Abstract
Medicaid enrollment varies considerably among states. This study examined the association of Medicaid enrollment with the use of substance health services in the longitudinal National Epidemiologic Survey on Alcohol and Related Conditions of 2001–2005. Instrumental variable methods were used to assess endogeneity of individual-level Medicaid enrollment using state-level data as instruments. Compared to the uninsured, Medicaid covered adults were more likely to use substance use disorder treatment services over the next three years. States that have opted to expand Medicaid enrollment under the Affordable Care Act will likely experience further increases in the use of these service over the coming years.
Keywords: Medicaid, service use, substance use treatment, instrumental variables
1. INTRODUCTION
Medicaid enrollment varies across the states considerably. In the years before the recent implementation of the Affordable Care Act (ACA), these variations were mainly due to 1115 waivers that allowed states to offer Medicaid to individuals who would not be eligible under traditional Medicaid programs, mostly low-income adults who did not meet the “categorical” requirements (Holahan, Coughlin, Ku, Lipson, & Rajan, 1995). These initiatives were further strengthened through the Bush Administration’s Health Insurance Flexibility and Accountability (HIFA) initiative, which encouraged states to extend Medicaid to those with incomes below 200% of the Federal Poverty Level (FPL). As of January 2004, 19 states had implemented Medicaid expansion under 1115 waivers and another six, under the HIFA initiative (Baumrucker, 2004).
Partly as a result of these initiatives, the number of individuals enrolled in Medicaid increased from 9.5% of the non-elderly US population in 2000 to 16.9% in 2010 (National Center for Health Statistics, 2012). Several studies have examined the effect of these individual state Medicaid expansion programs on utilization of services for substance use disorders (SUD) (Callahan, Shepard, Beinecke, Larson, & Cavanaugh, 1995; Deck & McFarland, 2002; Deck, McFarland, Titus, Laws, & Gabriel, 2000; Deck, Wiitala, & Laws, 2006; Saunders & Heflinger, 2003). Among the various state Medicaid programs, those in Massachusetts, Oregon, Tennessee and California were most extensively studied. Overall, these programs have been successful in enrolling newly eligible participants and were, for the most part, associated with increased use of substance use disorder (SUD) services in the states that implemented the expansion programs. However, with few exceptions (Wen, Druss, & Cummings, 2015) little research has investigated the impact of these Medicaid expansion programs on the use of SUD services at a national level. These effects are important to examine because state variations in Medicaid enrollment are likely to persist or even deepen in years following the Supreme court’s decision that made Medicaid expansion under the ACA optional for states (Berliner, 2013).
In this study, a large and nationally representative longitudinal survey of the US general population was used to examine the association of Medicaid enrollment with future use of SUD treatment services. More sepcifically, data from participants of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) (Grant, Stinson, Dawson, Chou, Dufour, et al., 2004; Grant, Stinson, Dawson, Chou, Ruan, et al., 2004) were used to examine whether Medicaid enrollment at baseline was associated with the use of SUD services over the subsequent three-year follow-up.
NESARC remains the most recent longitudinal survey of the US population in which SUD and its treatments were assessed. Although the mix of SUDs has somewhat changed since the years when these data were collected, the prevalence of SUD treatment seeking and the financing and structure of SUD services have not changed markedly in this period (Han, Hedden, Lipari, Copello, & Kroutil, 2015; Mark et al., 2016). As a result, the findings would have relevance to the current debates about the benefits of expasion of Medicaid enrollement at a national level.
Insurance status may have a reciprocal relationship with service use (Rabinowitz, Bromet, Lavelle, Hornak, & Rosen, 2001), and therefore it may be “endogenous” in models assessing its association with service use. This is because service providers may help eligible individuals enroll in public insurance. Thus, individuals who used services in the past may be more likely to have enrolled in Medicaid and also use services in future. Without accurate information on the dates of enrollment in Medicaid and the first service contact it is not possible to adjust for this potential confounding effect.
The present analysis assessed the possible endogeneity of Medicaid insurance enrollment in the NESARC sample by applying instrumental variable techniques and using state-level variations in Medicaid enrollment as an instruments. Instrumental variable techniques address the issue of endogeneity by modeling individual-level Medicaid enrollment as a function of state-level prevalence of Medicaid enrollment. Assuming the validity of instruments, the “instrumented” or predicted individual-level Medicaid enrollment variable in these models would be free from the effect of prior service use or other individual-level factors that could confound the association with the outcomes. The use of state-level Medicaid enrollment instruments in this study is similar to past research that has used state variations in Medicaid eligibility and enrollment as instrumental variables to assess the association of public insurance enrollment with mortality in HIV infected individuals (Bhattacharya, Goldman, & Sood, 2003).
Specifically, in this study, we tested the hypothesis that Medicaid enrollment at baseline would be associated with increased use of SUD treatment services at follow-up. It was further hypothesized that this increase would be more marked for services that are typically covered by insurance (e.g., outpatient services) as compared to services that are not covered by insurance (e.g., 12-step programs).
2. MATERIAL AND METHODS
2.1. Sample
The design and the sample characteristics of the NESARC have been previously described (Grant et al., 2009; Grant, Stinson, Dawson, Chou, Dufour, et al., 2004; Grant, Stinson, Dawson, Chou, Ruan, et al., 2004; Hasin, Goodwin, Stinson, & Grant, 2005; Sareen et al., 2016). Briefly, the NESARC is a longitudinal survey of the US general population, including residents of Hawaii and Alaska, sponsored by the National Institute on Alcohol Abuse and Alcoholism. The survey aimed to examine prevalence and comorbidities of substance use and mental disorders in the country. The interviews were completed in face-to-face encounters with the participants. The NESARC sample was weighted to adjust for the unequal probabilities of selection and to provide nationally representative estimates.
NESARC baseline (T1) was fielded between 2001 and 2002 and included 43,093 participants 18 years of age and older. Of these, 39,959 were eligible for follow-up (T2) interviews between 2004 and 2005. Ineligible respondents included those who at the time of the T2 interview were deceased, deported, mentally or physically impaired or on active military duty. A total of 34,625 eligible T1 participants were successfully interviewed in the T2 survey. The response rates for T1 and eligible T2 surveys were 81% and 87% respectively (Grant et al., 2009). Survey weights were adjusted to account for loss to follow-up at T2. The study sample was comprised of 10,216 participants who met the criteria for a lifetime DSM-IV SUD at T2 and who were asked questions about SUD treatment. Further sensitivity analyses were conducted in the full sample of 23,245 participants who were asked questions about SUD treatment irrespective of their SUD status.
2.2. Assessments
Health insurance status was assessed by a series of questions about current enrollment at interview. The questions included four types of enrollment: 1) Medicaid (or local name of the Medicaid insurance), 2) Medicare, 3) Civilian Health and Medical Program of the Uniformed Services (CHAMPUS), Civilian Health and Medical Program of the Department of Veterans Affairs (CHAMPVA), the US Department of Veteran Affairs (VA), or other military and, 4) health insurance obtained privately or through a current or former employer or union. Participants who did not endorse any of these insurance types were rated as uninsured.
The use of SUD treatment services between T1 and T2 was ascertained by the following question: “Since your last interview in (month/year), have you gone anywhere or seen anyone for a reason that was related in any way to your (drinking/use of medicines or drugs)—a physician, counselor, Alcoholics Anonymous, or any other community agency or professional?” Those who responded positively were then asked about different types of services, including: Alcoholics Anonymous, Narcotics or Cocaine Anonymous or any other 12-step meeting, family services or another social service, alcohol or drug detoxification ward or clinic, inpatient ward of a psychiatric or general hospital or community mental health program, outpatient clinic, including outreach programs and day or partial patient programs, alcohol or drug rehabilitation program, methadone maintenance program (asked only from people reporting non-alcohol drug use), emergency room, half-way house or therapeutic community, crisis center, Employee Assistance Program (EAP), clergy, priest rabbi, or any type of religious counselor, private physician, psychiatrist, psychologist, social worker, or any other professional and any other agency or professional. Questions about service use were asked only of participants who reported using alcohol or drugs between T1 and T2 and endorsed at least one of the symptoms of SUD in Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV) (American Psychiatric Association, 1994). SUD treatments were categorized into those that are typically covered by health insurance (e.g., outpatient services, hospitalization) and those that are not covered by insurance (e.g., Alcoholic Anonymous, social services).
