Abstract
Informal caregivers play a vital role in supporting seriously-ill patients. However, informal caregiving is burdensome, and can lead to negative health outcomes for the caregiver and the care recipient. The study’s aim was to evaluate relationships among caregiver burden, care recipient depressive symptomology, and race. Guided by the Social Exchange Perspective, we examined cross-sectional dyadic data from the National Long Term Care Survey (N= 1,279). Using ordinal logistic regression, we found that higher caregiver-reported objective burden was associated with higher care recipient depressive symptoms (p < .05); an association that was stronger for Blacks. Interestingly, despite significant levels of objective burden there was an association between lower depressive symptoms in Black care recipients when there was an exchange of the social good “helpful company” with a caregiver. These findings illustrate the importance of supporting reciprocal exchange as a promising component of maintaining balanced caregiver-care recipient relationships among Black older adults and their informal caregivers.
Keywords: Palliative Care, Race, Caregiving, Social Exchange, Depressive Symptoms, Burden, Older Adults
Understanding the complex relationship between informal family caregivers and care recipients is a key palliative care issue because many seriously-ill older adults rely on informal caregivers. In 2015, there were approximately 34.2 million informal caregivers who spent an average of 24.1 hours providing unpaid help to an older adult.1 Most informal caregivers are married, middle-aged, White women who do not hold a college degree and have a household income of less than $50,000 per year.1 Nearly half of care recipients are parents or parents-in-law; 10% are spouses or partners.1
Informal caregiving is physically, financially, and emotionally burdensome, and can lead to negative mental and physical health outcomes for the caregiver.2,3 Equally important are the potential consequences of these negative caregiver outcomes on the care recipient.4–6 Caregiver burden may not only negatively affect caregivers mental and physical health,2,7 but likely the quality of care recipients physical and mental health outcomes.8,9 In particular, caregivers and seriously-ill older adult care recipients are at high risk for depression. Depression is one of the most prevalent mood disorders among palliative care patients, and it is associated with impaired social functioning, reduced quality of life, poor prognosis, and higher mortality.10 In the United States, 1 to 5% of non-institutionalized older adults live with some form of depression. This estimate drastically increases to 11.5% of those who live in nursing homes, and 13.5% for those who receive home healthcare.11
The relationship between caregiver-care recipient depression and caregiver burden may be influenced by a variety of sociocultural factors, such as race, that can shape how caregivers respond to feelings of burden. Generally, compared to their Whites counterparts, African American caregivers have fewer financial resources and provide more care to their care recipients, but often report lower levels of burden, strain, and distress.1,12,13 It is possible that African Americans’ strong familial obligations and coping mechanisms such as prayer may cause them not to see the caregiving relationship and burden in the same way as Whites.14–16 The Social Exchange Perspective (SEP) provides a lens to help untangle some of these complex factors to better understand how sociocultural factors such as race might influence the relationships among caregiver burden and care recipient depressive symptomatology.
Social Exchange Perspective
The SEP posits that social relationships are a series of costs and rewards. However, the caregiver-care recipient relationship is unique; unlike other social relationships, this relationship is inherently imbalanced because the care recipient is dependent on the caregiver.2,17–19 This control-dependency relationship imbalance may be experienced by the caregiver as both subjective and objective burden (Figure 1) and by the care recipient as negative emotional response such as depressive symptoms.20,21 The care recipient may try to reduce the power differential by exchanging goods with the caregiver. These goods may be physical (e.g., help with chores), social (e.g., providing helpful company), or psychological (e.g., making the caregiver feel useful). In this study, we test how caregiver subjective and objective burden are associated with care recipient depressive symptoms and whether social exchange (including physical, social, and psychological exchange goods) moderates these factors.
Figure 1.
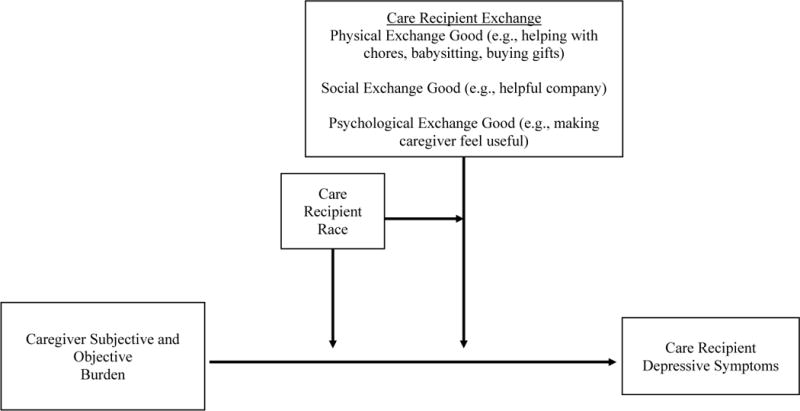
Model of associations between caregiver burden and care recipient depressive symptoms and the influence of care recipient exchange and race.
Social exchange among caregivers and care recipients may also be influenced by race. For Blacks, informal caregiving is normative largely because of a historical background of oppression, racism, and limited resource availability.14 As such, a care relationship in which resources are exchanged between caregivers and care recipients is common and can be quite beneficial. Thus, it is plausible that caregiver burden is less likely to be associated with depressive symptomology for Black care recipients in the presence of exchange.
