Abstract
This study explored the longitudinal relationships among maternal depressive symptoms, children’s depressive symptoms, aggression, and rule breaking and tested the moderating effects of maltreatment and child sex. A sample of 175 biological mother–child dyads (86 maltreated and 89 comparison) were seen at three time points, beginning at an average child age of 10.87 years. Results from cross-lagged models showed maternal depressive symptoms were related to higher levels of children’s depressive symptoms but not children’s aggression or rule breaking. Rule breaking predicted maternal depressive symptoms only in the comparison group. Child sex moderated some relationships. Boys’ depression predicted maternal depressive symptoms, whereas maternal depressive symptoms predicted aggression among girls. There was no evidence in this sample that child maltreatment increased the effects of maternal depressive symptoms on child outcomes. These results suggest that attention in clinical practice to the importance of addressing maternal depression as well as addressing children’s functioning should continue into adolescence.
Keywords: maternal depressive symptoms, maltreatment, adolescent, externalizing problems, internalizing problems
Two of the most serious risk factors for child and adolescent negative outcomes are being a victim of child maltreatment and having a mother who is depressed (Jonson-Reid, Kohl, & Drake, 2012; Weissman & Wickramaratne, et al., 2006). Although an extensive research base has outlined the negative outcomes that result from maternal depression and maltreatment individually, few studies have explored how these two experiences in combination predict outcomes. The purpose of this study was to examine the relationships among maternal depressive symptoms and children’s depressive symptoms, aggression, and rule breaking behaviors over time and whether those relationships were moderated by maltreatment or sex. We focused only on adolescents living with biological mothers because of the shared biological and environmental risks of depression (Elgar, McGrath, Waschbusch, Stewart, & Curtis, 2004; Silberg, Rutter, Neale, & Eaves, 2001).
The negative impact of maternal depression on both internalizing and externalizing problems for children has been noted across development (Nicholson, Deboeck, Farris, Boker, & Borkowski, 2011; Weismann & Wickramaratne, 2006). For example, exposure to maternal depression in infancy predicted a child’s depression at age 8 and 19 (Bureau, Easterbrooks, & Lyons-Ruth, 2009). The relationship between maternal depression and adolescent problems is not limited to exposure to maternal depression in early childhood, but continues with exposure in adolescence (Kouros & Garber, 2010). Studies also show that when a mother’s depression improves, her children’s internalizing and externalizing symptoms improve (Foster et al., 2008; Nicholson et al., 2011; Weissman, Pilowsky et al., 2006). Conversely, some studies find that an increased level of children’s problems results in worsening of maternal depression (Bagner, Pettit, Lewinsohn, Seeley, & Jaccard, 2013; Nicholson et al., 2011). Taken together the extant evidence suggests that the relationship between maternal depression and children’s problems may be bidirectional, maternal depression affects child symptoms while child symptoms also affect maternal depression (Bagner, et al., 2013; Nicholson et al., 2011). The National Research Council and Institute of Medicine (2009) provided a summary of research on the effects of parental depression on children throughout the life cycle. Of particular relevance to this study is the focus on the numerous psychological and behavioral problems associated with maternal depression in particular, and more functional impairment in children whose parents are depressed, and the continued influence of parental depression through childhood and into adolescence.
Research on the effects of maltreatment is equally pervasive. A wealth of research has supported the serious consequences of child abuse and neglect for children and adolescents (Jonson-Reid et al., 2012; Keyes et al., 2012). Maltreated children and adolescents are overrepresented among those with psychiatric and behavioral problems (Godinet, Li, & Berg, 2014; van Dam et al., 2015), substance abuse issues (Lo & Cheng, 2007), experiences with homelessness (Sundin & Baguley, 2015), and physical health problems (Palaszynski & Nemeroff, 2009). An excellent summary of research on the consequences of child maltreatment can be found in the Institute of Medicine and National Research Council’s 2014 report. This report expanded on their 1993 report, noted the many advances in knowledge regarding the mechanisms through which damage from child maltreatment occurs. Of particular relevance to this study is the emphasis on internalizing and externalizing symptoms that result from exposure.
In contrast, research on the combined effects of maternal depression and maltreatment has been quite limited. In an early study, Kinard (1995) used a matched sample of maltreated (substantiated by child protection services, n = 172) and comparison (n = 155) children and their mothers to investigate the relationship between maltreatment and maternal depression using both parent and teacher reports of behavior (Child Behavior Checklist [CBCL] and Teacher’s Report Form). Maltreated children were rated as having more problems by both parents and teachers. Mothers with depression rated their children as having more problems than mothers without depression, but this did not hold true for teacher reports. Another study examined whether physically abusive and neglectful parenting mediated the effects of parental depression on CBCL scores in a sample of children who had involvement with child welfare. Using data from the National Survey of Child and Adolescent Well-Being, parental depression predicted child outcomes (as measured by parent report on the CBCL) for preschoolers, school-age children, and adolescents. The tests for mediation were statistically significant only with preschool and school-age children, with neglectful parenting mediating the relationship between parental depression and child outcomes. Internalizing and externalizing scores were not reported. Although all of these parents had involvement with child welfare services, neglectful and abusive parenting was measured via scores on the parent–child version of the Conflict Tactics Scale rather than official reports (Mustillo, Dorsey, Conover, & Burns, 2011). Again, there was a relationship between parental depression and children’s problem levels, however, a limitation of the study was that children’s problems were measured by parental report only.
A study of the effects of neglect on young children’s cognitive and behavioral functioning (Dubowitz, Papas, Black, & Starr, 2002) recognized the possible confounding effects of maternal depression on outcomes. The authors measured maternal depression and found it was related to both internalizing and externalizing subscales of the parent-reported CBCL. However, they did not examine the interaction between neglect and maternal depression and therefore could not discern the potential combined effects.
Emotional maltreatment has also been found to affect the relationship between maternal depression and childhood behaviors. A study by McCullough and Shaffer (2014) found that in a sample of 62 mother–child dyads, maternal depression was related to children’s externalizing problems only in the presence of emotional maltreating behavior. Emotional maltreatment was defined by observation of interaction tasks in the lab rather than from child protection records and families were not known to be involved with child welfare.
Sex of the child has been found to be a determinant of the prevalence of both internalizing and externalizing behaviors in children and adolescents. Although rates of depression in childhood are similar by sex (Costello, Mustillo, Erkanli, Keeler, & Angold, 2003), adolescent girls are at increased risk of depression compared to boys (Avenevoli, Swendsen, He, Burstein, & Merikangas, 2015). On the other hand, boys are twice as likely as girls to be diagnosed with a behavior disorder throughout childhood (Costello et al., 2003). In addition, there is also evidence that maternal depression might have different effects on boys and girls, with boys more likely to develop externalizing problems in infancy related to their mother’s depression (Choe, Sameroff, & McDonough, 2013). Similarly, boys with low negative emotionality had higher levels of internalizing problems through decreased maternal warmth related to maternal depression (Hummel & Kiel, 2015).