SUDs were ascertained at both T1 and T2 using AUDADIS-IV. For this study, SUDs included abuse and dependence according to the DSM-IV criteria, involving alcohol, cannabis, crack/cocaine, hallucinogens, sedatives, tranquilizers, stimulants, heroin and other narcotics. The surveys also ascertained whether the respondent had met the criteria in the past year or before the past year.
Sociodemographic variables including sex, age, race-ethnicity (non-Hispanic white, non-Hispanic black, Hispanic and other), personal income, and state of residence were ascertained and included in the multivariable analyses.
2.3. Analysis
Analyses were conducted in three stages. In the first stage, the instrumental variable method of bivariate probit analysis (Bhattacharya, Goldman, & McCaffrey, 2006) was used to examine the association of Medicaid enrollment at T1 with SUD treatments during the time period between T1 and T2. The bivariate probit analysis model can be specified by the following simplified structural model (Waters, 1999):
| (1) |
In which the latent variable of treatment is a linear function of the exogenous variables (X) (e.g., sex, age) and a potentially endogenous variable (y), in this case Medicaid enrollment. Whether or not the individual actually receives treatment (Mi) is determined as follows:
| (2) |
The model for the endogenous variable is specified by the following equation:
| (3) |
In which, is the latent variable of the propensity of the individual to be enrolled in Medicaid and is a linear function of the exogenous variables in the model (X), as well as the identifying instrumental variables (Z), which in this case are state-level variables.
The observed yi is a function of the value of as follows:
| (4) |
The instrumental variables representing state-level enrollment in Medicaid in years 2001–2002 (corresponding to the years of NESARC T1 interview) were extracted from a report by the Kaiser Commission on Medicaid and the Uninsured (Hoffman & Wang, 2003) (Appendix Table A). Two variables based on these data were used: 1) the overall proportion of low-income residents of each state, defined by income <200% of the FPL, covered by Medicaid, and 2) the proportion of low-income residents in each state covered by Medicaid out of those either covered by Medicaid or uninsured. The second variable thus excluded individuals with other types of insurance.
Selection of instruments in instrumental variable analysis is based on the assumptions that the instruments are a) associated with the putative causal variable that is “instrumented” (in this case, individual Medicaid enrollment status), b) are exogenous in the regression model after adjusting for potential confounders (i.e., uncorrelated with the error term of the regression model), and c) associated with the outcomes of interest only through the instrumented variable. While the assumptions a and b can be tested empirically (see below), assumption c cannot be tested (Morgan & Winship, 2007).
Most importantly, the choice of the instrumental variables should be based on theoretical justifications. State variations in Medicaid enrollment are often determined by political and fiscal factors at the state level, few of which are directly related to state prevalence of SUD or need for SUD services because only a very small proportion of Medicaid spending is for SUD services. For example, in 2005 only 1.5 percent of Medicaid spending was for SUD treatment services (Mark, Levit, Vandivort-Warren, Buck, & Coffey, 2011). Nevertheless, Medicaid was the second largest payer for SUD services in this period (Mark et al., 2011). Thus, it is reasonable to assume that Medicaid enrollment would have an impact on SUD service use; whereas, availability or unmet need for SUD services would not be major drivers of state Medicaid policy.
There is also strong evidence that being enrolled in Medicaid is associated with increased use of health services in general (Gunja, Collins, Blumenthal, Doty, & Beutel, 2017), and mental health services, in particular (Deck & Ley, 2006; Frank, Goldman, & Hogan, 2003; Wen et al., 2015). However, the evidence for impact on SUD services is more limited (Wen et al., 2015; Zur & Mojtabai, 2013).
Furthermore, many of the individuals who are enrolled in Medicaid would have otherwise remained uninsured due to low income, unemployment or employment at jobs without health insurance (Bovbjerg, Hadley, Pohl, & Rockmore, 2002; Haber, Khatutsky, & Mitchell, 2000). The major target of the Medicaid expansion programs under 1115 waivers is to expand coverage to these low-income uninsured adults.
Therefore, we opted to use two instrumental variables: the percentage of low income adults enrolled in Medicaid among all low-income adults and the percentage among those who, without Medicaid would likely have remained uninsured. Thus, the latter variable captures the group of low-income adults targeted by Medicaid expansion programs more specifically.
The association of these state-level variables with the individual level variable of Medicaid enrollment is intuitive. Individuals who live in a state with a larger percentage of adults enrolled in Medicaid (a proxy for the states’ generosity in offering Medicaid insurance) would naturally be more likely to be enrolled in Medicaid. Indeed, this association was substantiated empirically as well (see below).
Using two instrumental variables also allowed us to conduct over-identification tests to assess whether the instrumental variables are associated with the error terms of the regression models. Following common practice (French & Popovici, 2009; Guilkey & Lance, 2014), the overidentification test was conducted by repeating the bivariate probit analysis with one of the two state-level variables as an instrumental variable and entering the other state-level variable as an independent variable in the models. Variables representing respondent sex, age, race/ethnicity, income, and SUD in the past year (at T1), other types of insurance enrollment (with the uninsured as the reference category) and dummy-coded variables for individual states were also included in the models. A significant association between the tested variable and the outcome in these models would indicate that the tested variable is not exogenous and not suitable as an instrumental variable.
The strength of the association of the state-level instrumental variables with individual Medicaid enrollment was assessed using adjusted F-tests. Values smaller than 10 suggest weak instruments (Staiger & Stock, 1997).
While instrumental variable models provide advantages over naïve regression models, they typically lead to a loss of efficiency by producing large standard errors. The need for using instrumental variable models can be assessed by examining the rho coefficients from these models which represent the correlations between the error terms of the two parts of the model (Є1 and Є2 in [1] and [2] above) and the endogeneity of individual-level Medicaid enrollment in these models. A large and statistically significant rho value indicates endogeneity and justifies the use of instrumental variable models. If rho is small and not statistically significant, it suggests that the putative casual variable (individual Medicaid enrollment status) is not endogenous in the model, and that the use of an instrumental variable model–which results in a loss of efficiency as compared to a naïve model–is unnecessary. The technical details of the of the bivariate probit model and its advantages over other instrumental variable models have been presented elsewhere (Bhattacharya et al., 2006).
In the second stage of the analyses, a naïve probit model in which individual Medicaid status at T1 was assumed to be exogenous (based on rho values) was used. The naïve probit model adjusted for the same set of variables used in the bivariate probit. While the samples for the bivariate and naïve probit analyses reported here were limited to adults with lifetime SUD, these analyses were repeated in the full sample of adults who responded to questions about the use of SUD services.
In the third stage of the analyses, the associations of T1 Medicaid enrollment with different types of SUD treatments were assessed using multivariable logistic regression models that adjusted for the same individual-level variables as in the probit models described above. The association of Medicaid enrollment with each individual service and with each of two general types of SUD treatment (i.e., typically covered by insurance and not covered) were assessed.
All analyses were conducted using the STATA 14 software (StataCorp, 2015) and adjusted for survey weights, clustering, and stratification of data. Bivariate probit analyses were conducted using the biprobit routine of Stata. All percentages reported are weighted. A p<.05 was used to determine statistical significance of tests.
3. RESULTS
3.1. Characteristics of the participants with SUD
The majority of NESARC participants in the study sample were male, younger than 40 years of age, non-Hispanic white, and had a personal income of less than $35,000 per year (Table 1). A total of 42.2% met the full criteria for an SUD in the past year and 4.4% were covered by Medicaid.
Table 1.
