Abstract
Recently, numerous side effects of synthetic drugs have lead to using medicinal plants as a reliable source of new therapy. Pain is a global public health problem with a high impact on life quality and a huge economic implication, becoming one of the most important enemies in modern medicine. The medicinal use of plants as analgesic or antinociceptive drugs in traditional therapy is estimated to be about 80% of the world population. The Lamiaceae family, one of the most important herbal families, incorporates a wide variety of plants with biological and medical applications. In this study, the analgesic activity, possible active compounds of Lamiaceae genus, and also the possible mechanism of actions of these plants are presented. The data highlighted in this review paper provide valuable scientific information for the specific implications of Lamiaceae plants in pain modulation that might be used for isolation of potentially active compounds from some of these medicinal plants in future and formulation of commercial therapeutic agents.
1. Introduction
Pain comes in many forms: acute, chronic, visceral, inflammatory, or neuropathic [1, 2]. It is not simply a result of tissue damage but also reflects the influence of many psychological variables such as attention, anxiety, stress [3], suggestion, or previous experiences and may have a significant genetic contribution [4]. Pain accompanies most pathologies present in current medical practice, and 25% percent of Americans, for example, experience pain on a daily basis. Having the numbers on its side, pain became a global public health problem and a leading cause of disability all over the world [5].
As life expectancy is rising and chronical pathologies along with it, the prevalence of accompanying pain is expected to increase yearly, with higher prevalence in elderly patients, where the treatment is also more sensitive [6, 7]. Considering the above, new therapeutic agents with increased efficacy, less side effects, and lower costs and leading to an improved quality of life [8–11] should become one of the primary objectives in modern medical research, together with constant monitoring [12] of the previous mentioned aspects.
The medicinal use of plants as analgesic drugs in folk medicine is an ancient tradition, far older than the current sciences of medicine in developing countries [13, 14]. According to estimations, up to 70,000 plant species are used ethnomedicinally worldwide. Effects of herbal extracts have been studied by different pain tests including writhing test, light tail flick test, tail immersion test, hot-plate test, and formalin test [15].
The exploration for new analgesic combinations from the enormous arrays of medicinal plant resources is growing. This is because such information holds guarantees for the finding of new therapeutic agents capable of inhibiting, decreasing, or relieving pain [16–28]. Plants characterize a vast natural supply of appreciated compounds that might achieve primary importance for the expansion of novel drugs [29]. The survey of the effectiveness of plant-based remedies used in the folk medicine has given great reflections because they are cheap and have reduced side effects.
According to the World Health Organization (WHO), about 80% of the world population still relies mainly on plant-based drugs [30], thus lowering at the same time the impact of self-medication side effects [6]. The data in biomedical literature presenting plants with medicinal capabilities are very similar to the array of publications depicting the modulatory effects certain ones have over pain perception.
The Lamiaceae family, one of the most important herbal families, incorporates a wide variety of plants with biological and medical applications. The most known members of this family are a variety of aromatic spices like thyme, mint, oregano, basil, sage, savory, rosemary, self-heal, hyssop, lemon balm, and some others with more limited use [31].
Our main objective was to perform a review of this literature for the specific implications of Lamiaceae family plants in pain modulation and thus aid the constant search for new potential agents of natural origin with analgesic effects.
2. Materials and Methods
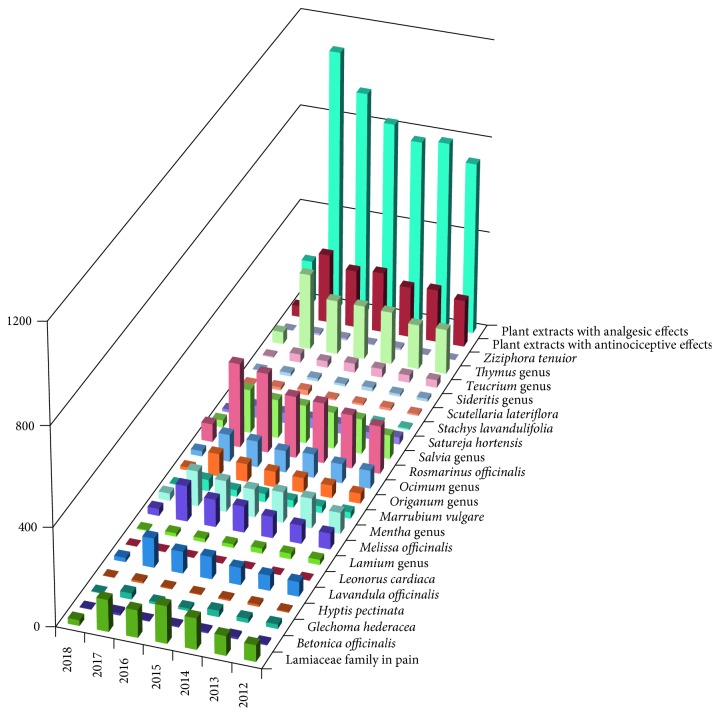
The search strategy employed in this review includes internationally accepted databases, namely, ScienceDirect, Scopus, Web of Science, and PubMed, using specific keywords of both whole plant products and plant extracts, pain, and analgesic and antinociceptive effects. For investigation, a combination of keywords was used [pain; analgesic; antinociceptive; plant extract] + [Betonica officinalis; Glechoma hederacea; Hyptis pectinata; Lavandula; Leonurus cardiaca; Lamium; Melissa officinalis; Mentha; Marrubium vulgare; Origanum; Ocimum; Rosmarinus officinalis; Salvia;Satureja hortensis; Stachys lavandulifolia; Scutellaria lateriflora; Sideritis; Teucrium; Thymus; Ziziphora tenuior] + [Lamiaceae; botanical genus]. Case reports, case studies, in vivo and in vitro relevant studies, and comparative studies were included in this search strategy. Additionally, text books and potentially relevant reviews were explored and included in the reference list. The literature search was confined to the period between 2003 and December 2017. Several articles before 2000 were also included in order to point out the universal interest in natural products with potential applicability in therapy. The dynamic character of the field is reflected in the number of recent publications. For example, a search with the keywords “Lamiaceae family and pain” in ScienceDirect yields 152 titles in 2015, 111 in 2016, and 129 in 2017, and 23 papers will be published in the first months of the next year (Figure 1).
Figure 1.
Number of publications according to ScienceDirect.
3. Species of the Lamiaceae Family with Potential Analgesic/Antinociceptive Effects
3.1. Rosmarinus Genus
Rosmarinus in the Lamiaceae family is a genus of woody, perennial herbs with fragrant evergreen needle-like leaves that is native to the Mediterranean Basin.
3.1.1. Rosmarinus officinalis
Rosmarinus officinalis L., commonly called rosemary, is a Mediterranean shrubby herb and widely spread in European, American, and Asian countries. It is a common spice used worldwide for culinary, medicinal, and commercial uses, including the fragrance and food industries [32]. The leaves of rosemary (fresh or dries) are used for their characteristic aroma in cooking or consumed in small amounts as herbal tea, while rosemary extracts are regularly used for their natural antioxidant active proprieties to improve the shelf life of perishable foods. Recently, rosemary extracts (E392) have been approved as a safe and effective natural antioxidant for food preservation by the European Union [33].
Phytochemical studies have revealed that leaves contain 0.5% to 2.5% volatile oil. The major components of rosemary oil include monoterpene hydrocarbons (alpha and beta-pinene), camphene, limonene, camphor (10% to 20%), borneol, cineole, linalool, and verbinol. Rosemary contains a widespread variety of volatile and aromatic components. Flavonoids in the plant consist of diosmetin, diosmin, genkwanin, luteolin, hispidulin, and apigenin [34–41]. Additionally, terpenoid components from rosemary consist of the triterpenes oleanolic and ursolic acid and the diterpene carnosol. Phenols in rosemary comprise caffeic, chlorogenic, labiatic, neochlorogenic, and rosmarinic acids. Rosemary covers high amounts of salicylates [42–48].
Modern pharmacological studies have indicated that rosemary and its constituents, especially caffeic acid derivatives such as rosmarinic acid, have various traditional uses in ethnomedicine including analgesic, anti-inflammatory, anticarcinogenic, antirheumatic, spasmolytic, antihepatotoxic, atherosclerotic, carminative, and choleretic applications [44–54], protection against UV and gamma radiation, and amelioration of stress [43].
The powdered leaves are used as an effective natural flea and tick repellent. Activity against certain bacteria including Staphylcoccus aureus, Staphylococcus albus, Vibrio cholerae, Escherichia coli, and Corynebacterium has been observed. One study found that rosemary oil is most active against “meat spoiling” Gram-negative (Pseudomonas) and Gram-positive (Lactobacillus) bacteria [49].
Even though rosemary oil is used safely as a food flavoring spice and whole leaves are used as a potherb for seasoning, ingestion of great quantities can be associated with toxicity characterized by stomach and intestinal irritation and kidney damage. While rosemary oil is irritating to rabbit skin, it is not usually considered to be a sensitizer for human skin [55].
Bioactive compounds such as flavonoids, diterpenes, phenols, and triterpenes from plant sources have been traditionally extracted by a conventional solid-liquid extraction. Nevertheless, this extraction technique presents several disadvantages, mainly because it is an arduous, time-consuming process that requires a high consumption of solvents, and in some cases provides low recovery. For that reason, in last years, new promising extraction methods are arising, which introduce some form of additional energy in order to facilitate the transfer of solutes from the sample to solvent in a faster process [54]. Thus, microwave-assisted extraction [56] and/or ultrasound-assisted ethanol, acetone, or n-hexane extraction represent alternatives to the conventional method, improving the speed and efficiency of the extraction process and reducing the consumption of solvents [57].
Previous studies have revealed that the rosemary extract may have analgesic and anti-inflammatory effects [58–62]. Therefore, data have shown that the ethanolic extract of rosemary inhibited acetic acid-induced pain in mice with an ED50 of 108.84 mg/kg−1 [23]. Furthermore, the extract inhibited the time mice spent licking and shaking induced by formalin injections. Nevertheless, the extract did not display any anti-inflammatory activity as evaluated by uric acid induced-hind limb edema in rats [23]. In an experiment conducted by Emami et al. [34], the effects of R. officinalis extract and its major constituent, carnosol, on plasma corticosterone levels and activity of the enzymes cyclooxygenase types 1 and 2 (COX1 and COX2) reduced pain in phase 2 of the formalin test, which was not inhibited by naloxone and/or memantine. In addition, pretreatment of the animals with R. officinalis extract and/or carnosol reduced the formalin-induced inflammation. Moreover, the extract and carnosol did not affect plasma corticosterone levels compared with the control group. Interestingly, both the extract and carnosol inhibited COX1 and COX2 activities. Going one step further, one can conclude that R. officinalis extract and carnosol suppress pain and inflammation induced by formalin injection, which may be due to inhibition of the activity of COX1 and COX2 enzymes.
3.2. Marrubium Genus
Marrubium is a genus of flowering plants that are included in the Lamiaceae family and are found in the temperate regions of Europe, North Africa, and Asia as far east as the Xinjiang region, and some species are also naturalized as far as North and South America. Marrubium, known as horehound or hoarhound, counts approximately 40 species of flowering plants native to the temperate countries of Europe, northern Africa, and Asia.
3.2.1. Marrubium vulgare
Marrubium vulgare L., commonly named as “marimba” or “marroio” in Brazil and white horehound in Europe, is regularly used in traditional medicine to cure a diversity of maladies [63, 64].
Phytochemical investigations on different parts of M. vulgare have reported the presence of alkaloids, lactones, steroids, tannins, a series of phenylpropanoid esters, diterpenoids [65], and flavonoids [64], together with their derivatives. Marrubiin, a furano labdane diterpenoid, was found to be the major chemotaxonomic marker isolated from leaves of the plant and exhibits potent antinociceptive properties and vasorelaxant activity [66–68].
Marrubiin, the main active ingredient of M. vulgare, seems to be generated as an artifact from premarrubiin during the extraction procedure when high temperatures are involved in extraction or concentration [69].
The leaves and stems are known to have antiseptic, antispasmodic, antidiabetic, diuretic, strongly expectorant, and tonic roles [70, 71]. The intensive modern research and clinical trials have confirmed several capabilities traditionally described to M. vulgare, such as antimicrobial against Gram-positive bacteria, antioxidant, analgesic [66, 67], anti-inflammatory [71], and anti-oedematogenic [72]. Furthermore, extracts of this plant have shown some effects on type II diabetes [73] and, recently, on neurological disorders [74, 75]. One study found that marrubiin has dose-related antinociceptive effects. The antinociceptive properties were observed using different routes of administration (systemic and oral), and the effect was sustained over a long period of time.
The great potencies observed in the writhing test and formalin-influenced pain test propose that marrubiin acts by some peripheral mechanism. In the hot-plate test, marrubiin did not increase the latency period of pain induced by the thermal stimuli. Reducing the lactone ring of marrubiin with the formation of marrubiinic acid and two esterified derivatives has conditioned the successful analgesic effect influencing the number of writhes in mice. Marrubiinic acid exhibited a high analgesic effect that has been long established in other experimental models of pain, suggesting the possibility to use it as a new and useful analgesic agent [67]. Marrubiin does not prove any cytotoxicity against 66 cancer cell lines according to the NIH PubMed website [Marrubiin-Compound Summary (CID 73401)]. In vivo experimental studies have documented an LD50 of 370 mg/kg body weight [68], and recent data have highlighted a safety limit up to 100 mg/kg body weight when injected into mice [71].
3.3. Sideritis Genus
Sideritis genus counts more than 150 species of plants that are situated primarily in the Mediterranean area and also in Atlantic regions, North Africa, and even Norway, with apparent differences in composition between the same species corresponding to the geographical place of provenience [76]. The species have been used as flavoring agents, widely as ingredients for tea preparation or with medicinal purposes [77] in some areas being listed as an endangered plant. Although the use in traditional medicine has been extensive in the abovementioned places, Sideritis species have reduced usage in western medicine [78], because medical literature are offering data mostly on the scardica, lotsy, and stricta species.
3.3.1. Sideritis scardica
S. scardica Gris. is also known as “Greek tea” or “mountain tea.” The components of scardica have been studied through various methods for their presence as well as medical role in both animal and human studies.
By using chromatographic separations (HPLC) and mass spectrometry, one study found six different flavonoid aglycones: luteolin, apigenin, hypolaetin, 4′-O-methylhypolaetin, isoscutellarein, and 4ʹ-O-methylisoscutellarein [79], and also other components like sterols, coumarins, flavonoids, essential oil, iridoids, terpenoids, and glycosides [76]. The presence of phenolic antioxidants (catechins) correlating to the antioxidant activity of Greek mountain tea was also established [80].
Gas chromatography with mass spectrometry (GC-MS) analysis demonstrated that the composition of S. scardica oil samples, however, varies from region to region. In the oil from Macedonia, for example, α-cadinol is predominant as compared to the Bulgarian version of the same plant oil which contains mostly diterpenic compounds and octadecenol. Interestingly, none contained menthol, nerol, or geraniol, which are the major components in the S. scardica oil from Yugoslavia [81].
For an overview of the Sideritis species in the Balkan area, mountain tea was analyzed by mass spectrometry coupled to high-performance liquid chromatography with diode-array detection. The analysis found that it contains 90% phenylethanoid glycosides and flavonoid acetylglycosides [82]. Turkish S. scardica oil has β-pinene in abundance as compared to the Greek version which contains α-pinene primarily. Both these varieties are mainly rich in monoterpene hydrocarbons unlike the ones from Macedonia and Bulgaria, which are poor in these compounds [83]. Significant differences in components have also been proven between the fresh and dried versions of the plant material [84].
An analysis of urine samples from humans who received oral administration of S. scardica showed that the flavonoid metabolites were dominant in urine samples and that hypolaetin and isoscutellarein had the largest number of metabolites (methylhypolaetin and methylisoscutellarein glucuronides) together with apigenin [85].
The pharmacological activity of S. scardica is attributed to the high content of flavonoid and phenolic compounds. Studies have demonstrated that plants from the Sideritis genus have antioxidant, anti-inflammatory, diuretic, antibacterial, analgesic, and antifungal effects [86]. In experimental ex vivo models, S. scardica showed a capacity to inhibit human serotonin transporter (hSERT) greater than in rat models [77]. Accordingly, the in vivo test in rats showed that S. scardica extract administered orally has been associated with psychostimulant and antidepressive effects, being classified as perhaps a substitute for adaptogens and thus useful for other pathologies correlated with depressive or altered mental status like sleep apnea or increased cardiovascular risks [87–89].
The antibacterial activity seems to be influenced by the method of obtaining the extract: carbon dioxide extraction being superior to hydrodistillation and is attributed partially to diterpenes and fatty acids and their derivates and also to other momentarily unknown elements that might be involved [90] but with a certain degree of effect on different types of pathogens.
The antioxidant activity was widely demonstrated, probably due to the content of catechins but not limited to this and has multiple health benefits and implications in pain treatment proving a possible valuable agent in limiting the use of analgesics, anti-inflammatory, and antipyretic forms of self-medication [6, 91].
In vivo models demonstrated the anti-inflammatory effects of S. scardica over a model of carrageenan-induced rat paw edema and proved gastroprotective activity over ethanol-induced acute stress ulcer in rats and also a promising cytotoxic activity [92], attributing in part to flavonoid constituents (apigenin and luteolin) that can induce cell-cycle arrest and cellular apoptosis in vitro [93]. In vivo models demonstrated a preventive capacity of S. scardica over Aβ-induced memory impairments in transgenic and nontransgenic mice and proved a possible positive effect in Alzheimer's disease, fully rescuing neuronal loss in transgenic mice, thus being flagged as a possible treatment forimproving memory in healthy adults and in dementia patients [78].
The usage of S. scardica in traditional and modern medicine has demonstrated various degrees of effectiveness with promising beneficial health results in a long series of pathologies from prevention of anemia, anxiety disorders, major depression, cardiovascular disease, attention-deficit hyperactivity disorder, mental impairment, or neurodegenerative diseases [77] to rheumatic problems [94], inflammatory pain, gastric ulcer [93], pulmonary pathologies (common cold, lung emphysema, bronchitis, and asthma) [85], and also an effective cytotoxic activity [92, 95]. The anti-inflammatory and edema-reducing capabilities should be considered as the basis for further studies of S. scardica implication in pain modulation.
3.3.2. Sideritis lotsyi
Sideritis lotsyi Pit. contains tetracyclic diterpenes (ent-kaur-16-ene and epicandicandiol 7β-monoacetate-18-palmitate), rhoiptelenol, hydrocarbon ent-trachylobane, amyrin, trachinodiol, a rare diterpene 16β,18-dihydroxy-ent-atisane, and 5-hydroxy-3,7,4′-trimethoxyflavone, but the content is different between S. lotsyi and S. lotsyi var. mascaensis [96]. S. lotsyi var. mascaensis extracts were studied in a comprehensive analysis for the antimicrobial activity, toxicity, and anti-inflammatory and analgesic proprieties.
A dose of 2 g/kg body weight S. lotsyi extracts administered orally in mice did not show any toxic effects; however, a dose of only 250 mg/kg ethanol extract administered orally has shown analgesic proprieties on the visceral pain produced during the writhing test, and the chloroform fraction demonstrated antinociceptive effect. The same extracts manifested anti-inflammatory effect on the early, histamin-mediated, phase of paw inflammation, but much more significant effects were observed in ear inflammation with topical administration. Contrary to S. scardica, no antimicrobial effect was noted [97].
3.3.3. Sideritis stricta
Sideritis stricta Benth. is listed as an endangered plant and is being used as an aromatic and medicinal plant containing essential oils with antimicrobial, cytotoxic, antiviral, and antioxidant properties [98]. The diterpenes composition was identified as sideroxol, 7-acetyl sideroxol, 7-epicandicandiol, linearol (5), ent-7α,15β,18-trihydroxy-kaur-16-ene, ent-7α-acetyl,15,18-dihydroxy-kaur-16-ene, foliol, sideridiol, siderol, and the recently identified ent-1β-hydroxy-7α-acetyl-15β,16β-epoxykaurane [99] together with two flavonoid glycosides and a phenolic fraction by means of spectroscopic evidence [100]. Although phenolic compounds did not manifest anti-inflammatory proprieties, the flavonoid glycosides show both anti-inflammatory and antinociceptive capabilities when combined [100]. Similarly to S. lotsyi, the acetone extract of S. stricta showed lower antimicrobial activity as compared to gentamicin [99], and no extensive data with the implications of S. stricta over pain are published.
3.4. Thymus Genus
Thymus genus, part of the Lamiaceae family, consists of over 350 species of aromatic plants with evergreen leaves. Geographically, these plants extend to Asia, North Africa, and Europe. Although more than one species is cultivated for culinary (cheese and liqueur flavor agent) or ornamental use, the most extensively studied in literature is Thymus vulgaris. Used for thousands of years in traditional medicine, the effects of Thymus species in medicine is wide, from antimicrobial and anti-inflammatory to possible treatment for dementia or oncological pathologies through apigenin [101].
3.4.1. Thymus vulgaris
GC-MS and GC-FID analyses revealed that the main active components in one type of Thymus vulgaris L. essential oil are thymol (41.0%), geraniol (26.4%), thujanol (42.2% cis-sabinene hydrate and 7.3% trans-sabinene hydrate), and linalool (72.5%) [102], and others also contain borneol and carvacrol. The chemotypes of thyme are determined based on oil compositions. Geographical provenience and weather influence the chemotype and composition [103], which was demonstrated by a study comparing essential oils from two regions of France (linalool chemotype with 76.2% linalool and thymol chemotype with 47.1% thymol) and two regions of Serbia (geraniol chemotype with 59.8% geraniol and sabinene hydrate chemotype with 30.8% cis-sabinene hydrate) [104].
The terpenoids associated with T. vulgaris anesthethic capabilities are thymol (2-isopropyl-5-methylphenol) and eugenol (4-allyl-2-methoxyphenol) [105]; moreover, thymol inhibits synthetisation of vitamin K and is implicated in the inhibition of platelet aggregation [106], resulting in potential anticoagulant activity [107].
In animals, hydroalcoholic extracts of propolis T. vulgaris showed promising results in the treatment of dermal leishmaniasis or Tetranychus urticae [108, 109]. T. vulgaris also has a spasmolytic, antimicrobial, anti-inflammatory, immunomodulatory, and antioxidant capabilities, these effects being attributed to the thymol contained in the volatile thyme oil [110]. Confirming the effect of T. vulgaris on respiratory pathologies and the spasmolytic effects underlined in ex vivo studies [111], a study also has indicated its promising potential for the treatment of gastrointestinal pathologies in animal models without any toxic potential.
By inhibiting, in vivo, TNF-α, lipopolysaccharide inflammatory induced cell influx, IL-6, protein concentration in bronchoalveolar lavage fluid, and NF-κB activation in the lung, thymol could be a promising therapeutical agent for acute lung injury [112].
The inhibitory role over the nitric oxide (NO) by limiting iNOS mRNA expression plays a major role in the anti-inflammatory proprieties of T. vulgaris extracts [113]. Also, because of the antioxidant capabilities and being an inhibitor of acetylcholinesterase, T. vulgaris could be a promising therapeutic agent for neurodegenerative disorders like dementia or Alzheimer's disease [114].
In vitro activity of T. vulgaris oil confirmed a high antibacterial activity over Gram-positive and also Gram-negative bacteria, though the effect was smaller on the latter [102].
In traditional medicine and in clinical practice, T. vulgaris is used, and T. vulgaris shows promising results on inflammatory skin disorders [115], scabies, herpes, wounds, alopecia, dental plaque [116], ringworm, and headaches [106]. Moreover, T. vulgaris showed a promising insecticidal effect on Culex pipiens, the vector for lymphatic filariasis [117], demonstrating an increased importance in many fields.
Probably in part due to the anti-inflammatory and antioxidant capabilities, Thymus extracts demonstrated analgesic, anti-inflammatory, and antipyretic activity in mouse models of pain. Therefore, the authors concluded that the extracts of Thymus may be used against pain, pyrexia, and inflammation [118], correlating with other similar findings that position T. vulgaris as a modulator agent over acute and chronic pain [119]. In clinical practice, comparative effects of T. vulgaris and ibuprofen on pain severity associated with primary dysmenorrhea were found [120].
3.4.2. Thymus pulegioides
Thymus pulegioides L. belongs to the genus Thymus, and together with three other species, it has a different phenolic content than T. vulgaris [121]. It grows on the European continent, and it is used as an antiseptic in local regions of Portugal [122].
In phytochemical analysis, Thymus pulegioides was found to have a high flavonoid content, tannins, and hydroxycinnamic acids. The T. pulegioides oil, in one analysiss, was characterized by the presence of high amounts of thymol and carvacrol [122]. The dose-dependent scavenging effect and the chelating activity of T. pulegioides are moderate to high, with an increased acetylcholinesterase inhibition [114]. A study in Italy places T. pulegioides among the first medicinal plants in traditional medicine and the second most relevant in respiratory pathologies usage [123].
It has an important antioxidant role [124], but as an anti-inflammatory agent, it elicits cell-type-dependent response [125]. Another consideration that increases the medicinal importance of T. pulegioides is that it has demonstrated considerable antifungal capacities [122]; however, more data are required to quantify its effect in pain modulation.
3.5. Satureja Genus
Satureja genus consists of aromatic plants of the Lamiaceae family that are related to rosemary and thyme. It is native to the North African region, southern and southeastern European regions, and the Middle East and Central Asian parts of the globe. A few species found on the American continent were formerly included in Satureja genus but were thereafter moved to other genera.
3.5.1. Satureja hortensis
Satureja hortensis L., also known as summer savory (culinary herbs), is an annual aromatic plant with origin in the Mediterranean region and wide distribution in the Mediterranean Sea region, Black Sea, Central and Southern Europe, Asia Minor, and Siberia, but nowadays cultivated worldwide [126]. The floral parts and leaves from the plant are used as aromatic spice. It is also used in medicinal purposes as decoctions, plasters, and compresses.
The main constituents of the plant were carvacrol, γ-terpinene, p-cymene, α-terpinene, and myrcene. The only notable sesquiterpene is β-bisabolene [126].
Regarding the biological activity, extracts from S. hortensis are covering a large spectrum of pathological conditions [127–132]: antimicrobial activity, antioxidant activity, cytotoxic activity, insecticidal activity, fumigant toxicity, insect repellant activity, antinociceptive and analgesic activity, antileishmanial activity, genotoxic activity, anti-inflammatory activity, effects on immune system, effects on productive performance, acaricidal activity, antidiarrheal activity, relaxant effect (antispasmoidal activity), antigenotoxic activity, antihepatoma activity, contact toxicity and persistence, effect on vitality and healthiness of cereals, molluscicidal activity, larvicidal activity, antihelmintic activity, inhibition on blood platelet adhesion, aggregation and secretion, effect on rhinosinusitis, amyloid beta protein aggregation inhibitory activity, and matrix metalloproteinase inhibitory activity.
Concerning the analgesic activity, S. hortensis extracts (hydroalcoholic extract, polyphenolic fraction, and essential oil of the aerial parts of the herb) were evaluated by use of tail flick, formalin, and acetic acid-induced writhing tests in mice. Results showed that, in the light tail flick test, neither the essential oil nor the extracts could exert any significant effect. The hydroalcoholic extract (2000 mg/kg, p.o.) and the essential oil (200 mg/kg, p.o.) inhibited the mice writhing responses caused by acetic acid. In the formalin test, hydroalcoholic extract (500–2000 mg/kg, p.o.), polyphenolic fraction (250–1000 mg/kg, p.o.), and the essential oil (50–200 mg/kg, p.o.) showed analgesic activity, and pretreatment with naloxone (1 mg/kg, i.p.) or caffeine (20 mg/kg, i.p.) failed to reverse this antinociceptive activity. Authors suggested that antinociceptive effect could be due to the involvement of opioid and adenosine receptors in the antinociception mediation [133].
3.6. Stachys Genus
Stachys genus is one of the largest genera in the flowering plant family of Lamiaceae. Estimates of the number of species in the genus are ranging between 300 and about 450.
3.6.1. Stachys lavandulifolia
Stachys lavandulifolia Vahl., a type of Stachys, also known as mountain tea (Chay-e-Kouhi) has been distributed in a variety of climatic conditions including diverse areas of Europe, Asia, Africa, and Australia. The plant is known as Chay-e-kouhi in Persian, whereas in English it is called Betony. Also, its common names include heal-all, self-heal, woundwort, betony, lamb's ears, and hedge nettle [134].
Based on recent studies on this herb, 79 compounds were identified, representing 98.2% of the essential oil, in which the major components were germacrene-D (13.2%), β-phellandrene (12.7%), β-pinene (10.2%), myrcene (9.4%), α-pinene (8.4%), and Z-β-ocimene (5.8%). In another study, spathulenol (35.0%) and caryophyllene oxide (25.6%) were the main components of the oil [135]. Another study revealed the existence of α-thujone (0.3%–32.3%), Δ-cadinene (11.6%) and 1,4-methano-1H-indene (10.1%) [136].
The aqueous extract obtained from the aerial parts of S. lavandulifolia is used in antipyretic, anti-inflammatory, spasmolytic, sedative, and hypnotic treatment [137]. Also, this plant has antibacterial, antioxidant, anxiolytic, analgesic, and wound-healing effects. Decoctions or infusions of Stachys are applied as tonics to treat skin or taken internally for stomach disorders [138].
