Abstract
Background
Leukocyte-poor platelet-rich plasma (LP-PRP) from peripheral blood is currently used as a concentrated source of growth factors to stimulate repair at sites of soft tissue injury. Fibroblasts are primary mediators of wound healing. Thus, we aimed to assess the positive effect of LP-PRP on human fibroblast proliferation in vitro.
Methods
LP-PRP was prepared from 49 donors. The fibroblasts were seeded, and at 24 hours after seeding, 1 × 107/10 µL LP-PRP was added once to each well. The cells were harvested 10 times during study period at our planned points, and we examined cell proliferation using the water-soluble tetrazolium salt-1 assay. We collected the supernatants and measured the amount of growth factors such as platelet-derived growth factor (PDGF)-AB/BB, insulin-like growth factor-1 (IGF-1), transforming growth factor-β1 (TGF-β1), and vascular endothelial growth factor (VEGF), which are known to be involved in wound healing processes, by multiplex assay.
Results
Human fibroblasts treated with LP-PRP showed a significant increase in proliferation when compared to untreated controls (p < 0.001 at days 4, 6, and 8). Multiplex cytokine assays revealed various secretion patterns. PDGF-AB/BB appeared at early time points and peaked before fibroblast proliferation. IGF-1 and TGF-β1 secretion gradually increased and peaked on days 4 and 6 post-treatment. The early VEGF concentration was lower than the concentration of other growth factors but increased along with cell proliferation.
Conclusions
Platelets in LP-PRP release growth factors such as PDGF, IGF-1, TGF-β1 and VEGF, and these growth factors have a promoting effect for human fibroblast proliferation, one of the important mediators of wound healing. These results suggest that growth factors derived from LP-PRP enhance the proliferation of human fibroblast.
Keywords: Fibroblast, Platelet-rich plasma, Platelet-derived growth factor, Transforming growth factor-β1
Platelet-rich plasma (PRP) is a blood concentrate that is extracted and refined from peripheral blood. Platelets in PRP release several growth factors, such as insulin-like growth factor-1 (IGF-1), platelet-derived growth factor (PDGF), vascular endothelial growth factor (VEGF), and transforming growth factor-β (TGF-β).1,2) Recent studies suggest that growth factors promote tissue repair, bone formation, and regeneration.2,3,4) As such, PRP has been increasingly used in recent years in the fields of orthopedics, orthopedic arthroscopic surgery, periodontics, maxillofacial surgery, urology, plastic surgery, and sports medicine,5) where it facilitates healing in the tendons, ligaments, and cartilage.6,7,8) However, although factors that originate from platelet α-granules influence tissue regeneration, catabolic signals from leukocytes may hinder healing in association with inflammatory cytokine expression.1,6,9) Thus, leukocyte-poor PRP (LP-PRP) preparations are commonly used for therapeutic purposes.10,11,12)
PRP can be prepared by a single-spin centrifugation protocol or with commercially available kits.13,14) LP-PRP produced from peripheral blood is currently used at orthopedic surgical sites, e.g., in operations for knee degenerative arthritis and lateral epicondylar tendinopathy.10,11,12) Compared with other conventional PRP isolations, LP-PRP requires less blood and preparation time, is relatively affordable, and is easy to utilize, because it takes relatively less centrifuging rpm and time for preparing LP-PRP.15,16)
Human fibroblasts play an important role in wound healing.17) Platelets and growth factors, such as PDGF-AB/BB, IGF-1, TGF-β, and VEGF, are known to stimulate fibroblast proliferation and wound healing, respectively.1,2,6,18) As such, the purpose of this study was to assess the positive effects of LP-PRP on human fibroblast proliferation. We also sought to characterize the various factors in LP-PRP that may mediate this effect.