Characteristics of participants in the total sample and sub-samples for the examining the association of Medicaid enrollment at T1 and use of services between T1 and T2 in the National Epidemiologic Survey on Alcohol and Related Conditions.
| Total sample (N= 34,653) |
Sub-sample for assessment of substance use disorder treatments (N= 10,216) |
|||
|---|---|---|---|---|
| Variable | N | Percent | N | Percent |
| Sex | ||||
| Female | 20,089 | 52.1 | 4,144 | 35.7 |
| Male | 14,564 | 47.9 | 6,072 | 64.3 |
| Age, years | ||||
| 18–29 | 6,719 | 21.8 | 2,600 | 28.5 |
| 30–39 | 7,299 | 20.1 | 2,659 | 24.8 |
| 40–54 | 10,226 | 29.6 | 3,356 | 31.9 |
| 55+ | 10,409 | 28.5 | 1,601 | 14.9 |
| Race/ethnicity | ||||
| Non-Hispanic white | 20,174 | 70.9 | 7,007 | 78.5 |
| Non-Hispanic black | 6,577 | 11.0 | 1,337 | 7.8 |
| Hispanic | 6,356 | 11.6 | 1,504 | 9.0 |
| Other | 1,546 | 6.5 | 368 | 4.7 |
| Personal income in $1,000 | ||||
| <20 | 16,385 | 46.2 | 3,787 | 37.4 |
| 20 - <35 | 8,093 | 22.8 | 2,522 | 23.7 |
| 35 - <60 | 6,519 | 19.1 | 2,393 | 23.0 |
| 60+ | 3,656 | 11.8 | 1,514 | 15.9 |
| SUD in past year (at T1) | 4,813 | 14.7 | 4,313 | 42.2 |
| Health Insurance at T1 | ||||
| Medicaid | 2,610 | 5.7 | 586 | 4.4 |
| Medicare | 6,889 | 18.2 | 929 | 8.3 |
| Private insurance | 23,125 | 69.7 | 7,316 | 73.2 |
| Other insurance | 1,183 | 3.5 | 391 | 4.0 |
| No insurance | 6,248 | 18.0 | 1,912 | 18.7 |
Abbreviations: T1 represents baseline interview and T2, the follow-up interview. SUD stands for substance use disorder.
3.2. Association of Medicaid enrollment with the use of SUD treatments
Table 2 present the results of bivariate and naïve probit models for the association of Medicaid enrollment at T1 with receipt of SUD treatments between T1 and T2 (Appendix Table B presents full table with dummy-coded state variables). The instrumental variables were significantly associated with individual Medicaid enrollment status, with F-test values exceeding 10 (F [2, 64]=12.29, p<.001 for the joint test of these variables in the model). The F-test values for each individual instrument in the just-identified models were similarly high. Neither of the overidentification tests were significant, supporting the validity of the instrumental variables (Appendix Table B). However, the rho coefficient in the model was relatively small and not different from 0 at a statistically significant level, suggesting that the individual-level Medicaid status is not endogenous in the model and instrumental variable modeling is not necessary to obtain unbiased estimates of the association of Medicaid enrollment with SUD treatment. The reduced form regression coefficient for the instrumented individual-level Medicaid variable was not statistically significant due to the inefficiency of the model.
Table 2.
Association of Medicaid enrollment at T1 with substance use disorder treatment between T1 and T2 in participants of National Epidemiologic Survey on Alcohol and Related Conditions.a
| Bivariate probit model | Naïve probit model | |||||
|---|---|---|---|---|---|---|
| B | SE | p | B | SE | p | |
| Health insurance (Ref: uninsured) | ||||||
| Medicaid | .200 | .638 | .755 | .246 | .121 | .046 |
| Medicare | .044 | .106 | .680 | .044 | .106 | .680 |
| Private insurance | −.201 | .061 | .002 | −.201 | .061 | .002 |
| Other insurance | .163 | .133 | .227 | .163 | .133 | .228 |
| Female sex | −.180 | .052 | .001 | −.180 | .052 | .001 |
| Age, years (Ref:18–29) | ||||||
| 30–39 | −.023 | .075 | .761 | −.023 | .075 | .761 |
| 40–54 | .020 | .069 | .776 | .020 | .069 | .776 |
| 55+ | −.555 | .108 | <.001 | −.555 | .108 | <.001 |
| Race/ethnicity (Ref.: Non-Hispanic white) | ||||||
| Non-Hispanic black | −.050 | .089 | .575 | −.050 | .089 | .575 |
| Hispanic | −.038 | .085 | .654 | −.038 | .085 | .654 |
| Other | −.126 | .157 | .423 | −.126 | .157 | .423 |
| Personal income in $1,000 (Ref: <20) | ||||||
| 20-<35 | −.113 | .071 | .120 | −.113 | .071 | .120 |
| 35-<60 | −.290 | .087 | .001 | −.290 | .087 | .001 |
| 60+ | −.361 | .101 | .001 | −.361 | .101 | .001 |
| SUD in past year (at T1) | .256 | .052 | <.001 | .256 | .052 | <.001 |
| Constant | −1.266 | −1.268 | ||||
| Model predicting individual Medicaid enrollment | ||||||
| Instrumental variables | ||||||
| % of low-income covered by Medicaid | .027 | .010 | .009 | |||
| % of low-income covered by Medicaid among those with Medicaid or uninsured | .004 | .007 | .586 | |||
| Constant | −2.672 | |||||
| rho | .021 | .282 | .941 | |||
Abbreviations: T1 represents baseline interview and T2, the follow-up interview. B stands for the regression coefficient, SE, for standard error, and SSI for supplemental security income.
The models also adjusted for the state fixed effects. The full analyses results are presented in Appendix Table B.
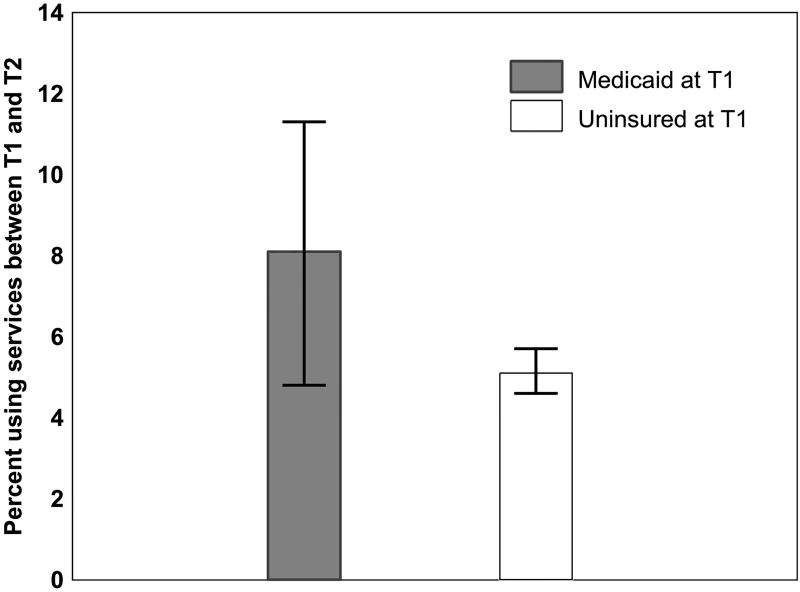
Therefore, a naïve probit analysis was conducted. As a further test of unbiasedness of the naïve model results the predicted values from the bivariate probit model as well as the naïve probit model were computed. Comparison of these predicted probabilities revealed remarkable consistency. The predicted probabilities for receipt of SUD treatment were 8.1% for those with Medicaid vs. with 5.1% in the uninsured (risk difference=2.9%) in both the bivariate and naïve probit models. This finding further supports the use of the more efficient naïve probit model.
The probabilities of service use among participants with and without Medicaid enrollment at T1 are presented in Figure 1. In addition to Medicaid insurance, past-year SUD was associated with greater likelihood of SUD treatment; whereas, private insurance, female sex, age 55 and older, and annual personal income of $35,000 or more were associated with lower likelihood of receiving such treatment. The associations of private insurance and income with SUD treatment may reflect the social consequences of more severe SUD which in turn is associated with greater likelihood of using services. The results of bivariate and naïve probit analyses for the full sample of participants who were asked about SUD service were very similar to the analyses for participants with lifetime SUD (Appendix Table C).
Figure 1.
Adjusted probabilities of substance use disorder treatments between T1 and T2 according to Medicaid enrollment status at T1 based on the naïve probit model presented in Table 2; the National Epidemiologic Survey on Alcohol and Related Conditions.
3.3. Types of services
The adjusted comparisons of the use of various types of services are presented in Table 3. Compared to the uninsured, participants with Medicaid had higher odds of receiving SUD treatments that are potentially covered by health insurance, such as detoxification and rehabilitation services. However, Medicaid-covered participants were not more likely than the uninsured to receive treatments not covered by insurance, such as 12-step, with the exception of family and social services, which was more commonly used by individuals with Medicaid.