The purpose of this study was to evaluate the associations between caregiver subjective and objective burden, care recipient depressive symptomology and exchange goods; and to evaluate associations between caregiver burden, care recipient depressive symptoms and care recipient race. We hypothesized that higher levels of caregiver subjective and objective burden would be associated with an increase in care recipient depressive symptoms (Hypothesis 1). Second, we expected that any positive association between caregiver burden and care recipient depressive symptoms would be lower for Black than for non-Black care recipients (Hypothesis 2). Third, the exchange of physical, social and psychological goods by the care recipient to the caregiver would be associated with a decrease in care recipient depressive symptoms (Hypothesis 3). Finally, we hypothesized that any negative association between exchange goods and care recipient depressive symptoms would be greater for Black than for non-Black care recipients (Hypothesis 4).
Methods
Sample and Setting
We used the most recent wave of the National Long Term Care Survey (NLTCS) to evaluate the associations between caregiver subjective and objective burden and the care recipient depressive symptoms.22 The NLTCS is a nationally representative sample of physically disabled Medicare recipients age 65 years or older living in the community or in formal institutions such as nursing homes and assisted living facilities. Our focus was on community-dwelling older adults. The Institutional Review Board of University of Alabama at Birmingham approved this study (N140228001).
The NLTCS was administered through in-home and scheduled-structured telephone interviews in which care recipients were asked about physical disabilities, medical conditions, recent hospitalizations, family support, activities of daily living (ADLs) and instrumental activities of daily living (IADLs), cognitive functioning, and the use of formal and informal caregiving.22 Care recipients also provided information on all informal caregivers who assisted them. From the information provided by the care recipient, primary informal caregivers were identified and surveyed in a supplemental survey. An eligible caregiver was defined as one who provides unpaid help with at least one activity of daily living (ADL) or instrumental activity of daily living (IADL) for at least 1 hour in the week prior to participating in the National Informal Caregiver Survey (NICS).23,24 When there was more than one individual who met the caregiver criteria, a primary caregiver was selected based on the individual who spent the most time providing help.24 Caregivers were asked about the type of help that they provided for the care recipient (i.e., objective burden), as well as questions on physical, emotional, and financial hardship to themselves (i.e., subjective burden) caused by the caregiving relationship.24
The initial 2004 wave of the NLTCS included a total of 20,474 respondents.1 For our sample we used four inclusion criteria: first, the sample was restricted to care recipients who had a caregiver and whose caregivers responded to the NICS (N = 4,272). Second, it included only care recipients whose caregiver received no remuneration for the care provided (N = 1,837). Third, the sample was restricted to care recipients who did not have dementia or other related diseases (N = 1,289). Finally, we only included care recipients who answered all three depression questions, resulting in an analytic sample of 1,279 respondents.
Measures
Caregiver self-reported subjective and objective burden
Caregiver subjective and objective burden were the two focal independent variables. Caregiver self-reported subjective burden was measured by a modified version of the Zarit Burden Interview.25 This study featured a three-item scale in which respondents were asked about the emotional stress, financial strain, and physical hardship that they experience from being a caregiver. The caregiver was asked, “How emotionally stressful would you say that caring for [the care recipient] is for you? Response options were coded as not stressful at all (0), a little stressful (1), moderately stressful (2), pretty stressful (3), and very stressful (4). The caregiver was asked in the same manner about physical strain and financial hardship. Scale scores range from 0 to 12, with 0 representing no subjective burden and 12 represent high levels of subjective burden. The Cronbach’s alpha = 0.77 for this three-item scale, suggesting acceptable internal consistency.
Caregiver self-reported objective caregiver burden was measured by a modified version of the Screen for Caregiver Burden index.26 The original Screen for Caregiver Burden (SCB) is a 25-item scale used to evaluate the occurrence of stressful events of caregiving and the severity of distress suffered by the caregiver.26,27 The scale in the NLTCS contains a modified 15-item version that does not include the measures of caregiver distress. In this survey, respondents were asked how many times in the past week they were tasked with dealing with behavioral issues of the care recipient. For example, caregivers were asked, “In the past week, on how many days did you personally have to deal with the following behavior of [the care recipient]? How many days did [he/she] keep you up at night?” Possible response options include no days (coded as 0), 1 to 2 days (1), 3 to 4 days (2), and 5 or more days (3). Scores range from 0 to 45. A score of 0 represents no objective burden and 45 represents high objective burden (Cronbach’s alpha = .81).
Care recipient depressive symptoms
Care recipient depressive symptomology, the outcome of interest, was measured by an abbreviated version of the Center for Epidemiologic Studies depression (CES-D) scale provided in the NLTCS. This is a three-item scale in which the respondents were asked questions about recent depressed mood. The older adult care recipient respondent was asked: “During the last 2 weeks, have you felt so sad, blue, or depressed that you, a) did not feel like doing things you usually do, b) could not sleep like you usually do, c) lost your appetite or could not eat like you usually do?” The responses were yes (1) and no (0) on each of the three questions. The scores were then summed, and the scale ranged from 0 to 3, with 0 representing no depressive symptoms, and 3 representing three depressive symptoms (Cronbach’s alpha = .71).