METHODS
Sample Collection
Total 49 patients, who underwent surgery for chronic rotator cuff tear at Hallym University Kangnam Sacred Heart Hospital, participated in this study. Patients with malignancy or metastatic disease, acute inflammatory state, traumatic cuff tears, previous transfusion history or PRP treatment were excluded from the study. All participants provided written informed consent for this study. All experiments were performed with human fibroblasts isolated from human rotator cuff tendons with degenerative tears as approved by the Institutional Review Board of Hallym University Kangnam Sacred Heart Hospital (IRB No. 2015-01-01). The isolation protocol has been published elsewhere.19)
Whole blood (16 mL) was collected through a 21-gauge needle from a peripheral vein of 49 participants (35 males and 14 females; mean age, 54.74 ± 16.29 years). Some blood (2 mL) was transferred to a BD Vacutainer serum-separator tube (BD Diagnostics, Franklin Lakes, NJ, USA) for a complete blood count analysis, and the remainder of the obtained blood was used for LP-PRP preparation and analysis.
LP-PRP Preparation
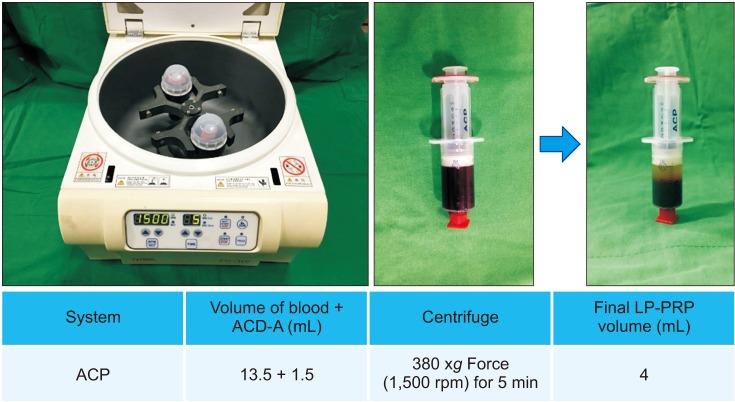
LP-PRP was prepared using an ACP preparation kit (Arthrex, Naples, FL, USA) according to the manufacturer's instructions. Briefly, 13.5 mL of blood mixed with 1.5 mL of anticoagulant citrate dextrose solution A (ACD-A) was transferred to a double ACP syringe, mixed with gentle rotation, and then centrifuged at 380 ×g (1,500 rpm) for 5 minutes to separate the red blood cell/leukocyte and plasma-platelet layers. The syringe was carefully removed, and the smaller plunger gently pulled 4 mL of clear yellow-orange LP-PRP (Fig. 1). Due to the cost problem and manual preparation that can cause minimal errors in samples, the most complete nine LP-PRP suspensions were prepared from the 49 donors.
Fig. 1. Leukocyte-poor platelet-rich plasma (LP-PRP) Arthrex ACP platelet separation system. Blood (13.5 mL) and anticoagulant citrate dextrose solution A (ACD-A, 1.5 mL) were mixed and transferred into a double ACP syringe and centrifuged at 380 ×g (1,500 rpm) for 5 minutes to separate the red blood cell/leukocyte and plasma-platelet layers, the latter of which was collected as LP-PRP (about 4 mL).
Complete Blood Cell Counts
All LP-PRP and whole blood samples were analyzed for complete blood count immediately after collection with a hematology analyzer (Siemens ADVIA 2120i; Siemens Healthcare Diagnostics, Erlangen, Germany). The relative numbers of platelets, neutrophils, monocytes, lymphocytes, and basophils and eosinophils were determined.
Fibroblast Culture and LP-PRP Treatment
Fibroblasts were cultured in Dulbecco's modified eagle medium supplemented with 1% antibiotics, including penicillin and streptomycin, and 10% fetal bovine serum in 5% CO2 at 37℃.
