Abstract
Background
Achieving neutral limb alignment during total knee arthroplasty (TKA) has been considered an important determinant in the long-term prosthesis survival. The purpose of this study was to evaluate the association between the immediate postoperative mechanical alignment of the lower limb and the rate of revision TKA by comparing an acceptable mechanical axis group (within ± 3° from neutral alignment) and an outlier group (> 3° deviation from neutral alignment).
Methods
Between 2000 and 2006, clinical and radiographic data of 334 primary TKAs were retrospectively reviewed to determine the 10-year Kaplan-Meier survival rate. Patients were divided into acceptable and outlier groups according to the mechanical axis checked postoperatively within a month. Clinical outcomes were assessed using Hospital for Special Surgery, Knee Society Score, and Western Ontario and McMaster Universities Osteoarthritis Index score preoperatively and at the final follow-up. Postoperative complications and revision rates were also evaluated.
Results
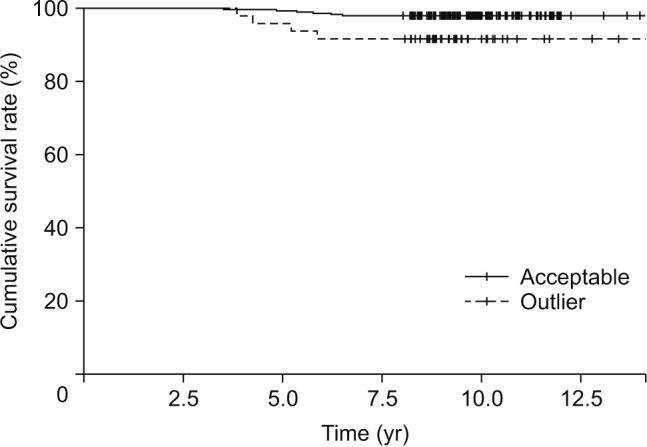
The mean change in mechanical axis between the immediate postoperative examination and the last follow-up was greater in the outlier group (1.6 ± 2.7) than in the acceptable group (0.8 ± 2.4). The revision rates were significantly different between the two groups (p = 0.04). At the last follow-up, clinical scores were all improved in both groups compared to each preoperative condition. There were no significant differences in clinical scores between the two groups at the last follow-up. The 10-year Kaplan-Meier survival analysis showed a tendency towards better survival with restoration of neutral mechanical axis. However, the difference was not statistically significant (p = 0.25).
Conclusions
Restoration of neutral limb alignment is a factor that can result in a lower revision rate and higher longevity in TKA. However, there were no significant differences in clinical outcomes between the two groups.
Keywords: Total knee arthroplasty, Mechanical alignment, Outliers, Survival rate
One long-held tenet of total knee arthroplasty (TKA) is that the overall postoperative limb alignment should be corrected to within 0° ± 3° of the mechanical axis to promote implant durability.1) Traditionally, the goal in TKA has been to create a neutral mechanical alignment, which can be achieved by using conventional instrumentation or advanced methods, including computer navigation systems and customized patient instrumentation.2,3)
However, in spite of the greater accuracy afforded by various modern implants and techniques, a substantial proportion of patients are not satisfied after TKA due to continued pain and poor function in daily living.4) In addition, several recent studies have reported that there is no significant difference in survivorship when the traditional safe zone of mechanical axis of 0° ± 3° is used to differentiate well-aligned versus malaligned knees. Some literatures have suggested that scientific and clinical evidence that supports the association between the postoperative mechanical axis of 0° ± 3° and improved implant survival after TKA is weak.1,5,6,7,8,9,10,11) Bellemans et al.12) introduced the so-called constitutional varus: 32% of males and 17% of females have varus alignment since attainment of skeletal maturity. Restoring neutral alignment could have undesirable and negative influence in these cases, resulting in overcorrection. However, this does not mean neutralization of limb alignment though the traditional bone cutting method is not important in TKA because it has resulted in successful outcomes in most patients. Most previous studies have reported that patients with neutrally aligned TKAs have improved long-term clinical and functional outcomes.13,14)
The fundamental assumption in the literature is that correction of the mechanical axis is associated with the long-term durability of TKA. Thus, the hypothesis of this study was that a mechanical axis in the 0° ± 3° range after surgery would provide better clinical results and lower revision rates than a postoperative mechanical axis beyond that range. The purpose of this study was to evaluate the association between the immediate postoperative mechanical alignment of the lower limb and the rate of revision TKA by comparing an acceptable mechanical axis group (within ± 3° from neutral alignment) and an outlier group where the mechanical axis deviated from neutral by > 3°.
