Abstract
Background
Various imaging techniques have been utilized for the diagnosis of chronic lateral ankle ligament injury. This systemic review will explore the effectiveness of different imaging techniques in diagnosing chronic lateral ankle ligament injury.
Methods
Relative studies were retrieved after searching 3 databases (MEDLINE, EMBASE, and Cochrane Central Register of Controlled Trails). Eligible studies were summarized. Data were extracted to calculate pooled sensitivity and specificity of magnetic resonance imaging (MRI), ultrasonography (US), stress radiography, and arthrography.
Results
Fifteen studies met our inclusion and exclusion criteria. A total of 695 participants were included. The pooled sensitivities in diagnosing chronic ATFL injury were 0.83 [0.78, 0.87] for MRI, 0.99 [0.96, 1.00] for US, and 0.81 [0.68, 0.90] for stress radiography. The pooled specificities in diagnosing chronic ATFL injury were 0.79 [0.69, 0.87] for MRI, 0.91 [0.82, 0.97] for US, and 0.92 [0.79, 0.98] for stress radiography. The pooled sensitivities in diagnosing chronic CFL injury were 0.56 [0.46, 0.66] for MRI, 0.94 [0.85, 0.98] for US, and 0.90 [0.73, 0.98] for arthrography. The pooled specificities in diagnosing chronic CFL injury were 0.88 [0.82, 0.93] for MRI, 0.91 [0.80, 0.97] for US, and 0.90 [0.77, 0.97] for arthrography.
Conclusion
This systematic review with meta-analysis investigated the accuracy of imaging for the diagnosis of chronic lateral ankle ligament injury. Ultrasound manifested high diagnostic accuracy in diagnosing chronic lateral ankle ligament injury. Clinicians should be aware of the limitations of MRI in detecting chronic CFL injuries.
Keywords: Ankle ligaments, Meta-analysis, Imaging, Diagnostic accuracy
Background
Ankle sprain is one of the most common sports injuries [1–3]. The injury mechanism, a combination of inversion and adduction in foot plantar flexion, can cause damage to the lateral ankle ligaments [4]. Lateral ankle ligaments comprise anterior talofibular ligament (ATFL), calcaneofibular ligament (CFL), and posterior talofibular ligament (PTFL) [5]. Chronic lateral ankle ligament injury is a long-term outcome in patients suffering acute ankle sprain. Some long-term cohort studies showed that 10 to 20% patients eventually developed persistent symptoms, including pain, swelling, perception of instability, and recurrent ankle sprain [6–9]. The precise cause of these symptoms is still in debate and probably multifactorial [5, 10–12]. But identifying chronic lateral ankle ligament injury is critical for locating primal symptoms, and thus, the decision making of surgical intervention [13].
Compared to acute ligament injury, the proper diagnosis of chronic ligament injury is difficult because of the uncertain association between initial inversion trauma history and ligament injury and diversified manifestation of chronic injuries on images [14, 15]. The patients’ history and clinical tests are important in diagnosis. A meta-analysis discussed the accuracy of clinical tests in diagnosing ankle ligament injury and claimed that clinicians cannot rule out ligamentous injury when physical tests are negative, and additional imaging is warranted [16]. Imaging is a helpful diagnostic method according to consensus of experts [17, 18]. However, different from acute injury, chronic ligament injury could show as either stretching, rupture, scarring, or thickening of the ligament on images, which confuses the clinical practitioners [19]. Magnetic resonance imaging (MRI), ultrasonography (US), stress radiography, and arthrography are often utilized for diagnosing chronic lateral ankle ligament injury. Separate studies on various imaging diagnostic techniques have been reported; however, the diagnostic effectiveness of different imaging techniques was still controversial, partly due to different existing reference standards [20, 21].
A previous systematic review assessed US for diagnosis of chronic ankle instability, but utilized variable gold standards, and did not provide pooled data [20]. Studies of MRI, US, stress radiography, and arthrography for diagnosis of chronic lateral ankle ligament injury were reported, but no previous systemic review provided synthesized data. This systemic review with meta-analysis is trying to analyze studies on diagnostic accuracy of different imaging techniques on chronic lateral ligament injury. Arthroscopic or surgical findings are set as the gold standards of ligament injuries [12, 22].
Methods
Inclusion and exclusion criteria
The studies that met the following criteria were included: (1) cohort-type or cross-sectional studies; (2) evaluated MRI and/or US and/or stress radiography and/or arthrography for the diagnosis of chronic ATFL and/or CFL injury (regarding the classification of acute and chronic ligament injuries, we followed the decisions adopted by the authors of the studies included); (3) comparing imaging results with arthroscopic or surgical findings as reference standards, and (4) reported data that enabled the calculation of the number of true positive (TP), true negative (TN), false positive (FP), and false negative (FN).
The following criteria were used to exclude underqualified studies: (1) acute injury patients; (2) patients with confounding factors like ankle fracture, history of previous foot, and ankle surgeries; (3) without clearly described arthroscopic or surgical findings as their reference standards; (4) cadaveric studies or studies utilizing animal models; and (5) non-English articles.
Search strategy
A systematical literature search was conducted to include the following three databases: MEDLINE, EMBASE, and Cochrane Central Register of Controlled Trails (CENTRAL). The detailed search strategies (Table 1) were first developed in MEDLINE and were then adjusted and applied in the other two databases.
Table 1.
Detailed search strategies
| Step | MEDLINE | EMBASE | CENTRAL |
|---|---|---|---|
| 1 | accuracy[Title/Abstract] OR accurate rate[Title/Abstract] OR diagnostic value[Title/Abstract] | exp diagnostic accuracy/ or exp accuracy/ or exp measurement accuracy/ or exp. diagnostic test accuracy study/ | MeSH descriptor: [Sensitivity and Specificity] explode all trees |
| 2 | sensitivity and specificity[MeSH Terms] | sensitivity.mp.[mp=title, original title, abstract, name of substance word, subject heading word] | accuracy: ti, ab, kw or accurate rate: ti, ab, kw or diagnostic value: ti, ab, kw(Word variations have been searched) |
| 3 | chronic ankle instability OR functional ankle instability OR lateral ankle instability | specificity.mp.[mp=title, original title, abstract, name of substance word, subject heading word] | MeSH descriptor: [Lateral ligament, Ankle] explode all trees |
| 4 | PTFL OR CFL OR ATFL | exp ankle ligament/ | PTFL OR CFL OR ATFL(Word variations have been searched) |
| 5 | talofibular[Text Word] OR calcaneofibular[Text Word] OR posterior talofibular[Text Word] OR anterior talofibular[Text Word] | ATFL.mp.[mp=title, original title, abstract, name of substance word, subject heading word] | chronic ankle instability OR functional ankle instability OR lateral ankle instability(Word variations have been searched) |
| 6 | lateral ligament, ankle[MeSH Terms] | CFL.mp.[mp=title, original title, abstract, name of substance word, subject heading word] | talofibular OR calcaneofibular OR posterior talofibular OR anterior talofibular(Word variations have been searched) |
| 7 | (1 OR 2) AND (3 OR 4 OR 5 OR 6) | PTFL.mp.[mp=title, original title, abstract, name of substance word, subject heading word] | (1 OR 2) AND (3 OR 4 OR 5 OR 6) |
| 8 | exp ankle instability/ | ||
| 9 | (1 OR 2 OR 3) AND (4 OR 5 OR 6 OR 7 OR 8) |
Abbreviations: exp explode, ti title, ab abstract, kw key words
Retrieved articles from each database were at first screened for duplication. Then, after titles and abstracts screening, relevant studies for this systemic review underwent full-text screening. Eligible studies were included according to the aforementioned inclusion and exclusion criteria.
