Abstract
Objective:
The aim of the present study was to assess the technical feasibility and safety of the unilateral pulmonary artery occlusion (UPAO) test in pre-operative evaluation of pneumonectomy or pleuropneumonectomy for lung or pleural tumours.
Methods:
The UPAO test was performed on 91 patients who were scheduled to undergo or were being considered for pneumonectomy or pleuropneumonectomy between June 2003 and July 2016. There were 74 males and 17 females, with a median age of 65 years (range, 23–80). The technical success rate, procedure time and complication rate were evaluated. Technical success was defined as completion of the UPAO test.
Results:
The diagnoses of the 91 patients were as follows: lung cancer in 63, malignant pleural mesothelioma in 21, thymoma in 5, lung metastasis in 1 and lung carcinoid in 1. The UPAO test was performed successfully on 88 out of 91 patients (technical success rate: 97%). The median procedure time was 57 min (range, 34–120). Cardiac arrest due to migration of the balloon catheter to the pulmonary trunk occurred in 1 patient (complication rate: 1.1%).
Conclusion:
The UPAO test in pre-operative evaluation of pneumonectomy or pleuropneumonectomy for lung or pleural tumours appears to be technically feasible. However, it needs to be performed with care in order to avoid severe complications.
Advances in knowledge:
The UPAO test can be safely performed and is helpful in evaluating patients for pneumonectomy or pleuropneumonectomy.
Introduction
After surgical resection of a lung or pleural tumour, the decrease in lung volume leads to reduced ventilation and a smaller pulmonary vascular bed, resulting in an increased risk of complications, such as acute respiratory distress syndrome, respiratory failure and pulmonary hypertension.1,2 The unilateral pulmonary artery occlusion (UPAO) test is a method used to evaluate cardiopulmonary function and pre-operatively establish whether patients will be able to tolerate pneumonectomy or pleuropneumonectomy.3–7 The UPAO test simulates the condition of a decreased pulmonary vascular bed after lung resection, and evaluates the reserve power of right heart function. When the mean pulmonary artery pressure (PAP) is 30 mmHg or higher after 15 min, the cardiopulmonary function of the patient is considered to be intolerable for pneumonectomy and pleuropneumonectomy, according to previously reported evidence.6,7 This criterion is supported by the following findings: in patients with pulmonary hypertension or thromboembolism not undergoing pneumonectomy or pleuropneumonectomy, 5-year survival rates were 10–54% with mean PAP > 50 mmHg, 50–63% with mean PAP of 30–50 mmHg and almost 100% with mean PAP < 30 mmHg.6 In cardiology, pulmonary hypertension is diagnosed when the mean PAP is higher than 25 mm Hg at rest or 30 mm Hg during physical activity.8
Recent advances in MRI have made it possible to evaluate pulmonary hypertension and estimate PAP.9–12 However, difficulties are still associated with estimating PAP under occluded conditions. Therefore, the UPAO test remains a relevant procedure. The purpose of the present study was to assess the technical feasibility and safety of the UPAO test in a pre-operative evaluation of pneumonectomy or pleuropneumonectomy for lung or pleural tumours.
Methods and Materials
Patients and endpoints
This retrospective study was approved by the Institutional Review Board. Written informed consent for the procedure was obtained from each patient. The UPAO test was performed on all 91 patients who were scheduled to undergo or were being considered for pneumonectomy or pleuropneumonectomy between June 2003 and July 2016. 74 patients were males and 17 were females, and their median age was 65 years (range, 23–80). The technical success rate, procedure time and complication rate were evaluated. Technical success was defined as completion of the UPAO test. Close observations for complications associated with the UPAO test were conducted during the procedure and post-procedural admission.
Technique of the UPAO test
All procedures were performed via an ultrasound guided common femoral vein 12-Fr. sheath (SuperSheath; Medikit, Tokyo, Japan). In order to prevent the formation of thrombus during the procedure, 3,000 units (1,000 units ml−1) of heparin was administered intravenously, with an additional 1,000 units being added every hour. Carbon dioxide was used to inflate the balloon catheters instead of a contrast. It enables quicker inflation and deflation of the balloon. In the event of a balloon rupture carbon dioxide is safe as it is absorbed in the pulmonary bed. Initially, a 7-Fr. balloon catheter (Balloon Angiographic Catheter, Harmac Medical Products, Buffalo, NY) was advanced into the pulmonary artery (PA), because it is easier to manipulate owing to its small balloon size and soft shaft, compared with the triple-lumen balloon catheter (Serecon MP catheter II; Terumo, Tokyo, Japan), which was used for the UPAO test. On inflation of the 7-Fr. balloon catheter in the PA on the side of the planned pneumonectomy or pleuropneumonectomy, it was carried into the PA by the blood flow. Pulmonary angiography was performed after the balloon was deflated. The 7-Fr. balloon catheter was then exchanged for the triple-lumen balloon catheter over a hydrophilic guidewire (Radifocus; Terumo, Tokyo, Japan).
