) during adolescence (12–19 years). Virtually all were white (83%) or black (15%). Table 4 shows the number of repeat measures in the total cohort for each variable.
Table 4.
Number (% of total) of i3C cohort members* with repeated measures for each variable
| Variable | Number of cohort members (N and % of total) by number of repeated measures for each variable in between ages of 3 and 19 years | |||||
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5+ | Total** | |
| Body mass index | 20746 (49.4) | 6659 (15.8) | 5753 (13.7) | 3701 (8.8) | 5176 (12.3) | 42035 |
| Weight | 20755 (49.4) | 6660 (15.8) | 5755 (13.7) | 3700 (8.8) | 5179 (12.3) | 42049 |
| Height | 20754 (49.4) | 6642 (15.8) | 5760 (13.7) | 3708 (8.8) | 5184 (12.3) | 42048 |
| Total cholesterol | 12028 (38.6) | 8095 (26.0) | 5775 (18.5) | 3438 (11.0) | 1812 (5.8) | 31148 |
| Low-density lipoprotein cholesterol | 11116 (48.6) | 4519 (19.7) | 3724 (16.3) | 1954 (8.5) | 1569 (6.9) | 22882 |
| High-density lipoprotein cholesterol | 11390 (49.2) | 4514 (19.5) | 3739 (16.2) | 1940 (8.4) | 1556 (6.7) | 23139 |
| Triglycerides | 11877 (39.2) | 8113 (26.8) | 5748 (19.0) | 3188 (10.5) | 1371 (4.5) | 30297 |
| Systolic blood pressure | 14807 (41.3) | 6436 (18.0) | 5862 (16.4) | 3530 (9.9) | 5186 (14.5) | 35821 |
| Diastolic blood pressure phase V | 14724 (41.3) | 6780 (19.0) | 5532 (15.5) | 3511 (9.9) | 5095 (14.3) | 35642 |
| Glucose | 8958 (57.8) | 3533 (22.8) | 1918 (12.4) | 884 (5.7) | 212 (1.4) | 15505 |
| Insulin | 5885 (46.1) | 3588 (28.1) | 3078 (24.1) | 218 (1.7) | 8 (0.1) | 12777 |
Ages 3–19
Total number of cohort members with at least one measure for the given variable
The results presented herein represent progress through the initial two years of study funding, i.e., from December 1, 2014 through December 31, 2016. The study is funded through November 30, 2019. Based on experience by each of the cohort Principal Investigators, it was anticipated that the sites would be able to locate approximately 31,000 of the approximately 40,000 total cohort members and that approximately 22,000 would agree to participate in this study, i.e., complete the HHS (Table 2).
As of December 31, 2016, data were successfully obtained for 10,968 participants. This includes 3,596 from the Young Finns Study, which uses the Finnish national health service data base, thus precluding the need to search for participants and resulting in obtaining needed clinical data. In contrast, the U.S. and Australia (even though the latter has a national health care system) do not have access to national health records. Thus, the need to search for participants from U.S. and Australian cohorts has resulted in a lower percentage of participants being found. The percentages of completed HHS by U.S. and Australia sites according to the number of attempted participant contacts is as follows: BHS 30%, CDAH 65%, MN 53%, MUSC 57%, NGHS 41%, PLRS 32%. The majority of HHS (57%) were completed by direct telephone interviews by site recruiters, 6% were completed by participants using paper forms mailed to them and returned by mail, 24% were completed by online survey, and 13% were completed in Bogalusa by participants coming into a dedicated clinic or recruiters going out to find participants in the community. Based on self-reporting, as recorded on the HHS, 44 (0.7%) reported Type 1 Diabetes, 482 (7.5%) reported Type 2 Diabetes, 2110 (33%) reported hypertension, and 755 (12.8%) reported a CV event. Table 5 shows that recruitment and completion of the HHS form have been most successful in participants seen during adulthood, (i.e., generally within the past 15–20 years), in addition to either childhood, adolescence or both.
Table 5.
