Abstract
Objective:
To retrospectively evaluate the feasibility of CT fluoroscopy-guided percutaneous marking using a 25-gauge needle and indigo carmine before video-assisted thoracoscopic surgery (VATS) for small lung lesions.
Methods:
21 patients, 14 males and 7 females, with a median age of 69 years (range, 40–79), underwent CT fluoroscopy-guided percutaneous VATS marking using a 25-gauge, 70-mm needle and 1.5-ml indigo carmine. The mean diameter of the lung lesions was 14 mm (range, 6–27). We evaluated the technical success rate, surgical success rate and complications related to this procedure by reviewing medical records and images. Technical success was defined as completion of this procedure. Surgical success was defined as resection of the target lesion with negative margins on pathological examination after VATS. Complications that required advanced levels of care were classified as major complications, and the remaining complications were considered minor.
Results:
The technical success rate was 100%. In all cases, VATS was successfully performed as planned, and the target lesion was resected with negative margins on pathological examination after VATS. Thus, the surgical success rate was 100%. Mild pneumothorax was found in two cases, but further treatment was not required. The minor complication rate was 9.5% (2/21), and major complication rate was 0%. Only two patients (9.5%) complained of slight pain upon puncture, but local anaesthesia was not required.
Conclusion:
Percutaneous CT fluoroscopy-guided VATS marking using a 25-gauge needle without local anaesthesia appears feasible and safe.
Advances in knowledge:
This technique expands a possibility of the CT-guided marking.
Introduction
The mortality of lung cancer is higher than that of any other cancers and NIH has reported that lung cancer is the cancer with the worst mortality in their 2016 announcement.1 Recently, due to technological innovation in CT, small lung lesions, including adenocarcinoma in situ and minimally invasive adenocarcinoma, can be detected.2–4 To diagnose malignancy, however, histological examination is mandatory. Generally, bronchoscopic lung biopsy is the first choice, but sometimes it is difficult to reach peripheral lesions.5 CT-guided percutaneous biopsy is another option, but it has a risk of complications such as pneumothorax, haemothorax and air embolism.6 Thus, video-assisted thoracoscopic surgery (VATS) has recently gained widespread acceptance for both diagnosis and treatment of such lesions because it can minimize post-operative morbidity and remove as small a volume of lung tissue as possible.7, 8 However, the disadvantage of VATS is the difficulty in detecting small subpleural lesions, which are frequently neither visible nor palpable. Therefore, pre-operative CT fluoroscopy-guided percutaneous marking of a pulmonary lesion often plays an important role. Conventionally, 20- to 23-gauge needles have been used for local anaesthesia and marking, but it often produces local pain.9, 10 On the other hand, a 25-gauge needle is fine and anaesthesia is not necessary to puncture the skin; therefore, we considered that this needle should be usable for CT fluoroscopy-guided percutaneous VATS marking. In this study, we evaluated feasibility of the new technique of CT fluoroscopy-guided percutaneous VATS marking using a 25-gauge needle and indigo carmine.
Methods and materials
The study was approved by the Ethics Committee of Nagoya City Hospital Bureau (16-04-384-42).
The authors have no conflicts of interest directly relevant to the content of this article.
This retrospective study was approved by the Institutional Review Board, and written informed consent for the procedure was obtained from each patient.
21 patients, 14 males and 7 females with a median age of 69 years (range, 40–79 years), underwent CT fluoroscopy-guided percutaneous VATS marking using a 25-gauge needle. All lesions were diagnosed as adenocarcinoma in situ, lepidic predominant adenocarcinoma, atypical adenomatous hyperplasia or adenomatous hyperplasia by chest radiologists, and VATS was considered to be indicated. The mean diameter of the lesions was 14 mm (range 6–27). 19 lesions (91.5%) had solid opacity, and 2 (9.5%) had only ground glass opacity. Location of the lesions was as follows; the right lung in 14 (upper lobe in 6, middle lobe in 2, lower lobe in 6) and left in 7 (upper lobe in 3, lower lobe in 4). We evaluated the technical success rate, surgical success rate and complications related to this procedure by reviewing medical records and images. Technical success was defined as completion of this procedure. Surgical success was defined as resection of the target lesion with negative margins on pathological examination after VATS. Complications that required advanced levels of care were classified as major complications, and the remaining complications were considered minor.
