Abstract
Lumbar spine fusion has been widely accepted as a treatment for various spinal pathologies, including the degenerative spinal diseases. Transforaminal interbody fusion (TLIF) using minimally invasive surgery (MIS-TLIF) is well-known for reducing muscle damage. However, the need to use a tubular retractor during MIS-TLIF may contribute to some limitations of instrument handling, and a great deal of difficulty in confirming contralateral decompression and accurate endplate preparation. Several studies in spinal surgery have reported the use of the unilateral biportal endoscopic spinal surgery (technique for decompression or discectomy). The purpose of this study is to describe the process of and technical tips for TLIF using the biportal endoscopic spinal surgery technique. Biportal endoscopic TLIF is similar to MIS-TLIF except that there is no need for a tubular retractor. It is supposed to be another option for alternating open lumbar fusion and MIS fusion in degenerative lumbar disease that needs fusion surgery.
Keywords: Lumbar, Stenosis, Spinal fusion, Surgical procedure, Arthroscopic
Decompression by lumbar spinal fusion is considered to be the gold standard treatment for a variety of lumbar degenerative diseases.1) The open transforaminal interbody fusion (TLIF) approach was developed by Harms and Jeszenszky.2) Although TLIF has been a safe and proven technique for successful lumbar fusion, it has also been associated with severe morbidity, due to the extensive muscle dissection and retraction required in the surgical approach.3) In open surgery, degeneration and regeneration are closely related to the retraction pressure time, suggesting that muscle degeneration is secondary to long-term muscle traction.4) Foley et al.5) developed a TLIF using minimally invasive surgery (MIS-TLIF) that counteracts the disadvantages of the open TLIF. The use of a tubular retractor during MIS-TLIF surely presents a beneficial alternative for preserving the back muscles.6) However, long tubular retractors are still difficult to work with in a deep operative field with limited working space. Recently, several studies and techniques related to spinal surgery using the unilateral biportal endoscopic technique have been reported.7,8) Here, we have described a method for TLIF using the biportal endoscopic technique (BE-TLIF) to overcome the aforementioned drawbacks of MIS-TLIF.
TECHNIQUE
General Preparation
The patients were placed in the prone position on the operating table with radiolucent chest frames. All operations were performed under general anesthesia. The arthroscopy system (Arthrex, Naples, FL, USA) for general orthopedic joints was used.
Surgical Procedure
The portal was checked under fluoroscopic guidance and marked. A spinal needle was used to accurately locate the intervertebral space in the lateral view under fluoroscopy. Markings were made at 1 cm above and 1 cm below the needle, and markings were made below the pedicle in the anteroposterior view. A transverse incision of about 1 cm was made and extended to a size sufficient for the instrument to cross-cut the superficial fascia and allow adequate saline flow. A muscle detacher was used to make room for the water to flow through a portion of the proximal lamina and the interlaminar space. In the left-sided approach, the upper portal was used as the viewing portal and the lower portal was used as the working portal. An arthroscopic irrigation system was used in the BE-TLIF, such that the saline irrigation fluid would drain from the viewing portal to the working portal. When the drainage flow was poor, a small arthroscopic retractor was used to make the fluid flow more smoothly to ensure adequate visibility and to reduce the swelling of soft tissues.