Association between the pattern of U.S. and Australia age-related clinic visits and recruitment of cohort members into the Outcomes Study
| Pattern of Age-related clinic visits | ||||
|---|---|---|---|---|
| Childhood (3–11 years) | Adolescence (12–19 years) | Adulthood (20+ years) | Number of cohort members with this pattern | Completion of HHS form: N (%) |
| Yes | Yes | Yes | 6057 | 3368 (56%) |
| Yes | Yes | No | 7509 | 1431 (19%) |
| No | Yes | Yes | 7341 | 3955 (54%) |
| No | Yes | No | 5973 | 569 (10%) |
| Yes | No | Yes | 2876 | 985 (34%) |
| Yes | No | No | 12,433 | 660 (5%) |
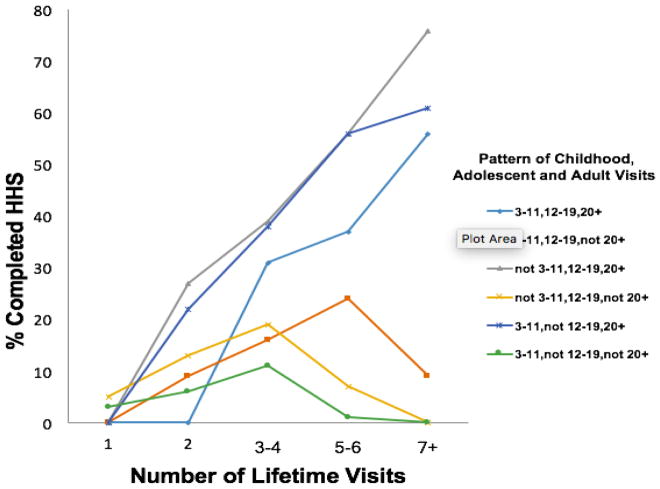
Table 5 and Figure 2 shows that U.S. and Australia cohort members who participated in more repeated examinations prior to the Outcomes Study were more likely to complete a HHS. However, as also shown in the figure, particularly in the group seen in childhood and adolescence but not adulthood, the number of repeated measures was not as influential in recruitment as having had an adult visit.
Figure 2.
Recruitment success (completion of HHS) according to number and age of longitudinal visits in U.S. and Australia cohorts
Table 6 compares the data obtained at the initial enrollment into the cohorts between the recruited participants (i.e., those completing the HHS) and the not-recruited participants.
Table 6.
Comparison of variables between recruited and not recruited, according to first measures
| Recruited (completed HHS) (N=10968)** | Not recruited (N=31221) | Difference* (Recruited vs. Not) | ||||
|---|---|---|---|---|---|---|
| N | Mean (SD) or % | N | Mean (SD) or % | Mean (SE) or % | P for diff | |
| Sex | ||||||
| Male | 4832 | 44.1% | 16149 | 51.7% | −7.6% | <0.001 |
| Female | 6136 | 55.9% | 15072 | 48.3% | ||
| Race | <0.001 | |||||
| White | 9880 | 90.1% | 24989 | 80.0% | 10.1% | |
| Black | 1006 | 9.2% | 5548 | 17.8% | −8.6% | |
| Other | 82 | 0.7% | 684 | 2.2% | −1.5% | |
| Age, year | 10968 | 10.4 (4.0) | 31221 | 9.5 (3.3) | 0.9 (0.1) | <0.001 |
| Age range at first visit | ||||||
| Early childhood (3–11 year) | 6444 | 58.8% | 22431 | 71.8% | −13.0% | <0.001 |
| Adolescence (12–19 year) | 4524 | 41.2% | 8790 | 28.2% | ||
| Body mass index, kg/m2 | 10944 | 18.3 (3.6) | 31091 | 18.0 (3.5) | 0.3 (0.1) | <0.001 |
| Weight, kg | 10947 | 39.2 (17.2) | 31102 | 35.6 (15.5) | 3.6 (0.2) | <0.001 |
| Height, cm | 10944 | 142.3 (21.6) | 31104 | 137.5 (18.8) | 4.8 (0.2) | <0.001 |
| Total cholesterol, mmol/L | 9301 | 4.63 (0.97) | 21847 | 4.21 (0.75) | 0.42 (0.01) | <0.001 |
| Low-density lipoprotein cholesterol, mmol/L | 7027 | 2.97 (0.89) | 15855 | 2.48 (0.67) | 0.49 (0.01) | <0.001 |
| High-density lipoprotein cholesterol, mmol/L | 7091 | 1.52 (0.38) | 16048 | 1.51 (0.45) | 0.01 (0.01) | 0.27 |
| Triglycerides, mmol/L | 9201 | 0.79 (0.41) | 21096 | 0.79 (0.41) | 0.00 (0.01) | 0.83 |
| Systolic blood pressure, mmHg | 9888 | 108.4 (13.4) | 25933 | 102.6 (12.7) | 5.8 (0.2) | <0.001 |
| Diastolic blood pressure phase V, mmHg | 9805 | 62.2 (13.8) | 25837 | 54.7 (15.0) | 7.5 (0.2) | <0.001 |
| Glucose, mmol/L | 4355 | 4.69 (0.78) | 11150 | 4.65 (0.59) | 0.04 (0.01) | <0.001 |
| Insulin, umol/l | 5210 | 10.20 (7.45) | 7567 | 10.10 (8.63) | 0.10 (0.15) | 0.50 |
SD: standard deviation; SE: standard error of the mean difference; HHS: Heart Health Survey
All differences, except high-density lipoprotein cholesterol, triglycerides and insulin, are significant (P<0.05). Differences in proportion or mean values (standard error) were present
