Hypertrophic pyloric stenosis (HPS) and esophageal achalasia are conditions in which abnormal functioning of the sphincters of the digestive tract lead to impaired transition of luminal contents. Both conditions can have the same cause, such as inhibition of nitric oxide synthase.1 However, there are few reports of HPS associated with esophageal achalasia.1, 2, 3
A 47-year-old woman presented because of progressive dysphagia and postprandial vomiting for 3 months. She received a radiographic diagnosis of esophageal achalasia with typical findings, including the absence of a gastric air bubble. Endoscopy demonstrated narrowing of the lower esophagus and the pyloric ring. Retrospectively, the gastric symptoms seemed to be masked with achalasia. The patient underwent laparoscopic Heller myotomy for achalasia. However, she had panperitonitis and a significantly distended stomach. An urgent operation revealed a 20-mm tear on the stomach at a site sutured for fundoplication.
To release the gastric outlet obstruction, endoscopic pyloroplasty was performed (Video 1, available online at www.VideoGIE.org). The stenosis was approximately 30-mm long in the antrum and was more significant in the lesser curvature involving the pyloric ring (Fig. 1). The procedure was initiated by an incision of the lesser curvature of the stenotic site with a needle-knife (DualKnife; Olympus Medical Systems, Tokyo, Japan) (Fig. 2). After dissecting the mucosal and submucosal layers, we identified the abnormally thickened muscularis, which seemed to be responsible for the outlet obstruction (Fig. 3). Repeated incisions were made into the hypertrophic muscularis tissues, parallel to the axis of the stomach (Fig. 4). The incisions were lengthened and deepened up to the level of the surrounding mucosal surface. Then, balloon dilation was added to ensure dilation of the pyloric ring (18-mm CRE fixed wire; Boston Scientific, Natick, Mass) (Figure 5, Figure 6). Mainly to prevent the recurrence of stenosis, the mucosal edges of the longitudinal incision were transversely approximated by placement of 7 hemoclips (QuickClip Pro and HX-610-090L; Olympus Medical Systems) (Fig. 7). Finally, 80 mg of triamcinolone was injected into the submucosa around the wound.
Figure 1.
Pyloric stenosis, “cervix sign.”
Figure 2.
Incision of the lesser curvature of the stenotic site.
Figure 3.
Exposed abnormally thickened inner muscularis.
Figure 4.
Incision of the hypertrophic inner muscularis parallel to the axis of the stomach.
Figure 5.
Dilation of the incised pyloric ring with an 18-mm balloon.
Figure 6.
Full opening of the pyloric stenosis after incision and balloon dilation.
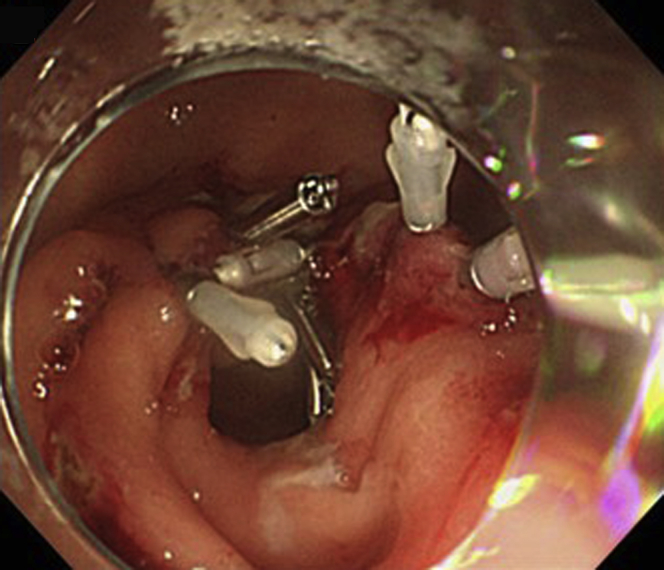
Figure 7.
Transverse closure of the longitudinal incision with hemoclips.
Follow-up endoscopy 1 month later revealed that the pylorus remained loosened, with a minor mucosal deformity (Fig. 8). The patient remained asymptomatic and gained weight during the follow-up period.
Figure 8.
Follow-up endoscopic view at 1 month showing that the pylorus remained loosened, with a minor mucosal deformity.
The endoscopic pyloroplasty technique described here may become a less-invasive therapeutic alternative to surgery for adult patients with HPS.
Disclosure
All authors disclosed no financial relationships relevant to this publication.
Footnotes
Written transcript of the video audio is available online at www.VideoGIE.org.
Supplementary data
Endoscopic pyloroplasty technique for the treatment of adult hypertrophic pyloric stenosis in a 47-year-old woman.
References
- 1.Castro A., Mearin F., Gil-Vernet J.M. Infantile hypertrophic pyloric stenosis and achalasia: NO-related or non-related conditions? Digestion. 1997;58:596–598. doi: 10.1159/000201508. [DOI] [PubMed] [Google Scholar]
- 2.Blades B., Adkins P.C., Gwathmey O. Combined surgical treatment of achalasia of the esophagus and hypertrophic pyloric stenosis; report of a case. Med Ann Dist Columbia. 1957;26:180–182. [PubMed] [Google Scholar]
- 3.Cataliotti F., LiVoti G., Di Pace M.R. Esophageal achalasia and hypertrophic pyloric stenosis associated with a phytobezoar in an adolescent. J Pediatr Surg. 2002;37:1363–1364. doi: 10.1053/jpsu.2002.35017. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Endoscopic pyloroplasty technique for the treatment of adult hypertrophic pyloric stenosis in a 47-year-old woman.