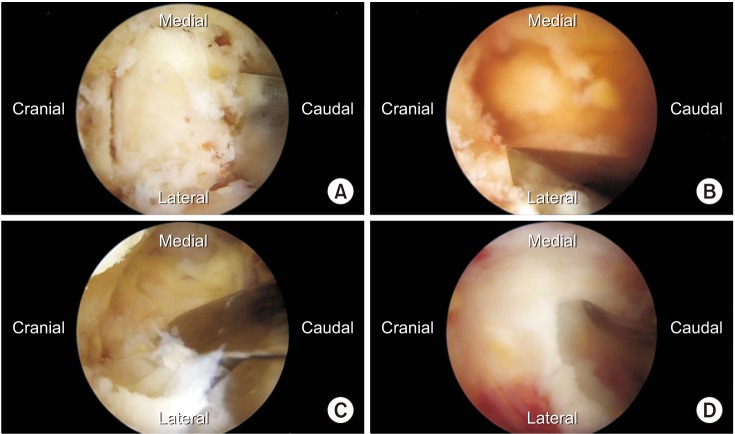
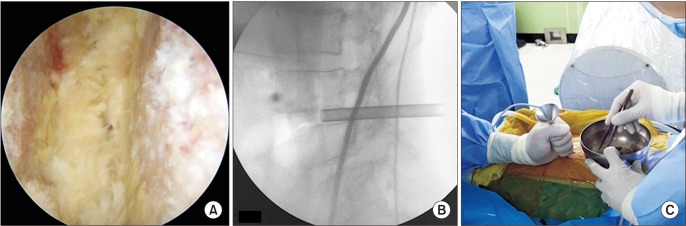
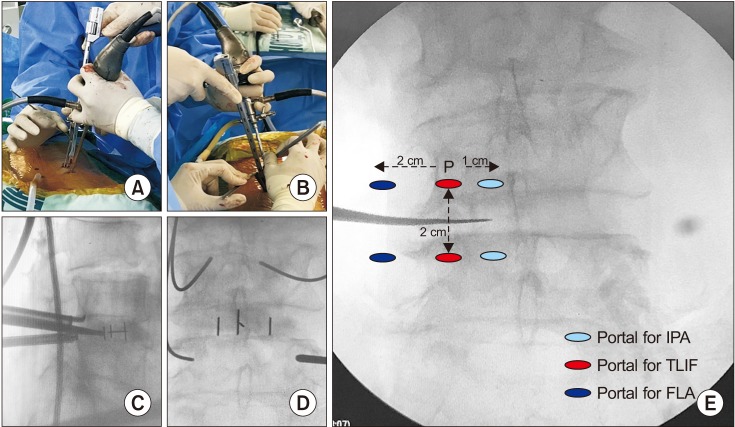
The surgical technique was performed in much the same way as the MIS-TLIF, using a tubular retractor. In MIS-TLIF, the surgery is performed using a tubular retractor and microscopy. In the case of BE-TLIF, the surgery is performed by making two incisions and using an arthroscopic irrigation system. The burr, a Kerrison punch, and an osteotome were used to perform the ipsilateral laminectomy. Subsequently, the contralateral sublaminar decompression was performed. The unilateral facetectomy was performed using osteotomes to harvest the autologous bone. After the removal of the inferior articular process, the osteotome and the Kerrison punch were used to remove the superior articular process, creating a space between the exiting nerve root and the traversing nerve root. After completion of the ipsilateral and contralateral decompressions and facectomies, the ligamentum flavum covering the dura and the nerve root was removed. An incision was made on the disc using an Indian knife specialized for endoscopy. A pair of pituitary forceps and a curette were used to perform the discectomy (Fig. 1). The arthroscope was inserted into the disc space to monitor that area, and the cartilaginous endplate was cleanly removed using a curette, to expose the subchondral bone. Allogenic bone chips and the autologous bone harvested from the lamina and facet were impacted under fluoroscopy using a specialized cannula (Fig. 2). A crescent-type cage was inserted vertically under fluoroscopic and arthroscopic guidance and then transversely positioned using a cage-specific instrument, with a retractor protecting the exiting and traversing nerve roots (Fig. 3). Two ipsilateral percutaneous pedicle screws were inserted using the two previously used portals. Two percutaneous pedicle screws on the contralateral side were inserted into two new incisions on the contralateral side, and in a manner similar to that previously described for the ipsilateral side, the two screws were connected by the percutaneous insertion of a rod. A drain catheter was then inserted to drain any possible epidural hematoma or small bony debris, and the operation was completed.
Fig. 1. Intraoperative arthroscopic images obtained during biportal endoscopic transforaminal lumbar interbody fusion. (A) Laminectomy using an osteotome for autologous bone harvest. (B) Ostectomy of the inferior articular process. (C) Removal of the foraminal ligament after facetectomy. (D) Disc incision using a biportal endoscopic specialized knife for discectomy.
Fig. 2. (A) Intraoperative arthroscopic view showing the intervertebral disc space with the cartilaginous endplate completely removed. (B) Intraoperative fluoroscopy. Bone grafting is performed using a specialized funnel in the biportal endoscopic transforaminal lumbar interbody fusion. (C) Intraoperative photograph. Fluoroscopy is used when bone grafting is performed.
Fig. 3. (A, B) Intraoperative photographs. When the cage is inserted, two semitubular retractors are used to protect the traversing and exiting roots. (C, D) Intraoperative anteroposterior and lateral views of fluoroscopy. The cage is inserted under the fluoroscopic guidance. (E) The portal locations of three different biportal endoscopic approaches. P: pedicle, IPA: ipsilateral posterior approach, TLIF: transforaminal lumbar interbody fusion, FLA: far lateral approach.