All Young Finns Study participants are included here, because the Finnish registry includes cardiovascular disease ascertainment in everyone; 2041 attended in 2010–12 and have other information that was included in the HHS
Statistical comparisons across cohorts were done using Chi-square for categorical variables and t-test for continuous variables.
Recruited cohort members were more likely to be female (56% vs. 48%), non-Hispanic white (90% vs. 80%), and were approximately one year older than the non-recruited cohort members (10.4 ± 3.8 years vs. 9.4 ± 3.3 years) at their initial study visit. Most of the mean values were slightly, but significantly, higher in the recruited group given the large sample sizes, consistent with the older age at first study visit.
Adjudication of reported CV events is in the early stages. Medical records have been reviewed by the adjudicating team from 247 participants reporting a CV event, with 78 (32%) judged to be true events. These results are consistent with the numbers of events expected in planning this study.
As of December 31, 2016, 1297 cohort deaths have been reported during the recruitment process, but, at this time, only 269 are confirmed deceased by either NDI search, proxy interview (i.e., interview with a relative) or death certificate.
9. Discussion
It has been approximately 50 years since the first childhood cohorts were recruited specifically for the study of CV risk factors, with a goal of ultimately relating childhood data to adult CV disease. Despite a wealth of information on childhood CV risk factor levels and CV risk factor tracking data from childhood into young adulthood, this goal has not yet been achieved and key questions remain unanswered: 1) Can individuals recruited in early life for detailed CV risk factor measurement be readily found in adulthood and to what extent will they participate in efforts to gain access to complex information on their health experiences; and 2) what is the strength of the relationship between childhood CV risk factor data and adult CV morbidity and mortality.
This i3C Outcomes Study has the potential to answer those questions and has been successful in its early stages in recruiting cohort members and obtaining the data required. Longitudinal recruitment quotas, calculated to achieve the number of participants needed for adequate statistical power, are being reached. The largest proportion of the recruitment comes from the most recently seen participants, i.e., seen as adults, and the group with the largest number of repeat visits. Thus, this is the group with whom the Consortium has the longest history of research, and we expect ultimately to recruit approximately 70% of them. Nevertheless, the results, to date, confirm the expectation in designing this study of potential difficulty in locating a significant number of childhood participants in the U.S. and Australia cohorts. This is in contrast to the ease of obtaining data from the Finnish health registry and emphasizes the additional resources and effort required to complete long-term follow-up in the U.S. and Australia.
Although recruitment goals are currently being met, modification of strategies for future recruitment is regularly discussed. The sites are turning toward a focus on telephone contact because of greater success with locating participants and completing HHS. In addition, cohorts are using current technology (e.g., social media), and cohorts in smaller population areas (i.e., Muscatine and Bogalusa) have had success and are increasing use of direct non-telephone town contacts and through participant relatives.