In summary, the existing research indicates that the combination of maternal depression and maltreatment may result in more internalizing and externalizing problems for children than either alone, although findings have not been definitive. This conclusion is also compromised by the use of a parent report measure (CBCL) in these studies. Maternal reports of children’s problems are often questionable (Hartung, McCarthy, Milich, & Martin, 2005; S. R. Smith, 2007; van der Meer, Dixon, & Rose, 2008) and may be influenced by the mother’s depression and other psychopathology (Briggs-Gowan, Carter, & Schwab-Stone, 1996; Gartstein, Bridgett, Dishion, & Kaufman, 2009; Kiss at al., 2007; Kroes, Veerman, & De Bruyn, 2003). In addition, the classification of maltreatment varied considerably in the studies. Only the Kinard (1995) study used a sample of children officially classified as maltreated, and it is possible that the other groups might not reach the level of harm needed for an official designation of maltreatment. The directionality of the relationships between maternal depression and children’s outcomes is not clear as only Mustillo, et al., (2011) used longitudinal data. Whether these relationships are different by sex is also unclear.
To address these limitations, we recruited a sample of young adolescents with careful documentation of child welfare reports of maltreatment and a comparison group from the same neighborhoods and used self-report measures for depressive symptoms, aggression, and rule breaking behaviors and maternal depressive symptoms across three time points. Child reports of externalizing behaviors have been found to highly correlate with peer reports (Wrobel, Lachar, & Worbel, 2005) and be more accurate than parents report of the same behaviors (Hartung, McCarthy, Milich, & Martin, 2005). Given that the adolescent developmental period is one of both vulnerability and risk (National Research Council, 2001), as well as the time when rates of depression begin to increase (Hankin et al., 2015), it seems particularly valuable to know how these dual risk factors influence these youth to assist in developing better interventions. We evaluated sex as a moderator because of the different incidence of depression and externalizing behaviors by sex. Our aims were:
To examine the relationship between maternal depressive symptoms and youth’s depressive symptoms, aggression and rule breaking over time.
To test whether these relationships were moderated by the youth’s maltreatment status or sex.
Methods
Participants
Data were from the first, second, and third assessment of an ongoing longitudinal study examining the effects of maltreatment on adolescent development. The second assessment was approximately 1 year after the first, and the third assessment was approximately 2.5 years after the first. The enrolled sample at Time 1 was 454 adolescents aged 9–13 years (241 boys and 213 girls; 303 maltreated and 151 comparison). At Time 2, 86.1% of the original sample was retained (n=391) and at Time 3 70.9% of the Time 1 sample was retained (n=322).
For the current analyses, the sample was restricted to adolescents whose birth mother completed the assessment with them at Time 1 (T1) and completed either one or both assessments at T2 or T3. We chose to use only birth mothers because: 1) we wanted the possible genetic influence to be constant across groups; 2) the effects of maternal depression can begin in infancy and we wanted to ensure consistency in the caregivers. If the child was in alternative care (foster or kin care) there could be unknown maternal depression in the child’s life before entry into the study. In previous work, we found that the level of problems between maltreated children placed in care and those who remained at home was not different (reference removed for blind review), therefore the exclusion of those in out- of-home care was not likely to decrease the problem levels of the children. We also restricted the sample to one adolescent per caregiver. If the mother had more than one adolescent in the study, we randomly chose one adolescent for inclusion. Based on these selection procedures, the final sample was 175 adolescent–birth mother dyads (85 adolescent boys, 90 adolescent girls; 89 comparison and 86 maltreated). Logistic regression was used to examine potential differences in demographic (age, sex, maltreatment status) and study variables (maternal depression, child depression, rule breaking, aggression) for participants retained versus not. Results showed that only maltreatment status predicted attrition (OR=2.55, 95% CI=1.13–5.73, p<.05).
Recruitment
The maltreatment group was recruited from active cases in the Los Angeles County Department of Children and Family Services (LACDCFS). The inclusion criteria for recruitment into the study were: (a) a newly opened case at LACDCFS during the preceding month for any type of maltreatment; (b) child age of 9–12 years (some children turned 13 between enrollment and interview); (c) child identified as Latino, African American, or Caucasian (non-Latino); and (d) child residing in one of 10 zip codes in Los Angeles at the time of referral to LACDCFS. With the approval of LACDCFS, the Juvenile Division of the Los Angeles Superior Court, and the Institutional Review Board of the affiliated university, we contacted potential participants with a letter explaining the study with a post card allowing them to opt out of follow up. The letters were followed up with a phone call asking for participation. Seventy-seven percent of the referred families agreed to participate.
The comparison group was recruited using school lists of children aged 9–12 years residing in the same 10 zip codes as the maltreated sample. We employed the same procedures to contact comparison caregivers as maltreated caregivers. Comparison families were asked about any previous or ongoing experience with child welfare agencies. Approximately 50% of the comparison families contacted agreed to participate.
Sample Demographics and Maltreatment Experiences
The average age of the adolescents was 10.87 years at T1, 12.04 years at T2, and 13.61 at T3 (see Table 1). There was a fairly equal number of boys and girls at all three time points. Most of the adolescent participants were African American or Latino. The mothers were on average 36.38 years old (SD = 6.50, range = 24–55) at entry into the study; 38% were African American, 42% Latino, 14% White, and 6% other (biracial, Asian). At T1, Maternal depression scores in the maltreatment group translated to a Tscore of 61 and the comparison group to a Tscore of 56. A score of 63 is the clinical cut off point for the non-patient group (Derogotis, 1993). In the maltreatment group, 73.6% of the mothers had some involvement in their child’s maltreatment. Characteristics of the children’s maltreatment can be found in Table 2. The large majority of the children (67.8%) experienced more than one type of maltreatment. Additional information on the children’s maltreatment experiences can be found in earlier work (reference removed for blind review)
Table 1.
Sample Characteristics for Children at Time 1, 2, and 3
| Time 1 | Time 2 | Time 3 | |
|---|---|---|---|
| (n = 175) | (n = 170) | (n = 150) | |
| n (%) or M (SD) | |||
| Age | 10.87 (1.09) | 12.03 (1.17) | 13.60 (1.33) |
| Gender | |||
| Male | 85 (48.57) | 82 (48.20) | 72 (48.00) |
| Female | 90 (51.43) | 88 (51.80) | 78 (52.00) |
| Maltreated | 86 (49.14) | 83 (48.82) | 66 (44.00) |
| Comparison | 89 (50.86) | 87 (51.18) | 84 (56.00) |
| Race and ethnicity | |||
| African American | 67 (38.29) | 65 (38.24) | 60 (40.00) |
| White | 15 (8.57) | 15 (8.82) | 14 (9.33) |
| Latino | 71 (40.57) | 68 (40.00) | 56 (37.33) |
| Mixed or biracial | 22 (12.57) | 22 (12.94) | 20 (13.33) |
Table 2.
Children’s Maltreatment Experiences
| Maltreatment Types | Number of Types Experienced | ||||
|---|---|---|---|---|---|
| Type | n | % | Types Experienced | n | % |
| Physical Abuse | 43 | 50.6 | 1 | 21 | 24.1 |
| Sexual Abuse | 18 | 21.2 | 2 | 24 | 27.6 |
| Neglect | 53 | 60.9 | 3 | 22 | 25.3 |
| Emotional Abuse | 44 | 51.8 | 4 | 10 | 11.4 |
| Caretaker Incapacity | 32 | 37.6 | 5 | 3 | 3.4 |
| Substantial Risk | 17 | 19.5 | At Risk Sibling or | 7 | 8 |
| At Risk Sibling | 32 | 37.6 | Substantial Risk Only | ||
Note: Totals > 100% because children experienced more than a single type of maltreatment
Procedures
Assessments were conducted at an urban research university office. After assent and consent were obtained from the adolescent and mother, respectively, the adolescent and mother completed questionnaires during a standardized four-hour protocol. The measures used in this analysis represent a subset of the interview measures collected at each time point. Both the adolescent and mother were paid for their participation according to the National Institutes of Health standard compensation rate for healthy volunteers.