Cell Proliferation Assay
Cell proliferation was determined by water-soluble tetrazolium salt-1 assays and Trypan blue staining. All evaluations were performed three times with three independent experiments. For analysis, fibroblasts were seeded at a density of 7 × 103 cells/100 µL in 96-well plates. The next day, the medium was replaced and 1 × 107/10 µL LP-PRP was added to each well. After culturing for the indicated times, 10 µL of EZ-Cytox reagent (Daeil Lab Service, Seoul, Korea) was added to each well and incubated for 0.5–4 hours at 37℃. The contents of the plates were then mixed thoroughly for 1 minute, and the absorbance at 450 nm was read using a microplate reader (Molecular Devices, Sunnyvale, CA, USA).
Alternatively, LP-PRP-treated fibroblasts were also examined by Trypan blue staining with a cell counter (Luna-II, Logos Biosystems, Anyang, Korea) at the indicated points. The cells were suspended in 100 µL of trypsin-ethylenediaminetetraacetic acid (EDTA), normalized with 200 µL of complete medium containing 10% fetal bovine serum, and then centrifuged at 210 ×g force (1,000 rpm) for 5 minutes. The cell pellets were resuspended with 100 µL of Trypan blue stock solution and immediately examined under a microscope using a hemocytometer.
Multiplex Cytokine Assay
Multiplex cytokine assays were used to quantify PDGF, IGF-1, TGF-β1, and VEGF levels in LP-PRP. LP-PRP cells were seeded at 1 × 105 cells/well in a 6-well plate. Culture medium (1 mL) was then collected and analyzed using a Milliplex human cytokine/chemokine magnetic panel kit (Millipore, Billerica, MA, USA) according to the manufacturer's instructions. We added 25 µL of the samples and 25 µL of beads to each well in a 96-well plate, and the plate was incubated overnight at 4℃. The next day, the contents of the plate were removed, and 25 µL of detection antibodies was added into each well. The plates were incubated for 1 hour at room temperature. After incubation, we added 25 L of streptavidin-phycoerythrin to each well of the plates containing the detection antibodies and added 150 µL of sheath fluid into each well. Finally, we read the cytokine/chemokine concentrations in the plates on a cytometer (Luminex 200; Luminex, Austin, TX, USA).
Period of Monitoring
Human fibroblast culture and proliferation were examined at the time of 10 minutes, 30 minutes, 1 hour, 24 hours, day 2, day 4, day 6, day 8, and day 10 after treatment. Growth factors including PDGF-AB/BB, IGF-1, TGF-β1, and VEGF concentration were monitored and compared to evaluate cell proliferation after treatment.
Statistical Analysis
Statistical analysis was performed in IBM SPSS ver. 22.0 (IBM Corp., Armonk, NY, USA). Complete blood cell count was compared by paired t-test. Fibroblast proliferation was analyzed with Mann-Whitney U-tests. The Kruskal-Wallis test, followed by post-hoc Bonferroni corrections, was used to evaluate differences among independent three experiments in cell-proliferation assay. A p < 0.05 was considered significant.
RESULTS
Complete Blood Cell Counts
Compared with whole blood, LP-PRP had a high platelet count (427.61 ± 154.76 × 103/µL) but low leukocyte concentration (2.61 ± 2.26 × 103/µL), as expected. Additionally, LP-PRP showed lower counts of neutrophils, lymphocytes, monocytes, eosinophils, and basophils, as well as lower hemoglobin levels, than whole blood (Table 1).
Table 1. Complete Blood Cell Counts in Whole Blood and LP-PRP from 49 Participants.
| Variable count (103/μL) | LP-PRP | Whole blood | p-value |
|---|---|---|---|
| Platelet | 427.61 ± 154.76 | 257.12 ± 86.22 | 0.000** |
| Leukocyte | 2.61 ± 2.26 | 6.96 ± 2.21 | 0.000** |
| Hemoglobin | 0.77 ± 1.43 | 13.71 ± 1.72 | 0.000** |
| Neutrophil | 0.74 ± 1.32 | 4.22 ± 2.03 | 0.000** |
| Lymphocyte | 1.86 ± 2.01 | 1.91 ± 0.64 | 0.886 |
| Monocyte | 0.30 ± 0.56 | 0.52 ± 0.40 | 0.030* |
| Eosinophil | 0.03 ± 0.05 | 0.23 ± 0.13 | 0.000** |
| Basophil | 0.02 ± 0.05 | 0.06 ± 0.05 | 0.003** |
Values are presented as mean ± standard deviation.