Some other biological activities of S. lavandulifolia were signaled, and the main of those being possibility of abortion depending on the dosage in animals, useful in controlling premenstrual syndrome (PMS) and primary dysmenorrhea symptoms, helps in strengthening stomach and preventing gastric ulcers caused by alcohol consumption, and useful in treating Leishmania major. Being useful to treat fatigue, nausea, and vomiting associated with primary dysmenorrhea, it could be a potentially effective treatment for dysmenorrhea, particularly because of its antipyretic and spasmolytic effects. As an undesired effect, it gives rise to failure in fetus survival and, consequently, abortion. Its action on insomnia is approved. It is also known for its antidepressive and appetite-stimulating effects [139, 140].
For the evaluation of the analgesic effect, hydroalcoholic, polyphenolic, and boiled extracts of the aerial parts from S. lavandulifolia were prepared, and their analgesic effects were studied in mice using formalin, acetic acid-induced writhing, and light tail flick tests. Results showed that all the tested extracts were able to reduce the abdominal constrictions in acetic acid-induced writhing test. These extracts also significantly (P < 0.001) suppressed both phases of the formalin test. In the light tail flick test, none of the extracts showed analgesic activity [141].
In another study regarding antinociceptive effects of S. lavandulifolia extracts, the implication of essential oil (EOSl) and (−)-α-bisabolol (BIS), its main compound, was studied in algogen-induced orofacial nociceptive behavior in mice. Authors have shown that the treatment with EOS1 and BIS has significantly reduced pain in different orofacial pain tests on mice, but BIS proved to be more effective, significantly reducing nociceptive behavior in all tests including both phases of the formalin test [142].
3.6.2. Stachys officinalis (Synonym Betonica officinalis)
It is commonly known as wood betony, purple betony, woundwort, or Bishop's wort; it is a perennial herb found in dry grassland, meadows, and open woods in most of Europe, western Asia, North and South America, Africa, and tropical regions. For centuries, Betonica officinalis herbs (roots and aerial parts) were used in traditional folk medicine for numerous purposes, either internally as tea or externally as compresses or baths. The beneficial properties include anti-inflammatory [143], antibacterial [144], antifungal, antioxidant [145, 146], and hypotensive activity [147]. Important analgesic effects and implications in the treatment of respiratory tract, gastrointestinal tract, nervous and cardiac systems, and skin and gynecological disorders were also observed. Also, a variety of Betonica species are used in food industry to improve the taste in preparation of jelly or yogurt, or as seasonings and flavorings [148].
The chemical composition of Betonica officinalis includes polyphenols such as tannins, phenolic acids, flavonoids, alkaloids trigonelline, and stachydrine (a pyrrolidine alkaloid), iridoids, diterpenes, phenylethanoid glycosides, fatty acids, betaine, volatile oils, and choline [149, 150]. According to the literature data, phenylethanoid glycosides, triterpenoids, and flavonoids are considered to be the active components responsible for the biological actions of the genus Stachys, but the anti-inflammatory or analgesic effects, or components of it, have not been elucidated completely so far.
3.6.3. Stachys inflata
A hydroalcoholic extract of Stachys inflata Benth., one of the Stachys species from Iran, induced antinociception and anti-inflammatory effects in two well-characterized inflammatory models in rats: carrageenan-induced paw edema and formalin-induced paw licking [151]. Intraperitoneal injection of the hydroalcoholic extract of the aerial parts from nonflowering stems of S. inflata, 60 min before induction of inflammation, was capable of attenuating both early and delayed phases of carrageenan-induced inflammation with a dose-related inhibition over the dose range of 50–200 mg/kg. Compared to a standard nonsteroidal anti-inflammatory drug, indomethacin, the hydroalcoholic extract of S. inflata inhibited the inflammation more effectively than indomethacin. Moreover, all three doses of the extract significantly inhibited the pain associated with the second phase (inflammatory component) of the formalin test, but with no effect against the first phase (0–5 min).
The obtained data suggest that the anti-inflammatory activity of hydroalcoholic extract of S. inflata may be related to the inhibition of the release or synthesis of cyclooxygenase products and polymorphonuclear leukocytes accumulation determined by myeloperoxidase activity. The effects of S. inflata extracts (200 mg/kg) on inflammation and myeloperoxidase activity were confirmed by histological examination where the extract considerably reduced the morphological injury and neutrophil infiltration in a carrageenan-induced model of local inflammation.
The results presented in this study are taken as the basis for further investigation on the exact mode of action of individual constituents of the extract. Several components quantified in Stachys extracts demonstrated in vivo anti-inflammatory and antinociceptive activity in carrageenan-induced hind paw edema and p-benzoquinone-induced abdominal constriction tests [100].
3.6.4. Stachys byzantina
Khanavi et al. [152] proved that acetone and methanol extracts of S. byzantina K. Koch, a species of Stachys, native to Turkey, Armenia, and Iran, play a significant role in the inhibition of pain and inflammatory processes by using two inflammatory models, namely, formalin test and carrageenan-induced paw edema.
Dried and finely powdered aerial parts were extracted with acetone at room temperature for 2 weeks in order to isolate and identify an acyclic diterpene ester (phytyl nonadecanoate), two normal alkanes (tritriacontane and hentriacontane), one fatty acid (oleic acid), and two sterols (stigmasterol and lawsaritol). Structures were established by conventional methods of analysis and confirmed by 1H, 13C NMR, and mass spectral analysis. All three doses of acetone/methanol extracts of Stachys byzantina (50, 100, and 200 mg/kg), administered by intraperitoneal injections, significantly inhibited the pain associated with the second phase (inflammatory component) of the formalin test, and the effect of the low dose was predominant. Compared to indomethacin (high dose of 5 mg/kg) as a nonsteroidal anti-inflammatory drug, the extracts decreased licking response in the late phase significantly, with the maximum inhibitory response obtained with 50 mg/kg of the extract.
The authors assumed that the analgesic effects of the extracts are probably mediated by interactions with inflammatory mediators (arachidonic acid metabolites), since the antinociceptive activities were observed in late phase (20 min after formalin injection). In the carrageenan-induced paw edema, both extracts revealed dose-related inhibitory effects, in both early and delayed phases, over the dose range 50–200 mg/kg, similar to a high dose of indomethacin (5 mg/kg). The present data demonstrated that the anti-inflammatory activity of acetone and methanol extracts of S. byzantina is probably related to the inhibition of the synthesis or release of COX2 products.
3.7. Glechoma Genus
Glechoma genus is composed of flowering plants in the mint family first described in 1753. This genus is distributed in both northern Asia and Europe. In Asia, however, it is most predominantly seen in China, and it is closely related to Marmoritis.
3.7.1. Glechoma hederacea
Glechoma hederacea L., more commonly known as ground ivy, is a perennial herb with creeping stem that can be found throughout Northern Europe and the neighboring regions of Asia. The aerial parts of the plant (consumed as salad or tea) have been used in both Asian and European traditional medicine as a remedy for several digestive, pulmonary, skeletal, and inflammatory conditions [153]. Active components include several polyphenols such as chlorogenic acid, caffeic acid, ferulic acid, rutin, genistin, rosmarinic acid, quercetin, or genistein [153] and triterpenoids such as ursolic acid and oleanoic acid [154, 155]. Additionally, studies report that G. hederacea leaves contain polyunsaturated fatty acids [156] and a type of insecticidal lectin called Gleheda [157].
Current preclinical data indicate that G. hederacea has several pharmacological effects. As such, hot water extracts of ground ivy have been shown to exhibit antibacterial, anticancer, insecticidal, and platelet-stimulating activity [157, 158]. Currently, there are no studies specifically addressing ground ivy's effect on pain. However, existing data point out that the plant has potent anti-inflammatory effects. An in vitro study revealed that incubating activated macrophages with a ground ivy decoction (3 h in boiling distilled water) led to a significant decrease in nitric oxide production. Furthermore, the authors noted that the expression of some inflammatory cytokines such as IL-12p70 and TNFα was significantly decreased [159]. Similarly, Kim et al. demonstrated that several compounds found in G. hederacea inhibit NF-κB production [154]. In vivo, hot water G. hederacea extract was shown to have an anti-inflammatory effect in a rat model of hepatic inflammation: rats that received 0.5 g/kg G. hederacea extract daily for four weeks were shown to have significantly lower levels of inflammatory cell infiltration/activation in the liver [153]. Additionally, several inflammatory markers, such as NF-κB, TNF-α, IL-1β, and IL-6, were decreased in these animals when compared with the control group.
Other possible mechanisms that make ground ivy a potential candidate as coanalgesic include its effects on extracellular calcium (Ca) levels [160] and on oxidation. Purified ethyl acetate extracts of ground ivy showed a strong antioxidant activity when used as a food additive in two different types of food (pork lard and sunflower oil) [161].
There are no reported side effects following G. hederacea administration. However, one in vitro study showed that G. hederacea ethanol extract concentrations exceeding 100 µg/dl are cytotoxic [160], and several studies now focus on the plant's ability to kill different types of cancer cells [162]. Due to its ability to target and kill cancerous cells, those extracts should also be included in preclinical screenings addressing pediatric cancerous cells (e.g., insulinomas being one of the most frequently encountered types of neuroendocrine pancreatic tumors [163]).
3.8. Scutellaria Genus
Scutellaria genus includes over 350 species, many of which have been used in traditional medicine and are documented to have medical proprieties.
3.8.1. Scutellaria lateriflora
Scutellaria lateriflora L., also known as American skullcap, is a member of Scutellaria genus and is native to North America and is best known for its sedative and anxiolytic effects. The plant is still widely used by herbal medicine practitioners for insomnia, nervous anorexia, headaches, depression, panic attacks, and fibromyalgia [164, 165]. Most often, it is prescribed as a tincture, although teas and tablets are also commercially available, with wide variability depending on the manufacturer and species of Scutellaria used [166]. Although rare, possible side effects of chronic treatment include drowsiness, mild digestive upset, and vivid dreaming [165].
The first clinical study assessing skullcap's effect on mood was performed on nineteen patients and had positive results [167]. In 2014, Brock et al. published the results of a larger randomized controlled clinical trial designed to assess the effect of a S. lateriflora extract on mood in healthy volunteers. Results indicated that global mood was significantly enhanced in individuals who received 350 mg of plant extract for two weeks without negative effects on energy and cognition [164]. Taking into account the fact that anxiety is a well-known enhancer of pain perception [168], S. lateriflora extracts could have clinical value as co-analgesics. Additionally, ethanolic and aqueous S. lateriflora extracts have been shown to have potent antioxidant effects, reducing ROS and lipid peroxides in tissue homogenates [169], most likely due to the flavonoids it contains.
S. lateriflora contains several active compounds such as baicalin (40 mg/g in a 50% EtOH extract), baicalein (33 mg/g in a 95% EtOH), GABA (1.6 mg/g in EtOH and H2O extracts), and glutamine (31 mg/g in H2O extract) [170]. Other flavonoids found in S. lateriflora include wogonin, oroxylin A, genkwanin, hesperetin, quercetin, rutin, naringenin, chrysin, and daidzein [167]. While its anxiolytic effects are probably related to some of the flavonoids that bind to one of the serotonin receptors [171], S. lateriflora's antioxidant activity is most likely due to its content of baicalein and its glucuronide, baicalin.
Baicalein can be extracted from S. lateriflora through alkali solution and acid isolation methods; for a high-purity extract (99.35%), hydrolysis of baicalin and column chromatography purification can be used [172]. As an isolated compound, baicalein has shown not only antioxidant activity but also significant anti-inflammatory activity in several in vitro and in vivo models, which has made it an interesting drug to be screened as an analgesic.
One study used several extracts from a plant of the Scutellaria genus and found that baicalein has a significant analgesic effect in the carrageenan-induced rat paw inflammatory model [173]. Similarly, baicalein was found to significantly decrease pain-related behavior and c-fos expression (a surrogate marker for pain intensity) in the spinal dorsal horn of animals exposed to painful stimuli [174]. A combination of baicalin and catechins was assessed in three widely used animal pain models and was found to have analgesic effects in visceral, nociceptive, and inflammatory pain [175].
Baicalin has also shown some efficacy in neuropathic pain: an in vivo study on spinal nerve ligation rats showed that tactile allodynia and thermal hyperalgesia were reversed by intrathecal baicalin administration. Additionally, baicalin significantly enhanced the effect of morphine in neuropathic animals, most likely by suppressing histone deacetylase 1 expression in the spinal dorsal horn [176]. The compound was also shown to be effective in cancer-induced bone pain: both intrathecal and oral baicalin administration reduced cytokine expression and inhibited pain-related signals as assessed by behavioral and biochemical tests [177, 178] in an animal model.
This compound most likely exerts its analgesic effects through modulating the inflammatory process. Baicalein's anti-inflammatory activity can partly be explained by its inhibitory effects on lipoxygenases—enzymes that play a key role in leukotriene and lipoxin synthesis, thus initiating the inflammatory response. Deschamps et al. found that baicalein inhibits both human platelet 12-lipoxygenase and human reticulocyte 15-lipoxygenase-1 [179]. Additionally, Hsieh et al. showed that baicalein inhibits IL-1β and TNF-α through modulation of the NK-κB pathway [180] while other authors found that it inhibits protein expression of inducible nitric oxide synthase [181] and COX2 gene expression [182]. Pretreatment with baicalein increased the concentration of antioxidant enzymes such as SOD, catalase, and GSH in an in vivo model of myocardial ischemic injury [183] and protected cells against lipid membrane peroxidation [184]. However, it is very likely that, taking into account the fact that baicalein is effective also in noninflammatory types of pain, it has other analgesic mechanisms as well. One hypothesis states that baicalein binds to the GABAA receptor, which has a modulatory effect on pain because GABA is the main inhibitory neurotransmitter. When directly injected into the central nervous system, baicalein has strong sedative and anxiolytic effects due to GABA binding [185]. Also, a recently published article indicated that through GABA modulation, baicalin could be used in orofacial pain modulation [186]. Another study also suggested that baicalein modulates both intracellular and extracellular calcium levels [187], which may play a role in cell signaling and pain transmission.
3.9. Ocimum Genus
Ocimum genus species are amongst the best-known medicinal plants, with historical reports of their antimicrobial, immunomodulatory, antistress, anti-inflammatory, antiulcer, antidiabetic, hepatoprotective, chemoprotective, antihyperlipidemic, cardioprotective, antioxidant, antitussive, radioprotective, memory enhancing, antiarthritic, antifertility, antihypertensive, anticoagulant, anticataract, anthelmintic, and antinociceptive activity [188]. As such, several members of the genus such as Ocimum sanctum, Ocimum gratissimum, or Ocimum micranthum have played a significant part in different traditional medicines and are currently considered as potential sources for innovative drugs.
3.9.1. Ocimum sanctum
Ocimum sanctum Linn., also known as tulsi, is an indigenous plant commonly found in India [189]. In Ayurvedic medicine, it is used in the form of a fresh leaf extract or a decoction with hot water to alleviate muscular pain, joint pain, and severe headache [190]. It contains (−)-linalool (30–40%), eugenol (8–30%), and methyl chavicol (15–27%). Minor constituents are (+)-delta-cadinene, 3-carene, α-humulene, citral, and (−)-trans-caryophyllene [191]. In recent years, the interest for evaluating the potential benefits of O. sanctum extracts in several conditions has significantly increased, especially in the anticancer, antimicrobial, and neurobiology fields. A double-blind clinical trial assessed the effects of oral ethanolic extract of O. sanctum on healthy volunteers and concluded that the drug has immunomodulatory effects and can be given for a period of four weeks without any significant side effects [192]. Although less numerous, there are some studies that have assessed the effect of O. sanctum extracts on different types of pain, most often inflammatory or neuropathic.
In vitro, O. sanctum leaf extracts exhibited significant anti-inflammatory effects in LPS-stimulated monocytic cells, reducing cytokine production and decreasing TNF-α secretion [193]. Different types of dried leaf extracts were also shown to be effective in reducing carrageenan-induced and leukotriene-induced paw edema [194]. More recently, a triple-blind randomized clinical study compared an ethanolic extract of O. sanctum with chlorhexidine mouthwash in regards to their effect on dental plaque and gingival inflammation and found that the two are equivalent. Additionally, the O. sanctum extract was better tolerated and had no side effects [195].
Regarding its effect on other pain models, there are several studies that have demonstrated that O. sanctum extracts alleviate neuropathic pain. The method of preparation was similar in most study designs: dried tulsi leaves were reduced to coarse powder and then extracted with a mixture of methanol and water (3 : 1) [189, 190] in order to obtain an oral preparation. 50 mg/kg b.w. of O. sanctum extract attenuated sciatic nerve transection-induced axonal degeneration, reduction of nociceptive threshold, and motor in-coordination [190]. Kaur et al. orally administered 100 mg/kg b.w. or 200 mg/kg b.w. of O. sanctum to rats that underwent chronic constriction injury in the sciatic nerve and found that the extract alleviated cold-induced hyperalgesia, mechanical allodynia, and paw-heat hyperalgesia [196]. In another study, a 200 mg/kg b.w. dose of the extract was used, and the authors concluded that it is effective in preventing vincristine-induced neuropathic pain in rats [189]. The same dose of O. sanctum extract was administered in rats with surgically induced focal cerebral ischemia/reperfusion injury and was shown to reduce both neurological deficit and oxidative damage [197].
3.9.2. Ocimum gratissimum
Ocimum gratissimum L. is widely found in several geographical regions in South America and Africa [198, 199] and still used as a medicinal plant with analgesic activity [198]. It contains several proanthocyanidins, which have been shown to exhibit significant antioxidant activity, and tannins, saponins, steroids, alkaloids, terpenoids, flavonoids, phenols, and cardiac glycosides [200]. O. gratissimum essential oil was orally administered to mice with chronic constriction injury and effectively alleviated neuropathic pain most likely due to eugenol's antihyperalgesic activity [199]. The same group demonstrated the efficacy of the aforementioned essential oil for increasing paw withdrawal latency in the hot-plate test and for decreasing formalin-induced hind paw inflammation and pain-evoked behaviors [201]. Another team used the essential oil of O. gratissimum in a model of visceral pain (the writhing test) and in the formalin test with equally favorable results [202]. Similar analgesic activity was demonstrated by O. gratissimum aqueous and hydroalcoholic extracts in two animal pain models: the acetic acid writhing test and the hot-plate test [198], indicating that it is efficient in nociceptive, neuropathic and inflammatory pain.
trans-Caryophyllene, a sesquiterpene from O. gratissimum, was shown to have dose-dependent analgesic effects in several experimental models of acute and chronic pain such as the formalin test, chronic constriction injury, and the hot-plate test. The authors evaluated the potential mechanisms responsible for the substance's properties and found that the analgesic effect was reversed by several types of antagonists [203], thus indicating the involvement of both the opioid and endocannabinoid system [204].
3.9.3. Ocimum micranthum
Ocimum micranthum Willd. or Ocimum campechianum Mill., more commonly known as Amazonian or Peruvian basil, has similar anti-inflammatory and antianalgesic effects in several animal models of pain, although it has been reported as less effective on the hot-plate test [205]. The difference in efficacy between plants is most likely due to their different compositions that additionally vary according to the geographical area. While some authors believe that the saponins these plants contain are responsible for their effect on pain [189], others have suggested that the volatile oil eugenol is in fact the most potent antioxidant and anti-inflammatory compound [197].
3.10. Lamium Genus
Lamium genus contains almost 40 herbaceous plants, some of which have been used as remedies for various conditions such as trauma, putrescence, paralysis, leucorrhoea, hypertension, or inflammation [206]. The Lamium species contain different concentrations of iridoids, flavonoids, phenylpropanoids, benzoxazinoids, and essential oil [207], which vary according to species and geographical area of cultivation. Although widely used in traditional medicine, there are only few studies that investigate the potential analgesic effects of this genus. One study screened several plants of the Lamium genus and concluded that Lamium purpureum has potent antioxidant effects, being able to rapidly scavenge free radicals in several in vitro assays [150].
Another screening study assessed potential anti-inflammatory and antinociceptive effects of different Lamium species and concluded that Lamium garganicum L. and L. purpureum L. extracts are as effective as indomethacin, a reference anti-inflammatory drug. In this study, all extracts were prepared by methanolic extraction of air-dried and powdered aerial plant parts (25 g plant in 250 mL methanol), which was then concentrated to dryness, suspended in water, partitioned, and lyophilized. The study showed that 200 mg/kg body weight of L. garganicum or L. purpureum methanolic extracts alleviate inflammatory pain in a model of ear edema and in carrageenan-induced and prostaglandin E2-induced hind paw edema [206].
3.11. Teucrium Genus
Teucrium genus contains several mostly perennial plants commonly referred to as germanders.
3.11.1. Teucrium polium
Teucrium polium L. is a perennial wild-growing plant, widely spread in several regions such as South-Western Asia, Europe, and North Africa [208], and has been used in traditional medicine for the treatment of inflammations, rheumatism, diabetes, and ulcers. Two major components of the dried leaf plant extract are flavons and flavonoids [209]; the essential oil contains α-pinene (25.769%) and myrcene (12.507), and the methanolic extract contains sinapic acid (15.553 mg/g) and eugenol (6.805 mg/g) [210]. A preclinical study showed that intraperitoneal administration of 100 or 200 mg/kg b.w. per day for two weeks reduced pain-related behavior in the diabetic rat formalin test [211]. A larger dose of 500 mg/kg body weight of ethanolic extract of T. polium inhibited carrageenan-induced inflammation and reduced granuloma formation [212]. Another study compared the effect of morphine and T. polium extract on the tail flick latency and found the two to be comparable in efficacy [213]. Both the total extract and the essential oil of the plant exhibited analgesic effects on the acetic acid-induced writhing test, thus suggesting it might be effective in visceral pain [214]. Subsequently, a triple-blind, randomized, clinical trial was designed in order to assess the plant's effects on dysmenorrhea. Seventy female students were randomly assigned to receive either T. polium powder every six hours for the first three days of their menstrual cycle or 250 mg mefenamic acid. Study results indicated that the two are equally effective, thus concluding that T. polium is effective in this type of pain [209].
3.11.2. Teucrium hyrcanicum
Teucrium hyrcanicum L., also known as “Purple Tails” is a plant native to Iran, which has been also shown to exhibit analgesic and anti-inflammatory activities in carrageenan-induced paw edema, acetic acid-induced writhing, tail flick, and formalin pain tests [215]. A recent study used a methanolic extract of dried aerial parts of T. hycranicum and observed that the high flavonoid content of the plant has significant antioxidant effects [216].
3.11.3. Teucrium chamaedrys
Teucrium chamaedrys L., also known as “The wall germander,” is an evergreen subshrub native to the Mediterranean region of Europe and North Africa, and to the Middle East. It has been used in traditional English medicine as part of the Portland Powder for treating rheumatism and gout [217]. A preclinical study identified teucrioside as the main active ingredient of the plant and concluded that it is effective in inhibiting calcineurin, thus potentially playing a role in reducing inflammatory states [218].
3.12. Hyptis Genus
Hyptis genus, also known in Brazil as “sambacaitá” or “canudinho,” is a genus of aromatic plants in the Lamiaceae family [219]. The genus Hyptis consists of approximately 400 species distributed from the southern United States to Argentina [220] and exhibits a major morphological diversity in the Brazilian Cerrado [221].
3.12.1. Hyptis pectinata
Hyptis pectinata L. Poit. is present very common in gardens, and it is frequently used as tea (decoctions or infusions) and mouthwash to treat inflammation due to being considered a natural antiphlogistic. In Brazilian folk medicine, the infusion of the fresh leaves is used to treat inflammations, bacterial infections, pain, gastrointestinal disorders, skin infections, nasal congestion, fever, cramps, inflammation, orofacial painful conditions and wound healing [222], fungal infections, and HIV.
Also, the plant has cytotoxicity and insecticide properties [223]. H. pectinata has an important neurogenic and inflammatory orofacial antinociceptive effects, without interference in the motor performance. The mechanism is currently unknown but seems to be related to vanilloid and glutamate receptors. The opioid system seems unlikely to participate in the antinociception caused by the extract [224]. The local application of dental gel based on H. pectinata has anti-inflammatory effect and also prevents alveolar bone resorption and weight loss in animals with periodontitis [223]. The healing effect of H. pectinata suggests that this plant may have antileishmanial action [219].
The aqueous extract of H. pectinata possesses antiedematogenic properties in the carrageenan-induced paw edema model. The association of the aqueous extract of H. pectinata leaves at 200 mg/kg with intraoperative laser therapy can stimulate liver regeneration and cause a reduction in liver mitochondrial respiratory function without altering its phosphorylative activity [225].
The antinociceptive effects of H. pectinata can be seen in the volatile oil [226]. The major constituents of oil are 1,8-cineole (12.46%), α-pinene (20.51%), and β-pinene (13.54%). β-Pinene may be considered a partial agonist of μ-opioid receptors [227]. Franco et al. [228] suggested that the essential oils have both peripheral and central analgesic actions without opioid system influence, although the central activity was more discrete. GC-MS analysis showed that β-caryophyllene (40.90%) and caryophyllene oxides (30.05%) were the main compounds present in the oil.
In 2011, Raymundo published the results that H. pectinata essential oil shows peripheral and central antinociceptive effects, likely mediated by opioid and cholinergic receptors, and anti-inflammatory activity through the inhibition of nitric oxide and PGE2 production [229]. The involvement of the opioid system in the antinociceptive activity of H. pectinata essential oil was evaluated in the hot-plate model by pretreating mice with an opioid antagonist, naloxone. The results suggest that naloxone reversed the antinociceptive activity of the essential oil. The antinociceptive effects were observed in other tests like acetic acid or hot-plate [230].
3.13. Melissa Genus
Melissa genus contains the perennial herbs from the Lamiaceae family, native from Europe and Asia but cultivated and naturalized in many other places.
3.13.1. Melissa officinalis
Melissa officinalis L., also known as lemon balm, English balm, garden balm, balm mint, common balm, melissa, sweet balm, and heart”s delight, is an aromatic herb from the mint family (Lamiaceae) that includes two subspecies: Melissa officinalis L. subsp. officinalis, the common cultivated lemon balm, and Melissa officinalis L. subsp. altissima, naturalized in New Zealand and known as bush balm. The first information about the usage of the plant was found in Greece, 2000 years ago. In 2007, Khare [231] published the results that the plant has antidepressant, antispasmodic, antihistaminic, and antiviral properties and can be used in cases of anxiety, neurosis and nervous excitability, palpitation and headache, and also in hyperthyroidism.
The known major components of lemon balm are hydroxycinnamic acid derivatives, particularly rosmarinic acid, caffeic acids, chlorogenic acid, and metrilic acid [232, 233], tannins [234], flavonoids, including luteolin, luteolin 7-O-beta-D-glucopyranoside, apigenin 7-O-beta-D-glucopyranoside, and luteolin 3′-O-beta-D-glucuronopyranoside [235, 236], monoterpene glycosides [237], sesquiterpenes, including β-caryophyllene and germacrene [237], triterpenes [238], and volatile oils, including citronellal, citral a (geranial), citral b (neral), methyl citronellate, ocimene, citronellol, geraniol, nerol, β-caryophyllene, β-caryophyllene oxide, linalool, and etheric oil [239].
M. officinalis exhibit antiviral effects against Newcastle disease virus, Semliki forest virus, influenza virus, myxoviruses, vaccinia [240], and herpes simplex virus types 1 and 2 [241], HIV-1 [242]. The antiviral effects are mediated by tannin and polyphenol constituents, rosmarinic, caffeic, and ferulic acids [240].
M. officinalis has antibacterial effects and can be used to treat oropharyngeal diseases produced by anaerobic and facultative aerobic periodontal bacteria like Porphyromonas gingivalis, Prevotella spp., Fusobacterium nucleatum, Capnocytophaga gingivalis, Veillonella parvula, Eikenella corrodens, Peptostreptococcus micros, and Actinomyces odontolyticus [243].
Englberger suggests that rosmarinic acid has anti-inflammatory effects because it reduces paw edema induced by cobra venom factor in rats and inhibit passive cutaneous anaphylaxis in rats at doses of 1–100 mg/kg by mouth. The same author says that rosmarinic acid has antithrombotic effects because it inhibits the classical pathway convertase and the alternative pathway convertase [244].
M. officinalis has antithyroid effects (inhibit the binding of bovine TSH to human thyroid plasma membranes and adenylate cyclase, inhibit the extrathyroidal enzymatic T4-5′-deiodination to both T3-and T4-5′-deiodination) [245], spasmolytic effects (observed only in in vitro studies on isolated duodenum of rat) [246], sedative effects (dose-dependent sedation, inducing sleep and potentiating subhypnotic and hypnotic doses of pentobarbital) [246], and cardiovascular effects (significant reduction in the cardiac rate by the stimulation of cardiac muscarinic receptors) [247, 248].
3.14. Origanum Genus
Origanum is a genus of herbaceous perennials and subshrubs in the Lamiaceae family, native to Europe, North Africa, and much of temperate Asia and can be found in open or mountainous environments. A few species also naturalized in North America and other regions. The plants have strongly aromatic leaves and abundant tubular flowers with long-lasting coloured bracts. The genus includes Origanum vulgare L. or common marjoram and Origanum majorana L. or sweet marjoram, the two species of Origanum that can be used with medicinal purposes.
3.14.1. Origanum vulgare
O. vulgare is an aromatic, woody-based perennial, native to the stony slopes and rocky mountain areas at a wide range of altitudes in the Mediterranean area (Portugal and Andalusia), Europe (including the British Isles), and south and central Asia [249].
The difference between these two plants is almost indistinguishable (taste aside) to the amateur gardener. In technical terms, the difference between marjoram and oregano is based on the shape of the calyx and not the leaves, how hairy they are, or the growth habit.
