Abstract
Uterine torsion is a rare condition which is part of a spectrum of gynecological emergencies. If diagnosis is delayed or the condition is left untreated, severe consequences such as infertility and life-threatening complications can arise. As presenting features are often non-specific and can be similar to commonly encountered gastrointestinal and urinary conditions, computed tomography is usually the first imaging modality utilized in an emergency setting. It is therefore important that the radiologist is familiar with recognizing computed tomography features of uterine torsion. We share our findings in a patient with uterine torsion in a non-gravid uterus, diagnosed on contrast-enhanced computed tomography with multiplanar reconstruction.
Keywords: Uterine torsion, adnexal torsion, ovarian torsion, computed tomography, ultrasonography, genitourinary
CASE REPORT
A nulliparous, post-menopausal 52-year-old lady presented to the emergency department with a 2-day history of worsening lower abdominal pain. She reported a background of gradual increase in abdominal girth for a year.
On physical examination, there was a tender, palpable central abdominal mass which was globular and approximately the size of a second trimester pregnancy. Vaginal examination revealed no mass or discharge, and cervical excitation test was negative. Digital rectal examination revealed an empty rectum with no palpable mass or blood. Preliminary blood tests showed normal hemoglobin, white blood cell count and electrolyte levels. Tumour markers (carcinoembryonic antigen, CA-125 and alpha-fetoprotein) were not raised. Serum beta human chorionic gonadotropin (hCG) was negative.
Computed tomography (CT) of the abdomen and pelvis was performed in the emergency department as the patient’s symptoms were unrelenting despite analgesia. On the CT, the uterus was severely enlarged, measuring 23.0 × 16.6 × 25.1 cm (transverse × anteroposterior × craniocaudal). In addition, there was a whorled structure in the right hemipelvis representing a twisted lower uterine segment, indicating torsion of the uterus (Fig. 1 & 2). The bilateral adnexa and ovarian veins were incorporated into the whorled structure, indicating torsion of the adnexal structures as well.
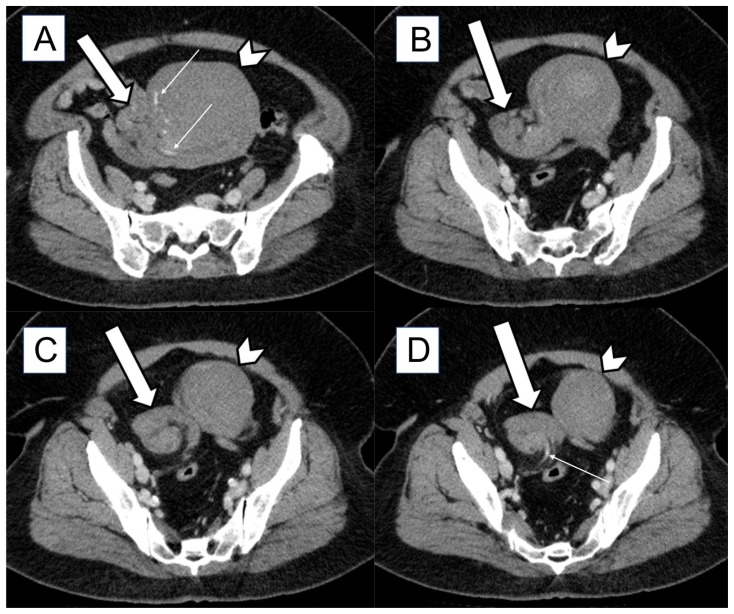
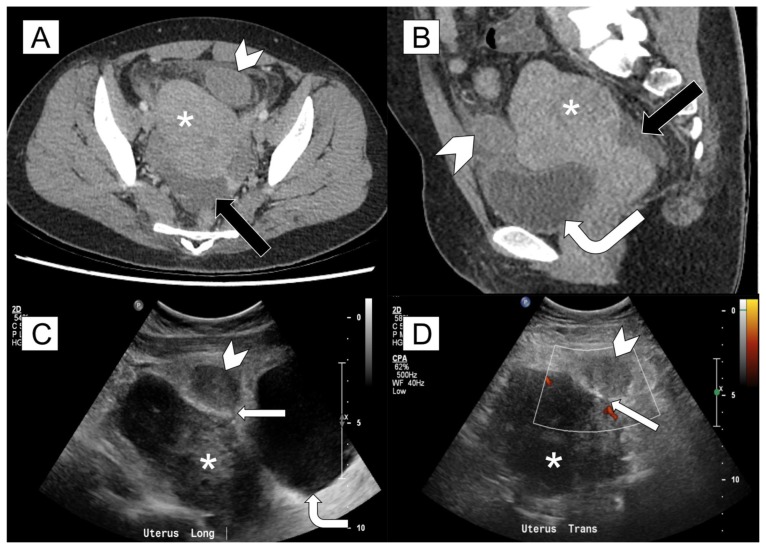
Figure 1.