LP-PRP: leukocyte-poor platelet-rich plasma.
Statistically significant: *p < 0.05, **p < 0.01.
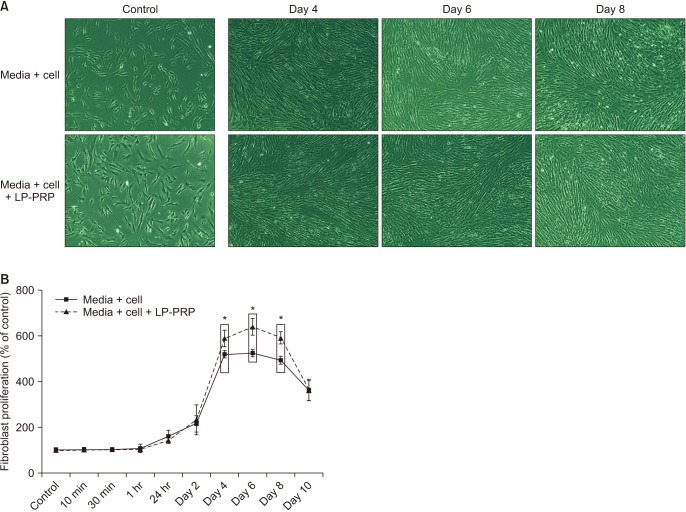
Human Fibroblast Proliferation
Proliferation analysis demonstrated that LP-PRP enhanced fibroblast proliferation. Although no differences in proliferation were observed immediately after treatment, a significant increase was found in treated cells cultured day 4 to day 8 (p < 0.001). Specifically, cell proliferation was most robust on day 6 posttreatment (Fig. 2). There were no significant differences among three times of independent experiments.
Fig. 2. (A) Human fibroblast culture and proliferation assay images of fibroblast cultures before and after leukocyte-poor platelet-rich plasma (LP-PRP) treatment. (B) Cell proliferation was examined at the indicated time points by water-soluble tetrazolium salt-1 assay. The LP-PRP-treated group showed the most robust growth on 4, 6, and 8 days. We performed this experiment in triplicate and three times. Values are presented as mean ± standard deviation of triplicate measures in three independent experiments. *p < 0.001.
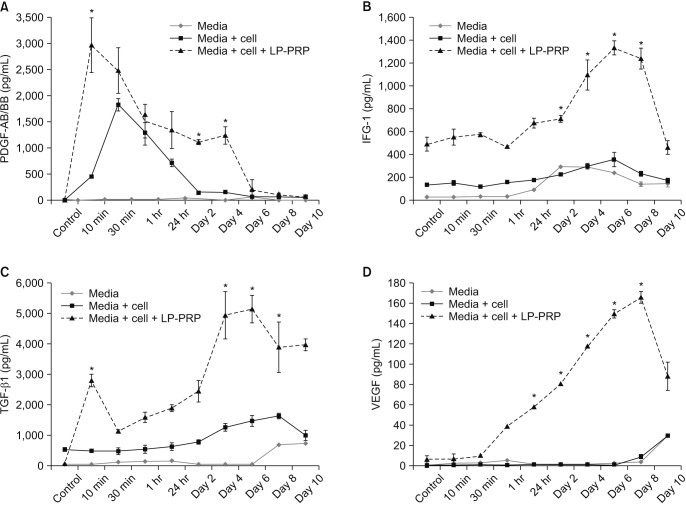
Relationship between Cell Proliferation and Growth Factor Secretion in LP-PRP-Treated Fibroblasts
We next investigated cytokine secretion following LP-PRP treatment to determine the mechanism underlying induced fibroblast proliferation. Notably, PDGF-AB/BB secretion peaked immediately after treatment and then gradually decreased over 10 days (Fig. 3A).