Physical, social, and psychological exchange goods
The social exchange perspective involves the exchange of physical, social, and psychological goods. These three types of goods were measured by proxy measures in the NICS in which caregivers were asked about resources provided to them by the care recipient. For physical exchange goods, the caregivers were asked if the care recipient helped with household chores, babysitting, or buying them things and giving them money. If the caregiver reported receiving none of the three, they were scored 0. If the caregiver reported receiving any one of the three, they were scored 1. Social exchange goods were measured by asking the caregiver whether the care recipient ever provided “helpful company” to them. Possible response options were no (0) and yes (1). To measure psychological goods the caregivers were asked whether the care recipient had made them feel useful and needed. Possible response options were also no (0) and yes (1).
Sociodemographic and health-related covariates
Sociodemographic covariates included the care recipient age, race, caregiver and care recipient gender, education level, and caregiver relationship to care recipient (e.g. spouse, child). Health-related covariates included care recipients’ self-rated health (ordinal measure ranging from poor health = 1 to excellent health = 4), cognitive function (measured using the Short Portable Mental Status Questionnaire (SPMSQ),28 and functional limitations (measured with the Index of Independence in Activities of Daily Living29 and the Instrumental Activities of Daily Living Scale30).
Statistical Analysis
All analyses were conducted using SPSS (version 23.0; SPSS Inc., Chicago, IL). Continuous variables were summarized using means and standard deviations. Categorical variables were described with frequencies and percentages. To analyze the relationships between caregiver burden and care recipient depressive symptoms, we used ordinal logistic regression models. The outcome variable (care recipient depressive symptoms) was regressed on each of the focal independent variables (subjective and objective burden) along with the sociodemographic and health-related covariates. Sociodemographic and health-related covariates were included in the models as potential confounders of the relationship between caregiver burden and care-recipient depressive symptoms. The conditional effects of race on the relationship between caregiver burden and care recipient depressive symptoms were assessed using interaction terms of race by subjective and objective caregiver burden.
In the second analysis, we examined the extent to which physical, social, and psychological exchange goods were associated with care recipient depressive symptoms net of caregiver burden, as indicated by the SEP. Physical, social, and psychological exchange goods are distinctly different dimensions of the social exchange perspective,21,31,32 and were each be analyzed separately. Again, using ordinal logistic regression models, we regressed care recipient depressive symptoms on subjective and objective caregiver burden, sociodemographic and health-related covariates, and exchange good measures. We also evaluated the extent to which any effects of physical, social, and psychological exchange goods were conditional on the race of the care recipient by including interaction terms of race by each of the social exchange goods.
Results
Sample Characteristics
Tables 1a and 1b provides care recipient and caregiver descriptive statistics overall (N=1279) and by care recipient race (non-Black=1167; Black=112). Overall, care recipients’ average age was 81.32 ± 9.04 years and most were female (66.8%). The average education for Blacks was 9th grade (5.72 ± 3.36) and high school diploma or GED for non-Blacks (9.70 ± 3.41). Mean ADLs and IADLs self-rated scores were similar for the full sample and by race. Care recipients reported fewer ADLs (1.03 ± 1.56 on a 7-point scale for the full sample; 1.08 ± 1.50 for Blacks; 1.03 ± 1.56 for non-Blacks) than IADLs (4.59 ± 2.20 on a 7-point scale for the full sample, 4.08 ± 2.32 for Blacks; 4.64 ± 2.18 for non-Blacks). Care recipients also reported good to very good health (2.50 ± .87, full sample; 2.39 ± .88, Blacks; 2.51 ± .86, non-Blacks). Most (75.1%) of the care recipients reported no depressive symptoms. By race, 77.7% of Blacks and 74.9% of non-Black reported no depressive symptoms.
Table 1a.
Care Recipient Descriptive Statistics: Overall and by Care Recipient Race
| Race
|
|||||||
|---|---|---|---|---|---|---|---|
| Full Sample | Black | Non-Black | p-value | ||||
| (N=1279) | (N = 112) | (N = 1167) | |||||
| N (%) | Mean (SD) | N (%) | Mean (SD) | N (%) | Mean (SD) | ||
| Demographics | |||||||
| Age | 81.32 (9.04) | 81.12 (11.11) | 81.34 (8.82) | .798 | |||
| Sex (Female) | 854 (66.80) | 85 (75.90) | 769 (65.90) | .032 | |||
| Education | 7.84 (3.47) | 5.72 (3.36) | 8.04 (3.41) | .000 | |||
| Functional Limitations | |||||||
| Number of ADLs | 1.03 (1.56) | 1.08 (1.50) | 1.03 (1.56) | .701 | |||
| Number of IADLs | 4.59 (2.20) | 4.08 (2.32) | 4.64 (2.18) | .010 | |||
| Self-rated Health Score | 2.50 (0.87) | 2.39 (0.88) | 2.51 (0.86) | .190 | |||
| Depressive symptoms | |||||||
| None | 961 (75.10) | 87 (77.70) | 874 (74.90) | .805 | |||
| One | 170 (13.30) | 9 (8.00) | 161 (13.80) | ||||
| Two | 89 (7.00) | 9 (8.00) | 80 (6.90) | ||||
| Three | 59 (4.60) | 7 (6.30) | 52 (4.50) | ||||
Table 1b.