The harmonized database, containing all data accumulated by the individual cohorts, has been completed, with the exception of smoking, diet and physical activity data which are currently being compiled. The most recent data review shows that the CV risk variables of the currently recruited participants, while statistically significantly different, are similar to the overall i3C Consortium participants and, in particular, to the not yet recruited individuals. The number of events being self-reported by recruited participants, a critical factor in this study, is meeting expectations, as is the percentage of events adjudicated to be true events.
It is highly unlikely that any single cohort will be able to provide meaningful data on the relation between childhood CV risk factors and adult CV events/outcomes, because their limited sizes result in limited statistical power. This Outcomes Study, a collaboration of seven cohorts followed from childhood into adulthood is designed to overcome those limitations. It will establish standards for childhood levels of CV risk factors based on actual documented CV endpoints and will have sufficient power to compare prediction of outcomes at developmental milestones (e.g., childhood vs adolescence).
There currently is limited evidence regarding the independent contribution of childhood CV risk factor profiles to adult disease. This is related, in part, to developmental changes in levels of risk factors during childhood (35–38) and developmental changes occurring as children progress into adulthood. For instance: 1) childhood BMI, which has a statistically significant tracking effect from childhood to adulthood (39,40), has been shown to have a relatively weak and inconsistent relationship with both adult CV disease and metabolic syndrome components; 2) overweight or obese children in the i3C consortium who became non-obese by adulthood had similar risks of type 2 diabetes (T2D), hypertension, dyslipidemia, and cIMT as found in individuals who were never obese (41); and 3) hypertensive children with normal BP as an adult have significantly lower cIMT compared to children with persistent hypertension or with incident adult hypertension (42). This Outcomes Study will clarify the relation of risk factor change between childhood and adolescence, as well as between adolescence and adulthood, to risk of adult CV endpoints.
The American Heart Association now emphasizes the importance of “ideal” CV health beginning in childhood as a goal to reduce adult CV disease (43). While we support the general philosophy and goals of ideal health, the fact remains that no studies have confirmed a beneficial relation of childhood ideal CV health to CV health in adulthood, and recent studies have shown a low prevalence of ideal CV health in both adults (44–46) and children (47).
Thus, the issue for childhood caregivers continues to be how to recognize the children at highest risk for CV disease, with the inference it will lead to effective intervention strategies and reduce the incidence of CV morbidity and mortality. To date, no studies have been able to comprehensively examine that relation. By assembling the only large set of longitudinal data available world-wide, and with the success, to date, of recruitment into this study, this Outcomes Study will be able to establish evidence-based guidelines for child health care providers, with the potential to clarify the relation to adult CV disease.
Acknowledgments
10. Funding
This work was supported by the National Institutes of Health (grant number RO1HL121230).