Data extraction and quality assessment
The extracted data include authors, publication years, demographic features of participants, study design, index tests, gold standards, and the numbers of true positive, false negative, false positive, and true negative subjects. The pathologic features of chronic injury lead to various manifestations on images [14, 19, 23]. We eliminated this diversity by dichotomized imaging results to “injured” and “intact” in this study for better comparability among different included studies. Different kind of injuries such as “stretching,” “rupture,” “scarring,” or “thickening” are all categorized as “injured.”
Two authors independently extracted these data and filled previously drafted forms for this review. Results of the two authors were cross-validated, and discrepancies were mediated by the third author. The quality of the included articles was assessed through revised Quality Assessment of Diagnostic Accuracy Studies (QUADAS-2) tool, a widely recommended scale for diagnostic test evaluation [24]. According to QUADAS-2 tool, risk of bias was assessed in terms of patient selection, index test, and reference standard.
Statistical analysis
Sensitivity and specificity of each index test in individual study were calculated in Meta-DiSc, version 1.4.0, using the extracted data of TP, FN, FP, and TN. Pooled sensitivity and specificity were calculated using the total number of TP, FN, FP, and TN subjects in all relevant studies. Likelihood ratio (LR) evaluates the discriminatory properties of the test results [25]. Positive and negative likelihood ratio evaluates the positive and negative test results respectively. Pooled positive and negative likelihood ratio was calculated using random effects model. The diagnostic odds ratio (DOR) is defined as (true positives × true negatives) / (false positives × false negatives), which evaluates the overall diagnostic test performance combining sensitivity, specificity, and likelihood ratio [26]. Pooled DORs were calculated using random effects model.
All final outcomes were presented with 95% confidential interval. Pooled sensitivity, specificity, likelihood ratio, and DOR are calculated concerning each subgroup. Heterogeneity testing was assessed using the I2 test. A value of I2 > 50% was considered to be significant heterogeneity among the pooled data.
Results
Description of included studies
A total of 178 articles were retrieved from MEDLINE. One hundred eighty-eight articles were retrieved from EMBASE. Fifteen articles were retrieved from Cochrane Central Register of Controlled Trails. After deleting duplications, a total of 249 studies were identified in the primary search of three aforementioned databases. Then, these studies were screened for eligible studies as presented in the flow chart (Fig. 1). Twenty-four studies underwent full-text screen, and 9 studies were excluded for the following reasons: inconsistent reference standards among subjects [21, 27–29], studies on other lesions associated with chronic ankle instability [30–33], and heterogeneous population with inadequate data for chronic injury group [34].
Fig. 1.
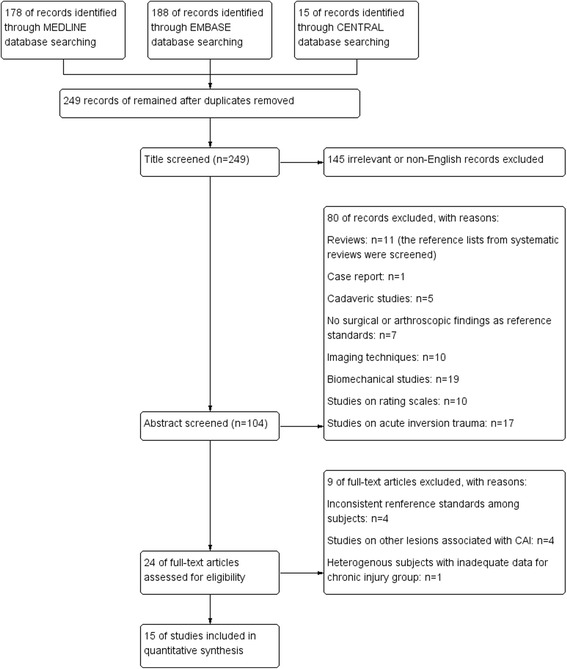
Flow diagram of search strategy
Overall, 15 studies [35–49] were eligible for this systemic review and are summarized in Table 2. A total of 695 participants were included. In 3 studies [39, 45, 49], participants were divided into acute injury group and chronic injury one, chronic injury groups of which were included in data synthesis. Two studies [42, 44] reported inter-rater reliability. In one study [48], a number of ankles instead of a number of participants were considered.
Table 2.
Summary of included studies
| Study (author and year) | Subject features | Age | Gender | Time from injury to study commencement/duration when patients presented with symptoms | Study design | Level of evidence | Index tests | Gold standard | Main conclusion |
|---|---|---|---|---|---|---|---|---|---|
| Cha et el. 2012 | 65 patients diagnosed with chronic lateral ankle instability who received preoperative MRI and arthroscopic examination | Not mentioned | 39 men and 26 women | Not mentioned | Case-control study | 3b | MRI | Arthroscopic findings | “However, inter-observer reliability and sensitivity of MRI findings were found to be relatively low in this study. Therefore, arthroscopic examination before ligament repair is a useful and recommended method for diagnosis and treatment of intra-articular lesions.” |
| Chandnani et al. 1994 | 17 chronic ankle instability patients | 24.5 years (ranged from 20 to 48 years) | 14 men and 3 women | Presented with symptoms of at least 6-months duration and did not respond to conservative therapy that included immobilization and early aggressive rehabilitation | Cohort study | 2b | Stress radiograph, MRI and MR arthrography | Findings from either diagnostic arthroscopy (n = 3) or open surgical repair (n = 14) | “In conclusion, our results suggest that MR arthrography may be a sensitive technique for detecting and staging tears of the lateral collateral ligaments and evaluating associated injuries in patients with chronic ankle instability. In patients for whom surgery is contemplated, MR arthrography may be a useful adjunct to conventional imaging techniques.” |
| Cheng et al. 2014 | 120 patients with a clinical suspicion of chronic ankle ligament injury | 32 years (ranged from 15 to 70 years) | 85 men and 35 women | Duration of symptoms ranged from 6 weeks to 20 years (mean, 2.2 years) | Cohort study | 2b | Ultrasonography | Arthroscopic findings (42 of these patients also underwent open surgery) | “In conclusion, ultrasonography as a convenient technique with low costs and real-time examination showed a satisfactory sensitivity and specificity for detecting lateral ligament injury.” |
| Cho et al. 2016 | 28 consecutive lateral ankle instability patients who underwent ankle arthroscopy | 32.4 ± 11.9 years (ranged from 15 to 55 years) | 19 men and 9 women | Conservative treatment had failed to substantially alleviate the symptoms for at least 3 months | Case-control study | 3b | MRI, manual anterior drawer test, stress ultrasonography, and stress X-ray | Arthroscopic findings | “Manual stress US is as precise as MRI in the detection of ligament injury and provides information on chronic ankle instability.” |