Caregiver Descriptive Statistics: Overall and by Care Recipient Race
| Race | p-value | ||||||
|---|---|---|---|---|---|---|---|
|
|
|||||||
| Full Sample | Black | Non-Black | |||||
| (N=1279) | (N = 112) | (N = 1167) | |||||
| N (%) | Mean (SD) | N (%) | Mean (SD) | N (%) | Mean (SD) | ||
| Demographics | |||||||
| Sex (Female) | 820 (64.10) | 86 (76.80) | 734 (62.90) | .003 | |||
| Education | 9.65 (3.13) | 9.27 (3.40) | 9.70 (3.41) | .168 | |||
| Relationship to Care recipient | |||||||
| Spouse | 459 (35.90) | 19 (17.00) | 440 (37.70) | .000 | |||
| Son/Daughter | 616 (48.20) | 59 (52.70) | 557 (47.70) | ||||
| Brother/Sister | 49 (3.80) | 10 (8.90) | 39 (3.40) | ||||
| Other Relationships | 155 (12.10) | 24 (21.40) | 131 (11.20) | ||||
| Social Exchange Perspective Measure | |||||||
| Physical Exchange Good (Yes) | 882 (69.00) | 79 (70.50) | 803 (68.80) | .706 | |||
| Social Exchange Good (Yes) | 1047 (81.90) | 96 (85.70) | 951 (81.50) | .268 | |||
| Psychological Exchange Good (Yes) | 1127 (88.10) | 102 (91.10) | 1025 (87.8) | .312 | |||
| Caregiver burden measures | |||||||
| Subjective | 2.09 (2.75) | 2.21 (3.10) | 2.08 (2.72) | .612 | |||
| Objective | 3.42 (4.92) | 4.16 (5.37) | 3.35 (4.87) | .096 | |||
Note. SD, standard deviation; Subjective burden scale ranges from 0 to 12; Objective burden scale ranges from 0 to 45. p-values <. 05 are bolded to denote statistical significance.
The average subjective caregiver burden score was similar for the full sample and by race (2.09 ± 2.75 on a 12-point scale, full sample; 2.21 ± 3.10, caregivers of Black care recipients; 2.08 ± 2.72, caregivers of non-Black care recipients). The average objective caregiver burden score differed by race, however. The mean objective burden score was higher for caregivers of Black care recipients (4.16 ± 5.37 on a 45-point scale) then for caregivers of non-Black care recipients (3.35 ± 4.87). Most caregivers reported that they did receive physical, social, and psychological goods from the care recipient.
Associations of Caregiver Burden, Care Recipient Depression, and Race
Table 2 reports odds ratios for a series of models predicting care recipient depressive symptoms. Care recipient depressive symptoms were associated with objective but not subjective caregiver burden. This partially supports our first hypothesis that states that higher levels of caregiver subjective and objective burden would be associated with an increase in care recipient depressive symptoms. Care recipients who reported better health and who had higher levels of education were more likely to report fewer depressive symptoms. Female care recipients were more likely to report depressive symptoms than men.
Table 2.
Results of a Ordinal Logistic Regression Predicting Care Recipient Depression Score by Caregiver Burden, Race, and Covariates (N= 1279)
| Model 1 | Model 2 | Model 3 | ||||
|---|---|---|---|---|---|---|
| OR | [95%CI] | OR | [95%CI] | OR | [95%CI] | |
| Subjective Caregiver Burden Score | .99 | [.94, 1.05] | .99 | [.94, 1.05] | .99 | [.94, 1.05] |
| Objective Caregiver Burden Score | 1.09* | [1.06, 1.12] | 1.09* | [1.06, 1.12] | 1.08* | [1.05, 1.11] |
| Age of Care Recipient | .99 | [.97, 1.00] | .99 | [.97, 1.00] | .99 | [.97, 1.00] |
| Sex of Care Recipient [Male = reference] | ||||||
| Female | 1.43* | [1.02, 2.01] | 1.43* | [1.02, 2.01] | 1.43* | [1.02, 2.01] |
| Race of the Care Recipient [Non-Black = reference] | ||||||
| Black | .75 | [.46, 1.20] | .69 | [.37, 1.26] | .47* | [.24, .94] |
| Education of Care Recipient | .94* | [.90, .98] | .94* | [.90, .98] | .94* | [.90, .98] |
| Number of Care Recipient ADLs | 1.07 | [.98, 1.17] | 1.07 | [.98, 1.17] | 1.07 | [.98, 1.17] |
| Number of Care Recipient IADLs | .99 | [.92, 1.06] | .99 | [.92, 1.06] | .99 | [.92, 1.06] |
| Care Recipient Self-Rated Health Score | .77* | [.66, .91] | .77* | [.66, .91] | .77* | [.66, .91] |
| Sex of Caregiver [Male = reference] | ||||||
| Female | .92 | [.68, 1.25] | .93 | [.68, 1.26] | .93 | [.68, 1.26] |
| Education of Caregiver | 1.00 | [.95, 1.05] | 1.00 | [.95, 1.05] | 1.00 | [.95, 1.05] |
| Relationship of Caregiver to Care Recipient [Spouse = reference] | ||||||
| Son/Daughter | .97 | [.68, 1.38] | .97 | [.68, 1.39] | .99 | [.69, 1.41] |
| Brother/Sister | .87 | [.42, 1.80] | .87 | [.42, 1.80] | .89 | [.43, 1.85] |
| All Other Relationships | .78 | [.47, 1.28] | .78 | [.47, 1.29] | .79 | [.48, 1.31] |
| Black × Subjective Burden | 1.03 | [.90, 1.18] | ||||
| Black × Objective Burden | 1.08* | [1.00, 1.18] | ||||
| Pseudo R2 | 0.093 | 0.093 | .097 | |||
Note. Subjective burden scale ranges from 0 to 12; Objective burden scale ranges from 0 to 45. Bolded estimate denotes unique variable to the model.
p<.05 level [2-tailed].