52-year-old nulliparous, menopausal lady with torsion of the uterus and adnexa
FINDINGS: Axial contrast-enhanced CT of abdomen and pelvis in the portal venous phase from superior to inferior (A to D) demonstrates the uterus (white arrowheads) twisted along its long axis, with a whorled structure (white block arrows) in the right hemipelvis representing a twisted lower uterine segment. Also noted is swirling of enhancing vessels (thin white arrows), indicating that both adnexa are incorporated into the whorled structure. The uterus is massive and contains multiple fibroids.
TECHNIQUE: CT (Toshiba Aquilion ONE) portal venous phase, 579 mA, 120 kV, 3.00 mm slice thickness, 80 ml Omnipaque 350
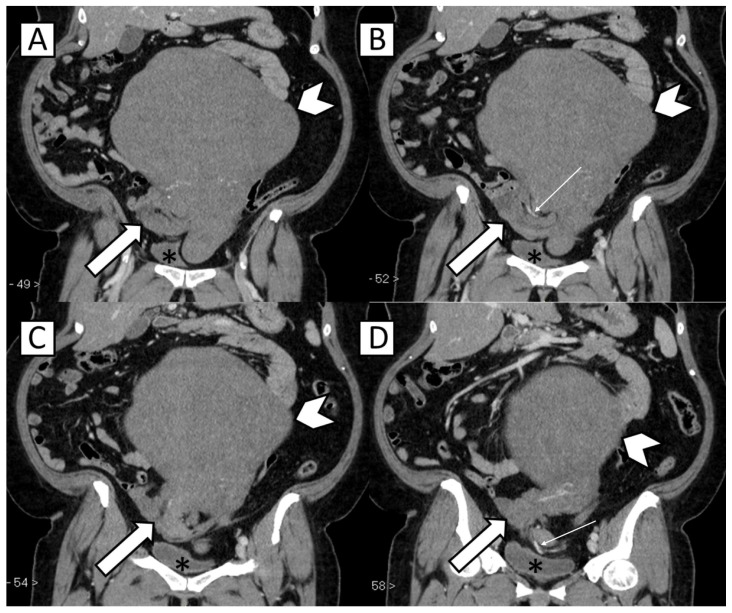
Figure 2.
52-year-old nulliparous, menopausal lady with torsion of the uterus and adnexa
FINDINGS: Coronal contrast-enhanced CT of abdomen and pelvis in the portal venous phase from anterior to posterior (A to D) demonstrates the uterus (white arrowheads) twisted along its long axis, with a whorled structure (white block arrows) in the right hemipelvis representing a twisted lower uterine segment. Also noted is swirling of enhancing vessels (thin white arrows), indicating that both adnexa are incorporated into the whorled structure. The uterus is massive and contains multiple fibroids. The urinary bladder (*) is located caudal to the above-mentioned changes.
