Abstract

Introduction:
Acne is a common condition that can result in permanent scarring. Acne scars can be broken down into three categories: atrophic; hypertrophic; and keloidal. Atrophic scars can be further sub-classified into: ice pick; rolling; and boxcar.
Objectives and Methods:
We have performed a comprehensive literature search of the last ten years in order to determine the efficacy and adverse reactions of commonly used treatments against post-acne scarring.
Results:
A total of 36 relevant articles were identified on the following interventions: subcision (n = 10), dermabrasion (n = 1), microneedling (n = 8), dermal fillers (n = 5), and chemical peeling (n = 12).
Discussion:
Improvement in the appearance of post-acne scarring following subcision is in the range of 10–100%. Microdermabrasion achieved the least significant results. A total of 27.3% patients did not achieve any benefit despite eight treatment sessions, and only 9.1% achieved good results. All patients treated with microneedling achieved some improvement in scar appearance in the range of 31–62%. Dermal fillers also led to favourable outcomes. In particular, treatment with PPMA led to improvement in 84% of patients. Utilising chemical peels, trichloroacetic acid (TCA) CROSS achieved >70% improvement in 73.3% of patients, whereas 20% glycolic acid did not lead to any improvement in 25%.
Conclusion:
Post-acne scarring is a common and challenging condition with no easy and definitive solution. The above interventions have been used with varying degrees of efficacy, each having both pros and cons. All have been deemed to be safe with few and transient adverse reactions. However, further trials with a larger number of patients are necessary in order to reach more concrete conclusions regarding their efficacy.
Keywords: acne, dermabrasion, evidence, fillers, microneedling, peeling, post-acne, review, scar, scarring, subcision
Lay summary
Acne is a common condition that can result in permanent scarring. We have performed a comprehensive literature search of the last 10 years in order to determine the efficacy and side effects of commonly used treatments against post-acne scarring. A total of 36 relevant articles were identified on the following interventions: subcision (10), dermabrasion (one), microneedling (eight), dermal fillers (five), and chemical peeling (12). Post acne scarring is a common and challenging condition with no easy and definitive solution. The above interventions have been used with varying degrees of efficacy, each having both pros and cons. All have been deemed to be safe with few and transient adverse reactions. However, further trials with larger number of patients are necessary in order to reach more concrete conclusions regarding their efficacy.
Introduction
Acne is a common condition with prevalence as high as 80% among adolescents.1 All body areas with high concentrations of pilosebaceous glands may be involved, but the commonest affected areas include the face, back and chest.2 Acne lesions can result in permanent scarring with a marked impact on quality of life. Genetic factors, disease severity and delay in treatment are the main factors influencing scar formation.2 The prevalence and severity of acne scarring in the population is largely unknown.1 A British study looking at 2133 volunteers with the age range of 18–70 years showed that 1% of the population reported having acne scars, 14% of which thought their scars to be disfiguring.3
Acne scars can be broken down into three main categories, depending on whether there is a net loss or gain of collagen: atrophic; hypertrophic; and keloidal. Of people with acne scars, 80–90% have scars associated with a loss of collagen (atrophic scars) compared with a minority who develop hypertrophic scars and keloids (more commonly seen on the chest and shoulders).2
Atrophic scars can be further sub-classified into: ice pick; rolling; and boxcar. The exact prevalence of each scar type is hard to calculate but some estimations report that within atrophic scars, the ice pick type represents 60–70%, boxcar 20–30%, and rolling scars 15–25%.2,4
Ice pick scars are narrow, sharply demarcated, V-shaped tracts, <2 mm in diameter, that extend into the deep dermis or even subcutaneous layer. Boxcar scars are wider (1–4 mm in diameter), U-shaped tracts, with sharp, vertical edges that extend 0.1–0.5 mm into the dermis. Rolling scars are characterised by dermal tethering of the dermis to the subcutis. They are generally ≥4 mm in diameter, irregular, with a rolling or undulating appearance.2
Hypertrophic scars are typically raised and firm scars that remain within the borders of the original site of injury. In contrast, keloid scars form as reddish-purple papules and nodules that extend beyond the borders of the original wound.5
Scar classification is important as it can help guide treatment options. Ice pick scars can extend deep into the dermis, which makes them resistant to conventional skin-resurfacing options. Rolling scars are wider and have fibrous anchoring to the subcutis, thus necessitating treatment at a sub-dermal level. Shallow boxcar scars are more amenable to skin resurfacing treatments whereas deeper boxcar scars are more resistant to such superficial treatments.6
However, it may be difficult to differentiate clinically between them, and different types of scars may also be present in the same patient (Table 1 and Figure 1).
Table 1.
Acne scar classification (adapted from Jacob et al [49]).
| Acne scars subtype | Clinical features |
|---|---|
| Ice pick | Ice pick scars are narrow (<2 mm), deep, sharply demarcated tracts that extend vertically to the deep dermis or subcutaneous tissue |
| Rolling | Rolling scars may reach ≥5 mm in diameter. They have a rolling or undulating appearance that occurs from fibrous tethering of the dermis to the subcutis |
| Boxcar | Boxcar scars are oval depressions with sharply demarcated vertical edges. They are wider at the surface than ice pick scars and do not taper to a point at the base |
Figure 1.
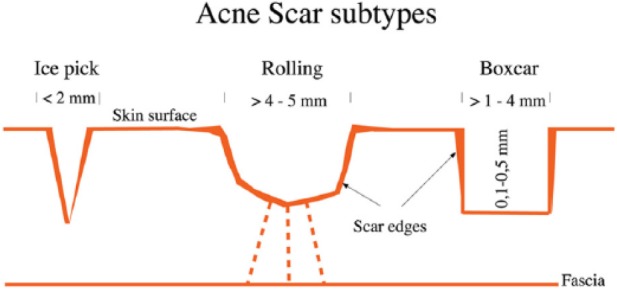
Acne scar subtypes (adapted from Fabbrocini et al [2]).
Scar severity is another important factor in the management of scars. It is used as a tool of identifying a suitable treatment to evaluate outcomes.7 Several different modalities have been devised. Such assessments can be objective (they require devices to measure their physical attributes) or subjective (observer dependent). Subjective methods can be either quantitative or qualitative and can be performed both by clinicians and/or the patients themselves. Examples of such grading scales include the Vancouver Scar Scale (VSS), Goodman and Baron Qualitative and Qualitative grading scales, Patient and Observer Scar Assessment Scale (POSAS), Visual Analog Scale (VAS) and the Patient Satisfaction Score (PSS) (Table 2).2,7–9
Table 2.
An example of a commonly used acne scar severity grading scale (adapted from Goodman et al [7]).
| Grade | Clinical features | |
|---|---|---|
| 1 | Macular | Macular erythematous, hyperpigmented or hypopigmented flat marks |
| 2 | Mild | Mild atrophic or hypertrophic scarring that may not be obvious at social distances of 50 cm or greater and easily covered by makeup or beard hair in men |
| 3 | Moderate | Moderate atrophic or hypertrophic scarring that is obvious at social distances of 50 cm or greater and is not covered easily by makeup or beard hair in men, but is still able to be flattened by manual stretching of the skin |
| 4 | Severe | Severe atrophic or hypertrophic scarring not flattened by manual stretching of the skin |
Treatment options can be broadly categorised into energy-based and non-energy-based. Commonly used energy-based technologies include ablative and non-ablative lasers, fractional radiofrequency, intense pulsed light and plasma skin regeneration. Non-energy-based devices include subcision, (micro)dermabrasion, microneedling, dermal fillers and chemical peels.