Measures
Child depressive symptoms
The Children’s Depression Inventory (CDI) is a 27-item, self-rated, symptom-oriented scale suitable for youth aged 7 to 17 (Kovacs, 1992, 2004). The symptoms are rated on a scale of 0–3 over the past 2 weeks. It had good internal consistency in standardization samples, with coefficient alphas from .70 to .86 (Kovacs, 1985). Test–retest reliability in 7- to 12-year-olds has been variable, with scores ranging from .82 to .76 (Finch, Saylor, Edwards, & McIntosh, 1987). Our sample α = .85. The CDI has been found to have good ability to screen children for depressive symptoms (Hodges, 1990; Smith, Mitchell, McCauley, & Calderon, 1990). In this study, the CDI was used as a continuous measure with higher scores indicating more depressive symptoms.
Child aggression and rule breaking
The aggression and rule-breaking subscales of the Youth Self Report (Achenbach, 1991) were used to evaluate those constructs. This widely used child report measure is a companion to the parent report CBCL (Achenbach, 1991) and has substantial evidence of reliability and validity in various populations (Achenbach, 1991; Achenbach & Rescorla, 2001). Items are rated from 0 to 2 (“not at all” to “a lot”, with 14 items in the aggression subscale and 10 items in the rule-breaking subscale for ranges of 0–28 and 0– 20, respectively. The aggression subscale includes items such as “I have a hot temper” and the rule-breaking subscale includes items such as “I disobey at school.” Higher scores reflect more problematic functioning. In our sample, alphas were .81 for aggression and .80 for rule breaking. No clinical cutoff score was used for these subscales. While these two constructs are related, there are important differences with rule breaking behavior demonstrating less heritability than aggressive behavior (Achenbach & Rescorla, 2001). We chose to use each separately following Burt’s (2012) suggestion to do so because they represent different dimensions of externalizing behavior.
Maternal depressive symptoms
The Brief Symptom Inventory is a psychological self-report symptom scale that was adapted from the Symptom Checklist-90-R (Derogatis, 1993; Derogatis & Melisaratos, 1983). The inventory has both good test–retest and internal consistency reliabilities for the primary symptom dimensions (Derogatis & Melisaratos, 1983) and has been used cross-culturally (Ruiperez, Ibanez, Lorente, Moro, & Ortet, 2001). Respondents are asked how often they have been bothered by certain symptoms during the preceding 7 days. Answers are rated on a 5-point Likert scale from 0 (never) to 5 (almost always). We used the depression subscale, which features a range of 0–30, with higher scores reflecting more problematic functioning. Our sample α = .87.
Data Analysis
Independent samples t-tests were used to examine mean differences between maltreated and comparison groups and between boys and girls for study variables.
For the substantive analyses, path models were tested using Mplus 7.2 (Muthen & Muthen, 2014). Item-level and longitudinal missingness was handled using Full Information Maximum Likelihood and non-normality was addressed using the MLR estimator. Cross-lagged models included maternal depressive symptoms, child depressive symptoms, and either rule breaking or aggression at all three time points. Rule breaking and aggression were not included in the same model because although they have been shown to have discriminant validity they are still highly correlated (rs>.60). Crossed paths from all T1 variables to all T2 variables and from all T2 variables to all T3 variables were included, as were autoregressive paths and within-time covariances. Time 1 age, sex, and maltreatment status were included as covariates. Fit indexes such as the χ2 (chi-square) goodness-of-fit statistic, the root mean square error of approximation (RMSEA), standardized root mean square residual (SRMR), and comparative fit index (CFI) were used to evaluate the fit of the model to the data. Overall, a good model fit is indicated by a small χ2, RMSEA and SRMR of .08 or less, and CFI greater than .90 (Browne & Cudeck, 1993; Shapiro & Levendosky, 1999). The models were first tested with the total sample controlling for T1 age, sex and maltreatment status. Then multiple-group models were used to test maltreatment status and sex as moderators. The one degree of freedom nested χ2 difference test was used to determine whether each parameter in the model (in turn) was significantly different between groups, which is evidence of significant moderation effects. Due to the use of MLR estimator the Scaled chi-square different test was used (Satorra & Bentler, 2001).
Results
Mean Differences
Differences between maltreated and comparison youth in terms of maternal depressive symptoms existed at all three time points, with higher levels reported in the maltreated group. Maltreated youth had higher levels of depressive symptoms at T1 and T2 (see Table 3). We found no differences in study variables for boys versus girls.
Table 3.
Means and Standard Deviations of Study Variables by Maltreatment Status and Sex
| Maltreatment Status | Sex | |||||
|---|---|---|---|---|---|---|
| Maltreated | Comparison | p | Male | Female | p | |
| Maternal depressive symptoms | ||||||
| Time 1 | 4.3 (4.3) | 2.3(2.9) | < .001 | 3.3 (3.4) | 3.2 (4.1) | .84 |
| Time 2 | 4.3 (5.0) | 1.6(3.3) | < .001 | 3.3 (4.6) | 2.6 (4.3) | .34 |
| Time 3 | 3.5 (4.4) | 2.0(4.0) | .03 | 3.0 (4.8) | 2.3 (3.6) | .37 |
| Child aggression | ||||||
| Time 1 | 5.3 (4.2) | 4.7(4.4) | .33 | 5.3 (4.6) | 4.6 (4.0) | .27 |
| Time 2 | 5.4 (4.9) | 4.9(4.5) | .52 | 5.0 (4) | 5.3 (5.4) | .67 |
| Time 3 | 5.9 (5.1) | 4.8(4.3) | .15 | 5.3 (4) | 5.2 (5.2) | .89 |
| Child rule breaking | ||||||
| Time 1 | 1.5 (1.9) | 1.1(2.3) | .25 | 1.5 (2.5) | 1.1 (1.5) | .19 |
| Time 2 | 1.5 (1.9) | 2.0(2.8) | .14 | 1.9 (2.0) | 1.7 (2.7) | .64 |
| Time 3 | 2.5 (2.8) | 2.4(2.6) | .82 | 2.4 (2.3) | 2.4 (2.9) | .91 |
| Child depressive symptoms | ||||||
| Time 1 | 9.6 (6.8) | 7.7(5.4) | .04 | 8.2 (5.9) | 9.0 (6.4) | .37 |
| Time 2 | 9.2 (7.0) | 7.0(5.6) | .03 | 8.0 (6.4) | 8.1 (6.4) | .99 |
| Time 3 | 8.8 (7.2) | 7.2(5.4) | .15 | 7.2 (5.4) | 8.5 (7.0) | .21 |
Note. Mean differences between groups tested using independent samples t-test.