TECHNIQUE: CT (Toshiba Aquilion ONE) portal venous phase, 579 mA, 120 kV, 3.00 mm slice thickness, 80 ml Omnipaque 350
The patient subsequently underwent total hysterectomy and bilateral salpingo-oophorectomy, with intra-operative findings confirming an enlarged uterus twisted twice around the cervix (Fig. 3) and congestion of the bilateral ovaries and fallopian tubes. Histology revealed a large, infarcted subserosal leiomyoma and smaller intramual leiomyomas in the uterus, as well as a seromucinous cystadenoma in the left ovary.
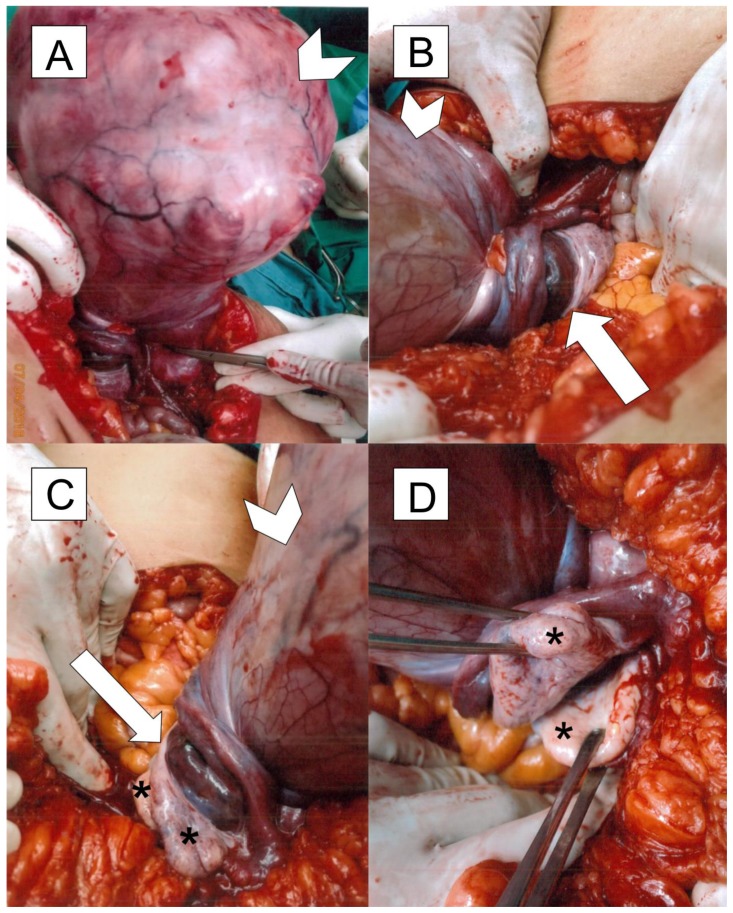
Figure 3.
52-year-old nulliparous, menopausal lady with torsion of the uterus and adnexa
FINDINGS: Intra-operative images show a grossly enlarged uterus (white arrowheads) which is twisted around its cervix (white arrows), along with the adnexa and ovaries (*).
DISCUSSION
Etiology & Demographics
To our knowledge, there has been no reported prevalence for uterine torsion. It has most commonly been reported in cases of pregnancy and underlying congenital uterine anomalies. Uterine torsion encountered in a non-gravid uterus is extremely rare [1,2]. A literature search reveals less than 50 reported cases of uterine torsion in a non-gravid uterus.
Uterine torsion is part of a spectrum of gynecological emergencies, which include conditions such as adnexal torsion. If left untreated, these can result in infertility and life-threatening complications such as infection and bleeding. It is thus important to ensure prompt and accurate diagnosis for good clinical outcomes and preservation of fertility. This can be challenging as the presenting complaints and physical examination findings are often non-specific, resulting in difficult pre-operative diagnosis [3].