Technique of the procedure
All marking procedures were performed on the day of VATS, and a 25-gauge needle (Figure 1, TOP® Spinal Needle, 25-gauge 70 cm, TOP Corporation, Tokyo, Japan) was used in all procedures. During the procedure, first, chest CT scan was performed to confirm the position of the pulmonary lesion. Then, after disinfection, the 25-gauge needle was punctured and the tip was placed within 10 mm of the lesion under CT fluoroscopy with breath-hold after expiration, without local anaesthesia. When it was confirmed by CT fluoroscopy that the needle was near the pulmonary lesion, 1.0 ml of indigo carmine (1 mg ml−1) was injected. Then, the needle was immediately withdrawn with injection of 0.5 ml of indigo carmine. The total amount of indigo carmine was 1.5 ml. Chest CT scan was repeated immediately after the procedure to evaluate the marking position and complications. In all cases, VATS was performed immediately after placement of the marker, usually within 1–3 h.
Figure 1. .

A 25-gauge needle (TOP® Spinal Needle).
Results
In 20 out of the 21 cases, puncture was successfully performed using the 25-gauge needle, and indigo carmine was injected as planned (Figure 2). Only in one case, the marking for the lesion was not enough due to poor deposition of indigo carmine, and the procedure was performed again in the same manner. In this case, the marking was completed successfully eventually. Thus, the technical success rate was 100%. All patients did not request any analgesia. In all cases, VATS was successfully performed as planned, without conversion to extended resection, and the target lesion was resected with negative margins on pathological examination after VATS. Thus, the surgical success rate was 100%. Slight pneumothorax was found in two cases, but further treatment was not required. There were no complications requiring advanced levels of care or procedure-related deaths. Thus, the minor complication rate was 9.5% (2/21), and major complication rate was 0%. Only two patients (9.5%) complained of slight pain upon puncture (Level 3–4 pain of the Numerical Rating Scale), but local anaesthesia was not required. The mean procedure time was 26 min (range, 19–49).
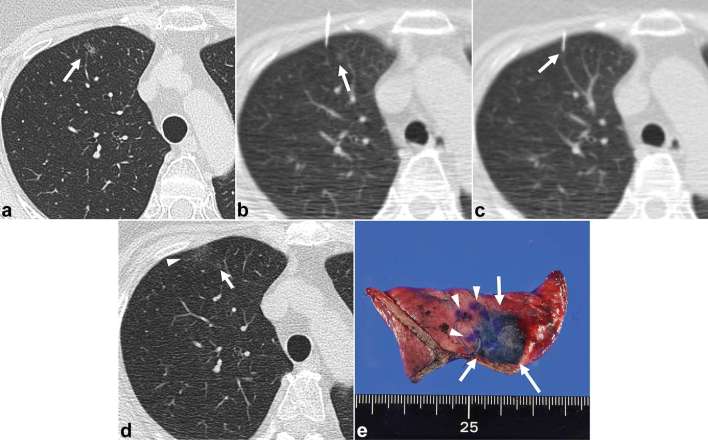
Figure 2. .
A 73-year-old female with a lung nodule in the right upper lobe. (a) CT shows the nodule in the right upper lobe lung (arrow). (b) CT fluoroscopy during the procedure shows the 25-gauge needle was inserted successfully near to the nodule (arrow). (c) CT fluoroscopy image 5 mm below shows the tip of the 25-gauge needle (arrow) was located within 10 mm of the nodule, and indigo carmine was injected. (d) CT after the procedure shows successful deposition of indigo carmine (arrow head) close to the nodule (arrow). (e) Macroscopically, deposition of indigo carmine is confirmed (arrows). Small purple areas are markings by surgeons using a pen to estimate the location of the nodule (arrow heads).
