Abstract
Laparoscopic Roux-en-Y gastric bypass has become the most common obesity surgery procedure worldwide over the last two decades. Many patients undergoing the procedure are women of reproductive age. This carries a risk for developing gastric bypass-related complications during pregnancy. One of the potentially serious risks is an internal hernia. We present a patient in the third trimester of pregnancy with an internal hernia following a laparoscopic Roux-en-Y gastric bypass for morbid obesity. We discuss the importance of computed tomography (CT) in the diagnosis of an internal hernia and review key CT findings including compression of the superior mesenteric vein, which proved to be crucial in diagnosing the internal hernia in this patient.
Keywords: Gastric bypass, Roux-en-Y gastric bypass, internal hernia, pregnancy, SMV compression, SMV beaking sign, swirl sign, CT scan
CASE REPORT
A 37-year-old woman (gravida 3, para 3) with a 31-week, four-day pregnancy presented to the hospital with severe abdominal pain. She had undergone an antecolic, antegastric laparoscopic Roux-en-Y gastric bypass (LRYGB) 7 years before admission. This was her first pregnancy after LRYGB. She had undergone surgery for an internal hernia (IH) 11 months before her current admission. Her past history also included an appendectomy and tubal ligation. Her current pregnancy was the result of in vitro fertilization.
Since the last IH operation, she had recurrent epigastric pain. She presented to the hospital at the 15th and 26th weeks of pregnancy with abdominal pain, which was attributed to constipation and treated medically with a positive outcome. At those times, she did not undergo any radiological examinations.
Currently, she presented to the emergency department with acute, diffuse epigastric abdominal pain a few hours in duration, which was not related to uterine contractions. This episode was accompanied by nausea without vomiting. Symptoms did not decline 30 minutes after morphine administration. The patient had passed the last normal stool on the morning of presentation. She stated that she had not passed gas in the last two hours.
Physical examination revealed tachypnea with normal blood pressure and pulse. The patient was afebrile. The abdominal exam showed a gravid uterus and soft abdomen with diffuse tenderness in the epigastrium and the right and left hypochondric and umbilical regions. Bowel sounds were decreased. The obstetrician on duty was consulted. The fetal heart rate and movements were normal. Blood chemistry, complete blood count, amylase, lipase, and liver function tests were in the normal range. Lactate levels were slightly elevated to 1.4 mmol/L [reference range 0.4–1.3 mmol/L].
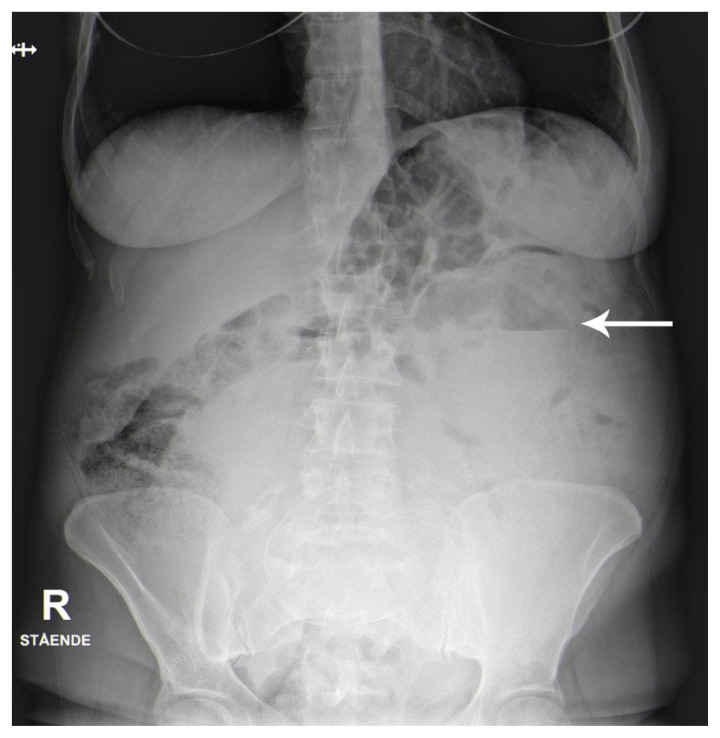
An upright abdominal radiograph was obtained (Fig. 1) on the suspicion of a small-bowel obstruction (SBO). Imaging showed slightly dilated loops of small bowel in the epigastric region with few air-fluid levels. The findings were suggestive of ileus but non-specific.
Figure 1.
37-year-old pregnant woman with an internal hernia.
Findings: Upright abdominal radiograph shows slightly dilated loops of the small bowel in the epigastric region with few air-fluid levels (arrow). The gravid uterus can be seen.
The decision was made to perform a CT examination of the abdomen and pelvis with intravenous contrast. Magnetic resonance imaging (MRI) was not available in the emergency setting and was not considered. Oral contrast was not given to avoid delaying the examination and because of severe nausea.