Table 3.
Association of Medicaid status at T1 with different types of substance use disorder treatments between the two waves in participants of the National Epidemiologic Survey on Alcohol and Related Conditions with lifetime SUD.
| Type of substance use treatment | Medicaid at T1 | Un-insured at T1 |
Comparison | ||||
|---|---|---|---|---|---|---|---|
| N | % | N | % | AOR | 95 %CI | p | |
| Any substance use treatment | 64 | 11.9 | 154 | 7.6 | 1.66 | 1.04,2.66 | .034 |
| Treatments potentially covered by health insurance | 60 | 11.3 | 118 | 6.0 | 2.05 | 1.28,3.31 | .004 |
| Outpatient clinic, including outreach programs and day or partial hospital | 24 | 4.0 | 37 | 1.4 | 2.24 | 1.05,4.79 | .038 |
| Inpatient ward of a psychiatric or general hospital | 20 | 4.3 | 21 | 0.8 | 3.59 | 1.49,8.66 | .005 |
| Detoxification ward or clinic | 26 | 4.9 | 41 | 2.1 | 2.36 | 1.15,4.84 | .020 |
| Rehabilitation program | 29 | 5.4 | 58 | 3.0 | 2.16 | 1.15,4.09 | .018 |
| Private office of physician, psychiatrist, psychologist, or social worker | 45 | 8.6 | 69 | 3.5 | 2.33 | 1.40,3.86 | .001 |
| Methadone Maintenance Program | 5 | 0.6 | 5 | 0.4 | 1.45 | 0.36,5.83 | .593 |
| Emergency room | 17 | 3.6 | 24 | 1.1 | 2.74 | 1.04,7.26 | .042 |
| Treatments not covered by insurance | 49 | 8.9 | 123 | 6.2 | 1.62 | 0.96,2.73 | .070 |
| Self-help groups (e.g., AA, NA) | 39 | 7.1 | 102 | 5.3 | 1.47 | 0.89,2.43 | .135 |
| Family services or other social services | 27 | 4.7 | 37 | 2.0 | 2.85 | 1.34,6.07 | .007 |
| Halfway house or therapeutic community | 7 | 1.1 | 14 | 0.6 | 1.55 | 0.47,5.17 | .468 |
| Crisis Center | 7 | 1.2 | 6 | 0.4 | 2.18 | 0.62–7.68 | .220 |
| Employee Assistance Program (EAP) | 2 | 0.2 | 5 | 0.3 | 1.08 | 0.19–6.07 | .933 |
| Help from clergyman, priest, rabbi, or any type of religious counselor | 13 | 2.0 | 25 | 1.2 | 1.36 | 0.58–3.22 | .477 |
Regression model adjusted for sex, age, race/ethnicity, income, employment status, receipt of SSI, substance use disorder and mood or anxiety disorders in the past year (at T1) as well as other types of insurance enrollment.
4. DISCUSSION
Medicaid remains the largest source of public funding for SUD services in the US (Mark et al., 2016). However, there have been significant variations in the eligibility criteria and enrollment in Medicaid across the states. As these variations are likely to continue or even increase in near future (Berliner, 2013), it is important to understand how policies that expand access to Medicaid affect SUD service use. Our findings indicate that Medicaid enrollment is significantly associated with the use of SUD treatment services, thus state policies that impact Medicaid enrollment would have an impact on SUD service use.
This finding has implications for future developments in Medicaid enrollment across states. As a large proportion of new enrollees under the ACA will have SUDs (Busch, Meara, Huskamp, & Barry, 2013; Tsai, Pilver, & Hoff, 2014), variations in Medicaid enrollment across states will likely contribute to growing disparities in service use in these individuals. Our findings also suggest that disparities in the treatment of SUD will be mainly for formal treatment services that are typically covered by health insurance such as outpatient, residential, and medication- assisted treatments. These are the services that have the strongest evidence base and should therefore be made more accessible to persons in need of treatment (Glasner-Edwards & Rawson, 2010).
A further finding of the study was the negative association of private health insurance with SUD treatment use. This finding is consistent with past research (Ali, Teich, & Mutter, 2015; Becker et al., 2008) and may be attributable to less severe impairment in privately insured individuals with SUD who typically obtained their health insurance through employment, or to the different set of barriers to SUD treatment that these individuals face (Ali, Teich, & Mutter, 2017).
The results of this longitudinal study are consistent with previous studies that found associations between individual state Medicaid extension initiatives and SUD service use (Callahan et al., 1995; Deck & McFarland, 2002; Deck et al., 2000; Deck et al., 2006; Saunders & Heflinger, 2003). The present study provides nationally representative data based on a longitudinal survey. Furthermore, the endogeneity of Medicaid enrollment in the prediction models could be assessed using instrumental variable techniques. The association of Medicaid insurance with SUD service utilization appeared to be stronger for the types of services that are typically covered by health insurance, further supporting the association of Medicaid insurance with SUD service use.
Despite these strengths, several limitations of the study should be considered. First, NESARC data collection spans the period of 2001–2005. The expansion of Medicaid programs in several states continued in the ensuing years and was further reinforced by the ACA in states that chose to expand Medicaid. The profiles of substance use have also changed over time (Center for Behavioral Health Statistics and Quality, 2016). For instance, the prevalence of opioid and cannabis use has increased over time. Thus, the provided estimates of the effect of Medicaid may not necessarily apply to more recent years. Nevertheless, the prevalence of treatment seeking for SUD in the population, the contribution of Medicaid to SUD treatment, and the mix of inpatient, outpatient and residential services for treatment of SUD did not appreciably change between 2004 and 2014 (Han et al., 2015; Mark et al., 2016). Furthermore, there is no evidence that SUD services covered under Medicaid have declined since early 2000s. Thus, the effects of Medicaid enrollment in the years following the implementation of ACA are not likely to be smaller than estimated in this study. Second, the findings of the study are at variance with some studies that examined the early effect of ACA expansion of health insurance. However, the results of these studies are mixed (McKenna, 2017; Saloner, Akosa Antwi, Maclean, & Cook, 2018; Saloner, Bandara, Bachhuber, & Barry, 2017; Wen, Hockenberry, Borders, & Druss, 2017). Furthermore, most studies cover only the first 1 or 2 years of the full implementation of ACA. It may take a longer time for any changes in service use to become detectable. Many of the state expansion programs that were captured in the current study were implemented in the 1999’s, thus allowing the clients and the services to adapt to changes in insurance availability (Aletraris, Edmond, & Roman, 2017). Third, many substance use treatment programs do not accept Medicaid due to regulatory policies, such as state requirements for physician involvement in service delivery (Andrews, 2014). Furthermore, in the years covered by this study, states varied considerably in the types of services offered and accessibility of those services, resulting in significant differences in patterns of SUD service use across states (Clark, Samnaliev, & McGovern, 2007). These policies could not be assessed in this analysis. Nevertheless, the use of state fixed effects adjusted for some of this unmeasured variability. Fourth, a significant proportion of substance use treatments are court-mandated. NESARC did not assess whether treatment was court-mandated or self-initiated. Court-mandated treatment may not be as responsive to availability of insurance as self-initiated treatment. Fifth, a number of states passed and implemented parity legislations over the past two decades. However, before ACA, these legislations mainly impacted privately insured individuals. ACA mandated that all state Medicaid agencies—including those that have opted out of expansion—were required to comply with parity requirements in benchmark and managed care plans. The extent of compliance with this requirement and its impact on SUD services need to be assessed in future research. Future research should also evaluate whether substance treatments received under Medicaid are effective in addressing the needs of clients with SUD.
5. CONCLUSIONS
In the context of the above limitations, the results provide useful longitudinal information on the impact of state Medicaid expansion initiatives on SUD treatment service use at a national level. Individuals with SUD have traditionally faced formidable barriers to care, including financial barriers and lack of insurance (Chen et al., 2013; Kaufmann, Chen, Crum, & Mojtabai, 2014; Mojtabai, 2005; Mojtabai et al., 2011). These data, in conjunction with data on the early impact of ACA (Saloner, Akosa Antwi, Maclean, & Cook, 2017) highlight the potential beneficial effects of Medicaid expansion on reducing these financial barriers and making services more readily accessible to this vulnerable population.
