Abstract
Introduction
Healthcare workers are at increased risk for respiratory disorders. The purpose of our respiratory health survey was to estimate the prevalence of current asthma and asthma-like symptoms and their association with workplace exposures and tasks among healthcare workers at a Veterans Administration (VA) Medical Center.
Material and methods
Information on respiratory health and work characteristics, including tasks performed, products used, and exposures, were collected by questionnaire from a convenience sample of workers employed at the VA Medical Center during 2012–2014. Associations of asthma and asthma-like symptoms with cleaning and disinfecting tasks and products as well as exposure to dampness and molds, and construction dust were evaluated using log-binomial regression.
Results
The prevalence of current asthma was 17.6% and almost half of all workers reported asthma-like symptoms. We observed elevated prevalence of current asthma among the VA healthcare workers compared to the U.S. general and working adult populations. Asthma and asthma-like symptoms were significantly associated with mold, dampness, and construction material exposures; cleaning and disinfecting products; and cleaning or disinfecting tasks.
Conclusions
Workplace exposures and tasks associated with current asthma and asthma-like symptoms were identified but further research is needed to investigate the temporal association between workplace exposures and current asthma and asthma-like symptoms.
Keywords: Asthma, Asthma-like symptoms, Healthcare workers, Hospital, Respiratory
1. Introduction
Asthma is a chronic inflammatory disorder of the airways and includes variable and recurring respiratory symptoms (NAEPP, 2007). An estimated 9.7% of ever-employed adults with current asthma in the U.S. have work-related asthma (WRA), which is potentially preventable by reducing exposure to asthmagens in the workplace (Knoeller et al., 2011). Healthcare workers are at an increased risk for WRA, asthma caused by or existing asthma made worse by workplace conditions (Delclos et al., 2007; Pechter et al., 2005; Tarlo et al., 2008), and allergic respiratory diseases (Mazurek and Weissman, 2016). Healthcare workers may be exposed to a variety of agents in the healthcare setting associated with asthma and/or asthma-like symptoms. These agents include latex, indoor air pollution, pharmaceuticals (administering), and chemical products used to disinfect, sterilize, or clean instruments or surfaces (Arif and Delclos, 2012; Delclos et al., 2007; Mirabelli et al., 2007; Pechter et al., 2005; Tarlo et al., 2008). Surveillance data from four states (California, Massachusetts, Michigan, and New Jersey) indicated that healthcare workers accounted for 15.6% of reported WRA cases but represented only 8.0% of the total workforce in those states (Pechter et al., 2005). Specific healthcare occupations have a higher risk of WRA including nurses, nursing aides/technicians, radiology technicians, laboratory workers and cleaners/housekeepers (Mirabelli et al., 2007; Quinn et al., 2015).
In 2000, the U.S. Department of Veterans Affairs and the Centers for Disease Control and Prevention’s National Institute for Occupational Safety and Health (NIOSH) collaborated to examine hypersensitivity to latex proteins in healthcare workers at three Veterans Administration (VA) Medical Centers (Sussman, 2003; Zeiss et al., 2003). Results from the study indicated few symptomatic participants were sensitized to latex, but the prevalence of current asthma was 8.8% (95% CI = 7.6–10.1) and varied by occupation ranging from 0% for dental professionals to 21.4% among respiratory therapists. In 2012, we administered a respiratory health questionnaire survey at one of the three VA Medical Centers to gain insight into the prevalence of current asthma and asthma-like symptoms by occupational group as well as the prevalence of workplace exposures and tasks and their association with current asthma and asthma-like symptoms among participating healthcare workers.
2. Materials and methods
2.1. Study population and data collection
Information on respiratory health and work characteristics was collected by questionnaire from workers employed at the VA Medical Center. Participation in the cross-sectional study was open to all current employees from July 2012 through August 2014. Workers were invited to complete the questionnaire either during normal work hours or on their own time. Attempts were made to enroll workers through employee email, in person outreach, and general advertisements. The participating VA Medical Center and NIOSH human subjects committees approved survey protocol. By completing the questionnaire, the participants indicated consent to take part in the survey.
Questionnaire data were securely collected, entered, stored, and managed using the internet-based Research Electronic Data Capture (REDCap) system. Questionnaire data were directly entered into REDCap by participants completing the computer-based questionnaire or by study coordinators when a participant completed a paper questionnaire. A total of 687 questionnaires were received, of which 44 were excluded because the participant did not consent to participate or did not provide complete data. Eighty one participants submitted more than one questionnaire and only the most complete, earliest dated questionnaire was analyzed for a total of 562 participants.
2.2. Questionnaire
We updated a previously used questionnaire that collected details about demographic characteristics, respiratory health, and occupational characteristics to include questions on workplace exposures and tasks (Zeiss et al., 2003). Participants provided their age at the time of the survey, sex, and race. Race was defined as white, African-American, Asian, American Indian or Alaska Native, Native Hawaiian or other Pacific Islander, and other. We categorized cigarette smoking status as never smoker if workers “smoked less than 100 cigarettes during your lifetime”, former smoker if they “ever smoked cigarettes regularly” but do not “still smoke cigarettes”, and current smoker if they “ever smoked cigarettes regularly” and “still smoke cigarettes”.
Participants provided the total years they worked or trained in healthcare (“seniority”), the number of days per week working at this VA Medical Center, their primary work building, and their current occupation. The VA Medical Center includes multiple buildings of various sizes (ranging from < 50 to > 500 workers), functions (e.g., office building, rehabilitation services, art therapy), and conditions. We limited our analysis to a large subsample of participants working in the main hospital building (n = 347) because the main hospital includes healthcare workers of diverse occupations and recruiting efforts were focused on the main hospital employees. Results for participants working in the other buildings are reported in the Supplemental Material (Supplement Tables 1–3, Fig. 1). Due to small sample size, we combined the current occupations into ten occupational groups: clinical nurses (e.g., non-operating room clinical nurse, clinical nurse specialist, registered nurse) (n = 105), office and administrative support (e.g., administrator, dietician, office/medical records worker, psychologist, social worker, ward clerk) (n = 95), patient care (e.g., nurse practitioner, nursing assistant, occupational therapist, physician assistant, non-surgical physician, physical therapist) (n = 51), clinical and medical laboratory (n = 33), medication dispensing and administration (n = 18), cleaning, laundry, disinfection, and food services (n = 14), facility maintenance and safety (n = 11), surgical (n = 4), technicians/technologists (n = 6), and other occupations (n = 9). We focused our analyses on the three occupational groups in the main hospital with the highest participation: clinical nurses, office and administrative support, and patient care. Participants also reported workplace sterilizing, disinfecting, or cleaning tasks; mold, dampness, and construction material exposure; and sterilizing, disinfecting, or cleaning product use.