| Chou et al. 2006 | 50 patients suffering from ankle instability (17 of them who would receive surgical intervention were included in this review.) | Ranged from 14 to 77 years, n = 50 | 29 men and 21 women, n = 50 | Not mentioned | Cohort study | 2b | MRI and MR arthrography | Surgical findings | “For evaluating ankle disability, using plain MRI alone is not adequate for correctly detecting lateral collateral ligamentous injury of the ankle joint. MR arthrography improves the sensitivity and the accuracy for ATaF and CF ligament injuries. It also helps in assessing coexisting pathologic lesions of ankle joints.” |
| Hua et al. 2012 | 83 consecutive patients underwent ankle arthroscopy for different diagnosis | 32.2 years (ranged from 17 to 57 years) | 51 men and 32 women | Not mentioned | Case-control study | 3b | Ultrasonography | Arthroscopic findings | “US examination is a reliable and accurate method to evaluate chronic ATFL injury.” |
| Joshy et al. 2010 | 24 patients underwent arthroscopy as well as MRI for chronic ankle pain and/or instability | 39 years (range from 11 to 65 years) | 12 men and 12 women | Not mentioned | Case-control study | 3b | MRI | Arthroscopic findings | “MRI scan has very high specificity and positive predictive value in diagnosing tears of ATFT, CFL and osteochondral lesions. However sensitivity and negative predictive value is low with MRI.” |
| Kim et al. 2015 | 79 patients who would undergo ankle arthroscopy for different diagnosis. | 34.6 years (ranged from 21 to 67 years) | 44 men and 35 women | Mean duration of symptoms was 25.9 weeks (range, 11 to 52 weeks) | Cohort study | 2b | MRI | Arthroscopic findings | “The specificity and positive predictive value of MRI in the diagnosis of ATFL injuries were very high, whereas the sensitivity and negative predictive value of MRI were relatively low.” |
| Kumar et al. 2007 | 58 patients with symptomatic instability of their ankle | 28 years (ranged from 18 to 50 years) | 47 men and 11 women | Unresponsive to physiotherapy and non-operative management for at least 6 months | Cohort study | 2b | MRI and stress radiography | Arthroscopic findings | “MRI did not demonstrate any distinct advantage over the examination under anesthesia and stress radiography in the diagnosis of grade III lateral ankle ligament injuries.” |
| Lee et al. 2012 | 34 patients who underwent ankle MRI because of ankle sprains or ankle instability | 29 years (ranged from 13 to 53 years) | 22 men and 12 women | Not mentioned | Cohort study | 2b | MRI | Arthroscopic findings | “|A cortical defect with a bright dot-like or curvilinear high-signal-intensity lesion on T2-weighted MRI may be regarded as an additional finding to help increase the diagnostic performance for detecting anterior talofibular ligament injuries, including partial tears.” |
| Oae et al. 2010 | 34 consecutive patients needed an operation because of severe problems such as osteochondral lesions, synovitis and instability (15 chronic cases of them were included in this review.) | 29 years (ranged from 13 to 55 years), n = 34 | 19 men and 15 women, n = 34 | With a history of ankle injury of more than 4 weeks | Cohort study | 2b | Stress radiography, ultrasonography, and MRI | Arthroscopic findings | “We obtained satisfactory results with US and MR imaging.” |
| Park et al. 2012 | 48 people suspected of chronic ankle ligament injury | 36 years (ranged from 19 to 64 years) | 25 men and 23 women | The duration of symptoms ranging from several months to several years | Cohort study | 2b | MRI | Surgical findings | “In conclusion, MRI does not show perfect sensitivity for the evaluation of chronic lateral ankle ligament injury, such as those to the ATFL and CFL. Diagnosis of a complete tear of the ATFL on MRI is more sensitive than the diagnosis of a complete tear of the CFL. MRI findings of CFL injury were diagnostically specific but were not sensitive.” |
| Staats et al. 2017 | 30 patients with CAI and failed conservative treatment | 39.1 years (ranged from 18 to 71 years) | 15 men and 15 women | Not mentioned | Cohort study | 2b | MRI | Arthroscopic findings | “MRI is a helpful tool for preoperative evaluation, but arthroscopy remains gold standard in the diagnosis of associated lesions in patients with CAI” |
| Sugimoto et al. 2002 | 37 ft of 35 patients in whom recurrent instability of the ankle was diagnosed | 29.1 years (ranged from 11 to 56 years) | 16 men and 19 women | Mean interval between the injury and arthrography was 4 years 3 months (range, 6 months–22 years) | Cohort study | 2b | Subtalar arthrography, manual anterior drawer test and talar tilt test | Surgical findings | “Subtalar arthrography is valuable in making the diagnosis of calcaneofibular ligament injury in recurrent instability of the ankle.” |
| Tan et al. 2017 | 82 patients with ankle inversion trauma history (42 in the chronic group were included in this review.) | 24.8 years (ranged from 17 to 48 years), n = 42 | 36 men and 6 women, n = 42 | Interval from time of injury to time of MRI more than 3 months | Cohort study | 2b | MRI | Surgical findings | “MRI was able to accurately diagnose lateral ankle ligament tears in most cases. Diagnosis of a complete ATFL tear on MRI is more sensitive than that of complete CFL tear. The MRI findings of CFL injury were diagnostically specific but were not sensitive.” |
Methodological quality assessment
Methodological quality assessment was conducted for each study using QUADAS-2 tool (Fig. 2). All studies mentioned that participants were diagnosed of chronic ligament injury, of which 9 studies [36–38, 42, 43, 45, 46, 48, 49] mentioned the time from initial ankle inversion trauma to study commencement or duration when patients presented with chronic symptoms. Six of 15 studies [35, 38, 39, 41, 44, 47] were categorized as high risk of bias due to patient selection. All studies mentioned arthroscopic or surgical findings as their reference standards, of which 3 studies [37, 40, 46] mentioned that the reference standard results were interpreted without knowledge of the results of the index tests. All studies mentioned that investigators were blind to arthroscopic or surgical findings when interpreting the diagnostic imaging.
Fig. 2.
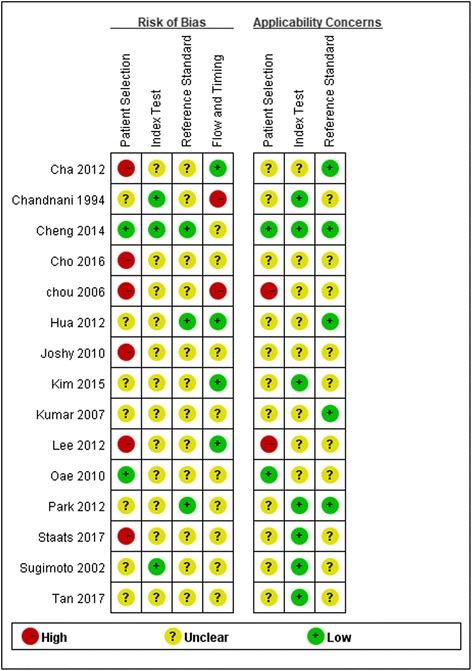
Methodological quality assessment of included studies using QUADAS-2 tool. Red stands for high risk. Green stands for low risk. Yellow stands for unclear risk
Diagnostic accuracy of imaging techniques
Considering the combination of different ligaments (ATFL and CFL) and imaging techniques (MRI, US, stress radiography, and arthrography), 8 subgroups were analyzed. Extracted data of 8 subgroups are listed in Fig. 3. Pooled sensitivity, pooled specificity, and their 95% confidential interval are listed in Fig. 4 in the form of zones of mostly bad imaging efficacy (ZOMBIE) plot as Richardson [50] described. Detailed pooled data are listed in Table 3.
Fig. 3.