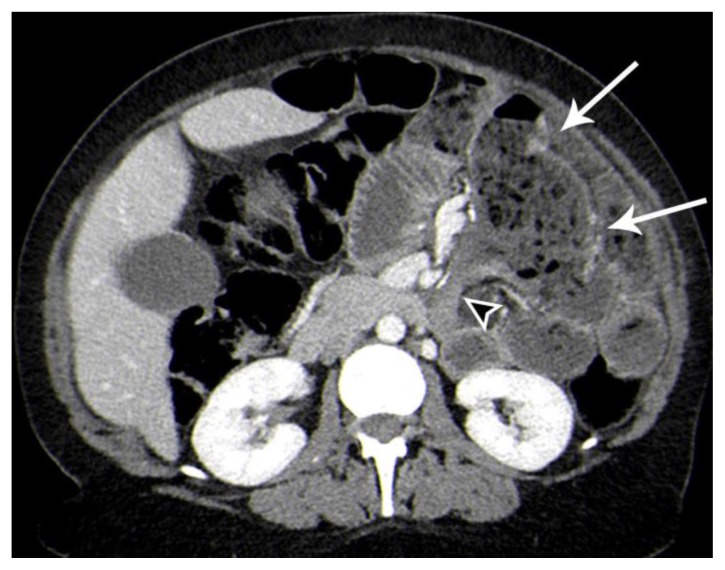
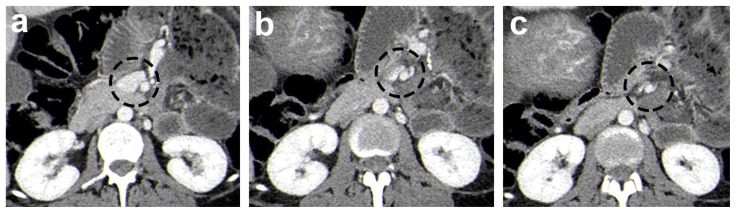
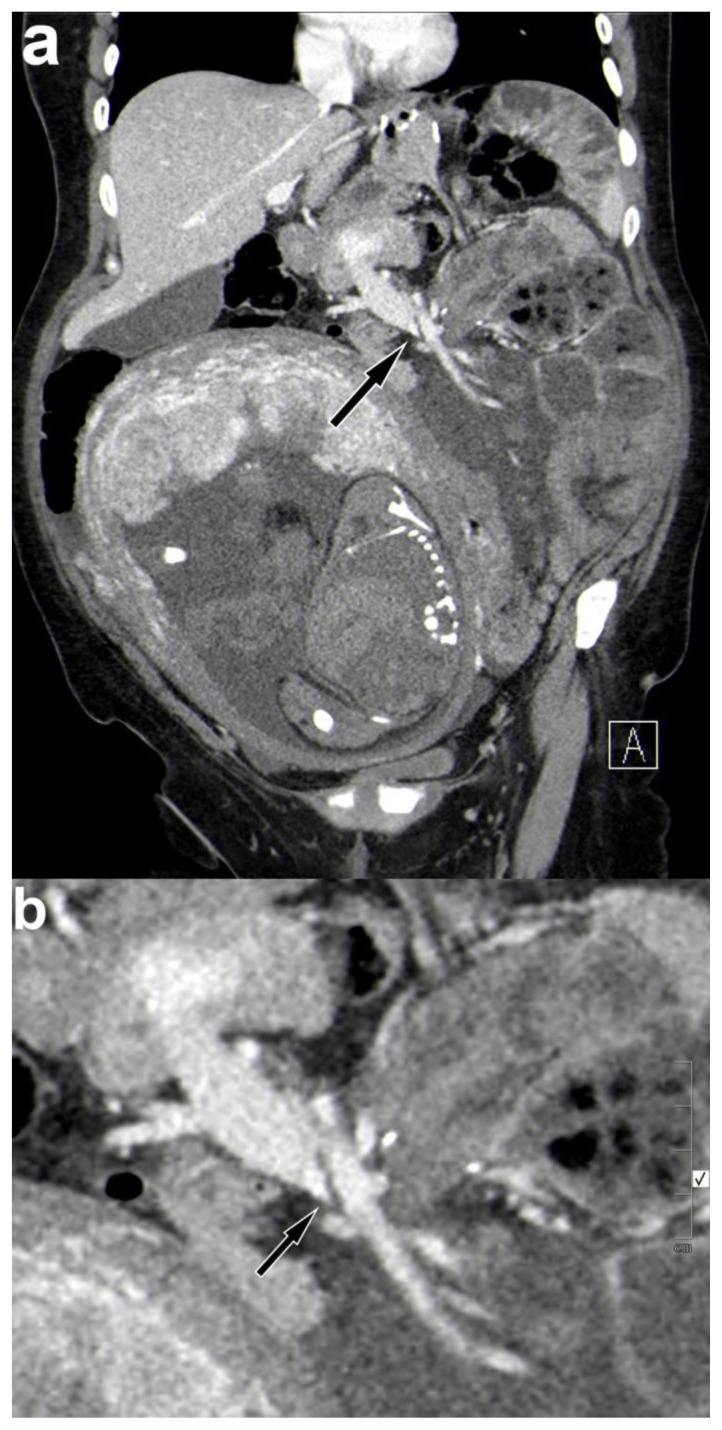
The CT scan confirmed dilated small bowel loops, up to 45 mm, in the left upper abdominal quadrant combined with the small-bowel feces sign (Fig. 2). There was an abrupt small bowel caliber change and obstruction adjacent to the level of jejuno-jejunal anastomosis (Fig. 2). At the same level, there was a “cutoff” of the superior mesenteric vein (SMV) (Fig. 3, Fig. 4). In addition, the images showed engorgement of the mesenteric veins with associated mesenteric edema (Fig. 5), most likely due to the obstruction of the SMV. There was also a small amount of free intraperitoneal fluid. The findings were suggestive of an internal herniation. There was preserved contrast enhancement in the intestinal wall. The distal ileum was collapsed. No free air was identified. The solid organs were unremarkable.