Fig. 1.
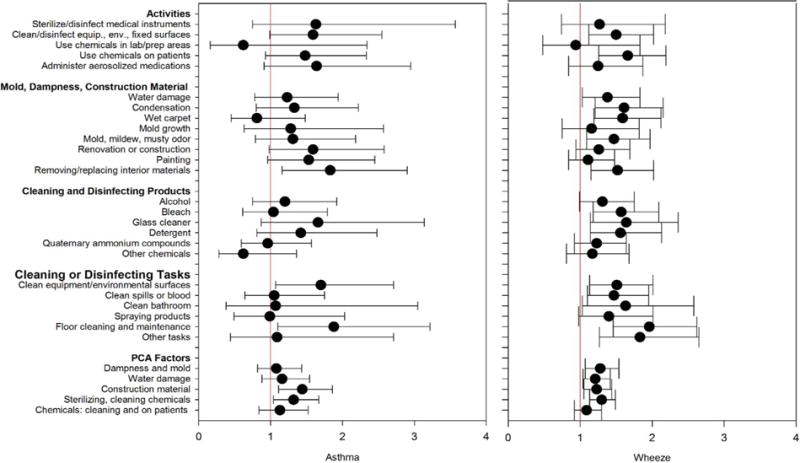
Prevalence ratios (95% CI) of current asthma and wheeze by workplace exposure and tasks, (n = 347).
PCA, Principal components analysis.
Current asthma was defined as a positive response to each of the following three questions: “Have you ever had asthma?”, “Was your asthma confirmed/diagnosed by a doctor or a healthcare professional?”, and “Do you still have asthma?” [(DHHS, 2015; CDC, 2015)]. Participants reported asthma-like symptoms including “wheezing or whistling in your chest at any time”, “woken up with a feeling of tightness in your chest first thing in the morning”, “attack of shortness of breath when not doing anything strenuous”, “attack of shortness of breath that came on after you stopped exercising”, and “woken up at night by an attack of shortness of breath” within the 12 months prior to and also the 4 weeks prior to the administration of the questionnaire. Participants answering “yes” to any of the above asthma-like symptoms questions, having an attack of asthma at any time in the last 12 months or 4 weeks, or currently taking medicines for asthma were considered to have “breathing problems”. Evidence of possible work-relatedness was assessed among participants reporting breathing problems by asking about the status of breathing problems when away from work (i.e., on vacation, on days off, or on a lay-off). Participants ever having at least one of the following: atopic dermatitis, allergic eye symptoms, or seasonal allergic rhinitis were classified as having a positive allergic status.
Statistical analyses were performed using SAS® V.9.3 (SAS Institute Inc. Cary, NC) and JMP V.9.0 (SAS Institute Inc.). Frequencies of demographic characteristics, occupational characteristics, current asthma, and asthma-like symptoms were calculated overall and for the three most common participating occupational groups in the main hospital. Frequencies of asthma-like symptoms and workplace exposures and tasks overall and by current asthma status were also calculated. Pearson’s chi-square tests or Fisher’s exact tests (when expected cell count was < 5) were used to compare frequencies and were considered significant at p < 0.05.
Current asthma and asthma-like symptoms were relatively common in this cross-sectional sample of workers, so we calculated prevalence ratios (PRs) with corresponding 95% confidence intervals (CI) by workplace exposures and tasks with the SAS Proc Genmod log-binomial regression procedure. Negative binomial regression was used as an alternative to account for overdispersion when a variable’s variance was greater than its mean. Adjusted PRs for age, sex, race, smoking status, and allergic status were calculated but are not presented because the adjusted models did not converge.
Hierarchical clustering was performed on respiratory symptom questions (wheeze, chest tightness, shortness of breath, asthma attack, cough, phlegm, nose symptoms, eye symptoms, and sinus symptoms) using JMP software to group participants based on similarity of their profile with regards to respiratory symptom responses. Clusters were combined using Ward’s linkage method and Euclidean distance measure (Friesen et al., 2015). A plot of the dendrogram, which is a tree diagram illustrating the hierarchical clustering pattern, combined with a heat-map was generated from two way clustering of the participants by the variables to visually identify the high loading variables in each cluster. Four clusters were extracted from the cluster tree and were examined for similar patterns in the variables included in the cluster analysis and by calculating within-cluster mean response values to indicate the percent of workers with a “yes” response to symptom questions. The four symptom groups were labelled: no/low symptoms (no symptoms or some wheezing with irritation), upper chest symptoms (cough, phlegm, irritation, with or without wheeze), lower chest symptoms (shortness of breath, asthma attack, with or without irritation), and mixed symptoms (wheeze, cough, irritation with or without wheeze). The symptom grouping was used as an outcome variable with the SAS Proc Genmod procedure to explore the association with work exposure and tasks (Supplement Fig. 1).