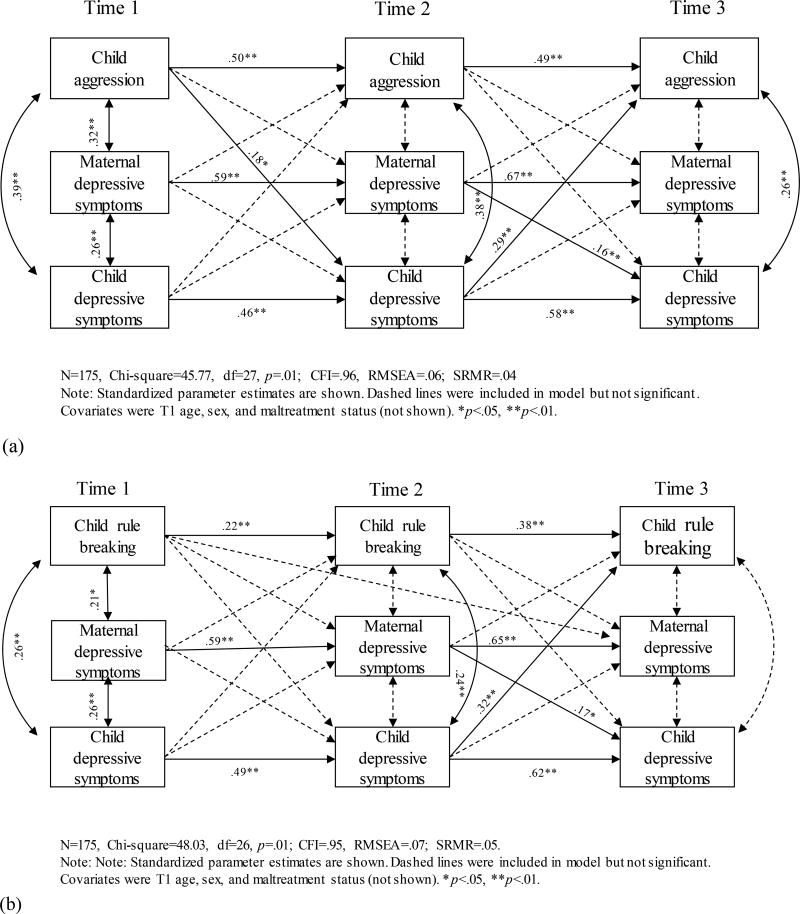
Total Sample
The model with maternal depressive symptoms, child depressive symptoms, and child aggression fit the data adequately (χ2(27) = 45.77, p=.01; RMSEA = .06; SRMR=.04; CFI = .96). There were significant associations between T1 child aggression and T2 child depressive symptoms (β = .18, p < .05), T2 child depressive symptoms and T3 aggression (β = .29, p < .01), and T2 maternal depressive symptoms and T3 child depressive symptoms (β = .16, p < .01). There were also significant autoregressive effects from T1 to T2 to T3 variables and within-time covariances between child aggression and depression (see Figure 1a).
Figure 1.
Maternal depressive symptoms, child’s depressive symptoms, and (a) child’s aggression or (b) rule breaking
The model including rule breaking also fit the data adequately (χ2(26) = 48.03, p=.01; RMSEA = .07; SRMR=.05; CFI = .95). Significant parameter estimates existed between T2 maternal depressive symptoms and T3 child depressive symptoms (β = .17, p < .01) and T2 child depressive symptoms and T3 rule breaking (β = .32, p < .01). As with the previous model, we found significant autoregressive effects for all variables and significant within-time covariances only for T1 and T2 child rule breaking and depression (see Figure 1b).
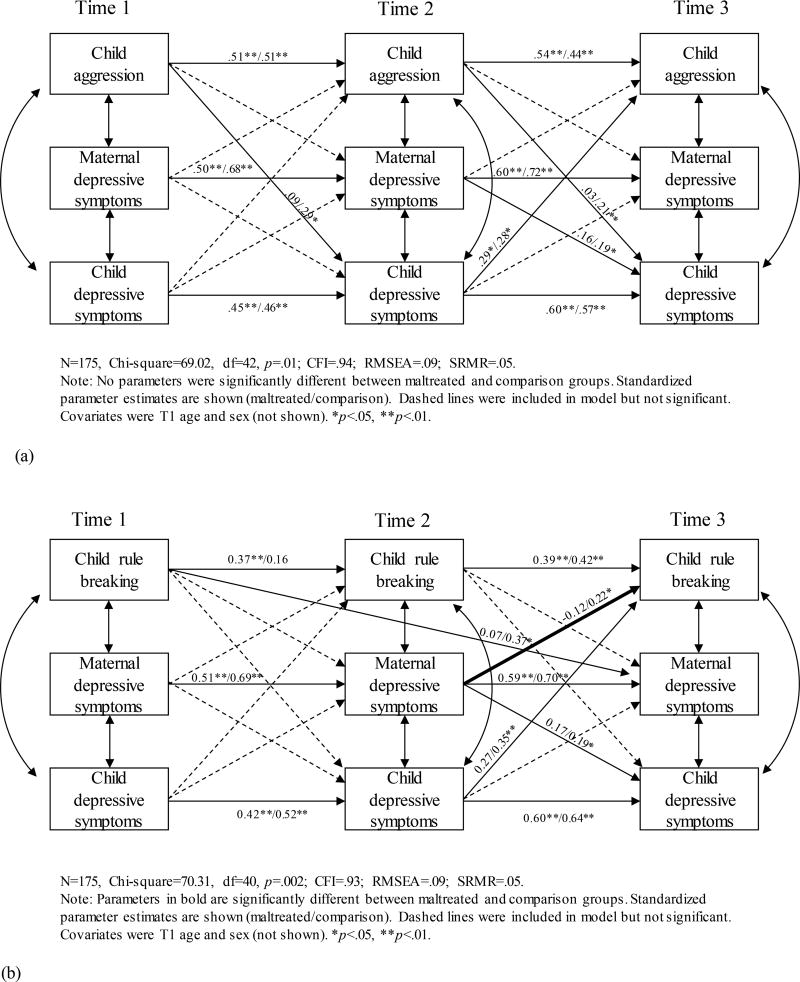
Multiple-Group Models: Maltreated vs. Comparison
The model with child aggression, depressive symptoms, and maternal depressive symptoms fit the data adequately (χ2(42) = 69.02, p=.01; RMSEA = .09; SRMR=.05; CFI = .94). None of the parameters significantly degraded the model fit when restricted to equality. See Figure 2a.
Figure 2.
Maternal depressive symptoms, child’s depressive symptoms, and (a) child’s aggression or (b) rule breaking by maltreatment status (maltreated/comparison)
The model including rule breaking rather than aggression showed adequate fit (χ2(40) = 70.31, p=.002; RMSEA = .09; SRMR=.05; CFI = .93). One of the parameters significantly degraded the model fit when restricted to equality. Specifically, the parameter from T2 maternal depressive symptoms to T3 rule breaking (Δχ2(1) = 7.44, p < .01) was significant for the comparison group (β = .22, p < .05) but not the maltreated group (β = −.12, p > .05). See Figure 2b.