Figure 2.
37-year-old pregnant woman with a small-bowel obstruction secondary to an internal hernia.
Findings: Axial contrast-enhanced CT image of the abdomen in the portal venous phase demonstrates dilated small bowel loops in the left upper abdominal quadrant combined with a small bowel feces sign (arrows). There is an abrupt small bowel caliber change and obstruction adjacent to the level of jejuno-jejunal anastomosis (arrow head).
Technique: Axial CT (Siemen’s SOMATOM Definition AS 128-slice), 388 mAs, 100 kV, 3 mm slice thickness, 120 ml Omnipaque, DLP 745.5 mGycm
Figure 3.
37-year-old pregnant woman with an internal hernia.
Findings: Axial contrast-enhanced CT series (a, b, c) of the abdomen in the portal venous phase following the course of the superior mesenteric vein craniocaudally. Slices demonstrate the gradual compression of the superior mesenteric vein (black dashed circles), with complete obstruction of the SMV on the last slice.
Technique: Axial CT (Siemen’s SOMATOM Definition AS 128-slice), 388 mAs, 100 kV, 3 mm slice thickness, 120 ml Omnipaque, DLP 745.5 mGycm
Figure 4.
37-year-old pregnant woman with an internal hernia.
Findings: Coronal reconstructed contrast-enhanced CT images (a) of the abdomen in the portal venous phase demonstrate the compression of the main stem of the superior mesenteric vein (arrow), also described in the literature as the SMV "beaking" sign (b magnified).
Technique: Coronal reconstructed CT (Siemen’s SOMATOM Definition AS 128-slice), 388 mAs, 100 kV, 3 mm slice thickness, 120 ml Omnipaque, DLP 745.5 mGycm
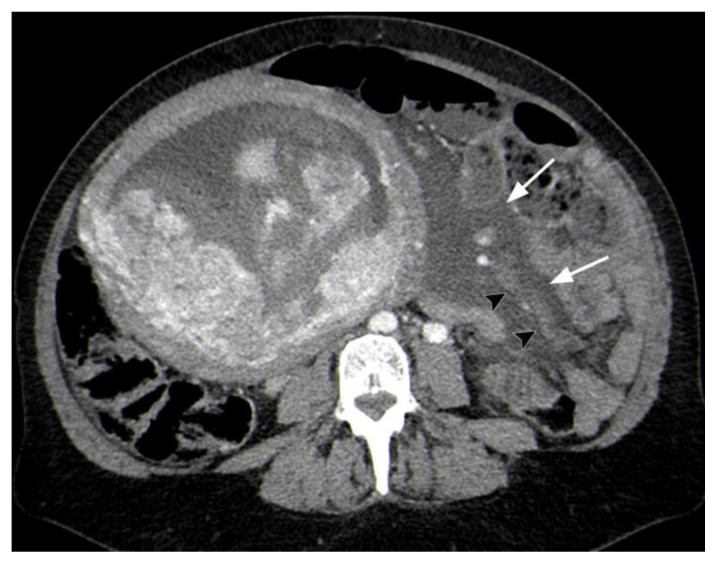
Figure 5.
37-year-old pregnant woman with an internal hernia.
Findings: Axial contrast-enhanced CT image of the abdomen in the portal venous phase demonstrates the engorgement of the mesenteric veins (arrow heads), most likely due to the obstruction of the superior mesenteric vein. Note the increase in the density of mesenteric fat due to mesenteric edema and free intraperitoneal fluid (white arrows).
Technique: Axial CT (Siemen’s SOMATOM Definition AS 128-slice), 388 mAs, 100 kV, 3 mm slice thickness, 120 ml Omnipaque, DLP 745.5 mGycm
The patient was transferred to the operating room. Laparoscopy showed an IH at the mesenteric defect at the jejunojejunostomy with a herniated common channel and volvulus of the anastomosis. Most of the IH was gently reduced, but a part of the jejuno-jejunal anastomosis was still twisted and adhered to the posterior abdominal wall. Due to limited space for maneuvering a median laparotomy was performed, which allowed detorsion of the jejuno-jejunal anastomosis and complete reduction of the hernia. The small bowel appeared viable after the reduction. The defect at the jejuno-jejunal anastomosis was closed using non-absorbable sutures. The patient was discharged seven days later and completed her pregnancy without complications.