METHODS
We conducted this study in compliance with the principle of the Declaration of Helsinki. The design and protocol of this retrospective study were approved by the Institutional Review Board of Chonnam National University Hwasun Hospital (IRB No. CNUHH-2017-128), and informed consent was waived. This retrospective study was performed to evaluate the impact of lower limb alignment on clinical and radiographic outcomes of TKA and analyze the long-term implant survival in 334 primary TKAs (334 patients) from January 2000 to May 2006 except for infection cases. From January 2000 to March 2006, total 1,176 TKAs were performed at our institution. Of the patients, 339 patients underwent TKA with Zimmer or E.motion implants. Five of the 339 patients who underwent revision surgery due to infection during follow-up were excluded from the study. One single senior surgeon (EKS) operated all patients at our institution. Standardized pre- and postoperative standing long-leg radiographs were obtained from all patients.
The indications for surgery were primary osteoarthritis, rheumatoid arthritis, posttraumatic arthritis, and arthritis caused by a systemic disease. Three types of TKA implant designs were used in this series: Nexgen, cruciate retaining (CR) prosthesis (Zimmer, Warsaw, IN, USA) in 83 knees; Nexgen, posterior stabilized (PS) prosthesis (Zimmer) in 108 knees; and E.motion-PS-Pro (B. Braun- Aesculap, Tuttlingen, Germany) in 143 knees. Of the total, 132 patients underwent navigation-assisted TKA.
Navigation-assisted TKAs were performed using a standard medial parapatellar approach with patellar eversion and the OrthoPilot (ver. 4.08, Aesculap) navigation system. After removal of all osteophytes and proximal tibial cutting at 0° in the coronal and sagittal planes, adequate medial soft tissue release was performed to achieve collateral balancing. The distal femoral cutting block was placed for a perpendicular cut in the coronal and sagittal planes, and the cut was completed. Then, a 4-in-1 cutting block was placed for a chamfer cut, which was done to equalize flexion and extension gaps. Conventional TKAs were performed with the same approach used in the navigation-assisted TKA. A tibial cut was performed using extramedullary instrumentation, with the goal of achieving a cut perpendicular to the tibial shaft in both coronal and sagittal planes. Intramedullary instrumentation was used for femoral alignment, and a 6° valgus cut was selected for all knees. Further, soft tissue release was performed to achieve a gap difference between the medial and lateral aspects of the tibia of less than 2 mm. Subsequently, the resection line, which was parallel to the resected proximal tibia, was drawn on the cut surface of the distal femur. Bone resection was performed after positioning the anteroposterior and chamfer cutting blocks along the resection line. Stability was confirmed after a trial insertion and then the actual component was inserted.
Radiographic Evaluation
According to the Knee Society Roentgenographic Evaluation System, all radiographic assessments on preoperative radiographs were performed by two observers (KJC and NHL) respectively. Picture archiving and communication system (PACS) digital radiographic software (Infinitt Healthcare, Seoul, Korea) was used for all measurements.