Demographic Data of Biportal Endoscopic TLIF
Fourteen consecutive patients (six males and eight females) with degenerative lumbar diseases who were treated with BE-TLIF were enrolled in this study. The average patient age at the time of surgery was 68.7 ± 8.5 years (range, 49 to 85 years). The causes of disease included eight patients with central spinal stenosis with foraminal stenosis, four patients with degenerative spondylolisthesis, and two patients with isthmic spondylolisthesis. On the level of operation, three cases were at L3–4, nine cases were at L4–5 and two cases were at L5–S1. The mean operative time was 169 ± 10 minutes. The mean estimated blood loss (drainage blood) was recorded at 74 ± 9 mL. VAS scores were improved from a preoperative average of 7.4 to 2.7 at postoperative 2 months. Two complications occurred, including one dura tear and one L5 root palsy. The dura tear was managed by conservative treatment. The patient who had L5 root palsy is undergoing follow-up treatment in the outpatient clinic (Table 1).
Table 1. Demographic Data of Biportal Endoscopic TLIF.
| Variable | Value |
|---|---|
| Mean age (yr) | 68.7 |
| Sex (male:female) | 6 : 8 |
| Diagnosis | |
| Spinal stenosis (central stenosis with foraminal stenosis) | 8 |
| Degenerative spondylolisthesis | 4 |
| Isthmic spondylolisthesis | 2 |
| Disc level treated | |
| L3–4 | 3 |
| L4–5 | 9 |
| L5–S1 | 2 |
| Operative time (min) | 169 ± 10 |
| Postoperative blood loss (mL) | 74 ± 9 |
| Preoperative VAS | 7.4 |
| Postoperative 2-month VAS | 2.7 |
| Postoperative complication | |
| L5 Paralysis | 1 |
| Dura tear | 1 |
Values are presented as mean ± standard deviation.
TLIF: transforaminal interbody fusion, VAS: visual analogue scale.
DISCUSSION
Although traditional open TLIF and posterior lumbar interbody fusion (PLIF) surgeries are effective treatments for degenerative spinal diseases, excessive damage to muscle, bone, and ligamentous structures resulting from these surgeries can cause denervation of the back muscles, loss of muscle support, and increased biomechanical strain, ultimately leading to failed back syndrome.9) The MIS fusion technique was developed by Foley et al.5) to solve this problem. In the case of MIS-TLIF, unilateral laminotomy and bilateral decompression including facetectomy are performed, followed by discectomy and bone graft with cage placement. However, the microscopic approach requires more muscle dissection in obese individuals, and tends to be relatively difficult with respect to visualization of the contralateral side. In addition, since it requires the use of a tubular retractor with a small diameter, working is relatively constrained and it is difficult to observe the endplate at the point in time when endplate preparation should occur. However, in the BE-TLIF technique, the muscular attachment of the posterior paraspinal muscle and the entire muscle group of the contralateral side can be preserved. Muscular attachments can be preserved bilaterally, and muscle ischemia can be prevented because the tubular retractor is not used in the case of BE-TLIF.
The learning curve for the BE-TLIF technique is complex, and in the early stages of learning, the procedure may be associated with an increased risk of complications (Table 1). Additionally, there are some technical pitfalls associated with MIS-TLIF and the biportal endoscopic spinal surgery.10) The BE-TLIF technique has the advantages of the use of the spinal retractor, Kerrison punch, and osteotome, which are used in open spine surgeries, as well as the use of the 4-mm head burr and 3-mm radiofrequency, which are used in arthroscopic joint surgeries. The basic technique of BE-TLIF is similar to that of MIS-TLIF, but because arthroscopy is used in BE-TLIF, it has the advantage of magnifying the view of the contralateral sublaminar decompression.8) Since saline irrigation is performed continuously during surgery, there are the additional advantages of reduced intraoperative bleeding and prevention of infection.
One of the greatest advantages of BE-TLIF surgery is the method of endplate preparation. One of the essential tasks for fusion in lumbar fusion surgery is the endplate preparation. However, endplates cannot be identified directly during either the direct lateral interbody fusion or the oblique lumbar interbody fusion procedures. The surgeon cannot accurately determine how well the endplate has been prepared. It is virtually impossible to directly prepare and identify endplates during open lumbar surgeries, such as TLIF and PLIF. In contrast, in the case of BE-TLIF, the endplate can be directly identified using arthroscopy, and preparation of the endplate is possible, thus eliminating the complete cartilage. It is also easier to perform a bone graft using a funnel specially designed for BE-TLIF under fluoroscopic guidance than it is via arthroscopy.