Fig. 3. Growth factor concentrations in leukocyte-poor platelet-rich plasma (LP-PRP) platelet-derived growth factor (PDGF)-AB/BB (A), insulin-like growth factor-1 (IGF-1) (B), transforming growth factor-β1 (TGF-β1) (C), and vascular endothelial growth factor (VEGF) (D) were monitored at the indicated time intervals. Values are presented as mean ± standard deviation of triplicate measures in three independent experiments. *p < 0.001.
IGF-1 was secreted initially at a constant level and then its level increased along with fibroblast proliferation on days 4, 6, and 8 post-treatment (Fig. 3B). TGF-β1 secretion also increased rapidly at the same time that fibroblast proliferation peaked, i.e., on days 4, 6, and 8 (Fig. 3C). In contrast, VEGF secretion rapidly increased 2 days after treatment and was maintained until day 8 (Fig. 3D).
DISCUSSION
PRP is a potential treatment option to stimulate soft tissue healing and regeneration.1) Various PRP preparation kits are commercially available;20) however, the products of each system may result in different therapeutic effects in treated patients due to varying concentrations of leukocytes, platelets, and growth factors.15,20)
Our findings show that LP-PRP contains a higher concentration of platelets and lower numbers of leukocytes as compared to whole blood, consistent with previous reports.1,13) Increased platelet concentrations convey positive effects on osteoblast and fibroblast proliferation in vitro,18) although concentrations > 2 × 105/µL are required for a therapeutic effect.14)
Our preparation method resulted in a LP-PRP isolate with 2.7-fold fewer leukocytes than in whole blood, similar to other studies.1,21,22) The leukocyte concentration in PRP correlates with inflammatory cytokine expression;1,6,9) however, little is known regarding the contribution of leukocytes in PRP to healing.23)
Several human studies have reported the anti-infection activity and immunoregulatory roles of leukocytes in PRP.15) Platelet α-granules contain several growth factors, including PDGF, IGF-1, TGF-β, and VEGF.1,2) In our study, LP-PRP-treated cultures demonstrated significant increases in PDGF-AB/BB secretion when compared to untreated controls. This increase was observed before the induction of cell proliferation, suggesting that PDGF-AB/BB acts as an acute phase initiator to boost the production of other growth factors and fibroblast proliferation. PDGF potentiates wound healing by acting as a chemotactic for macrophages and fibroblasts and by inducing glycosaminoglycan and fibronectin deposition to increase cell activity in acute healing.1,6) Moreover, PDGF has important functions in many physiological processes, including wound healing and angiogenesis, and plays a synergistic role with other factors such as IGF-1.24,25) PDGF also decreases healing time in experimentally induced wounds.26)
In our study, IGF-1 secretion was increased along with fibroblast proliferation from the time of treatment, suggesting that it triggers an increase in other growth factors as an initiator. Alternatively, IGF-1 stimulates collagen production, facilitates tendon healing, and is a potent stimulator of cell proliferation.27) Similarly, TGF-β1 secretion was also increased rapidly at the same time when fibroblast proliferation peaked, which suggests that it stimulates fibroblast proliferation similarly to IGF-1. TGF-β1 is also known to play an important role in wound healing;12) it enhances collagen synthesis and deposition in vitro1) and influences fracture healing in vivo.1,6,28) In addition, VEGF secretion in the present study rapidly increased 1 hour after treatment, which suggests that VEGF secretion was influenced by fibroblast proliferation. In healthy adults, VEGF plays a major role in angiogenesis during wound healing and attracts circulating monocytes and neutrophils to injured sites as part of the normal inflammatory response.29) Moreover, VEGF also increases permeability by changing the endothelial cell junction proteins, which could increase the formation of granulation tissue.30) Overall, the results of our study indicate that LP-PRP enhances fibroblast proliferation via PDGF-AB/BB, TGF-β, IGF-1, and VEGF secretion.