Subcision (subcutaneous incisionless surgery) is a non-operative technique that involves a needle being inserted subcutaneously and handled in a fanning motion in order to untether the fibrous strands within the scar, and stimulate new connective tissue formation that will help elevate the depressed surface of scars. Local anaesthetic agents are often applied to reduce procedure-related pain. In post-acne scarring, subcision has been used mainly in the treatment of rolling atrophic scars.10
Dermabrasion (DA) and microdermabrasion (MDA) are facial-resurfacing techniques that mechanically ablate damaged skin in order to promote re-epithelialisation. Although the act of physical abrasion of the skin is common to both procedures, DA and MDA employ different instruments with a different technical execution.2
DA completely removes the epidermis and penetrates to the level of the papillary or reticular dermis, inducing remodelling of the skin’s structural proteins, and is performed under local or general anaesthesia. A motorised hand piece rotates a wire brush or a diamond fraise. There is often pinpoint bleeding of the raw wound that subsides with appropriate wound care.2
MDA is a much more superficial treatment and only removes the stratum corneum, accelerating the natural process of exfoliation.2,11 A variety of different devices are available that differ on the source of the abrasive component. Unlike DA, MDA can be repeated at short intervals, has no down time, is painless, does not require anaesthesia and is thought to cause fewer complications, but also a lesser effect on scars.2,11
Skin microneedling involves puncturing the skin multiple times using a dermaroller and is used to treat several skin conditions, such as pigmentary disorders, wrinkles, post-acne atrophic scars and burn scars.
Skin needling is thought to have a lower risk of post-inflammatory hyperpigmentation than other procedures and can be safely performed on all skin types. Due to the pain associated with microneedling, topical anaesthetic creams are often necessary.2,12
Dermal fillers involve the injection of foreign body gels into the dermal or subdermal tissue in order to provide localised volume gain.13 Multiple fillers with different properties are available and can be classified according to their biodegradability into temporary, semi-permanent or permanent.14
Chemical peeling is the process of applying chemicals to the skin in order to destroy the outer damaged layers, thus accelerating the normal process of exfoliation, leading to tissue remodelling, thereby decreasing scar appearance.15 Different agents have different depths of penetration and can be categorised into four different groups: very superficial; superficial; medium; and deep (Table 3).1 Deep peels require sedation and have the potential to cause cardiotoxicity and hypo-/hyperpigmentation.16 Pre-treatment with tretinoin and other desquamating agents is often used prior to medium and deep peeling in order to enhance the even penetration of peeling agents and minimise the risk of post-peel hyperpigmentation.17
Table 3.
Classification of peeling agents (adapted from Gozali et al [1]).
| Depth of penetration | Histologic level | Peeling agents |
|---|---|---|
| Very superficial | Destruction of the stratum corneum without creating a wound below the stratum granulosum | • GA, 30–50%, applied briefly (1–2 min) • Jessner’s solution, applied in 1 to 3 coats TCA 10%, applied in 1 coat |
| Superficial | Destruction of part or all of the epidermis, anywhere from the stratum granulosum to the basal cell layer | • GA, 50–70%, applied for a variable time (2–20
min) • Jessner’s solution, applied in 4 to 10 coats • TCA, 10–30% |
| Medium depth | Destruction of the epidermis and part or all of the papillary dermis | • GA 70%, applied for a variable time (3–30 min) • TCA, 35–50% Augmented TCA (CO2 plus TCA 35%; Jessner’s solution plus TCA 35%; GA 70% plus TCA 35%) |
| Deep | Destruction of the epidermis and papillary dermis, extending into the reticular dermis | • Phenol 88% • Baker-Gordon phenol formula |
Objectives and methods
The objective of this review is to provide an overview of the classification methods of post-acne scarring according to type and degree of severity and determine the efficacy and indications of the treatments commonly used in post-acne scarring.
A comprehensive literature search of the last ten years was performed on PubMed. A search using the keywords [(Scar(s), scarring) AND (acne)] was utilised. Selected articles were those focusing on the commonly used non-energy techniques, namely subcision, DA, MDA, microneedling, chemical peeling and dermal fillers. Individual case reports and articles not written in English were excluded. A total of 36 relevant articles were identified following review of their abstracts.
Results
Subcision
The treatment of post-acne scarring with subcision was assessed in ten studies. The scars treated were mainly of the rolling type, with some studies including a combination of the other types. In six papers, subcision was used in isolation; in one it was used in conjunction with subsequent suctioning; in one with either dermaroller or cryoroller application; in one with 15% trichloroacetic acid (TCA) peel; and in one study with 50% TCA peel (Table 4).
Table 4.
A synopsis of subcision studies.
| Authors | Publication year | Patient no. | Level of evidence | Indication | Cosmetic outcome | Adverse effects |
|---|---|---|---|---|---|---|
| Balighi et al. | 2008 | 20 | 2.d | Rolling acne scars | Subcision only: moderate improvement 20%, mild 70%, none 10%; subcision with implant: moderate improvement 10%, mild 75%, none 15% | Swelling, skin infections, bruising |
| Sage et al. | 2011 | 10 | 2.c | Various morphologic acne scar types | 2.95 mean improvement (3 = minimal, 4 = moderate improvement) |
Pain, erythema, swelling, discolouration, bruising and lumpiness |
| Ramadan et al. | 2011 | 20 | 2.d | Rolling acne scars | Mean decrease in scar size: 0.3867 ± 0.09 cm2 | Erythema |
| Harandi et al. | 2011 | 58 | 2.d | Various types, 77.6% acne, 22.4% non-acne depressed scars | Group A (regular suctioning): 60–90% scar
improvement group B (suctioning with longer intervals): 30–60% improvement |
Oedema, bruising, hyperpigmentation, haemorrhagic papule and pustule formation, hypertrophic scarring |
| Al-Dhalimi et al. | 2012 | 34 | 2.d | Mainly rolling acne scars | Mild scarring: 0% pre-Tx, 52.94% post-Tx Moderate: 76.48% pre-Tx, 44.11% post-Tx Severe: 23.52% pre-Tx, 2.92% post-Tx |
Erythema, bruising, swelling, mild pain, lumpiness |
| Gadkari et al. | 2014 | 30 | 2.d | Various morphologic acne scar types | Subcision plus dermaroller: 40% improvement; subcision plus cryoroller: 57% improvement | Oedema, hematoma formation, erythema, hyperpigmentation |
| Gard et al. | 2014 | 49 | 2.d | Various morphologic acne scar types | Grade 4 scars: 75% of patients reported 50–74% improvement and 25% reported 25–29% improvement; grade 3 scars: 36.4% of patients reported 75–100% improvement and 63.6% reported 50–74% improvement; grade 2 scars: 100% of patients reported 75–100% improvement | Erythema, oedema, exfoliation, hyper-pigmentation, cervical lymphadenopathy |
| Kaur et al. | 2014 | 10 | 2.d | Various morphologic acne scar types | Subcision plus TCA: 100% scar improvement from grade 4 to grade 2 | Erythema, oedema, crusting, hyperpigmentation |
| Nilforoushzadeh et al. | 2015 | 8 | 2.d | Rolling acne scars | Average number of lesions pre-Tx: 24.8 ± 12.1; average number of lesions post-Tx: 12.8 ± 2.1 | Swelling and inflammation |
| Barikbin et al. | 2016 | 18 | 2.d | Mainly rolling acne scars | Marked improvement 50%, moderate 33.3%, mild 16.7% | Tenderness, swelling, periorbital ecchymoses |
Balighi et al. performed a split-faced study in 20 patients.18 Using 18-gauge needles, one side of the face underwent subcision and the other side underwent subcision in conjunction with subdermal implant of an absorbable size 0 suture. At six-month follow-up on the subcision side, two (10%) patients had no improvement, 14 (70%) had mild improvement and four (20%) had moderate improvement. On the subcision with implant side, three (15%) patients had no improvement, 15 (75%) had mild improvement and two (10%) had moderate improvement.