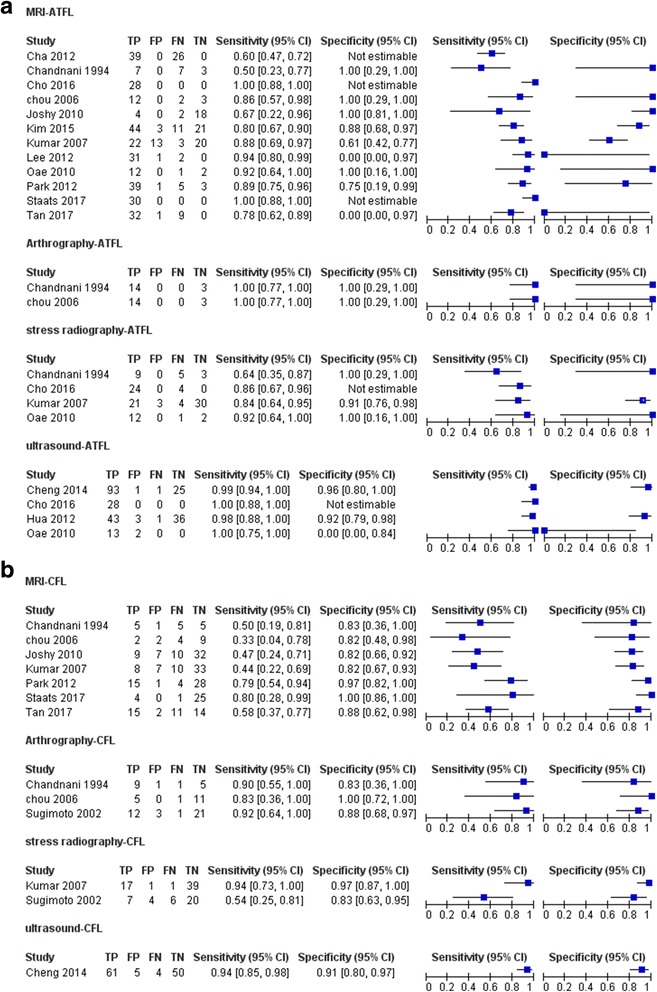
Forest plot showing sensitivity and specificity for each included study. MRI, US, stress radiography, and arthrography studies for ATFL and CFL are listed in a and b. TP, true positive; FP, false positive; FN, false negative; TN, true negative
Fig. 4.
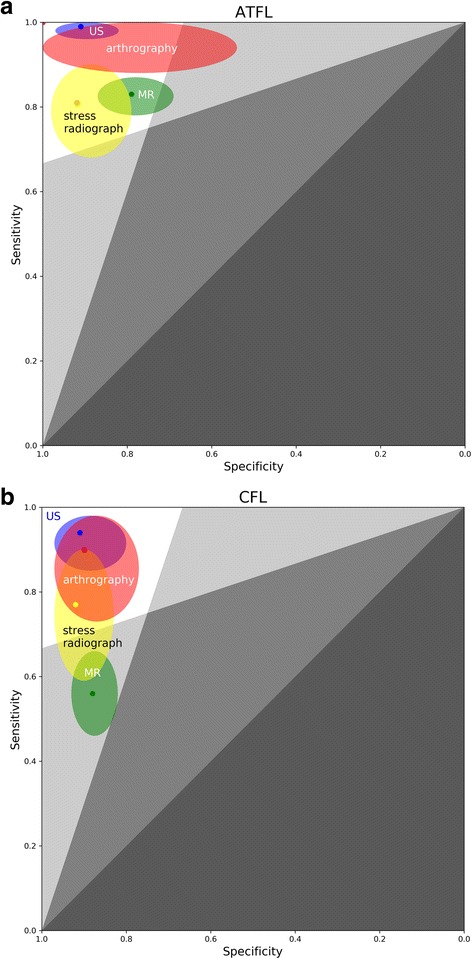
Zones of mostly bad imaging efficacy (ZOMBIE) plot for ATFL (a) and CFL (b). This is based on the receiver operating characteristic (ROC) plot. The colored dot stands for pooled sensitivity and specificity of each imaging technique, and the colored oval stands for 95% confidence interval of each imaging technique (green, MR; blue, US; red, arthrography; yellow, stress radiograph). Upper-left boomerang-shaped area formed by white and light grey zones defines zone of acceptable efficacy. Upper arm of the boomerang-shaped area stands for negative likelihood ratio below 0.33. Left arm of the boomerang-shaped area stands for positive likelihood ratio above 3
Table 3.
Results of pooled data
| Test | Ligament | Studies | Participants | TP | FP | FN | TN | Pooled sensitivity | Pooled specificity | Pooled LR+ | Pooled LR− | Pooled DOR | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Value [95%CI] | I 2 | Value [95%CI] | I 2 | Value [95%CI] | I 2 | Value [95%CI] | I 2 | Value [95%CI] | I 2 | ||||||||
| MRI | ATFL | 12 | 457 | 300 | 19 | 68 | 70 | 0.83 [0.78, 0.87] | 50.4% | 0.79 [0.69, 0.87] | 68.6% | 2.72 [1.41–5.24] | 60.4% | 0.28 [0.19–0.41] | 20.7% | 16.25 [7.65–34.53] | 0.0% |
| MRI | CFL | 7 | 269 | 58 | 20 | 45 | 146 | 0.56 [0.46, 0.66] | 30.5% | 0.88 [0.82, 0.93] | 48.9% | 3.84 [1.99–7.40] | 36.5% | 0.55 [0.41–0.74] | 38.8% | 8.28 [3.08–22.24] | 48.7% |
| US | ATFL | 4 | 246 | 177 | 6 | 2 | 61 | 0.99 [0.96, 1.00] | 0% | 0.91 [0.82, 0.97] | 71.6% | 15.08 [5.85–38.87] | 0% | 0.02 [0.00–0.07] | 0% | 946.51 [159.33–5622.80] | 0% |
| US | CFL | 1 | 120 | 61 | 5 | 4 | 50 | 0.94 [0.85, 0.98] | – | 0.91 [0.80, 0.97] | – | 10.3 [4.5–23.9] | – | 0.07 [0.03–0.18] | – | 153 [7–3550] | – |
| stress radiography | ATFL | 4 | 118 | 66 | 3 | 14 | 35 | 0.81 [0.68, 0.90] | 44.9% | 0.92 [0.79, 0.98] | 0% | 7.94 [3.11–20.28] | 0% | 0.24 [0.11–0.54] | 46% | 39.24 [10.50–146.56] | 0% |
| stress radiography | CFL | 2 | 95 | 24 | 5 | 7 | 59 | 0.77 [0.59, 0.90] | 86.6% | 0.92 [0.83, 0.97] | 75.7% | 9.88 [0.65–149.20] | 83.8% | 0.20 [0.01–4.14] | 89.3% | 53.40 [0.50–5752.7] | 88.2% |
| Arthrography | ATFL | 2 | 34 | 28 | 0 | 0 | 6 | 1.00 [0.88, 1.00] | 0% | 1.00 [0.54, 1.00] | 0% | – | – | – | – | – | – |
| Arthrography | CFL | 3 | 70 | 26 | 4 | 3 | 37 | 0.90 [0.73, 0.98] | 0% | 0.90 [0.77, 0.97] | 26.5% | 7.55 [3.15–18.05] | 0% | 0.15 [0.06–0.39] | 0% | 69.85 [13.77–354.41] | 0% |
Abbreviation: US ultrasonography, ATFL anterior talofibular ligament, CFL calcaneofibular ligament, TP true positive, FP false positive, FN false negative, TN true negative, LR+ positive likelihood ratio, LR− negative likelihood ratio, DOR diagnostic odds ratio
MRI exhibited the pooled sensitivities of 0.83 [0.78, 0.87] in diagnosing chronic ATFL injury and 0.56 [0.46, 0.66] in diagnosing chronic CFL injury. The pooled specificities were 0.88 [0.82, 0.93] in diagnosing chronic CFL injury and 0.79 [0.69, 0.87] in diagnosing chronic ATFL injury.
US presented the pooled sensitivities of 0.99 [0.96, 1.00] in diagnosing chronic ATFL injury and 0.94 [0.85, 0.98] in diagnosing CFL injury. The pooled specificities were 0.91 [0.82, 0.97] in diagnosing chronic ATFL injury and 0.91 [0.80, 0.97] in diagnosing chronic CFL injury.