There are a lot of information about Origanum. So, Hippocrates used O. majorana as an antiseptic agent. The ancient Greeks consider Origanum as a symbol of love, honour, and happiness. Aristotle declares that Origanum is an antipoison. The people from old Egypt used Origanum to disinfect and preserve food [250].
The major compound of Origanum oil is terpinen-4-ol (26%), cis-sabinene (13.3%), o-cymene (9.3%), g-terpinen (5.8%), trans-sabinene (5.7%), p-menth-1-en-8-ol (5.1%), b-thujene (4.9%), and α-terpinen (3.5%). The extracts obtained by supercritical CO2 presented higher concentrations of oxygenated monoterpenes, without significant differences between fractions 1 and 2. A study from Iran shows that the composition of essential oils in O. vulgare was dominant in β-caryophyllene, germacrene D, and cis-sabinene hydrate [251]. Another study from Italy shows that the main components of essential oil in the O. vulgare ssp. vulgare were β-caryophyllene, thymol, terpinen-4-ol, and p-cymene [252]. Biochemical compounds of O. majorana are the essential oil and tannins. The difference between the essential oil obtained from O. vulgare and O. majorana is in quantity (0.67% and 1.5%) [253]. The maximum quantity was obtained in the full flowering stage. The major component is germacrene D for O. vulgare and terpinen-4-ol for O. majorana [254].
In the folk medicine, Origanum was used to treat several illnesses such as spasmodic, antimicrobial, digestive, expectorant, and aromatic for the whooping and convulsive coughs [255, 256]. O. vulgare (oregano) and O. majorana (marjoram) inhibit the growth of the bacteria and fungus (inhibited the growth of Candida albicans) [257] and the synthesis of the microbial metabolites [258, 259]. The leaves of Origanum were used to cure diabetes, insomnia, catarrh, and asthma [260]. O. majorana has stimulatory properties and vasodilatatory activity [261]. By acting also on cardiovascular system and being used as an adjuvant for diabetes control, Origanum subsp. could both prevent and treat more complex diseases associative developed as: atrial fibrillation development [262–265].
3.15. Ziziphora Genus
Ziziphora genus is an aromatic herb of the Lamiaceae family, native to Ukraine, Russia, Siberia, Central Asia, Xinjiang, Afghanistan, Irancaner, Turkey, and Middle East. Ziziphora species were used as culinary herb in Iran [266].
In traditional medicine, Ziziphora is used as infusion, decoction, and maceration for various purposes such as sedative, stomach tonic, heart disorders, common cold, inflammation, carminative, diarrhea, expectorant, coughing, antiseptic, migraine, fever, and depression. Moreover, essential oils are used for treating some diseases such as edema, insomnia, lung abscess, tracheitis, hemorrhoids, and hypertension [267]. The antimicrobial activity of the essential oil of Salmonella typhi Vi-positive makes it useful in the treatment of typhoid fever, too. The plant extract can modulate immune response by induction of CD40 expression on DCs and cytokine production and inhibition of T-cell stimulating activity of dendritic cells in high concentration [268].
3.15.1. Ziziphora tenuior
Ziziphora tenuior L. may possess an antidepressant-like effect, and its effect is similar to fluoxetine [269]. The composition of the ethanolic extract of Ziziphora tenuior contains two new flavonoids named as “ziziphorin A and ziziphorin B,” 1-hentetracontanol [270], ursolic acid [271], oleanolic acid (5) [272], β-sitosterol-3-O-β-glucoside [273], and apigenin [274].
The composition of Z. tenuior essential oil may therefore vary with plant genetics, environmental conditions, extraction methods, and geographic origin, including climate, soil, elevation, and topography. The main components of Z. tenuior, which are identified by GC/MS analysis of the extracts, are 53.977% of p-menth-3-en-8-ol, 38.481% of pulegone, and 1.651% of p-menth-3,8-diene. The essential oil also contained smaller percentages of β-pinene; 4aα-, 7α-, and 7aα-nepetalactone; α-thujene; caryophyllene oxide; limonene; E-caryophyllene; and terpinolene. p-Menth-3-en-8-ol and pulegone are the main components of Z. tenuior, and they are responsible for the antimicrobial activities of the essential oil [275]. Essential oils of Z. tenuior aerial parts were characterized by high levels of oxygenated monoterpenes, especially pulegone [276].
3.16. Salvia Genus
Salvia genus belongs to the subfamily Nepetoideae in the Lamiaceae family. In traditional medicine, salvia is one of the oldest medicinal plants used by humans, and it is considered as a universal panacea, used for its antibacterial, antiviral, antioxidative, antimalarial, anti-inflammatory, antidiabetic, cardiovascular, and antitumor effects.
Salvia can be used as infusion, tincture with diuretic, hemostatic, and spasmolytic activities, volatile oils with antiseptic role, and essential oil with antimicrobial effect.
The pharmacological effects of Salvia essential oils are based on the presence of more than 100 active compounds, which can be categorized into monoterpene hydrocarbons, oxygenated monoterpenes, sesquiterpene hydrocarbons, diterpenes, nonisoprenoid compounds and oxygenated sesquiterpenes [277, 278]. The most abundant components are 1,8-cineole, camphor, and a wide variety of thujenes [279].
Analysis made by spectrophotometry and HPLC shows that Salvia officinalis L. has the highest total content (1.785 g %) expressed in gram equivalent caffeic acid, and the highest value for rosmarinic acid (728.68 mg %). Rosmarinic acid is the major component, and it has adstringent, anti-iflammatory, antibacterial, and antiviral activity [280]. S. officinalis is the most valuable species in terms of biologically active principal contents compared to other species studied, followed by Salvia verticillata L. and Salvia glutinosa L. [281].
3.17. Leonurus Genus
Leonurus genus natively grows in the temperate zone of Asia and Europe and was lately adapted in America and Africa. About 24 species of Leonurus have been identified, of which 13 species are spread in China. Plants belonging to Leonurus genus are traditionally used for antigynecological disorder in East Asia, and as sedative in Europe. Chemical investigations of the genus enriched the natural products library and also enlarged the pharmacological applications of this traditional herb [282].
3.17.1. Leonurus cardiaca
Leonurus cardiaca L. is a perennial herb widespread in Europe, throughout the plains and hills, as well as in East Asia to the Himalayas and eastern Siberia, Northern Africa, and North America [283]. The common name of L. cardiaca is motherwort, but it is also known as throw-wort, lion's ear, or lion's tail. For centuries, motherwort extract has been used as a medicinal plant to treat cardiac and vascular diseases, especially tachycardia associated with anxiety, tension, and stress, and also for hypertension to reduce the risk of thrombosis to inhibit artery calcification formation [284].
The ethanolic extract has been prepared by adding 96% ethanol over aerial parts of the plants for 24–36 hours. The supernatant was collected and concentrated by vacuum distillation at a temperature of 50°C. The extract was completely dried under sterile conditions using an autoclave at temperatures lower than 50°C.
In the aerial parts of L. cardiaca, many compounds were identified: terpene compounds: monoterpenes (iridoids: leonuride, ajugoside, galiridoside, and reptoside) [285], diterpenes (of clerodane, furanolabdane, and labdane types) [286], triterpenes (ursolic acid, oleanolic acids, corosolic acid, euscaphic acid, and ilelatifol D) [287], nitrogen-containing compounds (leonurine, stachydrine, and amine choline), and phenylpropanoids (lavandulifolioside), as well as flavonoids, phenolic acids, volatile oils, sterols (β-sitosterol and stigmasterol), and tannins. The phenolic compounds comprise phenylpropanoid glycosides such as lavandulifolioside (arabinoside) [288], phenolic acids such as chlorogenic, rosmarinic, caffeic, p-coumaric, p-hydroxybenzoic, vanillic, and ferulic acids, and phenolic glycoside [289]. The volatile oils mainly contain sesquiterpenes such as germacrene D, epicedrol, β-caryophyllene, α-humulene, and spathulenol and monoterpenes such as α-pinene and dehydro-1,8 cineole [290, 291]. Of these, ursolic acid proved a stronger anti-inflammatory activity than indomethacin and acetylsalicylic acid, and furanolabdane-type diterpenes inhibited abdominal cramps more effectively than the parallel-given aspirin or acetaminophen.
Pharmacological studies have established that L. cardiaca possesses additional antimicrobial [286, 292], antioxidant [289, 293], anti-inflammatory [294, 295], antinociceptive [296], neuroprotective [297], sedative [298], and even anticancer effects [299]. The findings obtained by Rezaee-Asl and coworkers, using the formalin, tail flick, and hot-plate tests, assess that central and peripheral mechanisms are involved in the antinociceptive activity of the motherwort extract. According to the tail flick test of this study, L. cardiaca extract only at the maximum dose (500 mg/kg) could alleviate the pain in all times of tail flick test, whereas the lower doses (125 and 250 mg/kg) reduced only late pain. The formalin test showed that the L. cardiaca extract at a dose of 500 mg/kg and 250 mg/kg was more effective in the first and second phases, suggesting peripheral and central antinociceptive mechanism. The second phase of the formalin test is related to a peripheral inflammatory process [296].
As a conclusion, the studies concerning the analgesic activity of L. cardiaca extract afford a justification for the use of this plant in pain and inflammatory disorders. Further research should be accomplished for the isolation of new phytochemicals and to fully understand the antinociceptive mechanism exhibited by the plant extract.
As undesirable effects, one can mention the potential to increase the risk of bleeding due to its antithrombotic and antiplatelet effects, and the synergistic sedative effect when associated with benzodiazepines, which may result in coma [300].
3.18. Mentha Genus
Mentha is a genus of plants in the Lamiaceae family, with an estimated number of 13 to 18 species, lacking the exact distinction between them [301]. Hybridization between some of the species occurs naturally. The genus has a wide distribution across Europe, Africa, Asia, Australia, and North America. While the Mentha species can be found in many environments, most grow best in wet surroundings and moist soils. The mint stems grow 10–120 cm tall and tend to spread uncontrollably over an indeterminate area; hence, they are sometimes considered invasive. The most common and popular mints for commercial cultivation are Mentha piperita, Mentha spicata, Mentha gracilis, Mentha arvensis, and Mentha suaveolens. Mint was originally used as a medicinal herb to relieve stomachache and chest pains [302].
3.18.1. Mentha piperita
Mentha piperita L. (peppermint) is a hybrid of M. spicata and M. aquatica. This plant was cultivated since the time of ancient Egyptians and established in the Icelandic Pharmacopoeia of the thirteenth century. The list of benefits and uses of peppermint as a folk remedy or alternative medical therapy include biliary maladies, dyspepsia, enteritis, flatulence, gastritis, intestinal colic, and spasms of the bile duct, gallbladder, or gastrointestinal (GI) tract [303].
The phytochemical occurrence in peppermint leaves and oil depends on plant maturity, variety, geographical origin, and processing methods' conditions [304–307]. As fatty acids, there have been found palmitic, linoleic, and linolenic acids [308]. The main components identified in the volatile oil of peppermint are menthol (33–60%), menthone (15–32%), isomenthone (2–8%), 1,8-cineole (eucalyptol) (5–13%), menthyl acetate (2–11%), menthofuran (1–10%), limonene (1–7%), β-myrcene (0.1–1.7%), β-caryophyllene (2–4%), pulegone (0.5–1.6%), and carvone (1%) [304, 309]. The fresh leaves contain 1.2–3.9% (v/w) of essential oil, while the dried leaves is reported to contain only 21% of the original oil [310].
Carotenoids, chlorophylls, α- and γ-tocopherols, and ascorbic acid have also been reported in the plant extract [311]. The major minerals in dried peppermint leaves include K, Ca, Mg, and Na, along with smaller amounts of Fe, Mn, Zn, and Cu and trace amounts of Cr, I, and Se [312]. The polyphenols isolated from peppermint leaves include mainly eriocitrin and rosmarinic acid, luteolin 7-O-rutinoside, and hesperidin [313, 314].
The extraction of essential oils has been approached through different techniques, of which hydrodistillation is still the most common to achieve volatile oils from medicinal plants, including Mentha [315]. In order to diminish the extraction time and for higher extraction yields along with an increased quality extracts, a number of extraction procedures have also been implemented, such as microwave-assisted extraction, pressurized solvent extraction, supercritical fluid extraction, and ultrasound-assisted extraction [316–319].
In vitro and in vivo pharmacological studies have proved multiple therapeutic effects, which are mentioned as follows: antioxidant capacity (radical scavenging capacity being higher than that of M. aquatica or M. longifolia) [46, 320], antitumor activity on different cell lines [321, 322], antiallergenic activity [323, 324], antiviral activity with significant results on herpes simplex viruses (HSV-1 and HSV-2) and against human immunodeficiency virus-1 (HIV-1) [242, 325–327], antibacterial activity against different bacterial strains, including Gram-positive cocci and rods and Gram-negative rods (e.g., S. aureus, Salmonella enteritidis, Shigella sonnei, some strains of E. coli, Heli cobacter pylori, Haemophilus influenzae, Streptococcus pneumoniae, Streptococcus pyogenes, and many other pathogens) [328–331], modulatory effects on hepatic and renal functions [332–334], nervous system actions as analgesic and local anesthetic, and anti-inflammatory actions [335, 336].
The antinociceptive activity of M. piperita aqueous extract has been investigated by Yousef A. Taher using in vivo tests on mice [336]. According to these studies, the plant extract showed inhibition of acetic acid-induced abdominal constrictions in mice at both 200 and 400 mg/kg doses. The hot-plate test has shown that administration of M. piperita aqueous extract (using the same abovementioned doses) caused a significant latency of the response to thermal stimulation. The carrageenan-induced paw edema test disclosed an increase in paw thickness; hence, it is assumed that the aqueous extract has a noninflammatory pain reliever activity, in contrast with previous research when the phytochemical compounds were obtained by the ethanolic extraction [335]. On the other hand, the methanolic extract of different Mentha species displayed different analgesic effects, indicating that these effects are species- and extract-form dependent [337, 338]. These findings indicate that the phytochemicals present in the M. piperita extract exhibit analgesic effect arising from both CNS and peripheral actions since the response appears to both thermal and chemical pain stimuli. A similar efficacy is characteristic of central analgesics, such as morphine, which inhibits equally inflammatory and noninflammatory pains. The results concerning analgesic effects produced by M. piperita strongly recommend this plant as pain reducing and encourage further studies for a better understanding of the nociception mechanism in order to find new options in pain therapy, with less side effects.
Toxicology studies of peppermint oil and its components completed in animals have shown no adverse effects or histopathological modifications. There are no chronic toxicity studies of peppermint in humans, although the use of peppermint oil has been reported as contraindicated in patients with bile duct, gallbladder, and liver disorders. The use of peppermint oil capsules in patients with GI reflux, hiatal hernia, or kidney stones needs also caution [339].
3.18.2. Mentha spicata
Mentha spicata L., also known as spearmint, originated in Bangladesh and is traditionally used as herbal remedy for various disorders. Hajjaj Yousuf et al. have performed a study which aimed at evaluating the analgesic, anti-inflammatory, and antipyretic effects of M. spicata on animal models, using hot-plate, acetic acid-induced writhing test, carrageenan-induced rat paw edema, and yeast-induced pyrexia methods [340]. The hot-plate results suggest a centrally antinociceptive action with a higher pain inhibition at 180 minutes after administration, being comparable to a standard drug. The acetic acid-induced writhing method evaluates the peripherally analgesic action, which took place through inhibition of local peritoneal receptors, most probably by inhibition of cyclooxygenase activity. The anti-inflammatory effect was maintained at a significant level for a 6-hour period, showing efficiency in the late phase of inflammation due to the presence of certain components that interfere with the release of prostaglandins.
Many other research studies on Mentha species such as M. longifolia [341], M. arvensis [342], or M. villosa [343] were also carried out regarding the analgesic activity. Although the phytochemical occurrence is not identical, different mechanisms have been consequently involved in achieving the antinociception, with competitive results.
3.19. Lavandula Genus
Lavandula genus includes more than 39 known species, mostly distributed in Arabia, Mediterranean Coasts, Asia, Middle East, and Northern Africa. Lavandula officinalis, Lavandula angustifolia, Lavandula hybrida, and Lavandula vera have been considered as antidepressive, antispasmodic, antiflatulent, antiemetic, diuretic, anticonvulsant, antibacterial, antiepileptogenic, antioxidant, antibacterial, antifungal, sedative, antinociceptive, and gastroprotective effects [344–348]. Lavender comprised over 100 constituents, among which the primary components are polyphenols, anthocyanins, carotenoids, linalool and linalyl acetate, α-pinene, limonene, 1,8-cineole, cis- and trans-ocimene, 3-octanone, camphor, caryophyllene, terpinen-4-ol, and flavonoids [349, 350].
3.19.1. Lavandula angustifolia
Lavandula angustifolia Mill. is one of the most famous aromatic and medicinal plants [351] used in fresh state or dry condition, containing 1–6% volatile oils (monoterpenic compounds, alcohols, and esters), triterpenic acids, coumarins, flavones, resins, and polyphenols [352]. As medicinal activity, L. angustifolia extracts or essential oils possess antispastic, carminative, analgesic, sedative, hypotensive, antiseptic, antimicrobial, antifungic, diuretic, and general tonic action, but little information on lavender analgesic properties is available in the literature.
3.19.2. Lavandula officinalis
Lavandula officinalis Chaix is used in traditional and herbal medicine for the treatment of pain and in the reduction of the inflammatory pain. In pharmacological and biological tests, extracts, fractions, and essential oils of L. officinalis are reported to have analgesic effects. The literature data show that L. officinalis extract contains linalool, acetate linalool, monotril, sesquiterpene, luteolin, ursolic acid, coumarin, and umbelliferone. Hajhashemi and Ghannadi [349] showed that the aquatic, alcoholic, and phenolic extracts have antinociception effects in the second phase of the formalin test, but only the phenolic and alcoholic extracts had been able to prevent the first phase of the formalin test. Barocelli et al. (2004) [353] proved that L. officinalis leaves inhalation attenuates pain evoked by hot-plate test, and stomach graze induced by high-dose administration of ethanol and ascetic acid. Husseini et al. (2015) [354] demonstrated that L. officinalis hydroalcoholic extracts inhibit inflammation and pain induced by formalin and cyclooxygenase (COX) type 1 and 2 activity in mice, using the formalin and hot-plate tests. The administration of the extract (100, 200, 250, 300, 400, and 800 mg/kg, i.p.) has inhibitory effects on inflammation induced by formalin injection into the animals hind paw, effects equal to morphine, dexamethasone, and indomethacin. The extract in 100, 200, and 300 mg/kg significantly reduced heat-induced pain and COX activity in dose-dependent manner.
3.19.3. Lavandula hybrida
In 2004, Barocelli et al. [353] demonstrated the antinociceptive and the gastroprotective effects of orally administered (100 mg/kg) or inhaled Lavandula hybrida Reverchon “Grosso” essential oil, and its principal constituents linalool and linalyl acetate in rodents. In the hot-plate test, the analgesic activity was observed after oil inhalation was inhibited by naloxone, atropine, and mecamylamine pretreatment, suggesting the involvement of opioidergic as well as cholinergic pathways. Therefore, the lavender oil reveals an interesting analgesic activity mainly relevant after inhalation, at doses devoid of sedative side effect, suggesting the interest for potential application of this oil in aromatherapy.
4. Identification of Secondary Metabolites
The identification of secondary metabolites from essential oils was achieved by gas chromatography coupled with mass spectrometry and from aqueous or alcoholic extracts by liquid chromatography coupled with mass spectrometry. Due to the high selectivity and sensitivity, mass spectrometry coupled to separation techniques such as gas chromatography and liquid chromatography represents a valuable technique for the qualitative and quantitative analysis of chemical substances present in essential oils and plant extracts.
The determination of the chemical composition belonging to essential oils for the following 14 species of the Lamiaceae family of plants: Hyptis pectinata [357], Lavandula angustifolia [349], Lavandula officinalis [356], Leonurus cardiaca [290], Lamium purpureum [357], Melissa officinalis [358], Mentha spicata [359], Marrubium vulgare [360], Origanum vulgare [361], Ocimum basilicum [362], Rosmarinus officinalis [363], Salvia officinalis [364], Satureja hortensis, and Thymus vulgaris [365], included in most of the scientific articles follow the same steps: (i) collection of flowering aerial parts and drying of the plant material, (ii) hydrodistillation of the dried plant material using a Clevenger apparatus for 1 to 5 hours, (iii) drying the essential oil using anhydrous sodium sulfate (Na2SO4), storing the essential oil in the dark at 4°C, i.v. injection of 0.1–1 μl of the essential oil in the capillary column of a gas chromatograph, and separation of the chemical compounds, (v) ionization and detection of each volatile substance in a mass spectrometer, and (vi) identification of the components performed based on their retention indices established in relation with a series of n-alkanes (C8–C32) and based on the mass spectra stored in NIST 21, NIST 107, Wiley spectral libraries, or reported in scientific articles.
The volatile substances isolated from the 14 species of plants and analyzed by gas chromatography coupled with mass spectrometry are presented for each of the essential oils in Table 1.
Table 1.
Compounds identified by GC-MS in essential oil.
| Number | Compound | Plant name | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hyptis pectinata | Lavandula angustifolia | Lavandula officinalis | Leonurus cardiaca | Lamium purpureum | Melissa officinalis | Mentha spicata | Marrubium vulgare | Origanum vulgare | Ocimum basilicum | Rosmarinus officinalis | Salvia officinalis | Satureja hortensis | Thymus vulgaris | References | ||
| 1 | Sabinene | + | + | + | + | + | + | [355, 357–359, 361, 364] | ||||||||
| 2 | β-Pinene | + | + | + | + | + | + | + | + | + | + | [355, 357, 359–361, 363–365] | ||||
| 3 | 1-Octen-3-ol | + | + | + | [355, 358, 361] | |||||||||||
| 4 | Limonene | + | + | + | + | + | + | + | + | [290, 355, 357, 358, 364, 365] | ||||||
| 5 | β-(E)-Ocimene | + | + | + | + | + | [349, 355, 357, 358, 361] | |||||||||
| 6 | Linalool | + | + | + | + | + | + | + | + | + | [349, 355, 356, 360–363] | |||||
| 7 | α-Copaene | + | + | + | + | + | [355, 356, 357, 358, 362] | |||||||||
| 8 | β-Elemene | + | + | + | [355, 357, 362] | |||||||||||
| 9 | β-Caryophyllene | + | + | + | + | + | + | + | + | + | + | + | + | + | [349, 355–359, 361, 363–365] | |
| 10 | Aromadendrene | + | + | [355, 364] | ||||||||||||
| 11 | cis-Muurola-3,5-diene | + | [355] | |||||||||||||
| 12 | α-Humulene | + | + | + | + | + | + | + | + | [290, 355, 356, 358, 360–362, 364] | ||||||
| 13 | Germacrene D | + | + | + | + | + | + | + | + | [290, 349, 355, 358, 360–362] | ||||||
| 14 | cis-β-Guaiene | + | [355] | |||||||||||||
| 15 | γ-Patchoulene | + | [355] | |||||||||||||
| 16 | Germacrene A | + | [355] | |||||||||||||
| 17 | γ-Cadinene | + | + | + | + | + | + | [290, 355, 357, 358, 361, 362] | ||||||||
| 18 | trans-Calamenene | + | [355] | |||||||||||||
| 19 | Germacrene B | + | + | [355, 356] | ||||||||||||
| 20 | Caryophyllene oxide | + | + | + | + | [290, 355, 358, 364] | ||||||||||
| 21 | 1,10-Di-epi-cubenol | + | [355] | |||||||||||||
| 22 | Calamusenone | + | [355] | |||||||||||||
| 23 | Cyperotundone | + | [355] | |||||||||||||
| 24 | α-Thujene | + | + | + | + | + | + | [349, 357, 361, 363–365] | ||||||||
| 25 | α-Pinene | + | + | + | + | + | + | + | + | + | + | + | + | [290, 349, 356–361, 363–365] | ||
| 26 | α-Fenchene | + | + | [349, 364] | ||||||||||||
| 27 | Camphene | + | + | + | + | + | + | + | + | [349, 356, 360, 361, 363–365] | ||||||
| 28 | Delta-3-carene | + | [349] | |||||||||||||
| 29 | 1,8-Cineole | + | + | + | + | + | + | + | + | [349, 356, 358–360, 362–364] | ||||||
| 30 | γ-Terpinene | + | + | + | + | + | + | + | + | [349, 356, 358, 359, 361, 364, 365] | ||||||
| 31 | Terpinolene | + | + | + | + | + | + | [290, 349, 358, 363–365] | ||||||||
| 32 | Camphor | + | + | + | + | + | [349, 356, 360, 363, 364] | |||||||||
| 33 | Borneol | + | + | + | + | + | + | [349, 360, 363–365] | ||||||||
| 34 | Lavandulol | + | [349] | |||||||||||||
| 35 | 4-Terpineol | + | + | + | + | + | + | [349, 356, 358, 359, 364, 365] | ||||||||
| 36 | α-Terpineol | + | + | + | + | + | + | + | + | [349, 356, 358, 359, 361, 364, 365] | ||||||
| 37 | Linalyl acetate | + | + | + | [349, 361, 364] | |||||||||||
| 38 | Bornyl acetate | + | + | + | + | + | + | [349, 356, 358, 362–364] | ||||||||
| 39 | cis-β-Farnesene | + | [349] | |||||||||||||
| 40 | Verbenene | + | [356] | |||||||||||||
| 41 | 1,3,5-cycloheptatriene | + | [356] | |||||||||||||
| 42 | 3-Octanone | + | + | [356, 357] | ||||||||||||
| 43 | β-myrcene | + | + | + | + | + | + | + | + | + | [356, 357–359, 361, 364–365] | |||||
| 44 | 3-Octanol | + | + | [356, 357] | ||||||||||||
| 45 | α-Phellandrene | + | + | + | + | [356, 361, 363, 365] | ||||||||||
| 46 | o-Isopropenyl toluene | + | [356] | |||||||||||||
| 47 | α-Terpinene | + | + | + | + | + | [356, 358, 361, 364, 365] | |||||||||
| 48 | p-Cymene | + | + | + | + | + | + | + | + | [290, 356, 358, 359, 361, 364, 365] | ||||||
| 49 | Linalool oxide | + | [356] | |||||||||||||
| 50 | Methyl benzoate | + | [356] | |||||||||||||
| 51 | Thujancis | + | [356] | |||||||||||||
| 52 | D-fenchyl alcohol | + | [356] | |||||||||||||
| 53 | Pinocarveol | + | [356] | |||||||||||||
| 54 | Isopinocamphone | + | + | [356, 364] | ||||||||||||
| 55 | Pinocarvone | + | [356] | |||||||||||||
| 56 | Pinocamphone | + | + | [356, 364] | ||||||||||||
| 57 | Naphthalene | + | [356] | |||||||||||||
| 58 | p-Cymen-8-ol | + | + | [356, 364] | ||||||||||||
| 59 | Myrtenol | + | [356] | |||||||||||||
| 60 | Verbenone | + | [356] | |||||||||||||
| 61 | trans-Carveol | + | + | [356, 359] | ||||||||||||
| 62 | β-Citronellol | + | + | [356, 360] | ||||||||||||
| 63 | Pulegone | + | + | + | [356, 358, 359] | |||||||||||
| 64 | Piperitone | + | + | [356, 359] | ||||||||||||
| 65 | Cinnamaldehyde | + | [356] | |||||||||||||
| 66 | Thymol | + | + | + | + | + | [356, 358, 361, 364, 365] | |||||||||
| 67 | 2-Hydroxy-4-isopropyl-1-methylbenzene | + | [356] | |||||||||||||
| 68 | Carvacrol | + | + | + | + | + | [356, 361, 364, 365] | |||||||||
| 69 | Piperitenone | + | + | [356, 358] | ||||||||||||
| 70 | α-Cubebene | + | [356] | |||||||||||||
| 71 | Thymyl acetate | + | [356] | |||||||||||||
| 72 | Farnesene | + | + | + | [356, 357, 362] | |||||||||||
| 73 | β-Acoradiene | + | [356] | |||||||||||||
| 74 | α-Cedrene | + | [356] | |||||||||||||
| 75 | Spathulenol | + | + | + | + | + | [290, 356, 358, 362, 365] | |||||||||
| 76 | Butylidenephthalide | + | [356] | |||||||||||||
| 77 | 3N Butylphthalide | + | [356] | |||||||||||||
| 78 | Butylidene dihydrophthalide | + | [356] | |||||||||||||
| 79 | 3-Methyl butanal | + | [290] | |||||||||||||
| 80 | (E,E)-2,4-Hexadienal | + | [290] | |||||||||||||
| 81 | Benzaldehyde | + | [290] | |||||||||||||
| 82 | Dehydro-1,8-cineole | + | [290] | |||||||||||||
| 83 | Phenylacetaldehyde | + | [290] | |||||||||||||
| 84 | p-Menth-1,5-dien-8-ol | + | [290] | |||||||||||||
| 85 | Dodecane | + | [290] | |||||||||||||
| 86 | Dihydroedulan I | + | [290] | |||||||||||||
| 87 | (E)-α-ionone | + | [290] | |||||||||||||
| 88 | β-Humulene | + | [290] | |||||||||||||
| 89 | Geranyl acetone | + | [290] | |||||||||||||
| 90 | (E)-β-ionone | + | [290] | |||||||||||||
| 91 | β-Selinene | + | [290] | |||||||||||||
| 92 | Eugenyl acetate | + | [290] | |||||||||||||
| 93 | (E)-nerolidol | + | [290] | |||||||||||||
| 94 | trans-Sesquisabinene hydrate | + | [290] | |||||||||||||
| 95 | Presilphiperfolan-8-ol | + | [290] | |||||||||||||
| 96 | β-Atlantol | + | [290] | |||||||||||||
| 97 | Epi-cedrol | + | [290] | |||||||||||||
| 98 | α-Bisabolol | + | [290] | |||||||||||||
| 99 | (2E, 6E)-farnesol | + | [290] | |||||||||||||
| 100 | 8-Cedren-13-ol acetate | + | [290] | |||||||||||||
| 101 | 6,10,14-Trimethyl-2-pentadecanone | + | [290] | |||||||||||||
| 102 | (2Z, 6E)-farnesyl acetate | + | [290] | |||||||||||||
| 103 | Methyl-linolenate | + | [290] | |||||||||||||
| 104 | Allo-aromadendrene epoxide | + | [290] | |||||||||||||
| 105 | Eicosane | + | [290] | |||||||||||||
| 106 | Heneicosane | + | [290] | |||||||||||||
| 107 | (E)-3-hexen-1-ol | + | [349] | |||||||||||||
| 108 | Heptanal | + | [357] | |||||||||||||
| 109 | 1-Octen-3-one | + | [357] | |||||||||||||
| 110 | (E,E)-2,4-Heptadienal | + | [357] | |||||||||||||
| 111 | Z-β-ocimene | + | + | + | [356, 357, 361] | |||||||||||
| 112 | Undecane | + | [357] | |||||||||||||
| 113 | Nonanal | + | [357] | |||||||||||||
| 114 | Decanal | + | [357] | |||||||||||||
| 115 | β-Cyclocitral | + | [357] | |||||||||||||
| 116 | N-tridecane | + | [357] | |||||||||||||
| 117 | Delta-elemene | + | + | [357, 361] | ||||||||||||
| 118 | (E)-β-damascenone | + | [357] | |||||||||||||
| 119 | β-bourbonene | + | + | + | + | [290, 357, 359, 361] | ||||||||||
| 120 | (E)-β-farnesene | + | [357] | |||||||||||||
| 121 | Farnesane | + | [357] | |||||||||||||
| 122 | Bicyclogermacrene | + | + | + | [357, 358, 365] | |||||||||||
| 123 | n-Pentadecane | + | [357] | |||||||||||||
| 124 | (E)-hydrate de sabinene | + | [358] | |||||||||||||
| 125 | p-Menth-3,8-diene | + | [358] | |||||||||||||
| 126 | Z-hydrate de sabinene | + | + | [358, 365] | ||||||||||||
| 127 | 1-Octen-3-ol acetate | + | [358] | |||||||||||||
| 128 | 3-Octenyl acetate | + | [358] | |||||||||||||
| 129 | p-Menth-3-en-8-ol | + | [358] | |||||||||||||
| 130 | Menthone | + | + | [358, 359] | ||||||||||||
| 131 | Isomenthone | + | + | + | + | [358–360, 364] | ||||||||||
| 132 | Neomenthol | + | [358] | |||||||||||||
| 133 | Z-Piperitone oxide | + | [358] | |||||||||||||
| 134 | Pseudodisphenol | + | [358] | |||||||||||||
| 135 | Isopulegyl acetate 1 | + | [358] | |||||||||||||
| 136 | Neomenthylacetate | + | + | [358, 359] | ||||||||||||
| 137 | Diosphenol | + | [358] | |||||||||||||
| 138 | Menthylacetate | + | + | [358, 359] | ||||||||||||
| 139 | Piperitenone oxide | + | [358] | |||||||||||||
| 140 | (E)-jasmone | + | [358] | |||||||||||||
| 141 | Nepetalactone | + | [358] | |||||||||||||
| 142 | p-Menth-1,2,3-triol | + | [358] | |||||||||||||
| 143 | α-Gurjunene | + | [358] | |||||||||||||
| 144 | Cadina-3,5-diene | + | [358] | |||||||||||||
| 145 | Delta-cadinene | + | + | [358, 360] | ||||||||||||
| 146 | Viridiflorol | + | [358] | |||||||||||||
| 147 | 1,10-Di-epi-cubenol | + | [358] | |||||||||||||
| 148 | α-cadinol | + | + | [358, 362] | ||||||||||||
| 149 | 2-Octanol | + | [359] | |||||||||||||
| 150 | Menthol | + | [359] | |||||||||||||
| 151 | Isomenthol | + | [359] | |||||||||||||
| 152 | Dihydrocarveol | + | + | + | [359, 364] | |||||||||||
| 153 | Carvone | + | + | [357, 359] | ||||||||||||
| 154 | cis-Carveol | + | [359] | |||||||||||||
| 155 | trans-Anethole | + | [359] | |||||||||||||
| 156 | Menthyl camphor | + | [359] | |||||||||||||
| 157 | Eugenol | + | + | [359, 362] | ||||||||||||
| 158 | N-trimethylsilyl trifluoroacetamide | + | [360] | |||||||||||||
| 159 | N,Nʹ-bis(trimethylsilyl) trifluoroacetamide | + | [360] | |||||||||||||
| 160 | α-Thujone | + | [360] | |||||||||||||
| 161 | 1-Vinyl cyclohexane | + | [360] | |||||||||||||
| 162 | Geraniol | + | + | [360, 364] | ||||||||||||
| 163 | Citronellyl formate | + | [360] | |||||||||||||
| 164 | α-Muurolene | + | [360] | |||||||||||||
| 165 | α-Amorphene | + | + | [360, 362] | ||||||||||||
| 166 | Neoalloocimene | + | [360] | |||||||||||||
| 167 | Neryl acetate | + | [360] | |||||||||||||
| 168 | Ledene | + | [360] | |||||||||||||
| 169 | β-Bisabolene | + | + | + | [360, 361, 365] | |||||||||||
| 170 | α-Agarofuran | + | [360] | |||||||||||||
| 171 | γ-Eudesmol | + | [360] | |||||||||||||
| 172 | Furan-2-one, 4-phenyltetrahydro | + | [360] | |||||||||||||
| 173 | β-Cubebene | + | [360] | |||||||||||||
| 174 | Citronellyl butanoate | + | [360] | |||||||||||||
| 175 | Geranyl tiglate | + | [360] | |||||||||||||
| 176 | Cyclononasiloxane, octadecamethyl | + | [360] | |||||||||||||
| 177 | Eicosamethylcyclodecasiloxane | + | [360] | |||||||||||||
| 178 | β-Phellandrene | + | + | + | [361, 365] | |||||||||||
| 179 | Carvacrol methyl ether | + | + | [361, 365] | ||||||||||||
| 180 | Allo-aromadendrene | + | + | + | [361, 362, 364] | |||||||||||
| 181 | cis-Epoxy-ocimen | + | [362] | |||||||||||||
| 182 | cis-Caryophyllene | + | [362] | |||||||||||||
| 183 | α-Guaiene | + | [362] | |||||||||||||
| 184 | Delta-guaiene | + | [362] | |||||||||||||
| 185 | cis-Calamenene | + | [362] | |||||||||||||
| 186 | Epi-bicyclosesquiphellandrene | + | [365] | |||||||||||||
| 187 | β-Eudesmol | + | [362] | |||||||||||||
| 188 | α-Selinene | + | [362] | |||||||||||||
| 189 | Zingiberene | + | [362] | |||||||||||||
| 190 | Tricyclene | + | [360] | |||||||||||||
| 191 | o-Cymene | + | + | + | [358, 363, 364] | |||||||||||
| 192 | Trifluoroacetyl-α- | |||||||||||||||
| Terpineol | + | [363] | ||||||||||||||
| 193 | Carene | + | [363] | |||||||||||||
| 194 | cis-α-Terpineol | + | [363] | |||||||||||||
| 195 | 2-Bornanone | + | [363] | |||||||||||||
| 196 | Isoborneol | + | + | [363, 364] | ||||||||||||
| 197 | trans-Pinocarveol | + | [364] | |||||||||||||
| 198 | (-)-Citronellal | + | + | [363] | ||||||||||||
| 199 | Myrtenal | + | + | [363] | ||||||||||||
| 200 | Myrtenol | + | + | [363] | ||||||||||||
| 201 | Isobornyl acetate | + | [363] | |||||||||||||
| 202 | β-Cedrene | + | [363] | |||||||||||||
| 203 | γ-Gurjunene | + | [363] | |||||||||||||
| 204 | α-7-Epi-selinene | + | [363] | |||||||||||||
| 205 | Carvacrol acetate | + | [361] | |||||||||||||
The chemical compounds identified by LC-ESI-MS in extracts prepared for the 9 species of plants that are included in the Lamiaceae family are also presented in Table 2.