The amount of radiation received by the fetus (fetal dose) during the CT scan and abdominal radiograph was estimated. Based on the average mA value, the fetal dose was 27 mGy during the CT scan. Based on the maximum mA value, the calculated fetal dose was 34 mGy. In addition to the previously calculated fetal dose, the abdominal radiograph added a fetal dose of 1.4 mGy.
DISCUSSION
Etiology & Demographics
Obesity is a problem that affects millions of people worldwide and is the cause of serious morbidity [1,2]. Since its introduction in 1994, LRYGB has become the most frequently performed procedure for the treatment of morbid obesity worldwide [2,3,4,5,6,7]. As the majority (70–80 %) of patients undergoing bariatric surgery are females with the mean age of approximately 40 +/− 10 years, many are of childbearing age [2,6,8,9].
Weight loss in obese women is associated with increased fertility and pregnancy rates [10,11]. In general, pregnancy in women with previous bariatric surgery is considered safe [2]. Nevertheless, it has been recommended that pregnancy should be delayed 12–24 months post-operatively, mainly to prevent undue fetal development and spontaneous abortion due to maternal malnutrition after gastric bypass surgery [6,11].
Although the laparoscopic Roux-en-Y procedure has been shown to reduce weight, and thus reduce the incidence of diseases associated with obesity, it raises the risk of developing gastric bypass-related complications. One of the potentially most serious risks is an IH, which can result in bowel obstruction and intestinal ischemia. The incidence range reported in the literature is 0–6.9 % [12].
It is well known that the location of the IH depends on the Roux-en-Y gastric bypass (RYGB) technique [13]. After antecolic, antegastric LRYGB, which is currently the preferred approach [8], IH can occur at the mesenteric defect at the jejunojejunostomy and the Petersen’s space (open space between the mesentery of the alimentary (Roux) limb and the transverse colon) [14].
IHs are described in the literature as the most common late complication (> 30 days post-operatively) of LRYGB and thus the most common cause of bowel obstruction after the procedure, accounting for 42 % of cases [15,16,17]. IHs typically occur after major weight loss, which results in reduced intraperitoneal fat and leads to larger mesenteric defects [18]. It can appear at any time, but often presents months or years after surgery [6,14,17,18]. It is suggested that pregnancy can predispose individuals to IH formation as a result of anatomic changes. The enlargement of the uterus and increased abdominal pressure combined with weight loss due to RYGB may lead to displacement of the small intestine and internal herniation [2,6,14]. Several cases of internal herniation during pregnancy have been reported, and maternal and fetal deaths have been described [6,11].
Clinical & Imaging Findings
The clinical diagnosis in patients with an IH is known to be challenging because symptoms are non-specific and associated with diverse differential diagnoses. In addition, a substantial number of patients readmitted after LRYGB suffer from unexplained “nonsurgical” abdominal pain [15]. The diagnosis of abdominal pain in pregnancy is even more difficult, and any delay in diagnosis can have severe consequences for both the fetus and the mother.
Imaging the pregnant patient is often a challenge due to concerns regarding radiation exposure and the use of intravenous contrast, but CT is still the modality of choice in such cases [11,13]. Indications for CT scanning in pregnant patients should always be considered on an individual basis with consideration of the risks versus benefits for any given clinical scenario. A CT scan should not be withheld from a pregnant patient when it is deemed necessary and may help identify the underlying maternal pathologic condition. It can show some classical features associated with IHs, detect small-bowel obstruction and guide the surgical approach when intervention is needed. Further complications of IHs, such as bowel infarction or perforation, can also be detected.
Radiation exposure from a CT scan is usually at a dose much lower than the exposure associated with fetal harm. The risk of fetal effects is negligible at doses of less than 50 mGy [19,20,21]. In our case, the fetal dose was far below this level.
When an IH is suspected, the use of intravenous contrast is crucial for the detection of several CT features that are important to evaluate, such as mesenteric vasculature and bowel viability. The administration of intravenous contrast enables us to assess bowel wall enhancement. The lack of bowel wall enhancement combined with gas in the intestinal wall can indicate bowel wall necrosis. Intravenous iodinated contrast material is generally thought to be safe during pregnancy [20,21].
Many CT signs of an IH have been described in the literature. These include the swirled appearance of mesenteric fat or vessels at the root of the mesentery (the swirl sign), the mushroom sign, the hurricane sign, small-bowel obstruction, clustered loops, small bowel behind the superior mesenteric artery, right-sided anastomosis, and compression of the main stem of the SMV, also described in the literature as the SMV “beaking” sign [7,22,23]. Since antecolic procedures are preferred today and many of these findings relate to descriptions of retrocolic procedures, they are of limited value [7].