Uterine torsion is defined as a rotation of the uterus on its long axis of more than 45° [3,4], and usually occurs at the level of the uterine isthmus at the junction of the uterine body and cervix. Important predisposing factors include large uterine fibroids (as in our case), a gravid uterus (sometimes with abnormal presentation of the fetus), congenital uterine anomalies, pelvic adhesions, and adnexal masses. In a non-gravid uterus, uterine fibroids are the commonest predisposing factor. A large fibroid can rotate and exert traction on the uterus, leading to torsion of the uterus simultaneously. As uterine torsion can result in vascular compromise and potentially lead to irreversible uterine ischemia and rapid clinical deterioration, accurate pre-operative diagnosis is important so that expedient surgery can be performed, especially in young patients who wish to preserve fertility.
Clinical & Imaging Findings
Symptoms of uterine torsion can range from abdominal pain, gastrointestinal or urinary discomfort and vaginal bleeding, to more severe and life-threatening symptoms related to shock [1,3].
Due to the often non-specific clinical presentation of uterine torsion, CT is commonly the first imaging study utilized in an emergency setting, even though ultrasonography (US) and magnetic resonance imaging (MRI) are well established preferred imaging modalities for evaluation of the female pelvis owing to their many advantages [5]. It is thus imperative that the radiologist is familiar with recognizing CT features of uterine torsion, which are often unsuspected.
On CT, there is considerable variation in morphologic features, size and position of the normal female pelvic organs, depending on patient age, phase of menstrual cycle, hormonal status and parity. Multiplanar reformatted (MPR) images in the standard sagittal and coronal planes are therefore useful in the evaluation of both normal and variant female pelvic anatomy [5,6].
In uterine torsion, a whorled structure representing the twisted uterine cervix is seen – this is reminiscent of the twisted pedicle of ovarian torsion, which is pathognomonic and the most specific imaging finding for adnexal torsion. Gas in the uterine cavity has also been described, presumably related to necrosis of the uterine wall [7].
It would be difficult to identify a twisted uterine cervix on pelvic US, especially if large uterine fibroids are present. Ancillary findings such as a fluid-distended endometrial cavity, hydrosalpinx and underlying uterine anomalies may point the radiologist towards a diagnosis of uterine torsion in the appropriate clinical context [8].
Treatment & Prognosis
If left untreated, uterine torsion can result in life-threatening complications and even mortality. It is thus imperative that expedient treatment is provided to ensure good clinical outcomes. Surgery is the mainstay of curative treatment. The choice between hysterectomy or fertility-sparing surgery should take into account the patient’s reproductive status as well as the viability of the uterus. In uncomplicated cases in women who wish to preserve fertility, surgical procedures are performed to correct anatomical causes of torsion. Surgical considerations will include myomectomy and detorsion of the uterus to its anatomical position [1,9]. Furthermore, bilateral plication of the uterosacral ligaments may be performed to prevent recurrence of torsion. In women past reproductive age or in cases where the viability of the uterus is compromised, hysterectomy should be considered [1].
Differential Diagnoses
As the presenting complaints and physical examination findings can be non-specific, more commonly encountered gastrointestinal and urologic conditions can be considered as initial differential diagnoses. These include acute appendicitis, diverticulitis and urinary calculi. It would be prudent to include other gynecological emergencies such as adnexal torsion and torsion of pedunculated uterine leiomyomas in the pre-imaging differential list as well.
Depending on associated symptoms and physical examination findings, a CT of the abdomen and pelvis or pelvic US may be performed. Occasionally an MRI may be obtained, although this is less common in the emergency setting. The main differential diagnoses can be limited to radiological differentials for a whorled structure seen in the pelvis on CT.
a. Torsion of the Adnexa
Adnexal torsion can involve the ovary, fallopian tube, or both. Concomitant ovarian and tubal torsion is encountered in up to 67% of cases [8]. Ovarian torsion is the twisting of the ovary and its vascular pedicle in its ligamentous supports, usually with an underlying ovarian mass serving as a lead point [10].