In order to determine the mechanical axis on the coronal plane, we used the angle between the mechanical axis of the femur (line connecting the center of femoral head and center of intercondylar notch) and the mechanical axis of the tibia (line connecting the center of tibial plateau with the center of the ankle). Additional radiographic evaluations were performed within 1 month after the operation and at the latest follow-up using standing full leg radiographs. The patients were divided into two groups according to the coronal alignment angle of the lower extremity. The first group was an acceptable group (286 knees [85.6%] with mechanical axis within 0° ± 3°). The second group was an outlier group (48 knees [14.4%] with mechanical axis beyond 3°). The change in mechanical axis between the postoperative assessment and the last follow-up was evaluated. Preoperative demographic data and postoperative radiographic results are summarized in Table 1.
Table 1. Patient Demographics.
| Variable | Acceptable (n = 286) | Outlier (n = 48) | p-value* |
|---|---|---|---|
| Sex (male:female) | 23 : 263 | 4 : 44 | 0.378 |
| Age (yr) | 70.2 ± 9.0 | 71.0 ± 8.0 | 0.476 |
| Body mass index (kg/m2) | 27.05 | 29.41 | 0.113 |
| Preoperative ROM | 129.3 ± 19.2 | 127.5 ± 15.7 | 0.421 |
| Mean MA (°) | 11.7 ± 7.0 | 11.4 ± 6.1 | 0.526 |
| Immediate postoperative MA (°) | 0.7 ± 1.7 | 3.5 ± 4.5 | 0.000 |
| Follow-up duration (yr) | 10.0 ± 0.5 | 10.3 ± 0.6 | 0.741 |
| Etiology | |||
| Osteoarthritis | 272 (95.1) | 46 (95.8) | 0.511 |
| Rheumatoid arthritis | 8 (2.8) | 1 (2.1) | 0.120 |
| Others | 6 (2.1) | 1 (2.1) | 0.273 |
| Implant type | |||
| Nexgen CR | 72 (26) | 11 (23) | 0.422 |
| Nexgen PS | 92 (32) | 16 (33) | 0.742 |
| E.motion CR | 122 (42) | 21 (44) | 0.676 |
Values are presented as mean ± standard deviation or number (%).
ROM: range of motion, MA: mechanical axis, CR: cruciate retaining, PS: posterior stabilized.
*Independent t-test. The p-values are of intergroup comparisons. Statistical significance was considered when p-values were below 0.05.
A radiolucent line was considered progressive if it increased in size or progressed from one zone to an adjacent zone gradually. Loosening was considered present if there was evidence of component subsidence, greater than 2-mm change in position, or an angular change of greater than 3° compared to the surrounding bone on successive radiographs or compared to previous radiographs. For instability, we defined “mild” varus/valgus and anteroposterior instability as within 3° to 6° varus/valgus deformity and within 5 mm anteroposterior instability, respectively.
Inter- and intraobserver comparisons of angle measurements at two different time points (2 weeks after first measurement) were performed to confirm the reliability of radiographic measurements.15) The intra- and interobserver measurement errors were < 1° for all analyzed angles.
Clinical Outcomes and Implant Survival Evaluation
During annual visits, clinical assessments were performed at 3, 6, and 12 months after the operation. Clinical evaluations were performed at each visit. One of the authors (KJC) conducted analysis of data collected preoperatively and at the latest follow-up. Two observers (HYY and SHL) who were not involved in surgery also analyzed the collected data. The clinical outcomes were assessed using the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) score, ranges of motion, Hospital for Special Surgery (HSS) score, and Knee Society Score (KSS) score (pain/function). We evaluated the incidence of postoperative complications and revision that might influence the survival rates of implants.
Statistical Analysis
Statistical analyses were conducted using IBM SPSS ver. 20.0 (IBM Corp., Armonk, NY, USA). For analysis of postoperative HSS and WOMAC scores, range of motion (ROM), independent t-test was used. Each parameter was compared using either chi-square test or Fisher exact test as appropriate. The p-values of < 0.05 were considered statistically significant. The Kaplan-Meier technique was used to estimate the implant survival rate. A confidence interval at 95% level was determined. The endpoint was defined as revision for any reason, including revision for mechanical failure, aseptic loosening, radiographic wear, or patellar complications.