In a randomised split-face study of ten patients, the effects of subcision with an 18-gauge Nokor needle were compared with those of collagen fillers in the treatment of different types of depressed acne scars.19
Results were measured using the following scale: 1 = worse than before treatment; 2 = no change; 3 = minimal disappearance; 4 = moderate disappearance; 5 = complete disappearance.
Blinded mean physician assessment at six-month follow-up for global improvement was graded as 2.95 and 3.05 (P = 0.69), and mean patient rating as 3.9 and 2.9 (P = 0.19) for subcision and fillers, respectively.
Ramadan et al. performed a split-face study on 20 patients with rolling acne scars, comparing the effects of subcision with those of 100% TCA CROSS (chemical reconstruction of skin scars) chemical peel. Subcision was performed using a 1.5-in. NoKor Admix needle.20
The authors reported a mean decrease in the size of scars following subcision and peeling by 0.3867 ± 0.09 cm2 and 0.08657 ± 0.090 cm2 (P <0.01), respectively. Depths of all scars were also found to have decreased following subcision (P <0.01).
Another study reported the results of a novel technique that included subcision with subsequent suctioning for a two-week period.21 They treated 58 patients (45 with acne scars and 13 with depressed non-acne scars) using mainly 23-gauge needles and applying suctioning with the hand piece of a MDA device. The aim behind suctioning was the avoidance of scar re-depression.
In Group A (46 patients who started suctioning three days after subcision and had almost daily or every other day suctioning), both investigators and patients observed a 60–90% scar improvement. In Group B (12 patients who started suctioning five to seven days after subcision, and/or had intervals of two to three days between sessions), improvement was in the range of 30–60%.
Al-Dhalimi et al. used subcision with an 18-gauge needle on 34 Iraqi patients with predominantly rolling scars. Of them, no patients had mild grade scarring, 26 (76.48%) had moderate scarring and eight (23.52%) had severe scarring.22 At six-month follow-up, 18 (53%) patients had mild scarring, 15 (44%) had moderate scarring and one (3%) had severe scarring.
Seven (21%) patients reported being partially or moderately satisfied by the procedure, 22 (65%) reported being greatly satisfied and five (15%) reported being fully satisfied.
A split-face study on 30 patients with multiple types of acne scarring assessed subcision followed by dermaroller on one side and subcision followed by cryoroller on the other. Instruments used included: 20-gauge hypodermic needles; 192 needles (2.5 mm each) dermaroller; and liquid nitrogen –20° cryoroller.23
On the subcision and cryoroller side, mean percentage improvement was documented as 57%. On the subcision and dermaroller side, mean percentage improvement was 40%.
Gard et al. treated 49 patients with subcision using a 24-gauge needle.24 Subsequently, the patients were treated further with repeated sessions of dermaroller (192 needles of 1.5 mm size) and 15% TCA peel two-weekly for six sessions each.
All 49 patients (100%) had improvement in their scars by some grade. In patients with grade 4 scars (Goodman and Baron Qualitative grading scale), 12 patients (75%) graded their response to treatment as very good (50–74% improvement) and four patients (25%) as good (25–29% improvement). In patients with grade 3 scars, eight patients (36.4%) graded their response to treatment as excellent (75–100% improvement) and 14 patients (63.6%) as very good (50–74% improvement). All 11 patients (100%) with grade 2 scars graded their response as excellent (improvement 75–100%). A poor response with 0–24% improvement in scars was not reported by any of the patients.
A different study used a combination of subcision followed by 50% TCA peel to treat ten patients with atrophic acne scars of severity grade 4 (GBQ scale).25 Subcision was performed using an 18-gauge hypodermic needle and was followed by 50% TCA CROSS at four-week intervals for three sessions. In all patients (100%), scar grading improved from grade 4 to grade 2.
When asked, six patients reported personal satisfaction as excellent (greater than 70% improvement), three as good (50–70% improvement) and one as fair (30–50% improvement).
In a further study, subcision was performed on eight patients with rolling scars using an 18-gauge spinal needle.26 Results showed good and very good improvement in 88% of patients. The average number of lesions before treatment was 24.8 ± 12.1. Following treatment, this was reduced to 12.8 ± 2.1 (P <0.05).
All patients expressed treatment satisfaction as either good or very good.
The most recent subcision study treated 18 patients with primarily rolling scars using a ‘blunt subcision blade’ (a stainless steel blade with tapering edges, 6 cm or 13 cm in length and 1.5 mm in width).27 At six-month follow-up they achieved overall marked aesthetic improvement of scars in nine cases (50%), moderate improvement in six cases (33.3%) and mild improvement in three patients (16.7%). Twelve patients (66.7%) expressed high satisfaction with the results, five (27.8%) were moderately satisfied and one (5.5%) reported no improvement.
Dermabrasion and microdermabrasion
Only one study was identified that assessed the efficacy of MDA. It included 11 patients with moderate to severe post-acne atrophic scarring of various types who underwent a series of eight weekly treatment sessions.11 They used suction powers in the range of 40–60 kpa and four to six passes in each direction were performed (directed horizontally, vertically and obliquely). The average treatment lasted approximately 15 min, with the endpoint being clinical erythema (conservative MDA, aiming to remove only the stratum corneum).
Patients were evaluated clinically by two physicians and response graded on a five-point scale (None = 0% improvement, Mild = 1–25% improvement, Moderate = 26–50% improvement, Good = 51–75% improvement, Very good = 76–100% improvement).
Following eight sessions of MDA, three (27.3%) patients achieved no improvement, five (45.4%) mild improvement, two (18.2%) moderate improvement and one (9.1%) good improvement. No patients (0%) were found to have achieved very good improvement in scar appearance.
Microneedling
A total of eight studies utilised microneedling in the treatment of post-acne scarring. Treated scars were of various morphologic subtypes. In five papers, microneedling was used in isolation, in one it was compared with glycolic acid (GA) peeling and in another it was used in conjunction with platelet-rich plasma (PRP) (Table 5).
Table 5.