Highlights.
States have traditionally varied in Medicaid eligibility and enrollment.
Medicaid enrollment is associated with increased odds of future use of substance use services.
The association is more pronounced for services that are typically covered by insurance.
Acknowledgments
Funding
Ramin Mojtabai, Mark Olfson and Rosa Crum’s work on this project was supported by the National Institutes on Drug Abuse grant number R01 DA039863. Ms. Krawczyk and Tormohlen’s work was supported by grant number T32DA007292 (PI: Renee M. Johnson)
Appendix
Table A.
Medicaid enrollment and the percent uninsured among the non-elderly US adults with family income<200% of Federal Poverty Level, 2001–2002.
| State | Medicaid | Uninsured |
|---|---|---|
| Alabama | 19.1% | 35.3% |
| Alaska | 21.5% | 44.8% |
| Arizona | 17.6% | 41.6% |
| Arkansas | 13.8% | 38.6% |
| California | 18.8% | 44.1% |
| Colorado | 9.5% | 43.9% |
| Connecticut | 19.2% | 32.7% |
| Delaware | 21.9% | 27.7% |
| District of Columbia | 30.2% | 33.4% |
| Florida | 14.7% | 43.2% |
| Georgia | 12.0% | 39.4% |
| Hawaii | 17.8% | 23.9% |
| Idaho | 16.0% | 41.1% |
| Illinois | 16.9% | 37.6% |
| Indiana | 11.5% | 35.2% |
| Iowa | 16.5% | 29.8% |
| Kansas | 12.2% | 36.6% |
| Kentucky | 15.8% | 33.4% |
| Louisiana | 15.7% | 44.4% |
| Maine | 29.5% | 29.7% |
| Maryland | 12.2% | 43.6% |
| Massachusetts | 34.2% | 25.5% |
| Michigan | 19.9% | 31.6% |
| Minnesota | 21.5% | 28.8% |
| Mississippi | 24.4% | 37.9% |
| Missouri | 18.9% | 33.8% |
| Montana | 16.6% | 33.0% |
| Nebraska | 15.0% | 29.1% |
| Nevada | 6.2% | 44.7% |
| New Hampshire | 12.3% | 34.2% |
| New Jersey | 19.8% | 40.5% |
| New Mexico | 16.4% | 46.8% |
| New York | 25.2% | 39.3% |
| North Carolina | 16.1% | 39.7% |
| North Dakota | 16.6% | 27.9% |
| Ohio | 18.5% | 34.8% |
| Oklahoma | 13.6% | 43.9% |
| Oregon | 24.5% | 33.7% |
| Pennsylvania | 21.9% | 29.2% |
| Rhode Island | 30.2% | 28.4% |
| South Carolina | 22.8% | 34.4% |
| South Dakota | 13.7% | 30.4% |
| Tennessee | 32.3% | 25.6% |
| Texas | 10.0% | 53.3% |
| Utah | 11.6% | 35.3% |
| Vermont | 31.3% | 25.5% |
| Virginia | 12.8% | 35.3% |
| Washington | 20.6% | 33.3% |
| West Virginia | 23.3% | 33.2% |
| Wisconsin | 20.8% | 27.6% |
| Wyoming | 12.5% | 42.7% |
Source of data: Hoffman, C., & Wang, M. (2003). Health insurance coverage in America: 2002 data update. Retrieved from https://kaiserfamilyfoundation.files.wordpress.com/2013/01/health-insurance-coverage-in-america-2002-data-update.pdf
Table B.
Association of Medicaid enrollment at T1 with substance use disorder treatment between T1 and T2 in participants of National Epidemiologic Survey on Alcohol and Related Conditions with a lifetime SUD who were asked about the use of SUD services at T2.
| Bivariate probit model | Naïve probit model | |||||
|---|---|---|---|---|---|---|
| B | SE | p | B | SE | p | |
| Medicaid | .200 | .638 | .755 | .246 | .121 | .046 |
| Medicare | .044 | .106 | .680 | .044 | .106 | .680 |
| Private insurance | −.201 | .061 | .002 | −.201 | .061 | .002 |
| CHAMPUS/VA | .163 | .133 | .227 | .163 | .133 | .228 |
| Male sex | Ref. | . | . | Ref. | . | . |
| Female sex | −.180 | .052 | .001 | −.180 | .052 | .001 |
| Age 18–29 yrs | Ref. | . | . | Ref. | . | . |
| Age 30–39 yrs | −.023 | .075 | .761 | −.023 | .075 | .761 |
| Age 40–54 yrs | .020 | .069 | .776 | .020 | .069 | .776 |
| Age 55+ | −.555 | .108 | <.001 | −.555 | .108 | <.001 |
| Non-Hispanic white | Ref. | . | . | Ref. | . | . |
| Non-Hispanic black | −.050 | .089 | .575 | −.050 | .089 | .575 |
| Hispanic | −.038 | .085 | .654 | −.038 | .085 | .654 |
| Other | −.126 | .157 | .423 | −.126 | .157 | .423 |
| Personal income <$20K | Ref. | . | . | Ref. | . | . |
| Personal income $20K - <$35K | −.113 | .071 | .120 | −.113 | .071 | .120 |
| Personal income $35K - <$60K | −.290 | .087 | .001 | −.290 | .087 | .001 |
| Personal income $60K+ | −.361 | .101 | .001 | −.361 | .101 | .001 |
| Any 12-month SUD | .256 | .052 | <.001 | .256 | .052 | <.001 |
| States | ||||||
| Alabama | Ref. | . | . | Ref. | . | . |
| Alaska | −.676 | .390 | .088 | −.677 | .390 | .088 |
| Arizona | −.031 | .256 | .904 | −.031 | .256 | .905 |
| Arkansas | −.159 | .464 | .733 | −.159 | .464 | .733 |
| California | −.033 | .265 | .901 | −.033 | .265 | .901 |
| Colorado | −.030 | .278 | .913 | −.029 | .276 | .918 |
| Connecticut | −.042 | .283 | .881 | −.042 | .283 | .882 |
| Delaware | .699 | .307 | .026 | .699 | .307 | .026 |
| District of Columbia | −.217 | .257 | .402 | −.219 | .255 | .392 |
| Florida | −.185 | .266 | .488 | −.185 | .266 | .489 |
| Georgia | −.503 | .308 | .107 | −.502 | .308 | .107 |
| Hawaii | .116 | .266 | .665 | .116 | .266 | .664 |
| Idaho | −.346 | .330 | .299 | −.345 | .330 | .299 |
| Illinois | .079 | .269 | .770 | .080 | .269 | .768 |
| Indiana | .237 | .285 | .408 | .238 | .285 | .406 |
| Iowa | .122 | .299 | .685 | .122 | .299 | .685 |
| Kansas | −.492 | .263 | .066 | −.492 | .263 | .066 |
| Kentucky | .188 | .314 | .552 | .188 | .314 | .552 |
| Louisiana | −.535 | .321 | .101 | −.536 | .321 | .101 |
| Maine | −.754 | .434 | .087 | −.756 | .433 | .086 |
| Maryland | .004 | .291 | .989 | .005 | .291 | .986 |
| Massachusetts | −.149 | .293 | .612 | −.152 | .289 | .601 |
| Michigan | −.113 | .265 | .671 | −.113 | .265 | .671 |
| Minnesota | .048 | .262 | .855 | .048 | .262 | .855 |
| Mississippi | −.137 | .335 | .684 | −.139 | .334 | .679 |
| Missouri | −.135 | .278 | .628 | −.136 | .277 | .626 |
| Montana | −.847 | .548 | .127 | −.846 | .548 | .127 |
| Nebraska | −.155 | .298 | .605 | −.155 | .298 | .604 |
| Nevada | .032 | .385 | .934 | .034 | .385 | .930 |
| New Hampshire | −.395 | .304 | .198 | −.395 | .304 | .199 |
| New Jersey | −.268 | .288 | .355 | −.268 | .288 | .355 |
| New Mexico | .093 | .286 | .745 | .093 | .286 | .746 |
| New York | −.073 | .269 | .786 | −.074 | .268 | .782 |
| North Carolina | .102 | .324 | .754 | .102 | .324 | .754 |
| North Dakota | .098 | .377 | .796 | .098 | .377 | .795 |
| Ohio | −.165 | .318 | .607 | −.165 | .318 | .607 |
| Oklahoma | −.390 | .278 | .165 | −.389 | .278 | .166 |
| Oregon | .144 | .290 | .622 | .143 | .290 | .623 |
| Pennsylvania | −.225 | .276 | .419 | −.225 | .276 | .418 |
| Rhode Island | .137 | .257 | .595 | .135 | .254 | .597 |
| South Carolina | −.165 | .338 | .627 | −.166 | .338 | .625 |
| South Dakota | --a | --a | --a | --a | --a | --a |
| Tennessee | −.149 | .395 | .708 | −.152 | .380 | .691 |
| Texas | −.503 | .268 | .065 | −.502 | .268 | .066 |
| Utah | .093 | .284 | .744 | .094 | .284 | .741 |
| Vermont | .160 | .295 | .589 | .156 | .288 | .590 |
| Virginia | −.072 | .287 | .803 | −.071 | .287 | .805 |