The triple-lumen balloon catheter has three roles in the UPAO test: (1) measuring proximal PAP via a proximal side hole; (2) occlusion of the target PA with the balloon and (3) distal heparinized saline perfusion (5,000 units heparin in 500 ml saline) to prevent thrombus formation during the time of arrested flow. Following carbon dioxide inflation of the balloon, the proximal PAP was measured immediately after inflation and then at 5, 10 and 15 min. The balloon was then deflated, and PAP was measured immediately after deflation. The inferior vena cava (IVC) pressure was also measured.
If the mean PAP at 15 min was 30 mmHg or higher, the cardiopulmonary reserve was considered to be insufficient for pneumonectomy and pleuropneumonectomy. During the UPAO test, the patient was closely observed for any clinical symptoms and the peripheral oxygen saturation was monitored via pulse oximetry. In addition to the UPAO test, cardiopulmonary function was assessed with spirometry, electrocardiography and echocardiography.
Results
The diagnoses of the 91 patients were as follows: lung cancer in 63, malignant pleural mesothelioma in 21, thymoma in 5, lung metastasis in 1 and lung carcinoid in 1. The UPAO test was performed successfully on 88 out of 91 patients (technical success rate: 97%). In the remaining 3 patients, the UPAO test was terminated because of difficulties encountered when advancing the catheter to the PA on the side of planned pneumonectomy or pleuropneumonectomy in 2, and procedure-related cardiac arrest in 1. Unilateral chest abnormalities evaluated with CT, smoking history and sputum analysis results are summarized in Table 1. Stenosis of the PA on the side of planned surgery due to nodal enlargement or a tumour was detected in 7 out of 91 patients (7.7%); the UPAO test was successfully performed on these 7 patients. The median procedure time was 57 min (range, 34–120). Cardiac arrest due to migration of the balloon catheter to the pulmonary trunk occurred in one patient who underwent UPAO test for left lung cancer (complication rate: 1.1%). In this case, the balloon was deflated immediately, and the patient’s cardiac beat recovered spontaneously. Pneumonectomy was then performed without the UPAO test as initially scheduled based on informed consent.
Table 1.
Summary of unilateral chest abnormality
| CT finding (n = 91) | |
|---|---|
| Emphysema | 36 |
| Partial atelectasis | 7 |
| Pleural effusion | 19 |
| Hilar/mediastinal nodal enlargement | 49 |
| Stenosis of the pulmonary arterya | 7 |
| Distant metastases | 0 |
| History of smoking (n = 91) | |
| Yes | 71 |
| Sputum analysis (n = 46) | |
| Presence of bacterium | 24 |
aStenosis of the pulmonary artery of the side of planned pneumonectomy or pleuropneumonectomy due to nodal enlargement or tumour.
In 88 patients subjected to the UPAO test, the median values of mean PAP, systolic PAP and diastolic PAP after 15 min were 20 (range, 12–42), 33 (range, 19–64) and 11 mmHg (range, 3–36), respectively. Details of UPAO test results are summarized in Table 2. Mean PAP was less than 30 mmHg in 79 out of the 88 patients; in the remaining nine patients, the mean PAP after 15 min was 30–42 mmHg (median, 31). In practice, pneumonectomy was performed on 34 patients and pleuropneumonectomy on 19. The UPAO test was performed on 17 patients because pneumonectomy or pleuropneumonectomy was a treatment option; however, lobectomy or segmental resection was ultimately conducted based on intraoperative findings. Eight patients did not complete the planned surgery: 7 were deemed inoperable due to excessively invasive tumours in 5 and intraoperative bleeding and ventricular tachycardia in one each. In one patient, chemoradiation therapy was considered more appropriate than surgery after the UPAO test because of tumour invasion to the esophagus and heart, even though the mean PAP after 15 min was 18 mmHg. In one patient with lung cancer, mean PAP after 15 min was 28 mmHg and oxygen saturation in the peripheral artery decreased from 97 to 83% during the UPAO test. Thus, pneumonectomy was avoided and radiation therapy was administered.