A synopsis of microneedling studies.
| Authors | Publication year | Patient no. | Level of evidence | Indication | Cosmetic outcome | Adverse effects |
|---|---|---|---|---|---|---|
| Fabbrocini et al. | 2008 | 32 | 2.d | Rolling acne scars | All patients achieved evident improvement in scar appearance | Erythema and swelling |
| Alam et al. | 2014 | 15 | 1.c | Various morphologic acne scar types | Mean improvement of 3.4 (based on the quantitative global scarring grading system) | Pain, erythema and oedema |
| Chawla et al. | 2014 | 27 | 2.d | Various morphologic acne scar types | Microneedling plus PRP: 18.5% achieved two-grade
improvement; microneedling plus PRP: 7% achieved two-grade improvement (based on the quantitative global scarring grading system) |
Hyperpigmentation |
| Dogra et al. | 2014 | 30 | 2.d | Various morphologic acne scar types | Moderate scaring: 4.56 ± 1.31 improvement; severe scaring: 6.00 ± 1.66 improvement (based on a 9-point scale) |
Pain, erythema, swelling, hyperpigmentation, tram-track scarring and ecchymoses |
| Nofal et al. | 2014 | 35 | 2.d | Various morphologic acne scar types | Pre Tx: 34 patients with grade 4 scarring; post Tx: 23 patients improved to grade 2 and 3 scaring | Pain, bruising, hyperpigmentation, erythema and oedema |
| El-Domyati et al. | 2015 | 10 | 2.d | Various morphologic acne scar types | 51–60% improvement in the appearance of scars and 40–50% improvement in skin texture | Oedema, pain and erythema |
| Asif et al. | 2016 | 50 | 2.d | Various morphologic acne scar types | Microneedling plus PRP: 62.20%
improvement; microneedling plus water: 45.84% improvement |
Acne flare-up, hyperpigmentation, milia, erythema, bruising |
Fabbrocini et al. treated 32 patients with two sessions (eight weeks apart) of microneedling using an MS4 dermaroller with 96 1.5 mm long and 0.25 mm wide needles.28 Eight weeks after the first session, all patients had smoother facial skin and a slight reduction in scar severity. Eight weeks after the second session, there was evident improvement in the scar appearance.
Another study compared the effects of microneedling with those of microneedling plus GA peeling.29 They treated 30 patients with multiple types of atrophic scars who were split equally between the two groups. Microneedling was performed every six weeks for five sessions with an MF8 dermaroller (a drum-shaped device with 192 needles, each with a width of 0.25 mm and length of 1.5 mm). Group B underwent the same process of microneedling followed by 35% GA peel three weeks later.
At three-month follow-up, scar scoring in group B was better than that of group A (P = 0.001). The mean improvement in scars in group A was 31.33%, while that in group B was found to be 62%. In addition to the improvement in scars, there was also an improvement in skin texture and tone.
Alam et al. performed a randomised, split-face, placebo-controlled clinical trial in order to investigate the effects of microneedling on a mixture of various morphologic scar subtypes.30 Fifteen individuals received three needling treatments that were performed at two-week intervals using an MTS Roller, CR10 (1.0 mm) or CR20 (2.0 mm). The roller depth was determined by clinical evaluation of skin thickness and scar severity. Two blinded dermatologists separately rated participants’ acne scars based on the quantitative global scarring grading system.
Mean scar scores were significantly lower in the treatment group compared with baseline at six months (mean difference, 3.4; 95% confidence interval [CI], 0.2–6.5; P = 0.03) and nominally but not significantly lower compared with baseline at three months (mean difference, 2.4; 95% CI, −0.01 – 4.8; P = 0.052). In the control group, mean scar scores did not vary significantly from baseline at three months (mean difference, 1.0; 95% CI, −1.4 – 3.4; P = 0.96) and at six months (mean difference, 0.4; 95% CI, −2.3 – 3.5; P >0.99). The mean pain rating was recorded as 1.08/10.
A further split-face study on 27 patients assessed the effects of microneedling with PRP versus microneedling with vitamin C application.31 Microneedling was carried out with a 1.5 mm, 192-needle dermaroller. Scaring improvement was rated using the Goodman and Baron scale. An improvement by two grades was considered excellent, one grade was rated as good and no change was labelled as a poor response. Twenty-three patients achieved reduction in scarring by one to two grades. Excellent response was seen in five (18.5%) patients with PRP compared with two (7%) patients who received treatment with vitamin C.
Dogra et al. reviewed the response to five monthly sessions of dermaroller treatment in 30 patients with mixed types of atrophic acne scaring.32 The equipment used was a 192-needle drum-shaped dermaroller with 1.5 mm long and 0.1 mm wide needles. The procedure was concluded when uniform pinpoint bleeding was achieved. Scar assessment was performed on a nice-point scale.
At baseline, mean acne scar assessment scoring was 11.73 ± 3.12. At five-month follow-up, the mean scoring had reduced to 6.5 ± 2.71. Mean scoring difference in patients with moderate and severe grade scarring was 4.56 ± 1.31 and 6.00 ± 1.66, respectively. Four patients (13.3%) reported results as excellent, 20 (66.6%) as good and six (20.0%) as poor.
Another study compared the effects of PRP versus the CROSS peeling technique with 100% TCA versus combined microneedling and PRP in the treatment of atrophic acne scars.33 Forty-five patients with atrophic acne scars were split equally between the three groups. Each patient underwent three sessions at two-week intervals. Microneedling was performed using an MT20 dermaroller with 192 2 mm long needles.
Using the qualitative global scarring grading system, it was found that the three groups showed highly significant improvement in the severity of acne scars after treatment (P <0.001). Before treatment, there were 34 patients with grade 4 acne scarring. After treatment, 23 patients improved to grades 2 and 3. There was no statistically significant difference in the degree of improvement between the three groups (P = 0.87). There was no statistically significant difference in patient satisfaction between the three groups either (P = 0.6).
El-Domyati et al. evaluated the response of microneedling on ten patients with different types of post-acne atrophic scaring.34 They utilised a dermaroller with 192 1.5 mm long and 0.25 mm wide needles. Clinical improvement was evaluated using a five-point scale (None = 0%, Mild = 1–25%, Moderate = 26–50%, Good = 51–75%, and Very good = 76–100%).
At three-month follow-up, patients were found to have a 51–60% improvement in the appearance of scars (P = 0.01) and 40–50% improvement in skin texture (P = 0.01). Patient satisfaction was documented as being 80–85% (P = 0.001).
Finally, in a split-face study with 50 patients, the effects of microneedling along with topical application and intradermal injections of PRP were compared with those of microneedling and intradermal administration of distilled water.12 Microneedling was performed on all patients using a dermaroller device with 192 needles, each 1.5 mm in size. Pinpoint bleeding was taken as the endpoint of microneedling
On evaluation of Goodman’s Qualitative scores, the PRP half of the face showed a reduction of two grades in 20 (40%) patients and a reduction of one grade in 30 (60%) patients. The other half of the face showed a reduction of two grades in five (10%) patients, a reduction of one grade in 42 (84%) patients and no reduction of grade in three (6%) patients.
Goodman’s Quantitative scores of the two halves of the face had equal mean scores of 19.24 before treatment. After treatment, the mean score of PRP treated face was 7.08, with a 62.20% improvement in acne scars. The other half of the face had a mean score of 10.42, with 45.84% improvement of acne scars following treatment (P <0.00001).
Patient satisfaction evaluation on the water-treated side revealed excellent response in nine patients, good response in 30 patients, fair response in ten patients and poor response in one patient. The PRP-treated half of the face showed excellent response in three patients, good response in 12 patients, fair response in 31 patients and poor response in three patients (P <0.00001).
Dermal fillers
Five studies assessed the effects of dermal fillers, mainly in patients with rolling type scars. Two studies utilised poly-L-lactic acid (PLLA), one collagen, one polymethyl methacrylate (PMMA) and one hyaluronic acid (HA) (Table 6).
Table 6.