Intraobserver reliability between the two sets of measurements obtained by observer (KJC) and interobserver reliability between two observers A and B (KJC and NHL) were analyzed using Pearson correlation coefficient and the intraclass correlation coefficient (ICC). An ICC > 0.75 was regarded as excellent; ICC 0.40–0.75, fair to good; and ICC < 0.40, poor.
RESULTS
Radiological Outcomes
Preoperatively, most knees were in varus alignment (11.6° ± 6.8° of varus [range, 26° of varus to 20° of valgus]). After the operation, knees were corrected to neutral (0.8° ± 2.2° [range, 10° of varus to 8° of valgus]). The postoperative mechanical axis alignment was a mean 0.74° ± 1.66° in the acceptable group and 3.50° ± 4.53° in the outlier group, which were changed to 1.55° ± 2.20° and 5.13° ± 3.62°, respectively, at the last follow-up, showing significant differences between groups (p < 0.05) (Table 2). There were intergroup changes at the final follow-up: three in the outlier group were changed to the acceptable group and 26 in the acceptable group were changed to the outlier group.
Table 2. Intergroup Comparison of Change in Mechanical Axis.
| Variable | Acceptable (n = 286) | Outlier (n = 48) | p-value |
|---|---|---|---|
| Immediate postoperative | 0.7 ± 1.7 | 3.5 ± 4.5 | 0.000 |
| Last follow-up | 1.6 ± 2.2 | 5.1 ± 3.6 | 0.010 |
| Interval change | 0.8 ± 2.4 | 1.6 ± 2.7 | 0.012 |
Values are presented as mean ± standard deviation.
Clinical Outcomes
There were no significant differences in preoperative patient demographics, age, or mean mechanical axis between the acceptable group and the outlier group (Table 1). Preoperative functional evaluation (HSS, WOMAC, and ROM) did not show a meaningful difference, either (Table 3). At the last follow-up, clinical scores were all improved in both groups compared to each preoperative condition. There were no significant differences in clinical scores between the two groups at the last follow-up (Table 3).
Table 3. Comparison of Pre- and Postoperative Clinical Findings between Two Groups.
| Variable | Preoperative | Postoperative | ||||
|---|---|---|---|---|---|---|
| Acceptable (n = 286) | Outlier (n = 48) | p-value* | Acceptable (n = 286) | Outlier (n = 48) | p-value* | |
| ROM | 129.3 ± 19.2 | 127.5 ± 15.7 | 0.421 | 135.7 ± 19.2 | 132.3 ± 15.2 | 0.471 |
| HSS | 64.9 ± 8.2 | 63.2 ± 11.4 | 0.417 | 90.7 ± 9.6 | 91.3 ± 9.3 | 0.243 |
| WOMAC | 41.9 ± 9.0 | 43.9 ± 9.0 | 0.122 | 11.9 ± 14.1 | 11.7 ± 10.7 | 0.189 |
| KSS pain | 14.7 ± 6.8 | 15.5 ± 7.1 | 0.290 | 46.2 ± 8.8 | 47.2 ± 9.2 | 0.497 |
| KSS function | 73.8 ± 16.7 | 72.2 ± 23.4 | 0.464 | 86.7 ± 13.3 | 89.5 ± 13.2 | 0.195 |
Values are presented as mean ± standard deviation.
ROM: range of motion, HSS: hospital for special surgery, WOMAC: Western Ontario and McMaster Universities Osteoarthritis Index, KSS: Knee Society Score.
*Independent t-test. The p-values are of intergroup comparisons. Statistical significance was considered when p-values were below 0.05.