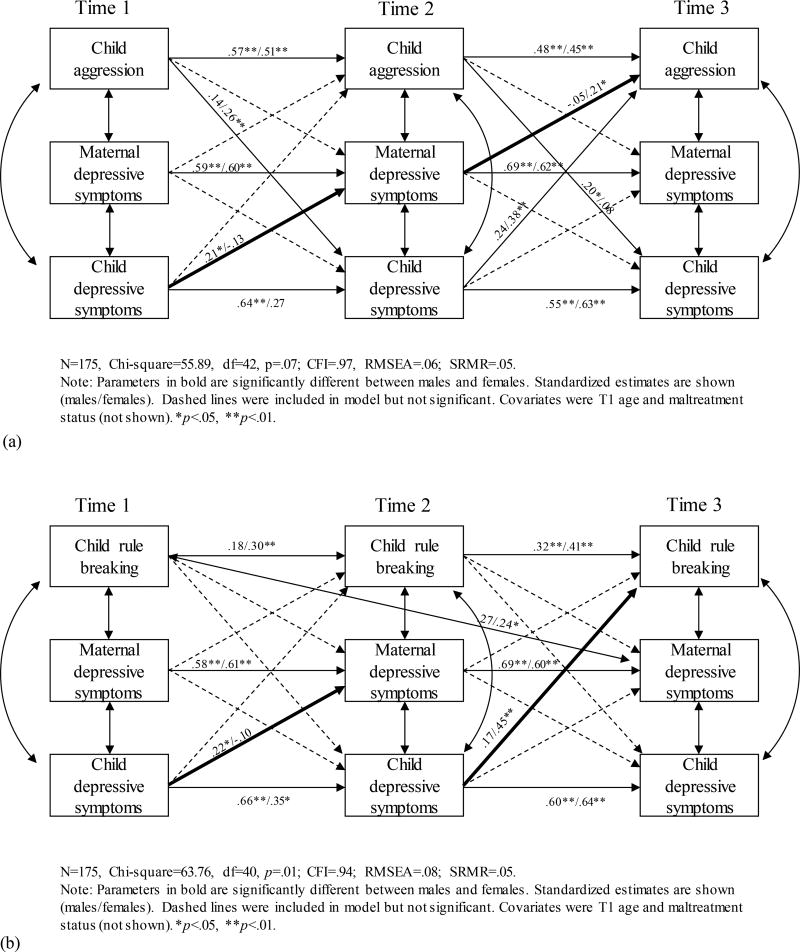
Multiple-Group Models: Males vs. Females
The model with aggression fit the data well (χ2(42) = 55.89, p=.07; RMSEA = .06; SRMR=.05; CFI = .97). Two parameters were moderated by sex: T1 child depressive symptoms to T2 maternal depressive symptoms (Δχ2(1) = 46.40, p < .01) and T2 maternal depressive symptoms to T3 aggression (Δχ2(1) = 12.03, p < .01). The path from T1 child depressive symptoms to T2 maternal depressive symptoms was significant only for boys (β = .21, p < .05), not girls (β = −.13, p > .05). The path from T2 maternal depressive symptoms to T3 child aggression was significant only for girls (β = .21, p < .05), not boys (β = −.05, p > .05). See Figure 3a.
Figure 3.
Maternal depressive symptoms, child’s depressive symptoms, and (a) child’s aggression or (b) rule breaking by gender (male/female)
The model including rule breaking also fit the data adequately (χ2(40) = 63.76, p=.01; RMSEA = .08; SR<R=.05; CFI = .95). Two parameters were moderated by sex: T1 child depressive symptoms to T2 maternal depressive symptoms (Δχ2(1) = 26.06, p < .01) and T2 child depressive symptoms to T3 rule breaking (Δχ2(1) = 23.63, p < .01). The path from T1 child depressive symptoms to T2 maternal depressive symptoms was significant only for boys (β =.22, p < .05), not girls (β = −.10, p > .05). The path from T2 child depressive symptoms to T3 child rule breaking was significant only for girls (β =.45, p < .05), not boys (β = .17, p > .05). See Figure 3b.
Discussion
The aims for our study were to examine the relationships among maternal depressive symptoms and children’s depressive symptoms, aggression, and rule breaking over time and to determine if these relationships were moderated by maltreatment or sex. We found complex relationships. Maternal depressive symptoms were related to child depressive symptoms in that maternal depressive symptoms at T2 predicted child depression at T3. This is consistent with studies that have found maternal depression predicts child’s depression in the future (Bureau et al., 2009; Hughes & Gullone, 2010). Maternal depressive symptoms were not related to either child’s rule breaking or aggression in the sample as a whole. Maternal depressive symptoms were constant across the three assessments; elevated depressive symptoms at one point continued at future time points. Of note is that the mean score of the mothers in the maltreated group is only slightly below that of the clinical cut off point indicating that a subgroup of mothers suffered from depression.
The presence of maltreatment did not seem to amplify the effect of maternal depressive symptoms on either child depressive symptoms or aggression and rule breaking in youth. In fact, maternal depressive symptoms predicted rule breaking only for the comparison group. This result is somewhat surprising because maltreated children experienced two serious risk factors (i.e., maltreatment and exposure to maternal depressive symptoms) and earlier studies suggested that the presence of both maternal depressive symptoms and maltreatment increased children’s internalizing and externalizing behaviors (e.g. McCullough and Shaffer, 2014). There are several possible explanations for the discordance between our findings and previous research. The experience of maltreatment may interfere with the mother–child relationship (Katz, Hammen, & Brennan, 2013), possibly making children less sensitive to the effects of maternal depressive symptoms. Reliance on parent report of children’s problems in previous studies may not have given an accurate measure of the children’s problems and may have been influenced by the mother’s depressive symptoms. It is also possible that some of the associations found in previous studies were due to neighborhood environmental problems experienced by children that were not measured. Our children came from very similar neighborhoods [location omitted for review] and thus would have experienced similar levels of poverty, community violence, and neighborhood disadvantage that have been found to be related to both internalizing and externalizing problems (Booth & Crouter, 2001; Brooks-Gunn, Duncan, & Aber, 1997). Another possibility relates to our sample. We only included children who lived with biological mothers, thus eliminating any children placed outside the home. There is evidence that children whose maltreatment is seen as more severe may be more likely to be placed out of the home (Britner & Mossler, 2002); if true, this could indicate that our maltreatment sample was diluted. However, we have not found differences by placement in our previous work (Authors, blinded for review), thus we find this explanation unlikely.
Differences by sex were also somewhat surprising. For boys, depressive symptoms at T1 predicted maternal depressive symptoms at T2, which was not the case for girls. There is some support for this finding. Hughes and Gullone (2010) found that adolescent internalizing problems predicted maternal internalizing problems at a future time point, but they did not look at differences by sex. The opposite has also been found, with Kouros and Garber (2010) finding that lower levels of depressive symptoms in children predicted higher levels of depression in mothers at subsequent times. One possible explanation for our finding that boys’ depression predicted maternal depressive symptoms may be that mothers perceive depression as more unusual among sons entering adolescence (the boys averaged nearly 11 years old at T1), which aggravates their own depression. Maternal depressive symptoms at T2 predicted aggression at T3 for girls, but not boys. Increased aggression in girls may be related to possible decreases in parental supervision caused by maternal depressive symptoms. Girls receive more parental supervision than boys in adolescence (Webb, Bray, Getz, & Adams, 2002) and the decrease in monitoring may be related to more problem behaviors (Aalsma, Liu, & Wiehe, 2011; Beyers, Goossens, Vansant, & Moors, 2003). At T2 these girls were entering adolescence (average age 12.03), when girls are more likely to begin exhibiting aggressive and antisocial behaviors (Silverthorn & Frick, 1999), thus making them more at risk if parental monitoring decreases.