A synopsis of dermal filler studies.
| Authors | Publication year | Patient no. | Level of evidence | Indication | Dermal filler | Cosmetic outcome | Adverse effects |
|---|---|---|---|---|---|---|---|
| Beer et al. | 2007 | 16 | 2.d | Acne or varicella rolling and ice pick scars | Poly-L-lactic acid | 46.4% cumulative reduction in scar severity | None identified |
| Sage et al. | 2011 | 10 | 2.c | Various morphologic acne scar types | Collagen | 3.05 mean improvement (3 = minimal, 4 = moderate improvement) | Pain, erythema, swelling, discolouration, bruising and lumpiness |
| Karnik et al. | 2014 | 147 | 1.c | Rolling acne scars | PPMA | 84% of scars improved (based on the Physician Global Aesthetic Improvement Scale score) | Pain, tenderness and swelling |
| Sapra et al. | 2015 | 22 | 2.d | Rolling acne scars | Poly-L-lactic acid | 63.6% of patients achieved a much to excellent improvement (score of ≤2 using a 4-point scale) | Nodule formation, eczema and hyperpigmentation |
| Goodman et al. | 2016 | 5 | 2.d | Various morphologic acne scar types | Hyaluronic acid | Pre Tx mean score: 3.2; post Tx mean score: 2.6 (based on the quantitative global scarring grading system) | N/A |
Beer et al. treated 16 patients with severe scarring from acne or varicella using injectable PLLA fillers.35 They achieved a maximum cumulative scar severity reduction of 46.4% at the seventh treatment visit (P <0.0001).
In a multicenter, randomised, double-blinded, controlled trial, Karnik et al. assessed the effects of PMMA versus placebo for the treatment of atrophic rolling acne scars.36 Participants were randomised to receive either PMMA or saline injections. A total of 147 patients were included in the study with a total of 1288 scars. Scar severity was assessed using a proprietary Acne Scar Rating Scale (ASRS) four-point scale (1 = minimal scarring, 2 = mild, 3 = moderate, and 4 = severe). At six-month follow-up, 64% of PMMA-treated participants achieved a two-point improvement in the ASRS score for at least 50% of scars, compared with 33% in the control group (P = 0.0005). The overall proportion of scars that improved by at least two points was 50% for PMMA and 21% for the control. A one-point improvement in the ASRS score was achieved in 91% of PMMA-treated scars and in 76% for saline-treated scars. Using the Physician Global Aesthetic Improvement Scale score, 84% of PMMA-treated participants were found to have improved compared with 54% in the control group (P = 0.0003). A total of 84% of PMMA-treated participants were satisfied with treatment, compared with 52% from the control group.
In a different study, PLLA fillers were used to treat 22 participants with facial rolling scars.37 Results were recorded using a four-point scale and satisfactory response was considered a post-treatment score of ≤2. A satisfactory response was achieved in 63.6% of patients when assessed by physicians, 68.2% when assessed by blinded evaluators and 45.5% when assessed by the patients themselves. Of the patients, 54.5% graded their post-procedure satisfaction as very good or excellent.
Goodman treated five patients with atrophic acne scarring using HA fillers administered utilising a modified tower technique.38 Among all patients, the mean scar count dropped from 48.8 on the first injection to 41.8 two weeks later to 15.4 after two injection sessions. Fewer than 30% of the scars were still visible after these two injection sessions at one-month follow-up. Results were assessed using the quantitative global scarring grading system. Scars showed an improvement from a pre-treatment mean value of 3.2, to 3.0 after one treatment, to 2.6 one month after the second treatment. The degree of improvement according to patients was found to be +5.4, one month after two injection sessions, using a −3 to +10 scale. This value was also maintained at the three-month follow up (+5.5), indicating good to excellent improvement from a patient’s perspective.
Chemical peeling
A total of 12 studies were identified in this section that utilized multiple different peeling agents and treated patients with various morphological acne scars but predominantly of the ice pick type (Table 7).
Table 7.
A synopsis of chemical peel studies.
| Authors | Publication year | Patient no. | Level of evidence | Indication | Chemical peel | Cosmetic outcome | Adverse effects |
|---|---|---|---|---|---|---|---|
| Park et al. | 2007 | 11 | 2.d | Various morphologic acne scar types | Modified phenol peel (Exoderm) | Average improvement score was 2.73 (based on a 4-point scale) | Hyper and hypopigmentation, keloid and milia formation |
| Garg et al. | 2008 | 44 | 2.d | Ice pick, boxcar and rolling scars | 35% glycolic acid OR 20% salicylic–10% mandelic acid | Ice pick scars: 10.4% improvement with GA, 13.2% improvement with SPM; boxcar scars: 20.1% improvement with GA, 23.3% improvement with SPM; rolling scars: no improvement identified with either agent | Burning or stinging sensation, desquamation, dryness, photosensitivity and acne flaring |
| Bhardwaj et al. | 2010 | 10 | 2.d | Predominantly ice pick acne scarring | 100% TCA CROSS | 8 patients (80%) achieved excellent improvement; 2 patients (20%) achieved good improvement | Transient hypopigmentation, burning sensation, frosting, erythema and oedema |
| Sachdeva et al. | 2010 | 7 | 2.d | Predominantly ice pick acne scarring | 92% lactic acid | Significant improvement (>75% clearance): 1 patient
(14%); good improvement (51–75% clearance): 3 patients (42%); moderate improvement (26–50% clearance): 2 patients (28%); mild improvement (1–25% clearance): 1 patient (14%) |
Hyperpigmentation |
| Khunger et al. | 2011 | 30 | 2.d | Predominantly ice pick acne scarring | 100% TCA CROSS | 22 (73.3%) patients achieved excellent results (>70%
reduction of scarring); 6 (20%) patients good results
(51–70% reduction of scarring); 2 (6.7%) patients achieved average results (<30% reduction of scarring) |
Burning, frosting, erythema, oedema, hyper- and hypopigmentation |
| Ramadan et al. | 2011 | 20 | 2.d | Rolling acne scars | 100% TCA CROSS | Scar size improved by a mean of 0.08657 ± 0.090 cm2 | Erythema, hyper- and hypopigmentation |
| Leheta et al. | 2012 | 20 | 2.c | Various morphologic acne scar types | 60% oil phenol OR dermaroller and 20% TCA | 60% oil phenol: mean improvement of 75.12%; dermaroller and 20% TCA: mean improvement of 69.43% | Acneiform eruptions, erythema, hyperpigmentation, pain and swelling |
| Agarwal et al. | 2015 | 54 | 2.d | Various morphologic acne scar types | 70% TCA CROSS | 12 (22.6%) patients achieved excellent (>75%) improvement; 23 (43.4%) patients achieved good (51–75%) improvement | Hyperpigmentation, crusting |
| Chandrashekar et al. | 2015 | 35 | 2.d | Various morphologic acne scar types | Retinoic acid 0.025% and GA 12% | (Based on the quantitative global scarring grading system) | N/A |
| Puri et al. | 2015 | 50 | 2.d | Various morphologic acne scar types | Jessner’s peel and 20% TCA OR 20% TCA alone | Jessner’s peel and 20% TCA: mild improvement in 8%, moderate in 32%, and marked in 60%; TCA alone: mild improvement in 32%, moderate in 40%, and marked in 28% | Erythema, burning sensation, hyperpigmentation, pruritus, swelling and folliculitis |
| Dalpizzol et al. | 2016 | 15 | 2.d | Ice pick and boxcar-acne scars | 88% phenolic acid CROSS OR 90% TCA CROSS | Mean improvement of 6.9 points on both sides of the face (based on a 10-point scale) | Erythema, hyperpigmentation, hypochromia and scar widening |
| Kurokawa et al. | 2016 | 20 | 2.d | Various morphologic acne scar types | 20% glycolic acid and subsequent iontophoresis | Excellent results: 5 (25%) patients; good: 6 (30%) patients; fair: 4 (20%) patients; no improvement: 5 (25%) patients | Redness and irritation |
Park et al. treated 11 patients with post-acne scarring using a modified phenol deep peel known as Exoderm. Results were assessed using a four-point scale.39 Seven of 11 patients (64%) improved by 51% or more with an average improvement score of 2.73.