Our study had some limitations. First, the sample size was small. Second, we did not determine the optimal concentration of PRP for fibroblast proliferation. Third, we were not able to determine how each growth factor affected fibroblast proliferation. Fourth, in Fig. 3, we included the media only group as a control group. This was because the unit of data was too small as pg/mL, measurement error could not be ruled out; we had to compare with a control group to reduce errors caused by measurement.
Further studies should verify these data, and in the future, in vivo research will be needed to better understand the optimal concentration of platelets for fibroblast proliferation.
In addition, there was no comparison between the PRP only group and the LP-PRP group included. But it was expected that the LP-PRP group would show better results in fibroblast proliferation than PRP group because the catabolic effect of leukocyte interferes with cell proliferation. A comparative analysis will be needed through further experiments.
Our study is significant as it was performed in the presence of human fibroblasts, whereas previous growth factor studies were performed without cells. Thus, these data would be far more applicable to subsequent physiological studies to assess the therapeutic significance of LP-PRP therapy. The ultimate purpose of our study was to demonstrate that LP-PRP has a positive effect on wound healing and tissue degeneration. Our primary findings suggest that LP-PRP promotes proliferation in human fibroblasts, which is then potentiated by growth factor secretion; nevertheless, further studies using injured animal models are necessary to validate these findings.
Platelets in LP-PRP release growth factors such as PDGF, IGF-1, TGF-β1 and VEGF. According to our study, these growth factors have a promoting effect for human fibroblast proliferation, one of the important mediators of wound healing. We have analyzed the secretion levels of each growth factors during the study period from 10 minutes to day 10 after fibroblast treatment with LP-PRP and found that there is a positive effect by increasing level of secretion. These results suggest that growth factors derived from LP-PRP enhance the proliferation of human fibroblast, therefore we expect to be able to use LP-PRP injection for therapeutic purpose in diseases such as tendinopathy.
ACKNOWLEDGEMENTS
The authors thank Ms. Miseon Son, Department of Nursing, Konkuk University GLOCAL Campus, for her invaluable technical assistance and contributions to the statistical analysis and graphic design.
Footnotes
CONFLICT OF INTEREST: Arthrex Inc. (Naples, FL, USA) provided the ACP kits for preparation of autologous platelet-rich plasma. No other potential conflict of interest relevant to this article was reported.
References
- 1.Sundman EA, Cole BJ, Fortier LA. Growth factor and catabolic cytokine concentrations are influenced by the cellular composition of platelet-rich plasma. Am J Sports Med. 2011;39(10):2135–2140. doi: 10.1177/0363546511417792. [DOI] [PubMed] [Google Scholar]
- 2.Werner S, Grose R. Regulation of wound healing by growth factors and cytokines. Physiol Rev. 2003;83(3):835–870. doi: 10.1152/physrev.2003.83.3.835. [DOI] [PubMed] [Google Scholar]
- 3.Yun JH, Han SH, Choi SH, et al. Effects of bone marrow-derived mesenchymal stem cells and platelet-rich plasma on bone regeneration for osseointegration of dental implants: preliminary study in canine three-wall intrabony defects. J Biomed Mater Res B Appl Biomater. 2014;102(5):1021–1030. doi: 10.1002/jbm.b.33084. [DOI] [PubMed] [Google Scholar]