Also of note is that the relationship between maternal depression and adolescent depression is significant only between T2 and T3. Developmentally, the effect of maternal depression at this time point may be due to increased prevalence of depressive symptoms in mid-adolescence. In addition, the confluence of physical, social and cognitive changes that are occurring around this age may make adolescents more susceptible to parenting deficits evidenced by their mother with depressive symptoms. The improvements in cognitive functioning may also make them more cognizant of the parenting deficits and more easily identify them due to social comparisons with their friends’ mothers.
Different associations were found for aggression versus rule breaking in relation to maternal depression. Aggression but not rule-breaking predicted Time 2 maternal depression, whereas maternal depression only predicted rule-breaking at T3 and not aggression, One explanation is that these differences are largely due to developmental changes in externalizing behaviors, that the stress of having an aggressive child contributed to maternal depressive symptoms but being exposed to maternal depressive symptoms led to acting-out behavior of rule-breaking because of the age of the children at T3 These differential associations are supported by researchers who suggest that the two constructs while highly correlated represent different dimensions of antisocial behavior and have different relationships to outcomes (Burt, 2012).
Limitations
There are a number of limitations to our study. We did not have a diagnosis of depression for mothers, but used a symptom measurement that yielded a continuous measure of depression. We decided to use a continuous measure of depression symptoms rather than a depression diagnosis to identify how changes in mothers’ symptomology were related to children’s behavioral changes. It is also possible that comparison youth may have had maltreatment experiences that were not reported to the child welfare system. However, there is research that indicates that children who have official reports of maltreatment are different from those in similar environments with no reports (Jonson-Reid, Kohl, & Drake, (2011). In addition, the youth in this study were primarily from urban and minority backgrounds, which limits the generalizability of the findings. Also our measurement did not begin until the youth were in late childhood and young adolescence, so we are unable to determine whether mothers were depressed in early childhood when many problematic behaviors begin (Goodman et al., 2011). There are limitations to a cross-lagged approach in that we were not testing specific hypotheses regarding the temporal order of maternal depression and child problems. In addition, we tested only structural invariance for the specific parameters we were interested in (e.g. crossed paths), and there may have been group differences in the residual variances that we did not test for.
Summary and Future Directions
Our study also has strengths. Recruitment of maltreated and comparison children from the same neighborhoods allowed a better comparison of the study variables because community factors were similar for all children. In addition, we were able to follow these families over three timepoints to assess the bidirectionality of these associations.
In summary, we found that maternal depressive symptoms influence children’s development into mid-adolescence but maltreatment does not seem to compound the effect. Our results suggest that more research is needed on the interaction between maternal depressive symptoms and child maltreatment to better understand the interactions of these high-risk factors. Of particular importance is recruiting samples of children at younger ages, when the effects of both maltreatment and maternal depressive symptoms may be even more salient to behavior (Guyon-Harris, Huth-Bocks, Lauterbach, & Janisse, 2015). In addition, we will continue to explore how the effects of maternal depressive symptoms influence our study participants as they move into young adulthood.
Implications
Maternal depression continues to have an impact on youth as they move into adolescence and this needs to be addressed when these youth encounter difficulties whether it is through the child welfare system, mental health system, juvenile justice system or primary health care system. Given the bi- directionality of symptoms between children and mothers, when depression is diagnosed in a child, assessment for the mother should also be encouraged with appropriate treatment made available. Access to appropriate evidence based intervention for both the youth and their mothers is necessary to more effectively deal with the struggles in these families.
Acknowledgments
This research was supported by grants from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (RO1-HD39129, PI: Trickett; K01-HD069457, PI: Negriff; K01-HD05798, PI: Schneiderman) and the National Institute on Drug Abuse (R01 DA02456902, PI: Trickett).
Footnotes
A previous version of this paper was presented at the 2016 Annual Meeting of the Society for Social Work and Research
Contributor Information
Ferol E. Mennen, Department of Children, Youth and Families, School of Social Work, University of Southern California
Sonya Negriff, Department of Children, Youth and Families, School of Social Work, University of Southern California.
Janet U. Schneiderman, Department of Children, Youth and Families, School of Social Work, University of Southern California
Penelope K. Trickett, Department of Children, Youth and Families, School of Social Work, University of Southern California
References
- Authors. 2010 [Google Scholar]
- Authors. 2010 [Google Scholar]
- Aalsma MC, Liu GC, Wiehe SE. The role of perceived parent monitoring and support on urban child and adolescent problem behavior. Community Mental Health Journal. 2011;47:61–66. doi: 10.1007/s10597-009-9251-2. [DOI] [PubMed] [Google Scholar]
- Achenbach TM. Manual for the Child Behavior Checklist/4–18 and 1991 profile. Burlington, VT: University of Vermont, Department of Psychiatry; 1991. [Google Scholar]
- Achenbach TM, Rescorla LA. Manual for the ASEBA school-age forms & profiles: Child Behavior Checklist for ages 6–18, Teacher’s Report Form, & Youth Self-Report. Burlington, VT: University of Vermont, Research Center for Children, Youth & Families; 2001. [Google Scholar]
- Avenevoli S, Swendsen J, He J-P, Burstein M, Merikangas KR. Major depression in the National Comorbidity Survey-Adolescent Supplement: Prevalence, correlates, and treatment. Journal of the American Academy of Child & Adolescent Psychiatry. 2015;54:37–44. doi: 10.1016/j.jaac.2014.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bagner DM, Pettit JW, Lewinsohn PM, Seeley JR, Jaccard J. Disentangling the temporal relationship between parental depressive symptoms and early child behavior problems: A transactional framework. Journal of Clinical Child & Adolescent Psychology. 2013;42:78–90. doi: 10.1080/15374416.2012.715368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beyers W, Goossens L, Vansant I, Moors E. A structural model of autonomy in middle and late adolescence: Connectedness, separation, detachment, and agency. Journal of Youth and Adolescence. 2003;32:351–365. doi: 10.1023/A:1024922031510. [DOI] [Google Scholar]
