Abstract
Aim
To identify factors associated with completion of Advance Care Planning (ACP) by patients seen in primary care in developed countries. We hypothesized that the quality of primary care is associated.
Method
We analysed respondent reported individual and healthcare utilization factors associated with the completion of ACP activities from the 2014 Commonwealth Fund International Health Policy Survey of Older Adults in 11 Countries. The primary outcome is the combined number of ACP activities completed. ACP activities included discussion of treatment preferences, documentation of healthcare wishes, or documentation of a surrogate decision maker. A quality of primary care index was calculated.
Results
Respondents averaged 69 years old. Most were women, graduated high school, rated their income as average or higher, and rated their health as good or better. A minority reported multimorbidity, accessed the emergency department or hospital, or were informal caregivers. Out of 25530 survey respondents, 13409 (53%) reported completion of any ACP activity; 11579 (45%) had discussed treatment preferences. Generalized linear mixed model results suggest that hospitalization (rate ratio [RR] 1.18), multimorbidity (RR 1.16), informal caregiving (RR 1.13), higher education level (RR 1.14), income (RR 1.05), access to higher quality primary care (RR 1.04) and ED visits (RR 1.04) were associated with higher rates of ACP activities. Male gender (RR 0.85) and higher perceived health status (RR 0.96) were associated with lower rates.
Conclusions
In this international study, individuals with greater interaction with the healthcare system through hospitalization, multimorbidity, access to quality primary care and informal caregiving reported more ACP activities.
Keywords: Chronic disease, continuity of care, geriatrics, health services research, palliative care, primary care, survey research
Introduction
Advance care planning (ACP) is a process supporting individuals to understand and share their personal values, life goals and preferences regarding future medical care. ACP helps to ensure that people receive medical care that is consistent with their values and preferences during serious and chronic illness. Because ACP has the potential to better align end-of-life care with patient preferences (1,2), it is important to identify potentially modifiable factors associated with individuals participating in the ACP process.
The factors associated with ACP completion in the USA and other developed countries reveal a diverse array of patient characteristics and experiences. Older age and female gender are associated with ACP completion (3–6). In the USA, non-white race is inversely associated with ACP completion (4,5). Socioeconomic status plays a limited and inconsistent role as a predictor (7,8). Patients’ diagnoses and healthcare system utilization have also been examined. Chronic disease, greater perceived functional impairment and a cancer diagnosis are positively associated with ACP completion (6). Utilization factors positively associated include receiving an explanation about ACP, being asked to complete ACP, undergoing major surgery (3) and being hospitalized overnight (7).
The clinical setting of a patient’s interaction with the healthcare system may play an important role in predicting ACP completion. Therefore, evaluating the potential impact of patient interactions with different healthcare settings in which ACP counselling occurs, such as primary care, emergency departments and hospitals, is warranted. Primary care, serving as the foundation of quality patient-centred healthcare models, is a natural venue for ACP engagement. A usual source of care (4) and having contact with a general practitioner in the last week of life (9) are known to positively influence ACP completion. However, ACP within primary care practice is not routine (10). Whether the quality of primary care (defined by user-reported accessibility, longitudinal care, ability to coordinate care and interpersonal relationship and communication with the primary care practitioner (11)) influences ACP has not been explored.
The purpose of this study is to identify individual and healthcare utilization factors that are associated with participating in ACP across healthcare systems. First, we described the prevalence of ACP actions in nationally representative samples of adults aged 55 and older from 11 developed countries. Then, we determined which factors were associated with ACP, including the potential impact of access to quality primary care.
Methods
Data source
The 2014 Commonwealth Fund International Health Policy Survey of Older Adults in 11 Countries dataset was used for this study. This survey consists of computer-assisted telephone interviews of nationally representative random samples of adults aged 55 or older from 11 countries (Australia, Canada, France, Germany, Netherlands, New Zealand, Norway, Sweden, Switzerland, the USA and the UK). The survey was translated and adjusted for country-specific wording as needed. Complete survey data and methods are available (12). This Commonwealth Fund survey is one of a series of International Health Policy (IHP) surveys used to collect nationally representative data from citizens in several Organization for Economic Cooperation and Development (OECD) countries to compare features of health system performance. This study was approved by the Colorado Multiple Institutional Review Board.