Table 2.
PAP (mmHg) at UPAO test (median and range)
| Before inflation | Immediately after inflation | 5 min | 10 min | 15 min | Immediately after deflation | IVC | |
|---|---|---|---|---|---|---|---|
| Mean | 16.5 (5–34) | 21 (8–41) | 21 (12–40) | 20 (12–42) | 20 (12–42) | 17 (8–42) | 6 (0–14) |
| Systolic | 24 (14–58) | 32 (18–71) | 33 (18–70) | 32.5 (17–69) | 33 (19–64) | 27 (15–58) | 9 (1–25) |
| Diastolic | 11 (3–32) | 13 (1–26) | 13 (4–36) | 12 (4–36) | 11 (3–36) | 10 (2–36) | 4 (0–17) |
IVC, inferior vena cava; PAP, pulmonary artery pressure; UPAO, unilateral pulmonary artery occlusion.
In 52 out of the 53 patients (98%) who underwent pneumonectomy or pleuropneumonectomy after passing the UPAO test, cardiopulmonary complications did not occur during a median follow-up period of 29 months (range, 1–160). The remaining one patient underwent pneumonectomy for lung cancer because his mean PAP after 15 min was 23 mmHg. He developed exertional dyspnea 70 months later. His systolic, diastolic and mean PAP measured through a pulmonary catheter were 67, 19 and 40 mmHg, respectively, and he was diagnosed with pulmonary hypertension (1/53 = 1.9%). On the next day of the examination, he died of arrhythmia.
Pneumonectomy or pleuropneumonectomy was avoided in nine patients with mean PAP of 30 mmHg or higher. Among these patients, lobectomy or segmental resection was performed on seven, and chemotherapy and/or radiation therapy was administered to the other two patients. In patients who underwent lobectomy or segmental resection, no cardiopulmonary complications occurred in a median follow-up period of 22 months (range, 2–133). In all three patients who were unable to complete the UPAO test due to one cardiac arrest and two technical failures, pneumonectomy or pleuropneumonectomy was performed successfully based on informed consent, and cardiopulmonary complications did not occur during a median follow-up period of 36 months (range, 30–74).
Discussion
The UPAO test for pre-operative evaluation of pneumonectomy or pleuropneumonectomy for lung or pleural tumours had a technical success rate of 97% in this study. A major complication, procedure-related cardiac arrest due to migration of the balloon catheter to the pulmonary trunk, occurred in one left UPAO test (1.1%), with spontaneous cardiac recovery on balloon deflation. In this case, we suspected that the balloon was placed too proximally in the left PA and occluded the pulmonary trunk. We recommend that the position of the balloon be checked using a left anterior oblique view, which shows the left PA longitudinally when performing a left UPAO test (Figure 1).
Figure 1.
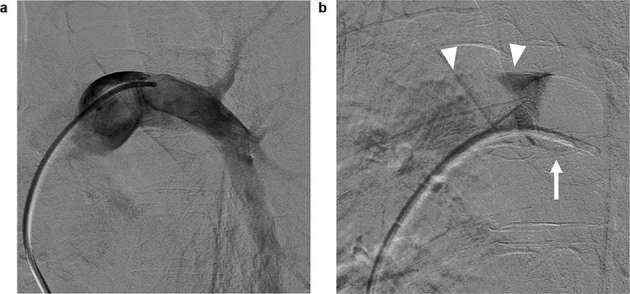
A 43-year-old male presented with left malignant pleural mesothelioma. (a) Left anterior oblique view of angiography performed before the UPAO test showing the left PA longitudinally. (b) Angiography shows compete occlusion of the left PA. The balloon was placed at the distal site of the main left PA (arrow), and there was a sufficient distance to the pulmonary trunk as a margin (arrow heads). The UPAO test was then performed successfully. Mean PAP at 15 min was 15 mmHg, and cardiopulmonary function was considered tolerable for pleuropneumonectomy. This patient then successfully underwent surgery. PA, pulmonary artery; UPAO, unilateral pulmonary artery occlusion.