- Booth A, Crouter AC. Does it take a village? Community effects on children, adolescents, and families. Mahwah, NJ: Lawrence Erlbaum; 2001. [Google Scholar]
- Briggs-Gowan MJ, Carter AS, Schwab-Stone M. Discrepancies among mother, child, and teacher reports: Examining the contributions of maternal depression and anxiety. Journal of Abnormal Child Psychology. 1996;24:749–765. doi: 10.1007/BF01664738. [DOI] [PubMed] [Google Scholar]
- Britner PA, Mossler DG. Professionals’ decision-making about out-of-home placements following instances of child abuse. Child Abuse & Neglect. 2002;26:317–332. doi: 10.1016/S0145-2134(02)00311-3. [DOI] [PubMed] [Google Scholar]
- Brooks-Gunn J, Duncan G, Aber JL. Neighborhood poverty: Context and consequences for children. New York, NY: Russell Sage Foundation; 1997. [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Best methods for the analysis of change. Thousand Oaks, CA: Sage; 1993. pp. 136–162. [Google Scholar]
- Bureau J-F, Easterbrooks MA, Lyons-Ruth K. Maternal depressive symptoms in infancy: Unique contribution to children’s depressive symptoms in childhood and adolescence? Development and Psychopathology. 2009;21:519–537. doi: 10.1017/S0954579409000285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burt SA. How do we optimally conceptualize the heterogeneity within antisocial behavior? an argument for aggressive versus non-aggressive behavioral dimensions. Clinical Psychology Review. 2012;32(4):263–279. doi: 10.1016/j.cpr.2012.02.006. doi: http://dx.doi.org.libproxy1.usc.edu/10.1016/j.cpr.2012.02.006. [DOI] [PubMed] [Google Scholar]
- Choe DE, Sameroff AJ, McDonough SC. Infant functional regulatory problems and gender moderate bidirectional effects between externalizing behavior and maternal depressive symptoms. Infant Behavior & Development. 2013;36:307–318. doi: 10.1016/j.infbeh.2013.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Archives of General Psychiatry. 2003;60:837–844. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- Derogatis LR. SCL-90-R: Administration, scoring and procedures: Manual II. Towson, MD: Clinical Psychometric Research; 1993. [Google Scholar]
- Derogatis LR, Melisaratos N. The Brief Symptom Inventory: An introductory report. Psychological Medicine. 1983;13:595–605. doi: 10.1017/S0033291700048017. [DOI] [PubMed] [Google Scholar]
- Dubowitz H, Papas MA, Black MM, Starr RH., Jr Child neglect: Outcomes in high-risk urban preschoolers. Pediatrics. 2002;109:1100–1107. doi: 10.1542/peds.109.6.1100. [DOI] [PubMed] [Google Scholar]
- Elgar FJ, McGrath PJ, Waschbusch DA, Stewart SH, Curtis LJ. Mutual influences on maternal depression and child adjustment problems. Clinical Psychology Review. 2004;24:441–459. doi: 10.1016/j.cpr.2004.02.002. [DOI] [PubMed] [Google Scholar]
- Finch AJ, Jr, Saylor CF, Edwards GL, McIntosh JA. Children’s Depression Inventory: Reliability over repeated administrations. Journal of Clinical Child Psychology. 1987;16:339–341. doi: 10.1207/s15374424jccp1604_7. [DOI] [Google Scholar]
- Foster CE, Webster MC, Weissman MM, Pilowsky DJ, Wickramaratne PJ, Talati A, King CA. Remission of maternal depression: Relations to family functioning and youth internalizing and externalizing symptoms. Journal of Clinical Child & Adolescent Psychology. 2008;37:714–724. doi: 10.1080/15374410802359726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gartstein MA, Bridgett DJ, Dishion TJ, Kaufman NK. Depressed mood and maternal report of child behavior problems: Another look at the depression-distortion hypothesis. Journal of Applied Developmental Psychology. 2009;30:149–160. doi: 10.1016/j.appdev.2008.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Godinet MT, Li F, Berg T. Early childhood maltreatment and trajectories of behavioral problems: Exploring gender and racial differences. Child Abuse & Neglect. 2014;38:544–556. doi: 10.1016/j.chiabu.2013.07.018. doi: http://dx.doi.org.libproxy2.usc.edu/10.1016/j.chiabu.2013.07.018. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Rouse MH, Connell AM, Broth MR, Hall CM, Heyward D. Maternal depression and child psychopathology: A meta-analytic review. Clinical Child and Family Psychology Review. 2011;14:1–27. doi: 10.1007/s10567-010-0080-1. [DOI] [PubMed] [Google Scholar]
- Guyon-Harris K, Huth-Bocks A, Lauterbach D, Janisse H. Trajectories of maternal depressive symptoms across the birth of a child: Associations with toddler emotional development. Archives of Women’s Mental Health. 2015 doi: 10.1007/s00737-015-0546-8. Advance online publication. [DOI] [PubMed] [Google Scholar]
- Hankin BL, Young JF, Abela JRZ, Smolen A, Jenness JL, Gulley LD, Oppenheimer CW. Depression from childhood into late adolescence: Influence of gender, development, genetic susceptibility, and peer stress. Journal of Abnormal Psychology. 2015;124(4):803–816. doi: 10.1037/abn0000089. Retrieved from http://libproxy.usc.edu/login?url=http://search.proquest.com.libproxy1.usc.edu/docview/1735911448?accountid=14749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanington L, Ramchandani P, Stein A. Parental depression and child temperament: Assessing child to parent effects in a longitudinal population study. Infant Behavior and Development. 2010;33:88–95. doi: 10.1016/j.infbeh.2009.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartung CM, McCarthy DM, Milich R, Martin CA. Parent-adolescent agreement on disruptive behavior symptoms: A multitrait-multimethod model. Journal of Psychopathology and Behavioral Assessment. 2005;27:159–168. doi: 10.1007/s10862-005-0632-8. [DOI] [Google Scholar]
- Hodges K. Depression and anxiety in children: A comparison of self-report questionnaires to clinical interview. Psychological Assessment. 1990;2:376–381. doi: 10.1037/1040-3590.2.4.376. [DOI] [Google Scholar]
- Hughes EK, Gullone E. Reciprocal relationships between parent and adolescent internalizing symptoms. Journal of Family Psychology. 2010;24:115–124. doi: 10.1037/a0018788. [DOI] [PubMed] [Google Scholar]
- Hummel AC, Kiel EJ. Maternal depressive symptoms, maternal behavior, and toddler internalizing outcomes: A moderated mediation model. Child Psychiatry and Human Development. 2015;46:21–33. doi: 10.1007/s10578-014-0448-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine & National Research Council. New directions in child abuse and neglect research. Washington, DC: National Academies Press; 2014. [PubMed] [Google Scholar]
- Jonson-Reid M, Kohl PL, Drake B. Child and adult outcomes of chronic child maltreatment. Pediatrics. 2012;129:839–845. doi: 10.1542/peds.2011-2529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz SJ, Hammen CL, Brennan PA. Maternal depression and the intergenerational transmission of relational impairment. Journal of Family Psychology. 2013;27:86–95. doi: 10.1037/a0031411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes KM, Eaton NR, Krueger RF, McLaughlin KA, Wall MM, Grant BF, Hasin DS. Childhood maltreatment and the structure of common psychiatric disorders. British Journal of Psychiatry. 2012;200:107–115. doi: 10.1192/bjp.bp.111.093062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinard EM. Mother and teacher assessments of behavior problems in abused children. Journal of the American Academy of Child & Adolescent Psychiatry. 1995;34:1043–1053. doi: 10.1097/00004583-199508000-00014. [DOI] [PubMed] [Google Scholar]