Outcomes
Three survey questions address ACP activities: (i) In the event you become very ill or injured and you cannot make decisions for yourself, have you had a discussion with family, a close friend, or with a health care professional about what healthcare treatment you WANT, or DO NOT WANT? (ii) Do you have a written plan or document describing the health care treatment you want or do not want at the end of your life? (iii) Do you have a written document that names someone to make treatment decisions for you if you cannot make decisions for yourself? The total number of ACP activities was used as the primary outcome measure. A country-specific analysis of respondents’ report of each ACP activity for respondents age 65 and older has been published elsewhere (12).
Independent variables
Independent variables included respondent demographics (age, gender, education, income), individual health-related factors (health status, multimorbidity, informal caregiving), healthcare utilization (inpatient hospitalization, emergency department visit) and a quality of primary care index. Age was calculated by subtracting the year of birth from the year of the survey (2014). Education level was dichotomized into less than a high school education versus high school graduate or more. Income was dichotomized into below average versus average or greater based on the respondents’ report of income level normed for the respondents’ country. We dichotomized survey respondents’ report of health status (excellent, very good, good, fair, poor) into ‘excellent/very good/good’ versus ‘fair/poor’. Multimorbidity was defined as respondent report of 2 or more of the following: hypertension, heart disease, diabetes, asthma/chronic lung disease, depression/anxiety/other mental health problems, cancer, and joint pain/arthritis. Multimorbidity was dichotomized as 0–1 versus 2 or more conditions. Informal caregiving was based on respondent report of providing assistance at least once weekly to a person living with an age-related problem, chronic health condition or disability. Inpatient hospitalization was based on report of any inpatient hospitalization in the previous 2 years. Emergency Department (ED) utilization was based on report of any ED visit in the previous 2 years. Finally, a quality of primary care index was created using methods from Macinko and Guanais (11). They developed and tested an index assessing individuals’ experience of primary care using data from the 2013 IHP Survey. Questions in 2013 were repeated in the 2014 IHP survey, our data source. Our a priori hypothesis was that the quality of primary care would positively influence completion of ACP. This measure included questions about key functions of primary care: access to care, continuity of care, coordination of care by a primary care provider, and primary care provider communication, interpersonal relations, and cultural competence. To aid in interpretation, the quality of primary care index was coded in the opposite direction from the Macinko and Guanais method, with a higher score indicating higher quality primary care.
Data analysis
A generalized linear mixed model (GLMM) was used to model the counts of ACP activities reported by each respondent (0–3). These counts were assumed to follow a Poisson distribution. The respondent’s country was treated as a random effect to account for correlation among participants from the same country, this also adjusts for the number of respondents per country. All independent variables were included a priori for their potential clinical relevance to ACP activities, rather than selection and inclusion in the model based on model building strategies. All covariates used in the GLMM were recoded into binary variables, with the exception of age (range 55–106 years of age) and the quality of primary care index (possible range 0–14).
Beta of greater than 0.1 with a confidence interval that excluded zero was considered to be clinically meaningful. We used effect size to determine a clinically meaningful difference rather than P value because of the large sample size. Incidence rate ratio (IRR) was calculated to demonstrate the percentage increase or decrease in ACP activities associated with a one-unit change in the covariate of interest. Data management and analysis were performed using R 3.3.1 (13) and the R package lme4 (14).
Results
Table 1 describes 25550 respondents from 11 countries. We found low rates of missing data. The largest number of missing data was for the quality of primary care index (636 respondents, 2.5% of total sample). Respondent average age was 68.6 years (range 55–106 years of age); 43% were men. The average respondent had completed at least high school. Fifty-eight percent rated their health as good or better and 42% had two or more chronic health conditions. The average quality of primary care index score was 10 (range 0–13), which was lower than the average reported in the population where it was originally developed, after adjustment for the reverse coding (11).