| Washington | −.101 | .269 | .708 | −.101 | .269 | .707 |
| West Virginia | −.499 | .461 | .283 | −.500 | .460 | .282 |
| Wisconsin | −.166 | .306 | .588 | −.167 | .306 | .588 |
| Wyoming | --a | --a | --a | --a | --a | --a |
| Constant | −1.266 | .271 | <.001 | −1.268 | .269 | <.001 |
| Model predicting individual Medicaid enrollment | ||||||
| Instrumental variables | ||||||
| % of low-income covered by Medicaid | .027 | .010 | .009 | |||
| % of low-income covered by Medicaid among those with Medicaid or uninsured | .004 | .007 | .586 | |||
| Constant | −2.672 | |||||
| rho | .021 | .282 | .941 | |||
Validity Tests
Joint adjusted Wald test for the association of instrumental variables with the individual Medicaid enrollment status: F(2, 64)=12.29, p<.001
Overidentification tests:
Adjusted Wald test for the variable % of low-income covered by Medicaid: F(1, 65)=.01, p=.939
Adjusted Wald test for the variable % of low-income covered by Medicaid among those with Medicaid or uninsured: F(1, 65)=.96, p=.331
Abbreviations: T1 represents baseline interview and T2, the follow-up interview. B stands for the regression coefficient, SE, for standard error, and SSI for supplemental security income.
None of the participants from this state used SUD services between T1 and T2.
Table C.
Association of Medicaid enrollment at T1 with substance use disorder treatment between T1 and T2 in participants of National Epidemiologic Survey on Alcohol and Related Conditions who were asked about the use of SUD services at T2.
| Bivariate probit model | Naïve probit model | |||||
|---|---|---|---|---|---|---|
| B | SE | p | B | SE | p | |
| Medicaid | .308 | .769 | .690 | .237 | .103 | .024 |
| Medicare | .055 | .090 | .541 | .055 | .090 | .542 |
| Private insurance | −.185 | .057 | .002 | −.185 | .057 | .002 |
| CHAMPUS/VA | .157 | .122 | .204 | .157 | .122 | .204 |
| Male sex | Ref. | . | . | Ref. | . | . |
| Female sex | −.259 | .047 | <.001 | −.259 | .047 | <.001 |
| Age 18–29 yrs | Ref. | . | . | Ref. | . | . |
| Age 30–39 yrs | .011 | .066 | .866 | .011 | .066 | .867 |
| Age 40–54 yrs | .014 | .061 | .823 | .014 | .061 | .823 |
| Age 55+ | −.494 | .096 | <.001 | −.494 | .096 | <.001 |
| Non-Hispanic white | Ref. | . | . | Ref. | . | . |
| Non-Hispanic black | −.076 | .072 | .294 | −.076 | .072 | .294 |
| Hispanic | −.142 | .076 | .067 | −.142 | .076 | .067 |
| Other | −.187 | .129 | .152 | −.187 | .129 | .152 |
| Personal income <$20K | Ref. | . | . | Ref. | . | . |
| Personal income $20K - <$35K | −.123 | .064 | .058 | −.123 | .064 | .059 |
| Personal income $35K - <$60K | −.245 | .075 | .002 | −.245 | .075 | .002 |
| Personal income $60K+ | −.276 | .087 | .002 | −.276 | .087 | .002 |
| SUD in past year (at T1) | .660 | .047 | <.001 | .660 | .048 | <.001 |
| State | ||||||
| Alabama | Ref. | . | . | Ref. | . | . |
| Alaska | −.523 | .395 | .190 | −.522 | .395 | .191 |
| Arizona | .012 | .167 | .941 | .012 | .167 | .942 |
| Arkansas | −.130 | .435 | .766 | −.130 | .435 | .766 |
| California | −.050 | .177 | .779 | −.050 | .177 | .779 |
| Colorado | .001 | .192 | .997 | −.002 | .190 | .993 |
| Connecticut | −.094 | .205 | .646 | −.095 | .205 | .645 |
| Delaware | .382 | .207 | .070 | .383 | .207 | .069 |
| District of Columbia | −.135 | .165 | .415 | −.132 | .160 | .414 |
| Florida | −.150 | .184 | .419 | −.151 | .184 | .416 |
| Georgia | −.499 | .231 | .034 | −.499 | .231 | .034 |
| Hawaii | .114 | .176 | .518 | .114 | .176 | .519 |
| Idaho | −.267 | .255 | .298 | −.268 | .255 | .298 |
| Illinois | .058 | .177 | .744 | .057 | .177 | .746 |
| Indiana | .199 | .211 | .348 | .198 | .211 | .353 |
| Iowa | .161 | .194 | .409 | .161 | .194 | .410 |
| Kansas | −.462 | .180 | .012 | −.463 | .180 | .012 |
| Kentucky | .180 | .220 | .416 | .180 | .220 | .416 |
| Louisiana | −.383 | .255 | .138 | −.382 | .255 | .138 |
| Maine | −.776 | .369 | .039 | −.774 | .368 | .040 |
| Maryland | .037 | .193 | .848 | .036 | .193 | .853 |
| Massachusetts | −.185 | .215 | .392 | −.182 | .207 | .384 |
| Michigan | −.063 | .179 | .726 | −.062 | .179 | .728 |
| Minnesota | .064 | .170 | .710 | .064 | .170 | .710 |
| Mississippi | −.151 | .245 | .540 | −.149 | .243 | .543 |
| Missouri | −.104 | .186 | .576 | −.104 | .185 | .579 |
| Montana | −.759 | .498 | .132 | −.760 | .499 | .132 |
| Nebraska | −.104 | .215 | .628 | −.104 | .214 | .629 |
| Nevada | .196 | .250 | .434 | .194 | .250 | .441 |
| New Hampshire | −.365 | .233 | .123 | −.365 | .233 | .122 |
| New Jersey | −.307 | .200 | .129 | −.308 | .200 | .128 |
| New Mexico | .135 | .207 | .517 | .136 | .207 | .514 |
| New York | −.087 | .183 | .637 | −.085 | .182 | .641 |
| North Carolina | .074 | .249 | .768 | .073 | .249 | .769 |
| North Dakota | .037 | .340 | .914 | .036 | .340 | .915 |
| Ohio | −.139 | .243 | .571 | −.138 | .243 | .571 |
| Oklahoma | −.351 | .193 | .074 | −.351 | .193 | .074 |
| Oregon | .177 | .213 | .409 | .178 | .213 | .407 |
| Pennsylvania | −.183 | .193 | .345 | −.183 | .193 | .346 |
| Rhode Island | .079 | .168 | .642 | .082 | .162 | .613 |
| South Carolina | −.198 | .258 | .445 | −.197 | .257 | .447 |
| South Dakota | --a | --a | --a | --a | --a | --a |
| Tennessee | −.113 | .332 | .735 | −.109 | .316 | .732 |
| Texas | −.372 | .179 | .041 | −.373 | .180 | .042 |
| Utah | .172 | .204 | .401 | .172 | .204 | .404 |
| Vermont | .165 | .195 | .399 | .171 | .187 | .366 |
| Virginia | −.101 | .199 | .614 | −.102 | .199 | .609 |
| Washington | .059 | .176 | .737 | .060 | .176 | .735 |
| West Virginia | −.388 | .413 | .350 | −.387 | .412 | .352 |
| Wisconsin | −.100 | .211 | .637 | −.099 | .210 | .638 |
| Wyoming | --a | --a | --a | --a | --a | --a |
| Constant | −1.693 | −1.691 | ||||
| Model predicting individual Medicaid enrollment | ||||||
| Instrumental variables | ||||||
| % of low-income covered by Medicaid | .023 | .009 | .011 | |||
| % of low-income covered by Medicaid among those with Medicaid or uninsured | .005 | .006 | .423 | |||
| Constant | −2.620 | |||||
| rho | −.032 | .340 | .925 | |||
Validity Tests
Joint adjusted Wald test for the association of instrumental variables with the individual Medicaid enrollment status: F (2, 64)=20.45, p<.001
Overidentification tests:
Adjusted Wald test for the variable % of low-income covered by Medicaid: F (1, 65)=.20, p=.660
Adjusted Wald test for the variable % of low-income covered by Medicaid among those with Medicaid or uninsured: F (1, 65)=.67, p=.415
Abbreviations: T1 represents baseline interview and T2, the follow-up interview. B stands for the regression coefficient, SE, for standard error, and SSI for supplemental security income.