Discussion
In this study, we demonstrated a high technical success rate (100%) and surgical success rate (100%) with a low complication rate (minor 10%, major 0%) for our procedure of VATS marking. Generally, local anaesthesia is applied for the skin and pleura before marking. However, it was reported that 7% of patients felt strong pain during the VATS marking procedure even with local anaesthesia.11 On the other hand, in our study, only two patients (9.5%) complained of slight pain upon puncture, but they did not require local anaesthesia. We think the puncture with local anaesthesia may be as painful as this procedure. Thus, we think this percutaneous CT fluoroscopy-guided VATS marking using a 25-gauge needle without local anaesthesia can be a feasible and safe procedure.
There are two advantages of this method. First, in the conventional method, there is a risk of developing pneumothorax by local anaesthesia for the pleura. When pneumothorax occurs, appropriate puncture near to the lesion becomes difficult. In our method, however, puncture to the lung could be performed without pneumothorax in all cases. Thus, the puncture can be more easily performed. Second, elimination of local anaesthesia is useful especially for patients who have an allergy to drugs for local anaesthesia.
In the literature, several VATS marking methods were reported using a hook-wire, lipiodol or radioisotope.12–15 However, air embolism is a serious complication in the procedure using the hook-wire.6,16–18 Furthermore, there is a risk of drop out of the hook-wire before surgery.9, 11,15 The procedures using lipiodol or radioisotope are easy, but need fluoroscopy to confirm the location during surgery. Thus, the procedure using a dye is reported to be a much easier method, and several dyeing materials, such as indocyanine green, methylene blue and indigo carmine, have been reported.10, 19 Among them, indigo carmine has better stability compared with the other materials, and thus, we think indigo carmine is an appropriate material for VATS marking.20
On the other hand, a percutaneous ablation procedure recently has been reported for lung tumours.21, 22 We think it can be an alternative treatment option for small lung lesions in place of VATS. Unfortunately, however, it is not covered with medical insurance in our country at present. Thus, VATS is still an important option, and percutaneous CT fluoroscopy-guided marking is also a meaningful procedure.
Our study has several limitations. The small sample size and retrospective design were key limitations. In addition, the surgical success of our study may not accurately reflect the effectiveness of CT fluoroscopy-guided marking because surgery might be successfully performed even when marking was not in the correct place. Furthermore, in this study, we could not evaluate pain scales during the procedure objectively. We think there is a possibility that cases exist in which this procedure would be difficult to perform, especially for patients who are sensitive to pain. Thus, we think further prospective comparative studies with large patient numbers are required.
In conclusion, percutaneous CT fluoroscopy-guided VATS marking using a 25-gauge needle and indigo carmine appears to be feasible and safe.
Contributor Information
Yasuteru Shimamura, Email: yasuteru.shimamura@gmail.com.
Shigeru Sasaki, Email: ssasaki916@yahoo.co.jp.
Masashi Shimohira, Email: m_shimohira@yahoo.co.jp.
Hiroyuki Ogino, Email: oginogio@gmail.com.
Daisuke Yuki, Email: cdz89540@yahoo.co.jp.
Katsumi Nakamae, Email: k.nakamae.15@west-med.jp.
Masaki Hara, Email: mhs340129@gmail.com.
Yuta Shibamoto, Email: yshiba@med.nagoya-cu.ac.jp.
Funding
The study was approved by the Ethics Committee of Nagoya City Hospital Bureau (16-04-384-42). This retrospective study was approved by the Institutional Review Board, and written informed consent for the procedure was obtained from each patient.