Harmonization and other data work in Finland prior to obtaining NIH funding was supported by The Academy of Finland.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Cali AM, Caprio S. Obesity in children and adolescents. J Clin Endocrinol Metab. 2008;93(11 Suppl 1):S31–36. doi: 10.1210/jc.2008-1363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chiarelli F, Marcovecchio ML. Insulin resistance and obesity in childhood. Eur J Endocrinol. 2008;159(Suppl 1):S67–74. doi: 10.1530/EJE-08-0245. [DOI] [PubMed] [Google Scholar]
- 3.Freedman DS, Dietz WH, Srinivasan SR, Berenson GS. The relation of overweight to cardiovascular risk factors among children and adolescents: The Bogalusa Heart Study. Pediatrics. 1999;103(6 Pt 1):1175–1182. doi: 10.1016/j.jpeds.2006.08.042. [DOI] [PubMed] [Google Scholar]
- 4.Freedman DS, Mei Z, Srinivasan SR, Berenson GS, Dietz WH. Cardiovascular risk factors and excess adiposity among overweight children and adolescents: The Bogalusa Heart Study. J Pediatr. 2007;150:12–17 e2. doi: 10.1016/j.jpeds.2006.08.042. [DOI] [PubMed] [Google Scholar]
- 5.Goodman E, Dolan LM, Morrison JA, Daniels SR. Factor analysis of clustered cardiovascular risks in adolescence: obesity is the predominant correlate of risk among youth. Circulation. 2005;111:1970–1977. doi: 10.1161/01.CIR.0000161957.34198.2B. [DOI] [PubMed] [Google Scholar]
- 6.Nathan BM, Moran A. Metabolic complications of obesity in childhood and adolescence: more than just diabetes. Curr Opin Endocrinol Diabetes Obes. 2008;15:21–29. doi: 10.1097/MED.0b013e3282f43d19. [DOI] [PubMed] [Google Scholar]
- 7.Sinaiko AR, Jacobs DR, Jr, Steinberger J, Moran A, Luepker R, Rocchini AP, Prineas RJ. Insulin resistance syndrome in childhood: associations of the euglycemic insulin clamp and fasting insulin with fatness and other risk factors. Journal of Pediatrics. 2001;139:700–707. doi: 10.1067/mpd.2001.118535. [DOI] [PubMed] [Google Scholar]
- 8.Sinaiko AR, Steinberger J, Moran A, Prineas RJ, Vessby B, Basu S, Tracy R, Jacobs DR., Jr Relation of body mass index and insulin resistance to cardiovascular risk factors, inflammatory factors, and oxidative stress during adolescence. Circulation. 2005;111:1985–1991. doi: 10.1161/01.CIR.0000161837.23846.57. [DOI] [PubMed] [Google Scholar]
- 9.Warnberg J, Marcos A. Low-grade inflammation and the metabolic syndrome in children and adolescents. Curr Opin Lipidol. 2008;19:11–15. doi: 10.1097/MOL.0b013e3282f4096b. [DOI] [PubMed] [Google Scholar]
- 10.Mahoney LT, Lauer RM, Lee J, Clarke WR. Factors affecting tracking of coronary heart disease risk factors in children. The Muscatine Study. Annals of the New York Academy of Sciences. 1991;623:120–132. doi: 10.1111/j.1749-6632.1991.tb43723.x. [DOI] [PubMed] [Google Scholar]
- 11.Morrison JA, Friedman LA, Wang P, Glueck CJ. Metabolic syndrome in childhood predicts adult metabolic syndrome and type 2 diabetes mellitus 25 to 30 years later. J Pediatr. 1991;152:201–206. doi: 10.1016/j.jpeds.2007.09.010. [DOI] [PubMed] [Google Scholar]
- 12.Porkka KV, Viikari JS, Taimela S, Dahl M, Akerblom HK. Tracking and predictiveness of serum lipid and lipoprotein measurements in childhood: a 12-year follow-up. The Cardiovascular Risk in Young Finns study. Am J Epidemiol. 1994;140:1096–1110. doi: 10.1093/oxfordjournals.aje.a117210. [DOI] [PubMed] [Google Scholar]
- 13.Sinaiko AR, Steinberger J, Moran A, Hong CP, Prineas RJ, Jacobs DR., Jr Influence of insulin resistance, body mass index at age 13 on systolic blood pressure, triglycerides, and high-density lipoprotein cholesterol at age 19. Hypertension. 2006;48:730–736. doi: 10.1161/01.HYP.0000237863.24000.50. [DOI] [PubMed] [Google Scholar]