The portal location of BE-TLIF is slightly different from that of the existing biportal endoscopic spinal surgery portal. In the case of the ipsilateral posterior approach, the position of the portal is P −1 (interior portion of the pedicle), and it is located at P +2 or P +3 (outside the pedicle) for the far lateral approach in the horizontal position. However, the horizontal position of the portal during the biportal endoscopic TLIF is best located in the center of the pedicle (Fig. 3). The first reason is that when facetectomy is performed, it can be seen in a vertical position when removing the superior and inferior processes. Second, it is easy to insert the cage vertically while checking both the exiting and traversing nerve roots. Third, it is best to position the portal below the pedicle because inserting a screw at the location of the viewing and working portals avoids the need for additional incisions for pedicle screw fixation. When inserting the cage, it is important to identify and protect the exiting and traversing nerve roots to avoid nerve damage. When inserting the cage, it is best to switch the viewing and working portals for a time, so that viewing is provided by inserting the scope into the lower portal. Two root retractors are inserted at the same time into the upper portal to safely insert the cage, while protecting the exiting and traversing roots (Fig. 3). Technically, the biportal endoscopic TLIF is a sufficiently viable procedure. It achieves sufficient neural decompression and provides another option in the list of alternatives to open lumbar fusion and MIS fusion for degenerative lumbar diseases that require fusion surgery.
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Bagan B, Patel N, Deutsch H, et al. Perioperative complications of minimally invasive surgery (MIS): comparison of MIS and open interbody fusion techniques. Surg Technol Int. 2008;17:281–286. [PubMed] [Google Scholar]
- 2.Harms JG, Jeszenszky D. Die posteriore, lumbale, interkorporelle fusion in unilateraler transforaminaler technik. Oper Orthop Traumatol. 1998;10(2):90–102. doi: 10.1007/s00064-006-0112-7. [DOI] [PubMed] [Google Scholar]
- 3.Gejo R, Matsui H, Kawaguchi Y, Ishihara H, Tsuji H. Serial changes in trunk muscle performance after posterior lumbar surgery. Spine (Phila Pa 1976) 1999;24(10):1023–1028. doi: 10.1097/00007632-199905150-00017. [DOI] [PubMed] [Google Scholar]
- 4.Kawaguchi Y, Matsui H, Tsuji H. Back muscle injury after posterior lumbar spine surgery. Part 1: histologic and histochemical analyses in rats. Spine (Phila Pa 1976) 1994;19(22):2590–2597. doi: 10.1097/00007632-199411001-00017. [DOI] [PubMed] [Google Scholar]
- 5.Foley KT, Holly LT, Schwender JD. Minimally invasive lumbar fusion. Spine (Phila Pa 1976) 2003;28(15 Suppl):S26–S35. doi: 10.1097/01.BRS.0000076895.52418.5E. [DOI] [PubMed] [Google Scholar]
- 6.Kim CW. Scientific basis of minimally invasive spine surgery: prevention of multifidus muscle injury during posterior lumbar surgery. Spine (Phila Pa 1976) 2010;35(26 Suppl):S281–S286. doi: 10.1097/BRS.0b013e3182022d32. [DOI] [PubMed] [Google Scholar]
- 7.Choi CM, Chung JT, Lee SJ, Choi DJ. How I do it? Biportal endoscopic spinal surgery (BESS) for treatment of lumbar spinal stenosis. Acta Neurochir (Wien) 2016;158(3):459–463. doi: 10.1007/s00701-015-2670-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Eum JH, Heo DH, Son SK, Park CK. Percutaneous biportal endoscopic decompression for lumbar spinal stenosis: a technical note and preliminary clinical results. J Neurosurg Spine. 2016;24(4):602–607. doi: 10.3171/2015.7.SPINE15304. [DOI] [PubMed] [Google Scholar]
- 9.Sihvonen T, Herno A, Paljarvi L, Airaksinen O, Partanen J, Tapaninaho A. Local denervation atrophy of paraspinal muscles in postoperative failed back syndrome. Spine (Phila Pa 1976) 1993;18(5):575–581. doi: 10.1097/00007632-199304000-00009. [DOI] [PubMed] [Google Scholar]
- 10.Choi DJ, Choi CM, Jung JT, Lee SJ, Kim YS. Learning curve associated with complications in biportal endoscopic spinal surgery: challenges and strategies. Asian Spine J. 2016;10(4):624–629. doi: 10.4184/asj.2016.10.4.624. [DOI] [PMC free article] [PubMed] [Google Scholar]