Models 2 and 3 introduced interaction terms for race and subjective or objective caregiver burden. The significant positive interaction term for objective burden indicates that objective burden has a greater association with the odds of increasing depressive symptoms for Blacks than for non-Blacks. This contradicts our second hypothesis that caregiver burden would have a lower association with the odds of reporting depressive symptoms for Blacks than for non-Blacks.
Associations of Caregiver Burden, Care Recipient Depression, Social Exchange Measures, and Race
The next objective of this study was to analyze the relationships between exchange goods and care recipient depressive symptoms net of caregiver burden. Table 3 reports odds ratios for models that introduce the exchange measures into the analysis. We find that exchanging the social good of “helpful company” has a positive association with care recipient depressive symptoms, which partially contradicts Hypothesis 3 that states that the exchange of exchange goods would be associated with a decrease in depressive symptoms. We note that including the exchange measures in the model did not alter the relationships between care recipient depressive symptoms and objective caregiver burden, care recipient health, care recipient educational attainment, sex, and race noted above.
Table 3.
Results of a Ordinal Logistic Regression Predicting Care Recipient Depression Score by Caregiver Burden, Exchange Measures, Race, and Covariates (N= 1279)
| Model 1 | Model 2 | Model 3 | Model 4 | |||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| OR | [95%CI] | OR | [95%CI] | OR | [95%CI] | OR | [95%CI] | |
| Subjective Caregiver Burden Score | 1.00 | [.95, 1.06] | 1.00 | [.95, 1.06] | 1.00 | [.95, 1.06] | 1.00 | [.95, 1.06] |
| Objective Caregiver Burden Score | 1.09* | [1.06, 1.12] | 1.09* | [1.06, 1.12] | 1.09* | [1.05, 1.12] | 1.09* | [1.05, 1.12] |
| Age of Care Recipient | .99 | [.97, 1.01] | .99 | [.97, 1.01] | .99 | [.97, 1.01] | .99 | [.97, 1.01] |
| Sex of Care Recipient [Male = reference] | ||||||||
| Female | 1.42* | [1.01, 2.00] | 1.42* | [1.01, 2.00] | 1.41* | [1.00, 1.98] | 1.42* | [1.01, 2.00] |
| Race of the Care Recipient [Non-Black = reference] | ||||||||
| Black | .73 | [.46, 1.18] | .85 | [.37, 1.91] | 2.49 | [.87, 7.09] | 2.30 | [.63, 8.35] |
| Education of Care Recipient | .94* | [.90, .98] | .94* | [.90, .98] | .94* | [.90, .98] | .94* | [.90, .98] |
| Number of Care Recipient ADLs | 1.07 | [.98, 1.17] | 1.07 | [.98, 1.18] | 1.07 | [.98, 1.17] | 1.07 | [.98, 1.18] |
| Number of Care Recipient IADLs | .98 | [.91, 1.05] | .98 | [.91, 1.05] | .98 | [.91, 1.05] | .98 | [.91, 1.05] |
| Care Recipient Self-Rated Health Score | .77* | [.65, .91] | .77* | [.65, .91] | .77* | [.65, .91] | .77* | [.65, .91] |
| Sex of Caregiver [Male = reference] | ||||||||
| Female | .92 | [.68, 1.25] | .92 | [.68, 1.25] | .91 | [.67, 1.24] | .91 | [.67, 1.24] |
| Education of Caregiver | 1.00 | [.96, 1.05] | 1.00 | [.96, 1.05] | 1.01 | [.96, 1.05] | 1.01 | [.96, 1.05] |
| Relationship of Caregiver to Care Recipient [Spouse = reference] | ||||||||
| Son/Daughter | 1.03 | [.72, 1.47] | 1.03 | [.72, 1.47] | 1.04 | [.73, 1.49] | 1.03 | [.72. 1.48] |
| Brother/Sister | .93 | [.45, 1.93] | .93 | [.45, 1.94] | .91 | [.44, 1.91] | .90 | [.43, 1.89] |
| All Other Relationships | .86 | [.52, 1.42] | .86 | [.52, 1.43] | .87 | [.52, 1.44] | .88 | [.53, 1.46] |
| Physical Exchange Good [no = reference] | ||||||||
| Yes | 1.20 | [.86, 1.66] | 1.22 | [.87, 1.72] | 1.20 | [.86, 1.66] | 1.20 | [.87. 1.67] |
| Social Exchange Good [no = reference] | ||||||||
| Yes | 1.65* | [1.03, 2.63] | 1.64* | [1.03, 2.62] | 1.86* | [1.14, 3.03] | 1.69* | [1.05, 2.71] |
| Psychological Exchange Good [no = reference] | ||||||||
| Yes | .68 | [.41, 1.12] | .68 | [.41, 1.11] | .68 | [.42, 1.13] | 0.73 | [.44, 1.22] |
| Black × Physical Exchange Good | .81 | [.30, 2.17] | ||||||
| Black × Social Exchange Good | .23* | [.07, .75] | ||||||
| Black × Psychological Exchange Good | .28 | [.07, 1.11] | ||||||
| Pseudo R2 | .100 | .100 | .104 | .102 | ||||
Note. Subjective burden scale ranges from 0 to 12; Objective burden scale ranges from 0 to 45. Bolded estimate denotes unique variable to the model.
p<.05 level [2-tailed].