Complications and Survival Rate
Regarding the incidence of complications, aseptic loosening, instability, polyethylene wear, polyethylene breakage, and periprosthetic fracture occurred in 2, 4, 2, 2, and 2, respectively, in the acceptable group and in 1, 1, 2, 0, and 0, respectively, in the outlier group. According to the implant type, the incidence was 2, 2, 3, 0, and 1, respectively, in the CR type and 1, 3, 1, 2, and 1, respectively, in the PS type. Six of 286 (2.2%) were revised in the acceptable group: two for aseptic loosening, two for polyethylene wear, and two for polyethylene breakage. Of the four cases with instability, one was mild varus-valgus instability and three were clinical anteroposterior instability which have been under close observation. There were two periprosthetic fractures: one was due to tibial lateral cement breakage on the inferior-lateral side of the proximal tibia, in which the cement was additionally implanted to augment bony defect under the tibial component of the lateral side; one was patella vertical fracture due to slip down, which was treated conservatively. Four of 48 knees (8.3%) were revised in the outlier group: one for aseptic loosening, one for instability, and two for polyethylene wear. Only revision rates showed significant differences between the two groups (p = 0.04) (Table 4).
Table 4. Postoperative Complications in Both Groups.
| Variable | Acceptable (n = 286) | Outlier (n = 48) | p-value* |
|---|---|---|---|
| Aseptic loosening | 2 (2 Revision) | 1 (1 Revision) | 0.211 |
| Instability | 4 | 1 (1 Revision) | 0.211 |
| Polyethylene wear | 2 (2 Revision) | 2 (2 Revision) | 0.330 |
| Polyethylene breakage | 2 (2 Revision) | 0 | 0.357 |
| Periprosthetic fracture | 2 | 0 | 0.326 |
| Total | 12 (4.2) | 4 (8.3) | 0.107 |
| Revision rate | 6 (2.1) | 4 (8.3) | 0.041 |
Values are presented as number (%).
*Chi-square test. The p-values are of intergroup comparisons. Statistical significance was considered when p-values were below 0.05.
At the last follow-up, the 10-year Kaplan-Meier survival rate analysis was performed with the endpoint defined as revision. Six patients underwent revision TKA at a mean of 5.8 years after surgery in the acceptable group. Four patients underwent revision TKA at a mean of 4.7 years after surgery in the outlier group. The cumulative survival rates in the acceptable group and outlier group at 10 years were 97.9% and 91.7%, respectively. Kaplan-Meier survival analysis showed a tendency towards a higher 10- year survival rate with restoration of a neutral mechanical axis. However, the difference was not statistically significant (p = 0.25) (Fig. 1).
Fig. 1. Kaplan-Meier survival curve for acceptable and outlier groups for 10-year follow-up.
DISCUSSION
One long-term goal of TKA has been to achieve neutral postoperative limb alignment (within ± 3° of varus/valgus relative to mechanical axis).1) The mechanical axis of the lower extremity is determined by drawing a line from the center of the femoral head to the center of the ankle joint, which corresponds to an approximately 5°–7° of valgus relative to the tibiofemoral anatomic alignment. Neutral alignment could be obtained through perpendicular bone cutting of both distal femur and proximal tibia to the mechanical axis. Restoration of limb alignment is a crucial concept because a malaligned implant often decreases the survival rate and increases the wear rate and loosening of the prosthesis, which can lead to early failure and poor functional outcomes.16,17,18,19,20,21)
Several recent studies have reported that malalignment after TKA is not a determinant factor for the survival of prosthesis.22,23) Therefore, the concept that the mechanical axis should correspond to a safety zone defined as within 3° of neutral limb alignment is being challenged.24,25) Furthermore, some studies have suggested a change of paradigm in definitive, ideal coronal alignment and implant positioning for TKA.26) Among previous studies, Parratte et al.25) retrospectively reviewed the clinical and radiological data of 393 TKAs and found that postoperative mechanical axis ± 3° had association with a low survival rate in the 15-year follow-up. They concluded that the description of alignment as a dichotomous variable (aligned versus malaligned) provides little values in regards to durability. Vanlommel et al.27) have radiographically assessed a total of 143 cases with preoperative varus deformity and divided them into three groups (neutral, mild varus [3°–6°], and moderate varus [6°–9°]) by immediate postoperative alignment and analyzed functional outcomes. They found that the mild varus group had the most desirable result.27) Matziolis et al.24) reported that there was no significant difference in the survival rate of the prosthesis or clinical outcome between the neutral alignment group and the varus deformity group.