REFERENCES
- 1.SEER. Stat fact sheets: lung and bronchus cancer. 2016. Available from: https://seer.cancer.gov/statfacts/html/lungb.html
- 2.Munden RF, Pugatch RD, Liptay MJ, Sugarbaker DJ, Le LU. Small pulmonary lesions detected at CT: clinical importance. Radiology 1997; 202: 105–10. doi: https://doi.org/10.1148/radiology.202.1.8988198 [DOI] [PubMed] [Google Scholar]
- 3.Aberle DR, Adams AM, Berg CD, Black WC, Clapp JD, Fagerstrom RM, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med 2011; 365: 395–409. doi: https://doi.org/10.1056/NEJMoa1102873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bach PB, Mirkin JN, Oliver TK, Azzoli CG, Berry DA, Brawley OW, et al. Benefits and harms of CT screening for lung cancer: a systematic review. JAMA 2012; 307: 2418. doi: https://doi.org/10.1001/jama.2012.5521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guvenc C, Yserbyt J, Testelmans D, Zanca F, Carbonez A, Ninane V, et al. Computed tomography characteristics predictive for radial EBUS-miniprobe-guided diagnosis of pulmonary lesions. J Thorac Oncol 2015; 10: 472–8. doi: https://doi.org/10.1097/JTO.0000000000000410 [DOI] [PubMed] [Google Scholar]
- 6.Tomiyama N, Yasuhara Y, Nakajima Y, Adachi S, Arai Y, Kusumoto M, et al. CT-guided needle biopsy of lung lesions: a survey of severe complication based on 9783 biopsies in Japan. Eur J Radiol 2006; 59: 60–4. doi: https://doi.org/10.1016/j.ejrad.2006.02.001 [DOI] [PubMed] [Google Scholar]
- 7.Kaseda S, Aoki T, Hangai N, Shimizu K. Better pulmonary function and prognosis with video-assisted thoracic surgery than with thoracotomy. Ann Thorac Surg 2000; 70: 1644–6. doi: https://doi.org/10.1016/S0003-4975(00)01909-3 [DOI] [PubMed] [Google Scholar]
- 8.Yan TD, Black D, Bannon PG, McCaughan BC. Systematic review and meta-analysis of randomized and nonrandomized trials on safety and efficacy of video-assisted thoracic surgery lobectomy for early-stage non-small-cell lung cancer. J Clin Oncol 2009; 27: 2553–62. doi: https://doi.org/10.1200/JCO.2008.18.2733 [DOI] [PubMed] [Google Scholar]
- 9.Gonfiotti A, Davini F, Vaggelli L, De Francisci A, Caldarella A, Gigli PM, et al. Thoracoscopic localization techniques for patients with solitary pulmonary nodule: hookwire versus radio-guided surgery. Eur J Cardiothorac Surg 2007; 32: 843–7. doi: https://doi.org/10.1016/j.ejcts.2007.09.002 [DOI] [PubMed] [Google Scholar]
- 10.Chino S, Kuriyama K, Isohashi K, Murata M, Mitani H, Tsuda K, et al. Percutaneous localization of pulmonary nodules with CT guidance for lung resection: use of dyes. Nihon Igaku Hoshasen Gakkai Zasshi 2003; 63: 308–10. [PubMed] [Google Scholar]
- 11.Yoshida Y, Inoh S, Murakawa T, Ota S, Fukayama M, Nakajima J. Preoperative localization of small peripheral pulmonary nodules by percutaneous marking under computed tomography guidance. Interact Cardiovasc Thorac Surg 2011; 13: 25–8. doi: https://doi.org/10.1510/icvts.2011.266932 [DOI] [PubMed] [Google Scholar]
- 12.Saito H, Minamiya Y, Matsuzaki I, Tozawa K, Taguchi K, Nakagawa T, et al. Indication for preoperative localization of small peripheral pulmonary nodules in thoracoscopic surgery. J Thorac Cardiovasc Surg 2002; 124: 1198–202. doi: https://doi.org/10.1067/mtc.2002.127331 [DOI] [PubMed] [Google Scholar]