In the present study, we measured PAP at 5, 10 and 15 min in all patients. If PAP at 5 or 10 min had been extremely high (e.g. >50 mmHg), the procedure would have been terminated. Furthermore, if it is not possible to continue this procedure for 15 min for some reason such as the appearance of symptoms or catheter migration, PAP at 5 and 10 min still provides useful information to consider indications for surgery. IVC pressure was measured in order to confirm the accuracy of the measurement system for the UPAO test; an extremely high IVC pressure may indicate an issue with the measurement system, and the UPAO test needs to be performed again or the system recalibrated.
In this present study, 52 out of the 53 patients (98%) who underwent pneumonectomy or pleuropneumonectomy after passing the UPAO test did not develop pulmonary hypertension. The procedure time of the UPAO test was relatively short (median, 57 min). Thus, we consider the UPAO test to be a useful examination before surgery. On the other hand, no cardiopulmonary complications were observed in patients who underwent lobectomy in our cohort. However, Wei et al13 reported that pulmonary hypertension may occur even after lobectomy; patients who developed pulmonary hypertension had a lower pre-operative forced expiratory volume in 1 s and diffusion capacity of the lung for carbon monoxide and a higher incidence of tricuspid regurgitation and mitral regurgitation than patients without pulmonary hypertension. Thus, the UPAO test may have a role for patients with these risks, even when they are scheduled for lobectomy.
In one case report, pulmonary thrombosis developed during the UPAO test after 15 min of occlusion.14 In that case, the inside of the catheter was flushed with heparinized saline only once before occlusion. We recommend systemic heparinization and continuous heparinized saline flushing of the tip hole of the balloon catheter to prevent thrombus formation. Furthermore, PA injury induced by a PA catheter has been reported, particularly by Swan-Ganz catheters.15–17 This may be caused by over-inflation of the balloon or inadvertent partial inflation of the balloon in a small branch vessel. When performing the UPAO test in patients with pulmonary hilar tumours, the possibility of tumour invasion to the right or left PA needs to be considered. In the present study, stenosis of the PA due to nodal enlargement or a tumour was detected in 7 out of 91 patients (7.7%). Cautious manipulation of the balloon catheter and appropriate inflation of the balloon is important to avoid PA injury. In the present study, one patient who underwent pneumonectomy after passing the UPAO test developed pulmonary hypertension 70 months later; his mean PAP after 15 min after balloon inflation was 23 mmHg. Since this only occurred in one out of the 53 patients who underwent pneumonectomy or pleuropneumonectomy after passing the UPAO test (1.9%), its incidence was low. Therefore, the threshold of this test appears to be appropriate; but the results obtained indicate that the UPAO test does not definitely predict the absence of post-operative pulmonary hypertension. Finally, limitations of this study include the relatively short follow up on some patients.
In conclusion, the UPAO test is a useful additional investigation to be considered in the pre-operative evaluation of pneumonectomy or pleuropneumonectomy for lung or pleural tumours and has a high technical success rate. Careful procedure technique is required to avoid major complications.
Contributor Information
Masashi Shimohira, Email: mshimohira@gmail.com.
Takuya Hashizume, Email: tky300@gmail.com.
Kengo Ohta, Email: yesterday.is.yesterday@gmail.com.
Motoo Nakagawa, Email: lmloltlolol@gmail.com.
Satoru Moriyama, Email: morihige@med.nagoya-cu.ac.jp.
Ryoichi Nakanishi, Email: ryoichi@med.nagoya-cu.ac.jp.
Yuta Shibamoto, Email: yshiba@med.nagoya-cu.ac.jp.