Models 2 through 4 introduced interaction terms between race and each of the measures of exchange. We found a statistically significant interaction for the social good of providing “helpful company” that indicates that for Blacks, care recipients having exchanged the social good of “helpful company” with his/her caregiver substantially reduced the care recipients’ odds of reporting depressive symptoms. This is consistent with Hypothesis 4 and suggests that the positive relationship between exchanging the social good of “helpful company” and depressive symptoms holds among non-Blacks.
Discussion
Using a nationally representative survey, this study attempted to untangle the complex relationship between caregiver burden and care recipient depression by examining factors (social exchange and race) that may have a positive or negative impact on that relationship. We found that greater caregiver objective burden levels (e.g., increased time spent up at night taking care of the care recipient, dealing with a bowel or bladder accident) were associated with increased odds of care recipients reporting more depressive symptoms. In contrast, subjective burden was not associated with care recipient depressive symptoms. We then examined whether social exchange and race impacted this relationship. We found that although the exchange of psychological and physical goods (e.g., making the caregiver feel useful and needed, helping with household chores) did not vary by race; the exchange of the social good of “helpful company”, substantially reduced the odds of Blacks reporting more depressive symptoms. These findings suggest that Black care recipients benefit by exchanging helpful company with their caregiver in efforts to bring balance to the care relationship thus reducing ‘social burden’.
Because Blacks have an earlier onset of chronic diseases, it is likely that Black care recipients receive informal care much longer than their non-Black counterparts.31 As a result, Blacks may have a longer period over which to satisfy the norm of reciprocity and equalize the exchange by providing helpful company as a way to give back. The finding that social good exchange reduces care recipients depressive symptoms, suggests that clinicians might consider reinforcing this to aide seriously-ill Black older adults to see the value of their company even when they are unable to help the family in other ways.
Surprisingly, exchanging helpful company did not hold true for non-Black care recipients; non-Black care recipients had an increased odds of reporting depressive symptoms in the presence of social exchange. This finding supports the potentially positive cultural impact of race on the caregiver-care recipient relationship.32 It is possible that there is a greater acceptance of interdependency within Black family life. Whereas non-Black care recipients may find exchange goods not a strong enough value to overcome dependency.
Limitations and Future Directions
Guided by the SEP, we used a nationally-representative sample to examine the buffering effects of exchanging goods on the relationship between caregiver objective and subjective burden and care recipient depressive symptoms. Research in this area has primarily focused on unidirectional giving, with the caregiver providing help to the care recipient.33–36 Hence, this study sheds light on the effect of bi-directional exchange between caregivers and care recipients.
However, as in any secondary analysis of an existing data set there are a number of study limitations. First, the data are over 10 years old. We should bear in mind that more recent older adult cohorts may have less illness and disability in older age, compared to their older counterparts.37 Thus, today’s care recipients may not be as ill as those in the dataset. Second, the NLTCS data does not measure depressive symptoms of caregivers and includes only a limited measure of care recipient depressive symptoms, (i.e., three items of the CES-D scale). This scale, however, has been used in previously published studies.38
Third, the NLTCS includes only a three-item scale to measure subjective burden. This measure may not have been robust enough to evaluate the complex concept of subjective burden. We are mindful that measures of exchange are subjective. This may differ from the actual goods that caregivers were provided by the care recipients or care given to the care recipient by the caregiver. However, having a dataset that measures exchange goods and burden among caregiver-care recipient dyads provided a unique opportunity to test the theory of social exchange. Also, the study relied on cross-sectional data and we cannot rule out the possibility of reverse causality— (i.e., that care recipient depression is a source of caregiver burden). This is a challenging issue to address because of the high levels of attrition with longitudinal data among older respondents. Nonetheless, future researchers should explore alternative research designs or collect longitudinal data at more frequent intervals than the NLTCS to help address potential reverse causality.
Conclusions
Findings from this study contribute to the literature in illustrating the importance of reciprocal exchange in maintaining balanced caregiver-care recipient relationships among seriously-ill African American older adults and their informal caregivers. In addition, the finding that exchange was not helpful in reducing depressive symptoms for non-Black care recipients reveals an area for further research. Given the complexity of the relationship among care recipients and their informal caregivers, longitudinal mixed methods studies would be helpful to investigate caregiver burden’s effects on the mental health of chronically-ill older adult care recipients over time. Qualitative researchers should elicit care recipients’ perspective on the meaning of dependency and how it affects their relationship with their family caregivers. Future research could also further explore the concept “helpful company” since it was found to be associated with fewer depressive symptoms among African American care recipients. We also found that despite the presence of exchange, caregivers still experience objective burden associated with their caregiving roles. This highlights the need for interventions that support family members in their roles as caregivers and promotion of self-care behaviors that improve mental health outcomes among this group.