- 4.Kaigler D, Avila G, Wisner-Lynch L, et al. Platelet-derived growth factor applications in periodontal and peri-implant bone regeneration. Expert Opin Biol Ther. 2011;11(3):375–385. doi: 10.1517/14712598.2011.554814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Frechette JP, Martineau I, Gagnon G. Platelet-rich plasmas: growth factor content and roles in wound healing. J Dent Res. 2005;84(5):434–439. doi: 10.1177/154405910508400507. [DOI] [PubMed] [Google Scholar]
- 6.Wasterlain AS, Braun HJ, Dragoo JL. Contents and formulations of platelet-rich plasma. Oper Tech Orthop. 2012;22(1):33–42. [Google Scholar]
- 7.Sanchez M, Anitua E, Azofra J, Aguirre JJ, Andia I. Intra-articular injection of an autologous preparation rich in growth factors for the treatment of knee OA: a retrospective cohort study. Clin Exp Rheumatol. 2008;26(5):910–913. [PubMed] [Google Scholar]
- 8.Radice F, Yanez R, Gutierrez V, Rosales J, Pinedo M, Coda S. Comparison of magnetic resonance imaging findings in anterior cruciate ligament grafts with and without autologous platelet-derived growth factors. Arthroscopy. 2010;26(1):50–57. doi: 10.1016/j.arthro.2009.06.030. [DOI] [PubMed] [Google Scholar]
- 9.McCarrel TM, Minas T, Fortier LA. Optimization of leukocyte concentration in platelet-rich plasma for the treatment of tendinopathy. J Bone Joint Surg Am. 2012;94(19):e143. doi: 10.2106/JBJS.L.00019. [DOI] [PubMed] [Google Scholar]
- 10.Duif C, Vogel T, Topcuoglu F, Spyrou G, von Schulze Pellengahr C, Lahner M. Does intraoperative application of leukocyte-poor platelet-rich plasma during arthroscopy for knee degeneration affect postoperative pain, function and quality of life? A 12-month randomized controlled double-blind trial. Arch Orthop Trauma Surg. 2015;135(7):971–977. doi: 10.1007/s00402-015-2227-5. [DOI] [PubMed] [Google Scholar]
- 11.Smith PA. Intra-articular autologous conditioned plasma injections provide safe and efficacious treatment for knee osteoarthritis: an FDA-sanctioned, randomized, double-blind, placebo-controlled clinical trial. Am J Sports Med. 2016;44(4):884–891. doi: 10.1177/0363546515624678. [DOI] [PubMed] [Google Scholar]
- 12.Behera P, Dhillon M, Aggarwal S, Marwaha N, Prakash M. Leukocyte-poor platelet-rich plasma versus bupivacaine for recalcitrant lateral epicondylar tendinopathy. J Orthop Surg (Hong Kong) 2015;23(1):6–10. doi: 10.1177/230949901502300102. [DOI] [PubMed] [Google Scholar]
- 13.Osterman C, McCarthy MB, Cote MP, et al. Platelet-rich plasma increases anti-inflammatory markers in a human coculture model for osteoarthritis. Am J Sports Med. 2015;43(6):1474–1484. doi: 10.1177/0363546515570463. [DOI] [PubMed] [Google Scholar]
- 14.Mazzucco L, Balbo V, Cattana E, Guaschino R, Borzini P. Not every PRP-gel is born equal. Evaluation of growth factor availability for tissues through four PRP-gel preparations: Fibrinet, RegenPRP-Kit, Plateltex and one manual procedure. Vox Sang. 2009;97(2):110–118. doi: 10.1111/j.1423-0410.2009.01188.x. [DOI] [PubMed] [Google Scholar]
- 15.DeLong JM, Russell RP, Mazzocca AD. Platelet-rich plasma: the PAW classification system. Arthroscopy. 2012;28(7):998–1009. doi: 10.1016/j.arthro.2012.04.148. [DOI] [PubMed] [Google Scholar]
- 16.Magalon J, Bausset O, Serratrice N, et al. Characterization and comparison of 5 platelet-rich plasma preparations in a single-donor model. Arthroscopy. 2014;30(5):629–638. doi: 10.1016/j.arthro.2014.02.020. [DOI] [PubMed] [Google Scholar]