Stress radiography demonstrated a sensitivity of 0.81 [0.68, 0.90] and a specificity of 0.92 [0.79, 0.98] in diagnosing chronic ATFL injury. Two studies regarding stress radiography for CFL showed high heterogeneity [43, 48], with I2 for pooled data above 50%.
Sample size regarding arthrography in diagnosing chronic ATFL injury is relatively small, with only 34 subjects included. Arthrography presented the pooled sensitivity of 0.90 [0.73, 0.98] and the pooled specificity of 0.90 [0.77, 0.97] in diagnosing chronic CFL injury.
Discussion
Accurate diagnosis of chronic lateral ankle ligament injury is considered critical for surgical intervention of chronic ankle instability [13]. Imaging diagnosis is usually non-invasive and can be of value when physical tests are ambiguous [16]. Results for the four including imaging diagnostic techniques have been reported; however, the diagnostic accuracy of each imaging technique is variable in different studies, partly due to different reference standards applied [20, 21]. Our study set arthroscopic or surgical findings as the gold standard to investigate four imaging techniques. This gold standard reduced the heterogeneity of different studies.
In our results, the pooled sensitivities and specificities of US in diagnosing chronic ATFL and CFL injury were all above 0.90. When diagnosing chronic ankle instability, another systemic review involving 6 articles reported sensitivity of US ranged from 84.6 to 100% and specificity of US ranged from 90.9 to 100% [20]. In agreement with this systemic review, our results demonstrated US is an effective imaging technique in diagnosing chronic lateral ankle ligament injury.
US can precisely discriminate different ligamentous conditions, such as torn, lax, or thickened ligaments [40]. Comparing US results of healthy people and patients with chronic ankle instability, Liu et al. reported the differences in the thickness of ATFL [51] and Croy et al. reported differences in the length of ATFL [52]. Lee et al. recommended stress US over regular one for diagnosis of chronic lateral ankle ligament injury [53]. The study of Cho et al., which was included in the current review [38], utilized stress US. Other studies included in the current review did not utilize stress US technique, but still presented high diagnostic accuracy. However, US is of limited value in assessing bone or cartilage and highly experience-reliant and may be much less efficacious in less experienced hands. Moreover, only 4 studies [37, 38, 40, 45] included in this systemic review were related to the US examination of chronic lateral ankle ligament injuries, of them only one study [37] involved CFL injuries. Only two included studies [38, 45] compared US with MRI findings and reported similar diagnostic effectiveness. US is an effective imaging technique in diagnosing chronic lateral ankle ligament injury, yet more studies are warranted to compare US with other imaging techniques.
In our results, MRI exhibited the pooled sensitivities of 0.83 in diagnosing chronic ATFL injury and 0.56 in diagnosing chronic CFL injury. The pooled specificities were around 0.8 in diagnosing chronic ATFL and CFL injury. In clinical practice, MRI is highly recommended in diagnosing ligamentous injuries [54]. Also, MRI was reported to be effective in diagnosing intra-articular lesions of chronic ankle instability, including osteochondral lesions of talus, syndesmotic injuries, and impingement syndromes [55, 56]. Using MRI, Tao et al. [57] reported more cartilage lesions in patients with combined injuries of the ATFL and CFL, compared to patients with only ATFL injury. A study showed that 86.7% of the experts recommended MRI before considering surgery in chronic ankle instability patients [18]. However, according to our results, MRI did not provide the highest sensitivity or specificity in diagnosing chronic ligament injuries. It presented different patterns in diagnosing chronic ATFL and CFL injuries. The sensitivity for diagnosing chronic ATFL injury (0.83 [0.78, 0.87]) was higher than that for diagnosing chronic CFL injury (0.56 [0.46, 0.66]). MRI is still irreplaceable in assessing chronic lateral ankle ligament injury because it is frequently performed to confirm or exclude the presence of concomitant lesions and influence the precise surgical technique for a certain patient. Two included studies [38, 45] in the current systemic review compared US with MRI findings and did not report significantly different diagnostic effectiveness.
Arthroscopy was recommended as a complementary to MRI for definitive diagnosis [17, 18, 22]. An expert consensus from Guillo et al. recommended that an arthroscopy should be performed at the time of surgery unless intra-articular pathology has been excluded by MRI scan and there is no history of pain [17].
In our results, stress radiography demonstrated a sensitivity of 0.81 and a specificity of 0.92 in diagnosing chronic ATFL injury. Tourné et al. suggested that stress radiography presented high specificity (up to 100%) but low sensitivity (57%), suggesting dynamic radiographs only have diagnostic value if they are positive [58]. According to our results, stress radiography showed similar high specificity as US. When diagnosing chronic ATFL injury, the sensitivity of stress radiography is still above 0.80, and the pooled LR− is 0.24 [0.11–0.54], similar as that of MRI. Negative stress radiographic findings decreases the post-test probability of chronic ATFL and CFL injury in patients with ankle inversion trauma history. However, ligamentous laxity detected through stress radiography is not synonymous with chronic ankle instability [59]. Large variability in talar tilt and anterior drawer stress radiography precludes their routine use in diagnosing chronic ankle instability [60].
The role of anesthesia in stress radiography was reported by McCaskie et al. [61], suggesting larger discriminative capability under anesthesia. Amongst studies included in the current review, only one study reported stress radiography under anesthesia [43]. The large heterogeneity between stress radiography results for chronic CFL injury may partly explained by anesthetic condition. Though stress radiography is helpful in the diagnosis, it is hardly a useful tool in predicting surgical outcomes. Jeong et al. reported stress radiography-positive patients were not statistically significantly different from stress radiography-negative patients in prognostic features [62].
Arthrography is indicated for staging and detecting intra-articular lesions of chronic lateral ankle instability [63]. Samoto et al. reported that patients with combined injuries of the ATFL and CFL diagnosed through arthrography had worse prognosis than patients with only ATFL injury [64]. Arthrography is an invasive imaging technique. With the spread of arthroscopy, which is also invasive but much more accurate, this technique is now losing its popularity. Only 3 studies before year 2010 discussed arthrography [36, 39, 48].
There are several limitations in the current systemic review. First, 6 of the 15 included studies were graded as high risk of bias due to patient selection. Unlike meta-analysis of clinical intervention, in meta-analysis of diagnostic tests, it is common to include case-control studies considered as high risk of bias [65]. Case-control studies create a preselected patient population and should be interpreted with caution. Second, associated lesions of chronic lateral ankle ligament injury were not discussed in the current review; however, these associated lesions spotted on images would certainly affect the judgement of clinicians. Third, some studies compared the diagnostic accuracy of identical imaging technique with different parameters and/or configurations on diagnosing chronic lateral ankle ligament injury. Strength of the MRI machines varied among different studies. This diversity in configuration may cause the heterogeneity within each subgroup in this study. Moreover, the size of the included studies was relatively small. Of the 15 included studies, only a total of 695 participants were included. Studies reporting the imaging diagnosis of PTFL injury are not sufficient to draw meaningful conclusion. The studies comparing different imaging techniques for the same group of subjects are limited. This suggests more diagnostic studies with high quality are warranted for imaging diagnosing chronic lateral ankle ligament injury.
Conclusion
This systematic review with meta-analysis investigated the accuracy of imaging for the diagnosis of chronic lateral ankle ligament injury. Our results demonstrated that ultrasound manifested high diagnostic accuracy in diagnosing chronic lateral ankle ligament injury. MRI presented the diagnostic sensitivity and specificity around 0.8 for chronic ATFL injuries, but much lower sensitivity for chronic CFL injuries. Clinicians should be aware of the limitations of MRI in detecting chronic CFL injuries. Stress radiography showed similar high specificity as US in diagnosing chronic lateral ankle ligament injury and showed diagnostic value of both positive and negative results. Arthrography demonstrated sensitivity and specificity around 0.9 in diagnosing chronic CFL injury, but limited literature recommended arthrography due to invasiveness, especially in recent years. When the diagnosis of chronic lateral ankle ligament injury is uncertain after careful inquiry of the patient’s history and physical tests, US may be a helpful imaging technique in experienced hands.