Table 2.
Compounds identified by HPLC-ESI-MS in aqueous and alcoholic extracts.
| Number | Compound | Plant name | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Lamium garganicum subsp. Laevigatum | Melissa officinalis | Mentha spicata | Mentha pulegium | Marrubium vulgare | Origanum vulgare | Ocimum basilicum | Rosmarinus officinalis | Salvia officinalis | References | ||
| 1 | Lamalbidee | + | [366] | ||||||||
| 2 | Sesamoside | + | [366] | ||||||||
| 3 | Lamiide | + | [366] | ||||||||
| 4 | 6-β-OH ipolamiide | + | [366] | ||||||||
| 5 | Shanzhiside methyl ester | + | [366] | ||||||||
| 6 | Dehydropenstemoside | + | [366] | ||||||||
| 7 | 8-O-acetyl shanzhiside methyl ester | + | [366] | ||||||||
| 8 | 6-Syringyl-8-O-acetyl shanzhiside methyl ester | + | [366] | ||||||||
| 9 | 3-(3,4-Dihydroxyphenyl)-lactic acid | + | [367] | ||||||||
| 10 | Caftaric acid | + | + | [367, 372] | |||||||
| 11 | Caffeic acid hexoside | + | + | [367, 370] | |||||||
| 12 | Fertaric acid | + | [367] | ||||||||
| 13 | Caffeic acid | + | + | + | + | + | + | + | [367, 369, 370, 372, 373] | ||
| 14 | Sulfated rosmarinic acid | + | [367] | ||||||||
| 15 | Yunnaneic acid E | + | [367] | ||||||||
| 16 | Prolithospermic acid | + | [367] | ||||||||
| 17 | Lithospermic acid A isomer | + | [367] | ||||||||
| 18 | Chicoric acid | + | [367] | ||||||||
| 19 | Salvianolic acid C derivative | + | [367] | ||||||||
| 20 | Sagerinic acid | + | + | [367, 372] | |||||||
| 21 | cis-Rosmarinic acid | + | [367] | ||||||||
| 22 | trans-Rosmarinic acid | + | [367] | ||||||||
| 23 | Salvianolic acid A isomer | + | [367] | ||||||||
| 24 | Protocatechuic acid | + | + | + | + | [370–373] | |||||
| 25 | Hydroxybenzoic acid | + | + | [372, 373] | |||||||
| 26 | Hydroxyphenyllactic acid | + | [372] | ||||||||
| 27 | Luteolin-8-C-glucoside (orientin) | + | [372] | ||||||||
| 28 | 3′-Caffeoylquinic (neochlorogenic acid) | + | + | [370, 372] | |||||||
| 29 | Coumaric acid | + | + | [370, 372] | |||||||
| 30 | Salvianolic acid F | + | [372] | ||||||||
| 31 | Dicaffeic acid | + | [372] | ||||||||
| 32 | 5′-Caffeoylquinic (chlorogenic acid) | + | + | + | + | + | [56, 370–373] | ||||
| 33 | Feruloylquinic acid | + | [372] | ||||||||
| 34 | Rosmarinic acid-O-caffeic acid | + | [372] | ||||||||
| 35 | Rosmarinic acid-rutinoside | + | [372] | ||||||||
| 36 | Salvianolic acid J isomer | + | [372] | ||||||||
| 37 | Luteolin-rutinoside | + | + | + | [56, 372] | ||||||
| 38 | Rosmarinic acid-O-hexoside | + | + | [370, 372] | |||||||
| 39 | Luteolin-hexoside | + | + | + | [372, 373] | ||||||
| 40 | Luteolin-7-glucuronide | + | + | + | + | [371–373] | |||||
| 41 | Salvianolic acid B/E isomer | + | [372] | ||||||||
| 42 | Narirutin (naringenin-7-O-rutinoside) | + | [372] | ||||||||
| 43 | Salvianolic acid D | + | [372] | ||||||||
| 44 | Salvianolic acid E | + | + | [56, 372] | |||||||
| 45 | Rosmarinic acid | + | + | + | + | + | + | [56, 370–373] | |||
| 46 | Sagerinic acid isomer | + | [372] | ||||||||
| 47 | Salvianolic acid A derivative | + | [372] | ||||||||
| 48 | Lithospermic acid | + | + | [56, 372] | |||||||
| 49 | Salvianolic acid B | + | + | [56, 372] | |||||||
| 50 | Dehydrorosmarinic acid | + | [372] | ||||||||
| 51 | Rosmarinic acid dihexoside | + | [372] | ||||||||
| 52 | Salvianolic acid A | + | [372] | ||||||||
| 53 | Apigenin | + | + | + | + | + | [56, 369–372] | ||||
| 54 | Hydroxybenzoic acid hexose isomer 1 | + | + | [56, 373] | |||||||
| 55 | Vanillyl alcohol | + | [8] | ||||||||
| 56 | Dihydroxybenzoic acid hexose | + | [8] | ||||||||
| 57 | Vanillic acid hexose | + | + | [4, 8] | |||||||
| 58 | Syringic acid | + | + | + | [56, 370, 371] | ||||||
| 59 | Hydroxybenzoic acid hexose isomer 2 | + | [8] | ||||||||
| 60 | Dihydroxybenzoic acid | + | [8] | ||||||||
| 61 | Syringic acid hexose | + | [8] | ||||||||
| 62 | Caffeic acid glucuronide isomer 1 | + | [8] | ||||||||
| 63 | Caffeic acid glucuronide isomer 2 | + | [56] | ||||||||
| 64 | p-Coumaric acid | + | + | + | [56, 371, 372] | ||||||
| 65 | Salvianolic acid I | + | [56] | ||||||||
| 66 | Salvianolic acid H | + | [56] | ||||||||
| 67 | Isosalvianolic acid B | + | [56] | ||||||||
| 68 | Eukovoside | + | [56] | ||||||||
| 69 | Salvianolic acid C | + | [56] | ||||||||
| 70 | Catechin-4-ol-O-glycopyranoside | + | [56] | ||||||||
| 71 | Gallocatechin isomer 1 | + | [56] | ||||||||
| 72 | (+)-Catechin hydrated | + | [56] | ||||||||
| 73 | Diosmin | + | [56] | ||||||||
| 74 | Acacetin rutinoside | + | [56] | ||||||||
| 75 | Hesperidin | + | [56] | ||||||||
| 76 | Isosakuranetin-O-rutinoside | + | [56] | ||||||||
| 77 | Syringetin | + | [56] | ||||||||
| 78 | Jaceidin isomer 1 | + | [56] | ||||||||
| 79 | Geshoidin | + | [369] | ||||||||
| 80 | Decaffeoylverbascoside | + | [369] | ||||||||
| 81 | Sacranoside A | + | [369] | ||||||||
| 82 | Marruboside | + | [369] | ||||||||
| 83 | Forsythoside B (isomer 1) | + | [369] | ||||||||
| 84 | Forsythoside B (isomer 2) | + | [369] | ||||||||
| 85 | Verbascosin | + | [369] | ||||||||
| 86 | Luteolin-O-glucoside | + | + | [369, 373] | |||||||
| 87 | Alyssonoside | + | [369] | ||||||||
| 88 | Leukoceptoside A | + | [369] | ||||||||
| 89 | Apigenin-O-glucoside | + | [369] | ||||||||
| 90 | Deacetylforskolin (isomer 1) | + | [369] | ||||||||
| 91 | Preleosibirin | + | [369] | ||||||||
| 92 | Deacetylforskolin (isomer 2) | + | [369] | ||||||||
| 93 | Garcinone E (isomer 1) | + | [369] | ||||||||
| 94 | Terniflorin (isomer 1) | + | [369] | ||||||||
| 95 | Garcinone E (isomer 2) | + | [369] | ||||||||
| 96 | Luteolin | + | + | + | [369, 371, 372] | ||||||
| 97 | Premarrubiin (isomer 1) | + | [369] | ||||||||
| 98 | Terniflorin (isomer 2) | + | [369] | ||||||||
| 99 | Premarrubiin (isomer 2) | + | [369] | ||||||||
| 100 | Deacetylforskolin (isomer 3) | + | [369] | ||||||||
| 101 | Terniflorin (isomer 3) | + | [369] | ||||||||
| 102 | Deacetylforskolin (isomer 4) | + | [369] | ||||||||
| 103 | Deacetylforskolin (isomer 5) | + | [369] | ||||||||
| 104 | Marrulibacetal A (isomer 1) | + | [369] | ||||||||
| 105 | Marrulibacetal A (isomer 2) | + | [369] | ||||||||
| 106 | Premarrubiin (isomer 3) | + | [369] | ||||||||
| 107 | Premarrubiin (isomer 4) | + | [369] | ||||||||
| 108 | Anisofolin A (isomer 1) | + | [369] | ||||||||
| 109 | Anisofolin A (isomer 2) | + | [369] | ||||||||
| 110 | Marrubenol | + | [369] | ||||||||
| 111 | Gallic acid | + | + | [372, 373] | |||||||
| 112 | p-Hydroxybenzoic acid | + | + | + | [371, 372] | ||||||
| 113 | m-Hydroxybenzoic acid | + | [370] | ||||||||
| 114 | Coumaric acid-O-hexoside | + | [370] | ||||||||
| 115 | Cryptochlorogenic acid (4-O-caffeoylquinic acid) | + | [370] | ||||||||
| 116 | Homovanilic acid | + | [370] | ||||||||
| 117 | Apigenin-C-hexoside-C-hexoside | + | [370] | ||||||||
| 118 | 4-O-p-coumaroylqunic acid | + | [370] | ||||||||
| 119 | Kaempferol-O-dihexoside | + | [370] | ||||||||
| 120 | Ferulic acid | + | + | [370, 371] | |||||||
| 121 | Kaempferol-3-O-rutinoside | + | + | [370, 371] | |||||||
| 122 | Quercetin-3-O-glucoside | + | + | [370, 371] | |||||||
| 123 | Kaempferol-3-O-glucoside | + | [370] | ||||||||
| 124 | Dicaffeoylquinic acid | + | [370] | ||||||||
| 125 | Hesperidin | + | [370] | ||||||||
| 126 | Apigenin-7-O-glucoside | + | + | + | [370–372] | ||||||
| 127 | Kaempferol | + | + | [370, 371] | |||||||
| 128 | Quercetin | + | + | [370, 371] | |||||||
| 129 | Hesperidin (hesperetin-7-O-rutinoside) | + | + | [370, 371] | |||||||
| 130 | Rosmanol | + | + | [370, 372] | |||||||
| 131 | Carnosic acid | + | + | + | [370, 372, 373] | ||||||
| 132 | Quercetin-3-O-rutinoside (rutin) | + | [371] | ||||||||
| 133 | Quercetin-3-O-malonylglucoside | + | [371] | ||||||||
| 134 | Apigenin-7-O-glucuronide | + | + | [371, 373] | |||||||
| 135 | Eugenol | + | [371] | ||||||||
| 136 | Coniferaldehyde | + | [371] | ||||||||
| 137 | Isothymusin | + | [371] | ||||||||
| 138 | Kaempferide | + | [371] | ||||||||
| 139 | Cirsiliol | + | [371] | ||||||||
| 140 | Cirsimaritin | + | [371] | ||||||||
| 141 | Cirsilineol | + | [371] | ||||||||
| 142 | Nevadensin | + | [371] | ||||||||
| 143 | Acacetin | + | [371] | ||||||||
| 144 | 5-Desmethylsinensetin | + | [371] | ||||||||
| 145 | Methyleugenol | + | [371] | ||||||||
| 146 | Salvigenin | + | [371] | ||||||||
| 147 | Methoxyeugenol | + | [371] | ||||||||
| 148 | Gardenin B | + | [371] | ||||||||
| 149 | Apigenin-7,4-dimethylether | + | [371] | ||||||||
| 150 | Oleanolic acid | + | [371] | ||||||||
| 151 | Ursolic acid | + | [371] | ||||||||
| 152 | Galloylglucose | + | [371] | ||||||||
| 153 | Etylprotocatechuate | + | [371] | ||||||||
| 154 | Methylgallate | + | [371] | ||||||||
| 155 | Sinapinic acid | + | [371] | ||||||||
| 156 | Methylprotocatechuate | + | [371] | ||||||||
| 157 | Vanillic acid | + | [371] | ||||||||
| 158 | Ethyl caffeate | + | [371] | ||||||||
| 159 | Medioresinol | + | [372] | ||||||||
| 160 | Isorhamnetin-3-O-hexoside | + | [372] | ||||||||
| 161 | Homoplantaginin (hispidulin 7-glucoside) | + | [372] | ||||||||
| 162 | Dihydroxy-dimethoxyflavone derivative | + | [372] | ||||||||
| 163 | Dihydroxy-dimethoxyflavone | + | [372] | ||||||||
| 164 | Medioresinol derivative | + | [372] | ||||||||
| 165 | Luteolin-3′-acetyl-O-glucuronide | + | [372] | ||||||||
| 166 | Medioresinol-glucuronide | + | [372] | ||||||||
| 167 | Eriodictyol | + | [372] | ||||||||
| 168 | Isorhamnetin-rutinoside | + | [372] | ||||||||
| 169 | Isorhamnetin | + | [372] | ||||||||
| 170 | Trihydroxy-methoxyflavone | + | [372] | ||||||||
| 171 | Methylrosmarinate | + | [372] | ||||||||
| 172 | Apigenin-7-O-rutinoside | + | [372] | ||||||||
| 173 | Hispidulin-rutinoside | + | [372] | ||||||||
| 174 | Hesperetin | + | [372] | ||||||||
| 175 | 5,6,7,10-Tetrahydro-7-hydroxyrosmariquinone derivative | + | [372] | ||||||||
| 176 | Cirsimaritin | + | [372] | ||||||||
| 177 | Carnosol methyl ether isomer | + | [372] | ||||||||
| 178 | Rosmanol quinone | + | [372] | ||||||||
| 179 | Epirosmanol | + | [372] | ||||||||
| 180 | Carnosol quinone | + | [372] | ||||||||
| 181 | Isosakuranetin | + | [372] | ||||||||
| 182 | Genkwanin | + | [372] | ||||||||
| 183 | Carnosic acid hexoside | + | [372] | ||||||||
| 184 | Rosmanol isomer | + | [372] | ||||||||
| 185 | Carnosol | + | [372] | ||||||||
| 186 | Carnosic acid quinone | + | [372] | ||||||||
| 187 | 4′-Methoxytectochrysin | + | [372] | ||||||||
| 188 | Rosmadial | + | [372] | ||||||||
| 189 | Rosmaridiphenol | + | [372] | ||||||||
| 190 | 5,6,7,10-Tetrahydro-7-hydroxyrosmariquinone | + | [372] | ||||||||
| 191 | 12-O-methylcarnosic acid | + | [372] | ||||||||
| 192 | Betulinic acid | + | [372] | ||||||||
| 193 | Salvianic acid A | + | [373] | ||||||||
| 194 | Protocatechuoyl-hexose | + | [373] | ||||||||
| 195 | Dimethoxybenzoic acid | + | [373] | ||||||||
| 196 | Coumaroyl hexose | + | [373] | ||||||||
| 197 | Caffeoyl-fructosyl-glucose | + | [373] | ||||||||
| 198 | Coumaroyl-apiosyl-glucose-isomer | + | [373] | ||||||||
| 199 | Chlorogenic acid isomer | + | [373] | ||||||||
| 200 | Methyldihydrojasmonic acid isomer | + | [373] | ||||||||
| 201 | Feruloyl-glucose isomer | + | [373] | ||||||||
| 202 | Salvianolic acid I isomer | + | [373] | ||||||||
| 203 | Saponarin (apigenin-6-C-glucoside-7-O-glucoside) | + | [373] | ||||||||
| 204 | Salvianolic F isomer | + | [373] | ||||||||
| 205 | Luteolin diglucuronide | + | [373] | ||||||||
| 206 | Eriocitrin | + | [373] | ||||||||
| 207 | Hydroxy-luteolin-glucuronide | + | [373] | ||||||||
| 208 | Methylmelitric acid A | + | [373] | ||||||||
| 209 | Apigenin-diglucuronide | + | [373] | ||||||||
| 210 | Sagecoumarin | + | [373] | ||||||||
| 211 | Luteolin-rutinoside isomer | + | [373] | ||||||||
| 212 | Apigenin rutinoside isomer | + | [373] | ||||||||
| 213 | Apigenin hexoside | + | [373] | ||||||||
| 214 | Hispiludin-glucuronide | + | [373] | ||||||||
| 215 | Salvianolic acid B | + | [373] | ||||||||
| 216 | Salvianolic acid K isomer | + | [373] | ||||||||
| 217 | Carnosol isomer | + | [373] | ||||||||
| 218 | Epirosmanol | + | [373] | ||||||||
| 219 | Carnosic acid isomer | + | [373] | ||||||||
Yalçin and the collaborators showed, using HPLC-ESI-MS, that the n-butanol extract of Lamium garganicum subsp. Laevigatum, which was previously shown to possess anti-inflammatory and antinociceptive activity, contains nine iridoid glycosides [366].
The decoction prepared from Melissa officinalis dry leaves was filtered through a Whatman no. 4 filter paper, frozen and lyophilized. The phenolic compounds were separated and analyzed by HPLC coupled with an ESI-triple quadrupole-ion trap mass spectrometer using the negative-ion mode. The identification of the phenolic compounds was carried out based on the comparison of their retention time, UV-Vis, and mass spectra with those obtained from solutions prepared with standard substances. For the compounds for which no standard substance was available, the identification was performed based on the scientific literature [367].
Based on the UHPLC-ESI-MS data reported by Martina Cirlini et al. [368], the methanolic extract of Mentha spicata contains 88% of rosmarinic acid derivatives when calculating the amount of rosmarinic acid derivatives as percentage of the total amount of detected phenols. For the salvianolic acids, a percentage of 5.6% of the total amount of detected phenols was calculated.
Taamalli and collaborators reported the analyses of the methanolic extract of Mentha pulegium performed using an UPLC-ESI-QTOF mass spectrometer coupled with a liquid chromatograph and detected metabolites from the following groups: hydroxybenzoic acids, hydroxycinnamic acids, flavanols, flavones, flavanones, flavonols, organic acids, nucleosides, amino acids, and fatty acids [56]. In the methanolic extract of Mentha pulegium, the authors identified a very high amount of gallocatechin.
In the case of the plant Marrubium vulgare, Amessis-Ouchemoukh Nadia and collaborators prepared the methanolic extract and analyzed it using an UHPLC-ESI-QTOF instrument. The mass spectra were acquired in the negative-ion mode and showed the presence of the metabolites presented in Table 2 [369].
Anna Vallverdú-Queralt et al. identified the phenolic compounds present in the ethanolic acidified extract of Origanum vulgare (Table 2) [370]. After the first extraction with a hydroalcoholic solvent, the extracted plant material was centrifuged, dried, ground, and stored. An aliquot of 1 g of extracted and dried plant material was subjected to extraction, 3 times, with 5 mL of 50% aqueous ethanol containing 0.1% formic acid. All the supernatants were combined, and the organic solvent was evaporated under nitrogen flow. The dried residue was dissolved in 0.1% formic acid and subjected to solid-phase extraction using mixed-mode anion-exchange cartridges in order to reduce potential interferences from plant extracts. For accurate mass measurement, the separation and mass spectrometric analyses were performed using a LC-ESI-LTQ-Orbitrap mass spectrometer operated in negative-ion mode. The quantification of the compounds identified was performed using a triple-quadrupole mass spectrometer.
Pandey and Kumar performed extraction of dried leaves of Ocimum basilicum using 80% aqueous methanol [371]. A liquid chromatograph coupled to an ESI-Q-TOF mass spectrometer was used for the identification of the compounds, and the results are summarized in Table 2.
5. In Vivo Evaluation of Phytochemicals Analgesic Activity
Over the decades, just a few studies tried to find alternatives to the classical treatment of pain, such as the application of the Lamiaceae phytochemicals.
Marrubiin, the broadly known diterpenoid lactone, has been associated with the bitter principle of the horehound (Marrubium vulgare, M. deserti de Noe, M. alysson, and M. thessalum) and other traditionally important Lamiaceae species (Leonotis leonurus, L. nepetifolia, and Phlomis bracteosa) [67, 374–379]. According to recent literature, extensive pharmacological studies have revealed that marrubiin shows a suite of activities such as antinociceptive, antispasmodic, antihypertensive, antidiabetic, gastroprotective, anti-inflammatory, antimicrobial, anticancerous, antioxidant, and antihepatotoxic [65, 67, 71–73, 75, 374, 376–378].
Over time, the antinociceptive profile of marrubiin was analyzed in some animal models of pain. De Jesus et al.'s [64] results showed that marrubiin reveals potent and dose-related antinociceptive effects in mice, whose calculated ID50 values (μmol/kg, i.p.) were as follows: 2.2 in the writhing test, 6.6 (first phase) and 6.3 (second phase) in the formalin-induced pain test, and 28.8 when evaluated over the capsaicin test. These findings show that it is more potent than some other well-known analgesic drugs. The antinociception produced by the marrubiin is not reversed by naloxone when analyzed against the writhing test. Its exact mechanism of action remains however still to be determined, but the results suggest that marrubiin, like the hydroalcoholic extract of M. vulgare, does not interact with opioid systems.