In a different study, 44 patients were treated with active acne or post-acne scarring.15 The patients were divided into two age- and sex-matched groups. Group A comprised 22 patients who received fortnightly 35% GA peels, and group B comprised 22 patients who received fortnightly 20% salicylic–10% mandelic acid peels (SPM). A total of six peeling sessions were conducted for each group.
Objective evaluation of treatment outcomes done by the treating physician revealed the following:
Ice pick scars: There was a 10.4% improvement in the appearance of ice pick scars with GA peels and a 13.2% improvement with SPMs (P = 0.3).
Boxcar scars: The change in boxcar scars from baseline was 20.1% with GA peels and 23.3% with SPMs (P = 0.02).
Rolling scars: There was no change in rolling scars with either of the two agents (P = 1.00 for both agents).
In yet another study, ten patients were treated using 100% with the TCA CROSS technique.40 The improvement was assessed using a four-point scale and results were interpreted as excellent if >70% reduction was observed, good if 50–70%, fair if 30–50% and poor if <30% improvement was observed.
After four applications of peeling, eight patients (80%) achieved excellent improvement and the remaining two (20%) achieved good improvement of scarring. The feedback received from patients was comparable to that measured by the physicians.
Sachdeva et al. assessed the effect of 92% lactic acid peels in seven patients with mainly ice pick scarring.41 Significant improvement (>75% clearance of lesions) occurred in one patient, good improvement (51–75% clearance) in three patients, moderate improvement (26–50% clearance) in two patients and mild improvement (1–25% clearance) in one patient.
In a study assessing the efficacy of 100% TCA CROSS, 30 patients with predominantly ice pick scarring were treated every two weeks for a total of four sessions.42
Improvement was considered excellent if >70% reduction of scars was observed, good if 51–70% improvement, fair if 30–50% improvement and poor if <30% improvement was seen. Twenty-two (73.3%) patients achieved excellent improvement, six (20%) patients showed good improvement and two (6.7%) showed average improvement.
Leheta et al. performed a randomised, controlled, single-blinded trial on 20 patients with atrophic post-acne scarring.43 Patients were randomly equally divided into two groups; group A underwent deep peeling using a non-hydro-alcoholic solution of 60% oil phenol with few drops of croton oil and group B underwent four sessions (six weeks apart) of dermaroller-induced percutaneous collagen induction combined with 20% TCA in the same session. The severity of lesions was scored according to the following scale: 3 points for deep, 2 points for shallow and 1 point for superficial scars. Scar improvement was graded with the following method: 0 = minimal improvement <25%, 1 = mild improvement 25–50%, 2 = moderate improvement 51–75%, 3 = significant improvement >75%.
Acne scarring improved in 100% of patients. The overall scar severity score improved by a mean of 75.12% (95% CI, 71.44–78.80) (P <0.001) in group A and a mean of 69.43% (95% CI, 60.01–78.85) (P <0.001) in group B. The difference in the degree of improvement was not statistically significant when comparing both groups. Regarding the global response, the degree of improvement was significant in ten patients (50%), moderate in eight (40%) and mild in two patients (10%). In group A, there was no significant difference in the degree of improvement in between the different types of scars after treatment. In group B, the highest degree of improvement was seen in rolling types scars. Ninety percent of patients reported subjective improvement of their acne scars, in the range of 50–75%.
Agarwal et al. treated 53 patients with multiple types of atrophic acne scars using 70% TCA using the CROSS technique, where TCA is focally applied to the base of scars with the use of a toothpick.44 Treatment effects were assessed using the following four-point scale: poor results = 0–25%, fair = 26–50%, good = 51–75%, and excellent = >75%. At three-month follow-up, physician assessment revealed that 35 patients (66%) had achieved >50% clinical improvement. Of them, 12 (22.6%) achieved excellent (>75%) improvement and 23 (43.4%) achieved good (51–75%) improvement. Patient self-assessment revealed that 35 patients (66%) perceived an >50% clinical improvement. Of them, six (11.3%) reported excellent improvement and 29 (54.7%) stated good improvement. None of the patients reported a poor response. Forty-three out of 53 patients (81.1%) were either satisfied (n = 30, 56.6%) or very satisfied (n = 13, 24.5%) with their treatment.
In a retrospective study of 35 patients, Chandrashekar et al. studied the efficacy of topical RA 0.025% and GA 12% combination.45 The acne scars were graded according to Goodman and Baron’s quantitative global scarring grading system at baseline and after 12 weeks of treatment. When the difference between the GSGS score was zero, the status was categorised as no improvement; when difference was 1–5 points, the improvement was categorised as mild; moderate improvement was when scar grades reduced by 6–10 points; good improvement was when scar grades decreased by 11–15 points; and very good improvement was when scar grades reduced by more than 15 points.
Of the 35 patients, three showed no improvement at the end of 12 weeks of follow-up, while 16 patients demonstrated a mild improvement in their scars. Thirteen patients had moderate improvement in their acne scars, two had good improvement and one patient demonstrated very good improvement.
Puri et al. performed a comparative study between Jessner’s peel and 20% TCA versus 20% TCA peel in isolation.46 Fifty patients were randomly divided into two groups of 25 patients each. Chemical peeling was done in both the groups. Group I underwent chemical peeling with Jessner’s peel and 20% TCA, and group II underwent treatment with 20% TCA peel alone. The improvement of the patients was categorised as follows: marked improvement if >70% response, moderate if 40–70% improvement and mild if <40% improvement. In group I, mild improvement of acne scars was seen in 8% cases, moderate improvement in 32% cases and marked improvement in 60% of patients. In group II, mild improvement was seen in 32% cases, moderate improvement in 40% cases and marked improvement was seen in 28% patients. This difference in improvement between the two groups was not statistically significant (P >0.05).
In a split-face study, Dalpizzol et al. compared the results of 88% phenolic acid CROSS with those of 90% TCA CROSS on 15 patients with ice pick and boxcar acne scars. The results were assessed using a 10-point scale.47
Physician assessment revealed a mean improvement of 6.9 points on both sides of the face (P <0.001). Patient self-assessment revealed that the mean improvement for the side treated with phenol was 6.8 points and for the side treated with TCA was 6.9 points, indicating no statistical difference (P >0.05) between the two.
Kurokawa et al. used a combination of chemical peeling with 20% GA, followed by iontophoresis to treat 31 patients with acne vulgaris and post-acne atrophic scarring.48 Treatments were performed three to four times at two-monthly intervals, at which point the effect of treatment was evaluated. Non-inflamed atrophic scars without erythema were evaluated in 20 cases. Excellent results were achieved in five patients, good in six, fair in four and no improvement was seen in five patients.