- 14.Sun SS, Grave GD, Siervogel RM, Pickoff AA, Arslanian SS, Daniels SR. Systolic blood pressure in childhood predicts hypertension and metabolic syndrome later in life. Pediatrics. 2007;119:237–246. doi: 10.1542/peds.2006-2543. [DOI] [PubMed] [Google Scholar]
- 15.Webber LS, Srinivasan SR, Wattigney WA, Berenson GS. Tracking of serum lipids and lipoproteins from childhood to adulthood. The Bogalusa Heart Study. Am J Epidemiol. 1991;133:884–899. doi: 10.1093/oxfordjournals.aje.a115968. [DOI] [PubMed] [Google Scholar]
- 16.Laitinen TT, Pahkala K, Venn A, Woo JG, Oikonen M, Dwyer T, Mikkila V, Hutri-Kahonen N, Smith KJ, Gall SL, Morrison JA, Viikari JS, Raitakari OT, Magnussen CG, Juonala M. Childhood lifestyle and clinical determinants of adult ideal cardiovascular health: The Cardiovascular Risk in Young Finns Study, the Childhood Determinants of Adult Health Study, the Princeton Follow-up Study. Int J Cardiol. 2013;169:126–133. doi: 10.1016/j.ijcard.2013.08.090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sinaiko AR, Donahue RP, Jacobs DR, Jr, Prineas RJ. Relation of weight and rate of increase in weight during childhood and adolescence to body size, blood pressure, fasting insulin, and lipids in young adults. The Minneapolis Children’s Blood Pressure Study. Circulation. 1999;99:1471–1476. doi: 10.1161/01.CIR.99.11.1471. [DOI] [PubMed] [Google Scholar]
- 18.Juhola J, Magnussen CG, Viikari JS, Kahonen M, Hutri-Kahonen N, Jula A, Lehtimaki T, Akerblom M, Pietikainen HK, Laitinen T, Jokinen E, Taittonen L, Raitakari OT, Juonala M. Tracking of serum lipid levels, blood pressure, and body mass index from childhood to adulthood: the Cardiovascular Risk in Young Finns Study. J Pediatr. 2011;159:584–590. doi: 10.1016/j.jpeds.2011.03.021. [DOI] [PubMed] [Google Scholar]
- 19.Berenson GS, Srinivasan SR, Bao W, Newman WP, 3rd, Tracy RE, Wattigney WA. Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults. The Bogalusa Heart Study. N Engl J Med. 1998;338:1650–1656. doi: 10.1056/NEJM199806043382302. [DOI] [PubMed] [Google Scholar]
- 20.McGill HC, Jr, McMahan CA, Gidding SS. Preventing Heart Disease in the 21st Century: Implications of the Pathobiological Determinants of Atherosclerosis in Youth (PDAY) Study. Circulation. 2008;117:1216–1227. doi: 10.1161/CIRCULATIONAHA.107.717033. [DOI] [PubMed] [Google Scholar]
- 21.Davis PH, Dawson JD, Riley WA, Lauer RM. Carotid intimal-medial thickness is related to cardiovascular risk factors measured from childhood through middle age: The Muscatine Study. Circulation. 2001;104:2815–2819. doi: 10.1161/hc4601.099486. [DOI] [PubMed] [Google Scholar]
- 22.Raitakari OT, Juonala M, Kähönen M, Taittonen L, Laitinen T, Mäki-Torkko N, Järvisalo MJ, Uhari M, Jokinen E, Rönnemaa T, Akerblom HK, Viikari JS. Cardiovascular risk factors in childhood and carotid artery intima-media thickness in adulthood: The Cardiovascular Risk in Young Finns Study. JAMA. 2003;290:2277–2283. doi: 10.1001/jama.290.17.2277. [DOI] [PubMed] [Google Scholar]
- 23.Li S, Chen W, Srinivasan S, Bond MG, Tang R, Urbina EM, Berenson GS. Childhood cardiovascular risk factors and carotid vascular changes in adulthood: The Bogalusa Heart Study. JAMA. 2003;290:2271–2276. doi: 10.1001/jama.290.17.2271. [DOI] [PubMed] [Google Scholar]
- 24.Mahoney LT, Burns TL, Stanford W, Thompson BH, Witt JD, Rost CA, Lauer RM. Coronary risk factors measured in childhood and young adult life are associated with coronary artery calcification in young adults: the Muscatine Study. J Am Coll Cardiol. 1996;27:277–284. doi: 10.1016/0735-1097(95)00461-0. [DOI] [PubMed] [Google Scholar]