This study is a large retrospective clinical series with a mean follow-up of 10 years to evaluate whether postoperative mechanical alignment could affect the revision rate or survival rate in the acceptable range group and in the outlier group. The result of this study was different from that of Parratte et al.25) The present study supports the notion that has been widely accepted so far: restoration of neutral alignment and traditional bone cutting are the most important factors in TKA for successful outocme.28) Several studies based on biomechanical26) and clinical6) results have shown that malalignment, especially varus deformity, will result in higher failure rates with increased strain and worse functional outcomes. Green et al.28) observed increased pressure on the posteromedial side of the proximal tibia in the knee with a tibial component placed in 5° of varus. However, neutral alignment allows for uniform distribution of pressure over the whole surface, exerting a protective effect. These findings were verified through finite element analysis,29) which also showed a peak contact stress and von Mises strain with varus tilt of the tibia. Varus deformity has been reported to be a definite factor of poor clinical outcome of TKA with 3,152 cases.1) Failure of the tibial insert is often combined with medial bony destruction which is strongly related to over 3° of tibial varus deformity, over 33.7 of body mass index, and postoperative varus deformity.1) As noted above, coronal alignment is definitely a factor that determines the outcome of TKA, although it may not be the most important factor. The rationale for restoration of neutral mechanical alignment is to improve the implant durability and patient's function following surgery. However, against our expectations, there were no significant differences in clinical outcomes between the acceptable group and the outlier group. Although technical development has decreased intraoperative errors, there still exist epidemiological outliers in 9% of tibiofemoral alignments, 4.9% of femoral implants, and 4% of tibial implants.30) The acceptable range of alignment in the present study, as in most contemporary studies, resulted in a lower revision rate. This means that postoperative restoration of neutral alignment might be a required condition to prevent failure of the prosthesis.
This study has some limitations. First, the ideal target value for alignment after TKA could not be defined more precisely. In addition, a larger number of patients is needed to bolster our argument and rationale for neutral mechanical alignment. Another limitation is the relatively small-sized outlier group compared to the acceptable group. Furthermore, the type of prosthesis was not identical: PS and CR implants were used. Lastly, there was no consideration into the sagittal plane and rotational alignment with the study only focusing on the coronal alignment. However, the significance of this study is that we confirmed that the well-aligned mechanical axis allows for lower revision rates and better durability after TKA.
Restoration of neutral limb alignment can be a factor that contributes to lower revision rates after TKA with increased longevity. However, there were no significant differences in clinical outcomes between the acceptable range group and the outlier group.
ACKNOWLEDGMENTS
The authors would like to thank Seung-Hoon Lee, orthopedic surgeon at Suncheon Hana Hospital and Hong-Yeol Yang, orthopedic fellow at Chonnam National University Hospital, for their valuable comments and analysis of this study.