None of the participants from this state used SUD services between T1 and T2.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest:
The authors have no conflict of interest.
Contributor Information
Ramin Mojtabai, Department of Mental Health, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD..
Kenneth A. Feder, Department of Mental Health, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD..
Marc Kealhofer, Lieber Institute for Brain Development, Baltimore, MD..
Noa Krawczyk, Department of Mental Health, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD..
Carla Storr, Department of Nursing, University of Maryland, Baltimore, MD..
Kayla N. Tormohlen, Department of Mental Health, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD..
Andrea S. Young, Department of Psychiatry and Substance Sciences, Johns Hopkins University, Baltimore, MD..
Mark Olfson, Department of Psychiatry and Substance Science, Columbia University, New York, NY..
Rosa M. Crum, Department of Epidemiology, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD..
References
- Aletraris L, Edmond MB, Roman PM. Insurance Receipt and Readiness for Opportunities under the Affordable Care Act: A National Survey of Treatment Providers for Substance Use Disorders. J Psychoactive Drugs. 2017;49(2):141–150. doi: 10.1080/02791072.2017.1306661. [DOI] [PubMed] [Google Scholar]
- Ali MM, Teich JL, Mutter R. The role of perceived need and health insurance in substance use treatment: implications for the Affordable Care Act. J Subst Abuse Treat. 2015;54:14–20. doi: 10.1016/j.jsat.2015.02.002. [DOI] [PubMed] [Google Scholar]
- Ali MM, Teich JL, Mutter R. Reasons for Not Seeking Substance Use Disorder Treatment: Variations by Health Insurance Coverage. J Behav Health Serv Res. 2017;44(1):63–74. doi: 10.1007/s11414-016-9538-3. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders : DSM-IV. 4. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- Andrews CM. The relationship of state Medicaid coverage to Medicaid acceptance among substance abuse providers in the United States. J Behav Health Serv Res. 2014;41(4):460–472. doi: 10.1007/s11414-013-9387-2. [DOI] [PubMed] [Google Scholar]
- Baumrucker EP. Medicaid and SCHIP Section 1115 Research and Demonstration Waivers. CRS Report for Congress. 2004 Retrieved from http://research.policyarchive.org/3528.pdf.
- Becker WC, Fiellin DA, Merrill JO, Schulman B, Finkelstein R, Olsen Y, Busch SH. Opioid use disorder in the United States: insurance status and treatment access. Drug Alcohol Depend. 2008;94(1–3):207–213. doi: 10.1016/j.drugalcdep.2007.11.018. [DOI] [PubMed] [Google Scholar]
- Berliner HS. Medicaid after the Supreme Court decision. Health Econ Policy Law. 2013;8(1):133–137. doi: 10.1017/S1744133112000400. [DOI] [PubMed] [Google Scholar]
- Bhattacharya J, Goldman D, McCaffrey D. Estimating probit models with self-selected treatments. Stat Med. 2006;25(3):389–413. doi: 10.1002/sim.2226. [DOI] [PubMed] [Google Scholar]
- Bhattacharya J, Goldman D, Sood N. The link between public and private insurance and HIV-related mortality. J Health Econ. 2003;22(6):1105–1122. doi: 10.1016/j.jhealeco.2003.07.001. [DOI] [PubMed] [Google Scholar]
- Bovbjerg RR, Hadley J, Pohl MB, Rockmore M. Medicaid coverage for the working uninsured: the role of state policy. Health Aff (Millwood) 2002;21(6):231–243. doi: 10.1377/hlthaff.21.6.231. [DOI] [PubMed] [Google Scholar]
- Busch SH, Meara E, Huskamp HA, Barry CL. Characteristics of adults with substance use disorders expected to be eligible for Medicaid under the ACA. Psychiatr Serv. 2013;64(6):520–526. doi: 10.1176/appi.ps.201200011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callahan JJ, Shepard DS, Beinecke RH, Larson MJ, Cavanaugh D. Mental health/substance abuse treatment in managed care: the Massachusetts Medicaid experience. Health Aff (Millwood) 1995;14(3):173–184. doi: 10.1377/hlthaff.14.3.173. [DOI] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality. Key substance use and mental health indicators in the United States: Results from the 2015 National Survey on Drug Use and Health. 2016 Retrieved from https://www.samhsa.gov/data/sites/default/files/NSDUH-FFR1-2015/NSDUH-FFR1-2015/NSDUH-FFR1-2015.pdf.
- Chen LY, Crum RM, Martins SS, Kaufmann CN, Strain EC, Mojtabai R. Service use and barriers to mental health care among adults with major depression and comorbid substance dependence. Psychiatr Serv. 2013;64(9):863–870. doi: 10.1176/appi.ps.201200289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark RE, Samnaliev M, McGovern MP. Treatment for co-occurring mental and substance use disorders in five state Medicaid programs. Psychiatr Serv. 2007;58(7):942–948. doi: 10.1176/ps.2007.58.7.942. [DOI] [PubMed] [Google Scholar]
- Deck DD, Ley KV. Medicaid eligibility and access to mental health services among adolescents in substance abuse treatment. Psychiatr Serv. 2006;57(2):263–265. doi: 10.1176/appi.ps.57.2.263. [DOI] [PubMed] [Google Scholar]
- Deck DD, McFarland BH. Datapoints: Medicaid managed care and substance abuse treatment. Psychiatr Serv. 2002;53(7):802–802. doi: 10.1176/appi.ps.53.7.802. [DOI] [PubMed] [Google Scholar]
- Deck DD, McFarland BH, Titus JM, Laws KE, Gabriel RM. Access to substance abuse treatment services under the Oregon Health Plan. JAMA. 2000;284(16):2093–2099. doi: 10.1001/jama.284.16.2093. [DOI] [PubMed] [Google Scholar]
- Deck DD, Wiitala WL, Laws KE. Medicaid coverage and access to publicly funded opiate treatment. J Behav Health Serv Res. 2006;33(3):324–334. doi: 10.1007/s11414-006-9018-2. [DOI] [PubMed] [Google Scholar]
- Frank RG, Goldman HH, Hogan M. Medicaid and mental health: be careful what you ask for. Health Aff (Millwood) 2003;22(1):101–113. doi: 10.1377/hlthaff.22.1.101. [DOI] [PubMed] [Google Scholar]
- French MT, Popovici I. That instrument is lousy! In search of agreement when using instrumental variables estimation in substance use research. Health Econ. 2009 doi: 10.1002/hec.1572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasner-Edwards S, Rawson R. Evidence-based practices in addiction treatment: review and recommendations for public policy. Health Policy. 2010;97(2–3):93–104. doi: 10.1016/j.healthpol.2010.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Goldstein RB, Chou SP, Huang B, Stinson FS, Dawson DA, Compton WM. Sociodemographic and psychopathologic predictors of first incidence of DSM-IV substance use, mood and anxiety disorders: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Mol Psychiatry. 2009;14(11):1051–1066. doi: 10.1038/mp.2008.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, Kaplan K. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61(8):807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Ruan WJ, Pickering RP. Cooccurrence of 12-month alcohol and drug use disorders and personality disorders in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61(4):361–368. doi: 10.1001/archpsyc.61.4.361. [DOI] [PubMed] [Google Scholar]
- Guilkey DK, Lance PM. Program impact estimation with binary outcome variables: Monte Carlo results for alternative estimators and empirical examples. In: Sickles RC, Horrace WC, editors. Festschrift in Honor of Peter Schmidt. New York, NY: Springer; 2014. pp. 5–46. [Google Scholar]
- Gunja MZ, Collins SR, Blumenthal D, Doty MM, Beutel S. How Medicaid Enrollees Fare Compared with Privately Insured and Uninsured Adults: Findings from the Commonwealth Fund Biennial Health Insurance Survey, 2016. Issue Brief (Commonw Fund) 2017;10:1–10. [PubMed] [Google Scholar]
- Haber SG, Khatutsky G, Mitchell JB. Covering uninsured adults through Medicaid: lessons from the Oregon health plan. Health Care Financ Rev. 2000;22(2):119–135. [PubMed] [Google Scholar]
- Han B, Hedden S, Lipari R, Copello E, Kroutil L. Receipt of services for behavioral health problems: Results from the 2014 National Survey on Drug Use and Health. Rockville, MD: 2015. Retrieved from. [Google Scholar]
- Hasin D, Goodwin RD, Stinson FS, Grant BF. Epidemiology of major depressive disorder: results from the National Epidemiologic Survey on Alcoholism and Related Conditions. Arch Gen Psychiatry. 2005;62(10):1097–1106. doi: 10.1001/archpsyc.62.10.1097. [DOI] [PubMed] [Google Scholar]
- Hoffman C, Wang M. Health insurance coverage in America: 2002 data update. 2003 Retrieved from https://kaiserfamilyfoundation.files.wordpress.com/2013/01/health-insurance-coverage-in-america-2002-data-update.pdf.