Ovarian torsion is commonly associated with benign ovarian masses greater than 5 cm, usually large cysts and cystic neoplasms such as mature cystic teratomas, cystadenomas and hemorrhagic cysts. Malignant ovarian masses and endometriotic cysts are less likely to cause torsion because adhesions render the ovaries less mobile [4,8,10]. The most common tumour associated with ovarian torsion is a mature cystic teratoma [11].
CT features can be classified into direct and indirect findings [4,8,10]. Direct findings include a thickened and twisted pedicle (Fig. 4), which is considered pathognomonic and the most specific imaging finding for adnexal torsion. The twisted pedicle contains a thickened fallopian tube which is continuous with the uterus. The helical structure of the twisted pedicle is not always apparent and may require multiplanar reformations to identify. It occasionally appears as an amorphous or tubular mass-like structure. Another direct finding is ipsilateral deviation of the uterus to the affected side due to a shortened adnexal ligament, although this finding is less specific.
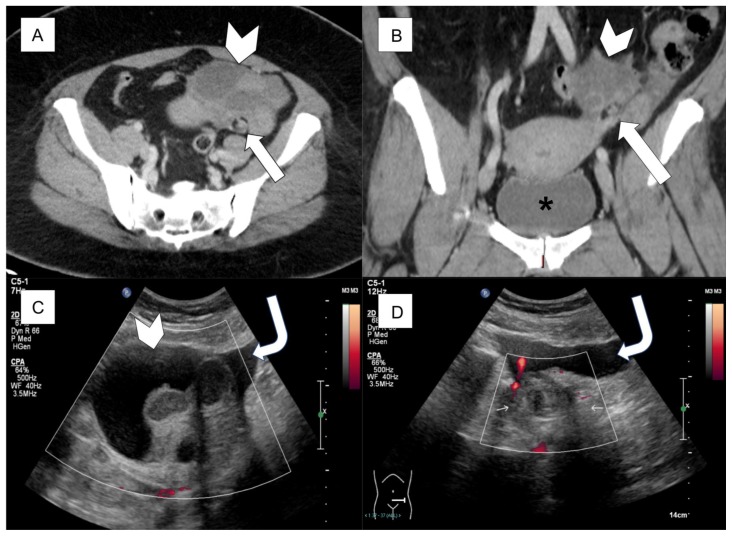
Figure 4.
45-year-old lady with torsion of the adnexa
FINDINGS:
A, B: Axial and coronal contrast-enhanced CT of abdomen and pelvis in the portal venous phase show a predominantly cystic mass (white arrowheads) containing internal septation and peripheral solid-appearing components in the left adnexa. Postero-inferior to the mass, there is a whorled structure representing a thickened and twisted pedicle (white block arrows). The urinary bladder (*) is seen caudal to the uterus.
C: Ultrasound image confirms a complex cystic mass (white arrowhead) in the left adnexa with no internal vascularity. Free fluid is seen around this mass (curved white arrow).
D: Ultrasound image shows a thick, avascular whorled structure (thin white arrows) in the left adnexa, corresponding to the thickened, twisted pedicle seen on CT. Free fluid is seen around this whorled structure (curved white arrow).
TECHNIQUE:
A, B: CT (Toshiba Aquilion ONE) portal venous phase, 750 mA, 120 kV, 3.00 mm slice thickness, 80 ml Omnipaque 350
C, D: Transabdominal ultrasonography on Philips iU22 using 5-1 MHz curved transducer
Indirect findings of ovarian torsion are a result of interruption of venous and lymphatic outflow. An asymmetrically enlarged ovary (more than 4.0 cm) is the most common finding, albeit non-specific. An enlarged ovary with central afollicular stroma and peripherally displaced hypo-attenuating follicles is more specific [10]. Other indirect findings include thickening of the fallopian tube, smooth wall thickening of the adnexal mass, non-enhancement of the mass, hemorrhage within the mass, inflammatory fat stranding, ascites and hemoperitoneum [4,8,10].