References
- 1.Deslauriers J, Ginsberg RJ, Dubois P, Beaulieu M, Goldberg M, Piraux M. Current operative morbidity associated with elective surgical resection for lung cancer. Can J Surg 1989; 32: 335–9. [PubMed] [Google Scholar]
- 2.Harpole DH, DeCamp MM, Daley J, Hur K, Oprian CA, Henderson WG, et al. Prognostic models of thirty-day mortality and morbidity after major pulmonary resection. J Thorac Cardiovasc Surg 1999; 117: 969–79. [DOI] [PubMed] [Google Scholar]
- 3.Carlens E, Hanson HE, Nordenstrom B. Temporary unilateral occlusion of the pulmonary artery; a new method of determining separate lung function and of radiologic examinations. J Thorac Surg 1951; 22: 527–36. [PubMed] [Google Scholar]
- 4.Ikeda T, Onuki T, Nishiuchi M, Kanzaki M, Nitta S. Clinical assessment of unilateral pulmonary artery occlusion test with dobutamine infusion. Expansion of surgical indications in patients with primary lung cancer and impaired cardiopulmonary functions. Jpn J Thorac Cardiovasc Surg 2000; 48: 802–8. [DOI] [PubMed] [Google Scholar]
- 5.Nagamatsu Y, Ohkita A, Kimura NY, Nakayama G, Hayashida R, Yamana H, et al. Retrospective investigation of pulmonary resection in patients with high total pulmonary vascular resistance during preoperative unilateral pulmonary artery occlusion. Gen Thorac Cardiovasc Surg 2009; 57: 244–9. [DOI] [PubMed] [Google Scholar]
- 6.Tanita T, Tomoyasu M, Deguchi H, Mizuno M, Kawazoe K. Review of preoperative functional evaluation for lung resection using the right ventricular hemodynamic functions. Ann Thorac Cardiovasc Surg 2004; 10: 333–9. [PubMed] [Google Scholar]
- 7.Hayashi A, Takamori S, Mitsuoka M, Miwa K, Fukunaga M, Matono K, et al. The UPAO test in preoperative evaluation for major pulmonary resection: an operative case with markedly improved ventilatory function after radical pulmonary resection for lung cancer associated with pulmonary emphysema. Ann Thorac Cardiovasc Surg 2002; 8: 154–9. [PubMed] [Google Scholar]
- 8.Stringham R, Shah NR. Pulmonary arterial hypertension: an update on diagnosis and treatment. Am Fam Physician 2010; 82: 370–7. [PubMed] [Google Scholar]
- 9.Zhang Z, Wang M, Yang Z, Yang F, Li D, Yu T, et al. Noninvasive prediction of pulmonary artery pressure and vascular resistance by using cardiac magnetic resonance indices. Int J Cardiol 2017; 227: 915–22. [DOI] [PubMed] [Google Scholar]
- 10.Swift AJ, Rajaram S, Hurdman J, Hill C, Davies C, Sproson TW, et al. Noninvasive estimation of PA pressure, flow, and resistance with CMR imaging: derivation and prospective validation study from the ASPIRE registry. JACC Cardiovasc Imaging 2013; 6: 103647. [DOI] [PubMed] [Google Scholar]
- 11.Reiter U, Reiter G, Fuchsjäger M. MR phase-contrast imaging in pulmonary hypertension. Br J Radiol 2016; 89: 20150995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Junqueira FP, Lima CM, Coutinho AC, Parente DB, Bittencourt LK, Bessa LG, et al. Pulmonary arterial hypertension: an imaging review comparing MR pulmonary angiography and perfusion with multidetector CT angiography. Br J Radiol 2012; 85: 1446–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wei B, D'Amico T, Samad Z, Hasan R, Berry MF. The impact of pulmonary hypertension on morbidity and mortality following major lung resection. Eur J Cardiothorac Surg 2014; 45: 1028–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kobayashi R, Nogimura H, Suzuki K, Harada Y, Horiguchi T, Sugimura H. A case of the pulmonary thrombosis caused by unilateral pulmonary artery occulusion test. Jpn J Thorac Cardiovasc Surg 1998; 46: 491–5. [DOI] [PubMed] [Google Scholar]
- 15.Ferretti GR, Thony F, Link KM, Durand M, Wollschläger K, Blin D, et al. False aneurysm of the pulmonary artery induced by a Swan-Ganz catheter: clinical presentation and radiologic management. AJR Am J Roentgenol 1996; 167: 941–5. [DOI] [PubMed] [Google Scholar]
- 16.Burrel M, Real MI, Barrufet M, Arguis P, Sánchez M, Berrocal L, et al. Pulmonary artery pseudoaneurysm after Swan-Ganz catheter placement: embolization with vascular plugs. J Vasc Interv Radiol 2010; 21: 577–81. [DOI] [PubMed] [Google Scholar]
- 17.Rudziński PN, Henzel J, Dzielińska Z, Lubiszewska BM, Michałowska I, Szymański P, et al. Pulmonary artery rupture as a complication of Swan-Ganz catheter application. Diagnosis and endovascular treatment: a single centre’s experience. Postepy Kardiol Interwencyjnej 2016; 12: 135–9. [DOI] [PMC free article] [PubMed] [Google Scholar]