Discussion
Acne scarring is a common and persistent complication of acne vulgaris that affects a large proportion of the population. Despite its high prevalence, there is no single treatment modality that has been shown to be universally effective, posing a significant challenge for the treating physician.38 However, there are multiple methods for the treatment of acne scars available, each with both pros and cons. Selection of the appropriate treatment for each patient should depend on a number of factors such as: type of scars; efficacy; side effects; physician’s expertise; and patient’s expectations.21 For example, in chemical peels, considerable factor is the associated downtime, whereas in dermal fillers time of improvement persistency.
Reviewing outcomes by scar type, we note that rolling scars have the highest rates of treatment failure (10–15% with subcision in one study and 100% with chemical peeling in another). Several other studies, however, reported significant improvement in the appearance of rolling scars, such as PMMA (which lead to improvement in appearance in 84% of scars), particularly following treatment with subcision. Interestingly, as a result of the safety and efficacy presented in the above study, PMMA is now FDA approved for the treatment of acne scarring and to date is the only such filler to have this approval in the management of acne scarring.
Ice pick scars seem to be particularly responsive to treatment with chemical peels, especially when treated with TCA CROSS, suggesting that there is still an important role in the otherwise declining use of this technique.
Looking at the different treatment modalities, the least significant results were achieved in the one study that utilised MDA. There, despite eight treatment sessions, no patients achieved very good improvement in scar appearance and 45.4% did not achieve any improvement at all. The most impressive results were seen following application of chemical peels, with excellent response rates often achieved in >70% of patients. Combination treatments are shown to have a favourable outcome too. When cryoroller treatment was used in addition to subcision, response rates went up by 17%, compared with subcision used in isolation. In addition, particularly effective seem to be the combination treatments with microneedling/GA peeling and microneedling/PRP.
The papers reviewed above are very variable with regards to their sample size, study design and patient demographics. In addition, different scar grading scales have been used by different studies, and even when the same scale is utilised, serial measurements are influenced by subjective bias and can be inconsistent even when performed by the same person. Such heterogeneity, in addition to operator-dependent variation in the delivery of treatment, makes further comparison of outcomes difficult to perform.
Conclusions
We can conclude that post-acne scarring is a very common and challenging condition with no easy and definitive solution. Subcision, microneedling, MDA, dermal fillers and chemical peels have all been used with varying degrees of efficacy but an overall positive outcome. Each technique has pros and cons. Some are suited for specific types of scars, others need to be applied repeatedly, and all carry a potential risk of adverse reactions.
Despite the multitude of information provided above, it is hard to make further judgements about each technique for a number of different reasons: few studies examine head-to-head success rates; study designs are variable; most studies have only a small numbers of participants; there is significant measurement bias due to the difficulty of achieving consistent objective measurements of scar severity; and long-term follow-up data are lacking.
Our work only encompasses articles that have been published over the last ten years. Therefore, the conclusions presented above could be skewed due to the potential exclusion of existing studies with significant evidence for or against certain modalities.
In part 2 of this review, we will discuss the treatment of post-acne scarring with energy-based devices, including indications, methods of application, therapeutic outcomes and adverse reactions.
Footnotes
Declaration of conflicting interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1. Gozali MV, Zhou B. Effective treatments of atrophic acne scars. J Clin Aesthet Dermatol 2015; 8: 33–40. [PMC free article] [PubMed] [Google Scholar]
- 2. Fabbrocini G, Annunziata MC, D’Arco V, et al. Acne scars: pathogenesis, classification and treatment. Dermatol Res Pract 2010; 2010: 893080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Cunliffe WJ, Gould DJ. Prevalence of facial acne vulgaris in late adolescence and in adults. Br Med J 1979; 28: 1109–1110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Jacob CI, Dover JS, Kaminer MS. Acne scarring: a classification system and review of treatment options. J Am Acad Dermatol 2001; 45: 109–117. [DOI] [PubMed] [Google Scholar]
- 5. Sánchez Viera M. Management of acne scars: fulfilling our duty of care for patients. Br J Dermatol 2015; 172 (Suppl. 1): 47–51. [DOI] [PubMed] [Google Scholar]
- 6. Simmons BJ, Griffith RD, Falto-Aizpurua LA, et al. Use of radiofrequency in cosmetic dermatology: focus on nonablative treatment of acne scars. Clin Cosmet Investig Dermatol 2014; 12; 335–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Goodman GJ, Baron JA. Postacne scarring: a qualitative global scarring grading system. Dermatol Surg 2006; 32: 1458–1466. [DOI] [PubMed] [Google Scholar]
- 8. Goodman GJ, Baron JA. Postacne scarring—a quantitative global scarring grading system. J Cosmet Dermatol 2006; 5: 48–52. [DOI] [PubMed] [Google Scholar]
- 9. Fearmonti R, Bond J, Erdmann D, et al. A review of scar scales and scar measuring devices. Eplasty 2010; 10: e43. [PMC free article] [PubMed] [Google Scholar]
- 10. Aalami Harandi S, Balighi K, et al. Subcision-suction method: a new successful combination therapy in treatment of atrophic acne scars and other depressed scars. J Eur Acad Dermatol Venereol 2011; 25: 92–99. [DOI] [PubMed] [Google Scholar]
- 11. El-Domyati M, Hosam W, Abdel-Azim E, et al. Microdermabrasion: a clinical, histometric, and histopathologic study. J Cosmet Dermatol 2016; 15: 503–513. [DOI] [PubMed] [Google Scholar]
- 12. Asif M, Kanodia S, Singh K. Combined autologous platelet-rich plasma with microneedling verses microneedling with distilled water in the treatment of atrophic acne scars: a concurrent split-face study. J Cosmet Dermatol 2016; 15: 434–443. [DOI] [PubMed] [Google Scholar]
- 13. Narins RS, Bowman PH. Injectable skin fillers. Clin Plast Surg 2005; 32: 151–162. [DOI] [PubMed] [Google Scholar]
- 14. Alhede M, Er Ö, Eickhardt S, et al. Bacterial biofilm formation and treatment in soft tissue fillers. Pathog Dis 2014; 70: 339–346. [DOI] [PubMed] [Google Scholar]
- 15. Garg VK, Sinha S, Sarkar R. Glycolic acid peels versus salicylic-mandelic acid peels in active acne vulgaris and post-acne scarring and hyperpigmentation: a comparative study. Dermatol Surg 2009; 35: 59–65. [DOI] [PubMed] [Google Scholar]
- 16. Alhede M, Er Ö, Eickhardt S, et al. Bacterial biofilm formation and treatment in soft tissue fillers. Pathog Dis 2014; 70: 339–346. [DOI] [PubMed] [Google Scholar]