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Jeffery RS, Morris RW, Denham RA. Coronal alignment after total knee replacement. J Bone Joint Surg Br. 1991;73(5):709–714. doi: 10.1302/0301-620X.73B5.1894655. [DOI] [PubMed] [Google Scholar]
- 2.Bauwens K, Matthes G, Wich M, et al. Navigated total knee replacement: a meta-analysis. J Bone Joint Surg Am. 2007;89(2):261–269. doi: 10.2106/JBJS.F.00601. [DOI] [PubMed] [Google Scholar]
- 3.Matziolis G, Krocker D, Weiss U, Tohtz S, Perka C. A prospective, randomized study of computer-assisted and conventional total knee arthroplasty: three-dimensional evaluation of implant alignment and rotation. J Bone Joint Surg Am. 2007;89(2):236–243. doi: 10.2106/JBJS.F.00386. [DOI] [PubMed] [Google Scholar]
- 4.Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KD. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res. 2010;468(1):57–63. doi: 10.1007/s11999-009-1119-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bargren JH, Blaha JD, Freeman MA. Alignment in total knee arthroplasty: correlated biomechanical and clinical observations. Clin Orthop Relat Res. 1983;(173):178–183. [PubMed] [Google Scholar]
- 6.Howell SM, Howell SJ, Kuznik KT, Cohen J, Hull ML. Does a kinematically aligned total knee arthroplasty restore function without failure regardless of alignment category? Clin Orthop Relat Res. 2013;471(3):1000–1007. doi: 10.1007/s11999-012-2613-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Howell SM, Papadopoulos S, Kuznik KT, Hull ML. Accurate alignment and high function after kinematically aligned TKA performed with generic instruments. Knee Surg Sports Traumatol Arthrosc. 2013;21(10):2271–2280. doi: 10.1007/s00167-013-2621-x. [DOI] [PubMed] [Google Scholar]
- 8.Hsu RW, Himeno S, Coventry MB, Chao EY. Normal axial alignment of the lower extremity and load-bearing distribution at the knee. Clin Orthop Relat Res. 1990;(255):215–227. [PubMed] [Google Scholar]
- 9.Hvid I, Nielsen S. Total condylar knee arthroplasty: prosthetic component positioning and radiolucent lines. Acta Orthop Scand. 1984;55(2):160–165. doi: 10.3109/17453678408992329. [DOI] [PubMed] [Google Scholar]
- 10.Lotke PA, Ecker ML. Influence of positioning of prosthesis in total knee replacement. J Bone Joint Surg Am. 1977;59(1):77–79. [PubMed] [Google Scholar]
- 11.Ritter MA, Faris PM, Keating EM, Meding JB. Postoperative alignment of total knee replacement: its effect on survival. Clin Orthop Relat Res. 1994;(299):153–156. [PubMed] [Google Scholar]
- 12.Bellemans J, Colyn W, Vandenneucker H, Victor J. The Chitranjan Ranawat award: is neutral mechanical alignment normal for all patients? The concept of constitutional varus? Clin Orthop Relat Res. 2012;470(1):45–53. doi: 10.1007/s11999-011-1936-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Choong PF, Dowsey MM, Stoney JD. Does accurate anatomical alignment result in better function and quality of life? Comparing conventional and computer-assisted total knee arthroplasty. J Arthroplasty. 2009;24(4):560–569. doi: 10.1016/j.arth.2008.02.018. [DOI] [PubMed] [Google Scholar]
- 14.Longstaff LM, Sloan K, Stamp N, Scaddan M, Beaver R. Good alignment after total knee arthroplasty leads to faster rehabilitation and better function. J Arthroplasty. 2009;24(4):570–578. doi: 10.1016/j.arth.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 15.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1(8476):307–310. [PubMed] [Google Scholar]
- 16.Tew M, Waugh W. Estimating the survival time of knee replacement. J Bone Joint Surg Br. 1982;64(5):579–582. doi: 10.1302/0301-620X.64B5.7142266. [DOI] [PubMed] [Google Scholar]