Table 1.
Description of 25550 primary care respondents to 2014 Commonwealth Fund Survey from 11 developed countries
| Variable | N (%) |
|---|---|
| Age in years (mean, SD) | 68.6 (9.2) |
| Male Gender | 10877 (42.6%) |
| Education: High school graduate or higher | 16669 (65.2%) |
| Income Group: Average or above average | 14832 (58.1%) |
| Self-Reported Health Status: Good, Very Good, or Excellent | 14 685 (57.5%) |
| Multimorbidity: At least 2 chronic conditions | 10646 (41.7%) |
| Informal Caregiving | 5111 (20.0%) |
| Inpatient Hospitalization in previous 2 years | 5974 (23.4%) |
| Emergency Department Use in previous 2 years | 8053 (31.5%) |
| Quality Primary Care Index (mean, SD) | 10.0 (2.3) |
| Country of Residence | |
| Australia | 3310 (13.0%) |
| Canada | 5269 (20.6%) |
| France | 1500 (5.9%) |
| Germany | 928 (3.6%) |
| Netherlands | 1000 (3.9%) |
| New Zealand | 750 (2.9%) |
| Norway | 1000 (3.9%) |
| Sweden | 7206 (28.2%) |
| Switzerland | 1812 (7.1%) |
| UK | 1000 (3.9%) |
| USA | 1755 (6.7%) |
All variables are dichotomized except age and quality of primary care, an index scoring 0–14 (reported scores ranged 0–13), with higher scores indicating better quality.
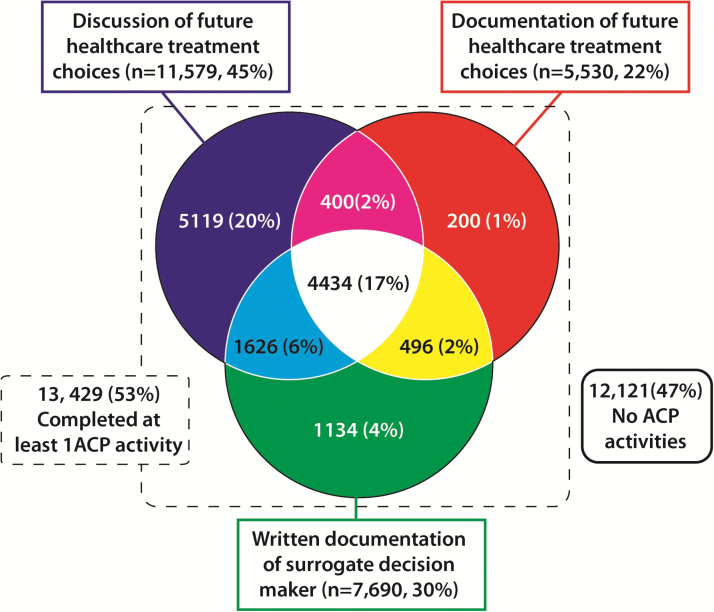
With respect to ACP, the mean number of activities completed by respondents was 0.97 (SD = 1.1), with a median of 1 and a mode of 0 (n = 12121, 47%). Figure 1 shows reported completion of each ACP activity. Respondents most frequently reported discussion of future healthcare treatment choices with a family, close friend or health care professional (n = 11579, 45%) as a completed ACP activity. A minority of respondents reported completing all three ACP activities (n = 4434, 17%). A depiction of number of ACP activities by country is available in Online Supplementary Figure 1.
Figure 1.
Distribution of 25 550 respondents by type of ACP activities completed.