Acknowledgments
Funding
Dr. Xin Ma is currently receiving grants from National Natural Science Foundation of China (Grant No. 81171670 and Grant No. 81472037). Dr. Chen Wang is currently receiving grants from National Natural Science Foundation of China (Grant No. 81601862).
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
- ATFL
Anterior talofibular ligament
- CENTRAL
Cochrane Central Register of Controlled Trails
- CFL
Calcaneofibular ligament
- DOR
Diagnostic odds ratio
- FN
False negative
- FP
False positive
- LR
Likelihood ratio
- MRI
Magnetic resonance imaging
- PTFL
Posterior talofibular ligament
- QUADAS-2
Revised Quality Assessment of Diagnostic Accuracy Studies
- TN
True negative
- TP
True positive
- US
Ultrasonography
- ZOMBIE plot
Zones of mostly bad imaging efficacy plot
Authors’ contributions
All authors were fully involved in the study and preparation of the manuscript. SC and CW contributed to the study design and preparation of the manuscript. XM contributed to the search strategies. XW contributed to the statistical analysis. JH and CZ contributed to the article screening and data extraction. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Footnotes
Shengxuan Cao and Chen Wang contributed equally to this work.
Contributor Information
Shengxuan Cao, Email: csx6616@126.com.
Chen Wang, Email: wangch890825@163.com.
Xin Ma, Email: prof.xin.ma@qq.com.
Xu Wang, Email: wangxufoot@163.com.
Jiazhang Huang, Email: Jiazhanghuang@126.com.
Chao Zhang, Email: 13795207716@163.com.
References
- 1.Doherty C, Delahunt E, Caulfield B, Hertel J, Ryan J, Bleakley C. The incidence and prevalence of ankle sprain injury: a systematic review and meta-analysis of prospective epidemiological studies. Sports Med. 2014;44(1):123–140. doi: 10.1007/s40279-013-0102-5. [DOI] [PubMed] [Google Scholar]
- 2.Fong DT, Hong Y, Chan LK, Yung PS, Chan KM. A systematic review on ankle injury and ankle sprain in sports. Sports Med. 2007;37(1):73–94. doi: 10.2165/00007256-200737010-00006. [DOI] [PubMed] [Google Scholar]
- 3.Waterman BR, Owens BD, Davey S, Zacchilli MA, Belmont PJ., Jr The epidemiology of ankle sprains in the United States. J Bone Joint Surg Am. 2010;92(13):2279–2284. doi: 10.2106/JBJS.I.01537. [DOI] [PubMed] [Google Scholar]
- 4.Bonnel F, Toullec E, Mabit C, Tourne Y. Chronic ankle instability: biomechanics and pathomechanics of ligaments injury and associated lesions. Orthop Traumatol Surg Res. 2010;96(4):424–432. doi: 10.1016/j.otsr.2010.04.003. [DOI] [PubMed] [Google Scholar]
- 5.Hertel J. Functional anatomy, pathomechanics, and pathophysiology of lateral ankle instability. J Athl Train. 2002;37(4):364–375. [PMC free article] [PubMed] [Google Scholar]
- 6.Delahunt E, Coughlan GF, Caulfield B, Nightingale EJ, Lin CWC, Hiller CE. Inclusion criteria when investigating insufficiencies in chronic ankle instability. Med Sci Sports Exerc. 2010;42(11):2106–2121. doi: 10.1249/MSS.0b013e3181de7a8a. [DOI] [PubMed] [Google Scholar]
- 7.de Vries JS, Krips R, Sierevelt IN, Blankevoort L, van Dijk CN. Interventions for treating chronic ankle instability. Cochrane Database Syst Rev. 2011; 10(8):Cd004124. [DOI] [PubMed]
- 8.Mailuhu AKE, Oei EHG, van Putte-Katier N, van Ochten JM, Bindels PJE, Bierma-Zeinstra SMA, van Middelkoop M. Clinical and radiological predictors for persistent complaints five years after a lateral ankle sprain: a long-term follow-up study in primary care. J Sci Med Sport. 2017; 21(3):250–6. [DOI] [PubMed]
- 9.Pourkazemi F, Hiller CE, Raymond J, Nightingale EJ, Refshauge KM. Predictors of chronic ankle instability after an index lateral ankle sprain: a systematic review. J Sci Med Sport. 2014;17(6):568–573. doi: 10.1016/j.jsams.2014.01.005. [DOI] [PubMed] [Google Scholar]
- 10.Vega J, Pena F, Golano P. Minor or occult ankle instability as a cause of anterolateral pain after ankle sprain. Knee Surg Sports Traumatol Arthrosc. 2016;24(4):1116–1123. doi: 10.1007/s00167-014-3454-y. [DOI] [PubMed] [Google Scholar]
- 11.Hubbard TJ, Hertel J, Olmsted-Kramer L, Denegar CR. Contributing factors to chronic ankle instability. Med Sci Sports Exerc. 2006;38(5):S86–S87. doi: 10.1249/00005768-200605001-01266. [DOI] [Google Scholar]
- 12.Kerr HL, Bayley E, Jackson R, Kothari P. The role of arthroscopy in the treatment of functional instability of the ankle. Foot Ankle Surg. 2013;19(4):273–275. doi: 10.1016/j.fas.2013.06.008. [DOI] [PubMed] [Google Scholar]
- 13.Rodriguez-Merchan EC. Chronic ankle instability: diagnosis and treatment. Arch Orthop Trauma Sur. 2012;132(2):211–219. doi: 10.1007/s00402-011-1421-3. [DOI] [PubMed] [Google Scholar]
- 14.Meehan TM, Martinez-Salazar EL, Torriani M. Aftermath of ankle inversion injuries: spectrum of MR imaging findings. Magn Reson Imaging Clin N Am. 2017;25(1):45–61. doi: 10.1016/j.mric.2016.08.012. [DOI] [PubMed] [Google Scholar]
- 15.Hashimoto T, Inokuchi S, Kokubo T. Clinical study of chronic lateral ankle instability: injured ligaments compared with stress X-ray examination. J Orthop Sci. 2009;14(6):699–703. doi: 10.1007/s00776-009-1386-z. [DOI] [PubMed] [Google Scholar]
- 16.Schneiders A, Karas S. The accuracy of clinical tests in diagnosing ankle ligament injury. Eur J Phys. 2016;18(4):245–253. [Google Scholar]
- 17.Guillo S, Bauer T, Lee JW, Takao M, Kong SW, Stone JW, Mangone PG, Molloy A, Perera A, Pearce CJ, et al. Consensus in chronic ankle instability: aetiology, assessment, surgical indications and place for arthroscopy. Orthop Traumat Surg Res. 2013;99(8 Suppl):S411–S419. doi: 10.1016/j.otsr.2013.10.009. [DOI] [PubMed] [Google Scholar]
- 18.Michels F, Pereira H, Calder J, Matricali G, Glazebrook M, Guillo S, Karlsson J, Acevedo J, Batista J, Bauer T, et al. Searching for consensus in the approach to patients with chronic lateral ankle instability: ask the expert. Knee Surg Sports Traumatol Arthros. 2017. https://doi.org/10.1007/s00167-017-4556-0. [DOI] [PubMed]
- 19.Kwon DG, Sung KH, Chung CY, Park MS, Kim TW, Lee SH, Lee KM. Associations between MRI findings and symptoms in patients with chronic ankle sprain. J Foot Ankle Surg. 2014;53(4):411–414. doi: 10.1053/j.jfas.2014.02.018. [DOI] [PubMed] [Google Scholar]