- 25.Hartiala O, Magnussen CG, Kajander S, Knuuti J, Ukkonen H, Saraste A, Rinta-Kiikka I, Kainulainen S, Kähönen M, Hutri-Kähönen N, Laitinen T, Lehtimäki T, Viikari JS, Hartiala J, Juonala M, Raitakari OT. Adolescence risk factors are predictive of coronary artery calcification at middle age: the cardiovascular risk in young Finns study. J Am Coll Cardiol. 2012;60:1364–1370. doi: 10.1016/j.jacc.2012.05.045. [DOI] [PubMed] [Google Scholar]
- 26.Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report. Pediatrics. 2011;128(Suppl 5):S213–256. doi: 10.1542/peds.2009-2107C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.The Fourth Report on the Diagnosis, Evaluation, and Treatment of High Blood Pressure in Children and Adolescents. Pediatrics. 2004;114(2 Suppl 4th Report):555–576. doi: 10.1542/peds.114.2.S2.555. [DOI] [PubMed] [Google Scholar]
- 28.Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, Wei R, Curtin LR, Roche AF, Johnson CL. 2000 CDC Growth Charts for the United States: Methods and Development, in Vital Health Statistics. National Center for Health Statistics; 2002. [PubMed] [Google Scholar]
- 29.Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120(Suppl 4):S164–192. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 30.American Academy of Pediatrics. National Cholesterol Education Program: Report of the Expert Panel on Blood Cholesterol Levels in Children and Adolescents. Pediatrics. 1992;89(3 Pt 2):525–584. [PubMed] [Google Scholar]
- 31.Type 2 diabetes in children and adolescents. American Diabetes Association. Diabetes Care. 2000;23:381–389. doi: 10.2337/diacare.23.3.381. [DOI] [PubMed] [Google Scholar]
- 32.Dwyer T, Sun C, Magnussen CG, Raitakari OT, Schork NJ, Venn A, Burns TL, Juonala M, Steinberger J, Sinaiko AR, Prineas RJ, Davis PH, Woo JG, Morrison JA, Daniels SR, Chen W, Srinivasan SR, Viikari I, Berenson GS. Cohort Profile: The International Childhood Cardiovascular Cohort (i3C) Consortium. Int J Epidemiol. 2013;42:86–96. doi: 10.1093/ije/dys004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Roge VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Makuc DM, Marcus GM, Marelli A, Matchar DB, Moy CS, Mozaffarian D, Mussolino ME, Nichol G, Paynter NP, Soliman EZ, Sorlie PD, Sotoodehnia N, Turan TN, Virani SS, Wong ND, Woo D, Turner MB. Heart disease and stroke statistics—2012 update: a report from the American Heart Association. Circulation. 2012;125:e2–e220. doi: 10.1161/CIR.0b013e3182456d46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Friedman GD, Cutter GR, Donahue RP, Hughes GH, Hulley SB, Jacobs DR, Jr, Liu K, Savage PJ. CARDIA: study design, recruitment, and some characteristics of the examined subjects. J Clin Epidemiol. 1988;41:1105–1116. doi: 10.1016/0895-4356(88)90080-7. [DOI] [PubMed] [Google Scholar]
- 35.Berenson GS, Srinivasan SR, Cresanta JL, Foster TA, Webber LS. Dynamic changes of serum lipoproteins in children during adolescence and sexual maturation. Am J Epidemiol. 1981;113:157–70. doi: 10.1093/oxfordjournals.aje.a113080. [DOI] [PubMed] [Google Scholar]
- 36.deGroot I, Morrison JA, Kelly KA, Rauh JL, Mellies MJ, Edwards BK, Glueck CJ. Lipids in schoolchildren 6 to 17 years of age: upper normal limits. Pediatrics. 1977;60:437–443. [PubMed] [Google Scholar]
- 37.Moran A, Jacobs DR, Jr, Steinberger J, Hong CP, Prineas R, Luepker R, Sinaiko AR. Insulin resistance during puberty: results from clamp studies in 357 children. Diabetes. 1999;48:2039–2044. doi: 10.2337/diabetes.48.10.2039. [DOI] [PubMed] [Google Scholar]