Principal components analysis (PCA) was performed with JMP software using workplace exposure and task input variables to reduce the dimensionality of data and to group correlated variables sharing common, underlying characteristics (Burstyn, 2004; Preller et al., 2004). To characterize dampness and mold exposure at work, responses to five questions were used as input variables and included water damage, condensation, wet carpet, mold growth, and mold odor. Exposure to construction materials was characterized by responses to the four input variables: renovation or construction work at primary workstation; painting; removing and replacing walls, woodwork, or partitions; and removing and replacing carpets. To characterize mixed exposure to chemicals, entry questions to six modules were used as input variables and included sterilizing or disinfecting medical instruments; cleaning or disinfecting equipment, environmental, or fixed surfaces; using chemicals in laboratory or patient/chemical preparation areas; using chemicals, adhesives, antiseptics, alcohols, or solvents on patients; administering aerosolized medications to patients; and exposure to dental-related chemicals. Principal components with Eigenvalues > 1 were transformed using Varimax rotation to maximize the loadings to a few variables to better differentiate the factors and simplify interpretation; the resulting factors were labelled based on high (> 0.4) factor loadings. PCA on the dampness and mold questions resulted in two rotated factors, labelled as evidence of dampness and mold and evidence of water damage. The construction exposure questions resulted in one factor including loadings from all construction material input variables. The mixed exposure questions resulted in two factors labelled exposure to sterilizing, cleaning, disinfecting chemicals and exposure to cleaning chemicals, chemicals used on patients. We used factor scores as metrics of work exposure and tasks to model current asthma and symptoms using Proc Genmod procedure because factor scores are orthogonal and minimize collinearity when used together in a model.
3. Results
The mean age of the 347 participants was 46.5 years (SD = 11.7) and most were female (78.1%), white (91.2%), and never smokers (60.9%) (Table 1). The number of years a participant worked or trained in healthcare ranged from < 1 year to 50 years (mean = 19.2 years, SD = 12.5), and most participants (85.1%) worked more than four days per week at the VA Medical Center. Participants in the three occupational groups were also primarily female (80.4–89.5%), white (86.0–95.2%), never smokers (55.8–70.6%), and worked more than four days per week (79.1–90.4%). (Supplement Tables I–III include results for all participants by building [n = 562].)
Table 1.
Demographic and Occupational Characteristics Overall and by Select Occupational Groups (n = 347).
| All participants N (%) | Clinical nurses N (%) | Office and administrative support N (%) | Patient care N (%) | |
|---|---|---|---|---|
| Total | 347 (100.0) | 105 (30.3) | 95 (27.4) | 51 (14.7) |
| Age quartile | ||||
| 21–37 years | 89 (25.7) | 25 (23.8) | 22 (23.2) | 13 (25.5) |
| 38–49 years | 90 (25.9) | 29 (27.6) | 22 (23.2) | 17 (33.3) |
| 50–56 years | 94 (27.1) | 32 (30.5) | 29 (30.5) | 9 (17.7) |
| 57–73 years | 74 (21.3) | 19 (18.1) | 22 (23.2) | 12 (23.5) |
| Sex | * | * | * | * |
| Female | 271 (78.1) | 94 (89.5) | 83 (87.4) | 41 (80.4) |
| Male | 76 (21.9) | 11 (10.5) | 12 (12.6) | 10 (19.6) |
| Raceb | * | * | * | * |
| White | 312 (91.2) | 100 (95.2) | 87 (91.6) | 43 (86.0) |
| Otherb | 30 (8.8) | 5 (4.8) | 8 (8.4) | 7 (14.0) |
| Smoking statusa | * | * | * | * |
| Never smoker | 210 (60.9) | 58 (55.8) | 58 (61.1) | 36 (70.6) |
| Former smoker | 96 (27.8) | 33 (31.7) | 29 (30.5) | 11 (21.6) |
| Current smoker | 39 (11.3) | 13 (12.5) | 8 (8.4) | 4 (7.8) |
| Seniority quartilea | ||||
| < 1–7 years | 87 (25.1) | 18 (17.1) | 27 (28.7) | 12 (23.5) |
| 8–19 years | 88 (25.4) | 27 (25.7) | 29 (30.9) | 8 (15.7) |
| 20–29 years | 86 (24.9) | 24 (22.9) | 20 (21.3) | 17 (33.3) |
| 30–50 years | 85 (24.6) | 36 (34.3) | 18 (19.2) | 14 (27.5) |
| Days per week workinga | * | * | * | * |
| ≤4 days | 51 (14.9) | 22 (21.0) | 9 (9.6) | 9 (18.8) |
| > 4 days | 291 (85.1) | 83 (79.1) | 85 (90.4) | 39 (81.3) |
N, number.
In all participants, demographic and occupational data were missing for race (n = 5), smoking status (n = 2), seniority (n = 1), and days per week working (n = 5). Demographic and occupational characteristics by occupational group may not add up to the total number in the occupational group due to missing values.
“Other” race category includes African American, Asian, American Indian or Alaska Native, Native Hawaiian or other Pacific Islander, and other.
p- value < 0.05 based on Pearson’s chi-square or Fisher’s exact test.
The prevalence of current asthma in the main hospital participants was 17.6% (Table 2). Most participants with current asthma were classified as having a positive allergic status (88.5%). Among those with current asthma, wheeze was the most reported asthma-like symptom in the past 12 months (91.8%) and in the past four weeks (49.2%) followed by shortness of breath after exercise in the past 12 months (57.4%) and in the past four weeks (44.3%). The analysis by symptom groups created by hierarchical clustering grouped 55.6% of participants into the no/low symptoms group. The upper chest, lower chest, and mixed symptoms groups each included 14.4–15.3% of participants. Of participants with current asthma, 41.0% were in the lower chest symptoms group and 24.6% were in the mixed symptoms group.
Table 2.
Prevalence of Current Asthma and Asthma-like Symptoms Overall and by Select Occupational Groups.