Analgesic activity success was obtained by reducing lactonic function of the marrubiin, in the formation of marrubiinic acid and two esterified derivatives, which have shown significant analgesic effect on the writhing test in mice [68, 374]. The pharmacological studies specified that marrubiinic acid presents an important (p < 0.05) and dose-dependent antinociceptive effect, against the writhing test, in intraperitoneal administration, with ID50 value of 12 μmol/kg, being about 11-fold more active than the standard drugs used as reference, but less active than marrubiin [64].
Marrubiinic acid, given orally, at a dose of 50 mg/kg, produced a marked analgesic effect, reducing 76 ± 0.9% of the number of abdominal constrictions induced by acetic acid, which may recommend that it can be well absorbed by the gastrointestinal tract. However, it was not effective in abolishing pain in a nonopioid way, showing the lack of antinociceptive effects in the hot-plate test [64]. When verified against the capsaicin test, it provided more direct evidence of the analgesic potential on neurogenic pain, causing an inhibition of 37.3 ± 3.8% at 10 mg/kg of capsaicin-induced licking, signifying its involvement with the antagonism of vanilloid receptor [74].
The specific mechanism underlying the antinociceptive action of marrubiinic acid has yet to be determined, but it is unlikely that it is associated with the interaction of opioid peptides. Although marrubiinic acid displayed lesser analgesic properties than marrubiin, it is more potent than some clinically used drugs. In summary, these results show that it could be used as a model to obtain new and more potent analgesic drugs [67].
In 2013, the analgesic activity of the aqueous extracts obtained from leaves (AEL) and stems (AES) of Rosmarinus officinalis, as well as its isolated compound—rosmarinic acid (RA)—were analyzed by Lucarini et al. [379]. The analysis is based upon abdominal constriction and formalin tests in mice. The extracts were used at doses of 100, 200, and 400 mg·kg−1, and the compounds were tested at 10, 20, and 40 mg·kg−1. Orally administered AEL, AES, and RA were not significantly active at any of the doses tested during the abdominal constriction test; the acetyl ester derivative of RA presented significant analgesic activity. These data recommend that the analgesic effects of the acetyl derivative of RA function through a peripheral-mediated mechanism. The acetyl ester derivative of RA is theoretically applicable as a new lead compound for the management of pain.
Takaki et al. [23] investigated the antinociceptive effects of rosemary essential oil (REO) using the acetic acid-induced writhing and hot-plate tests in mice. REO is very common in folk medicine because of its antispasmodic, analgesic, antirheumatic, and carminative effects. In the hot-plate test, the administration of REO in doses of 125, 250, and 500 mg/kg revealed unremarkable effects on response latency, whereas control injection of meperidine induced significant antinociceptive effects.
Moreover, the REO inhibited licking and shaking induced by formalin injections. Instead, at doses of 70, 125, and 250 mg/kg, REO displayed a substantial antinociceptive effect in the acetic acid-induced abdominal writhing test compared with control animals. The results suggest that REO possesses peripheral antinociceptive activity. Similarly, Martinez et al. [363] described the antinociceptive effect of this essential oil using a rat model of arthritic pain. The essential oil with intraperitoneal administration in doses of 100, 300, and 600 mg/kg determined a dose-dependent antinociceptive effect, manifested as a remarkable reduction of the dysfunction in the pain-induced functional impairment model in the rat, mostly at high doses. Emami et al. [34] indicate that rosemary essential oil can inhibit carrageenan-induced paw edema tests in rats and acetic acid-induced writhing model of visceral pain and hot-plate tests in mice, suggesting that rosemary essential oil possesses anti-inflammatory and peripheral antinociceptive activity [23, 380, 381].
Investigations of the effects of carnosol as one of the constituents of rosemary essential oil extract have also shown that carnosol inhibited LPS-stimulated nitric oxide production (LPS (lipopolysaccharide)) in Raw 264.7 cells and reduced inflammation [382]. Moreover, carnosol inhibited proinflammatory leukotrienes in intact polymorph nuclear leukocytes [383], inhibited 5-lipoxygenase, antagonized mobilization of intracellular calcium ions, and inhibited cyclooxygenase type 2 (COX2) in inflamed skin in male Balb/C mice [384].
A recent work demonstrated that extracts from R. officinalis can control pain by inhibiting its progression during a persistent noxious condition. As an essential characteristic, rosemary extract prevents damage to the nervous system. Thus, rosemary applies effects on the origins of neuropathic pain and offers a mean to directly modulate nervous signaling. The antineuropathic effects are mainly due to the terpenoid fraction in a mecamylamine-reversed manner, suggesting a pharmacodynamic role of nicotinic acetylcholine receptors [385, 386].
Husseini et al. [355] analyzed the effects of L. officinalis hydroalcoholic extract on pain induced by formalin and also cyclooxygenase (COX) type 1 and 2 activity in mice. The administration of the extract intraperitoneally in doses of 100, 200, 250, 300, 400, and 800 mg/kg, respectively, produces significant analgesic and anti-inflammatory activity in the chronic phase of the formalin test and also in hot-plate test in mice with no noted effect on the acute phase of the formalin test.
Moreover, this inhibitory effect is equal to the effects of morphine (10 mg/kg, s.c.), dexamethasone (10 mg/kg, i.p.), and indomethacin (10 mg/kg, i.p.). The extract in doses of 100, 200, and 300 mg/kg significantly reduced heat-induced pain and also reduced COX activity in a dose-dependent manner, where the inhibitory effect on COX1 activity was 33% and on COX2 activity was 45%. Therefore, these results indicate that the possible mechanism of analgesic and anti-inflammatory effects of the extract may be through modulation of COX2 activity.
Other studies [349] have also revealed that the extract of L. officinalis leaves might inhibit the formalin-induced chronic pain, abdomen writhing, and carrageenan-evoked edema. High doses of the essential oils and polyphenolic fraction of L. officinalis have similar effects by blocking acetic acid evoked pain [353]. This pharmacological activity could be derived from the contribution of various active principles composing the whole oil such as linalool, myrcene, and 1–8 cineole, previously proved to possess antinociceptive proprieties [387–389]. However, administration of the essential oil with naloxone, atropine, and mecamylamine could eliminate the analgesic effect of the extract, which indicates that the analgesic activity of the extract is dependent on cholinergic and opioid systems [349].
The antinociceptive and analgesic effects of the essential oil of Mentha spp. (EOM) leaves and its major constituent, piperitenone oxide (PO), were investigated in mice [390]. After an oral administration of 200 mg/kg of EOM and PO, the antinociceptive activity was demonstrated by an important reduction in the acetic acid-induced number of writhings and the second phase of the formalin test, while in the similar range of doses, they did not interfere with the nociception associated with the hot-plate and tail immersion tests. The hot-plate and tail immersion tests are reported to be useful tests in discriminating analgesic agents acting primarily at the spinal medulla level and at higher central nervous system levels (positive results) from those acting through peripheral mechanisms (negative results) [391].
These findings suggest that EOM and PO are acting by peripheral mechanisms. In addition, EOM caused a reduction in the paw licking time for the second phase of the formalin test, when administered at higher doses (100 and 200 mg/kg). At 100 and 200 mg/kg, PO reduced this second phase to 8.3 ± 2.7 s (N = 12) and 3.0 ± 1.2 s (N = 10), respectively. The antinociceptive activity induced by EOM and PO in the writhing and formalin tests was not altered by naloxone, demonstrating that their actions do not depend on opioid receptors [392], supporting the anti-inflammatory hypothesis for their mechanism of action. Thus, it is reasonable to suggest that EOM and PO have an analgesic activity, which is probably indirect and attributed to the anti-inflammatory activity, which does not involve the central nervous system [393].
6. Future Perspectives and Conclusions
The Lamiaceae family includes numerous known species that are used as traditional medicine. The present review summarizes the general aspects, traditional uses, pharmacology, and in vitro and in vivo studies of Betonica officinalis, Glechoma hederacea, Hyptis pectinata, Lavandula genus, Leonurus cardiaca, Lamium genus, Melissa officinalis, Mentha genus, Marrubium vulgare, Origanum genus, Ocimum genus, Rosmarinus officinalis, Salvia genus, Satureja hortensis, Stachys lavandulifolia, Scutellaria lateriflora, Sideritis genus, Teucrium genus, Thymus genus, and Ziziphora tenuior, belonging to Lamiaceae botanical genus. The above-referred studies reported that the abovementioned medicinal plants have potent analgesic and antinociceptive activity. The findings of this review are promising, regarding new potential therapeutic agents with possible modulation in pain therapy. Most of the extracts identified did not present any toxic capabilities or known side effects and were at least as efficient as currently used synthetic drugs. Overall, although promising information evidence the efficacy of Lamiaceae genus in the treatment of pain associated disorders, the data are too preliminary and mostly fail to explain the exact cellular and molecular mechanisms of action and the respective active compounds. Therefore, future studies should be focused on investigating mechanisms of actions, realistic dosages, clinical efficacy, and safety of the extracts and active compounds in pain treatment. This review covers a useful approach for further identification of new compounds from various medicinal plants, which may be effective in pain management.
Conflicts of Interest
The authors declare that there are no conflicts of interest regarding the publication of this paper.
Authors' Contributions
All authors contributed equally to this work.
References
- 1.Masuda R., Ajimi J., Murata T. Pharmacotherapy for neuropathic pain in Japan. 2017;84(6):258–267. doi: 10.1272/jnms.84.258. [DOI] [PubMed] [Google Scholar]
- 2.Tamba B. I., Leon M.-M., Petreus T. Common trace elements alleviate pain in an experimental mouse model. 2013;91(4):554–561. doi: 10.1002/jnr.23191. [DOI] [PubMed] [Google Scholar]
- 3.Iuliana Alexa A., Cantemir A., Ciobica A., et al. Preliminary data regarding decreased catalase specific activity in the tears as a result of environmental stress. 2017;68(1) [Google Scholar]
- 4.Zorina-Lichtenwalter K., Parisien M., Diatchenko L. Genetic studies of human neuropathic pain conditions. 2017:p. 1. doi: 10.1097/j.pain.0000000000001099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gedin F., Skeppholm M., Burström K., Sparring V., Tessma M., Zethraeus N. Effectiveness, costs and cost-effectiveness of chiropractic care and physiotherapy compared with information and advice in the treatment of non-specific chronic low back pain: study protocol for a randomised controlled trial. 2017;18(1):p. 613. doi: 10.1186/s13063-017-2351-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alexa I. D., Pancu A. G., Moroşanu A. I., et al. The impact of self-medication with NSAIDS/analgesics in a north-eastern region of Romania. 2014;62 [Google Scholar]
- 7.Scurrah A., Shiner C. T., Stevens J. A., Faux S. G. Regional nerve blockade for early analgesic management of elderly patients with hip fracture-a narrative review. 2017 doi: 10.1111/anae.14178. In press. [DOI] [PubMed] [Google Scholar]
- 8.Gardikiotis I., Azoicai D., Popa M., Manole A. M., Iorga M. The impact of body image and self-perceived physical ability on the well-being after mastectomy without reconstruction. 2015;11(4):143–149. doi: 10.7438/1584-9341-11-4-5. [DOI] [Google Scholar]
- 9.Luca A., Alexa T., Dondaş A., Crăcană I.-M., Bădescu M., Bohotin C. The effects of riboflavin and methylene blue on nociception and visceral pain. 2015;119(2):466–472. [PubMed] [Google Scholar]
- 10.Cobzaru R., Dumitrescu A.-M., Glodeanu A., Leon M., Constantin S., Luca M. Pain and physical deformity elephantiasis. 2013;117:29–32. [Google Scholar]
- 11.Iurea (Rata) D. M., Popa M., Chailan J.-F., Tamba B. I., Tudorancea I., Peptu C. A. Ibuprofen-loaded chitosan/poly(maleic anhydride-alt-vinyl acetate) submicronic capsules for pain treatment. 2013;28(4):368–384. doi: 10.1177/0883911513490336. [DOI] [Google Scholar]
- 12.Iorga M., Sztankovszky L.-Z., Soponaru C., Gardikiotis I. Pharmacists’ attitude and practices about drug dispensing in Romania. 2015;63(4):601–606. [Google Scholar]
- 13.Ullah R., Ahmad S., Atiq A., et al. Quantification and antibacterial activity of flavonoids in coffee samples. 2015;12(4):p. 84. doi: 10.4314/ajtcam.v12i4.13. [DOI] [Google Scholar]
- 14.Ayaz M., Junaid M., Ullah F., et al. Molecularly characterized solvent extracts and saponins from Polygonum hydropiper L. show high anti-angiogenic, anti-tumor, brine shrimp, and fibroblast NIH/3T3 cell line cytotoxicity. 2016;7:p. 74. doi: 10.3389/fphar.2016.00074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Haq F., Ahmad H., Ullah R., Iqbal Z. Species diversity and ethno botanical classes of the flora of Allai valley District Battagram, Pakistan. 2012;2(4):111–123. doi: 10.5923/j.plant.20120204.03. [DOI] [Google Scholar]
- 16.Anilkumar M. Ethnomedicinal plants as anti-inflammatory and analgesic agents. 2010;37661:267–293. [Google Scholar]
- 17.Alexa-Stratulat T., Luca A., Bădescu M., Bohotin C.-R., Alexa I. D. New York, NY, USA: Elsevier; 2017. Nutritional modulators in chemotherapy-induced neuropathic pain; pp. 9–33. [Google Scholar]
- 18.Tamba B. I., Alexa-Stratulat T. New York, NY, USA: Elsevier; 2017. Trace elements alleviate pain in mice and humans; pp. 199–216. [Google Scholar]
- 19.Peptu C., Rotaru R., Ignat L., et al. Nanotechnology approaches for pain therapy through transdermal drug delivery. 2015;21(42):6125–6139. doi: 10.2174/1381612821666151027152752. [DOI] [PubMed] [Google Scholar]
- 20.Alexa T., Marza A., Voloseniuc T., Tamba B. Enhanced analgesic effects of tramadol and common trace element coadministration in mice. 2015;93(10):1534–1541. doi: 10.1002/jnr.23609. [DOI] [PubMed] [Google Scholar]
- 21.Tamba B. I., Dondas A., Leon M., et al. Silica nanoparticles: preparation, characterization and in vitro/in vivo biodistribution studies. 2015;71:46–55. doi: 10.1016/j.ejps.2015.02.002. [DOI] [PubMed] [Google Scholar]
- 22.Silion M., Hritcu D., Jaba I. M., et al. In vitro and in vivo behavior of ketoprofen intercalated into layered double hydroxides. 2010;21(11):3009–3018. doi: 10.1007/s10856-010-4151-0. [DOI] [PubMed] [Google Scholar]
- 23.Takaki I., Bersani-Amado L. E., Vendruscolo A., et al. Anti-inflammatory and antinociceptive effects of Rosmarinus officinalis L. essential oil in experimental animal models. 2008;11(4):741–746. doi: 10.1089/jmf.2007.0524. [DOI] [PubMed] [Google Scholar]
- 24.Jaba I. M., Vasincu D., Manolidis G., Haulică I., Mungiu O. C. Experimental data regarding the implications of certain minimum structure enkephalin-like peptides in nociceptive processing. 2004;41(1-2):119–126. [PubMed] [Google Scholar]
- 25.Alexa T., Luca A., Dondas A., Bohotin C. R. Preconditioning with cobalt chloride modifies pain perception in mice. 2015;9(10):1465–1469. doi: 10.3892/etm.2015.2235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Luca A., Alexa T., Dondaş A., et al. Pain modulation by curcumin and ascorbic acid in mice. 2015;118(2):346–351. [PubMed] [Google Scholar]
- 27.Ababei D. C., Besche Chiriac S., Bild W., et al. Synergistic effects of the doxepin-candesartan combination on the thermoalgesic sensibility in mice. 2017;65:726–730. [Google Scholar]
- 28.Tamba B. I., Petreus T., Constaintian M.-M. L., Rezus C., Floria M., Rezus E. Heavy metal trace elements induced antinociception in an experimental mouse model. 2015;66(7):976–982. [Google Scholar]
- 29.Kakoti B. B., Pradhan P., Borah S., Mahato K., Kumar M. Analgesic and anti-inflammatory activities of the methanolic stem bark extract of Nyctanthes arbor-tristis Linn. 2013;2013:6. doi: 10.1155/2013/826295.826295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bahmani M., Shirzad H., Majlesi M., Shahinfard N., Rafieian-Kopaei M. A review study on analgesic applications of Iranian medicinal plants. 2014;7:S43–S53. doi: 10.1016/S1995-7645(14)60202-9. [DOI] [PubMed] [Google Scholar]
- 31.Bekut M., Brkić S., Kladar N., Dragović G., Gavarić N., Božin B. Potential of selected Lamiaceae plants in anti(retro)viral therapy. 2017 doi: 10.1016/j.phrs.2017.12.016. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.al-Sereiti M. R., Abu-Amer K. M., Sen P. Pharmacology of rosemary (Rosmarinus officinalis Linn.) and its therapeutic potentials. 1999;37(2):124–130. [PubMed] [Google Scholar]
- 33.Altinier G., Sosa S., Aquino R. P., Mencherini T., Della Loggia R., Tubaro A. Characterization of topical antiinflammatory compounds in Rosmarinus officinalis L. 2007;55(5):1718–1723. doi: 10.1021/jf062610+. [DOI] [PubMed] [Google Scholar]
- 34.Emami F., Ali-Beig H., Farahbakhs S., et al. Hydroalcoholic extract of rosemary (Rosmarinus officinalis L.) and its constituent carnosol inhibit formalin-induced pain and inflammation in mice. 2013;16(7):309–316. doi: 10.3923/pjbs.2013.309.316. [DOI] [PubMed] [Google Scholar]
- 35.Sotelo-Félix J. I., Martinez-Fong D., Muriel P., Santillán R. L., Castillo D., Yahuaca P. Evaluation of the effectiveness of Rosmarinus officinalis (Lamiaceae) in the alleviation of carbon tetrachloride-induced acute hepatotoxicity in the rat. 2002;81(2):145–154. doi: 10.1016/S0378-8741(02)00090-9. [DOI] [PubMed] [Google Scholar]
- 36.Visanji J. M., Thompson D. G., Padfield P. J. Induction of G2/M phase cell cycle arrest by carnosol and carnosic acid is associated with alteration of cyclin A and cyclin B1 levels. 2006;237:130–136. doi: 10.1016/j.canlet.2005.05.045. [DOI] [PubMed] [Google Scholar]
- 37.Okamura N., Haraguchi H., Hashimoto K., Yagi A. Flavonoids in Rosmarinus officinalis leaves. 1994;37(5):1463–1466. doi: 10.1016/S0031-9422(00)90434-5. [DOI] [PubMed] [Google Scholar]
- 38.Señoráns F. J., Ibañez E., Cavero S., Tabera J., Reglero G. Liquid chromatographic-mass spectrometric analysis of supercritical-fluid extracts of rosemary plants. 2000;870(1-2):491–499. doi: 10.1016/S0021-9673(99)00941-3. [DOI] [PubMed] [Google Scholar]
- 39.Thorsen M. A., Hildebrandt K. S. Quantitative determination of phenolic diterpenes in rosemary extracts. Aspects of accurate quantification. 2003;995:119–125. doi: 10.1016/S0021-9673(03)00487-4. [DOI] [PubMed] [Google Scholar]
- 40.Almela L., Sánchez-Muñoz B., Fernández-López J. A., Roca M. J., Rabe V. Liquid chromatograpic–mass spectrometric analysis of phenolics and free radical scavenging activity of rosemary extract from different raw material. 2006;1120(1-2):221–229. doi: 10.1016/j.chroma.2006.02.056. [DOI] [PubMed] [Google Scholar]
- 41.Ramírez P., García-Risco M. R., Santoyo S., Señoráns F. J., Ibáñez E., Reglero G. Isolation of functional ingredients from rosemary by preparative-supercritical fluid chromatography (Prep-SFC) 2006;41(5):1606–1613. doi: 10.1016/j.jpba.2006.02.001. [DOI] [PubMed] [Google Scholar]
- 42.Dörrie J., Sapala K., Zunino S. J. Carnosol-induced apoptosis and downregulation of Bcl-2 in B-lineage leukemia cells. 2001;170(1):33–39. doi: 10.1016/s0304-3835(01)00549-3. [DOI] [PubMed] [Google Scholar]
- 43.Lo A.-H., Liang Y.-C., Lin-Shiau S.-Y., Ho C.-T., Lin J.-K. Carnosol, an antioxidant in rosemary, suppresses inducible nitric oxide synthase through down-regulating nuclear factor-κB in mouse macrophages. 2002;23(6):983–991. doi: 10.1093/carcin/23.6.983. [DOI] [PubMed] [Google Scholar]
- 44.Huang S.-C., Ho C.-T., Lin-Shiau S.-Y., Lin J.-K. Carnosol inhibits the invasion of B16/F10 mouse melanoma cells by suppressing metalloproteinase-9 through down-regulating nuclear factor-κB and c-Jun. 2005;69(2):221–232. doi: 10.1016/j.bcp.2004.09.019. [DOI] [PubMed] [Google Scholar]
- 45.Del Campo J., Amiot M. J., Nguyen-The C. Antimicrobial effect of rosemary extracts. 2000;63(10):1359–1368. doi: 10.4315/0362-028x-63.10.1359. [DOI] [PubMed] [Google Scholar]
- 46.Bozin B., Mimica-Dukic N., Samojlik I., Jovin E. Antimicrobial and antioxidant properties of rosemary and sage (Rosmarinus officinalis L. and Salvia officinalis L., Lamiaceae) essential oils. 2007;55(19):7879–7885. doi: 10.1021/jf0715323. [DOI] [PubMed] [Google Scholar]
- 47.Rasooli I., Fakoor M. H., Yadegarinia D., Gachkar L., Allameh A., Rezaei M. B. Antimycotoxigenic characteristics of Rosmarinus officinalis and Trachyspermum copticum L. essential oils. 2008;122(1-2):135–139. doi: 10.1016/j.ijfoodmicro.2007.11.048. [DOI] [PubMed] [Google Scholar]
- 48.Bernardes W. A., Lucarini R., Tozatti M. G., et al. Antimicrobial activity of Rosmarinus officinalis against oral pathogens: relevance of carnosic acid and carnosol. 2010;7(7):1835–1840. doi: 10.1002/cbdv.200900301. [DOI] [PubMed] [Google Scholar]
- 49.Ouattara B., Simard R. E., Holley R. A., Piette G. J., Bégin A. Antibacterial activity of selected fatty acids and essential oils against six meat spoilage organisms. 1997;37(2-3):155–162. doi: 10.1016/S0168-1605(97)00070-6. [DOI] [PubMed] [Google Scholar]
- 50.Yamamoto J., Yamada K., Naemura A., Yamashita T., Arai R. Testing various herbs for antithrombotic effect. 2005;21(5):580–587. doi: 10.1016/j.nut.2004.09.016. [DOI] [PubMed] [Google Scholar]
- 51.Haloui M., Louedec L., Michel J. B., Lyoussi B. Experimental diuretic effects of Rosmarinus officinalis and Centaurium erythraea. 2000;71(3):465–472. doi: 10.1016/s0378-8741(00)00184-7. [DOI] [PubMed] [Google Scholar]
- 52.Bakırel T., Bakırel U., Keleş O. Ü., Ülgen S. G., Yardibi H. In vivo assessment of antidiabetic and antioxidant activities of rosemary (Rosmarinus officinalis) in alloxan-diabetic rabbits. 2008;116(1):64–73. doi: 10.1016/j.jep.2007.10.039. [DOI] [PubMed] [Google Scholar]
- 53.Fahim F. A., Esmat A. Y., Fadel H. M., Hassan K. F. Allied studies on the effect of Rosmarinus officinalis L. on experimental hepatotoxicity and mutagenesis. 1999;50(6):413–427. doi: 10.1080/096374899100987. [DOI] [PubMed] [Google Scholar]
- 54.Pérez-Fons L., GarzÓn M. T., Micol V. Relationship between the antioxidant capacity and effect of rosemary (Rosmarinus officinalis L.) polyphenols on membrane phospholipid order. 2010;58(1):161–171. doi: 10.1021/jf9026487. [DOI] [PubMed] [Google Scholar]
- 55.Fernandez L., Duque S., Sanchez I., Quiñones D., Rodriguez F., Garcia-Abujeta J. L. Allergic contact dermatitis from rosemary (Rosmarinus officinalis L.) 1997;37(5):248–249. doi: 10.1111/j.1600-0536.1997.tb02455.x. [DOI] [PubMed] [Google Scholar]
- 56.Taamalli A., Arráez-Román D., Ibañez E., Zarrouk M., Segura-Carretero A., Fernández-Gutiérrez A. Optimization of microwave-assisted extraction for the characterization of olive leaf phenolic compounds by using HPLC-ESI-TOF-MS/IT-MS 2. 2012;60(3):791–798. doi: 10.1021/jf204233u. [DOI] [PubMed] [Google Scholar]
- 57.Proestos C., Komaitis M. Application of microwave-assisted extraction to the fast extraction of plant phenolic compounds. 2008;41(4):652–659. doi: 10.1016/j.lwt.2007.04.013. [DOI] [Google Scholar]
- 58.Peng C.-H., Su J.-D., Chyau C.-C., et al. Supercritical fluid extracts of rosemary leaves exhibit potent anti-inflammation and anti-tumor effects. 2007;71(9):2223–2232. doi: 10.1271/bbb.70199. [DOI] [PubMed] [Google Scholar]
- 59.Chan M. M., Ho C. T., Huang H. I. Effects of three dietary phytochemicals from tea, rosemary and turmeric on inflammation-induced nitrite production. 1995;96(1):23–9. doi: 10.1016/0304-3835(95)03913-h. [DOI] [PubMed] [Google Scholar]
- 60.Inoue K.-I., Takano H., Shiga A., et al. Effects of volatile constituents of a rosemary extract on allergic airway inflammation related to house dust mite allergen in mice. 2005;16:315–319. [PubMed] [Google Scholar]
- 61.Inoue K., Takano H., Shiga A., et al. Effects of volatile constituents of rosemary extract on lung inflammation induced by diesel exhaust particles. 2006;99(1):52–57. doi: 10.1111/j.1742-7843.2006.pto_401.x. [DOI] [PubMed] [Google Scholar]
- 62.González-Trujano M. E., Peña E. I., Martínez A. L., et al. Evaluation of the antinociceptive effect of Rosmarinus officinalis L. using three different experimental models in rodents. 2007;111(3):476–482. doi: 10.1016/j.jep.2006.12.011. [DOI] [PubMed] [Google Scholar]
- 63.Meyre-Silva C., Cechinel-Filho V. A review of the chemical and pharmacological aspects of the genus marrubium. 2010;16(31):3503–3518. doi: 10.2174/138161210793563392. [DOI] [PubMed] [Google Scholar]
- 64.De Jesus R. A., Cechinel-Filho V., Oliveira A. E., Schlemper V. Analysis of the antinociceptive properties of marrubiin isolated from Marrubium vulgare. 2000;7(2):111–115. doi: 10.1016/S0944-7113(00)80082-3. [DOI] [PubMed] [Google Scholar]