The SMV compression and the mesenteric swirl sign have been described as the best indicators for the diagnosis of an IH [7,23]. These two signs may coincide in some patients with an IH. However, in our patient the SMV compression was the only sign. In addition we could also detect small-bowel obstruction and clustered loops, but these signs are, as mentioned before, less specific. The dilation of the small bowel can support the diagnosis, as in the case of our patient. However, many patients with an IH present without small bowel dilation [7].
Additional findings in our patient were severe mesenteric edema and a small amount of ascites. As suggested by Maier et al., mesenteric edema and ascites, although nonspecific, can be relevant in evaluating the CT scans of patients with a suspected IH [7].
The utility of MRI was not considered in our case because it was not available on an emergency basis in our institution. As reported by Rosenkratz at el., the MRI findings of an IH can match some CT signs, such as clustered loops, dilated and displaced bowel loops, or mesenteric edema [24]. These signs are, however, as previously discussed, less specific and can be challenging to interpret. The advantage of MRI in pregnant patients is the lack of ionizing radiation. However, the potential risk of using gadolinium-based contrast media in pregnant patients is a limitation in evaluating signs of an IH. The most suggestive findings of IHs involve changes in the mesenteric vasculature (SMV compression and mesenteric swirl sign), which cannot be optimally assessed by unenhanced MRI.
Treatment & Prognosis
An IH is a potentially fatal complication and should be managed operatively. A delay in diagnosis and treatment may lead to obstruction, bowel infarction, perforation, and death. As internal herniation is the most common late complication, this should be ruled out in all patients with previous LRYGB and abdominal pain. The prognosis depends on the development of further complications, including bowel infarction and perforation. Cases of a transient IH that reduces itself spontaneously are also well known in the literature, but keeping in mind the potential risk, the threshold in performing a laparoscopy should be very low [12].
Differential Diagnosis
After LRYGB, the differential diagnosis of an IH is based on excluding other causes of small-bowel obstruction [17]. There is some degree of overlap between the findings of IHs and adhesions. In addition, obstructions after LRYGB may be secondary to anastomotic strictures, incisional hernia, and occasionally intussusceptions or bezoars [4,17]. CT is the modality of choice in the differential diagnosis of an IH (Table 2).
Table 2.
Differential diagnosis table for an internal hernia based on causes of small-bowel obstruction after a laparoscopic Roux-en-Y gastric bypass.
| X-ray | US | CT | MRI | |
|---|---|---|---|---|
| Internal hernia | -Non-specific -When small bowel obstruction (SBO) is present- dilated loops of small bowel with air-fluid levels |
-Of limited value | -Compression of the main stem of the superior mesenteric vein (SMV “beaking” sign) -Swirled appearance of mesenteric fat or vessels at the root of the mesentery (the swirl sign) -SBO and mesenteric edema can be present |
-Not routinely used -T2-weighted fast imaging techniques: can match some less specific CT signs, such as clustered loops, dilated and displaced bowel loops, or mesenteric edema |
| Adhesions | -Non-specific; dilated bowel loops proximal to the place of obstruction and air-fluid levels -Absence of gas in the distal collapsed bowel |
-Of limited value | -An abrupt transition point from dilated to collapsed bowel segments | -Not routinely used in an emergency situation |
| Anastomotic strictures | -Radiography with contrast material-delay in the passage of contrast through the anastomosis -Dilated bowel loops with air-fluid levels proximal to obstruction |
-Of limited value | -Narrowing at the level of anastomosis with bowel obstruction proximal to it | -Not routinely used |
| Incisional hernia | -Dilated loops of bowel with air-fluid levels proximal to the place of obstruction -Absence of gas in the distal collapsed bowel |
-Defect in the abdominal wall with the herniation of a bowel loop | -Herniation of a bowel loop through a defect in the abdominal wall -Dilated bowel loops proximal to the hernia and collapsed or normal bowel distal to the obstruction |
-Not routinely used |
| Intussusception | -May demonstrate a soft tissue mass -Dilated obstructed bowel loops with air-fluid levels |
-Modality of choice in the pediatric population -Can demonstrate the characteristic appearance of the target sign |
-Characteristic appearance with bowel-within-bowel configuration | - T2-weighted fast imaging techniques: bowel within-bowel configuration |
| Bezoar | -Usually not possible to identify a bezoar on radiographs alone -Dilated obstructed bowel loops with air-fluid levels in patients with SBO |
-Hardly visible due to the accumulated gas in the bowels affecting the ultrasonic sound -Intraluminal mass with a hyperechoic arc-like surface casting a posterior acoustic shadow |
-Obstructive inhomogeneous mass with regular margins mottled with gas bubbles -Dilated bowel proximal to the mass |
- T1- and T2-weighted fast imaging techniques: ovoid mass containing mottled low signal intensities, which represent air bubbles |
Adhesions
Abdominal adhesions are less common after LRYGB than after an open operation, with reported incidences of less than 1% [17]. Furthermore, it has been suggested that the laparoscopic approach is associated with a higher incidence of IH formation, likely due to reduced postoperative adhesions and thus more bowel mobility [12,17]. Adhesions are in most cases invisible on CT, but CT helps in the detection of adhesion-related complications, such as bowel obstruction or bowel ischemia. The same complications can occur in patients with an IH. An abrupt transition point from dilated to collapsed bowel segments may be the only finding depicted on CT in patients with adhesions. Radiography, although non-specific may demonstrate dilated bowel loops with air-fluid levels proximal to the place of obstruction and the absence of gas in the distal collapsed bowel.