Acknowledgments
Funding
This work was supported by the University of Alabama at Birmingham Comprehensive Minority Faculty and Student Development Program (CMFSDP) Fellowship and the NIH/NINR (3R01NR03665-02S1).
Footnotes
Preliminary analyses examined the feasibility of making use of both the 1999 and 2004 waves of the NLTCS for a longitudinal analysis, but the degree of attrition was too high. To resolve the sample size issue, we opted for cross-sectional analyses using the most recent wave (2004) of the NLTCS.
Declaration of Conflicting Interests
The authors declare that there is no conflict of interest.
References
- 1.National Alliance for Caregiving, AARP Public Policy Institute. Caregivng in the U.S. 2015 - Focused look at caregivers of adults age 50+ Bethesda, MD: National Alliance for Caregiving; 2015. [Google Scholar]
- 2.Bevans M, Sternberg EM. Caregiving burden, stress, and health effects among family caregivers of adult cancer patients. Journal of the American Medical Association. 2012;307(4):398–403. doi: 10.1001/jama.2012.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dionne-Odom JN, Azuero A, Lyons KD, et al. Benefits of early versus delayed palliative care to informal family caregivers of patients with advanced cancer: outcomes from the ENABLE III randomized controlled trial. Journal of Clinical Oncology. 2015;33(13):1446–1452. doi: 10.1200/JCO.2014.58.7824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Godwin KM, Swank PR, Vaeth P, Ostwald SK. The longitudinal and dyadic effects of mutuality on perceived stress for stroke survivors and their spousal caregivers. Aging & Mental Health. 2013;17(4):423–431. doi: 10.1080/13607863.2012.756457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Milbury K, Badr H, Fossella F, Pisters KM, Carmack CL. Longitudinal associations between caregiver burden and patient and spouse distress in couples coping with lung cancer. Supportive Care in Cancer. 2013;21(9):2371–2379. doi: 10.1007/s00520-013-1795-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vellone E, Chung ML, Cocchieri A, Rocco G, Alvaro R, Riegel B. Effects of self-care on quality of life in adults with heart failure and their spousal caregivers: Testing dyadic dynamics using the actor–partner interdependence model. Journal of Family Nursing. 2014;20(1):120–141. doi: 10.1177/1074840713510205. [DOI] [PubMed] [Google Scholar]
- 7.Viana MC, Gruber MJ, Shahly V, et al. Family burden related to mental and physical disorders in the world: results from the WHO World Mental Health (WMH) surveys. Revista Brasileira de Psiquiatria. 2013;35(2):115–125. doi: 10.1590/1516-4446-2012-0919. [DOI] [PubMed] [Google Scholar]
- 8.Bass DM, Judge KS, Snow AL, et al. Negative caregiving effects among caregivers of veterans with dementia. The American Journal of Geriatric Psychiatry. 2012;20(3):239–247. doi: 10.1097/JGP.0b013e31824108ca. [DOI] [PubMed] [Google Scholar]
- 9.Morse JQ, Shaffer DR, Williamson GM, Dooley WK, Schulz R. Models of self and others and their relation to positive and negative caregiving responses. Psychology and Aging. 2012;27(1):211. doi: 10.1037/a0023960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Warmenhoven F, van Rijswijk E, van Hoogstraten E, et al. How Family Physicians Address Diagnosis and Management of Depression in Palliative Care Patients. The Annals of Family Medicine. 2012;10(4):330–336. doi: 10.1370/afm.1373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Center for Disease Control. Current depression among adults-United States, 2006-2010. Morbidity and Mortality Weekly Report. 2010 http://www.cdc.gov/features/dsdepression/revised_table_estimates_for_depression_mmwr_erratum_feb-2011.pdf. [PubMed]
- 12.Clay OJ, Grant JS, Wadley VG, Perkins MM, Haley WE, Roth DL. Correlates of health-related quality of life in African American and Caucasian stroke caregivers. Rehabilitation Psychology. 2013;58(1):28. doi: 10.1037/a0031726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Glueckauf RL, Davis WS, Willis F, et al. Telephone-based, cognitive-behavioral therapy for African American dementia caregivers with depression: initial findings. Rehabilitation Psychology. 2012;57(2):124. doi: 10.1037/a0028688. [DOI] [PubMed] [Google Scholar]
- 14.Dilworth-Anderson P, Gibson B, Burke I. Working with African American families. Ethnicity and the Dementias Second Edition. 2013;127 [Google Scholar]
- 15.Heo GJ, Koeske G. The role of religious coping and race in Alzheimer’s disease caregiving. Journal of Applied Gerontology. 2013;32(5):582–604. doi: 10.1177/0733464811433484. [DOI] [PubMed] [Google Scholar]
- 16.Sterba KR, Burris JL, Heiney SP, Ruppel MB, Ford ME, Zapka J. “We both just trusted and leaned on the Lord”: A qualitative study of religiousness and spirituality among African American breast cancer survivors and their caregivers. Quality of Life Research. 2014;23(7):1909–1920. doi: 10.1007/s11136-014-0654-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Adelman RD, Tmanova LL, Delgado D, Dion S, Lachs MS. Caregiver burden: a clinical review. Journal of the American Medical Association. 2014;311(10):1052–1060. doi: 10.1001/jama.2014.304. [DOI] [PubMed] [Google Scholar]