| All participants N (%) n = 347 | Participants with current asthma N (%) n = 61 | Clinical nurses N (%) n = 105 | Office and administrative support N (%) n = 95 | Patient care N (%) n = 51 | |
|---|---|---|---|---|---|
| Current asthma | 61 (17.6) | 61 (100.0) | 23 (21.9) | 21 (22.1) | 9 (17.6) |
| Positive allergic status a | 221 (63.7) | 54 (88.5) | 66 (62.9) | 73 (76.8) | 31 (60.8) |
| Asthma-like symptoms, past 12 months | |||||
| Wheeze | 123 (35.5) | 56 (91.8) | 41 (39.1) | 33 (34.7) | 14 (27.5) |
| Chest tightness, awoken with | 70 (20.2) | 34 (55.7) | 25 (23.8) | 23 (24.2) | 6 (11.8) |
| Shortness of breath at rest | 64 (18.4) | 33 (54.1) | 20 (19.1) | 19 (20.0) | 9 (17.7) |
| Shortness of breath after exercise | 79 (22.8) | 35 (57.4) | 28 (26.7) | 21 (22.1) | 10 (19.6) |
| Shortness of breath, awoken by | 45 (13.0) | 23 (37.7) | 15 (14.3) | 12 (12.6) | 5 (9.8) |
| Asthma-like symptoms, past 4 weeks | |||||
| Wheeze | 62 (17.9) | 30 (49.2) | 22 (21.0) | 18 (19.0) | 7 (13.7) |
| Chest tightness, awoken with | 34 (9.8) | 17 (27.9) | 11 (10.5) | 10 (10.5) | 2 (3.9) |
| Shortness of breath at rest | 38 (11.0) | 21 (34.4) | 14 (13.3) | 8 (8.4) | 4 (7.8) |
| Shortness of breath after exercise | 49 (14.1) | 27 (44.3) | 20 (19.1) | 10 (10.5) | 6 (11.8) |
| Shortness of breath, awoken by | 22 (6.3) | 14 (23.0) | 8 (7.6) | 6 (6.3) | 1 (2.0) |
| Symptom groups | |||||
| No/low symptoms | 193 (55.6) | 14 (23.0) | 62 (59.1) | 47 (49.5) | 34 (66.7) |
| Upper chest symptoms | 51 (14.7) | 7 (11.5) | 11 (10.5) | 16 (16.8) | 6 (11.8) |
| Lower chest symptoms | 53 (15.3) | 25 (41.0) | 19 (18.1) | 17 (17.9) | 5 (9.8) |
| Mixed symptoms | 50 (14.4) | 15 (24.6) | 13 (12.4) | 15 (15.8) | 6 (11.8) |
| Breathing problems b | 166 (47.8) | 60 (98.4) | 53 (50.4) | 45 (47.4) | 19 (37.3) |
| Improved away from work | 61 (38.4) | 24 (40.7) | 27 (50.9) | 11 (24.4) | 9 (47.4) |
N, number.
Positive allergic status was defined as at least one of the following reported conditions: atopic dermatitis, allergic eye symptoms, or seasonal allergic rhinitis.
In all participants, 6 participants were missing data for status of breathing problems when away from work. The percentage for Improved away from work is calculated using the number with breathing problems reporting the status of breathing problems when away from work as the denominator specific to each column.
The prevalence of current asthma was 21.9% for clinical nurses, 22.1% for office and administrative support workers, and 17.6% for patient care workers (Table 2). There were no significant differences between symptoms for these three occupational groups. Approximately two-thirds of patient care workers were in the no/low symptoms group (66.7%) followed by 59.1% of clinical nurses and 49.5% of office and administrative support workers.
Of 166 participants with breathing problems reporting the status of these problems when away from work, 38.4% reported their breathing problems were better away from work which may indicate evidence of possible work-related breathing problems (Table 2. Among these participants reporting improved breathing problems away from work, 44.3% (n = 27) were clinical nurses, 18.0% (n = 11) were office and administrative support workers, 14.8% (n = 9) were patient care workers (Table 2), and the remaining 22.9% (n = 14) had other occupations (data not shown).
Of 162 participants with breathing problems responding (4 missing), 34.6% (n = 56) reported their breathing problems were so severe that they had to take time off work (data not shown). Of 336 participants responding, 2.4% (n = 8) reported they changed a job, job duties, or job location because the job affected their breathing, and 50.0% of the 8 had current asthma. Five of the 8 (62.5%) reported their breathing problems got better with the change (data not shown).
Table 3 shows workplace exposures and tasks reported by workers in the main hospital by current asthma and wheeze. Approximately half of all participants reported cleaning or disinfecting equipment, environmental, or fixed surfaces (51.0%) and 32.0% reported using chemicals, adhesives, antiseptics, alcohols, or solvents on patients. Most participants (71.2%) reported any mold, dampness, and construction material exposure, with the most common of these exposures being renovation or construction exposures (54.5%), painting (50.1%), and water damage (49.0%). Mold, dampness, and construction material exposure were reported by 80.3% with current asthma and 75.6% with wheeze. Renovation or construction exposures were also the most common among participants with current asthma (65.6%) and wheeze (60.2%).Approximately half of all participants in the main hospital reported any cleaning and disinfecting product use (49.3%) and the most commonly reported products used to sterilize, disinfect, or clean were alcohol (32.0%) and quaternary ammonium compounds (32.0%). Over half of participants with current asthma (60.7%) and wheeze (58.5%) reported any cleaning and disinfecting product use. Cleaning or disinfecting tasks were performed by approximately half (48.4%) of all participants and by 59% of participants with current asthma and 58.5% of participants with wheeze. Participants most commonly reported cleaning equipment and environmental surfaces (45.8%) and the prevalence was slightly higher for participants cleaning equipment and environmental surfaces with current asthma (59.0%) and wheeze (56.1%).
Table 3.
Prevalence of Workplace Exposures and Tasks in Current Job a by Current Asthma and Wheeze.