- 65.Rodrigues C. A., Savi A. O. S., Schlemper V., Reynaud F., Cechinel-Filho V. An improved extraction of marrubiim from Marrubium vulgare. 1998;47(7-8):449–450. doi: 10.1007/BF02466478. [DOI] [Google Scholar]
- 66.de Souza M. M., de Jesus R. A. P., Cechinel-Filho V., Schlemper V. Analgesic profile of hydroalcoholic extract obtained from Marrubium vulgare. 1998;5(2):103–107. doi: 10.1016/S0944-7113(98)80005-6. [DOI] [PubMed] [Google Scholar]
- 67.Meyre-Silva C., Yunes R. A., Schlemper V., Campos-Buzzi F., Cechinel-Filho V. Analgesic potential of marrubiin derivatives, a bioactive diterpene present in Marrubium vulgare (Lamiaceae) 2005;60(4):321–326. doi: 10.1016/j.farmac.2005.01.003. [DOI] [PubMed] [Google Scholar]
- 68.Popoola O., Elbagory A., Ameer F., Hussein A. Marrubiin. 2013;18(8):9049–9060. doi: 10.3390/molecules18089049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Yousefi K., Hamedeyazdan S., Torbati M., Fathiazad F. Vol. 6. Tabriz Univ. Med. Sci; 2016. pp. 131–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Novaes A. P., Rossi C., Poffo C., et al. Preliminary evaluation of the hypoglycemic effect of some Brazilian medicinal plants. 56(4):427–430. [PubMed] [Google Scholar]
- 71.Stulzer H. K., Tagliari M. P., Zampirolo J. A., Cechinel-Filho V., Schlemper V. Antioedematogenic effect of marrubiin obtained from Marrubium vulgare. 2006;108(3):379–84. doi: 10.1016/j.jep.2006.05.023. [DOI] [PubMed] [Google Scholar]
- 72.Herrera-Arellano A., Aguilar-Santamaría L., García-Hernández B., Nicasio-Torres P., Tortoriello J. Clinical trial of Cecropia obtusifolia and Marrubium vulgare leaf extracts on blood glucose and serum lipids in type 2 diabetics. 2004;11(7-8):561–566. doi: 10.1016/j.phymed.2004.01.006. [DOI] [PubMed] [Google Scholar]
- 73.Orhan I. E., Belhattab R., Şenol F. S., Gülpinar A. R., Hoşbaş S., Kartal M. Profiling of cholinesterase inhibitory and antioxidant activities of Artemisia absinthium, A. herba-alba, A. fragrans, Marrubium vulgare, M. astranicum, Origanum vulgare subsp. glandulossum and essential oil analysis of two Artemisia species. 2010;32(3):566–571. doi: 10.1016/j.indcrop.2010.07.005. [DOI] [Google Scholar]
- 74.Julius D., Caterina M. J., Schumacher M. A., Tominaga M., Rosen T. A., Levine J. D. The capsaicin receptor: a heat-activated ion channel in the pain pathway. 1997;389(6653):816–824. doi: 10.1038/39807. [DOI] [PubMed] [Google Scholar]
- 75.Çitoğlu G., Aksit F. Occurence of marrubiin and ladanein in Marrubium trachyticum Boiss. from Turkey. 2002;30(9):885–886. doi: 10.1016/S0305-1978(01)00148-X. [DOI] [Google Scholar]
- 76.Janeska B., Stefova M., Alipieva K. Assay of flavonoid aglycones from the species of genus Sideritis (Lamiaceae) from Macedonia with HPLC-UV DAD. 2007;57(3) doi: 10.2478/v10007-007-0030-8. [DOI] [PubMed] [Google Scholar]
- 77.Knörle R. Extracts of Sideritis scardica as triple monoamine reuptake inhibitors. 2012;119(12):1477–1482. doi: 10.1007/s00702-012-0824-9. [DOI] [PubMed] [Google Scholar]
- 78.Hofrichter J., Krohn M., Schumacher T., et al. Alzheimer’s β-amyloidosis mouse models and aged C57Bl/6 mice. 2016;53(3):967–80. doi: 10.3233/JAD-160301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Stanoeva J. P., Stefova M. Evaluation of the ion trap MS performance for quantification of flavonoids and comparison to UV detection. 2012;47(11):1395–1406. doi: 10.1002/jms.3053. [DOI] [PubMed] [Google Scholar]
- 80.Samanidou V., Tsagiannidis A., Sarakatsianos I. Simultaneous determination of polyphenols and major purine alkaloids in Greek Sideritis species, herbal extracts, green tea, black tea, and coffee by high-performance liquid chromatography-diode array detection. 2012;35(4):608–615. doi: 10.1002/jssc.201100894. [DOI] [PubMed] [Google Scholar]
- 81.Kostadinova E., Nikolova D., Alipieva K., et al. Chemical constituents of the essential oils of Sideritis scardica Griseb. and Sideritis raeseri Boiss and Heldr. from Bulgaria and Macedonia. 2007;21(9):819–823. doi: 10.1080/14786410701394142. [DOI] [PubMed] [Google Scholar]
- 82.Petreska J., Stefkov G., Kulevanova S., Alipieva K., Bankova V., Stefova M. Phenolic compounds of mountain tea from the Balkans: LC/DAD/ESI/MSn profile and content. 2011;6(1):21–30. [PubMed] [Google Scholar]
- 83.Trendafilova A. B., Todorova M. N., Evstatieva L. N., Antonova D. V. Variability in the essential-oil composition of Sideritis scardica Griseb. from native Bulgarian Populations. 2013;10(3):484–492. doi: 10.1002/cbdv.201200282. [DOI] [PubMed] [Google Scholar]
- 84.Qazimi B., Stefkov G., Karapandzova M., Cvetkovikj I., Kulevanova S. Aroma compounds of mountain tea (Sideritis scardica and S. raeseri) from western Balkan. 2014;9:1369–72. [PubMed] [Google Scholar]
- 85.Petreska Stanoeva J., Stefova M. Assay of urinary excretion of polyphenols after ingestion of a cup of mountain tea (Sideritis scardica) measured by HPLC-DAD-ESI-MS/MS. 2013;61(44):10488–10497. doi: 10.1021/jf403052w. [DOI] [PubMed] [Google Scholar]
- 86.González-Burgos E., Carretero M. E., Gómez-Serranillos M. P. Sideritis spp.: uses, chemical composition and pharmacological activities—a review. 2011;135(2):209–225. doi: 10.1016/j.jep.2011.03.014. [DOI] [PubMed] [Google Scholar]
- 87.Ghiciuc C. M., Dima-Cozma L. C., Bercea R. M., et al. Imbalance in the diurnal salivary testosterone/cortisol ratio in men with severe obstructive sleep apnea: an observational study. 2016;82(5):529–535. doi: 10.1016/J.BJORL.2015.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Dimpfel W. Pharmacological classification of herbal extracts by means of comparison to spectral EEG signatures induced by synthetic drugs in the freely moving rat. 2013;149(2):583–589. doi: 10.1016/j.jep.2013.07.029. [DOI] [PubMed] [Google Scholar]
- 89.Mitu O., Roca M., Leon M.-M., Gherasim A., Graur M., Mitu F. Association of health-related quality of life with cardiovascular risk factors and subclinical atherosclerosis in non-diabetic asymptomatic adults. 2016;27 [Google Scholar]
- 90.Tadić V., Bojović D., Arsić I., et al. Chemical and antimicrobial evaluation of supercritical and conventional Sideritis scardica Griseb., Lamiaceae extracts. 2012;17(3):2683–2703. doi: 10.3390/molecules17032683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Danesi F., Saha S., Kroon P. A., et al. Bioactive-rich Sideritis scardica tea (mountain tea) is as potent as Camellia sinensis tea at inducing cellular antioxidant defences and preventing oxidative stress. 2013;93(14):3558–3564. doi: 10.1002/jsfa.6214. [DOI] [PubMed] [Google Scholar]
- 92.Tadić V., Jeremic I., Dobric S., et al. Anti-inflammatory, gastroprotective, and cytotoxic effects of Sideritis scardica extracts. 2012;78(5):415–427. doi: 10.1055/s-0031-1298172. [DOI] [PubMed] [Google Scholar]
- 93.Jeremic I., Tadic V., Isakovic A., et al. The mechanisms of in vitro cytotoxicity of mountain tea, Sideritis scardica, against the C6 glioma cell line. 2013;79:1516–1524. doi: 10.1055/s-0033-1350809. [DOI] [PubMed] [Google Scholar]
- 94.Rezuş E., Grigoriu A., Rezuş C. Aggressive nature of rheumatic arthritis with citrullinated cyclic peptide antibodies. 2009;113(1):73–78. [PubMed] [Google Scholar]
- 95.Todorova M., Trendafilova A. Sideritis scardica Griseb., an endemic species of Balkan peninsula: traditional uses, cultivation, chemical composition, biological activity. 2014;152(2):256–265. doi: 10.1016/j.jep.2014.01.022. [DOI] [PubMed] [Google Scholar]
- 96.Fraga B. M., Hernández M. G., Fernández C., Santana J. M. H. A chemotaxonomic study of nine Canarian Sideritis species. 2009;70(8):1038–1048. doi: 10.1016/j.phytochem.2009.05.011. [DOI] [PubMed] [Google Scholar]
- 97.Hernández-Pérez M., Rabanal Gallego R. M. Analgesic and antiinflammatory properties of Sideritis lotsyi var. Mascaensis. 2002;16(3):264–266. doi: 10.1002/ptr.866. [DOI] [PubMed] [Google Scholar]
- 98.Yavuz D. Ö. Optimization of regeneration conditions and in vitro propagation of Sideritis Stricta Boiss & Heldr. 2016;90:59–62. doi: 10.1016/j.ijbiomac.2015.10.064. [DOI] [PubMed] [Google Scholar]
- 99.Kilic T. Isolation and biological activity of new and known isolation and biological activity of new and known diterpenoids from Sideritis stricta Boiss. & Heldr. 2006;11(4):257–262. doi: 10.3390/11040257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Küpeli E., Sahin F. P., Yeşilada E., Caliş I., Ezer N. In vivo anti-inflammatory and antinociceptive activity evaluation of phenolic compounds from Sideritis stricta. 2007;62(7-8):519–525. doi: 10.1515/znc-2007-7-810. [DOI] [PubMed] [Google Scholar]
- 101.Kang C.-H., Molagoda I. M. N., Choi Y. H., Park C., Moon D.-O., Kim G.-Y. Apigenin promotes TRAIL-mediated apoptosis regardless of ROS generation. 2018;111:623–630. doi: 10.1016/j.fct.2017.12.018. [DOI] [PubMed] [Google Scholar]
- 102.Schmidt E., Wanner J., Hiiferl M., et al. Chemical composition, olfactory analysis and antibacterial activity of Thymus vulgaris chemotypes geraniol, 4-thujanol/terpinen-4-ol, thymol and linalool cultivated in southern France. 2012;7:1095–1098. [PubMed] [Google Scholar]
- 103.Vaičiulytė V., Butkienė R., Ložienė K. Effects of meteorological conditions and plant growth stage on the accumulation of carvacrol and its precursors in Thymus pulegioides. 2016;128:20–26. doi: 10.1016/j.phytochem.2016.03.018. [DOI] [PubMed] [Google Scholar]
- 104.Satyal P., Murray B. L., McFeeters R. L., Setzer W. N. Essential oil characterization of Thymus vulgaris from various geographical locations. 2016;5(4):p. 78. doi: 10.3390/foods5040070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Tsuchiya H. Hironori, anesthetic agents of plant origin: a review of phytochemicals with anesthetic Activity. 2017;22(8):p. 1369. doi: 10.3390/molecules22081369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Akram M., Rashid A. Anti-coagulant activity of plants: mini review. 2017;44(3):406–411. doi: 10.1007/s11239-017-1546-5. [DOI] [PubMed] [Google Scholar]
- 107.Okazaki K., Kawazoe K., Takaishi Y. Human platelet aggregation inhibitors from thyme (Thymus vulgaris L.) 2002;16(4):398–399. doi: 10.1002/ptr.979. [DOI] [PubMed] [Google Scholar]
- 108.Soosaraei M., Fakhar M., Hosseini Teshnizi S., Ziaei Hezarjaribi H., Banimostafavi E. S. Medicinal plants with promising antileishmanial activity in Iran: a systematic review and meta-analysis. 2017;21:63–80. doi: 10.1016/j.amsu.2017.07.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Ebadollahi A., Sendi J. J., Aliakbar A. Efficacy of nanoencapsulated Thymus eriocalyx and Thymus kotschyanus essential oils by a mesoporous material MCM-41 against Tetranychus urticae (Acari: Tetranychidae) 2017;110(6):2413–2420. doi: 10.1093/jee/tox234. [DOI] [PubMed] [Google Scholar]
- 110.Schönknecht K., Krauss H., Jambor J., Fal A. M. Treatment of cough in respiratory tract infections-the effect of combining the natural active compounds with thymol. 2016;69(6):791–798. [PubMed] [Google Scholar]
- 111.Ayrle H., Mevissen M., Kaske M., et al. Medicinal plants–prophylactic and therapeutic options for gastrointestinal and respiratory diseases in calves and piglets? A systematic review. 2016;12(1):p. 89. doi: 10.1186/s12917-016-0714-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Wan L., Meng D., Wang H., et al. Preventive and therapeutic effects of thymol in a lipopolysaccharide-induced acute lung injury mice model. 2017;41(1) doi: 10.1007/s10753-017-0676-4. [DOI] [PubMed] [Google Scholar]
- 113.Vigo E., Cepeda A., Perez-Fernandez R., Gualillo O. In-vitro anti-inflammatory effect of Eucalyptus globulus and Thymus vulgaris : nitric oxide inhibition in J774A.1 murine macrophages. 2004;56(2):257–263. doi: 10.1211/0022357022665. [DOI] [PubMed] [Google Scholar]
- 114.Kindl M., Blažeković B., Bucar F., Vladimir-Knežević S. Antioxidant and anticholinesterase potential of six Thymus species. 2015;2015:10. doi: 10.1155/2015/403950.403950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Alabdullatif M., Boujezza I., Mekni M., et al. Enhancing blood donor skin disinfection using natural oils. 2017;57(12):2920–2927. doi: 10.1111/trf.14298. [DOI] [PubMed] [Google Scholar]
- 116.Basch E., Ulbricht C., Hammerness P., Bevins A., Sollars D. Thyme (Thymus vulgaris L.), thymol. 2004;4(1):49–67. doi: 10.1300/j157v04n01_07. [DOI] [PubMed] [Google Scholar]
- 117.El Zayyat E. A., Soliman M. I., Elleboudy N. A., Ofaa S. E. Bioefficacy of some Egyptian aromatic plants on Culex pipiens (Diptera: Culicidae) adults and larvae. 2017;11(1):147–155. [PMC free article] [PubMed] [Google Scholar]
- 118.Qadir M. I., Parveen A., Abbas K., Ali M. Analgesic, anti-inflammatory and anti-pyretic activities of Thymus linearis. 2016;29(2):591–594. [PubMed] [Google Scholar]
- 119.Taherian A. A., Babaei M., Vafaei A. A., Jarrahi M., Jadidi M., Sadeghi H. Antinociceptive effects of hydroalcoholic extract of Thymus vulgaris. 2009;22:83–89. [PubMed] [Google Scholar]
- 120.Salmalian H., Saghebi R., Moghadamnia A. A., et al. Comparative effect of Thymus vulgaris and ibuprofen on primary dysmenorrhea: a triple-blind clinical study. 2014;5(2):82–88. [PMC free article] [PubMed] [Google Scholar]
- 121.Orłowska M., Stanimirova I., Staszek D., Sajewicz M., Kowalska T., Waksmundzka-Hajnos M. Optimization of extraction based on the thin-layer chromatographic fingerprints of common thyme. 2014;97(5):1274–1281. doi: 10.5740/jaoacint.SGEOrlowska. [DOI] [PubMed] [Google Scholar]
- 122.Pinto E., Pina-Vaz C., Salgueiro L., et al. Antifungal activity of the essential oil of Thymus pulegioides on Candida, Aspergillus and Dermatophyte species. 2006;55(10):1367–1373. doi: 10.1099/jmm.0.46443-0. [DOI] [PubMed] [Google Scholar]
- 123.Vitalini S., Iriti M., Puricelli C., Ciuchi D., Segale A., Fico G. Traditional knowledge on medicinal and food plants used in Val San Giacomo (Sondrio, Italy)—an alpine ethnobotanical study. 2013;145(2):517–529. doi: 10.1016/j.jep.2012.11.024. [DOI] [PubMed] [Google Scholar]
- 124.Schaffer S., Eckert G. P., Müller W. E., et al. Hypochlorous acid scavenging properties of local Mediterranean plant foods. 2004;39(12):1239–1247. doi: 10.1007/s11745-004-1353-9. [DOI] [PubMed] [Google Scholar]
- 125.Stalińska K., Guzdek A., Rokicki M., Koj A. Transcription factors as targets of the anti-inflammatory treatment. A cell culture study with extracts from some Mediterranean diet plants. 2005;56(1):157–169. [PubMed] [Google Scholar]
- 126.Novak J., Bahoo L., Mitteregger U., Franz C. Composition of individual essential oil glands of savory (Satureja hortensis L., Lamiaceae) from Syria. 2006;21(4):731–734. doi: 10.1002/ffj.1725. [DOI] [Google Scholar]
- 127.Momtaz S., Abdollahi M. An update on pharmacology of Satureja species; from antioxidant, antimicrobial, antidiabetes and anti-hyperlipidemic to reproductive stimulation. 2010;6:454–461. doi: 10.3923/ijp.2010.346.353. [DOI] [Google Scholar]
- 128.Tepe B., Cilkiz M. A pharmacological and phytochemical overview on Satureja. 2016;54(3):375–412. doi: 10.3109/13880209.2015.1043560. [DOI] [PubMed] [Google Scholar]
- 129.Nikaein F., Babajafari S., Mazloomi S., et al. The effects of Satureja hortensis L. Dried leaves on serum sugar, lipid profiles, hs-CRP, and blood pressure in metabolic syndrome patients: a double-blind randomized clinical trial. 2017;19(1):p. e34931. doi: 10.5812/ircmj.34931. [DOI] [Google Scholar]
- 130.Jafari F., Ghavidel F., Zarshenas M. M. A critical overview on the pharmacological and clinical aspects of popular Satureja species. 2016;9(3):118–127. doi: 10.1016/j.jams.2016.04.003. [DOI] [PubMed] [Google Scholar]
- 131.Mašković P., Veličković V., Mitić M., et al. Summer savory extracts prepared by novel extraction methods resulted in enhanced biological activity. 2017;109:875–881. doi: 10.1016/J.INDCROP.2017.09.063. [DOI] [Google Scholar]
- 132.Ceker S., Agar G., Alpsoy L., Nardemir G., Kizil H. E. Antagonistic effects of Satureja hortensis essential oil against AFB, on human lymphocytes in vitro. 2014;48(5):327–332. doi: 10.3103/S0095452714050028. [DOI] [PubMed] [Google Scholar]
- 133.Hajhashem V., Zolfaghari B., Yousefi A. Antinociceptive and anti-inflammatory activities of Satureja hortensis seed essential oil, hydroalcoholic and polyphenolic extracts in animal models. 2012;21(2):178–182. doi: 10.1159/000333555. [DOI] [PubMed] [Google Scholar]
- 134.Mohammadhosseini M., Akbarzadeh A., Hashemi-Moghaddam H. Gas chromatographic-mass spectrometric analysis of volatiles obtained by HS-SPME-GC-MS technique from Stachys lavandulifolia and evaluation for biological activity: a review. 2016;19(6):1300–1327. doi: 10.1080/0972060X.2016.1221741. [DOI] [Google Scholar]
- 135.Javidnia K., Mojab F., Mojahedi S. A. Chemical constituents of the essential oil of Stachys lavandulifolia Vahl from Iran. 2003;19(6):174–178. doi: 10.1080/0972-060X.2003.10643347. [DOI] [Google Scholar]
- 136.Pirbalouti A. G., Mohammadi M. Phytochemical composition of the essential oil of different populations of Stachys lavandulifolia Vahl. 2013;3(2):123–128. doi: 10.1016/S2221-1691(13)60036-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Rouzbeh L. Antimicrobial activity and chemical composition of essential oils of Stachys lavandulifolia Vahl. from Mazandaran, Iran. 2012;6(24):4149–4158. doi: 10.5897/JMPR12.734. [DOI] [Google Scholar]
- 138.Oztürk M., Duru M. E., Aydoğmuş-Oztürk F., et al. GC-MS analysis and antimicrobial activity of essential oil of Stachys cretica subsp. smyrnaea. 2009;4(1):109–114. [PubMed] [Google Scholar]
- 139.Minae B., Sardari M., Sharifi H., Sedigh Rahim Abadi M., Sadeghpour O. Stachys lavandulifolia Vahl. and its relation with marmazad activities in traditional manuscripts. 2015;17(11):p. e19932. doi: 10.5812/ircmj.19932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Modarresi M., Hosseinzadeh L., Nematy N., Siavash-Haghighi Z. M., Ghanbari K. Acute and subchronic toxicological evaluation of Stachys lavandulifolia aqueous extract in Wistar rats. 2014;9(3):165–72. [PMC free article] [PubMed] [Google Scholar]
- 141.Hajhashemi V., Ghannadi A., Sedighifar S. Analgesic and anti-inflammatory properties of the hydroalcoholic, polyphenolic and boiled extracts of Stachys lavandulifolia. 2007;1:92–98. [Google Scholar]
- 142.Barreto R. S. S., Quintans J. S. S., Amarante R. K. L. R. S., et al. Evidence for the involvement of TNF-α and IL-1β in the antinociceptive and anti-inflammatory activity of Stachys lavandulifolia Vahl. (Lamiaceae) essential oil and (-)-α-bisabolol, its main compound, in mice. 2016;191:9–18. doi: 10.1016/j.jep.2016.06.022. [DOI] [PubMed] [Google Scholar]
- 143.Háznagy-Radnai E., Balogh Á., Czigle S., Máthé I., Hohmann J., Blazsó G. Antiinflammatory activities of Hungarian Stachys species and their iridoids. 2012;26(4):505–509. doi: 10.1002/ptr.3582. [DOI] [PubMed] [Google Scholar]
- 144.Skaltsa H. D., Demetzos C., Lazari D., Sokovic M. Essential oil analysis and antimicrobial activity of eight Stachys species from Greece. 2003;64(3):743–752. doi: 10.1016/S0031-9422(03)00386-8. [DOI] [PubMed] [Google Scholar]
- 145.Paun G., Neagu E., Albu C., Moroeanu V., Radu G.-L. Antioxidant activity and inhibitory effect of polyphenolic-rich extract from Betonica officinalis and Impatiens noli-tangere herbs on key enzyme linked to type 2 diabetes. 2016;60:1–7. doi: 10.1016/j.jtice.2015.10.005. [DOI] [Google Scholar]
- 146.Šliumpaitė I., Venskutonis P. R., Murkovic M., Ragažinskienė O. Antioxidant properties and phenolic composition of wood betony (Betonica officinalis L., syn. Stachys officinalis L.) 2013;50:715–722. doi: 10.1016/j.indcrop.2013.08.024. [DOI] [Google Scholar]
- 147.Russo E. Binghamton, NY, USA: Haworth Herbal Press; 2001. [Google Scholar]
- 148.Conforti F., Menichini F., Formisano C., et al. Comparative chemical composition, free radical-scavenging and cytotoxic properties of essential oils of six Stachys species from different regions of the Mediterranean area. 2009;116(4):898–905. doi: 10.1016/j.foodchem.2009.03.044. [DOI] [Google Scholar]
- 149.Paun G., Neagu E., Moroeanu V., et al. Phytochemical analysis and in vitro biological activity of Betonica officinalis and Salvia officinalis extracts. 2017;22(4) [Google Scholar]
- 150.Matkowski A., Piotrowska M. Antioxidant and free radical scavenging activities of some medicinal plants from the Lamiaceae. 2006;77(5):346–353. doi: 10.1016/j.fitote.2006.04.004. [DOI] [PubMed] [Google Scholar]
- 151.Maleki N., Garjani A., Nazemiyeh H., et al. Potent anti-inflammatory activities of hydroalcoholic extract from aerial parts of Stachys inflata on rats. 2001;75(2-3):213–218. doi: 10.1016/S0378-8741(01)00194-5. [DOI] [PubMed] [Google Scholar]
- 152.Khanavi M., Sharifzadeh M., Hadjiakhoondi A., Shafiee A. Phytochemical investigation and anti-inflammatory activity of aerial parts of Stachys byzanthina C. Koch. 2005;97(3):463–468. doi: 10.1016/j.jep.2004.11.037. [DOI] [PubMed] [Google Scholar]
- 153.Wang Y.-Y., Lin S.-Y., Chen W.-Y., et al. Glechoma hederacea extracts attenuate cholestatic liver injury in a bile duct-ligated rat model. 2017;204:58–66. doi: 10.1016/j.jep.2017.04.011. [DOI] [PubMed] [Google Scholar]
- 154.Kim J., Song S., Lee I., et al. Anti-inflammatory activity of constituents from Glechoma hederacea var. longituba. 2011;21(11):3483–3487. doi: 10.1016/j.bmcl.2011.02.002. [DOI] [PubMed] [Google Scholar]
- 155.Ohigashi H., Takamura H., Koshimizu K., Tokuda H., Ito Y. Search for possible antitumor promoters by inhibition of 12-O-tetradecanoylphorbol-13-acetate-induced Epstein-Barr virus activation; ursolic acid and oleanolic acid from an anti-inflammatory Chinese medicinal plant, Glechoma hederacea L. 1986;30(2):143–151. doi: 10.1016/0304-3835(86)90082-0. [DOI] [PubMed] [Google Scholar]
- 156.Kühn H., Wiesner R., Alder L., Schewe T. Occurrence of free and esterified lipoxygenase products in leaves of Glechoma hederacea L. and other Labiatae. 1989;186(1-2):155–62. doi: 10.1111/j.1432-1033.1989.tb15190.x. [DOI] [PubMed] [Google Scholar]
- 157.Singh T., Wu J. H., Peumans W. J., et al. Carbohydrate specificity of an insecticidal lectin isolated from the leaves of Glechoma hederacea (ground ivy) towards mammalian glycoconjugates. 2006;393(1):331–41. doi: 10.1042/BJ20051162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Kumarasamy Y., Cox P. J., Jaspars M., Nahar L., Sarker S. D. Biological activity of Glechoma hederacea. 2002;73(7-8):721–723. doi: 10.1016/S0367-326X(02)00237-X. [DOI] [PubMed] [Google Scholar]
- 159.An H.-J., Jeong H.-J., Um J.-Y., Kim H.-M., Hong S.-H. Glechoma hederacea inhibits inflammatory mediator release in IFN-γ and LPS-stimulated mouse peritoneal macrophages. 2006;106(3):418–424. doi: 10.1016/j.jep.2006.01.024. [DOI] [PubMed] [Google Scholar]
- 160.Hwang J. K., Erkhembaatar M., Gu D. R., et al. Glechoma hederacea suppresses RANKL-mediated osteoclastogenesis. 2014;93(7):685–690. doi: 10.1177/0022034514536579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Milovanovic M., Zivkovic D., Vucelic-Radovic B. Antioxidant effects of Glechoma hederacea as a food additive. 2010;5(1):61–63. [PubMed] [Google Scholar]
- 162.Belščak-Cvitanović A., Durgo K., Bušić A., Franekić J., Komes D. Phytochemical attributes of four conventionally extracted medicinal plants and cytotoxic evaluation of their extracts on human laryngeal carcinoma (HEp2) cells. 2014;17(2):206–217. doi: 10.1089/jmf.2013.0071. [DOI] [PubMed] [Google Scholar]
- 163.Miron I., Diaconescu S., Aprodu G., Ioniuc I., Diaconescu M. R., Miron L. Diagnostic difficulties in a pediatric insulinoma. 2016;95(11):p. e3045. doi: 10.1097/MD.0000000000003045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Brock C., Whitehouse J., Tewfik I., Towell T. American skullcap (Scutellaria lateriflora): a randomised, double-blind placebo-controlled crossover study of its effects on mood in healthy volunteers. 2014;28(5):692–698. doi: 10.1002/ptr.5044. [DOI] [PubMed] [Google Scholar]
- 165.Brock C., Whitehouse J., Tewfik I., Towell T. American skullcap (Scutellaria lateriflora): an ancient remedy for today’s anxiety? 2010;1(4):25–30. doi: 10.12968/bjow.2010.1.4.49168. [DOI] [Google Scholar]
- 166.Gao J., Sanchez-Medina A., Pendry B. A., Hughes M. J., Webb G. P., Corcoran O. Validation of a HPLC method for flavonoid biomarkers in skullcap (Scutellaria) and its use to illustrate wide variability in the quality of commercial tinctures. 2008;11(1):77–87. doi: 10.18433/j39g6v. [DOI] [PubMed] [Google Scholar]
- 167.Li J., Wang Y.-H., Smillie T. J., Khan I. A. Identification of phenolic compounds from Scutellaria lateriflora by liquid chromatography with ultraviolet photodiode array and electrospray ionization tandem mass spectrometry. 2012;63:120–127. doi: 10.1016/j.jpba.2012.01.027. [DOI] [PubMed] [Google Scholar]
- 168.Rhudy J. L., Meagher M. W. Fear and anxiety: divergent effects on human pain thresholds. 2000;84(1):65–75. doi: 10.1016/s0304-3959(99)00183-9. [DOI] [PubMed] [Google Scholar]
- 169.Lohani M., Ahuja M., Buabeid M. A., et al. Anti-oxidative and DNA protecting effects of flavonoids-rich Scutellaria lateriflora. 2013;8:1415–1418. [PubMed] [Google Scholar]
- 170.Awad R., Arnason J. T., Trudeau V., et al. Phytochemical and biological analysis of skullcap (Scutellaria lateriflora L.): a medicinal plant with anxiolytic properties. 2003;10(8):640–649. doi: 10.1078/0944-7113-00374. [DOI] [PubMed] [Google Scholar]
- 171.Gafner S., Bergeron C., Batcha L. L., et al. Inhibition of [3H]-LSD binding to 5-HT7 receptors by flavonoids from Scutellaria lateriflora. 2003;66(4):535–537. doi: 10.1021/NP0205102. [DOI] [PubMed] [Google Scholar]
- 172.Jianjun J., Huiru D. Preparation of high-purity baicalein from Scutellaria baicalensis Georgi. 2008;22(16):1410–1412. doi: 10.1080/14786410701823967. [DOI] [PubMed] [Google Scholar]