Several individual and healthcare system factors are associated with the number of ACP activities that respondents completed. Table 2 reports the results of the GLMM and shows that inpatient hospitalization, multimorbidity, higher education and being an informal caregiver were clinically meaningful covariates based on an effect size of at least 0.1 and a confidence interval that excluded zero (i.e. a IRR that excluded 1.0). Men had 15% lower rates of ACP activities completion than women (CI 0.82–0.87). Individuals with multimorbidity completed 16% more ACP activities compared to those without multimorbidity (CI 1.12–1.19) in a given country. Additionally, individuals participating in informal caregiving averaged 13% more ACP activities compared to those not reporting caregiving (CI 1.10–1.17). With respect to healthcare utilization, for a given country, individuals who had an inpatient hospitalization in the previous 2 years averaged 18% more ACP activities completed compared to those who had not been hospitalized (CI 1.14–1.21). For each 1-point increase in the quality of primary care index in a given country, the average number of ACP activities increased by 3.8%, not a clinically meaningful effect size. However, this equates to a nearly 50% increase in number of ACP activities for those with the highest versus lowest quality of primary care index score. A difference of 3 points on the quality primary care index would be considered to be associated with a clinically meaningful effect.
Table 2.
Factors associated with more advance care planning activities based on a generalized liner mixed model
| Variable | Rate Ratio | 95% CI | P value |
|---|---|---|---|
| Intercept | 0.21 | (0.15–0.30) | <0.001 |
| Age* | 1.01 | (1.01–1.01) | <0.001 |
| Male Gender | 0.85 | (0.82–0.87) | <0.001 |
| Higher Education | 1.14 | (1.10–1.17) | <0.001 |
| Income group | 1.05 | (0.95–1.16) | <0.001 |
| Higher Perceived Health status | 0.96 | (0.94–0.99) | 0.007 |
| Multimorbidity | 1.16 | (1.12–1.19) | <0.001 |
| Informal caregiving | 1.13 | (1.10–1.17) | <0.001 |
| Inpatient hospitalization | 1.18 | (1.14–1.21) | <0.001 |
| Emergency Department visits | 1.04 | (1.02–1.07) | 0.003 |
| Quality of Primary Care Index* | 1.04 | (1.03–1.04) | <0.001 |
| Country variance | 0.30 | ||
Country is included in the model as a random effect. Bolded covariates indicate clinically meaningful effect sizes based on incidence rate ratio >1.1.
*All covariates are binary, except for age and quality primary care index.
Conclusion
Summary
This study demonstrates that completion of ACP activities is associated with individual and healthcare system factors. With an international population, differing healthcare systems, and varying cultural perspectives, these results are similar to findings from prior research showing that completion of ACP activities is associated with older age, female gender, multimorbidity and hospitalization. Uniquely, our findings suggest that higher ACP completion is associated with higher quality primary care and providing informal caregiving.
Comparison with existing literature
A description and analysis of country-specific differences in each ACP activity from this 2014 IHP survey have been published (12). Our analysis sought to identify associations of ACP activities and individual and healthcare system factors. Previous research has shown that a regular source of care (4) and outpatient visits with a general practitioner (10,15) are associated with increased ACP completion. More involved primary care providers can result in fewer in-hospital deaths and more use of home health or hospice care (16). Medicare spending and ICU utilization are lower in US hospital referral regions with higher ratios of primary care versus specialist providers. Hospice utilization is also lower in these regions, suggesting that primary care providers may be providing primary palliative care (17). Clinicians consider delivering primary palliative care, including ACP, to be appropriate in primary care practice (18) particularly for specific groups of patients such as those with terminal illness (10). Recent studies seek to improve the identification of appropriate patients (19,20) and enhance the capacity of primary care physicians to facilitate ACP (21,22). Our analysis suggests that these efforts may be more successful in practices providing higher quality primary care overall.
Individuals also interact with the healthcare system as informal caregivers. We found informal caregiving to be meaningfully associated with increased ACP completion. Since healthcare utilization through emergency or inpatient care also is associated with such an increase, we postulate that the caregiver role exposes an individual to the health care system; caregivers are in effect ‘utilizers by proxy’. Previous qualitative research has identified the death of a loved one as a motivating factor to complete ACP (7); this report is the first study identifying a significant association between informal caregiving and ACP completion.