- 20.Radwan A, Bakowski J, Dew S, Greenwald B, Hyde E, Webber N. Effectiveness of ultrasonography in diagnosing chronic lateral ankle instability: a systematic review. Int J Sports Phys Ther. 2016;11(2):164–174. [PMC free article] [PubMed] [Google Scholar]
- 21.Jolman S, Robbins J, Lewis L, Wilkes M, Ryan P. Comparison of magnetic resonance imaging and stress radiographs in the evaluation of chronic lateral ankle instability. Foot Ankle Int. 2017;38(4):397–404. doi: 10.1177/1071100716685526. [DOI] [PubMed] [Google Scholar]
- 22.Takao M, Uchio Y, Naito K, Fukazawa I, Ochi M. Arthroscopic assessment for intra-articular disorders in residual ankle disability after sprain. Am J Sports Med. 2005;33(5):686–692. doi: 10.1177/0363546504270566. [DOI] [PubMed] [Google Scholar]
- 23.Jung HG, Kim NR, Kim TH, Eom JS, Lee DO. Magnetic resonance imaging and stress radiography in chronic lateral ankle instability. Foot Ankle Int. 2017;38(6):621–626. doi: 10.1177/1071100717693207. [DOI] [PubMed] [Google Scholar]
- 24.Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, Leeflang MM, Sterne JA, Bossuyt PM. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011;155(8):529–536. doi: 10.7326/0003-4819-155-8-201110180-00009. [DOI] [PubMed] [Google Scholar]
- 25.Deeks JJ, Altman DG. Diagnostic tests 4: likelihood ratios. BMJ (Clinical research ed) 2004;329(7458):168–169. doi: 10.1136/bmj.329.7458.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Deeks JJ. Systematic reviews in health care: systematic reviews of evaluations of diagnostic and screening tests. BMJ (Clinical research ed) 2001;323(7305):157–162. doi: 10.1136/bmj.323.7305.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Park HJ, Lee SY, Park NH, Kim E, Chung EC, Kook SH, Lee JW. Usefulness of the oblique coronal plane in ankle MRI of the calcaneofibular ligament. Clin Radiol. 2015;70(4):416–423. doi: 10.1016/j.crad.2014.12.008. [DOI] [PubMed] [Google Scholar]
- 28.Park HJ, Lee SY, Park NH, Rho MH, Chung EC, Park JH, Park SJ. Three-dimensional isotropic T2-weighted fast spin-echo (VISTA) ankle MRI versus two-dimensional fast spin-echo T2-weighted sequences for the evaluation of anterior talofibular ligament injury. Clin Radiol. 2016;71(4):349–355. doi: 10.1016/j.crad.2015.12.007. [DOI] [PubMed] [Google Scholar]
- 29.Park HJ, Lee SY, Choi YJ, Hong HP, Park SJ, Park JH, Kim E. 3D isotropic T2-weighted fast spin echo (VISTA) versus 2D T2-weighted fast spin echo in evaluation of the calcaneofibular ligament in the oblique coronal plane. Clin Radiol. 2017;72(2):176 e171–176 e177. doi: 10.1016/j.crad.2016.09.023. [DOI] [PubMed] [Google Scholar]
- 30.Scranton PE, McDermott JE, Rogers JV. The relationship between chronic ankle instability and variations in mortise anatomy and impingement spurs. Foot Ankle Int. 2000;21(8):657–664. doi: 10.1177/107110070002100805. [DOI] [PubMed] [Google Scholar]
- 31.O'Neill PJ, Van Aman SE, Guyton GP. Is MRI adequate to detect lesions in patients with ankle instability? Clin Orthop Relat Res. 2010;468(4):1115–1119. doi: 10.1007/s11999-009-1131-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Park HJ, Cha SD, Kim HS, Chung ST, Park NH, Yoo JH, Park JH, Kim JH, Lee TW, Lee CH, et al. Reliability of MRI findings of peroneal tendinopathy in patients with lateral chronic ankle instability. Clin Orthop Surg. 2010;2(4):237–243. doi: 10.4055/cios.2010.2.4.237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chun KY, Choi YS, Lee SH, Kim JS, Young KW, Jeong MS, Kim DJ. Deltoid ligament and tibiofibular syndesmosis injury in chronic lateral ankle instability: magnetic resonance imaging evaluation at 3T and comparison with arthroscopy. Korean J Radiol. 2015;16(5):1096–1103. doi: 10.3348/kjr.2015.16.5.1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yi J, Cha JG, Lee YK, Lee BR, Jeon CH. MRI of the anterior talofibular ligament, talar cartilage and os subfibulare: comparison of isotropic resolution 3D and conventional 2D T2-weighted fast spin-echo sequences at 3.0 T. Skelet Radiol. 2016;45(7):899–908. doi: 10.1007/s00256-016-2367-x. [DOI] [PubMed] [Google Scholar]
- 35.Cha SD, Kim HS, Chung ST, Yoo JH, Park JH, Kim JH, Hyung JW. Intra-articular lesions in chronic lateral ankle instability: comparison of arthroscopy with magnetic resonance imaging findings. Clin Orthop Surg. 2012;4(4):293–299. doi: 10.4055/cios.2012.4.4.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chandnani VP, Harper MT, Ficke JR, Gagliardi JA, Rolling L, Christensen KP, Hansen MF. Chronic ankle instability: evaluation with MR arthrography, MR imaging, and stress radiography. Radiology. 1994;192(1):189–194. doi: 10.1148/radiology.192.1.8208935. [DOI] [PubMed] [Google Scholar]
- 37.Cheng Y, Cai Y, Wang Y. Value of ultrasonography for detecting chronic injury of the lateral ligaments of the ankle joint compared with ultrasonography findings. Br J Radiol. 2014;87(1033):20130406. doi: 10.1259/bjr.20130406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cho JH, Lee DH, Song HK, Bang JY, Lee KT, Park YU. Value of stress ultrasound for the diagnosis of chronic ankle instability compared to manual anterior drawer test, stress radiography, magnetic resonance imaging, and arthroscopy. Knee Surg Sports Traumatol Arthrosc. 2016;24(4):1022–1028. doi: 10.1007/s00167-015-3828-9. [DOI] [PubMed] [Google Scholar]
- 39.Chou MC, Yeh LR, Chen CK, Pan HB, Chou YJ, Liang HL. Comparison of plain MRI and MR arthrography in the evaluation of lateral ligamentous injury of the ankle joint. J Chin Med Assoc. 2006;69(1):26–31. doi: 10.1016/S1726-4901(09)70107-8. [DOI] [PubMed] [Google Scholar]
- 40.Hua Y, Yang Y, Chen S, Cai Y. Ultrasound examination for the diagnosis of chronic anterior talofibular ligament injury. Acta Radiol. 2012;53(10):1142–1145. doi: 10.1258/ar.2012.120171. [DOI] [PubMed] [Google Scholar]
- 41.Joshy S, Abdulkadir U, Chaganti S, Sullivan B, Hariharan K. Accuracy of MRI scan in the diagnosis of ligamentous and chondral pathology in the ankle. Foot Ankle Surg. 2010;16(2):78–80. doi: 10.1016/j.fas.2009.05.012. [DOI] [PubMed] [Google Scholar]
- 42.Kim YS, Kim YB, Kim TG, Lee SW, Park SH, Lee HJ, Choi YJ, Koh YG. Reliability and validity of magnetic resonance imaging for the evaluation of the anterior talofibular ligament in patients undergoing ankle arthroscopy. Arthroscopy. 2015;31(8):1540–1547. doi: 10.1016/j.arthro.2015.02.024. [DOI] [PubMed] [Google Scholar]