- 13.Bommart S, Bourdin A, Marin G, Berthet JP, Pujol JL, Serre I, et al. Impact of preoperative marking coils on surgical and pathologic management of impalpable lung nodules. Ann Thorac Surg 2014; 97: 414–8. doi: https://doi.org/10.1016/j.athoracsur.2013.09.041 [DOI] [PubMed] [Google Scholar]
- 14.Mogi A, Yajima T, Tomizawa K, Onozato R, Tanaka S, Kuwano H. Video-assisted thoracoscopic surgery after preoperative CT-guided lipiodol marking of small or impalpable pulmonary nodules. Ann Thorac Cardiovasc Surg 2015; 21: 435–9. doi: https://doi.org/10.5761/atcs.oa.15-00018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Doo KW, Yong HS, Kim HK, Kim S, Kang EY, Choi YH. Needlescopic resection of small and superficial pulmonary nodule after computed tomographic fluoroscopy-guided dual localization with radiotracer and hookwire. Ann Surg Oncol 2015; 22: 331–7. doi: https://doi.org/10.1245/s10434-014-3884-2 [DOI] [PubMed] [Google Scholar]
- 16.Sakiyama S, Kondo K, Matsuoka H, Yoshida M, Miyoshi T, Yoshida S, et al. Fatal air embolism during computed tomography-guided pulmonary marking with a hook-type marker. J Thorac Cardiovasc Surg 2003; 126: 1207–9. doi: https://doi.org/10.1016/S0022-5223(03)00821-3 [DOI] [PubMed] [Google Scholar]
- 17.Nakagawa T, Kurihara N, Toyama S, Sato H, Saito H, Minamiya Y. A case of air embolism caused by CT-guided marking for small peripheral lung cancer. Jpn J Chest Surg 2014; 28: 966–70. doi: https://doi.org/10.2995/jacsurg.28.966 [Google Scholar]
- 18.Suzuki K, Shimohira M, Hashizume T, Ozawa Y, Sobue R, Mimura M, et al. Usefulness of CT-guided hookwire marking before video-assisted thoracoscopic surgery for small pulmonary lesions. J Med Imaging Radiat Oncol 2014; 58: 657–62. doi: https://doi.org/10.1111/1754-9485.12214 [DOI] [PubMed] [Google Scholar]
- 19.Vandoni RE, Cuttat JF, Wicky S, Suter M. CT-guided methylene-blue labelling before thoracoscopic resection of pulmonary nodules. Eur J Cardiothorac Surg 1998; 14: 265–70. doi: https://doi.org/10.1016/S1010-7940(98)00160-2 [DOI] [PubMed] [Google Scholar]
- 20.Endo M, Kotani Y, Satouchi M, Takada Y, Sakamoto T, Tsubota N, et al. CT fluoroscopy-guided bronchoscopic dye marking for resection of small peripheral pulmonary nodules. Chest 2004; 125: 1747–52. doi: https://doi.org/10.1378/chest.125.5.1747 [DOI] [PubMed] [Google Scholar]
- 21.VanSonnenberg E, Shankar S, Morrison PR, Nair RT, Silverman SG, Jaklitsch MT, et al. Radiofrequency ablation of thoracic lesions: part 2, initial clinical experience--technical and multidisciplinary considerations in 30 patients. AJR Am J Roentgenol 2005; 184: 381–90. doi: https://doi.org/10.2214/ajr.184.2.01840381 [DOI] [PubMed] [Google Scholar]
- 22.Smith SL, Jennings PE. Lung radiofrequency and microwave ablation: a review of indications, techniques and post-procedural imaging appearances. Br J Radiol 2015; 88: 20140598. doi: https://doi.org/10.1259/bjr.20140598 [DOI] [PMC free article] [PubMed] [Google Scholar]