Strengths and limitations
The primary strength of this study is that these are the only international data, collected through representative sampling, of individuals’ responses regarding ACP, currently a topic of clinical and policy debates (23). This study has several limitations. The analysis is limited to data from the IHP Survey and other factors, patient preferences for example, are not measured. Surveys were conducted in countries with predominantly white populations, and respondent race was only asked in the USA and England. Therefore, the impact of race and ethnicity is unknown. Additionally, this survey focused on individuals age 55 or older, and younger populations may participate in ACP differently. Our analysis took into account only the number of ACP activities completed. Whether there is a sequencing effect of patient completion of ACP activities was not directly addressed in the survey. Finally, despite the association between higher quality primary care and ACP completion, we cannot say whether ACP happened in the primary care setting or whether increased ACP completion is simply more common in healthcare systems that embody quality primary care.
Implications for research and/or practice
This study highlights opportunities to increase ACP activities. ACP seems to occur when a person is in closer proximity to mortality, through age and multimorbidity, and interacting with the healthcare system, either directly through hospitalization or while serving as an informal caregiver. These individuals are seen in primary care practice and higher quality practices may be better positioned to facilitate ACP. Regional and national policies and strategies may promote ACP in community-based and primary care settings. For example, the Centers for Medicare and Medicaid Services in the USA recently implemented healthcare provider reimbursement for ACP conversations, though impact on ACP activities remains unknown (24). Healthcare organizations and researchers are striving to identify consensus quality measures of ACP, which may also promote ACP in multiple settings (25). Future IHP Surveys, as well as country-specific evaluations, are well-positioned to evaluate the impact or consequences of policy changes. Additional research could elucidate the elements of quality primary care that facilitate ACP completion. Policy efforts aimed at enhancing completion of ACP should consider the overall context of improving primary care quality as a facilitation mechanism.
Declaration
Funding: Research reported in this publication was supported by the National Institute On Aging of the National Institutes of Health under Award Number K76AG054782 (PI Lum) and a National Palliative Care Research Center Junior Faculty Career Development Grant (PI Lum) from the National Palliative Care Research Center. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the Department of Veterans Affairs. The sponsors had no role in the design, methods, or preparation of the manuscript.
Ethical Approval: This study was approved by the Colorado Multiple Institutional Review Board
Conflict of interests: The authors declare that there is no conflict of interest. The views in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
Supplementary Material
Acknowledgements
This study was presented at the North American Primary Care Research Group Annual Meeting, November 12–16, 2016, Colorado Springs, Colorado.
References
- 1. Weathers E, O’Caoimh R, Cornally N et al. . Advance care planning: a systematic review of randomised controlled trials conducted with older adults. Maturitas 2016; 91: 101–9. [DOI] [PubMed] [Google Scholar]
- 2. Brinkman-Stoppelenburg A, Rietjens JA, van der Heide A. The effects of advance care planning on end-of-life care: a systematic review. Palliat Med 2014; 28: 1000–25. [DOI] [PubMed] [Google Scholar]
- 3. Alano GJ, Pekmezaris R, Tai JY et al. . Factors influencing older adults to complete advance directives. Palliat Support Care 2010; 8: 267–75. [DOI] [PubMed] [Google Scholar]
- 4. Rao JK, Anderson LA, Lin FC. et al. . Completion of advance directives among U.S. consumers. Am J Prev Med 2014; 46: 65–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lingler JH, Hirschman KB, Garand L et al. . Frequency and correlates of advance planning among cognitively impaired older adults. Am J Geriatr Psychiatry 2008; 16: 643–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lovell A, Yates P. Advance care planning in palliative care: a systematic literature review of the contextual factors influencing its uptake 2008-2012. Palliat Med 2014; 28: 1026–35. [DOI] [PubMed] [Google Scholar]