- Kiss E, Gentzler AM, George C, Kapornai K, Tamás Z, Kovacs M, Vetró Á. Factors influencing mother-child reports of depressive symptoms and agreement among clinically referred depressed youngsters in Hungary. Journal of Affective Disorders. 2007;100:143–151. doi: 10.1016/j.jad.2006.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kouros CD, Garber J. Dynamic associations between maternal depressive symptoms and adolescents’ depressive and externalizing symptoms. Journal of Abnormal Child Psychology. 2010;38:1069–1081. doi: 10.1007/s10802-010-9433-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovacs M. The Children’s Depression Inventory (CDI) Psychopharmacology Bulletin. 1985;21:995–998. [PubMed] [Google Scholar]
- Kovacs M. Children’s Depression Inventory manual. North Tonawanda, NY: Multi-Health Systems; 1992. [Google Scholar]
- Kovacs M. Children’s Depression Inventory (CDI) Toronto, Canada: Multi-Health Systems; 2004. [Google Scholar]
- Kroes G, Veerman JW, De Bruyn EEJ. Bias in parental reports? Maternal psychopathology and the reporting of problem behavior in clinic-referred children. European Journal of Psychological Assessment. 2003;19:195–203. doi: 10.1027//1015-5759.19.3.195. [DOI] [Google Scholar]
- Lo CC, Cheng TC. The impact of childhood maltreatment on young adults’ substance abuse. American Journal of Drug and Alcohol Abuse. 2007;33:139–146. doi: 10.1080/00952990601091119. [DOI] [PubMed] [Google Scholar]
- McCullough C, Shaffer A. Maternal depressive symptoms and child externalizing problems: Moderating effects of emotionally maltreating parenting behaviors. Journal of Child and Family Studies. 2014;23:389–398. doi: 10.1007/s10826-013-9804-4. [DOI] [Google Scholar]
- Mustillo SA, Dorsey S, Conover K, Burns BJ. Parental depression and child outcomes: The mediating effects of abuse and neglect. Journal of Marriage and Family. 2011;73:164–180. doi: 10.1111/j.1741-3737.2010.00796.x. [DOI] [Google Scholar]
- Muthen LK, Muthen BO. Mplus (version 7.2) Los Angeles, CA: Muthen & Muthen; 2014. [Google Scholar]
- National Research Council (US) and Institute of Medicine (US) Board on Children, Youth, and Families. Adolescent Risk and Vulnerability: Concepts and Measurement. In: Fischhoff B, Nightingale EO, Iannotta JG, editors. Vulnerability, Risk, and Protection. Vol. 3. Washington (DC): National Academies Press (US; 2001. Available from: https://www.ncbi.nlm.nih.gov/books/NBK223737/ [PubMed] [Google Scholar]
- National Research Council & Institute of Medicine. Depression in parents, parenting, and children: Opportunities to improve identification, treatment, and prevention. Washington, DC: National Academies Press; 2009. [PubMed] [Google Scholar]
- Nicholson JS, Deboeck PR, Farris JR, Boker SM, Borkowski JG. Maternal depressive symptomatology and child behavior: Transactional relationship with simultaneous bidirectional coupling. Developmental Psychology. 2011;47:1312–1323. doi: 10.1037/a0023912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palaszynski K, Nemeroff CB. The medical consequences of child abuse and neglect. Psychiatric Annals. 2009;39:1004–1009. doi: 10.3928/00485718-20091123-02. [DOI] [Google Scholar]
- Ruiperez MÁ, Ibáñez MI, Lorente E, Moro M, Ortet G. Psychometric properties of the Spanish version of the BSI: Contributions to the relationship between personality and psychopathology. European Journal of Psychological Assessment. 2001;17:241–250. doi: 10.1027//1015-5759.17.3.241. [DOI] [Google Scholar]
- Satorra A, Bentler PM. A scaled difference chi-square test statistic for moment structure analysis. Psychometrika. 2001;66(4):507–514. doi: 10.1007/s11336-009-9135-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shapiro DL, Levendosky AA. Adolescent survivors of childhood sexual abuse: The mediating role of attachment style and coping in psychological and interpersonal functioning. Child Abuse & Neglect. 1999;23:1175–1191. doi: 10.1016/S0145-2134(99)00085. [DOI] [PubMed] [Google Scholar]
- Silberg J, Rutter M, Neale M, Eaves L. Genetic moderation of environmental risk for depression and anxiety in adolescent girls. British Journal of Psychiatry. 2001;179:116–121. doi: 10.1192/bjp.179.2.116. [DOI] [PubMed] [Google Scholar]
- Silverthorn P, Frick PJ. Developmental pathways to antisocial behavior: The delayed-onset pathway in girls. Development and Psychopathology. 1999;11:101–126. doi: 10.1017/S0954579499001972. [DOI] [PubMed] [Google Scholar]
- Smith MS, Mitchell J, McCauley EA, Calderon R. Screening for anxiety and depression in an adolescent clinic. Pediatrics. 1990;85:2562–2566. [PubMed] [Google Scholar]
- Smith SR. Making sense of multiple informants in child and adolescent psychopathology. A guide for clinicians. Journal of Psychoeducational Assessment. 2007;25:139–149. doi: 10.1177/0734282906296233. [DOI] [Google Scholar]
- Sundin EC, Baguley T. Prevalence of childhood abuse among people who are homeless in Western countries: A systematic review and meta-analysis. Social Psychiatry and Psychiatric Epidemiology. 2015;50:183–194. doi: 10.1007/s00127-014-0937-6. [DOI] [PubMed] [Google Scholar]
- van Dam DS, van Nierop M, Viechtbauer W, Velthorst E, van Winkel R, Bruggeman R, Wiersma D. Childhood abuse and neglect in relation to the presence and persistence of psychotic and depressive symptomatology. Psychological Medicine. 2015;45:1363–1377. doi: 10.1017/S0033291714001561. [DOI] [PubMed] [Google Scholar]
- van der Meer M, Dixon A, Rose D. Parent and child agreement on reports of problem behaviour obtained from a screening questionnaire, the SDQ. European Child & Adolescent Psychiatry. 2008;17:491–497. doi: 10.1007/s00787-008-0691-y. [DOI] [PubMed] [Google Scholar]
- Webb JA, Bray JH, Getz JG, Adams G. Gender, perceived parental monitoring, and behavioral adjustment: Influences on adolescent alcohol use. American Journal of Orthopsychiatry. 2002;72:392–400. doi: 10.1037/0002-9432.72.3.392. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Pilowsky DJ, Wickramaratne PJ, Talati A, Wisniewski SR, Fava M, Rush AJ. Remissions in maternal depression and child psychopathology: A STAR*D-child report. Journal of the American Medical Association. 2006;295:1389–1398. doi: 10.1001/jama.295.12.1389. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Wickramaratne P, Nomura Y, Warner V, Pilowsky D, Verdeli H. Offspring of depressed parents: 20 years later. American Journal of Psychiatry. 2006;163:1001–1008. doi: 10.1176/ajp.2006.163.6.1001. [DOI] [PubMed] [Google Scholar]
- Wrobel NH, Lachar D, Wrobel TA. Self-report problem scales and subscales and behavioral ratings provided by peers: Unique evidence of test validity. Assessment. 2005;12(3):255–269. doi: 10.1177/1073191105278297. Retrieved from http://libproxy.usc.edu/login?url=http://search.proquest.com.libproxy1.usc.edu/docview/620863751?accountid=14749. [DOI] [PubMed] [Google Scholar]