- 43.Kumar V, Triantafyllopoulos I, Panagopoulos A, Fitzgerald S, Niekerk LV. Deficiencies of MRI in the diagnosis of chronic symptomatic lateral ankle ligament injuries. Foot Ankle Surg. 2007;13(4):171–176. doi: 10.1016/j.fas.2007.04.002. [DOI] [Google Scholar]
- 44.Lee MH, Cha JG, Lee YK, Choi GC, Paik SH, Lee HK, Park SJ, Kim HJ. The bright rim sign on MRI for anterior talofibular ligament injury with arthroscopic correlation. AJR Am J Roentgenol. 2012;198(4):885–890. doi: 10.2214/AJR.11.6868. [DOI] [PubMed] [Google Scholar]
- 45.Oae K, Takao M, Uchio Y, Ochi M. Evaluation of anterior talofibular ligament injury with stress radiography, ultrasonography and MR imaging. Skelet Radiol. 2010;39(1):41–47. doi: 10.1007/s00256-009-0767-x. [DOI] [PubMed] [Google Scholar]
- 46.Park HJ, Cha SD, Kim SS, Rho MH, Kwag HJ, Park NH, Lee SY. Accuracy of MRI findings in chronic lateral ankle ligament injury: comparison with surgical findings. Clin Radiol. 2012;67(4):313–318. doi: 10.1016/j.crad.2011.08.025. [DOI] [PubMed] [Google Scholar]
- 47.Staats K, Sabeti-Aschraf M, Apprich S, Platzgummer H, Puchner SE, Holinka J, Windhager R, Schuh R. Preoperative MRI is helpful but not sufficient to detect associated lesions in patients with chronic ankle instability. Knee Surg Sports Traumatol Arthrosc. 2017. https://doi.org/10.1007/s00167-017-4567-x [DOI] [PMC free article] [PubMed]
- 48.Sugimoto K, Takakura Y, Samoto N, Nakayama S, Tanaka Y. Subtalar arthrography in recurrent instability of the ankle. Clin Orthop Relat Res. 2002;394:169–176. doi: 10.1097/00003086-200201000-00020. [DOI] [PubMed] [Google Scholar]
- 49.Tan DW, Teh DJW, Chee YH. Accuracy of magnetic resonance imaging in diagnosing lateral ankle ligament injuries: a comparative study with surgical findings and timings of scans. Asia Pac J Sport Med Arthrosc Rehabil Technol. 2017;7:15–20. doi: 10.1016/j.asmart.2016.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Richardson ML. The Zombie plot: a simple graphic method for visualizing the efficacy of a diagnostic test. AJR Am J Roentgenol. 2016; 207(4):W43–W52. [DOI] [PubMed]
- 51.Liu K, Gustavsen G, Royer T, Wikstrom EA, Glutting J, Kaminski TW. Increased ligament thickness in previously sprained ankles as measured by musculoskeletal ultrasound. J Athl Train. 2015;50(2):193–198. doi: 10.4085/1062-6050-49.3.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Croy T, Saliba SA, Saliba E, Anderson MW, Hertel J. Differences in lateral ankle laxity measured via stress ultrasonography in individuals with chronic ankle instability, ankle sprain copers, and healthy individuals. J Orthop Sports Phys Ther. 2012;42(7):593–600. doi: 10.2519/jospt.2012.3923. [DOI] [PubMed] [Google Scholar]
- 53.Lee KT, Park YU, Jegal H, Park JW, Choi JP, Kim JS. New method of diagnosis for chronic ankle instability: comparison of manual anterior drawer test, stress radiography and stress ultrasound. Knee Surg Sports Traumatol Arthrosc. 2014;22(7):1701–1707. doi: 10.1007/s00167-013-2690-x. [DOI] [PubMed] [Google Scholar]
- 54.Martella I, Azzali E, Milanese G, Pratico FE, Ruggirello M, Trunfio V, Parziale R, Corrado M, Della Casa G, Capasso R, et al. MRI in acute ligamentous injuries of the ankle. Acta bio-medica : Atenei Parmensis. 2016;87(Suppl 3):13–19. [PubMed] [Google Scholar]
- 55.van Putte-Katier N, van Ochten JM, van Middelkoop M, Bierma-Zeinstra SM, Oei EH. Magnetic resonance imaging abnormalities after lateral ankle trauma in injured and contralateral ankles. Eur J Radiol. 2015;84(12):2586–2592. doi: 10.1016/j.ejrad.2015.09.028. [DOI] [PubMed] [Google Scholar]
- 56.Choi WJ, Lee JW, Han SH, Kim BS, Lee SK. Chronic lateral ankle instability: the effect of intra-articular lesions on clinical outcome. Am J Sports Med. 2008;36(11):2167–2172. doi: 10.1177/0363546508319050. [DOI] [PubMed] [Google Scholar]
- 57.Tao H, Hu Y, Qiao Y, Ma K, Yan X, Hua Y, Chen S. T2—mapping evaluation of early cartilage alteration of talus for chronic lateral ankle instability with isolated anterior talofibular ligament tear or combined with calcaneofibular ligament tear. J Magn Reson Imaging. 2017; 47(1):69–77. [DOI] [PubMed]
- 58.Tourne Y, Besse JL, Mabit C. Chronic ankle instability. Which tests to assess the lesions? Which therapeutic options? Orthop Traumatol, Surg Res. 2010;96(4):433–446. doi: 10.1016/j.otsr.2010.04.005. [DOI] [PubMed] [Google Scholar]
- 59.Ferran NA, Oliva F, Maffulli N. Ankle instability. Sports Med Arthrosc Rev. 2009;17(2):139–145. doi: 10.1097/JSA.0b013e3181a3d790. [DOI] [PubMed] [Google Scholar]
- 60.Frost SC, Amendola A. Is stress radiography necessary in the diagnosis of acute or chronic ankle instability? Clin J Sport Med. 1999;9(1):40–45. doi: 10.1097/00042752-199901000-00008. [DOI] [PubMed] [Google Scholar]
- 61.McCaskie AW, Gale DW, Finlay D, Allen MJ. Chronic ankle instability: the value of talar tilt under general anaesthesia. Br J Sports Med. 1995;29(2):103–104. doi: 10.1136/bjsm.29.2.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Jeong BO, Kim TY, Song WJ. Effect of preoperative stress radiographic findings on radiographic and clinical outcomes of the modified Brostrom procedure for chronic ankle instability. J Foot Ankle Surg. 2016;55(1):125–128. doi: 10.1053/j.jfas.2015.08.010. [DOI] [PubMed] [Google Scholar]
- 63.Trnka HJ, Ivanic G, Trattnig S. Arthrography of the foot and ankle. Ankle and subtalar joint. Foot Ankle Clin. 2000;5(1):49–62. [PubMed] [Google Scholar]
- 64.Samoto N, Sugimoto K, Takaoka T, Fujita T, Kitada C, Takakura Y. Comparative results of conservative treatments for isolated anterior talofibular ligament (ATFL) injury and injury to both the ATFL and calcaneofibular ligament of the ankle as assessed by subtalar arthrography. J Orthop Sci. 2007;12(1):49–54. doi: 10.1007/s00776-006-1090-1. [DOI] [PubMed] [Google Scholar]
- 65.Kopkow C, Freiberg A, Kirschner S, Seidler A, Schmitt J. Physical examination tests for the diagnosis of posterior cruciate ligament rupture: a systematic review. J Orthop Sports Phys Ther. 2013;43(11):804–813. doi: 10.2519/jospt.2013.4906. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article.