- 7. Carr D. The social stratification of older adults’ preparations for end-of-life health care. J Health Soc Behav 2012; 53: 297–312. [DOI] [PubMed] [Google Scholar]
- 8. Khosla N, Curl AL, Washington KT. Trends in engagement in advance care planning behaviors and the role of socioeconomic status. Am J Hosp Palliat Care 2016; 33: 651–7. [DOI] [PubMed] [Google Scholar]
- 9. Meeussen K, Van den Block L, Echteld M et al. . Advance care planning in Belgium and The Netherlands: a nationwide retrospective study via sentinel networks of general practitioners. J Pain Symptom Manage 2011; 42: 565–77. [DOI] [PubMed] [Google Scholar]
- 10. Glaudemans JJ, Moll van Charante EP, Willems DL. Advance care planning in primary care, only for severely ill patients? a structured review. Fam Pract 2015; 32: 16–26. [DOI] [PubMed] [Google Scholar]
- 11. Macinko J, Guanais FC. Population experiences of primary care in 11 organization for economic cooperation and development countries. Int J Qual Health Care 2015; 27: 443–50. [DOI] [PubMed] [Google Scholar]
- 12. Osborn R, Moulds D, Squires D et al. . International survey of older adults finds shortcomings in access, coordination, and patient-centered care. Health Aff (Millwood) 2014; 33: 2247–55. [DOI] [PubMed] [Google Scholar]
- 13. R Core Team. R: A Language and Environment for Statistical Computing. Vienna: R Foundation for Statistical Computing; 2014. [Google Scholar]
- 14. Bates D, Maechler M, Bolker B et al. . Fitting linear mixed-effects models using lme4. Journal of Statistical Software. 2015; 67: 1–48. [Google Scholar]
- 15. Mason B, Boyd K, Murray SA et al. . Developing a computerised search to help UK general practices identify more patients for palliative care planning: a feasibility study. BMC Family Practice 2015 August 8. [Epub ahead of print] doi:10.1186/s 12875-015-0312-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Advance Care Planning. Medicare Learning Network www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/Downloads/AdvanceCarePlanning.pdf (accessed on 25 October 2017).
- 17. Johnson SB, Butow PN, Kerridge I et al. . How well do current measures assess the impact of advance care planning on concordance between patient preferences for end of life care and the care received: a methodological review. Jr Pain Symptom Manage. 2017 September 21. [Epub ahead of print] doi:10.1016/j.jpainsymman.2017.09.008. [DOI] [PubMed] [Google Scholar]
- 18. Wu P, Lorenz KA, Chodosh J. Advance care planning among the oldest old. J Palliat Med 2008; 11: 152–7. [DOI] [PubMed] [Google Scholar]
- 19. Kim SL, Tarn DM. Effect of primary care involvement on end-of-life care outcomes: a systematic review. J Am Geriatr Soc 2016; 64: 1968–74. [DOI] [PubMed] [Google Scholar]
- 20. Ankuda CK, Petterson SM, Wingrove P et al. . Regional variation in primary care involvement at the end of life. Ann Fam Med 2017; 15: 63–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Nowels D, Jones J, Nowels CT et al. . Perspectives of primary care providers toward palliative care for their patients. J Am Board Fam Med 2016; 29: 748–58. [DOI] [PubMed] [Google Scholar]
- 22. Thoonsen B, Vissers K, Verhagen S et al. . Training general practitioners in early identification and anticipatory palliative care planning: a randomized controlled trial. BMC Fam Pract 2015; 16: 126–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Dunphy EJ, Conlon SC, O’Brien SA et al. . End-of-life planning with frail patients attending general practice: an exploratory prospective cross-sectional study. Br J Gen Pract 2016; 66: e661–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Gómez-Batiste X, Martínez-Muñoz M, Blay C et al. . Identifying needs and improving palliative care of chronically ill patients: a community-oriented, population-based, public-health approach. Curr Opin Support Palliat Care 2012; 6: 371–8. [DOI] [PubMed] [Google Scholar]
- 25. Fritz Z, Slowther AM, Perkins GD. Resuscitation policy should focus on the patient, not the decision. BMJ 2017; 356: j813. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.