Ultrasound and cine-MRI are imaging methods used for the detection of adhesions in patients with chronic abdominal pain but are not used in emergency situations. Transabdominal ultrasonography demonstrating reduced visceral sliding is useful only for the diagnosis of adhesions to the abdominal wall, but not those between the bowels [25].
Anastomotic strictures
Stricture at the jejunojejunal anastomosis with secondary obstruction of large bowel segments is a rare complication, occurring in 0.04–0.7 % of patients after LRYGB depending on the technique of anastomotic construction [17]. Narrowing at the gastrojejunal anastomosis is a relatively common complication in the immediate postoperative period and may be secondary to anastomotic edema [4,9]. CT can show narrowing at the level of anastomosis with bowel obstruction proximal to the anastomosis. MRI can also identify gas- and fluid-filled bowel loops proximal to obstruction, but MRI is not routinely used in patients with suspected anastomotic strictures. Plain radiographs may present dilated bowel loops with air-fluid levels proximal to the obstruction. Radiography with contrast material may show a delay in the passage of contrast through the anastomosis.
Incisional hernia
An incisional hernia through the trocar site is another rare cause of SBO after LRYGB with reported incidence in the literature of 0–0.5 % [17]. A trocar site hernia associated with SBO often occurs early, within 30 days post-operatively [17,26]. CT can show the herniation of a bowel loop through a defect in the abdominal wall, dilated bowel loops proximal to the hernia, and collapsed or normal bowel distal to the obstruction. CT signs indicating hernia incarceration include free fluid within the hernial sac, bowel wall thickening, or dilation of the herniated bowel loop. An abdominal wall ultrasound may be an alternative to CT for detecting incisional hernias. Sonographic signs of hernia incarceration include free fluid in the hernial sac, bowel wall thickening within the hernia, and fluid in the herniated bowel loop. An abdominal X-ray may demonstrate dilated loops of bowel with air-fluid levels proximal to the place of obstruction and the absence of gas in the distal collapsed bowel.
Intussusception
Intussusception is a rarely reported complication after LRYGB [17,27]. It can be diagnosed by its pathognomonic appearance on CT with bowel-within-bowel configuration. Similar MRI findings of intussusception have been described in the literature with the use of fast imaging techniques (T2-weighted turbo spin echo (TSE) sequences and half-Fourier acquisition single-shot turbo spin-echo (HASTE) images) [28].
Ultrasound is the modality of choice in the pediatric population. Classical ultrasound imaging features of intussusception include the target sign (concentric rings of alternating hyperechoic and hypoechoic layers). An abdominal X-ray may demonstrate a soft tissue mass and dilated obstructed bowel loops with air-fluid levels proximal to the mass.
Bezoar
Bezoars are one of the most unusual causes of bowel obstruction after gastric bypass surgery [29]. Bezoars are formed by the accumulation of indigestible materials. Patients who have had bariatric surgery are more prone to bezoar formation [29]. CT may demonstrate the bezoar as an obstructive mass mottled with gas bubbles with secondary SBO.
On MRI, a similar ovoid mass containing mottled low signal intensities, which represent air bubbles, may be seen on both T1- and T2-weighted fast imaging techniques [30]. Bezoars are hardly visible on sonography due to the accumulated gas in the bowels affecting the ultrasonic sound. Sonography may demonstrate an intraluminal mass with a hyperechoic arc-like surface casting a posterior acoustic shadow. An abdominal X-ray may show dilated obstructed bowel loops with air-fluid levels in patients with SBO. It is usually not possible to identify a bezoar on plain radiographs alone.
The presence of a classical feature of an IH, like SMV compression, and the fact that an IH is the most common late complication after gastric bypass, made it the most likely diagnosis in our case.
Conclusion
In conclusion, this case report confirms the importance of CT examination in the diagnosis of patients suffering from complications after gastric bypass surgery and confirms that it should not be withheld from pregnant patients if necessary. Key CT findings can aid clinicians in making an early diagnosis of an IH and an early decision of surgical intervention.
TEACHING POINT
Computed tomography (CT) examination is crucial in the diagnosis of patients suffering from complications after gastric bypass surgery. The mesenteric swirl sign and compression of the superior mesenteric vein combined with small-bowel obstruction are key CT findings in diagnosing an internal hernia in patients who have undergone laparoscopic Roux-en-Y gastric bypass.
Table 1.