| All participants N (%) n = 347 | Participants with current asthma N (%) n = 61 | Participants with wheeze N (%) n = 123 | |
|---|---|---|---|
| Sterilize or disinfect medical instruments | 18 (5.2) | 5 (8.2) | 8 (6.5) |
| Clean or disinfect equipment, environmental, or fixed surfaces | 177 (51.0) | 38 (62.3) | 75 (61.0) |
| Use chemicals in laboratory or patient/chemical preparation areas | 18 (5.2) | 2 (3.3) | 6 (4.9) |
| Use chemicals, adhesives, antiseptics, alcohols, or solvents on patients | 111 (32.0) | 25 (41.0) | 54 (43.9) |
| Administer aerosolized medications to patients | 37 (10.7) | 10 (16.4) | 16 (13.0) |
| Mold, dampness, construction material exposure (any) | 247 (71.2) | 49 (80.3) | 93 (75.6) |
| Water damage | 170 (49.0) | 33 (54.1) | 70 (56.9) |
| Condensation | 73 (21.0) | 16 (26.2) | 37 (30.1) |
| Wet carpet | 74 (21.3) | 11 (18.0) | 37 (30.1) |
| Mold growth | 32 (9.2) | 7 (11.5) | 13 (10.6) |
| Mold, mildew, musty odor | 74 (21.3) | 16 (26.2) | 35 (28.5) |
| Renovation or construction | 189 (54.5) | 40 (65.6) | 74 (60.2) |
| Painting | 174 (50.1) | 37 (60.7) | 65 (52.9) |
| Removing/replacing interior materials | 147 (42.4) | 35 (57.4) | 65 (52.9) |
| Cleaning and disinfecting products (any) | 171 (49.3) | 37 (60.7) | 72 (58.5) |
| Alcohol | 111 (32.0) | 22 (36.1) | 47 (38.2) |
| Bleach | 77 (22.2) | 14 (23.0) | 38 (30.9) |
| Glass cleaner | 29 (8.4) | 8 (13.1) | 16 (13.0) |
| Detergent | 51 (14.7) | 39 (13.6) | 26 (21.1) |
| Quaternary ammonium compounds | 111 (32.0) | 19 (31.2) | 45 (36.6) |
| Other chemicals b | 52 (15.0) | 6 (9.8) | 21 (17.1) |
| Cleaning or disinfecting tasks (any) | 168 (48.4) | 36 (59.0) | 72 (58.5) |
| Clean equipment and environmental surfaces | 159 (45.8) | 36 (59.0) | 69 (56.1) |
| Clean spills or blood | 93 (26.8) | 17 (27.9) | 43 (35.0) |
| Clean bathroom | 16 (4.6) | 3 (4.9) | 9 (7.3) |
| Spraying products | 40 (11.5) | 7 (11.5) | 19 (15.5) |
| Floor cleaning and maintenance | 40 (11.5) | 12 (19.7) | 25 (20.3) |
| Other tasks | 21 (6.1) | 4 (6.6) | 13 (10.6) |
Workplace exposures or tasks are reported for current job. Dampness and mold, construction material exposure are reported for the two year period prior to the survey.
Other chemicals include formaldehyde, hydrogen peroxide, acid, ammonia, phenolics, floor wax stripper, ethylene oxide, glutaraldehyde, ortho-phthalaldehydes, peracetic acid, and enzymatic cleaners.
Fig. 1 shows a summary of PRs for current asthma and wheeze by exposures and tasks and by PCA rotated factors for dampness and mold, construction material, and mixed exposures to chemicals for the main hospital participants (Supplement Fig. 1 presents PRs for all participants by building). Participants reporting exposure to removing and replacing interior materials had a significantly higher prevalence of current asthma compared to participants not exposed (PR = 1.83, [1.16–2.90]). Participants exposed to the tasks of cleaning equipment and environmental surfaces (PR = 1.70, [1.07–2.71]) and floor cleaning and maintenance (PR = 1.88, [1.10–3.22]) also had significantly higher prevalence of current asthma compared to participants not exposed. Participants cleaning or disinfecting surfaces (PR = 1.50, [1.12–2.02]) and using chemicals on patients (PR = 1.66, [1.26–2.19]) had significantly higher PRs of wheeze compared to those not performing these tasks. Participants exposed to a variety of mold, dampness, and construction materials; cleaning and disinfecting products (including bleach (PR = 1.57, [1.18–2.09]), glass cleaner (PR = 1.64, [1.14–2.36]), and detergent (PR = 1.56, [1.14–2.13])); and cleaning and disinfecting tasks (cleaning equipment and environmental surfaces (PR = 1.51, [1.13–2.01]); cleaning spills or blood (PR = 1.47, [1.10–1.95]); cleaning bathrooms (PR = 1.63, [1.03–2.58]); floor cleaning and maintenance (PR = 1.96, [1.46–2.62]); and other cleaning tasks (PR = 1.83, [1.27–2.65]) had significantly higher PRs for wheeze compared to participants not exposed. The dampness and mold and water damage PCA factors had significantly elevated prevalence of wheeze, and the construction exposure at work factor and mixed exposure to sterilizing, cleaning, disinfecting chemicals factor had significantly higher prevalence of current asthma and wheeze.
In an analysis determining the PRs of current asthma by work exposures and tasks for occupation groups (results not shown), clinical nurses had significantly higher PRs for current asthma with exposure to renovation or construction (PR = 4.27, [1.35–13.47]), painting (PR = 6.73, [1.66–27.18]), and removing and replacing interior materials (PR = 3.00, [1.28–7.01]) compared to unexposed clinical nurses. Clinical nurses also had a significantly higher prevalence of current asthma with exposure to floor cleaning and maintenance (PR = 2.41, [1.20–4.86]). The PRs for current asthma among office and administrative support workers were significantly higher among workers using detergent (PR = 2.47, [1.00–6.08]) and cleaning equipment and environmental surfaces (PR = 2.81, [1.38–5.72]). Patient care workers sterilizing or disinfecting medical instruments (PR = 3.36, [1.02–11.09]) had a significantly higher PR for current asthma compared to patient care participants not performing this activity. PRs were also significantly higher for current asthma among patient care participants using glass cleaner (PR = 4.57, [1.59–13.10]), cleaning bathrooms (PR = 4.57, [1.59–13.10]), and spraying products (deodorant/disinfectant, spray then wipe glass) (PR = 3.36, [1.02–11.09]).
4. Discussion
Our study identifies exposures and tasks in a workplace where the prevalence of current asthma is high and the risk for current asthma and asthma-like symptoms may be elevated. Results suggest that workplace exposures do affect current asthma and symptoms in this sample, and prevention efforts focused on mitigating exposures may benefit workers and reduce the prevalence of current asthma and symptoms.