- 38.van Stiphout WA, Hofman A, de Bruijn AM, Valkenburg HA. Distributions and determinants of total and high-density lipoprotein cholesterol in Dutch children and young adults. Prev Med. 1985;14:169–180. doi: 10.1016/0091-7435(85)90032-5. [DOI] [PubMed] [Google Scholar]
- 39.Freedman DS, Khan LK, Serdula MK, Dietz WH, Srinivasan SR, Berenson GS. Racial differences in the tracking of childhood BMI to adulthood. Obesity Research. 2005;13:928–35. doi: 10.1038/oby.2005.107. [DOI] [PubMed] [Google Scholar]
- 40.Bayer O, Kruger H, von Kries R, Toschke AM. Factors associated with tracking of BMI: a metaregression analysis on BMI tracking. Obesity (Silver Spring) 2011;19:1069–1076. doi: 10.1038/oby.2010.250. [DOI] [PubMed] [Google Scholar]
- 41.Juonala M, Magnussen CG, Berenson GS, Venn A, Burns TL, Sabin MA, Srinivasan SR, Daniels SR, Davis PH, Chen W, Sun C, Cheung M, Viikari JS, Dwyer T, Raitakari OT. Childhood adiposity, adult adiposity, and cardiovascular risk factors. N Engl J Med. 2011;365:1876–1885. doi: 10.1056/NEJMoa1010112. [DOI] [PubMed] [Google Scholar]
- 42.Juhola J, Magnussen CG, Berenson GS, Venn A, Burns TL, Sabin MA, Srinivasan SR, Daniels SR, Davis PH, Chen W, Kahonen M, Taittonen L, Urbina E, Viikar JS, Dwyer T, Raitakari OT, Juonala M. Combined effects of child and adult elevated blood pressure on subclinical atherosclerosis: The International Childhood Cardiovascular Cohort Consortium. Circulation. 2013;128:217–224. doi: 10.1161/CIRCULATIONAHA.113.001614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lloyd-Jones DM, Hong y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, Greenlund K, Daniels S, Nichol G, Tomaselli GF, Arnett DK, Fonarow GC, Ho PM, Lauer MS, Masoudi FA, Robertson RM, Roger V, Schwamm LH, Sorlie P, Yancy CW, Rosamond WD American Heart Association Strategic Planning Task F, and Statistics, C. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation. 2010;121:586–613. doi: 10.1161/CIRCULATIONAHA.109.192703. [DOI] [PubMed] [Google Scholar]
- 44.Oikonen M, Laitinen TT, Magnussen CG, Steinberger J, Sinaiko AR, Dwyer T, Venn A, Smith KJ, Hutri-Kahonen N, Pahkala K, Mikkila V, Prineas R, Viikari JS, Morrison JA, Woo JG, Chen W, Nicklas T, Srinivasan SR, Berenson G, Juonala M, Raitakari OT. Ideal cardiovascular health in young adult populations from the United States, Finland, and Australia and its association with cIMT: The International Childhood Cardiovascular Cohort Consortium. J Am Heart Assoc. 2010;2:e000244. doi: 10.1161/JAHA.113.000244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Huffman MD, Capewell S, Ning H, Shay CM, Ford ES, Lloyd-Jones DM. Cardiovascular health behavior and health factor changes (1988–2008) and projections to 2020: results from the National Health and Nutrition Examination Surveys. Circulation. 2011;125:2595–2602. doi: 10.1161/CIRCULATIONAHA.111.070722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Liu K, Daviglus ML, Loria CM, Colangelo LA, Spring B, Moller A, Lloyd-Jones DM. Healthy lifestyle through young adulthood and the presence of low cardiovascular disease risk profile in middle age: The Coronary Artery Risk Development in (Young) Adults (CARDIA) study. Circulation. 2012;125:996–1004. doi: 10.1161/CIRCULATIONAHA.111.060681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Shay CM, Ning H, Daniels SR, Rooks CR, Gidding SS, Lloyd-Jones DM. Status of cardiovascular health in US adolescents: prevalence estimates from the National Health and Nutrition Examination Surveys (NHANES) 2005–2010. Circulation. 2013;127:1369–1376. doi: 10.1161/CIRCULATIONAHA.113.001559. [DOI] [PubMed] [Google Scholar]