Summary table for an internal hernia after a laparoscopic Roux-en-Y gastric bypass.
| Etiology | Creation of potential spaces for an internal hernia after laparoscopic Roux-en-Y gastric bypass (LRYGB): mesenteric defect at the jejunojejunostomy and the Petersen’s space (after antecolic procedure) |
| Incidence | 0–6.9 % |
| Gender ratio | N/A |
| Age predilection | N/A |
| Risk factors | -Body weight loss (reduced intraperitoneal fat leads to larger mesenteric defects) -Pregnancy (increased abdominal pressure caused by the enlargement of the uterus) -Retrocolic procedure (antecolic LRYGB is currently the preferred approach) |
| Treatment | Surgery |
| Prognosis | Depends on the development of further complications, including bowel infarction and perforation |
| Findings on imaging | -Compression of the superior mesenteric vein and the mesenteric swirl sign -Small bowel obstruction can be present |
ABBREVIATIONS
- CT
Computed tomography
- IH
Internal hernia
- LRYGB
Laparoscopic Roux-en-Y gastric bypass
- MRI
Magnetic resonance imaging
- RYGB
Roux-en-Y gastric bypass
- SBO
Small-bowel obstruction
- SMV
Superior mesenteric vein
REFERENCES
- 1.Merali HS, Miller CA, Erbay N, Ghosh A. Importance of CT in evaluating internal hernias after Roux-en-Y gastric bypass surgery. J Radiol Case Rep. 2009;3(6):34–37. doi: 10.3941/jrcr.v3i6.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Andreasen LA, Nilas L, Kjær MM. Operative complications during pregnancy after gastric bypass-a register-based cohort study. Obes Surg. 2014;24:1634–1638. doi: 10.1007/s11695-014-1232-z. [DOI] [PubMed] [Google Scholar]
- 3.Wittgrove AC, Clark GW, Tremblay LJ. Laparoscopic gastric bypass, Roux-en-Y: Preliminary report of five cases. Obes Surg. 1994 Nov;4(4):353–357. doi: 10.1381/096089294765558331. [DOI] [PubMed] [Google Scholar]
- 4.Scheirey CD, Scholz FJ, Shah PC, Brams DM, Wong BB, Pedrosa M. Radiology of the laparoscopic Roux-en-Y gastric bypass procedure: conceptualization and precise interpretation of results. Radiographics. 2006;26(5):1355–71. doi: 10.1148/rg.265055123. [DOI] [PubMed] [Google Scholar]
- 5.Goudsmedt F, Deylgat B, Coenegrachts K, Van De Moortele K, Dillemans B. Internal hernia after laparoscopic Roux-en-Y gastric bypass: a correlation between radiological and operative findings. Obes Surg. 2015;25(4):622–627. doi: 10.1007/s11695-014-1433-5. [DOI] [PubMed] [Google Scholar]
- 6.Reijnierse Anniek, Burgers Janneke A, Go Attie TJI, Zengerink Johannes F, van der Weiden RobinMF. Late complications of bariatric surgery in pregnancy. JRSM Open. 2016;7(11):2054270416660935. doi: 10.1177/2054270416660935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Maier J, Herrasti Gallego A, Floyd AK. Compression of the superior mesenteric vein-a sign of acute internal herniation in patients with antecolic laparoscopic Roux-en-Y gastric bypass. Eur Radiol. 2017;27(4):1733–1739. doi: 10.1007/s00330-016-4526-9. [DOI] [PubMed] [Google Scholar]
- 8.Escalona A, Devaud N, Pérez G, et al. Antecolic versus retrocolic alimentary limb in laparoscopic Roux-en-Y gastric bypass: a comparative study. Surg Obes Relat Dis. 2007 Jul-Aug;3(4):423–7. doi: 10.1016/j.soard.2007.04.005. [DOI] [PubMed] [Google Scholar]
- 9.Higa K, Ho T, Tercero F, Yunus T, Boone KB. Laparoscopic Roux-en-Y gastric bypass: 10-year follow-up. Surg Obes Relat Dis. 2011 Jul-Aug;7(4):516–25. doi: 10.1016/j.soard.2010.10.019. [DOI] [PubMed] [Google Scholar]
- 10.Ahmed AR, O’Malley W. Internal hernia with Roux loop obstruction during pregnancy after gastric bypass surgery. Obes Surg. 2006;16(9):1246–8. doi: 10.1381/096089206778392310. [DOI] [PubMed] [Google Scholar]
- 11.Leal-González R, De la Garza-Ramos R, Guajardo-Pérez H, Ayala-Aguilera F, Rumbaut R. Internal hernias in pregnant women with history of gastric bypass surgery: Case series and review of literature. Int J Surg Case Rep. 2013;4(1):44–47. doi: 10.1016/j.ijscr.2012.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Al-Mansour MR, Mundy R, Canoy JM, Dulaimy K, Kuhn JN, Romanelli J. Internal hernia after laparoscopic antecolic Roux-en-Y gastric bypass. Obes Surg. 2015;25(11):2106–11. doi: 10.1007/s11695-015-1672-0. [DOI] [PubMed] [Google Scholar]