Results from our study, and other studies that monitored tasks and exposure in workers, indicated other healthcare occupations, in addition to housekeepers and cleaners, use cleaning products and disinfectants (Quinn et al., 2015; Saito et al., 2015). The tasks performed and products used may vary by occupation and include complex chemical mixtures (Quinn et al., 2015). While substitution of an agent is the preferred occupational asthma prevention approach, many of the products are necessary in the hospital setting to prevent healthcare-associated infections in patients, staff, and visitors (Heederik et al., 2012; Quinn et al., 2015). Using results from our study to focus on minimizing exposures and tasks associated with health effects but not directly related to preventing healthcare-associated infections may help reduce the respiratory disease and symptom burden in workers. For example, our results suggest construction-related exposures in this healthcare workplace are of concern but these exposures may be reduced if performing renovations or painting on weekends, when fewer workers are in the vicinity, or inside temporary containment structures. Construction-related exposures are important to minimize because construction, renovation, and remodelling materials and chemicals are often associated with respiratory symptoms and asthma. Dampness and mold exposures were also associated with current asthma and asthma-like symptoms in our sample. Dampness or excess moisture in buildings can cause growth of mold, fungi, and bacteria; the release of volatile organic compounds; and the breakdown of building materials which are associated with respiratory symptoms, asthma, hypersensitivity pneu-monitis, and other respiratory outcomes (NIOSH, 2012) and work-related respiratory symptoms in hospital workers (Cox-Ganser et al., 2009). Dampness and mold exposure may put an individual at risk for progression to a more severe disease if exposure continues and can lead to costly building repairs of water-damaged materials (NIOSH, 2012). Regularly inspecting building areas for dampness and remediating damaged areas may help reduce symptoms related to dampness and mold exposure (NIOSH, 2012). Minimizing the use of cleaning, disinfecting, or sterilizing products associated with health effects when suitable in non-patient care areas may also help reduce exposure without increasing the risk of healthcare-associated infections.
Continued exposure in people with WRA is associated with worsening of symptoms (Chan-Yeung and Malo, 1995) which is why workers with persistent or worsening asthma symptoms while at work are encouraged to see a healthcare provider (Baur et al., 2012; Tarlo et al., 2008). Whether symptomatic workers will need to control exposure in some manner to improve asthma and manage symptoms will depend on the asthma diagnosis, therefore confirmation of asthma and determination of work-relatedness and onset should be done first (Baur et al., 2012; Tarlo et al., 2008). Alternative work assignments are commonly suggested to help reduce symptoms and asthma exacerbation but are not always possible in some occupations where cleaning, disinfecting, and sterilizing tasks are a crucial part of the job. Implementing other types of controls such as eliminating a product, substituting a product with, for example, use of UV light as a non-chemical alternative to disinfection, applying engineering or administrative controls, or using personal protective equipment may help reduce exposures in the work environment (Baur et al., 2012; Heederik et al., 2012).
We noted a high prevalence classified as having a positive allergic status in our sample. Workers with a positive allergic status may potentially react and be sensitized to an occupational or environmental allergen and have allergic symptoms. Respiratory allergic conditions are associated with direct and indirect costs, including lost work days, and affect quality of life (Mazurek and Weissman, 2016). Rhinitis, which was not identified specifically in our study but included in the allergic status classification, may precede asthma, is associated with asthma, and may be an early marker of WRA (Mazurek and Weissman, 2016).
The prevalence of current asthma among participating VA health-care workers in the main hospital was 17.6% (95% CI = 13.5–21.5). The prevalence was among all 562 participating workers was 18.3% (95% CI = 15.1–21.5. The results of the state-specific 2013 Behavioral Risk Factor Surveillance System (BRFSS) survey indicated the prevalence of current asthma in a representative sample of the Wisconsin adult general population ≥ 18 years of age was 10.4% (95% CI = 9.2–11.6) and 9.0% (95% CI = 8.8–9.1) in the U.S. general population (DHHS, 2015). Wisconsin-specific estimates of current asthma by industry and occupation among employed adults indicated the highest prevalence of current asthma was in the healthcare and social assistance industry (11.4%, 95% CI = 6.8–15.9) (Dodd and Mazurek, 2016). In a representative sample of U.S. working adults ≥ 18 years of age (National Health Interview Survey 2004–2011), the prevalence of asthma was 7.5% (95% CI = 6.6–8.4) for health diagnosing and treating practitioners and 10.0% (95% CI = 8.4–11.5) for nursing, psychiatric, and home health aides (CDC, 2015). The 95% CIs for the VA study, BRFSS, and NHIS current asthma prevalence estimates were calculated using the formula: % prevalence ± t (standard error of the prevalence [sep]), where t is the z distribution value of 1.96. Our results indicate a statistically higher asthma burden among healthcare workers at the VA Medical Center compared to the U.S. general and working adult populations.
Our study adds value to the literature by examining the association between current asthma and asthma-like symptoms and workplace exposures and tasks, however, there are limitations to consider. Since our study was cross-sectional and used a convenience sample of current workers, temporal associations were not determined between employment at the VA Medical Center and current asthma even though some participants did report improvements in their symptoms when away from work which may suggest work-relatedness. Workers with current asthma or asthma-like symptoms may be overrepresented in the study due to self-selection bias. Our prevalence estimates may be influenced by workers with asthma selecting into or out of occupations and workplace exposures. For example, occupations perceived to have fewer exposures might attract and retain individuals with current asthma or asthma-like symptoms thus inflating the prevalence in the occupation. Individuals with current asthma or symptoms may select out of certain occupations, deflating the prevalence. Therefore, our results may be subject to healthy worker survivor effect since workers with asthma or asthma-like symptoms are more likely to reduce their workplace exposures by changing jobs or retiring early (Arrighi and Hertz-Picciotto, 1994).