- 17. Lee JC, Daniels MA, Roth MZ. Mesotherapy, microneedling, and chemical peels. Clin Plast Surg 2016; 43: 583–595. [DOI] [PubMed] [Google Scholar]
- 18. Balighi K, Robati RM, Moslehi H, et al. Subcision in acne scar with and without subdermal implant: a clinical trial. J Eur Acad Dermatol Venereol 2008; 22: 707–711. [DOI] [PubMed] [Google Scholar]
- 19. Sage RJ, Lopiccolo MC, Liu A, et al. Subcuticular incision versus naturally sourced porcine collagen filler for acne scars: a randomized split-face comparison. Dermatol Surg 2011; 37: 426–431. [DOI] [PubMed] [Google Scholar]
- 20. Ramadan SA, El-Komy MH, Bassiouny DA, et al. Subcision versus 100% trichloroacetic acid in the treatment of rolling acne scars. Dermatol Surg 2011; 37: 626–633. [DOI] [PubMed] [Google Scholar]
- 21. Harandi SA, Balighi K, Lajevardi V, et al. Subcision-suction method: a new successful combination therapy in treatment of atrophic acne scars and other depressed scars. J Eur Acad Dermatol Venereol 2011; 25: 92–99. [DOI] [PubMed] [Google Scholar]
- 22. Al-Dhalimi MA, Arnoos AA. Subcision for treatment of rolling acne scars in Iraqi patients: a clinical study. J Cosmet Dermatol 2012; 11: 144–150. [DOI] [PubMed] [Google Scholar]
- 23. Gadkari R, Nayak C. A split-face comparative study to evaluate efficacy of combined subcision and dermaroller against combined subcision and cryoroller in treatment of acne scars. J Cosmet Dermatol 2014; 13: 38–43. [DOI] [PubMed] [Google Scholar]
- 24. Garg S, Baveja S. Combination therapy in the management of atrophic acne scars. J Cutan Aesthet Surg 2014; 7: 18–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kaur J, Kalsy J. Subcision plus 50% trichloroacetic acid chemical reconstruction of skin scars in the management of atrophic acne scars: A cost-effective therapy. Indian Dermatol Online J 2014; 5: 95–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Nilforoushzadeh M, Lotfi E, Nickkholgh E, et al. Can subcision with the cannula be an acceptable alternative method in treatment of acne scars? Med Arch 2015; 69: 384–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Barikbin B, Akbari Z, Yousefi M, et al. Blunt blade subcision: an evolution in the treatment of atrophic acne scars. Dermatol Surg 2017; 43: S57–S63. [DOI] [PubMed] [Google Scholar]
- 28. Fabbrocini G, Fardella N, Monfrecola A, et al. Acne scarring treatment using skin needling. Clin Exp Dermatol 2009; 34: 874–879. [DOI] [PubMed] [Google Scholar]
- 29. Sharad J. Combination of microneedling and glycolic acid peels for the treatment of acne scars in dark skin. J Cosmet Dermatol 2011; 10: 317–323. [DOI] [PubMed] [Google Scholar]
- 30. Alam M, Han S, Pongprutthipan M, et al. Efficacy of a needling device for the treatment of acne scars: a randomized clinical trial. JAMA Dermatol 2014; 150: 844–849. [DOI] [PubMed] [Google Scholar]
- 31. Chawla S. Split face comparative study of microneedling with PRP versus microneedling with vitamin C in treating atrophic post acne scars. J Cutan Aesthet Surg 2014; 7: 209–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Dogra S, Yadav S, Sarangal R. Microneedling for acne scars in Asian skin type: an effective low cost treatment modality. J Cosmet Dermatol 2014; 13: 180–187. [DOI] [PubMed] [Google Scholar]
- 33. Nofal E, Helmy A, Nofal A, et al. Platelet-rich plasma versus CROSS technique with 100% trichloroacetic acid versus combined skin needling and platelet rich plasma in the treatment of atrophic acne scars: a comparative study. Dermatol Surg 2014; 40: 864–873. [DOI] [PubMed] [Google Scholar]
- 34. El-Domyati M, Barakat M, Awad S, et al. Microneedling therapy for atrophic acne scars: an objective evaluation. J Clin Aesthet Dermatol 2015; 8: 36–42. [PMC free article] [PubMed] [Google Scholar]
- 35. Beer K. A single-center, open-label study on the use of injectable poly-L-lactic acid for the treatment of moderate to severe scarring from acne or varicella. Dermatol Surg 2007; 33 (Suppl. 2): S159–167. [DOI] [PubMed] [Google Scholar]
- 36. Karnik J, Baumann L, Bruce S, et al. A double-blind, randomized, multicenter, controlled trial of suspended polymethylmethacrylate microspheres for the correction of atrophic facial acne scars. J Am Acad Dermatol 2014; 71: 77–83. [DOI] [PubMed] [Google Scholar]
- 37. Sapra S, Stewart JA, Mraud K, et al. A Canadian study of the use of poly-L-lactic acid dermal implant for the treatment of hill and valley acne scarring. Dermatol Surg 2015; 41: 587–594. [DOI] [PubMed] [Google Scholar]
- 38. Goodman GJ, Van Den Broek A. The modified tower vertical filler technique for the treatment of post-acne scarring. Australas J Dermatol 2016; 57: 19–23. [DOI] [PubMed] [Google Scholar]
- 39. Park JH, Choi YD, Kim SW, et al. Effectiveness of modified phenol peel (Exoderm) on facial wrinkles, acne scars and other skin problems of Asian patients. J Dermatol 2007; 34: 17–24. [DOI] [PubMed] [Google Scholar]
- 40. Bhardwaj D, Khunger N. An assessment of the efficacy and safety of CROSS technique with 100% TCA in the management of ice pick acne scars. J Cutan Aesthet Surg 2010; 3: 93–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Sachdeva S. Lactic acid peeling in superficial acne scarring in Indian skin. J Cosmet Dermatol 2010; 9: 246–248. [DOI] [PubMed] [Google Scholar]
- 42. Khunger N, Bhardwaj D, Khunger M. Evaluation of CROSS technique with 100% TCA in the management of ice pick acne scars in darker skin types. J Cosmet Dermatol 2011; 10: 51–57. [DOI] [PubMed] [Google Scholar]
- 43. Leheta TM, Abdel Hay RM, El Garem YF. Deep peeling using phenol versus percutaneous collagen induction combined with trichloroacetic acid 20% in atrophic post-acne scars; a randomized controlled trial. J Dermatolog Treat 2014; 25: 130–136. [DOI] [PubMed] [Google Scholar]
- 44. Agarwal N, Gupta LK, Khare AK, et al. Therapeutic response of 70% trichloroacetic acid CROSS in atrophic acne scars. Dermatol Surg 2015; 41: 597–604. [DOI] [PubMed] [Google Scholar]
- 45. Chandrashekar BS, Ashwini KR, Vasanth V, et al. Retinoic acid and glycolic acid combination in the treatment of acne scars. Indian Dermatol Online J 2015; 6: 84–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Puri N. Efficacy of modified Jessner’s peel and 20% TCA versus 20% TCA peel alone for the treatment of acne scars. J Cutan Aesthet Surg 2015; 8: 42–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Dalpizzol M, Weber MB, Mattiazzi AP, et al. Comparative study of the use of trichloroacetic acid and phenolic acid in the treatment of atrophic-type acne scars. Dermatol Surg 2016; 42: 377–383. [DOI] [PubMed] [Google Scholar]
- 48. Kurokawa I, Oiso N, Kawada A. Adjuvant alternative treatment with chemical peeling and subsequent iontophoresis for postinflammatory hyperpigmentation, erosion with inflamed red papules and non-inflamed atrophic scars in acne vulgaris. J Dermatol 2016. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 49. Jacob CI, Dover JS, Kaminer MS. Acne scarring: a classification system and review of treatment options. J Am Acad Dermatol 2001; 45: 109–117. [DOI] [PubMed] [Google Scholar]
How to cite this article
- Kravvas G, Al-Niaimi F. A systematic review of treatments for acne scarring. Part 1: Non-energy-based techniques. Scars, Burns & Healing, Volume 3, 2017. DOI: 10.1177/2059513117695312. [DOI] [PMC free article] [PubMed] [Google Scholar]