- 17.Berend ME, Ritter MA, Meding JB, et al. Tibial component failure mechanisms in total knee arthroplasty. Clin Orthop Relat Res. 2004;(428):26–34. doi: 10.1097/01.blo.0000148578.22729.0e. [DOI] [PubMed] [Google Scholar]
- 18.D'Lima DD, Chen PC, Colwell CW., Jr Polyethylene contact stresses, articular congruity, and knee alignment. Clin Orthop Relat Res. 2001;(392):232–238. doi: 10.1097/00003086-200111000-00029. [DOI] [PubMed] [Google Scholar]
- 19.D'Lima DD, Hermida JC, Chen PC, Colwell CW., Jr Polyethylene wear and variations in knee kinematics. Clin Orthop Relat Res. 2001;(392):124–130. doi: 10.1097/00003086-200111000-00015. [DOI] [PubMed] [Google Scholar]
- 20.Ensini A, Catani F, Leardini A, Romagnoli M, Giannini S. Alignments and clinical results in conventional and navigated total knee arthroplasty. Clin Orthop Relat Res. 2007;457:156–162. doi: 10.1097/BLO.0b013e3180316c92. [DOI] [PubMed] [Google Scholar]
- 21.Sikorski JM. Alignment in total knee replacement. J Bone Joint Surg Br. 2008;90(9):1121–1127. doi: 10.1302/0301-620X.90B9.20793. [DOI] [PubMed] [Google Scholar]
- 22.Schiavone Panni A, Falez F, D'Apolito R, Corona K, Perisano C, Vasso M. Long-term follow-up of a non-randomised prospective cohort of one hundred and ninety two total knee arthroplasties using the NexGen implant. Int Orthop. 2017;41(6):1155–1162. doi: 10.1007/s00264-017-3438-x. [DOI] [PubMed] [Google Scholar]
- 23.Howie DF, Love GJ, Deakin AH, Kinninmonth AW. Intraoperative deviation in limb alignment occurring at implantation in total knee arthroplasty. Knee. 2015;22(1):47–50. doi: 10.1016/j.knee.2014.11.005. [DOI] [PubMed] [Google Scholar]
- 24.Matziolis G, Adam J, Perka C. Varus malalignment has no influence on clinical outcome in midterm follow-up after total knee replacement. Arch Orthop Trauma Surg. 2010;130(12):1487–1491. doi: 10.1007/s00402-010-1064-9. [DOI] [PubMed] [Google Scholar]
- 25.Parratte S, Pagnano MW, Trousdale RT, Berry DJ. Effect of postoperative mechanical axis alignment on the fifteen-year survival of modern, cemented total knee replacements. J Bone Joint Surg Am. 2010;92(12):2143–2149. doi: 10.2106/JBJS.I.01398. [DOI] [PubMed] [Google Scholar]
- 26.Bellemans J. Neutral mechanical alignment: a requirement for successful TKA: opposes. Orthopedics. 2011;34(9):e507–e509. doi: 10.3928/01477447-20110714-41. [DOI] [PubMed] [Google Scholar]
- 27.Vanlommel L, Vanlommel J, Claes S, Bellemans J. Slight undercorrection following total knee arthroplasty results in superior clinical outcomes in varus knees. Knee Surg Sports Traumatol Arthrosc. 2013;21(10):2325–2330. doi: 10.1007/s00167-013-2481-4. [DOI] [PubMed] [Google Scholar]
- 28.Green GV, Berend KR, Berend ME, Glisson RR, Vail TP. The effects of varus tibial alignment on proximal tibial surface strain in total knee arthroplasty: the posteromedial hot spot. J Arthroplasty. 2002;17(8):1033–1039. doi: 10.1054/arth.2002.35796. [DOI] [PubMed] [Google Scholar]
- 29.Liau JJ, Cheng CK, Huang CH, Lo WH. The effect of malalignment on stresses in polyethylene component of total knee prostheses: a finite element analysis. Clin Biomech (Bristol, Avon) 2002;17(2):140–146. doi: 10.1016/s0268-0033(01)00109-7. [DOI] [PubMed] [Google Scholar]
- 30.Mason JB, Fehring TK, Estok R, Banel D, Fahrbach K. Metaanalysis of alignment outcomes in computer-assisted total knee arthroplasty surgery. J Arthroplasty. 2007;22(8):1097–1106. doi: 10.1016/j.arth.2007.08.001. [DOI] [PubMed] [Google Scholar]