The true response rate is undetermined. A mass email was sent to about 3500 VA employees inviting workers to participate in the survey. However, we are unsure of how many workers opened this email and received information about the survey. Response rates of 17.4% for clinical nurses, 24.2% for office and administrative support occupations, and 37.2% for patient care occupations were estimated for the three occupational groups with the highest participation using the total number of workers in each occupational group as the denominator. While a low participation rate may introduce bias, other studies have shown associations, which are the focus of our study, are still valid even when response rates are low (Eagan et al., 2002; Martikainen et al., 2007; Mealing et al., 2010; Van Loon et al., 2003). We only present results for participating VA Medical Center workers and do not extrapolate findings to all workers at this VA Medical Center or in other occupational groups. Furthermore, our results are not generalizable to workers at other healthcare facilities since healthcare facilities often use different cleaning products and workers perform a variety of occupational tasks specific to the facility. The reported overall response rate is likely an underestimate as the number of total workers in each building was unavailable and would likely suggest a higher response rate in the main hospital building. We compared VA human resources data and sample data using chi-square tests and determined that the sample age and sex distributions in our study were significantly different from the eligible population age and sex distributions. The observed age distributions in our sample were lower than those expected in the eligible population for some age categories (30–34, 35–44, and greater than 65 years of age) and higher in other categories (45–54 and 55–64). A higher percent of females participated in our study compared to the distribution of females in the eligible population. Comparisons of current asthma and asthma-like symptoms status were not available for the eligible population of healthcare workers.
Current asthma, asthma-like symptoms, allergic status, and exposures and tasks were self-reported and may be subject to recall and reporting bias and the survey did not include clinical or laboratory data to validate allergic status or current asthma status. Self-reported occupational exposures may be influenced by the asthma status of the respondent which can introduce bias into the results (de Vocht et al., 2005). Furthermore, hospital workers may underestimate their exposures when providing self-reports because they may not know the active ingredients in the products they use (Donnay et al., 2011). We did not account for exposures to products used by other healthcare workers in the vicinity. Real-time or personal sampling of workplace exposure may improve the reliability of exposure results and identify the prevalence of non-cleaning workers exposed when other workers are cleaning.
5. Conclusions
The findings from our study indicate that healthcare workers at this Medical Center have elevated prevalence of current asthma. Workplace exposures and tasks associated with current asthma and asthma-like symptoms were identified and further research is needed to investigate the temporal association between workplace exposures and tasks and current asthma and asthma-like symptoms among healthcare workers. The health and safety of healthcare workers should be considered by monitoring respiratory health and reducing or minimizing harmful workplace exposures in the healthcare setting.
Supplementary Material
Acknowledgments
The authors would like to acknowledge the participating healthcare workers, Douglas Dulaney, Brie Hawley, and Michael Hodgson.
Funding
The authors report that there was no grant funding source for the work that resulted in the article or the preparation of the article. Funding came from the VA and NIOSH.
Appendix A. Supplementary data
Supplementary data associated with this article can be found, in the online version, at http://dx.doi.org/10.1016/j.ijheh.2017.09.001.
Footnotes
Conflict of interest
The authors declare no conflicts of interest.
Institution and ethics approval and informed consent
Data collection was performed at the participating VA Medical Center. The work was reviewed and approved by the Department of Veterans Affairs Human Studies Subcommittee (2825-21) and NIOSH Institutional Review Board-Human Subjects Review Board (12-DRDS-01XP). A waiver of written informed consent was granted for this study and participants provided implied consent.
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the National Institute for Occupational Safety and Health. Mention of product names does not imply endorsement by NIOSH/CDC.
References
- Arif AA, Delclos GL. Association between cleaning-related chemicals and work-related asthma and asthma symptoms among healthcare professionals. Occup Environ Med. 2012;69:35–40. doi: 10.1136/oem.2011.064865. [DOI] [PubMed] [Google Scholar]
- Arrighi HM, Hertz-Picciotto I. The evolving concept of the healthy worker survivor effect. Epidemiology. 1994;5:189–196. doi: 10.1097/00001648-199403000-00009. [DOI] [PubMed] [Google Scholar]
- Baur X, Aasen TB, Burge PS, Heederik D, Henneberger PK, Maestrelli P, Schlünssen V, Vandenplas O, Wilken D. ERS Task Force on the Management of Work-related Asthma,. The management of work-related asthma guidelines: a broader perspective. Eur Respir Rev. 2012;21:125–139. doi: 10.1183/09059180.00004711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burstyn I. Principal component analysis is a powerful instrument in occupational hygiene inquiries. Ann Occup Hyg. 2004;48:655–661. doi: 10.1093/annhyg/meh075. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Current Asthma: Estimated Prevalence by Occupation and Sex. US working adults aged ≥18 years, NHIS 2004–2011. 2015 https://wwwn.cdc.gov/eworld/Data/Current_asthma_Estimated_prevalence_by_occupation_and_sex_US_working_adults_aged_18_years_NHIS_20042011/870 (Accessed 5.10.17)
- Chan-Yeung M, Malo JL. Occupational asthma. N Engl J Med. 1995;333:107–112. doi: 10.1056/NEJM199507133330207. [DOI] [PubMed] [Google Scholar]
- Cox-Ganser JM, Rao CY, Park JH, Schumpert JC, Kreiss K. Asthma and respiratory symptoms in hospital workers related to dampness and biological contaminants. Indoor Air. 2009;19:280–290. doi: 10.1111/j.1600-0668.2009.00586.x. [DOI] [PubMed] [Google Scholar]