- 13.Torres-Villalobos GM, Kellogg TA, Leslie DB, et al. Small bowel obstruction and internal hernias during pregnancy after gastric bypass surgery. Obes Surg. 2009;19(7):944–50. doi: 10.1007/s11695-008-9681-x. [DOI] [PubMed] [Google Scholar]
- 14.Gruetter F, Kraljevi? M, Nebiker CA, Delko T. Internal hernia in late pregnancy after laparoscopic Roux-en-Y gastric bypass. BMJ Case Rep. 2014 Dec;23:2014. doi: 10.1136/bcr-2014-206770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gagné DJ, DeVoogd K, Rutkoski JD, Papasavas PK, Urbandt JE. Laparoscopic repair of internal hernia during pregnancy after Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2010 Jan-Feb;6(1):88–92. doi: 10.1016/j.soard.2009.06.002. [DOI] [PubMed] [Google Scholar]
- 16.Errebo MB, Sommer T. Leakage and internal herniation are the most common complications after gastric bypass. Dan Med J. 2014 May;61(5):A4844. [PubMed] [Google Scholar]
- 17.Koppman JS, Li C, Gandsas A. Small bowel obstruction after laparoscopic Roux-en-Y gastric bypass: a review of 9,527 patients. J Am Coll Surg. 2008 Mar;206(3):571–84. doi: 10.1016/j.jamcollsurg.2007.10.008. [DOI] [PubMed] [Google Scholar]
- 18.Al Harakeh AB. Complications of laparoscopic Roux-en-Y gastric bypass. Surg Clin North Am. 2011 Dec;91(6):1225–37. doi: 10.1016/j.suc.2011.08.011. [DOI] [PubMed] [Google Scholar]
- 19.Guidelines for diagnostic imaging during pregnancy and lactation. Committee Opinion No. 656. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2016;127:e75–80. doi: 10.1097/AOG.0000000000001316. [DOI] [PubMed] [Google Scholar]
- 20.Tirada N, Dreizin D, Khati NJ, Akin EA, Zeman RK. Imaging pregnant and lactating patients. Radiographics. 2015;35(6):1751–65. doi: 10.1148/rg.2015150031. [DOI] [PubMed] [Google Scholar]
- 21.Wieseler KM, Bhargava P, Kanal KM, Vaidya S, Stewart BK, Dighe MK. Imaging in pregnant patients: examination appropriateness. Radiographics. 2010;30(5):1215–29. doi: 10.1148/rg.305105034. [DOI] [PubMed] [Google Scholar]
- 22.Lockhart ME, Tessler FN, Canon CL, et al. Internal hernia after gastric bypass: sensitivity and specificity of seven CT signs with surgical correlation and controls. AJR Am J Roentgenol. 2007;188(3):745–50. doi: 10.2214/AJR.06.0541. [DOI] [PubMed] [Google Scholar]
- 23.Dilauro M, McInnes MD, Schieda N, et al. Internal hernia after laparoscopic Roux-en-Y gastric bypass: optimal CT signs for diagnosis and clinical decision making. RNSA Radiology. 2017;282(3):752–760. doi: 10.1148/radiol.2016160956. [DOI] [PubMed] [Google Scholar]
- 24.Rosenkrantz AB, Kurian M, Kim D. MRI appearance of internal hernia following Roux-en-Y gastric bypass surgery in the pregnant patient. Clin Radiol. 2010 Mar;65(3):246–9. doi: 10.1016/j.crad.2009.12.002. [DOI] [PubMed] [Google Scholar]
- 25.Lang RA, Buhmann S, Hopman A, et al. Cine-MRI detection of intraabdominal adhesions: correlation with intraoperative findings in 89 consecutive cases. Surg Endosc. 2008 Nov;22(11):2455–61. doi: 10.1007/s00464-008-9763-9. [DOI] [PubMed] [Google Scholar]
- 26.Coblijn UK, de Raaff CA, van Wagensveld BA, van Tets WF, de Castro SM. Trocar port hernias after bariatric surgery. Obes Surg. 2016 Mar;26(3):546–51. doi: 10.1007/s11695-015-1779-3. [DOI] [PubMed] [Google Scholar]
- 27.Boudourakis LD, Divino C, Nguyen S. Retrograde intussusception seven years after a laparoscopic Roux-en-Y gastric bypass. J Minim Access Surg. 2013;9(2):82–83. doi: 10.4103/0972-9941.110969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Byrne AT, Geoghegan T, Govender P, Lyburn ID, Colhoun E, Torreggiani WC. The imaging of intussusception. Clin Radiol. 2005 Jan;60(1):39–46. doi: 10.1016/j.crad.2004.07.007. [DOI] [PubMed] [Google Scholar]
- 29.Sarhan Mohammad, Shyamali Bhakta, Fakulujo Adeshola, Ahmed Leaque. Jejunal bezoar causing obstruction after laparoscopic Roux-en-Y gastric bypass. JSLS. 2010 Oct-Dec;14(4):592–595. doi: 10.4293/108680810X12924466008682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lee JM, Jung SE, Lee KY. Small-bowel obstruction caused by phytobezoar: MR imaging findings. AJR Am J Roentgenol. 2002 Aug;179(2):538–9. doi: 10.2214/ajr.179.2.1790538. [DOI] [PubMed] [Google Scholar]