Gray-scale US features of adnexal torsion include a unilaterally enlarged ovary, co-existent mass within the twisted ovary, free pelvic fluid and a twisted vascular pedicle (Fig. 4d) [8]. Colour Doppler imaging features are highly variable and based on the degree of vascular compromise. These include decrease or absence of venous and/or arterial flow within the ovary and/or mass (Fig. 4c) [8,12].
b. Torsion of Pedunculated Uterine Leiomyomas
Uterine leiomyomas are the most common gynecologic tumours, with the subserosal type being the second most common after the intramural type. Pedunculated subserosal leiomyomas can rarely undergo torsion. Symptoms can subside if the torsion is partial and intermittent with spontaneous untwisting [13].
On CT, a mass connects to a normal uterus via a stalk. In comparison with ovarian torsion where the twisted pedicle is thick, the twisted pedicle of a pedunculated subserosal leiomyoma is thin. It may sometimes be difficult to identify on CT [4]. The mass may demonstrate poor enhancement due to infarction or ischemia. The ovaries, if visualized, should appear normal – thus eliminating ovarian torsion or ovarian tumours as differentials [4,13].
US features are similar to the above-mentioned CT findings. A thin stalk may be seen connecting a mass to the uterus (Fig. 5c). Depending on the degree of ischemia, there can be decreased or absent vascularity within the mass (Fig. 5d).
Figure 5.
33-year-old lady with torsion of a pedunculated uterine leiomyoma
FINDINGS: A, B: Axial and MPR sagittal contrast-enhanced CT of abdomen and pelvis in the portal venous phase show a circumscribed soft tissue mass (white arrowheads) at the left antero-lateral aspect of a bulky uterus containing fibroids (*). There is surrounding fat stranding and a small amount of free fluid in the pelvis (black arrows). The urinary bladder (curved white arrow) is adjacent to the uterus.
C, D: Ultrasound images confirm the presence of a soft tissue mass (white arrowheads) connected to the uterus (*) via a thin stalk (straight white arrows). No internal vascularity is seen within this mass. The urinary bladder (curved white arrow) is adjacent to the uterus.
TECHNIQUE: A, B: CT (Toshiba Aquilion ONE) portal venous phase, 663 mA, 120 kV, 3.00 mm slice thickness, 70 ml Omnipaque 350. C, D: Transabdominal ultrasonography on Philips iU22 using 5-1 MHz curved transducer
TEACHING POINT
Uterine torsion is a rare gynecological emergency and can be difficult to diagnose when unsuspected, especially when presenting symptoms are vague. Imaging findings include a whorled structure representing the twisted uterine cervix, and there may be gas in the uterine cavity. Expedient surgery will not only save lives, but also preserve fertility in the appropriate patients.
Table 1.
Summary table of key aspects of uterine torsion.
| Etiology | Uterine torsion is the rotation of the uterus on its long axis of more than 45°, usually occurring at the level of the uterine isthmus. |
| Incidence | Unknown. There are less than 50 reported cases of uterine torsion in a non-gravid uterus to date. |
| Gender Ratio | Exclusive to females |
| Age Predilection | Unknown |
| Risk Factors |
|
| Treatment | Surgery is the mainstay of curative treatment. The choice between hysterectomy or fertility-sparing surgery should take into account the patient’s reproductive status as well as the viability of the uterus. |
| Prognosis | This will depend on the initial clinical presentation, which can range from non-specific symptoms to a severely unwell patient requiring resuscitation. |
| Findings on Imaging | On CT, a whorled structure representing the twisted uterine cervix is seen. It would be useful to also search for findings which predispose to uterine torsion, such as uterine fibroids and adnexal masses. |
Table 2.