- Department of Health and Human Services. Department of Health and Human Services (DHHS) Adult Asthma Data. BRFSS prevalence tables and maps. 2015 https://www.cdc.gov/asthma/brfss/2013/brfssdata.htm (Accessed 5.10.17)
- Delclos GL, Gimeno D, Ariff AA, Burau KD, Carson A, Lusk C, Stock T, Symanski E, Whitehead LW, Zock JP, et al. Occupational risk factors and asthma among health care professionals. Am J Respir Crit Care Med. 2007;175:667–675. doi: 10.1164/rccm.200609-1331OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dodd KE, Mazurek JM. Asthma among employed adults, by industry and occupation-21 states, 2013. MMWR. 2016;65:1325–1331. doi: 10.15585/mmwr.mm6547a1. [DOI] [PubMed] [Google Scholar]
- Donnay C, Denis MA, Magis R, Fevotte J, Massin N, Dumas O, Pin I, Choudat D, Kauffmann F, Le Moual N. Under-estimation of self-reported occupational exposure by questionnaire in hospital workers. Occup Environ Med. 2011;68:611–617. doi: 10.1136/oem.2010.061671. [DOI] [PubMed] [Google Scholar]
- Eagan TML, Eide GE, Gulsvik A, Bakke PS. Nonresponse in a community cohort study – Predictors and consequences for exposure-disease associations. J Clin Epidemiol. 2002;55:775–781. doi: 10.1016/s0895-4356(02)00431-6. [DOI] [PubMed] [Google Scholar]
- Friesen MC, Shortreed SM, Wheeler DC, Burstyn I, Vermeulen R, Pronk A, Colt JS, Baris D, Karagas MR, Schwenn M, et al. Using hierarchical cluster models to systematically identify groups of jobs with similar occupational questionnaire response patterns to assist rule-based expert exposure assessment in population-based studies. Ann Occup Hyg. 2015;59:455–466. doi: 10.1093/annhyg/meu101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heederik D, Henneberger PK, Redlich CA. Primary prevention: exposure reduction, skin exposure and respiratory protection. Eur Respir Rev. 2012;21:112–124. doi: 10.1183/09059180.00005111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knoeller GE, Mazurek JM, Moorman JE. Work-related asthma among adults with current asthma in 33 states and DC: evidence from the Asthma Call-Back Survey, 2006-2007. Public Health Rep. 2011;126:603–611. doi: 10.1177/003335491112600419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martikainen P, Laaksonen M, Piha K, Lallukka T. Does survey non-response bias the association between occupational social class and health? Scand J Public Health. 2007;35:212–215. doi: 10.1080/14034940600996563. [DOI] [PubMed] [Google Scholar]
- Mazurek JM, Weissman DN. Occupational respiratory allergic diseases in healthcare workers. Curr Allergy Asthma Rep. 2016;16:1–10. doi: 10.1007/s11882-016-0657-y. [DOI] [PubMed] [Google Scholar]
- Mealing NM, Banks E, Jorm LR, Steel DG, Clements MS, Rogers KD. Investigation of relative risk estimates from studies of the same population with contrasting response rates and designs. BMC Med Res Methodol. 2010;10(26) doi: 10.1186/1471-2288-10-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mirabelli MC, Zock JP, Plana E, Antó JM, Benke G, Blanc PD, Dahlman-Höglund A, Jarvis DL, Kromhout H, Lillienberg L, et al. Occupational risk factors for asthma among nurses and related healthcare professionals in an international study. Occup Environ Med. 2007;64:474–479. doi: 10.1136/oem.2006.031203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Asthma Education and Prevention Program. Expert panel report 3 (EPR- 3): Guidelines for the diagnosis and management of asthma-summary report 2007. J Allergy Clin Immunol. 2007;120:S94–138. doi: 10.1016/j.jaci.2007.09.043. [DOI] [PubMed] [Google Scholar]
- National Institute for Occupational Safety and Health. NIOSH Alert: Preventing Occupational Respiratory Disease from Exposures Caused by Dampness in Office Buildings. Schools, and other nonindustrial buildings. 2012 https://www.cdc.gov/niosh/docs/2013-102/pdfs/2013-102.pdf (Accessed 5.10.17)
- Pechter E, Davis LK, Tumpowsky C, Flattery J, Harrison R, Reinisch F, Reilly M, Rosenman KD, Schill DP, Valiante D, et al. Work-related asthma among health care workers: surveillance data from california, massachusetts, michigan, and new Jersey, 1993–1997. Am J Ind Med. 2005;47:265–275. doi: 10.1002/ajim.20138. [DOI] [PubMed] [Google Scholar]
- Preller L, Burstyn I, De Pater N, Kromhout H. Characteristics of peaks of inhalation exposure to organic solvents. Ann Occup Hyg. 2004;48:643–652. doi: 10.1093/annhyg/meh045. [DOI] [PubMed] [Google Scholar]
- Quinn MM, Henneberger PK, Braun B, Delclos GL, Fagan K, Huang V, Knaack JL, Kusek L, Lee SJ, Le Moual N, et al. Cleaning and disinfecting environmental surfaces in health care: toward an integrated framework for infection and occupational illness prevention. Am J Infect Control. 2015;43(5):424–434. doi: 10.1016/j.ajic.2015.01.029. [DOI] [PubMed] [Google Scholar]
- Saito R, Virji MA, Henneberger PK, Humann MJ, Lebouf RF, Stanton ML. Characterization of cleaning and disinfecting tasks and product use among hospital occupations. Am J Ind Med. 2015;58:101–111. doi: 10.1002/ajim.22393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sussman G. Lessons learned from latex allergy. Ann Allergy Asthma Immunol. 2003;91:510–511. doi: 10.1016/S1081-1206(10)61525-6. [DOI] [PubMed] [Google Scholar]
- Tarlo SM, Balmes J, Balkissoon R, Beach J, Beckett W, Bernstein D, Blanc PD, Brooks SM, Cowl CT, Daroowalla F, et al. Diagnosis and management of work-related asthma: american college of chest physicians consensus statement. Chest. 2008;134(4):1S–41S. doi: 10.1378/chest.08-0201. [DOI] [PubMed] [Google Scholar]
- Van Loon AJM, Tijhuis M, Picavet HSJ, Surtees PG, Ormel J. Survey non-response in the Netherlands: effects on prevalence estimates and associations. Ann Epidemiol. 2003;13(2):105–110. doi: 10.1016/s1047-2797(02)00257-0. [DOI] [PubMed] [Google Scholar]
- Zeiss CR, Gomas A, Murphy FM, Weissman DN, Hodgson M, Foster D, Dejativongse S, Colella K, Kestenberg K, Kurup VP, et al. Latex hypersensitivity in Department of Veterans Affairs health care workers Glove use, symptoms, and sensitization. Ann Allergy Asthma Immunol. 2003;91:539–545. doi: 10.1016/S1081-1206(10)61531-1. [DOI] [PubMed] [Google Scholar]
- de Vocht F, Zock J, Kromhout H, Sunyer J, Antó JM, Burney P, Kogevinas M. Comparison of self-reported occupational exposure with a job exposure matrix in an international community-based study on asthma. Am J Ind Med. 2005;47:434–442. doi: 10.1002/ajim.20154. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