- 17.Le Pillouer-Prost A. Fibroblasts: what's new in cellular biology? J Cosmet Laser Ther. 2003;5(3-4):232–238. doi: 10.1080/14764170310021869. [DOI] [PubMed] [Google Scholar]
- 18.Graziani F, Ivanovski S, Cei S, Ducci F, Tonetti M, Gabriele M. The in vitro effect of different PRP concentrations on osteoblasts and fibroblasts. Clin Oral Implants Res. 2006;17(2):212–219. doi: 10.1111/j.1600-0501.2005.01203.x. [DOI] [PubMed] [Google Scholar]
- 19.Boyce ST, Ham RG. Calcium-regulated differentiation of normal human epidermal keratinocytes in chemically defined clonal culture and serum-free serial culture. J Invest Dermatol. 1983;81(1 Suppl):33s–40s. doi: 10.1111/1523-1747.ep12540422. [DOI] [PubMed] [Google Scholar]
- 20.Kushida S, Kakudo N, Morimoto N, et al. Platelet and growth factor concentrations in activated platelet-rich plasma: a comparison of seven commercial separation systems. J Artif Organs. 2014;17(2):186–192. doi: 10.1007/s10047-014-0761-5. [DOI] [PubMed] [Google Scholar]
- 21.Mazzocca AD, McCarthy MB, Chowaniec DM, et al. Platelet-rich plasma differs according to preparation method and human variability. J Bone Joint Surg Am. 2012;94(4):308–316. doi: 10.2106/JBJS.K.00430. [DOI] [PubMed] [Google Scholar]
- 22.Mazzocca AD, McCarthy MB, Chowaniec DM, et al. The positive effects of different platelet-rich plasma methods on human muscle, bone, and tendon cells. Am J Sports Med. 2012;40(8):1742–1749. doi: 10.1177/0363546512452713. [DOI] [PubMed] [Google Scholar]
- 23.Everts PA, Hoffmann J, Weibrich G, et al. Differences in platelet growth factor release and leucocyte kinetics during autologous platelet gel formation. Transfus Med. 2006;16(5):363–368. doi: 10.1111/j.1365-3148.2006.00708.x. [DOI] [PubMed] [Google Scholar]
- 24.Tokunaga A, Oya T, Ishii Y, et al. PDGF receptor beta is a potent regulator of mesenchymal stromal cell function. J Bone Miner Res. 2008;23(9):1519–1528. doi: 10.1359/jbmr.080409. [DOI] [PubMed] [Google Scholar]
- 25.Lynch SE, Nixon JC, Colvin RB, Antoniades HN. Role of platelet-derived growth factor in wound healing: synergistic effects with other growth factors. Proc Natl Acad Sci U S A. 1987;84(21):7696–7700. doi: 10.1073/pnas.84.21.7696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bennett NT, Schultz GS. Growth factors and wound healing: biochemical properties of growth factors and their receptors. Am J Surg. 1993;165(6):728–737. doi: 10.1016/s0002-9610(05)80797-4. [DOI] [PubMed] [Google Scholar]
- 27.Olesen JL, Heinemeier KM, Haddad F, et al. Expression of insulin-like growth factor I, insulin-like growth factor binding proteins, and collagen mRNA in mechanically loaded plantaris tendon. J Appl Physiol (1985) 2006;101(1):183–188. doi: 10.1152/japplphysiol.00636.2005. [DOI] [PubMed] [Google Scholar]
- 28.Lind M, Overgaard S, Nguyen T, Ongpipattanakul B, Bunger C, Soballe K. Transforming growth factor-beta stimulates bone ongrowth: hydroxyapatite-coated implants studied in dogs. Acta Orthop Scand. 1996;67(6):611–616. doi: 10.3109/17453679608997766. [DOI] [PubMed] [Google Scholar]
- 29.Byrne AM, Bouchier-Hayes DJ, Harmey JH. Angiogenic and cell survival functions of vascular endothelial growth factor (VEGF) J Cell Mol Med. 2005;9(4):777–794. doi: 10.1111/j.1582-4934.2005.tb00379.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dvorak HF, Detmar M, Claffey KP, Nagy JA, van de Water L, Senger DR. Vascular permeability factor/vascular endothelial growth factor: an important mediator of angiogenesis in malignancy and inflammation. Int Arch Allergy Immunol. 1995;107(1-3):233–235. doi: 10.1159/000236988. [DOI] [PubMed] [Google Scholar]