Differential diagnosis table for uterine torsion.
| Entity | Computed Tomography | Ultrasonography |
|---|---|---|
| Torsion of the uterus |
|
|
| Torsion of the adnexa | Direct findings
|
Gray-scale US
|
| Torsion of pedunculated uterine leiomyomas |
|
|
ABBREVIATIONS
- CT
computed tomography
- hCG
human chorionic gonadotropin
- MPR
multiplanar reformatted
- MRI
magnetic resonance imaging
- US
ultrasonography
REFERENCES
- 1.Luk SY, Leung JLY, Cheung ML, So S, Fung SH, Cheng SC. Torsion of a Nongravid Myomatous Uterus: Radiological Features and Literature Review. Hong Kong Med J. 2010 Aug;16(4):304–6. [PubMed] [Google Scholar]
- 2.Grover S, Sharma Y, Mittal S. Uterine Torsion: A Missed Diagnosis in Young Girls? Journal of Pediatric and Adolescent Gynecology. 2009 Feb;22(1):5–8. doi: 10.1016/j.jpag.2007.10.006. [DOI] [PubMed] [Google Scholar]
- 3.Jeong YY, Kang HK, Park JG, Choi HS. CT Features of Uterine Torsion. European Radiology. 2003 Dec;13:249–50. [PubMed] [Google Scholar]
- 4.Iraha Y, Okada M, Iraha R, Azama K, Yamashiro T, Tsubakimoto M, et al. CT and MR Imaging of Gynecologic Emergencies. RadioGraphics. 2017 Jul;37(5):1569–86. doi: 10.1148/rg.2017160170. [DOI] [PubMed] [Google Scholar]
- 5.Yitta S, Hecht EM, Slywotzky CM, Bennett GL. Added value of multiplanar reformation in the multidetector CT evaluation of the female pelvis: a pictorial review. RadioGraphics. 2009 Nov;29(7):1987–2003. doi: 10.1148/rg.297095710. [DOI] [PubMed] [Google Scholar]
- 6.Saksouk FA, Johnson SC. Recognition of the ovaries and ovarian origin of pelvic masses with CT. RadioGraphics. 2004 Oct;24:S133–46. doi: 10.1148/rg.24si045507. [DOI] [PubMed] [Google Scholar]
- 7.Davies JH. Case Report: Torsion of a Nongravid Nonmyomatous Uterus. Clinical Radiology. 1998 Oct;53(10):780–2. doi: 10.1016/s0009-9260(98)80326-7. [DOI] [PubMed] [Google Scholar]
- 8.Chang HC, Bhatt S, Dogra VS. Pearls and Pitfalls in Diagnosis of Ovarian Torsion. RadioGraphics. 2008 Sep;28(5):1355–68. doi: 10.1148/rg.285075130. [DOI] [PubMed] [Google Scholar]
- 9.Hawes CH. Acute axial torsion of the uterus. Annals of surgery. 1935 Jul;102(1):37. doi: 10.1097/00000658-193507000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Duigenan S, Oliva E, Lee SI. Ovarian Torsion: Diagnostic Features on CT and MRI with Pathologic Correlation. American Journal of Roentgenology. 2012 Feb;198(2):122–31. doi: 10.2214/AJR.10.7293. [DOI] [PubMed] [Google Scholar]
- 11.Stark JE, Siegel MJ. Ovarian torsion in prepubertal and pubertal girls: sonographic findings. American Journal of Roentgenology. 1994 Dec;163(6):1479–82. doi: 10.2214/ajr.163.6.7992751. [DOI] [PubMed] [Google Scholar]
- 12.Albayram F, Hamper UM. Ovarian and adnexal torsion: spectrum of sonographic findings with pathologic correlation. Journal of ultrasound in medicine. 2001 Oct;20(10):1083–9. doi: 10.7863/jum.2001.20.10.1083. [DOI] [PubMed] [Google Scholar]
- 13.Roy C, Bierry G, El Ghali S, Buy X, Rossini A. Acute Torsion of Uterine Leiomyoma: CT features. Abdominal Imaging. 2004 Jan;30(1):120–3. doi: 10.1007/s00261-004-0240-1. [DOI] [PubMed] [Google Scholar]