- Holahan J, Coughlin T, Ku L, Lipson DJ, Rajan S. Insuring the poor through Section 1115 Medicaid waivers. Health Aff (Millwood) 1995;14(1):199–216. doi: 10.1377/hlthaff.14.1.199. [DOI] [PubMed] [Google Scholar]
- Kaufmann CN, Chen LY, Crum RM, Mojtabai R. Treatment seeking and barriers to treatment for alcohol use in persons with alcohol use disorders and comorbid mood or anxiety disorders. Soc Psychiatry Psychiatr Epidemiol. 2014;49(9):1489–1499. doi: 10.1007/s00127-013-0740-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mark TL, Levit KR, Vandivort-Warren R, Buck JA, Coffey RM. Changes In US spending on Mental Health And Substance Abuse Treatment, 1986–2005, and implications for policy. Health Aff (Millwood) 2011;30(2):284–292. doi: 10.1377/hlthaff.2010.0765. [DOI] [PubMed] [Google Scholar]
- Mark TL, Yee T, Levit KR, Camacho-Cook J, Cutler E, Carroll CD. Insurance Financing Increased For Mental Health Conditions But Not For Substance Use Disorders, 1986–2014. Health Aff (Millwood) 2016;35(6):958–965. doi: 10.1377/hlthaff.2016.0002. [DOI] [PubMed] [Google Scholar]
- McKenna RM. Treatment use, sources of payment, and financial barriers to treatment among individuals with opioid use disorder following the national implementation of the ACA. Drug Alcohol Depend. 2017;179:87–92. doi: 10.1016/j.drugalcdep.2017.06.028. [DOI] [PubMed] [Google Scholar]
- Mojtabai R. Trends in contacts with mental health professionals and cost barriers to mental health care among adults with significant psychological distress in the United States: 1997–2002. Am J Public Health. 2005;95(11):2009–2014. doi: 10.2105/AJPH.2003.037630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mojtabai R, Olfson M, Sampson NA, Jin R, Druss B, Wang PS, Kessler RC. Barriers to mental health treatment: results from the National Comorbidity Survey Replication. Psychol Med. 2011;41(8):1751–1761. doi: 10.1017/S0033291710002291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan SL, Winship C. Counterfactuals and causal inference : methods and principles for social research. New York: Cambridge University Press; 2007. [Google Scholar]
- National Center for Health Statistics. Health, United States, 2011: With special feature on socioeconomic status and health. 2012 Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK98752/ [PubMed]
- Rabinowitz J, Bromet EJ, Lavelle J, Hornak KJ, Rosen B. Changes in insurance coverage and extent of care during the two years after first hospitalization for a psychotic disorder. Psychiatr Serv. 2001;52(1):87–91. doi: 10.1176/appi.ps.52.1.87. [DOI] [PubMed] [Google Scholar]
- Saloner B, Akosa Antwi Y, Maclean JC, Cook B. Access to Health Insurance and Utilization of Substance Use Disorder Treatment: Evidence from the Affordable Care Act Dependent Coverage Provision. Health Econ. 2017 doi: 10.1002/hec.3482. [DOI] [PubMed] [Google Scholar]
- Saloner B, Akosa Antwi Y, Maclean JC, Cook B. Access to Health Insurance and Utilization of Substance Use Disorder Treatment: Evidence from the Affordable Care Act Dependent Coverage Provision. Health Econ. 2018;27(1):50–75. doi: 10.1002/hec.3482. [DOI] [PubMed] [Google Scholar]
- Saloner B, Bandara S, Bachhuber M, Barry CL. Insurance Coverage and Treatment Use Under the Affordable Care Act Among Adults With Mental and Substance Use Disorders. Psychiatr Serv. 2017;68(6):542–548. doi: 10.1176/appi.ps.201600182. [DOI] [PubMed] [Google Scholar]
- Sareen J, Wang Y, Mota N, Henriksen CA, Bolton J, Lix LM, Afifi TO. Baseline insurance status and risk of common mental disorders: A propensity-based analysis of a longitudinal U.S. sample. Psychiatr Serv. 2016;67(1):62–70. doi: 10.1176/appi.ps.201400317. [DOI] [PubMed] [Google Scholar]
- Saunders RC, Heflinger CA. Access to and patterns of use of behavioral health services among children and adolescents in TennCare. Psychiatr Serv. 2003;54(10):1364–1371. doi: 10.1176/appi.ps.54.10.1364. [DOI] [PubMed] [Google Scholar]
- Staiger D, Stock JH. Instrumental variables regression with weak instruments. Econometrica. 1997;65:557–586. [Google Scholar]
- StataCorp. Stata Statistical Software, Release 14. College Station, TX: Stata Corporation; 2015. [Google Scholar]
- Tsai J, Pilver CE, Hoff RA. Potential mental health needs of US adult residents under different provisions of the Affordable Care Act. J Clin Psychiatry. 2014;75(12):1402–1410. doi: 10.4088/JCP.13m08885. [DOI] [PubMed] [Google Scholar]
- Waters HR. Measuring the impact of health insurance with a correction for selection bias--a case study of Ecuador. Health Econ. 1999;8(5):473–483. doi: 10.1002/(sici)1099-1050(199908)8:5<473::aid-hec453>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- Wen H, Druss BG, Cummings JR. Effect of Medicaid Expansions on Health Insurance Coverage and Access to Care among Low-Income Adults with Behavioral Health Conditions. Health Serv Res. 2015;50(6):1787–1809. doi: 10.1111/1475-6773.12411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen H, Hockenberry JM, Borders TF, Druss BG. Impact of Medicaid Expansion on Medicaid-covered Utilization of Buprenorphine for Opioid Use Disorder Treatment. Med Care. 2017;55(4):336–341. doi: 10.1097/MLR.0000000000000703. [DOI] [PubMed] [Google Scholar]
- Zur J, Mojtabai R. Medicaid expansion initiative in Massachusetts: enrollment among substance-abusing homeless adults. Am J Public Health. 2013;103(11):2007–2013. doi: 10.2105/AJPH.2013.301283. [DOI] [PMC free article] [PubMed] [Google Scholar]