- 18.Goren A, Gilloteau I, Lees M, daCosta DiBonaventura M. Quantifying the burden of informal caregiving for patients with cancer in Europe. Supportive Care in Cancer. 2014;22(6):1637–1646. doi: 10.1007/s00520-014-2122-6. [DOI] [PubMed] [Google Scholar]
- 19.Shahly V, Chatterji S, Gruber M, et al. Cross-national differences in the prevalence and correlates of burden among older family caregivers in the World Health Organization World Mental Health (WMH) Surveys. Psychological Medicine. 2013;43(04):865–879. doi: 10.1017/S0033291712001468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cook KS, Rice E. Social Exchange Theory. In: Delamatter J, editor. Handbook of Social Psychology. New York, NY: Kluwer Academic/Plenum Publishers; 2003. pp. 53–76. [Google Scholar]
- 21.Molm LD. Theoretical comparisons of forms of exchange. Sociological Theory. 2003;21(1):1–17. [Google Scholar]
- 22.Manton KG. National Long-Term Care Survey: 1982, 1984, 1989, 1994, 1999, and 2004. Inter-university Consortium for Political and Social Research (ICPSR) [distributor] 2010 [Google Scholar]
- 23.Boaz RF. Full-time employment and informal caregiving in the 1980s. Medical Care. 1996;34(6):524–536. doi: 10.1097/00005650-199606000-00003. [DOI] [PubMed] [Google Scholar]
- 24.Wolff JL, Kasper JD. Caregivers of frail elders: updating a national profile. Gerontologist. 2006;46(3):344–356. doi: 10.1093/geront/46.3.344. [DOI] [PubMed] [Google Scholar]
- 25.Bedard M, Molloy DW, Squire L, Dubois S, Lever JA, O’Donnell M. The Zarit Burden Interview: a new short version and screening version. Gerontologist. 2001;41(5):652–657. doi: 10.1093/geront/41.5.652. [DOI] [PubMed] [Google Scholar]
- 26.Vitaliano PP, Russo J, Young HM, Becker J, Maiuro RD. The screen for caregiver burden. Gerontologist. 1991;31(1):76–83. doi: 10.1093/geront/31.1.76. [DOI] [PubMed] [Google Scholar]
- 27.Hirschman KB, Shea JA, Xie SX, Karlawish JH. The development of a rapid screen for caregiver burden. Journal of the American Geriatrics Society. 2004;52(10):1724–1729. doi: 10.1111/j.1532-5415.2004.52468.x. [DOI] [PubMed] [Google Scholar]
- 28.Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. Journal of the American Geriatrics Society. 1975;23(10):433–441. doi: 10.1111/j.1532-5415.1975.tb00927.x. [DOI] [PubMed] [Google Scholar]
- 29.Katz S, Akpom CA. A measure of primary sociobiological functions. International journal of health services. 1976;6(3):493–508. doi: 10.2190/UURL-2RYU-WRYD-EY3K. [DOI] [PubMed] [Google Scholar]
- 30.Lawton MP, Brody EM, Médecin U. Instrumental activities of daily living (IADL) The Gerontologist. 1969;9:179–186. [PubMed] [Google Scholar]
- 31.Friedemann M-L, Buckwalter KC, Newman FL, Mauro AC. Patterns of caregiving of Cuban, other Hispanic, Caribbean Black, and White elders in south Florida. Journal of Cross-Cultural Gerontology. 2013;28(2):137–152. doi: 10.1007/s10823-013-9193-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Roth DL, Perkins M, Wadley VG, Temple EM, Haley WE. Family caregiving and emotional strain: associations with quality of life in a large national sample of middle-aged and older adults. Qual Life Res. 2009;18(6):679–688. doi: 10.1007/s11136-009-9482-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Djundeva M, Mills M, Wittek R, Steverink N. Receiving instrumental support in late parent–child relationships and parental depression. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2015;70(6):981–994. doi: 10.1093/geronb/gbu136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Grundy E, Read S. Social contacts and receipt of help among older people in england: are there benefits of having more children? The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2012;67(6):742–754. doi: 10.1093/geronb/gbs082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kalmijn M. How mothers allocate support among adult children: Evidence from a multiactor survey. The Journals of Gerontology: Series B. 2013;68(2):268–277. doi: 10.1093/geronb/gbs110. [DOI] [PubMed] [Google Scholar]
- 36.Tian Q. Intergeneration social support affects the subjective well-being of the elderly: Mediator roles of self-esteem and loneliness. Journal of Health Psychology. 2016;21(6):1137–1144. doi: 10.1177/1359105314547245. [DOI] [PubMed] [Google Scholar]
- 37.Ismail K, Nussbaum L, Sebastiani P, et al. Compression of morbidity is observed across cohorts with exceptional longevity. Journal of the American Geriatrics Society. 2016;64(8):1583–1591. doi: 10.1111/jgs.14222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ejem DB, Drentea P, Clay OJ. The effects of caregiver emotional stress on the depressive symptomatology of the care recipient. Aging & mental health. 2015;19(1):55–62. doi: 10.1080/13607863.2014.915919. [DOI] [PubMed] [Google Scholar]