- 173.Lin C.-C., Shieh D.-E. The anti-inflammatory activity of Scutellaria rivularis extracts and its active components, baicalin, baicalein and wogonin. 1996;24(1):31–36. doi: 10.1142/S0192415X96000050. [DOI] [PubMed] [Google Scholar]
- 174.Yoo S., Han S., Park Y. S., Lee J.-H., Oh U., Hwang S. W. Lipoxygenase inhibitors suppressed carrageenan-induced Fos-expression and inflammatory pain responses in the rat. 2009;27(4):417–422. doi: 10.1007/s10059-009-0059-2. [DOI] [PubMed] [Google Scholar]
- 175.Yimam M., Brownell L., Hodges M., Jia Q. Analgesic effects of a standardized bioflavonoid composition from Scutellaria baicalensis and Acacia catechu. 2012;9(3):155–65. doi: 10.3109/19390211.2012.708713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Cherng C.-H., Lee K.-C., Chien C.-C., et al. Baicalin ameliorates neuropathic pain by suppressing HDAC1 expression in the spinal cord of spinal nerve ligation rats. 2014;113(8):513–520. doi: 10.1016/j.jfma.2013.04.007. [DOI] [PubMed] [Google Scholar]
- 177.Hu S., Chen Y., Wang Z.-F., et al. The analgesic and antineuroinflammatory effect of baicalein in cancer-induced bone pain, evidence-based complement. 2015;2015:8. doi: 10.1155/2015/973524.973524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Pinzariu A. C., Pasca S. A., Sindilar A., et al. Adipose tissue remodeling by prolonged administration of high dose of vitamin D3 in rats treated to prevent sarcopenia. 2017;68:2139–2143. [Google Scholar]
- 179.Deschamps J. D., Kenyon V. A., Holman T. R. Baicalein is a potent in vitro inhibitor against both reticulocyte 15-human and platelet 12-human lipoxygenases. 2006;14:4295–4301. doi: 10.1016/j.bmc.2006.01.057. [DOI] [PubMed] [Google Scholar]
- 180.Hsieh C.-J., Hall K., Ha T., Li C., Krishnaswamy G., Chi D. S. Baicalein inhibits IL-1β- and TNF-α-induced inflammatory cytokine production from human mast cells via regulation of the NF-κB pathway. 2007;5(1):p. 5. doi: 10.1186/1476-7961-5-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Wakabayashi I. Inhibitory effects of baicalein and wogonin on lipopolysaccharide-induced nitric oxide production in macrophages. 1999;84(6):288–91. doi: 10.1111/j.1600-0773.1999.tb01496.x. [DOI] [PubMed] [Google Scholar]
- 182.Woo K. J., Lim J. H., Suh S.-I., et al. Differential inhibitory effects of baicalein and baicalin on LPS-induced cyclooxygenase-2 expression through inhibition of C/EBPβ DNA-binding activity. 2006;211(5):359–368. doi: 10.1016/j.imbio.2006.02.002. [DOI] [PubMed] [Google Scholar]
- 183.Kumar M., Kasala E. R., Bodduluru L. N., Dahiya V., Lahkar M. Baicalein protects isoproterenol induced myocardial ischemic injury in male Wistar rats by mitigating oxidative stress and inflammation. 2016;65(8):613–622. doi: 10.1007/s00011-016-0944-z. [DOI] [PubMed] [Google Scholar]
- 184.Xie Y., Song X., Sun X., et al. Identification of baicalein as a ferroptosis inhibitor by natural product library screening. 2016;473(4):775–780. doi: 10.1016/j.bbrc.2016.03.052. [DOI] [PubMed] [Google Scholar]
- 185.de Carvalho R. S. M., Duarte F. S., de Lima T. C. M. Involvement of GABAergic non-benzodiazepine sites in the anxiolytic-like and sedative effects of the flavonoid baicalein in mice. 2011;221(1):75–82. doi: 10.1016/j.bbr.2011.02.038. [DOI] [PubMed] [Google Scholar]
- 186.Yin H., Bhattarai J. P., Oh S. M., Park S. J., Ahn D. K., Han S. K. Baicalin activates glycine and γ-aminobutyric acid receptors on substantia gelatinosa neurons of the trigeminal subsnucleus caudalis in juvenile mice. 2016;44(2):389–400. doi: 10.1142/S0192415X16500221. [DOI] [PubMed] [Google Scholar]
- 187.Woo A., Cheng C., Waye M. Baicalein protects rat cardiomyocytes from hypoxia/reoxygenation damage via a prooxidant mechanism. 2005;65(1):244–253. doi: 10.1016/j.cardiores.2004.09.027. [DOI] [PubMed] [Google Scholar]
- 188.Mahajan N., Rawal S., Verma M., Poddar M., Alok S. A phytopharmacological overview on Ocimum species with special emphasis on Ocimum sanctum. 2013;3(2):185–192. doi: 10.1016/J.BIONUT.2012.08.002. [DOI] [Google Scholar]
- 189.Kaur G., Jaggi A. S., Singh N. Exploring the potential effect of Ocimum sanctum in vincristine-induced neuropathic pain in rats. 2010;5:p. 3. doi: 10.1186/1749-7221-5-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Muthuraman A., Diwan V., Jaggi A. S., Singh N., Singh D. Ameliorative effects of Ocimum sanctum in sciatic nerve transection-induced neuropathy in rats. 2008;120(1):56–62. doi: 10.1016/j.jep.2008.07.049. [DOI] [PubMed] [Google Scholar]
- 191.Bhattacharyya P., Bishayee A. Ocimum sanctum Linn. (Tulsi): an ethnomedicinal plant for the prevention and treatment of cancer. 2013;24(7):659–66. doi: 10.1097/CAD.0b013e328361aca1. [DOI] [PubMed] [Google Scholar]
- 192.Mondal S., Varma S., Bamola V. D., et al. Double-blinded randomized controlled trial for immunomodulatory effects of Tulsi (Ocimum sanctum Linn.) leaf extract on healthy volunteers. 2011;136:452–456. doi: 10.1016/j.jep.2011.05.012. [DOI] [PubMed] [Google Scholar]
- 193.Choudhury S. S., Bashyam L., Manthapuram N., Bitla P., Kollipara P., Tetali S. D. Ocimum sanctum leaf extracts attenuate human monocytic (THP-1) cell activation. 2014;154(1):148–155. doi: 10.1016/j.jep.2014.03.049. [DOI] [PubMed] [Google Scholar]
- 194.Singh S., Majumdar D. K., Rehan H. M. Evaluation of anti-inflammatory potential of fixed oil of Ocimum sanctum (holybasil) and its possible mechanism of action. 1996;54(1):19–26. doi: 10.1016/0378-8741(96)83992-4. [DOI] [PubMed] [Google Scholar]
- 195.Gupta D., Bhaskar D., Gupta R., et al. A randomized controlled clinical trial of Ocimum sanctum and chlorhexidine mouthwash on dental plaque and gingival inflammation. 2014;5:p. 109. doi: 10.4103/0975-9476.131727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Kaur G., Bali A., Singh N., Jaggi A. S. Ameliorative potential of Ocimum sanctum in chronic constriction injury-induced neuropathic pain in rats. 2015;87(1):417–429. doi: 10.1590/0001-3765201520130008. [DOI] [PubMed] [Google Scholar]
- 197.Ahmad A., Khan M. M., Raza S. S., et al. Ocimum sanctum attenuates oxidative damage and neurological deficits following focal cerebral ischemia/reperfusion injury in rats. 2012;33(6):1239–1247. doi: 10.1007/s10072-012-0940-1. [DOI] [PubMed] [Google Scholar]
- 198.Okiemy-Andissa N., Miguel M., Etou A., Ouamba J., Gbeassor M., Abena A. Analgesic effect of aqueous and hydroalcoholic extracts of three congolese medicinal plants: Hyptis suavolens, Nauclea latifolia and Ocimum gratissimum. 2004;7(9):1613–1615. doi: 10.3923/pjbs.2004.1613.1615. [DOI] [Google Scholar]
- 199.Paula-Freire L., Molska G., Andersen M., Carlini E. Ocimum gratissimum essential oil and its isolated compounds (eugenol and myrcene) reduce neuropathic pain in mice. 2015;82(3):211–216. doi: 10.1055/s-0035-1558165. [DOI] [PubMed] [Google Scholar]
- 200.Igbinosa E. O., Uzunuigbe E. O., Igbinosa I. H., Odjadjare E. E., Igiehon N. O., Emuedo O. A. In vitro assessment of antioxidant, phytochemical and nutritional properties of extracts from the leaves of Ocimum gratissimum (Linn) 2013;10(5):292–298. doi: 10.4314/ajtcam.v10i5.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Paula-Freire L. I. G., Andersen M. L., Molska G. R., Köhn D. O., Carlini E. L. A. Evaluation of the antinociceptive activity of Ocimum gratissimum l. (Lamiaceae) essential oil and its isolated active principles in mice. 2013;27(8):1220–1224. doi: 10.1002/ptr.4845. [DOI] [PubMed] [Google Scholar]
- 202.Rabelo M., Souza E. P., Soares P. M. G., Miranda A. V., Matos F. J. A., Criddle D. N. Antinociceptive properties of the essential oil of Ocimum gratissimum L. (Labiatae) in mice. 2003;36(4):521–524. doi: 10.1590/s0100-879x2003000400016. [DOI] [PubMed] [Google Scholar]
- 203.Paula-Freire L. I. G., Andersen M. L., Gama V. S., Molska G. R., Carlini E. L. A. The oral administration of trans-caryophyllene attenuates acute and chronic pain in mice. 2014;21(3):356–362. doi: 10.1016/j.phymed.2013.08.006. [DOI] [PubMed] [Google Scholar]
- 204.Katsuyama S., Mizoguchi H., Kuwahata H., et al. Involvement of peripheral cannabinoid and opioid receptors in β-caryophyllene-induced antinociception. 2013;17(5):664–675. doi: 10.1002/j.1532-2149.2012.00242.x. [DOI] [PubMed] [Google Scholar]
- 205.de Pinho J., Silva A., Pinheiro B., et al. Antinociceptive and antispasmodic effects of the essential oil of Ocimum micranthum : potential anti-inflammatory properties. 2012;78(7):681–685. doi: 10.1055/s-0031-1298372. [DOI] [PubMed] [Google Scholar]
- 206.Akkol E. K., Yalçın F. N., Kaya D., Çalış İ., Yesilada E., Ersöz T. In vivo anti-inflammatory and antinociceptive actions of some Lamium species. 2008;118(1):166–172. doi: 10.1016/j.jep.2008.04.001. [DOI] [PubMed] [Google Scholar]
- 207.Alipieva K., Evstatieva L., Handjieva N., Popov S. Comparative analysis of the composition of flower volatiles from Lamium L. species and Lamiastrum galeobdolon Heist. ex Fabr. 2003;58(11-12):779–782. doi: 10.1515/znc-2003-11-1204. [DOI] [PubMed] [Google Scholar]
- 208.Bahramikia S., Yazdanparast R. Phytochemistry and medicinal properties of Teucrium polium L. (Lamiaceae) 2012;26(11):1581–1593. doi: 10.1002/ptr.4617. [DOI] [PubMed] [Google Scholar]
- 209.Abadian K., Keshavarz Z., Mojab F., Alavi Majd H., Abbasi N. M. Comparison the effect of mefenamic acid and Teucrium polium on the severity and systemic symptoms of dysmenorrhea. 2016;22:12–15. doi: 10.1016/j.ctcp.2015.09.003. [DOI] [PubMed] [Google Scholar]
- 210.Purnavab S., Ketabchi S., Rowshan V. Chemical composition and antibacterial activity of methanolic extract and essential oil of Iranian Teucrium polium against some of phytobacteria. 2015;29(14):1376–1379. doi: 10.1080/14786419.2014.1000320. [DOI] [PubMed] [Google Scholar]
- 211.Baluchnejadmojarad T., Roghani M., Roghani-Dehkordi F. Antinociceptive effect of Teucrium polium leaf extract in the diabetic rat formalin test. 2005;97(2):207–210. doi: 10.1016/j.jep.2004.10.030. [DOI] [PubMed] [Google Scholar]
- 212.Tariq M., Ageel A. M., al-Yahya M. A., Mossa J. S., al-Said M. S. Anti-inflammatory activity of Teucrium polium. 1989;11(4):185–188. [PubMed] [Google Scholar]
- 213.Shahraki M., MirShekari H., Palan M. J. The comparison of nociceptive effect of Teucrium polium and morphine in female rats. 2006;12(1):10–14. [Google Scholar]
- 214.Abdollahi M., Karimpour H., Monsef-Esfehani H. R. Antinociceptive effects of Teucrium polium L total extract and essential oil in mouse writhing test. 2003;48:31–35. [PubMed] [Google Scholar]
- 215.Farshchi A., Ghiasi G., Asl A. A. Antinociceptive and antiinflammatory effects of Teucrium hyrcanicum aqueous extract in male mice and rats. 2010;14(1):78–84. [Google Scholar]
- 216.Golfakhrabadi F., Yousefbeyk F., Mirnezami T., Laghaei P., Hajimahmoodi M., Khanavi M. Antioxidant and antiacetylcholinesterase activity of Teucrium hyrcanicum. 2015;7(5):S15–S19. doi: 10.4103/0974-8490.157993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Nencini C., Galluzzi P., Pippi F., Menchiari A., Micheli L. Hepatotoxicity of Teucrium chamaedrys L. decoction: role of difference in the harvesting area and preparation method. 2014;46(2):181–184. doi: 10.4103/0253-7613.129313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Prescott T. A. K., Veitch N. C., Simmonds M. S. J. Direct inhibition of calcineurin by caffeoyl phenylethanoid glycosides from Teucrium chamaedrys and Nepeta cataria. 2011;137(3):1306–1310. doi: 10.1016/j.jep.2011.07.063. [DOI] [PubMed] [Google Scholar]
- 219.Falcao R. A., do Nascimento P. L. A., de Souza S. A., et al. Antileishmanial phenylpropanoids from the leaves of Hyptis pectinata (L.) Poit. 2013;2013:p. 460613. doi: 10.1155/2013/460613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Bordignon S. A. de L. Hyptis tetracephala (Labiatae), nova espécie do sul do Brasil. 1992;8:1–3. [Google Scholar]
- 221.Harley R. In: Proc. a Work. Neotrop. Distrib. Patterns. Vanzolini P., Heyer W., editors. Rio de Janeiro, Brazil: Academia Brasileira de Ciências; 1988. pp. 71–121. [Google Scholar]
- 222.Bispo M. D., Mourão R. H., Franzotti E. M., et al. Antinociceptive and antiedematogenic effects of the aqueous extract of Hyptis pectinata leaves in experimental animals. 2001;76(1):81–86. doi: 10.1016/s0378-8741(01)00172-6. [DOI] [PubMed] [Google Scholar]
- 223.Paixão M. S., Melo M. S., Damascena N. P., et al. Hyptis pectinata gel prevents alveolar bone resorption in experimental periodontitis in rats. 2015;25(1):35–41. doi: 10.1016/j.bjp.2014.12.002. [DOI] [Google Scholar]
- 224.Paixão M. S., Melo M. S., Oliveira M. G. B., et al. Hyptis pectinata: redox protection and orofacial antinociception. 2013;27(9):1328–1333. doi: 10.1002/ptr.4869. [DOI] [PubMed] [Google Scholar]
- 225.Melo G. B., Silva R. L., Melo V. A., et al. Enhancement of liver regeneration by the association of Hyptis pectinata with laser therapy. 2005;50(5):949–954. doi: 10.1007/s10620-005-2670-1. [DOI] [PubMed] [Google Scholar]
- 226.Arrigoni-Blank M. F., Silva-Mann R., Campos D. A., et al. Morphological, agronomical and pharmacological characterization of Hyptis pectinata (L.) Poit germplasm. 2005;15(4):298–303. doi: 10.1590/S0102-695X2005000400007. [DOI] [Google Scholar]
- 227.Liapi C., Anifandis G., Anifantis G., et al. Antinociceptive properties of 1,8-cineole and beta-pinene, from the essential oil of Eucalyptus camaldulensis leaves, in rodents. 2007;73(12):1247–54. doi: 10.1055/s-2007-990224. [DOI] [PubMed] [Google Scholar]
- 228.Franco C. R. P., Antoniolli Â. R., Guimarães A. G., et al. Bioassay-guided evaluation of antinociceptive properties and chemical variability of the essential oil of Hyptis fruticosa. 2011;25(11):1693–1699. doi: 10.1002/ptr.3455. [DOI] [PubMed] [Google Scholar]
- 229.Raymundo L. J. R. P., Guilhon C. C., Alviano D. S., et al. Characterisation of the anti-inflammatory and antinociceptive activities of the Hyptis pectinata (L.) Poit essential oil. 2011;134(3):725–732. doi: 10.1016/j.jep.2011.01.027. [DOI] [PubMed] [Google Scholar]
- 230.Sarmento-Neto J. F., Do Nascimento L. G., Felipe C. F. B., De Sousa D. P. Analgesic potential of essential oils. 2016;21:1–29. doi: 10.3390/molecules21010020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Khare C. P. New York, NY, USA: Springer New York; 2007. [DOI] [Google Scholar]
- 232.Agata I., Kusakabe H., Hatano T., Nishibe S., Okuda T. Melitric acids A and B, new trimeric caffeic acid derivatives from Melissa officinalis. 1993;41(9):1608–1611. doi: 10.1248/cpb.41.1608. [DOI] [Google Scholar]
- 233.Triantaphyllou K., Blekas G., Boskou D. Antioxidative properties of water extracts obtained from herbs of the species Lamiaceae. 2001;52(4):313–317. doi: 10.1080/09637480120057512. [DOI] [PubMed] [Google Scholar]
- 234.Felklová M., Nátherová L., Dusková K. Tannin compounds in leaves of Melissa officinalis L., invaded by Septoria melissae Desm. 1969;18(9):457–460. [PubMed] [Google Scholar]
- 235.Mrlianová M., Tekel’ová D., Felklová M., Reinöhl V., Tóth J. The influence of the harvest cut height on the quality of the herbal drugs Melissae folium and Melissae herba. 2002;68(2):178–80. doi: 10.1055/s-2002-20247. [DOI] [PubMed] [Google Scholar]
- 236.Patora J., Majda T., Góra J., Klimek B. Variability in the content and composition of essential oil from lemon balm (Melissa officinalis L.) cultivated in Poland. 2003;60(5):395–400. [PubMed] [Google Scholar]
- 237.Mikus J., Harkenthal M., Steverding D., Reichling J. In vitro effect of essential oils and isolated mono- and sesquiterpenes on Leishmania major and Trypanosoma brucei. 2000;66(4):366–368. doi: 10.1055/s-2000-8548. [DOI] [PubMed] [Google Scholar]
- 238.Brieskorn C. H., Krause W. Further triterpenes from Melissa officinalis L (author’s transl) 1974;307(8):603–12. doi: 10.1002/ardp.19743070805. [DOI] [PubMed] [Google Scholar]
- 239.Sarer E., Kökdil G. Constituents of the essential oil from Melissa officinalis. 1991;57(1):89–90. doi: 10.1055/s-2006-960032. [DOI] [PubMed] [Google Scholar]
- 240.Herrmann E. C., Kucera L. S. Antiviral substances in plants of the mint family (Labiatae). II. Nontannin polyphenol of Melissa officinalis. 1967;124:869–874. doi: 10.3181/00379727-124-31873. [DOI] [PubMed] [Google Scholar]
- 241.Lawrence M. S., Stojanov P., Polak P., et al. Mutational heterogeneity in cancer and the search for new cancer-associated genes. 2013;499(7457):214–218. doi: 10.1038/nature12213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Yamasaki K., Nakano M., Kawahata T., et al. Anti-HIV-1 activity of herbs in Labiatae. 1998;21(8):829–833. doi: 10.1248/bpb.21.829. [DOI] [PubMed] [Google Scholar]
- 243.Iauk L., Lo Bue A. M., Milazzo I., Rapisarda A., Blandino G. Antibacterial activity of medicinal plant extracts against periodontopathic bacteria. 2003;17(6):599–604. doi: 10.1002/ptr.1188. [DOI] [PubMed] [Google Scholar]
- 244.Englberger W., Hadding U., Etschenberg E., et al. Rosmarinic acid: a new inhibitor of complement C3-convertase with anti-inflammatory activity. 1988;10(6):729–737. doi: 10.1016/0192-0561(88)90026-4. [DOI] [PubMed] [Google Scholar]
- 245.Auf’mkolk M., Ingbar J. C., Amir S. M., et al. Inhibition by certain plant extracts of the binding and adenylate cyclase stimulatory effect of bovine thyrotropin in human thyroid membranes. 1984;115(2):527–534. doi: 10.1210/endo-115-2-527. [DOI] [PubMed] [Google Scholar]
- 246.Soulimani R., Fleurentin J., Mortier F., Misslin R., Derrieu G., Pelt J. M. Neurotropic action of the hydroalcoholic extract of Melissa officinalis in the mouse. 1991;57(2):105–109. doi: 10.1055/s-2006-960042. [DOI] [PubMed] [Google Scholar]
- 247.Gazola R., Machado D., Ruggiero C., Singi G., Macedo Alexandre M. Lippia alba, Melissa officinalis and Cymbopogon citratus: effects of the aqueous extracts on the isolated hearts of rats. 2004;50(5):477–480. doi: 10.1016/j.phrs.2004.01.012. [DOI] [PubMed] [Google Scholar]
- 248.Anca T., Alin Constantin P., Roxana Gabriela C., et al. Toxic effects of magnesium nitrate on cardiac muscle tissue of Gallus domesticus embryos and chicks. 2017;68:1343–1349. [Google Scholar]
- 249.Sahin F., Güllüce M. C., Daferera D., et al. Biological activities of the essential oils and methanol extract of Origanum vulgare in the Eastern Anatolia region of Turkey. 2004;15(7):549–557. doi: 10.1016/j.foodcont.2003.08.009. [DOI] [Google Scholar]
- 250.Prerna P., Vasudeva N. Origanum majorana L.phyto-pharmacological review. 2015;6:261–267. [Google Scholar]
- 251.Barazandeh M. Identification of the essential oil composition from Origanum majorana L. 2000;14:38–40. [Google Scholar]
- 252.Melegari M., Severi F., Bertoldi M., et al. Chemical characterization of essential oils of some Origanum vulgare L. subspecies of various origin. 1995;16(4):21–28. doi: 10.1590/1983-084x/10_120. [DOI] [Google Scholar]
- 253.Baranauskienė R., Venskutonis P. R., Dambrauskienė E., Viškelis P. Harvesting time influences the yield and oil composition of Origanum vulgare L. ssp. vulgare and ssp. hirtum. 2013;49:43–51. doi: 10.1016/j.indcrop.2013.04.024. [DOI] [Google Scholar]
- 254.Tahmasebi S., Majd A., Mehrafarin A., Jonoubi P. Comparative ontogenetic survey of the essential oil composition in Origanum vulgare L., and Origanum majorana L. 2016;60:105–111. [Google Scholar]
- 255.Dorman H. J., Deans S. G. Antimicrobial agents from plants: antibacterial activity of plant volatile oils. 2000;88(2):308–316. doi: 10.1046/j.1365-2672.2000.00969.x. [DOI] [PubMed] [Google Scholar]
- 256.Novák I., Zámbori-Németh É., Horváth H., Seregély Z., Kaffka K. Study of essential oil components in different Origanum species by GC and sensory analysis. 2003;32(2):141–150. doi: 10.1556/AAlim.32.2003.2.3. [DOI] [Google Scholar]
- 257.Lakhrissi B., Boukhraz A., Barrahi M., El H., Ouhssine M. Antifungal activity of essential oil of oregano (Origanum vulgare) 2016;3:14–17. [Google Scholar]
- 258.Marino M., Bersani C., Comi G. Impedance measurements to study the antimicrobial activity of essential oils from Lamiaceae and Compositae. 2001;67(3):187–95. doi: 10.1016/s0168-1605(01)00447-0. [DOI] [PubMed] [Google Scholar]
- 259.Baydar H., Sagdic O., Ozkan G., Karadogan T. Antibacterial activity and composition of essential oils from Origanum, Thymbra and Sartureja species with commercial importance in Turkey. 2004;15(3):169–172. doi: 10.1016/s0956-7135(03)00028-8. [DOI] [Google Scholar]
- 260.Cano J. H., Volpato G. Herbal mixtures in the traditional medicine of eastern Cuba. 2004;90(2-3):293–316. doi: 10.1016/j.jep.2003.10.012. [DOI] [PubMed] [Google Scholar]
- 261.Vági E., Simándi B., Suhajda Á., Héthelyi É. Essential oil composition and antimicrobial activity of Origanum majorana L. extracts obtained with ethyl alcohol and supercritical carbon dioxide. 2005;38(1):51–57. doi: 10.1016/j.foodres.2004.07.006. [DOI] [Google Scholar]
- 262.Floria M., Drug V. L. Atrial fibrillation and gastroesophageal reflux disease: from the cardiologist perspective. 2015;21(10):3154–3156. doi: 10.3748/wjg.v21.i10.3154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Floria M., Blommaert D., Lacrosse M., et al. Assessment of left atrial shape and volume in structural remodeling secondary to atrial fibrillation. 2009;25(3):167–170. doi: 10.1007/s10840-008-9349-4. [DOI] [PubMed] [Google Scholar]
- 264.Floria M., Barboi O., Rezus C., et al. Atrial fibrillation and gastro-oesophageal reflux disease-controversies and challenges. 2015;21(26):3829–3834. doi: 10.2174/1381612821666150319100003. [DOI] [PubMed] [Google Scholar]
- 265.Rezus E., Floria M., Grigoriu A., Tamba B. I., Rezus C. Cardiovascular risk factors in chronic inflammatory rheumatic diseases: modern assessment and diagnosis. 2015;13(6):716–724. doi: 10.2174/1570161113666150105112820. [DOI] [PubMed] [Google Scholar]
- 266.Talebi S., Rezakhanlou A., Isfahani G. S. Trichome plasticity in Ziziphora tenuior L. (Labiatae) in Iran: an ecological review. 2012;3:668–672. [Google Scholar]
- 267.Senejoux F., Girard C., Kerram P., et al. Mechanisms of vasorelaxation induced by Ziziphora clinopodioides Lam. (Lamiaceae) extract in rat thoracic aorta. 2010;132(1):268–273. doi: 10.1016/j.jep.2010.08.028. [DOI] [PubMed] [Google Scholar]
- 268.Azadmehr A., Latifi R., Mosalla S., Hajiaghaee R., Shahnazi M. Immunomodulatory effects of Ziziphora tenuior L. extract on the dendritic cells. 2014;22(1):p. 63. doi: 10.1186/s40199-014-0063-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Gharetapeh H. H., Maleki S. A., Asgharpanah J. Antidepressant effects of Ziziphora tenuior L. hydroalcoholic extract in animal models of depression. 2014;3(6):664–668. [Google Scholar]
- 270.Michielin E. M. Z., Salvador A. A., Riehl C. A. S., Smânia A., Smânia E. F. A., Ferreira S. R. S. Chemical composition and antibacterial activity of Cordia verbenacea extracts obtained by different methods. 2009;100(24):6615–6623. doi: 10.1016/j.biortech.2009.07.061. [DOI] [PubMed] [Google Scholar]
- 271.Ahmed U., Rahman A. U. Amsterdam, Netherlands: Elsevier; 1994. [Google Scholar]
- 272.Shiow-Yunn S., Feng-Lin H., Yu-Chan L. Two gallates from Quercus glauca. 1992;31(7):2465–2468. doi: 10.1016/0031-9422(92)83300-N. [DOI] [Google Scholar]
- 273.Voirin B. UV spectral differentiation of 5-hydroxy- and 5-hydroxy-3-methoxyflavones with mono-(4′), di-(3′,4′) or tri-(3′,4′,5′)-substituted B rings. 1983;22:2107–2145. doi: 10.1016/S0031-9422(00)80133-8. [DOI] [Google Scholar]
- 274.Mehmood R., Imran M., Malik A., Tareen R. B. Ziziphorins A and B. new flavonoids from Ziziphora tenuior. 2010;65(11):1397–1400. doi: 10.1002/chin.201110211. [DOI] [Google Scholar]
- 275.Darbandi T., Honarvar B., Sinaei M., Rezaei A. Extraction of Ziziphora tenuior essential oil using supercritical CO2. 2013;2(3):687–695. [Google Scholar]
- 276.Pirbalouti A. G., Amirkhosravi A., Bordbar F., Hamedi B. Diversity in the chemical composition of essential oils of Ziziphora tenuior as a potential source of pulegone. 2013;24(3):234–239. [Google Scholar]
- 277.Fu Z. H., Wang H., Hu X., Sun Z., Han C. The pharmacological properties of Salvia essential oils. 2013;3(7):122–127. doi: 10.7324/japs.2013.3723. [DOI] [Google Scholar]
- 278.Szentmihályi K., Csedo C., Then M. Comparative study on tannins, flavonoids, terpenes and mineral elements of some Salvia species. 2004;629:463–470. [Google Scholar]
- 279.Russo A., Formisano C., Rigano D., et al. Chemical composition and anticancer activity of essential oils of Mediterranean sage (Salvia officinalis L.) grown in different environmental conditions. 2013;55:42–47. doi: 10.1016/j.fct.2012.12.036. [DOI] [PubMed] [Google Scholar]
- 280.Coisin M., Necula R., Grigoras V., Gille E., Rosenhech E., Zamfirache M. Phytochemical evaluation of some Salvia species from Romanian flora. 2012;58(1):35–44. [Google Scholar]
- 281.Pop (Cuceu) A.-V., Maria T., Sonia S. A., et al. Comparative study regarding the chemical composition of essential oils of some salvia species. 2014 [Google Scholar]
- 282.Zhang R.-H., Liu Z.-K., Yang D.-S., Zhang X.-J., Sun H.-D., Xiao W.-L. Phytochemistry and pharmacology of the genus Leonurus : the herb to benefit the mothers and more. 2018;147:167–183. doi: 10.1016/j.phytochem.2017.12.016. [DOI] [PubMed] [Google Scholar]
- 283.Wojtyniak K., Szymański M., Matławska I. Leonurus cardiaca L. (Motherwort): a review of its phytochemistry and pharmacology. 2013;27(8):1115–1120. doi: 10.1002/ptr.4850. [DOI] [PubMed] [Google Scholar]
- 284. Motherwort Benefits, Uses and Side Effects, Assessment report on Leonurus cardiaca L., herba EMA/HMPC/127430/2010.
- 285.Wichtl M. Guildford, UK: Medpharm; 2004. [Google Scholar]
- 286.Agnihotri V., ElSohly H., Smillie T., Khan I., Walker L. New Labdane diterpenes from Leonurus cardiaca. 2008;74(3):1288–1290. doi: 10.1055/s-2008-1081304. [DOI] [PubMed] [Google Scholar]
- 287.Janicsák G., Veres K., Zoltán Kakasy A., Máthé I. Study of the oleanolic and ursolic acid contents of some species of the Lamiaceae. 2006;34(5):392–396. doi: 10.1016/J.BSE.2005.12.004. [DOI] [Google Scholar]
- 288.Miłkowska-Leyck K., Filipek B., Strzelecka H. Pharmacological effects of lavandulifolioside from Leonurus cardiaca. 2002;80(1):85–90. doi: 10.1016/s0378-8741(02)00016-8. [DOI] [PubMed] [Google Scholar]
- 289.Bernatoniene J., Kucinskaite A., Masteikova R., Kalveniene Z., Kasparaviciene G., Savickas A. The comparison of anti-oxidative kinetics in vitro of the fluid extract from maidenhair tree, motherwort and hawthorn. 2009;66(4):415–421. [PubMed] [Google Scholar]
- 290.Morteza-Semnani K., Saeedi M., Akbarzadeh M. The essential oil composition of Leonurus cardiaca L. 2008;20:107–109. doi: 10.1080/10412905.2008.9699966. [DOI] [Google Scholar]
- 291.Mockutë D., Bernotienë G., Judþentienë A. Storage-induced changes in essential oil composition of Leonurus cardiaca L. plants growing wild in Vilnius and of commercial herbs. 2005;16(2):29–32. [Google Scholar]
- 292.Sattar A. A., Bankova V., Kujumgiev A., et al. Chemical composition and biological activity of leaf exudates from some Lamiaceae plants. 1995;50:62–65. [PubMed] [Google Scholar]
- 293.Jafari S., Moradi A., Salaritabar A., Hadjiakhoondi A., Khanavi M. Determination of total phenolic and flavonoid contents of Leonurus cardiaca L. in compare with antioxidant activity. 2010;5:484–487. [Google Scholar]
- 294.Ali M. S., Ibrahim S. A., Jalil S., Choudhary M. I. Ursolic acid: a potent inhibitor of superoxides produced in the cellular system. 2007;21(6):558–561. doi: 10.1002/ptr.2108. [DOI] [PubMed] [Google Scholar]
- 295.Song X., Wang T., Zhang Z., et al. Leonurine exerts anti-inflammatory effect by regulating inflammatory signaling pathways and cytokines in LPS-induced mouse mastitis. 2015;38:79–88. doi: 10.1007/s10753-014-0009-9. [DOI] [PubMed] [Google Scholar]
- 296.Rezaee-Asl M., Sabour M., Nikoui V., et al. The study of analgesic effects of Leonurus cardiaca L. in mice by formalin, tail flick and hot plate tests. 2014;2014:1–5. doi: 10.1155/2014/687697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297.Qi J., Hong Z. Y., Xin H., Zhu Y. Z. Neuroprotective effects of leonurine on ischemia/reperfusion-induced mitochondrial dysfunctions in rat cerebral cortex. 2010;33(12):1958–1964. doi: 10.1248/bpb.33.1958. [DOI] [PubMed] [Google Scholar]
- 298.Ovanesov K. B., Ovanesova I. M., Arushanian E. B. Effects of melatonin and motherwort tincture on the emotional state and visual functions in anxious subjects. 2006;69(6):17–9. [PubMed] [Google Scholar]
- 299.Tao J., Zhang P., Liu G., et al. Cytotoxicity of Chinese motherwort (YiMuCao) aqueous ethanol extract is non-apoptotic and estrogen receptor independent on human breast cancer cells. 2009;122:234–239. doi: 10.1016/j.jep.2009.01.013. [DOI] [PubMed] [Google Scholar]
- 300.Tachjian A., Maria V. Use of herbal products and potential interactions in patients with cardiovascular diseases. 2011;55(6):515–525. doi: 10.1016/j.jacc.2009.07.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 301.Bunsawat J., Elliott N. E., Hertweck K. L., Sproles E., Alice L. A. Phylogenetics of Mentha (Lamiaceae): evidence from chloroplast DNA sequences. 2004;29(4):959–964. doi: 10.1600/0363644042450973. [DOI] [Google Scholar]
- 302.McKay D. L., Blumberg J. B. A review of the bioactivity and potential health benefits of peppermint tea (Mentha piperita L.) 2006;20(8):619–633. doi: 10.1002/ptr.1936. [DOI] [PubMed] [Google Scholar]
- 303.McKay D. L., Blumberg J. B. A review of the bioactivity and potential health benefits of peppermint tea (Mentha piperita L.) 2006;20(8):619–633. doi: 10.1002/ptr.1936. [DOI] [PubMed] [Google Scholar]
- 304.Gherman C., Culea M., Cozar O. Comparative analysis of some active principles of herb plants by GC/MS. 2000;53(1):253–262. doi: 10.1016/s0039-9140(00)00458-6. [DOI] [PubMed] [Google Scholar]
- 305.Pino J. A., Borges P., Martinez M. A., et al. Essential oil of Mentha piperita L. grown in Jalisco. 2002;14(3):189–190. doi: 10.1080/10412905.2002.9699820. [DOI] [Google Scholar]
- 306.Ruiz del Castillo M. L., Santa-María G., Herraiz M., Blanch G. P. A comparative study of the ability of different techniques to extract menthol from Mentha piperita. 2003;41(7):385–389. doi: 10.1093/chromsci/41.7.385. [DOI] [PubMed] [Google Scholar]
- 307.Blanco M. C. S. G., Ming L. C., Marques M. O. M., Bovi O. A. Drying temperature effects in peppermint essential oil content and composition. 2002;(569):95–98. doi: 10.17660/ActaHortic.2002.569.15. [DOI] [Google Scholar]
- 308.Maffei M., Scannerini S. Seasonal variations in fatty acids from non-polar lipids of developing peppermint leaves. 1992;31(2):479–484. doi: 10.1016/0031-9422(92)90020-Q. [DOI] [Google Scholar]
- 309.Clark R. J., Menary R. C. Variations in composition of peppermint oil in relation to production areas. 1981;35(1):59–69. doi: 10.1007/BF02859215. [DOI] [Google Scholar]
- 310.Fatih B., Madani K., Chibane M., Duez P. Bronx, NY, USA: InTech; 2017. Chemical composition and biological activities of Mentha species. [DOI] [Google Scholar]
- 311.Capecka E., Mareczek A., Leja M. Antioxidant activity of fresh and dry herbs of some Lamiaceae species. 2005;93(2):223–226. doi: 10.1016/j.foodchem.2004.09.020. [DOI] [Google Scholar]
- 312.Lozak A., Sołtyk K., Ostapczuk P., Fijałek Z. Determination of selected trace elements in herbs and their infusions. 2002;289(1–3):33–40. doi: 10.1016/s0048-9697(01)01015-4. [DOI] [PubMed] [Google Scholar]
- 313.ScienceDirect F. M., Valenta˜o P., Andrade P. B., Ferreres F., Seabra R. M. London, UK: Applied Science Publishers; 2001. [Google Scholar]
- 314.Zheng W., Wang S. Y. Antioxidant activity and phenolic compounds in selected herbs. 2001;49(11):5165–5170. doi: 10.1021/JF010697N. [DOI] [PubMed] [Google Scholar]
- 315.Gavahian M., Farahnaky A., Farhoosh R., Javidnia K., Shahidi F. Extraction of essential oils from Mentha piperita using advanced techniques: microwave versus ohmic assisted hydrodistillation. 2015;94:50–58. doi: 10.1016/j.fbp.2015.01.003. [DOI] [Google Scholar]
- 316.Kaufmann B., Christen P. Recent extraction techniques for natural products: microwave-assisted extraction and pressurised solvent extraction. 2002;13(2):105–113. doi: 10.1002/pca.631. [DOI] [PubMed] [Google Scholar]
- 317.Wang L., Weller C. L. Recent advances in extraction of nutraceuticals from plants. 2006;17(6):300–312. doi: 10.1016/j.tifs.2005.12.004. [DOI] [Google Scholar]
- 318.Mason T. J., Chemat F., Vinatoru M. The extraction of natural products using ultrasound or microwaves. 2011;15(2):237–247. doi: 10.2174/138527211793979871. [DOI] [Google Scholar]
- 319.Petigny L., Périno S., Minuti M., Visinoni F., Wajsman J., Chemat F. Simultaneous microwave extraction and separation of volatile and non-volatile organic compounds of boldo leaves. From lab to industrial scale. 2014;15(5):7183–7198. doi: 10.3390/ijms15057183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 320.Dragland S., Senoo H., Wake K., Holte K., Blomhoff R. Several culinary and medicinal herbs are important sources of dietary antioxidants. 2003;133(5):1286–1290. doi: 10.1093/jn/133.5.1286. [DOI] [PubMed] [Google Scholar]
- 321.Abirami S. K. G., Nirmala P. A comparative–invitro study of anticancer effect of Mentha piperita, Ocimum basilicum and Coleus aromaticus against human laryngeal epidermoid carcinoma (HEP-2) cell lines. 2014;2(1) [Google Scholar]
- 322.Ferreira P., Cardoso T., Ferreira F., Fernandes-Ferreira M., Piper P., Sousa M. J. Mentha piperita essential oil induces apoptosis in yeast associated with both cytosolic and mitochondrial ROS-mediated damage. 2014;14 doi: 10.1111/1567-1364.12189. [DOI] [PubMed] [Google Scholar]
- 323.Inoue T., Sugimoto Y., Masuda H., Kamei C. Antiallergic effect of flavonoid glycosides obtained from Mentha piperita L. 2002;25(2):256–259. doi: 10.1248/bpb.25.256. [DOI] [PubMed] [Google Scholar]
- 324.Sato A., Tamura H. High antiallergic activity of 5,6,4′-trihydroxy-7,8,3′-trimethoxyflavone and 5,6-dihydroxy-7,8,3′,4′-tetramethoxyflavone from eau de cologne mint (Mentha × piperita citrata) 2015;102:74–83. doi: 10.1016/j.fitote.2015.02.003. [DOI] [PubMed] [Google Scholar]
- 325.Schuhmacher A., Reichling J., Schnitzler P. Virucidal effect of peppermint oil on the enveloped viruses herpes simplex virus type 1 and type 2 in vitro. 2003;10(6-7):504–510. doi: 10.1078/094471103322331467. [DOI] [PubMed] [Google Scholar]
- 326.Omidian J., Sheikhi-Shooshtari F., Fazeli M. Inhibitory effect of Mentha Piperita extracts against herpes simplex virus isolated from eye infection. 2014;8(1):35–41. doi: 10.21859/isv.8.1.35. [DOI] [Google Scholar]
- 327.Singh R., Shushni M. A. M., Belkheir A. Antibacterial and antioxidant activities of Mentha piperita L. 2015;8(3):322–328. doi: 10.1016/j.arabjc.2011.01.019. [DOI] [Google Scholar]
- 328.Horváth P., Koščová J. In vitro antibacterial activity of Mentha essential oils against Staphylococcus aureus. 2017;61(3):71–77. doi: 10.1515/fv-2017-0030. [DOI] [Google Scholar]
- 329.Inouye S., Yamaguchi H., Takizawa T. Screening of the antibacterial effects of a variety of essential oils on respiratory tract pathogens, using a modified dilution assay method. 2001;7(4):251–254. doi: 10.1007/s101560170022. [DOI] [PubMed] [Google Scholar]
- 330.Shahbazi Y. Chemical composition and in vitro antibacterial activity of Mentha spicata essential oil against common food-borne pathogenic bacteria. 2015;2015:5. doi: 10.1155/2015/916305.916305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 331.Rasooli I., Owlia P., Taghizadeh M., Astaneh S. D. A., Sharafi S. M. Protective effects of bioactive phytochemicals from Mentha piperita with multiple health potentials. 2010;6(23):147–153. doi: 10.4103/0973-1296.66926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 332.Maliakal P. P., Wanwimolruk S. Effect of herbal teas on hepatic drug metabolizing enzymes in rats. 2001;53(10):1323–1329. doi: 10.1211/0022357011777819. [DOI] [PubMed] [Google Scholar]
- 333.Khalil A. F., Elkatry H. O., El Mehairy H. F. Protective effect of peppermint and parsley leaves oils against hepatotoxicity on experimental rats. 2015;60(2):353–359. doi: 10.1016/J.AOAS.2015.11.004. [DOI] [Google Scholar]
- 334.Ullah N., Khan M. A., Khan T., Asif A. H., Ahmad W. Mentha piperita in nephrotoxicity–a possible intervention to ameliorate renal derangements associated with gentamicin. 2014;46(2):166–170. doi: 10.4103/0253-7613.129309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 335.Atta A. H., Alkofahi A. Anti-nociceptive and anti-inflammatory effects of some Jordanian medicinal plant extracts. 1998;60(2):117–124. doi: 10.1016/s0378-8741(97)00137-2. [DOI] [PubMed] [Google Scholar]
- 336.Taher Y. A. Antinociceptive activity of Mentha piperita leaf aqueous extract in mice. 2012;7(1):p. 16205. doi: 10.3402/ljm.v7i0.16205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 337.Atta A. H., EL-Sooud K. A. The antinociceptive effect of some Egyptian medicinal plant extracts. 2004;95(2-3):235–238. doi: 10.1016/j.jep.2004.07.006. [DOI] [PubMed] [Google Scholar]
- 338.Moreno L., Bello R., Primo-Yúfera E., Esplugues J. Pharmacological properties of the methanol extract from Mentha suaveolens Ehrh. 2002;16(1):S10–S13. doi: 10.1002/ptr.744. [DOI] [PubMed] [Google Scholar]
- 339.Nair B. Final report on the safety assessment of Mentha piperita (peppermint) oil, Mentha piperita (peppermint) leaf extract, Mentha piperita (peppermint) leaf, and Mentha piperita (peppermint) leaf water. 2001;20(3):61–73. doi: 10.1080/10915810152902592. [DOI] [PubMed] [Google Scholar]
- 340.Yousuf P. M. H., Noba N. Y., Shohel M., Bhattacherjee R., Das B. K. Analgesic, anti-inflammatory and antipyretic effect of Mentha spicata (Spearmint) 2013;3(4):854–864. doi: 10.9734/bjpr/2014/4640. [DOI] [Google Scholar]
- 341.Amabeoku G. J., Erasmus S. J., Ojewole J. A. O., Mukinda J. T. Antipyretic and antinociceptive properties of Mentha longifolia Huds. (Lamiaceae) leaf aqueous extract in rats and mice. 2009;31(10):p. 645. doi: 10.1358/mf.2009.31.10.1441861. [DOI] [PubMed] [Google Scholar]
- 342.Biswas N. N., Saha S., Ali M. K. Antioxidant, antimicrobial, cytotoxic and analgesic activities of ethanolic extract of Mentha arvensis L. 2014;4(10):792–797. doi: 10.12980/APJTB.4.2014C1298. [DOI] [Google Scholar]
- 343.Adorjan B., Buchbauer G. Biological properties of essential oils: an updated review. 2010;25(6):407–426. doi: 10.1002/ffj.2024. [DOI] [Google Scholar]
- 344.Nicolai M., Pereira P., Vitor R. F., Reis C. P., Roberto A., Rijo P. Antioxidant activity and rosmarinic acid content of ultrasound-assisted ethanolic extracts of medicinal plants. 2016;89:328–332. doi: 10.1016/j.measurement.2016.04.033. [DOI] [Google Scholar]
- 345.Duda S. C., Mărghitaş L. A., Dezmirean D., Duda M., Mărgăoan R., Bobiş O. Changes in major bioactive compounds with antioxidant activity of Agastache foeniculum, Lavandula angustifolia, Melissa officinalis and Nepeta cataria : effect of harvest time and plant species. 2015;77:499–507. doi: 10.1016/j.indcrop.2015.09.045. [DOI] [Google Scholar]
- 346.Rabiei Z., Rafieian-Kopaei M., Mokhtari S., Alibabaei Z., Shahrani M. The effect of pretreatment with different doses of Lavandula officinalis ethanolic extract on memory, learning and nociception. 2014;4(1):71–76. doi: 10.1016/j.biomag.2013.10.006. [DOI] [Google Scholar]
- 347.Waller S. B., Cleff M. B., Serra E. F., et al. Plants from Lamiaceae family as source of antifungal molecules in humane and veterinary medicine. 2017;104:232–237. doi: 10.1016/j.micpath.2017.01.050. [DOI] [PubMed] [Google Scholar]
- 348.Xiao Z., Li Q., Niu Y., et al. Odor-active compounds of different lavender essential oils and their correlation with sensory attributes. 2017;108:748–755. doi: 10.1016/j.indcrop.2017.07.040. [DOI] [Google Scholar]
- 349.Hajhashemi V., Ghannadi A., Sharif B. Anti-inflammatory and analgesic properties of the leaf extracts and essential oil of Lavandula angustifolia Mill. 2003;89:67–71. doi: 10.1016/s0378-8741(03)00234-4. [DOI] [PubMed] [Google Scholar]
- 350.Rabiei Z., Rafieian-Kopaei M. Neuroprotective effect of pretreatment with Lavandula officinalis ethanolic extract on blood-brain barrier permeability in a rat stroke model. 2014;7:S421–S426. doi: 10.1016/S1995-7645(14)60269-8. [DOI] [PubMed] [Google Scholar]
- 351.Pistelli L., Najar B., Giovanelli S., Lorenzini L., Tavarini S., Angelini L. G. Agronomic and phytochemical evaluation of lavandin and lavender cultivars cultivated in the Tyrrhenian area of Tuscany (Italy) 2017;109:37–44. doi: 10.1016/j.indcrop.2017.07.041. [DOI] [Google Scholar]
- 352.Chrysargyris A., Panayiotou C., Tzortzakis N. Nitrogen and phosphorus levels affected plant growth, essential oil composition and antioxidant status of lavender plant (Lavandula angustifolia Mill.) 2016;83:577–586. doi: 10.1016/j.indcrop.2015.12.067. [DOI] [Google Scholar]
- 353.Barocelli E., Calcina F., Chiavarini M., et al. Antinociceptive and gastroprotective effects of inhaled and orally administered Lavandula hybrida Reverchon “grosso” essential oil. 2004;76(2):213–223. doi: 10.1016/j.lfs.2004.08.008. [DOI] [PubMed] [Google Scholar]
- 354.Husseini Y., Sahraei H., Meftahi G. H., et al. Analgesic and anti-inflammatory activities of hydro-alcoholic extract of Lavandula officinalis in mice: possible involvement of the cyclooxygenase type 1 and 2 enzymes. 2016;26:102–108. doi: 10.1016/j.bjp.2015.10.003. [DOI] [Google Scholar]
- 355.Serafini M. R., Campos M., Rabelo K., et al. Determination of chemical and physical properties of Hyptis pectinata essential oil and their redox active profile. 2012;3:1–9. [Google Scholar]
- 356.Gavanji S., Mohammadi E., Larki B., Bakhtari A. Antimicrobial and cytotoxic evaluation of some herbal essential oils in comparison with common antibiotics in bioassay condition. 2014;3(3):142–152. doi: 10.1016/j.imr.2014.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 357.Flamini G., Cioni P. L., Morelli I. Composition of the essential oils and in vivo emission of volatiles of four Lamium species from Italy: L. purpureum, L. hybridum, L. bifidum and L. amplexicaule. 2005;91(1):63–68. doi: 10.1016/j.foodchem.2004.05.047. [DOI] [Google Scholar]
- 358.El Ouadi Y., Manssouri M., Bouyanzer A., et al. Essential oil composition and antifungal activity of Melissa officinalis originating from north-east Morocco, against postharvest phytopathogenic fungi in apples. 2017;107:321–326. doi: 10.1016/j.micpath.2017.04.004. [DOI] [PubMed] [Google Scholar]
- 359.Mogosan C., Vostinaru O., Oprean R., et al. A comparative analysis of the chemical composition, anti-inflammatory, and antinociceptive effects of the essential oils from three species of Mentha cultivated in Romania. 2017;22(2):p. 263. doi: 10.3390/molecules22020263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 360.Kadri A., Zarai Z., Békir A., Gharsallah N., Damak M. Chemical composition and antioxidant activity of Marrubium vulgare L. essential oil from Tunisia. 2011;10(19):3908–3914. [Google Scholar]
- 361.De Mastro G., Tarraf W., Verdini L., Brunetti G., Ruta C. Essential oil diversity of Origanum vulgare L. populations from Southern Italy. 2017;235:1–6. doi: 10.1016/j.foodchem.2017.05.019. [DOI] [PubMed] [Google Scholar]
- 362.Benedec D., Oniga I., Oprean R., Tamas M. Chemical composition of the essential oils of Ocimum basilicum L. cultivated in Romania. 2009;57:625–629. [Google Scholar]
- 363.Martínez A. L., González-Trujano M. E., Pellicer F., López-Muñoz F. J., Navarrete A. Antinociceptive effect and GC/MS analysis of Rosmarinus officinalis L. essential oil from its aerial parts. 2009;75(5):508–511. doi: 10.1055/s-0029-1185319. [DOI] [PubMed] [Google Scholar]
- 364.De Martino L., De Feo V., Nazzaro F. Chemical composition and in vitro antimicrobial and mutagenic activities of seven Lamiaceae essential oils. 2009;14(10):4213–4230. doi: 10.3390/molecules14104213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 365.Moosavi-Nasab M., Saharkhiz M. J., Ziaee E., Moayedi F., Koshani R., Azizi R. Chemical compositions and antibacterial activities of five selected aromatic plants essential oils against food-borne pathogens and spoilage bacteria. 2016;28(3):241–251. doi: 10.1080/10412905.2015.1119762. [DOI] [Google Scholar]
- 366.Yalçin F. N., Kaya D., Çaliş I., Ersöz T., Palaska E. Determination of iridoid glycosides from four Turkish Lamium species by HPLC-ESI/MS. 2008;32(4):457–467. [Google Scholar]
- 367.Carocho M., Barros L., Calhelha R. C., et al. Melissa officinalis L. decoctions as functional beverages: a bioactive approach and chemical characterization. 2015;6:2240–2248. doi: 10.1039/C5FO00309A. [DOI] [PubMed] [Google Scholar]
- 368.Cirlini M., Mena P., Tassotti M., et al. Phenolic and volatile composition of a dry spearmint (Mentha spicata L.) extract. 2016;21:1–15. doi: 10.3390/molecules21081007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 369.Amessis-Ouchemoukh N., Abu-Reidah I. M., Quirantes-Piné R., Madani K., Segura-Carretero A. Phytochemical profiling, in vitro evaluation of total phenolic contents and antioxidant properties of Marrubium vulgare (horehound) leaves of plants growing in Algeria. 2014;61:120–129. doi: 10.1016/j.indcrop.2014.06.049. [DOI] [Google Scholar]
- 370.Vallverdú-Queralt A., Regueiro J., Martínez-Huélamo M., Rinaldi Alvarenga J. F., Leal L. N., Lamuela-Raventos R. M. A comprehensive study on the phenolic profile of widely used culinary herbs and spices: rosemary, thyme, oregano, cinnamon, cumin and bay. 2014;154:299–307. doi: 10.1016/j.foodchem.2013.12.106. [DOI] [PubMed] [Google Scholar]
- 371.Pandey R., Kumar B. HPLC-QTOF-MS/MS-based rapid screening of phenolics and triterpenic acids in leaf extracts of Ocimum species and their interspecies variation. 2016;39(4):225–238. doi: 10.1080/10826076.2016.1148048. [DOI] [Google Scholar]
- 372.Mena P., Cirlini M., Tassotti M., Herrlinger K. A., Dall’Asta C., Del Rio D. Phytochemical profiling of flavonoids, phenolic acids, terpenoids, and volatile fraction of a rosemary (Rosmarinus officinalis L.) extract. 2016;21(11):1–15. doi: 10.3390/molecules21111576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 373.Zimmermann B. F., Walch S. G., Tinzoh L. N., Stühlinger W., Lachenmeier D. W. Rapid UHPLC determination of polyphenols in aqueous infusions of Salvia officinalis L. (sage tea) 2011;879(24):2459–2464. doi: 10.1016/j.jchromb.2011.06.038. [DOI] [PubMed] [Google Scholar]
- 374.Marrelli M., Conforti F., Rigano D., et al. Cytotoxic properties of Marrubium globosum ssp. libanoticum and its bioactive components. 2013;8(5):567–569. [Google Scholar]
- 375.Mnonopi N., Levendal R., Davies-Coleman M. T., Frosta C. L. The cardioprotective effects of marrubiin, a diterpenoid found in Leonotis leonurus extracts. 2011;138(1):67–75. doi: 10.1016/j.jep.2011.08.041. [DOI] [PubMed] [Google Scholar]
- 376.Zaabat N., Hay A.-E., Michalet S., et al. Antioxidant and antigenotoxic properties of compounds isolated from Marrubium deserti de Noé. 2011;49(12):3328–3335. doi: 10.1016/j.fct.2011.08.026. [DOI] [PubMed] [Google Scholar]
- 377.Paula de Oliveira A., Santin J. R., Lemos M., et al. Gastroprotective activity of methanol extract and marrubiin obtained from leaves of Marrubium vulgare L. (Lamiaceae) 2011;63(9):1230–1237. doi: 10.1111/j.2042-7158.2011.01321.x. [DOI] [PubMed] [Google Scholar]
- 378.Mnonopi N., Levendal R.-A., Davies-Coleman M. T., Frost C. L. The cardioprotective effects of marrubiin, a diterpenoid found in Leonotis leonurus extracts. 2011;138(1):67–75. doi: 10.1016/j.jep.2011.08.041. [DOI] [PubMed] [Google Scholar]
- 379.Lucarini R., Bernardes W. A., Ferreira D. S., et al. In vivo analgesic and anti-inflammatory activities of Rosmarinus officinalis aqueous extracts, rosmarinic acid and its acetyl ester derivative. 2013;51(9):1087–1090. doi: 10.3109/13880209.2013.776613. [DOI] [PubMed] [Google Scholar]
- 380.Hosseinzadeh H., Nourbakhsh M. Effect of Rosmarinus offcinalis L. aerial parts extract on morphine withdrawal syndrome in mice. 2003;17(8):938–941. doi: 10.1002/ptr.1311. [DOI] [PubMed] [Google Scholar]
- 381.Chen C., Chen H., Hsieh C., Yang Y., Wung B. Upregulation of NF-E2-related factor-2-dependent glutathione by carnosol provokes a cytoprotective response and enhances cell survival. 2011;32(1):62–69. doi: 10.1038/aps.2010.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 382.Kuo C.-F., Su J.-D., Chiu C.-H., et al. Anti-inflammatory effects of supercritical carbon dioxide extract and its isolated carnosic acid from Rosmarinus officinalis leaves. 2011;59(8):3674–3685. doi: 10.1021/jf104837w. [DOI] [PubMed] [Google Scholar]
- 383.Shingai Y., Fujimoto A., Nakamura M., Masuda T. Structure and function of the oxidation products of polyphenols and identification of potent lipoxygenase inhibitors from fe-catalyzed oxidation of resveratrol. 2011;59(15):8180–8186. doi: 10.1021/jf202561p. [DOI] [PubMed] [Google Scholar]
- 384.Mengoni E. S., Vichera G., Rigano L. A., et al. Suppression of COX-2, IL-1β and TNF-α expression and leukocyte infiltration in inflamed skin by bioactive compounds from Rosmarinus officinalis L. 2011;82(3):414–421. doi: 10.1016/j.fitote.2010.11.023. [DOI] [PubMed] [Google Scholar]
- 385.Mannelli L. D. C., Micheli L., Maresca M., et al. Anti-neuropathic effects of Rosmarinus officinalis L. terpenoid fraction: relevance of nicotinic receptors. 2016;6:1–15. doi: 10.1038/srep34832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 386.Ivan M. V., Zala A., Agop A., et al. Several aspects about fractalitaty role in the dynamics of complex systems. 2017;79(3):235–246. [Google Scholar]
- 387.Peana A. T., D’Aquila P. S., Panin F., Serra G., Pippia P., Moretti M. D. L. Anti-inflammatory activity of linalool and linalyl acetate constituents of essential oils. 2002;9(8):721–726. doi: 10.1078/094471102321621322. [DOI] [PubMed] [Google Scholar]
- 388.Peana A. T., D’Aquila P. S., Chessa M. L., Moretti M. D. L., Serra G., Pippia P. (−)-Linalool produces antinociception in two experimental models of pain. 2003;460(1):37–41. doi: 10.1016/s0014-2999(02)02856-x. [DOI] [PubMed] [Google Scholar]
- 389.Rao V. S., Menezes A. M., Viana G. S. Effect of myrcene on nociception in mice. 1990;42:877–878. doi: 10.1111/j.2042-7158.1990.tb07046.x. [DOI] [PubMed] [Google Scholar]
- 390.Sousa P. J. C., Linard C. F. B. M., Azevedo-Batista D., Oliveira A. C., Coelho-de-Souza A. N., Leal-Cardoso J. H. Antinociceptive effects of the essential oil of Mentha x villosa leaf and its major constituent piperitenone oxide in mice. 2009;42(7):655–659. doi: 10.1590/s0100-879x2009000700010. [DOI] [PubMed] [Google Scholar]
- 391.Le Bars D., Gozariu M., Cadden S. W. Animal Models of Nociception. 2001;53(4):597–652. [PubMed] [Google Scholar]
- 392.Williamson E., Okpako D., Evans F. Hoboken, NJ, USA: John Wiley & Sons; 1996. [Google Scholar]
- 393.Bannon A. W., Malmberg A. B. Hoboken, NJ, USA: John Wiley & Sons, Inc.; 2007. [DOI] [Google Scholar]